The Effects of Complementary Therapies on Patient-Reported Outcomes: An Overview of Recent Systematic Reviews in Oncology
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
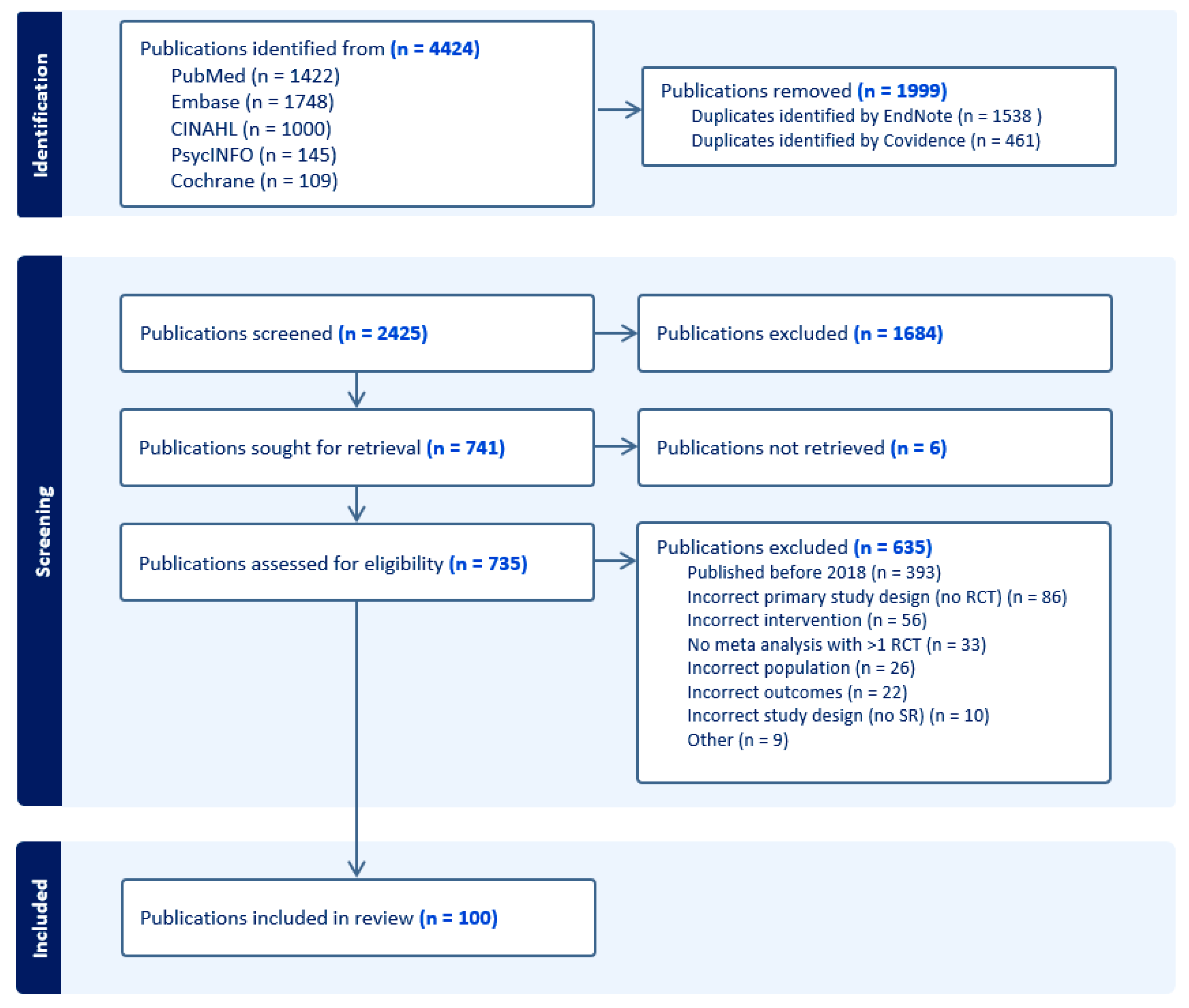
2.1. Search Strategy
2.2. Study Selection
2.3. Data Selection
2.4. Data Extraction
- Descriptive characteristics of the systematic reviews and the included primary studies (author, year, aim, participants, intervention, comparator, outcomes, outcome measures, number of primary studies (RCTs), number of participants in the RCTs).
- Quantitative outcome data (meta-analysis effect sizes of the eligible outcome–intervention combinations) and the overall conclusion.
2.5. Data Synthesis
2.6. Quality Appraisal
3. Results
3.1. Study Characteristics
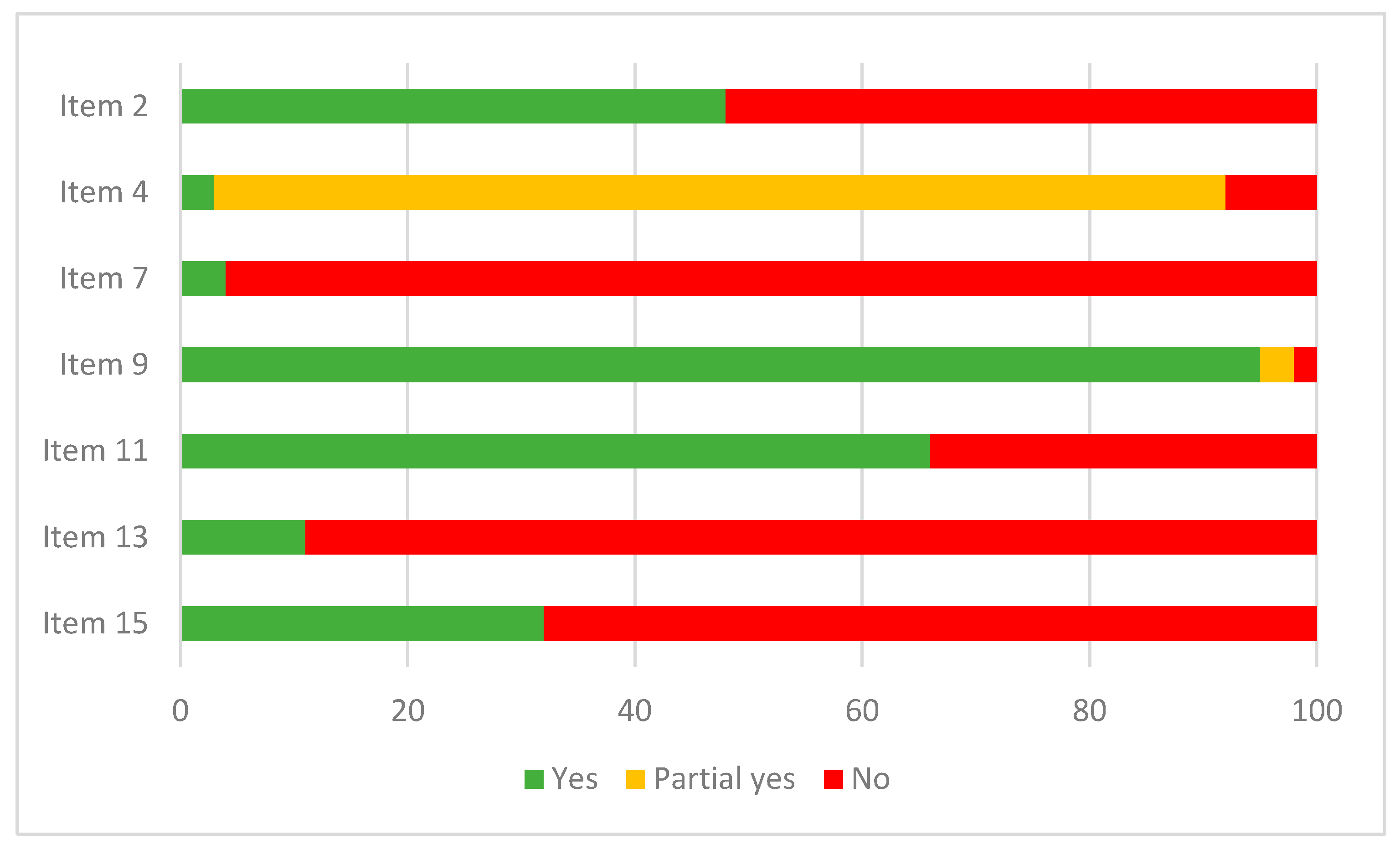
3.2. Methodological Quality
3.3. Efficacy of Complementary Therapies
3.3.1. Acupuncture
| Author and Year | Population | Pain | Neuropathy | Gastrointestinal Symptoms | Fatigue | Hot Flash Frequency | Menopausal Symptoms | Sleep Disturbance | Quality of Life |
|---|---|---|---|---|---|---|---|---|---|
| Chan 2021 [23] | Breast | 4 * 1 | 2 * | 6 * | 9 * | ||||
| Chien 2020 [31] | Breast | 4 | 5 * | ||||||
| Gao 2021 [24] | Breast | 2 * | |||||||
| Jang 2020—2 [32] | Breast | 3 | 3 | ||||||
| Kannan 2022 [25] | Breast | 2 * | |||||||
| Li 2021—1 [30] | Breast | 3 * 2 | 4 * 2 | 3 | 2 | ||||
| Liu 2020 [37] | Breast | 3 | |||||||
| Liu 2021 [22] | Breast | 3 * 1 | |||||||
| Wang 2018 [29] | Breast | 3 * 3 | |||||||
| Yuanqing 2020 [28] | Breast | 5 * | 5 | 4 * | 7 * | 3 | 8 | ||
| Zhang 2021 [27] | Breast | 4 * | 2 | 6 * | 4 | 4 * | 2 * | ||
| Zhu 2021 [33] | Breast | 4 * | 2 | ||||||
| Chien 2019 [26] | Mixed | 3 * | 4 * | ||||||
| Dai 2021 [38] | Mixed | 7 * | |||||||
| Dong 2021 [39] | Mixed | 12 * | |||||||
| He 2020 [40] | Mixed | 7 * | |||||||
| Hou 2020 [35] | Mixed | 18 * | |||||||
| Jang 2020—1 [41] | Mixed | 4 * | |||||||
| Jin 2020 [19] | Mixed | 4 * | 3 * | ||||||
| Li 2021—2 [17] | Mixed | 18 * | |||||||
| Lin 2019 [42] | Mixed | 3 | |||||||
| Tan 2021 [43] | Mixed | 2 | |||||||
| Zhang 2018 [44] | Mixed | 5 * |
3.3.2. Acupressure
3.3.3. Moxibustion
3.3.4. Herbal Medicine
| Author and Year | Population | Gastrointestinal Symptoms | Diarrhea | Nausea and Vomiting | Sleep Quality | Fatigue | Pain | Neuropathy | Functional Status | Quality of Life |
|---|---|---|---|---|---|---|---|---|---|---|
| Bai 2022 [69] | Breast | 5 * | 12 * | |||||||
| Li 2020 [54] | Breast | 4 * | 28 * 1 | |||||||
| Li 2021 [68] | Breast | 3 * | 4 * | 4 * | ||||||
| Shi 2021 [70] | Breast | 9 * | 6 * | |||||||
| Chen 2021 [55] | Colorectal | 20 * 2 | 13 * | 17 * | ||||||
| Liu 2019 [66] | Colorectal | 9 * | ||||||||
| Li 2020 [56] | Gastric | 8 * | 4 * | |||||||
| She 2021 [57] | Liver | 7 * | 11 * | |||||||
| Chen 2020 [71] | Lung | 14 * | 9 * | |||||||
| Jin 2021 [58] | Lung | 5 * | ||||||||
| Kwon 2021 [72] | Lung | 5 * | 2 * | |||||||
| Lu 2021 [62] | Lung | 8 * | 2 * | |||||||
| Wang 2020 [73] | Lung | 4 * | ||||||||
| Yang 2020 [59] | Lung | 3 * | 9 * | 5 * | ||||||
| Zhang 2018 [60] | Lung | 15 * | 3 * | 3 * | 28 * | |||||
| Chen 2019 [63] | Mixed | |||||||||
| Deng 2018 [65] | Mixed | 8 * | 4 * | |||||||
| Huang 2020 [74] | Mixed | 8 * 3 | 4 * | |||||||
| Li 2019 [75] | Mixed | 15 * | ||||||||
| Lin 2019 [42] | Mixed | 4 * | ||||||||
| Wang 2021 [76] | Mixed | 14 * | 7 * | |||||||
| Wu 2019 [77] | Mixed | 2 | 4 * | |||||||
| Yoon 2021 [78] | Mixed | 6 * | ||||||||
| Zhao 2020 [79] | Mixed | 10 * | ||||||||
| Wang 2019 [61] | Ovarian | 2 | 7 * | 3 | 9 * | 3 * | ||||
| Hu 2022 [64] | Pancreatic | 5 * | 5 | 4 * | 9 * |
3.3.5. Mindfulness-Based Stress Reduction (MBSR)
3.3.6. Music Interventions
3.3.7. Tai Chi
3.3.8. Qigong
3.3.9. Yoga
3.3.10. Art Therapy
3.3.11. Manual Therapy
3.3.12. Relaxation Therapy
3.4. Safety of Complementary Therapies
4. Discussion
4.1. Limitations
4.2. Applications
4.3. Future Studies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kemppainen, L.M.; Kemppainen, T.T.; Reippainen, J.A.; Salmenniemi, S.T.; Vuolanto, P.H. Use of complementary and alternative medicine in Europe: Health-related and sociodemographic determinants. Scand. J. Public Health 2018, 46, 448–455. [Google Scholar] [CrossRef]
- Kim, D.; Sung, S.H.; Shin, S.; Park, M. The effect of cancer on traditional, complementary and alternative medicine utilization in Korea: A fixed effect analysis using Korea Health Panel data. BMC Complement. Med. 2022, 22, 137. [Google Scholar] [CrossRef] [PubMed]
- Keene, M.R.; Heslop, I.M.; Sabesan, S.S.; Glass, B.D. Complementary and alternative medicine use in cancer: A systematic review. Complement. Ther. Clin. Pract. 2019, 35, 33–47. [Google Scholar] [CrossRef] [PubMed]
- King, N.; Balneaves, L.G.; Levin, G.T.; Nguyen, T.; Nation, J.G.; Card, C.; Truant, T.; Carlson, L.E. Surveys of cancer patients and cancer health care providers regarding complementary therapy use, communication, and information needs. Integr. Cancer Ther. 2015, 14, 515–524. [Google Scholar] [CrossRef]
- Uslu-Sahan, F.; Yesilcınar, I.; Kurt, G.; Hancer, E.; Guvenc, G. Effects of COVID-19 fear and anxiety on attitudes towards complementary and alternative medicine use in women with gynecological cancer during the COVID-19 pandemic. J. Integr. Med. 2023, 4, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Huebner, J.; Muenstedt, K.; Prott, F.J.; Stoll, C.; Micke, O.; Buentzel, J.; Muecke, R.; Senf, B. Online survey of patients with breast cancer on complementary and alternative medicine. Breast Care 2014, 9, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Davis, E.L.; Oh, B.; Butow, P.N.; Mullan, B.A.; Clarke, S. Cancer patient disclosure and patient-doctor communication of complementary and alternative medicine use: A systematic review. Oncologist 2012, 17, 1475. [Google Scholar] [CrossRef]
- Foley, H.; Steel, A.; Cramer, H.; Wardle, J.; Adams, J. Disclosure of complementary medicine use to medical providers: A systematic review and meta-analysis. Sci. Rep. 2019, 9, 1573. [Google Scholar] [CrossRef]
- Roter, D.L.; Yost, K.J.; O’Byrne, T.; Branda, M.; Leppin, A.; Kimball, B.; Fernandez, C.; Jatoi, A.; Kumbamu, A.; Montori, V. Communication predictors and consequences of Complementary and Alternative Medicine (CAM) discussions in oncology visits. Patient Educ. Couns. 2016, 99, 1519–1525. [Google Scholar] [CrossRef]
- Mazzocco, K.; Milani, A.; Ciccarelli, C.; Marzorati, C.; Pravettoni, G. Evidence for Choosing Qigong as an Integrated Intervention in Cancer Care: An Umbrella Review. Cancers 2023, 15, 1176. [Google Scholar] [CrossRef]
- Belloni, S.; Bonucci, M.; Arrigoni, C.; Dellafiore, F.; Caruso, R. A Systematic Review of Systematic Reviews and a Pooled Meta-Analysis on Complementary and Integrative Medicine for Improving Cancer-Related Fatigue. Clin. Ther. 2022, 45, e54–e73. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Gong, T.-T.; Xia, Y.; Wen, Z.-Y.; Zhao, L.-G.; Zhao, Y.-H.; Wu, Q.-J. Diet and ovarian cancer risk: An umbrella review of systematic reviews and meta-analyses of cohort studies. Clin. Nutr. 2021, 40, 1682–1690. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Mentink, M.; Noordman, J.; Busch, M.; van Vliet, L.; Timmer-Bonte, J.A.; van Dulmen, S. Towards an open and effective dialogue on complementary medicine in oncology: Protocol of patient participatory study ‘COMMON’. BMJ Open 2021, 11, e053005. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Choi, H.C.; Hyun, M.K. An Overview of Systematic Reviews: Complementary Therapies for Cancer Patients. Integr. Cancer Ther. 2019, 18, 1534735419890029. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Li, D.-H.; Su, Y.-F.; Fan, H.-F.; Guo, N.; Sun, C.-X. Acupuncture combined with three-step analgesic drug therapy for treatment of cancer pain: A systematic review and meta-analysis of randomised clinical trials. Evid. Based Complement. Alternat. Med. 2021, 2021, 5558590. [Google Scholar] [CrossRef]
- National Cancer Institute. Dictionary of Cancer Terms. Available online: https://www.cancer.gov/search/results?swKeyword=acupuncture (accessed on 8 May 2023).
- Jin, Y.; Wang, Y.; Zhang, J.; Xiao, X.; Zhang, Q. Efficacy and safety of acupuncture against chemotherapy-induced peripheral neuropathy: A systematic review and meta-analysis. Evid. Based Complement. Alternat. Med. 2020, 2020, 8875433. [Google Scholar] [CrossRef] [PubMed]
- Medicine, N.L.o. Medical Subject Headings (MeSH). Available online: https://www.ncbi.nlm.nih.gov/mesh/ (accessed on 8 May 2023).
- Kabat-Zinn, J.; Hanh, T.N. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness; Delta: Atlanta, GA, USA, 2009. [Google Scholar]
- Liu, X.; Lu, J.; Wang, G.; Chen, X.; Xv, H.; Huang, J.; Xue, M.; Tang, J. Acupuncture for arthralgia induced by aromatase inhibitors in patients with breast cancer: A systematic review and meta-analysis. Integr. Cancer Ther. 2021, 20, 1534735420980811. [Google Scholar] [CrossRef]
- Chan, Y.-T.; Wang, N.; Tam, C.-W.; Tan, H.-Y.; Lu, Y.; So, T.-h.; Chau-Leung Yu, E.; Lao, L.; Feng, Y. Systematic Review with Meta-Analysis: Effectiveness and Safety of Acupuncture as Adjuvant Therapy for Side Effects Management in Drug Therapy-Receiving Breast Cancer Patients. Evid. Based Complement. Alternat. Med. 2021, 2021, 9949777. [Google Scholar] [CrossRef]
- Gao, Y.; Ma, T.; Han, M.; Yu, M.; Wang, X.; Lv, Y.; Wang, X. Effects of Acupuncture and Moxibustion on Breast Cancer-Related Lymphedema: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Integr. Cancer Ther. 2021, 20, 15347354211044107. [Google Scholar] [CrossRef]
- Kannan, P.; Lam, H.Y.; Ma, T.K.; Lo, C.N.; Mui, T.Y.; Tang, W.Y. Efficacy of physical therapy interventions on quality of life and upper quadrant pain severity in women with post-mastectomy pain syndrome: A systematic review and meta-analysis. Qual. Life Res. 2022, 31, 951–973. [Google Scholar] [CrossRef] [PubMed]
- Chien, T.-J.; Liu, C.-Y.; Fang, C.-J.; Kuo, C.-Y. The efficacy of acupuncture in chemotherapy-induced peripheral neuropathy: Systematic review and meta-analysis. Integr. Cancer Ther. 2019, 18, 1534735419886662. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Sun, Y.; Li, D.; Liu, X.; Fang, C.; Yang, C.; Luo, T.; Lu, H.; Li, H.; Zhang, H. Acupuncture for breast cancer: A systematic review and meta-analysis of patient-reported outcomes. Front. Oncol. 2021, 11, 646315. [Google Scholar] [CrossRef] [PubMed]
- Yuanqing, P.; Yong, T.; Haiqian, L.; Gen, C.; Shen, X.; Dong, J.; Qi, C.; Miaomiao, Q. Acupuncture for Hormone Therapy–Related Side Effects in Breast Cancer Patients: A GRADE-Assessed Systematic Review and Updated Meta-Analysis. Integr. Cancer Ther. 2020, 19, 1534735420940394. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-P.; Zhang, D.-J.; Wei, X.-D.; Wang, J.-P.; Zhang, D.-Z. Acupuncture for the relief of hot flashes in breast cancer patients: A systematic review and meta-analysis of randomized controlled trials and observational studies. J. Cancer Res. Ther. 2018, 14, S600–S608. [Google Scholar] [PubMed]
- Li, H.; Schlaeger, J.M.; Jang, M.K.; Lin, Y.; Park, C.; Liu, T.; Sun, M.; Doorenbos, A.Z. Acupuncture improves multiple treatment-related symptoms in breast cancer survivors: A systematic review and meta-analysis. J. Altern. Complement. Med. 2021, 27, 1084–1097. [Google Scholar] [CrossRef] [PubMed]
- Chien, T.-J.; Liu, C.-Y.; Fang, C.-J.; Kuo, C.-Y. The maintenance effect of acupuncture on breast cancer-related menopause symptoms: A systematic review. Climacteric 2020, 23, 130–139. [Google Scholar] [CrossRef]
- Jang, S.; Ko, Y.; Sasaki, Y.; Park, S.; Jo, J.; Kang, N.-H.; Yoo, E.-S.; Park, N.-C.; hee Cho, S.; Jang, H. Acupuncture as an adjuvant therapy for management of treatment-related symptoms in breast cancer patients: Systematic review and meta-analysis (PRISMA-compliant). Medicine 2020, 99, e21820. [Google Scholar] [CrossRef]
- Zhu, X.-Y.; Li, Z.; Chen, C.; Feng, R.-L.; Cheng, B.-R.; Liu, R.-Y.; Wang, R.-T.; Xu, L.; Wang, Y.; Tao, X. Physical therapies for psychosomatic symptoms and quality of life induced by aromatase inhibitors in breast cancer patients: A systematic review and meta-analysis. Front. Oncol. 2021, 11, 745280. [Google Scholar] [CrossRef]
- Ni, X.; Tian, T.; Chen, D.; Liu, L.; Li, X.; Li, F.; Liang, F.; Zhao, L. Acupuncture for radiation-induced xerostomia in cancer patients: A systematic review and meta-analysis. Integr. Cancer Ther. 2020, 19, 1534735420980825. [Google Scholar] [CrossRef]
- Hou, X.-B.; Chen, D.-D. Effectiveness and safety of acupuncture on cancer pain: A meta-analysis. TMR Integr. Med. 2020, 4, e20018. [Google Scholar] [CrossRef]
- Xu, G.; Lei, H.; Zhou, Y.; Huang, L.; Tian, H.; Zhou, Z.; Zhao, L.; Liang, F. Acupuncture for Quality of Life of Patients with Defecation Dysfunction after Sphincter Preserving Surgery for Rectal Cancer: A Systematic Review. Evid. Based Complement. Alternat. Med. 2021, 2021, 7858252. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Nie, G.; Li, Y.; Wen, Z.; Lu, L.; Xie, L.; Cao, D.; Lai, Y.; Yang, H. Nonhormonal hot flash management for breast cancer survivors: A systematic review and network meta-analysis. Evid. Based Complement. Alternat. Med. 2020, 2020, 4243175. [Google Scholar] [CrossRef] [PubMed]
- Dai, L.; Liu, Y.; Ji, G.; Xu, Y. Acupuncture and derived therapies for pain in palliative cancer management: Systematic review and meta-analysis based on single-arm and controlled trials. J. Palliat. Med. 2021, 24, 1078–1099. [Google Scholar] [CrossRef] [PubMed]
- Dong, B.; Lin, L.; Chen, Q.; Qi, Y.; Wang, F.; Qian, K.; Tian, L. Wrist-ankle acupuncture has a positive effect on cancer pain: A meta-analysis. BMC Complement. Med. 2021, 21, 24. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Guo, X.; May, B.H.; Zhang, A.L.; Liu, Y.; Lu, C.; Mao, J.J.; Xue, C.C.; Zhang, H. Clinical evidence for association of acupuncture and acupressure with improved cancer pain: A systematic review and meta-analysis. JAMA Oncol. 2020, 6, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Jang, A.; Brown, C.; Lamoury, G.; Morgia, M.; Boyle, F.; Marr, I.; Clarke, S.; Back, M.; Oh, B. The effects of acupuncture on cancer-related fatigue: Updated systematic review and meta-analysis. Integr. Cancer Ther. 2020, 19, 1534735420949679. [Google Scholar] [CrossRef]
- Lin, W.-F.; Zhong, M.-F.; Zhou, Q.-H.; Zhang, Y.-R.; Wang, H.; Zhao, Z.-H.; Cheng, B.-B.; Ling, C.-Q. Efficacy of complementary and integrative medicine on health-related quality of life in cancer patients: A systematic review and meta-analysis. Cancer Manag. Res. 2019, 11, 6663. [Google Scholar] [CrossRef]
- Tan, J.-Y.B.; Wang, T.; Kirshbaum, M.N.; Zhao, I.; Eliseeva, S.; Polotan, M.J.; Yao, L.-Q.; Huang, H.-Q.; Zheng, S.-L. Acupoint stimulation for cancer-related fatigue: A quantitative synthesis of randomised controlled trials. Complement. Ther. Clin. Pract. 2021, 45, 101490. [Google Scholar] [CrossRef]
- Zhang, Y.; Lin, L.; Li, H.; Hu, Y.; Tian, L. Effects of acupuncture on cancer-related fatigue: A meta-analysis. Support Care Cancer 2018, 26, 415–425. [Google Scholar] [CrossRef]
- Mai, Q.; Li, X.; Yang, D.; Zhang, X.; Peng, K.; Hao, Y. Effects of acupressure on cancer-related pain management: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Integr. Med. 2022, 51, 102120. [Google Scholar] [CrossRef]
- Chen, L.; Wu, X.; Chen, X.; Zhou, C. Efficacy of auricular acupressure in prevention and treatment of chemotherapy-induced nausea and vomiting in patients with cancer: A systematic review and meta-analysis. Evid. Based Complement. Alternat. Med. 2021, 2021, 8868720. [Google Scholar] [PubMed]
- Chen, C.-Y.; Lin, X.-X.; Wang, X. Efficacy of non-invasive auricular acupressure for treating constipation in leukemia patients undergoing chemotherapy: A systematic review. Complement. Med. Res. 2018, 25, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Jing, X.; Liu, J.; Wang, C.; Ji, M.; Chen, X.; Mei, Y.; rong Zhu, Q. Auricular acupressure is an alternative in treating constipation in leukemia patients undergoing chemotherapy: A systematic review and meta-analysis. Complement. Ther. Clin. Pract. 2018, 31, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, S.-H.; Wu, C.-R.; Romadlon, D.S.; Hasan, F.; Chen, P.-Y.; Chiu, H.-Y. The effect of acupressure on relieving cancer-related fatigue: A systematic review and meta-analysis of randomized controlled trials. Cancer Nurs. 2021, 44, E578–E588. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, J.; Jin, Y.; Zhang, Q. Auricular acupressure therapy for patients with cancer with sleep disturbance: A systematic review and meta-analysis. Evid. Based Complement. Alternat. Med. 2021, 2021, 3996101. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.-L.; Lou, L.-F.; Sun, Z.-H.; Lv, B.-L.; Yang, B. The effectiveness of moxibustion for cancer-related fatigue: An updated systematic review and meta-analysis. Eur. J. Integr. Med. 2019, 30, 100960. [Google Scholar]
- Yao, Z.; Xu, Z.; Xu, T.; Liu, X.; Xu, S.; Wan, C.; Zhou, X. Moxibustion for alleviating chemotherapy-induced gastrointestinal adverse effects: A systematic review of randomized controlled trials. Complement. Ther. Clin. Pract. 2022, 46, 101527. [Google Scholar] [CrossRef]
- Zhang, H.W.; Lin, Z.X.; Cheung, F.; Cho, W.C.S.; Tang, J.L. Moxibustion for alleviating side effects of chemotherapy or radiotherapy in people with cancer. Cochrane Database Syst. Rev. 2018, 11, CD010559. [Google Scholar]
- Li, S.; So, T.-h.; Tang, G.; Tan, H.-Y.; Wang, N.; Ng, B.F.L.; Chan, C.K.W.; Yu, E.C.-L.; Feng, Y. Chinese herbal medicine for reducing chemotherapy-associated side-effects in breast cancer patients: A systematic review and meta-analysis. Front. Oncol. 2020, 10, 599073. [Google Scholar] [CrossRef]
- Chen, Y.; Cheng, C.-s.; Tan, H.-Y.; Tam, C.W.; Wang, N.; Feng, Y. Efficacy of Herbal Medicines Intervention for Colorectal Cancer Patients with Chemotherapy-Induced Gastrointestinal Toxicity—A Systematic Review and Meta-Analysis. Front. Oncol. 2021, 11, 629132. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Sui, X.; Su, Z.; Yu, C.; Shi, X.; Johnson, N.L.; Chu, F.; Li, Y.; Li, K.; Ding, X. Meta-analysis of paclitaxel-based chemotherapy combined with traditional Chinese medicines for gastric cancer treatment. Front. Pharmacol. 2020, 11, 132. [Google Scholar] [CrossRef] [PubMed]
- She, Y.; Huang, Q.; Ye, Z.; Hu, Y.; Wu, M.; Qin, K.; Wei, A.; Yang, X.; Liu, Y.; Zhang, C. The therapeutic principle of combined strengthening Qi and eliminating pathogens in treating middle-advanced primary liver cancer: A systematic review and meta-analysis. Front. Pharmacol. 2021, 12, 714287. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; Park, S.B.; Yoon, J.-H.; Lee, J.Y.; Kim, E.H.; Yoon, S.W. Traditional herbal medicine combined with first-line platinum-based chemotherapy for advanced non-small-cell lung cancer: A PRISMA-compliant systematic review and meta-analysis. Medicine 2021, 100, e27163. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhu, X.; Yuan, P.; Liu, J.; Wang, B.; Wang, G. Efficacy of traditional Chinese Medicine combined with chemotherapy in patients with non-small cell lung cancer (NSCLC): A meta-analysis of randomized clinical trials. Support Care Cancer 2020, 28, 3571–3579. [Google Scholar]
- Zhang, X.-W.; Liu, W.; Jiang, H.-L.; Mao, B. Chinese herbal medicine for advanced non-small-cell lung cancer: A systematic review and meta-analysis. Am. J. Chin. Med. 2018, 46, 923–952. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Sun, Q.; Wang, F.; Liu, Y.; Li, X.; Chen, T.; Wu, X.; Tang, H.; Zhou, M.; Zhang, S. Efficacy and safety of Chinese herbal medicine on ovarian cancer after reduction surgery and adjuvant chemotherapy: A systematic review and meta-analysis. Front. Oncol. 2019, 9, 730. [Google Scholar] [CrossRef]
- Lu, Y.; Sun, C.; Jiao, L.; Liu, Y.; Gong, Y.; Xu, L. Chinese herbal medicine combined with first-generation EGFR-TKIs in treatment of advanced non-small cell lung cancer with EGFR sensitizing mutation: A systematic review and meta-analysis. Front. Pharmacol. 2021, 12, 698371. [Google Scholar]
- Chen, Z.-Q.; Li, Z.-Y.; Yang, C.-Z.; Lin, R.-T.; Lin, L.-Z.; Sun, L.-L. Chinese herbal medicine for epidermal growth factor receptor inhibitor-induced skin rash in patients with malignancy: An updated meta-analysis of 23 randomized controlled trials. Complement. Ther. Med. 2019, 47, 102167. [Google Scholar] [CrossRef]
- Hu, J.; Jiang, J.; Liu, R.; Cheng, M.; Zhu, G.; He, S.; Shi, B.; Zhao, Y.; He, Z.; Yu, H. Clinical efficacy and safety of traditional medicine preparations combined with chemotherapy for advanced pancreatic cancer: A systematic review and meta-analysis. Front. Oncol. 2022, 12, 828450. [Google Scholar] [CrossRef]
- Deng, B.; Sun, W. Herbal medicine for hand–foot syndrome induced by fluoropyrimidines: A systematic review and meta-analysis. Phytother. Res. 2018, 32, 1211–1228. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; May, B.H.; Zhang, A.L.; Guo, X.; Lu, C.; Xue, C.C.; Zhang, H. Integrative herbal medicine for chemotherapy-induced peripheral neuropathy and hand-foot syndrome in colorectal cancer: A systematic review and meta-analysis. Integr. Cancer Ther. 2019, 18, 1534735418817833. [Google Scholar] [PubMed]
- Li, M.; Chen, Z.; Liu, Z.; Zhang, N.; Liu, J.; Wang, H.; Wang, W.; Liang, Y.; Chen, J.; Liu, Z. Twelve Chinese herbal preparations for the treatment of depression or depressive symptoms in cancer patients: A systematic review and meta-analysis of randomized controlled trials. BMC Complement. Altern. Med. 2019, 19, 28. [Google Scholar] [CrossRef]
- Li, L.; Wang, R.; Zhang, A.; Wang, L.; Ge, Q.; Liu, Y.; Chen, T.; Wang, C.C.; Leung, P.C.; Sun, Q. Evidence on efficacy and safety of Chinese medicines combined western medicines treatment for breast cancer with endocrine therapy. Front. Oncol. 2021, 11, 661925. [Google Scholar] [PubMed]
- Bai, X.; Ta, N.; Gong, G.-H.; Zhang, B.; Wei, C.-X. Effects of integrated Chinese traditional medicine and conventional western medicine on the quality of life of breast cancer patients: A systematic review and meta-analysis. Evid. Based Complement. Alternat. Med. 2022, 2022, 3123878. [Google Scholar] [CrossRef] [PubMed]
- Shi, G.; Yu, D.; Wu, J.; Liu, Y.; Huang, R.; Zhang, C.S. A systematic review and meta-analysis of traditional Chinese medicine with chemotherapy in breast cancer. Gland Surg. 2021, 10, 1744. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Bao, Y.; Xu, J.; Zhang, X.; He, S.; Zhang, Z.; Qi, R.; Jiang, J.; Liu, R.; Guo, Q. Efficacy and safety of TCM combined with chemotherapy for SCLC: A systematic review and meta-analysis. J. Cancer Res. Clin. Oncol. 2020, 146, 2913–2935. [Google Scholar]
- Kwon, C.Y.; Lee, B.; Kong, M.; Lee, S.H.; Jung, H.J.; Kim, K.I.; Lee, B.J. Effectiveness and safety of herbal medicine for cancer-related fatigue in lung cancer survivors: A systematic review and meta-analysis. Phytother. Res. 2021, 35, 751–770. [Google Scholar]
- Wang, L.-C.; Chang, Y.-Y.; Lee, I.-C.; Kuo, H.-C.; Tsai, M.-Y. Systematic review and meta-analysis of Chinese herbal medicine as adjuvant treatment in advanced non-small cell lung cancer patients. Complement. Ther. Med. 2020, 52, 102472. [Google Scholar] [CrossRef]
- Huang, Z.; Zhang, Q.; Fan, Y.; Zhou, J.; Liang, M.; Deng, X.; Liang, J. Effect of traditional Chinese medicine injection on cancer-related fatigue: A meta-analysis based on existing evidence. Evid. Based Complement. Alternat. Med. 2020, 2020, 2456873. [Google Scholar] [CrossRef]
- Li, Z.; Jin, H.; Yan, Q.; Sun, L.; Wasan, H.S.; Shen, M.; Ruan, S. The method of activating blood and dredging collaterals for reducing chemotherapy-induced peripheral neuropathy: A systematic review and meta-analysis. Evid. Based Complement. Alternat. Med. 2019, 2019, 1029626. [Google Scholar] [PubMed]
- Wang, Y.-H.; Chang, J.-Y.; Feng, L. Effect of oral Chinese medicine combined with Western medicine on cancer pain: A meta-analysis. Chin. J. Integr. Med. 2021, 27, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Liu, Y.; Fang, C.; Zhao, L.; Lin, L.; Lu, L. Traditional Chinese medicine preparation combined therapy may improve chemotherapy efficacy: A systematic review and meta-analysis. Evid. Based Complement. Alternat. Med. 2019, 2019, 5015824. [Google Scholar] [PubMed]
- Yoon, J.-H.; Kim, E.H.; Park, S.B.; Lee, J.Y.; Yoon, S.W. Traditional herbal medicine for insomnia in patients with cancer: A systematic review and meta-analysis. Front. Pharmacol. 2021, 12, 753140. [Google Scholar] [PubMed]
- Yueyang, Z.; Sumei, W.; Jinhua, L.; Yushu, Z.; Wanyin, W.; Hann, S.S. Effectiveness and safety of traditional Chinese medical therapy for cancer-related fatigue: A systematic review and Meta-analysis of randomized controlled trials. J. Tradit. Chin. Med. 2020, 40, 738. [Google Scholar]
- Chang, Y.-C.; Yeh, T.-L.; Chang, Y.-M.; Hu, W.-Y. Short-term effects of randomized mindfulness-based intervention in female breast cancer survivors: A systematic review and meta-analysis. Cancer Nurs. 2021, 44, E703–E714. [Google Scholar] [CrossRef] [PubMed]
- Schell, L.K.; Monsef, I.; Wöckel, A.; Skoetz, N. Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst. Rev. 2019, 3, CD011518. [Google Scholar] [CrossRef]
- Lin, L.-Y.; Lin, L.-H.; Tzeng, G.-L.; Huang, Y.-H.; Tai, J.-F.; Chen, Y.-L.; Wu, C.-J.; Chen, P.-H.; Lin, P.-C.; Hung, P.-L. Effects of mindfulness-based therapy for cancer patients: A systematic review and meta-analysis. J. Clin. Psychol. Med. Settings 2022, 29, 432–445. [Google Scholar] [CrossRef]
- Xunlin, N.; Lau, Y.; Klainin-Yobas, P. The effectiveness of mindfulness-based interventions among cancer patients and survivors: A systematic review and meta-analysis. Support Care Cancer 2020, 28, 1563–1578. [Google Scholar]
- He, J.; Hou, J.-h.; Qi, J.; Zhang, T.; Wang, Y.-l.; Qian, M. Mindfulness ased stress reduction interventions for cancer related fatigue: A meta-analysis and systematic review. J. Natl. Med. Assoc. 2020, 112, 387–394. [Google Scholar]
- Suh, H.-W.; Jeong, H.Y.; Hong, S.; Kim, J.W.; Yoon, S.W.; Lee, J.Y.; Chung, S.-Y. The mindfulness-based stress reduction program for improving sleep quality in cancer survivors: A systematic review and meta-analysis. Complement. Ther. Med. 2021, 57, 102667. [Google Scholar]
- Xie, C.; Dong, B.; Wang, L.; Jing, X.; Wu, Y.; Lin, L.; Tian, L. Mindfulness-based stress reduction can alleviate cancer-related fatigue: A meta-analysis. J. Psychosom. Res. 2020, 130, 109916. [Google Scholar] [PubMed]
- Yang, T.; Wang, S.; Wang, R.; Wei, Y.; Kang, Y.; Liu, Y.; Zhang, C. Effectiveness of five-element music therapy in cancer patients: A systematic review and meta-analysis. Complement. Ther. Clin. Pract. 2021, 44, 101416. [Google Scholar] [CrossRef]
- Li, Y.; Xing, X.; Shi, X.; Yan, P.; Chen, Y.; Li, M.; Zhang, W.; Li, X.; Yang, K. The effectiveness of music therapy for patients with cancer: A systematic review and meta-analysis. J. Adv. Nurs. 2020, 76, 1111–1123. [Google Scholar] [PubMed]
- Bro, M.L.; Jespersen, K.V.; Hansen, J.B.; Vuust, P.; Abildgaard, N.; Gram, J.; Johansen, C. Kind of blue: A systematic review and meta-analysis of music interventions in cancer treatment. Psycho-Oncol. 2018, 27, 386–400. [Google Scholar]
- Yangöz, Ş.T.; Özer, Z. The effect of music intervention on patients with cancer-related pain: A systematic review and meta-analysis of randomized controlled trials. J. Adv. Nurs. 2019, 75, 3362–3373. [Google Scholar]
- Qi, Y.; Lin, L.; Dong, B.; Xu, E.; Bao, Z.; Qi, J.; Chen, X.; Tian, L. Music interventions can alleviate cancer-related fatigue: A metaanalysis. Support Care Cancer 2021, 29, 3461–3470. [Google Scholar]
- Liu, C.; Qin, M.; Zheng, X.; Chen, R.; Zhu, J. A meta-analysis: Intervention effect of mind-body exercise on relieving cancer-related fatigue in breast cancer patients. Evid. Based Complement. Alternat. Med. 2021, 2021, 9980940. [Google Scholar]
- Luo, X.-C.; Liu, J.; Fu, J.; Yin, H.-Y.; Shen, L.; Liu, M.-L.; Lan, L.; Ying, J.; Qiao, X.-L.; Tang, C.-Z. Effect of Tai Chi Chuan in breast cancer patients: A systematic review and meta-analysis. Front. Oncol. 2020, 10, 607. [Google Scholar] [CrossRef]
- Ni, X.; Chan, R.J.; Yates, P.; Hu, W.; Huang, X.; Lou, Y. The effects of Tai Chi on quality of life of cancer survivors: A systematic review and meta-analysis. Support Care Cancer 2019, 27, 3701–3716. [Google Scholar]
- Song, S.; Yu, J.; Ruan, Y.; Liu, X.; Xiu, L.; Yue, X. Ameliorative effects of Tai Chi on cancer-related fatigue: A meta-analysis of randomized controlled trials. Support Care Cancer 2018, 26, 2091–2102. [Google Scholar] [PubMed]
- Cai, Q.; Cai, S.-B.; Chen, J.-K.; Bai, X.-H.; Jing, C.-X.; Zhang, X.; Li, J.-Q. Tai Chi for anxiety and depression symptoms in cancer, stroke, heart failure, and chronic obstructive pulmonary disease: A systematic review and meta-analysis. Complement. Ther. Clin. Pract. 2022, 46, 101510. [Google Scholar] [PubMed]
- Liu, L.; Tan, H.; Yu, S.; Yin, H.; Baxter, G.D. The effectiveness of tai chi in breast cancer patients: A systematic review and meta-analysis. Complement. Ther. Clin. Pract. 2020, 38, 101078. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.-C.; Wang, C.-C.; Chang, W.-L.; Liao, T.-C.; Chen, P.-E.; Tung, T.-H. Clinical effects of Baduanjin Qigong exercise on cancer patients: A systematic review and meta-analysis on randomized controlled trials. Evid. Based Complement. Alternat. Med. 2021, 2021, 6651238. [Google Scholar] [PubMed]
- Wang, R.; Huang, X.; Wu, Y.; Sun, D. Efficacy of qigong exercise for treatment of fatigue: A systematic review and meta-analysis. Front. Med. 2021, 8, 684058. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Tang, L.; Dishman, R.K. The efficacy of Qigong practice for cancer-related fatigue: A systematic review and meta-analysis of randomized controlled trials. Ment. Health Phys. Act. 2020, 19, 100347. [Google Scholar]
- Armer, J.S.; Lutgendorf, S.K. The impact of yoga on fatigue in cancer survivorship: A meta-analysis. JNCI Cancer Spectr. 2020, 4, pkz098. [Google Scholar]
- Dong, B.; Xie, C.; Jing, X.; Lin, L.; Tian, L. Yoga has a solid effect on cancer-related fatigue in patients with breast cancer: A meta-analysis. Breast Cancer Res. Treat. 2019, 177, 5–16. [Google Scholar]
- Haussmann, A.; Schmidt, M.E.; Illmann, M.L.; Schröter, M.; Hielscher, T.; Cramer, H.; Maatouk, I.; Horneber, M.; Steindorf, K. Meta-analysis of randomized controlled trials on yoga, psychosocial, and mindfulness-based interventions for cancer-related fatigue: What intervention characteristics are related to higher efficacy? Cancers 2022, 14, 2016. [Google Scholar]
- Hsueh, E.-J.; Loh, E.-W.; Lin, J.J.-A.; Tam, K.-W. Effects of yoga on improving quality of life in patients with breast cancer: A meta-analysis of randomized controlled trials. Breast Cancer 2021, 28, 264–276. [Google Scholar]
- Song, J. The effectiveness of yoga on cancer-related fatigue: A systematic review and meta-analysis. Oncol. Nurs. Forum 2021, 48, 207–228. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, M.; Samaroo, D.; Lopez, C.; Tomlinson, G.; Santa Mina, D.; Sabiston, C.; Culos-Reed, N.; Alibhai, S.M. The effect of yoga interventions on cancer-related fatigue and quality of life for women with breast cancer: A systematic review and meta-analysis of randomized controlled trials. Integr. Cancer Ther. 2020, 19, 1534735420959882. [Google Scholar] [CrossRef] [PubMed]
- Yi, L.-J.; Tian, X.; Jin, Y.-F.; Luo, M.-J.; Jimenez-Herrera, M.F. Effects of yoga on health-related quality, physical health and psychological health in women with breast cancer receiving chemotherapy: A systematic review and meta-analysis. Ann. Palliat. Med. 2021, 10, 1961–1975. [Google Scholar] [PubMed]
- Coutiño-Escamilla, L.; Piña-Pozas, M.; Garces, A.T.; Gamboa-Loira, B.; López-Carrillo, L. Non-pharmacological therapies for depressive symptoms in breast cancer patients: Systematic review and meta-analysis of randomized clinical trials. Breast 2019, 44, 135–143. [Google Scholar] [PubMed]
- Gonzalez, M.; Pascoe, M.C.; Yang, G.; de Manincor, M.; Grant, S.; Lacey, J.; Firth, J.; Sarris, J. Yoga for depression and anxiety symptoms in people with cancer: A systematic review and meta-analysis. Psycho-Oncol. 2021, 30, 1196–1208. [Google Scholar] [CrossRef] [PubMed]
- Tang, M.-F.; Chiu, H.-Y.; Xu, X.; Kwok, J.Y.; Cheung, D.S.T.; Chen, C.-Y.; Lin, C.-C. Walking is more effective than yoga at reducing sleep disturbance in cancer patients: A systematic review and meta-analysis of randomized controlled trials. Sleep Med. Rev. 2019, 47, 1–8. [Google Scholar] [PubMed]
- Wang, W.-L.; Chen, K.-H.; Pan, Y.-C.; Yang, S.-N.; Chan, Y.-Y. The effect of yoga on sleep quality and insomnia in women with sleep problems: A systematic review and meta-analysis. BMC Psychiatry 2020, 20, 195. [Google Scholar]
- Zeng, Y.; Dong, J.; Huang, M.; Zhang, J.-e.; Zhang, X.; Xie, M.; Wefel, J.S. Nonpharmacological interventions for cancer-related cognitive impairment in adult cancer patients: A network meta-analysis. Int. J. Nurs. Stud. 2020, 104, 103514. [Google Scholar]
- El-Hashimi, D.; Gorey, K.M. Yoga-specific enhancement of quality of life among women with breast cancer: Systematic review and exploratory meta-analysis of randomized controlled trials. J. Evid. Based Integr. Med. 2019, 24, 2515690X19828325. [Google Scholar]
- Danon, N.; Al-Gobari, M.; Burnand, B.; Rodondi, P.Y. Are mind–body therapies effective for relieving cancer-related pain in adults? A systematic review and meta-analysis. Psycho-Oncol. 2022, 31, 345–371. [Google Scholar] [CrossRef]
- Lin, Y.; Yang, Y.; Zhang, X.; Li, W.; Li, H.; Mu, D. Manual lymphatic drainage for breast cancer-related lymphedema: A systematic review and meta-analysis of randomized controlled trials. Clin. Breast Cancer 2022, 22, e664–e673. [Google Scholar] [CrossRef]
- Qiao, J.; Yang, L.-N.; Kong, Y.-H.; Huang, X.; Li, Y.; Bai, D.-Q. Effect of Manual Lymphatic Drainage on Breast Cancer–Related Postmastectomy Lymphedema: A Meta-analysis of Randomized Controlled Trials. Cancer Nurs. 2023, 46, 159–166. [Google Scholar] [CrossRef] [PubMed]
- da Silva, F.P.; Moreira, G.M.; Zomkowski, K.; de Noronha, M.A.; Sperandio, F.F. Manual therapy as treatment for chronic musculoskeletal pain in female breast cancer survivors: A systematic review and meta-analysis. J. Manip. Physiol. Ther. 2019, 42, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Sinha, M.K.; Barman, A.; Goyal, M.; Patra, S. Progressive muscle relaxation and guided imagery in breast cancer: A systematic review and meta-analysis of randomised controlled trials. Indian. J. Palliat. Care 2021, 27, 336. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Wang, L.; Cai, Q.; Wu, J.; Zhou, C. Effect of hypnosis before general anesthesia on postoperative outcomes in patients undergoing minor surgery for breast cancer: A systematic review and meta-analysis. Gland Surg. 2022, 11, 588. [Google Scholar] [CrossRef]
- Mao, J.J.; Ismaila, N.; Bao, T.; Barton, D.; Ben-Arye, E.; Garland, E.L.; Greenlee, H.; Leblanc, T.; Lee, R.T.; Lopez, A.M. Integrative Medicine for Pain Management in Oncology: Society for Integrative Oncology–ASCO Guideline. J. Clin. Oncol. 2022, 40, 3998–4024. [Google Scholar] [CrossRef] [PubMed]
- Greenlee, H.; DuPont-Reyes, M.J.; Balneaves, L.G.; Carlson, L.E.; Cohen, M.R.; Deng, G.; Johnson, J.A.; Mumber, M.; Seely, D.; Zick, S.M. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA Cancer J. Clin. 2017, 67, 194–232. [Google Scholar] [CrossRef]
- Deng, G.E.; Rausch, S.M.; Jones, L.W.; Gulati, A.; Kumar, N.B.; Greenlee, H.; Pietanza, M.C.; Cassileth, B.R. Complementary therapies and integrative medicine in lung cancer: Diagnosis and management of lung cancer: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143, e420S–e436S. [Google Scholar] [CrossRef]
- Lyman, G.H.; Greenlee, H.; Bohlke, K.; Bao, T.; DeMichele, A.M.; Deng, G.E.; Fouladbakhsh, J.M.; Gil, B.; Hershman, D.L.; Mansfield, S. Integrative therapies during and after breast cancer treatment: ASCO endorsement of the SIO clinical practice guideline. J. Clin. Oncol. 2018, 36, 2647–2655. [Google Scholar] [CrossRef]
- Boyd, C.; Crawford, C.; Paat, C.F.; Price, A.; Xenakis, L.; Zhang, W.; Evidence for Massage Therapy Working Group; Buckenmaier, C., III; Jerrilyn, C.; Christopher, D.; et al. The impact of massage therapy on function in pain populations—A systematic review and meta-analysis of randomized controlled trials: Part II, cancer pain populations. Pain Med. 2016, 17, 1553–1568. [Google Scholar] [CrossRef]
- Lee, S.-H.; Kim, J.-Y.; Yeo, S.; Kim, S.-H.; Lim, S. Meta-analysis of massage therapy on cancer pain. Integr. Cancer Ther. 2015, 14, 297–304. [Google Scholar] [CrossRef]
- Cohen, M.H.; Eisenberg, D.M. Potential physician malpractice liability associated with complementary and integrative medical therapies. Ann. Intern. Med. 2002, 136, 596–603. [Google Scholar] [CrossRef]
- Balneaves, L.G.; Watling, C.Z.; Hayward, E.N.; Ross, B.; Taylor-Brown, J.; Porcino, A.; Truant, T.L. Addressing complementary and alternative medicine use among individuals with cancer: An integrative review and clinical practice guideline. J. Natl. Cancer Inst. 2022, 114, 25–37. [Google Scholar] [CrossRef]
| Complementary Therapy (No. Included Meta-Analyses) | Definition |
|---|---|
| Herbal medicine [17] | A type of medicine that uses roots, stems, leaves, flowers or seeds of plants [18] (we did not include meta-analyses assessing the effectivity of individual herbs) |
| Acupuncture [19] | The technique of inserting thin needles through the skin at specific points on the body (including electroacupuncture in which pulses of weak electrical current are sent through acupuncture needles into acupuncture points in the skin) [18] |
| Yoga [16] | An ancient system of practices used to balance the mind and body through exercise, meditation (focusing thoughts), and control of breathing and emotions [18] |
| Mindfulness-based stress reduction [7] | A moment-to-moment awareness of one’s experience without judgment and as a state and not a trait [20] (we included only mindfulness-based stress reduction (MBSR), a structured group program of mindfulness training [21]) |
| Acupressure [7] | The application of pressure or localized massage to specific sites on the body [18] (including ear acupressure in which seeds or pellets are taped on auricular acupoints) |
| Tai Chi [6] | One of the martial arts and also a form of meditative exercise using methodically slow circular stretching movements and positions of body balance [20] |
| Music interventions [5] | A type of therapy that uses music to help improve a person’s overall health and well-being [18] (we included passive and active listening music interventions) |
| Manual therapy [5] | A type of therapy in which the therapist moves or manipulates one or more parts of the patient’s body [18] |
| Qigong [4] | An ancient Chinese system of postures, exercises, breathing techniques and meditations designed to improve and enhance the body’s Qi (e.g., vital energy) [20] |
| Moxibustion [4] | A type of heat therapy in which a herb is burned on or above the skin to warm and stimulate an acupuncture point or affected area [18] |
| Relaxation therapy [2] | Treatment to improve one’s health condition by using techniques that can reduce physiological stress, psychological stress, or both [20] |
| Art therapy [1] | Treatment that uses the making of art and the response to art to improve one’s physical, mental and emotional well-being [18] |
| Author and Year | Population | Pain | Fatigue | Sleep Quality | Nausea and Vomiting | Constipation | Diarrhea | Quality of Life |
|---|---|---|---|---|---|---|---|---|
| Chen 2018 [47] a | Leukemia | 3 * | 2 * | |||||
| Jing 2018 [48] a | Leukemia | 3 * | 2 * | |||||
| Chen 2021 [46] a | Mixed | 2 * | 10 * | 6 * | 2 * | |||
| Hsieh 2021 [49] | Mixed | 14 * | ||||||
| Mai 2022 [45] | Mixed | 11 * | 7 * | 8 * | ||||
| Tan 2021 [43] | Mixed | 2 | ||||||
| Wang 2021 [50] a | Mixed | 6 * |
| Author and Year | Population | Fatigue | Nausea and Vomiting | Constipation | Diarrhea | Lymphedema (Swelling) | Functional Status | Quality of Life |
|---|---|---|---|---|---|---|---|---|
| Gao 2021 [24] | Breast | 3 * | ||||||
| Ma 2019 [51] | Mixed | 10 * | 9 * | |||||
| Yao 2022 [52] | Mixed | 24 * | 7 * | 7 * | 6 * | 2 * | ||
| Zhang 2018 [53] | Mixed | 7 * | 4 * | 3 * |
| Author and Year | Population | Anxiety | Depression | Stress | Fatigue | Sleep Quality | Pain | Quality of Life |
|---|---|---|---|---|---|---|---|---|
| Chang 2021 [80] | Breast | 3 | 6 * | 3 | 4 * | 5 | 5 | 4 |
| Schell 2019 [81] | Breast | 6 * | 6 * | 5 * | 4 * | |||
| He 2020 [84] | Mixed | 5 * | ||||||
| Lin 2022 [82] | Mixed | 14 * | 12 * | 8 * | 4 * | 7 * | ||
| Suh 2021 [85] | Mixed | 9 * 1 | ||||||
| Xie 2020 [86] | Mixed | 14 * | ||||||
| Xunlin 2020 [83] | Mixed | 9 * |
| Author and Year | Population | Depression | Anxiety | Mood | Distress | Pain | Sleep Quality | Fatigue | Functional Status | Quality of Life |
|---|---|---|---|---|---|---|---|---|---|---|
| Bro 2018 [89] | Mixed | 2 | 9 * | 4 * | 2 | 9 * | 3 | 2 | ||
| Li 2020 [88] | Mixed | 6 * | 6 * | 5 * | 10 * | |||||
| Qi 2021 [91] | Mixed | 8 * | ||||||||
| Yang 2021 [87] | Mixed | 14 * | 8 1 | 4 * | 3 * | 7 * | ||||
| Yangöz 2019 [90] | Mixed | 6 * |
| Author and Year | Population | Fatigue | Anxiety | Depression | Sleep Quality | Pain | Quality of Life |
|---|---|---|---|---|---|---|---|
| Liu 2021 [92] | Breast | 2 * | |||||
| Liu 2020 [97] | Breast | 2 1 | 3 | 2 | 2 * | ||
| Luo 2020 [93] | Breast | 3 * | 2 * | 4 * | 5 * | ||
| Cai 2022 [96] | Mixed | 2 * | 4 | ||||
| Ni 2019 [94] | Mixed | 3 * | 3 * | 8 * 2 | |||
| Song 2018 [95] | Mixed | 6 * 3 |
| Author and Year | Population | Fatigue | Sleep Quality | Quality of Life |
|---|---|---|---|---|
| Kuo 2021 [98] | Mixed | 5 * | 2 * | 3 * |
| Lin 2019 [42] | Mixed | 3 | ||
| Wang 2021 [99] | Mixed | 4 * | ||
| Yin 2020 [100] | Mixed | 13 * 1 |
| Author and Year | Population | Fatigue | Anxiety | Depression | Stress | Sleep Disturbance | Pain | Quality of Life |
|---|---|---|---|---|---|---|---|---|
| Coutiño 2019 [108] | Breast | 5 * | ||||||
| Dong 2019 [102] | Breast | 18 * | ||||||
| El-Hashimi 2019 [113] | Breast | 8 | ||||||
| Hsueh 2021 [104] | Breast | 14 * | 8 * | 12 * | 4 * | 5 * | 5 * | 5 * 1 |
| Liu 2021 [92] | Breast | 13 * | ||||||
| O’Neill 2020 [106] | Breast | 18 * 2 | 10 * 2 | |||||
| Wang 2020 [111] | Breast | 7 3 | ||||||
| Yi 2021 [107] | Breast | 4 * 4 | 5 * | 6 * | 2 * 4 | 3 * | ||
| Armer 2020 [101] | Mixed | 29 * 2 | 12 * 2 | 17 | ||||
| Danon 2021 [114] | Mixed | 7 | ||||||
| Gonzalez 2021 [109] | Mixed | 15 * | 25 * | |||||
| Haussmann 2022 [103] | Mixed | 24 * | ||||||
| Jihong 2021 [105] | Mixed | 11 * | ||||||
| Lin 2019 [42] | Mixed | 7 | ||||||
| Tang 2019 [110] | Mixed | 13 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mentink, M.; Verbeek, D.; Noordman, J.; Timmer-Bonte, A.; von Rosenstiel, I.; van Dulmen, S. The Effects of Complementary Therapies on Patient-Reported Outcomes: An Overview of Recent Systematic Reviews in Oncology. Cancers 2023, 15, 4513. https://doi.org/10.3390/cancers15184513
Mentink M, Verbeek D, Noordman J, Timmer-Bonte A, von Rosenstiel I, van Dulmen S. The Effects of Complementary Therapies on Patient-Reported Outcomes: An Overview of Recent Systematic Reviews in Oncology. Cancers. 2023; 15(18):4513. https://doi.org/10.3390/cancers15184513
Chicago/Turabian StyleMentink, Marit, Daniëlle Verbeek, Janneke Noordman, Anja Timmer-Bonte, Ines von Rosenstiel, and Sandra van Dulmen. 2023. "The Effects of Complementary Therapies on Patient-Reported Outcomes: An Overview of Recent Systematic Reviews in Oncology" Cancers 15, no. 18: 4513. https://doi.org/10.3390/cancers15184513
APA StyleMentink, M., Verbeek, D., Noordman, J., Timmer-Bonte, A., von Rosenstiel, I., & van Dulmen, S. (2023). The Effects of Complementary Therapies on Patient-Reported Outcomes: An Overview of Recent Systematic Reviews in Oncology. Cancers, 15(18), 4513. https://doi.org/10.3390/cancers15184513







