Survival Evidence of Local Control for Colorectal Cancer Liver Metastases by Hepatectomy and/or Radiofrequency Ablation
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
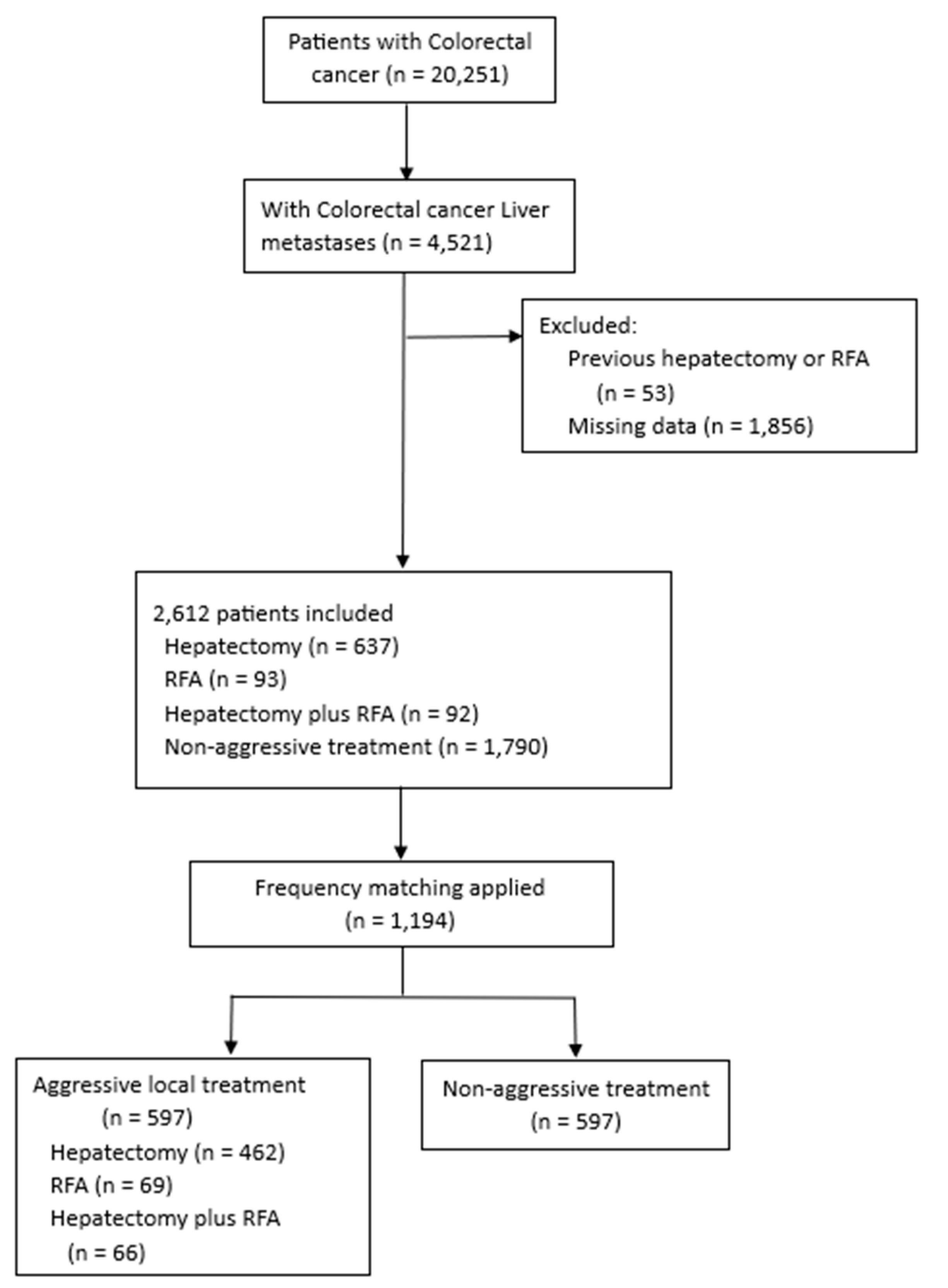
2.1. Patient Selection and Study Design
2.2. Frequency Matching Analysis
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
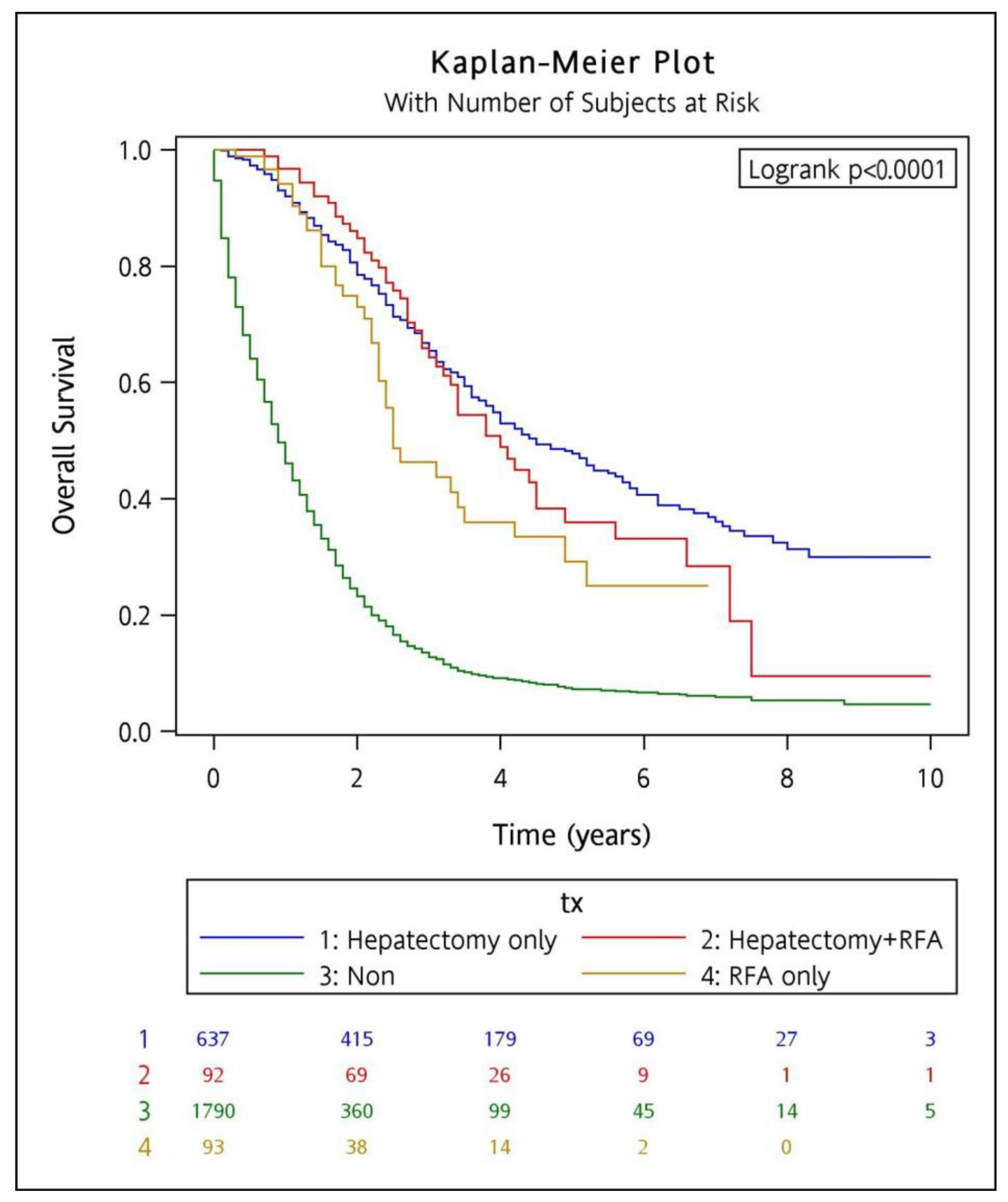
3.2. Survival Outcome and Its Associated Factors in the Entire Cohort
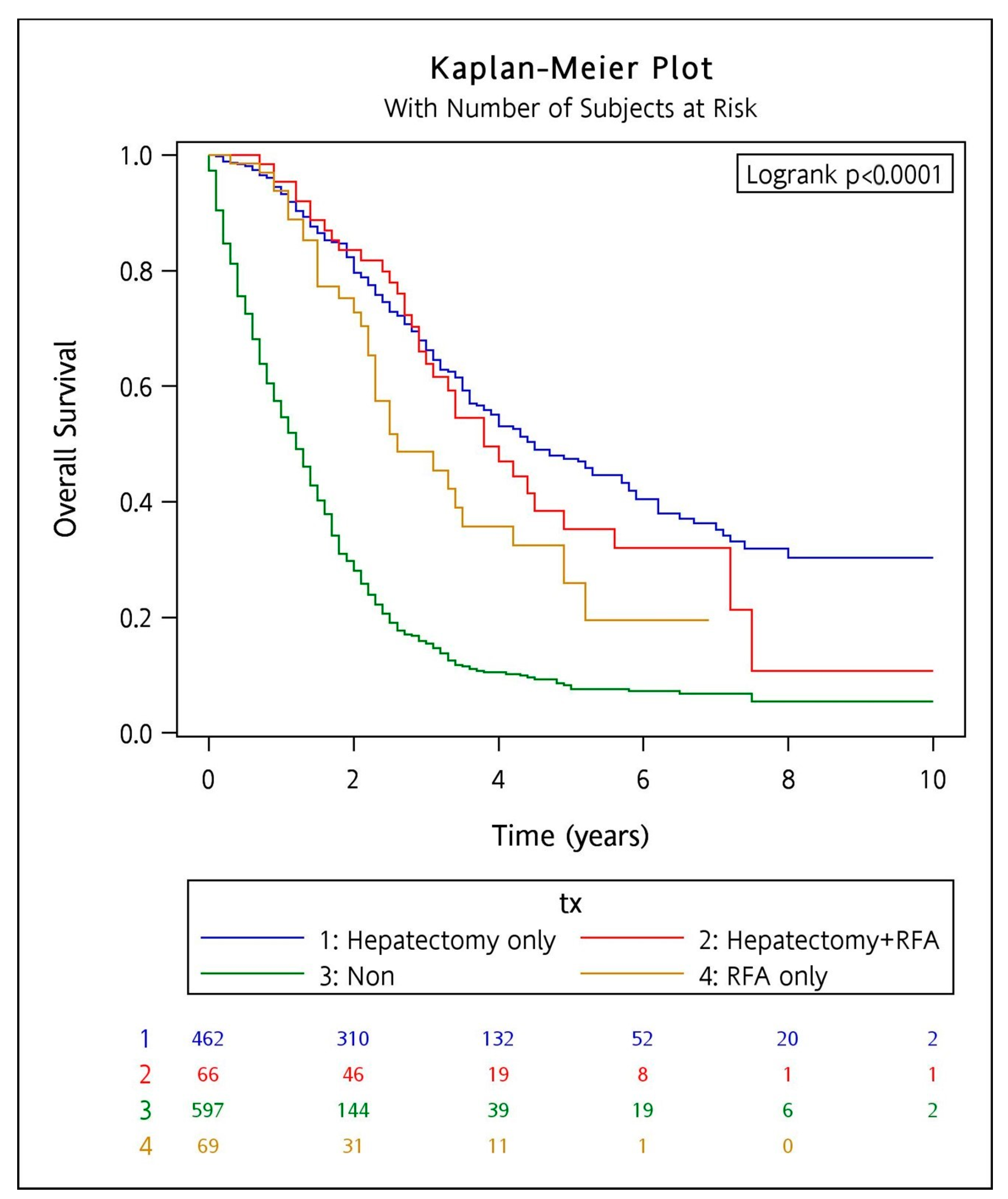
3.3. Survival Outcome in Frequency Matching Cohort
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization International Agency for Research on Cancer (IARC). GLOBOCAN 2020: Colorectal Cancer. Published December 2020. Available online: https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf (accessed on 2 June 2023).
- American Cancer Society. Colorectal Cancer Facts & Figures 2020–2022; American Cancer Society: Atlanta, GA, USA, 2020. [Google Scholar]
- Cervantes, A.; Adam, R.; Roselló, S.; Arnold, D.; Normanno, N.; Taïeb, J.; Seligmann, J.; De Baere, T.; Osterlund, P.; Yoshino, T.; et al. Metastatic colorectal cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2023, 34, 10–32. [Google Scholar] [CrossRef]
- Engstrand, J.; Nilsson, H.; Strömberg, C.; Jonas, E.; Freedman, J. Colorectal cancer liver metastases—A population-based study on incidence, management and survival. BMC Cancer 2018, 18, 78. [Google Scholar] [CrossRef] [PubMed]
- Cummings, L.C.; Payes, J.D.; Cooper, G.S. Survival after hepatic resection in metastatic colorectal cancer: A population-based study. Cancer 2007, 109, 718–726. [Google Scholar] [CrossRef]
- Manfredi, S.; Lepage, C.; Hatem, C.; Coatmeur, O.; Faivre, J.; Bouvier, A.M. Epidemiology and management of liver metastases from colorectal cancer. Ann. Surg. 2006, 244, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Väyrynen, V.; Wirta, E.V.; Seppälä, T.; Sihvo, E.; Mecklin, J.P.; Vasala, K.; Kellokumpu, I. Incidence and management of patients with colorectal cancer and synchronous and metachronous colorectal metastases: A population-based study. BJS Open 2020, 4, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Reboux, N.; Jooste, V.; Goungounga, J.; Robaszkiewicz, M.; Nousbaum, J.B.; Bouvier, A.M. Incidence and Survival in Synchronous and Metachronous Liver Metastases from Colorectal Cancer. JAMA Netw. Open 2022, 5, e2236666. [Google Scholar] [CrossRef]
- Park, J.H.; Kim, T.Y.; Lee, K.H.; Han, S.W.; Oh, D.Y.; Im, S.A.; Kang, G.H.; Chie, E.K.; Ha, S.W.; Jeong, S.Y.; et al. The beneficial effect of palliative resection in metastatic colorectal cancer. Br. J. Cancer 2013, 108, 1425–1431. [Google Scholar] [CrossRef]
- Gillams, A.; Goldberg, N.; Ahmed, M.; Bale, R.; Breen, D.; Callstrom, M.; Chen, M.H.; Choi, B.I.; de Baere, T.; Dupuy, D.; et al. Thermal ablation of colorectal liver metastases: A position paper by an international panel of ablation experts, The Interventional Oncology Sans Frontières meeting 2013. Eur. Radiol. 2015, 25, 3438–3454. [Google Scholar] [CrossRef]
- Luo, M.; Chen, S.L.; Chen, J.; Yan, H.; Qiu, Z.; Chen, G.; Lu, L.; Zhang, F. Resection vs. ablation for lesions characterized as resectable-ablative within the colorectal liver oligometastases criteria: A propensity score matching from retrospective study. PeerJ 2020, 8, e8398. [Google Scholar] [CrossRef]
- Wang, L.J.; Zhang, Z.Y.; Yan, X.L.; Yang, W.; Yan, K.; Xing, B.C. Radiofrequency ablation versus resection for technically resectable colorectal liver metastasis: A propensity score analysis. World J. Surg. Oncol. 2018, 16, 207. [Google Scholar] [CrossRef]
- Morris, V.K.; Kennedy, E.B.; Baxter, N.N.; Benson, A.B., 3rd; Cercek, A.; Cho, M.; Ciombor, K.K.; Cremolini, C.; Davis, A.; Deming, D.A.; et al. Treatment of Metastatic Colorectal Cancer: ASCO Guideline. J. Clin. Oncol. 2023, 41, 678–700. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, T.; Arnold, D.; Taniguchi, H.; Pentheroudakis, G.; Yamazaki, K.; Xu, R.H.; Kim, T.W.; Ismail, F.; Tan, I.B.; Yeh, K.H.; et al. Pan-Asian adapted ESMO consensus guidelines for the management of patients with metastatic colorectal cancer: A JSMO-ESMO initiative endorsed by CSCO, KACO, MOS, SSO and TOS. Ann. Oncol. 2018, 29, 44–70. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.H.; Ke, T.W.; Huang, C.W.; Jiang, J.K.; Chen, C.C.; Hsieh, Y.Y.; Teng, H.W.; Lin, B.W.; Liang, Y.H.; Su, Y.L.; et al. Taiwan Society of Colon and Rectal Surgeons Consensus on mCRC Treatment. Front. Oncol. 2021, 11, 764912. [Google Scholar] [CrossRef]
- Tsai, M.S.; Lin, M.H.; Lee, C.P.; Yang, Y.H.; Chen, W.C.; Chang, G.H.; Tsai, Y.T.; Chen, P.C.; Tsai, Y.H. Chang Gung Research Database: A multi-institutional database consisting of original medical records. Biomed. J. 2017, 40, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Berber, E.; Pelley, R.; Siperstein, A.E. Predictors of survival after radiofrequency thermal ablation of colorectal cancer metastases to the liver: A prospective study. J. Clin. Oncol. 2005, 23, 1358–1364. [Google Scholar] [CrossRef]
- Schindl, M.; Wigmore, S.J.; Currie, E.J.; Laengle, F.; Garden, O.J. Prognostic scoring in colorectal cancer liver metastases: Development and validation. Arch. Surg. 2005, 140, 183–189. [Google Scholar] [CrossRef]
- Bockhorn, M.; Frilling, A.; Frühauf, N.R.; Neuhaus, J.; Molmenti, E.; Trarbach, T.; Malagó, M.; Lang, H.; Broelsch, C.E. Survival of patients with synchronous and metachronous colorectal liver metastases—Is there a difference? J. Gastrointest. Surg. 2008, 12, 1399–1405. [Google Scholar] [CrossRef]
- Mao, R.; Zhao, J.J.; Bi, X.Y.; Zhang, Y.F.; Li, Z.Y.; Zhou, J.G.; Wu, X.L.; Xiao, C.; Zhao, H.; Cai, J.Q. A postoperative scoring system for post-hepatectomy early recurrence of colorectal liver metastases. Oncotarget 2017, 8, 102531–102539. [Google Scholar] [CrossRef]
- Fong, Y.; Fortner, J.; Sun, R.L.; Brennan, M.F.; Blumgart, L.H. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: Analysis of 1001 consecutive cases. Ann. Surg. 1999, 230, 309–321. [Google Scholar] [CrossRef]
- Nitsche, U.; Stögbauer, F.; Späth, C.; Haller, B.; Wilhelm, D.; Friess, H.; Bader, F.G. Right Sided Colon Cancer as a Distinct Histopathological Subtype with Reduced Prognosis. Dig. Surg. 2016, 33, 157–163. [Google Scholar] [CrossRef]
- Shen, H.; Yang, J.; Huang, Q.; Jiang, M.J.; Tan, Y.N.; Fu, J.F.; Zhu, L.Z.; Fang, X.F.; Yuan, Y. Different treatment strategies and molecular features between right-sided and left-sided colon cancers. World J. Gastroenterol. 2015, 21, 6470–6478. [Google Scholar] [CrossRef]
- Mekenkamp, L.J.; Koopman, M.; Teerenstra, S.; van Krieken, J.H.; Mol, L.; Nagtegaal, I.D.; Punt, C.J. Clinicopathological features and outcome in advanced colorectal cancer patients with synchronous vs metachronous metastases. Br. J. Cancer 2010, 103, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Quireze Junior, C.; Brasil, A.M.S.; Morais, L.K.; Campion, E.R.L.; Taveira, E.J.F.; Rassi, M.C. Metachronous Colorectal Liver Metastases has better Prognosis—Is it true? Arq. Gastroenterol. 2018, 55, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Ruers, T.; Van Coevorden, F.; Punt, C.J.; Pierie, J.E.; Borel-Rinkes, I.; Ledermann, J.A.; Poston, G.; Bechstein, W.; Lentz, M.A.; Mauer, M.; et al. Local Treatment of Unresectable Colorectal Liver Metastases: Results of a Randomized Phase II Trial. J. Natl. Cancer Inst. 2017, 109, djx015. [Google Scholar] [CrossRef] [PubMed]
- Chiappa, A.; Bertani, E.; Zbar, A.P.; Foschi, D.; Fazio, N.; Zampino, M.; Belluco, C.; Orsi, F.; Della Vigna, P.; Bonomo, G.; et al. Optimizing treatment of hepatic metastases from colorectal cancer: Resection or resection plus ablation? Int. J. Oncol. 2016, 48, 1280–1289. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Variable | Hepatectomy + RFA | Hepatectomy | RFA | Non-Aggressive | p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Total | 92 | 637 | 93 | 1790 | |||||
| Gender | 0.757 | ||||||||
| Female | 34 | (37.0) | 252 | (39.6) | 33 | (35.5) | 720 | (40.2) | |
| Male | 58 | (63.0) | 385 | (60.4) | 60 | (64.5) | 1070 | (59.8) | |
| Age (years) | <0.001 | ||||||||
| <60 | 49 | (53.3) | 303 | (47.6) | 35 | (37.6) | 676 | (37.8) | |
| ≥60 | 43 | (46.7) | 334 | (52.4) | 58 | (62.4) | 1114 | (62.2) | |
| Mean (SD) | 59.6 | (11.2) | 60.6 | (12.5) | 64.3 | (13.2) | 63.9 | (13.5) | <0.001 |
| DM | 0.147 | ||||||||
| No | 67 | (72.8) | 515 | (80.9) | 68 | (73.1) | 1414 | (79.0) | |
| Yes | 25 | (27.2) | 122 | (19.1) | 25 | (26.9) | 376 | (21.0) | |
| BMI (kg/m2), mean (SD) | 23.9 | (3.2) | 24.4 | (3.9) | 24.5 | (3.5) | 23.3 | (3.8) | <0.001 |
| CEA (ng/mL), mean (SD) | 109 | (434) | 120 | (752) | 53 | (178) | 432 | (1846) | <0.001 |
| Primary cancer site | 0.011 | ||||||||
| Left | 81 | (88.0) | 500 | (78.5) | 73 | (78.5) | 1339 | (74.8) | |
| Right | 11 | (12.0) | 137 | (21.5) | 20 | (21.5) | 451 | (25.2) | |
| Clinical staging | <0.001 | ||||||||
| I | 4 | (4.4) | 49 | (7.7) | 7 | (7.5) | 84 | (4.7) | |
| II | 7 | (7.6) | 74 | (11.6) | 8 | (8.6) | 146 | (8.2) | |
| III | 18 | (19.6) | 166 | (26.1) | 28 | (30.1) | 352 | (19.7) | |
| IV | 63 | (68.5) | 348 | (54.6) | 50 | (53.8) | 1208 | (67.5) | |
| Clinical T staging | <0.001 | ||||||||
| 1 | 3 | (3.3) | 5 | (0.8) | 1 | (1.1) | 18 | (1.0) | |
| 2 | 8 | (8.7) | 93 | (14.6) | 11 | (11.8) | 165 | (9.2) | |
| 3 | 51 | (55.4) | 350 | (55.0) | 56 | (60.2) | 857 | (47.9) | |
| 4 | 29 | (31.5) | 145 | (22.8) | 23 | (24.7) | 554 | (31.0) | |
| Missing | 1 | (1.1) | 44 | (6.9) | 2 | (2.2) | 196 | (11.0) | |
| Clinical N staging | <0.001 | ||||||||
| 0 | 20 | (21.7) | 178 | (27.9) | 21 | (22.6) | 365 | (20.4) | |
| 1 | 37 | (40.2) | 207 | (32.5) | 41 | (44.1) | 529 | (29.6) | |
| 2 | 30 | (32.6) | 205 | (32.2) | 27 | (29.0) | 665 | (37.2) | |
| Missing | 5 | (5.4) | 47 | (7.4) | 4 | (4.3) | 231 | (129) | |
| Clinical M staging | <0.001 | ||||||||
| 0 | 29 | (31.5) | 289 | (45.4) | 43 | (46.2) | 582 | (32.5) | |
| 1 | 63 | (68.5) | 348 | (54.6) | 50 | (53.8) | 1208 | (67.5) | |
| Missing | (0) | (0.1) | (0) | (0.2) | |||||
| Liver metastases timing * | 0.076 | ||||||||
| Synchronous | 45 | (48.9) | 290 | (45.5) | 30 | (32.3) | 814 | (45.5) | |
| Metachronous | 47 | (51.1) | 347 | (54.5) | 63 | (67.7) | 976 | (54.5) | |
| Extrahepatic metastasis | <0.001 | ||||||||
| No | 71 | (77.2) | 503 | (79.0) | 62 | (66.7) | 787 | (44.0) | |
| Yes | 21 | (22.8) | 134 | (21.0) | 31 | (33.3) | 1003 | (56.0) | |
| Systemic therapy | 0.030 | ||||||||
| No | 8 | (8.7) | 87 | (13.7) | 14 | (15.0) | 312 | (17.4) | |
| Yes | 84 | (91.3) | 550 | (86.3) | 79 | (85.0) | 1478 | (82.6) | |
| Neoadjuvant (Pre HR) | <0.001 | ||||||||
| No | 44 | (47.8) | 424 | (66.6) | 41 | (44.1) | - | - | |
| Yes | 48 | (52.2) | 213 | (33.4) | 52 | (55.9) | - | - | |
| Adjuvant (Post HR) | <0.001 | ||||||||
| No | 33 | (35.9) | 146 | (22.9) | 47 | (50.5) | - | - | |
| Yes | 59 | (64.1) | 491 | (77.1) | 46 | (49.5) | - | - | |
| Variable | HR (95% CI) | p-Value | aHR (95% CI) * | p-Value |
|---|---|---|---|---|
| Sex | ||||
| Female | Reference | Reference | ||
| Male | 0.91 (0.82–0.99) | 0.035 | 0.89 (0.81–0.97) | 0.011 |
| Age (years) | ||||
| <60 | Reference | Reference | ||
| ≥60 | 1.31 (1.20–1.44) | <0.001 | 1.20 (1.09–1.32) | <0.001 |
| DM | ||||
| No | Reference | Reference | ||
| Yes | 1.09 (0.97–1.22) | 0.138 | 1.00 (0.89–1.12) | 0.982 |
| BMI (kg/m2) | ||||
| <25 | Reference | Reference | ||
| ≥25 | 0.80 (0.72–0.88) | <0.001 | 0.92 (0.83–1.01) | 0.080 |
| CEA (ng/mL) | ||||
| ≤5 | Reference | Reference | ||
| >5 | 1.84 (1.64–2.07) | <0.001 | 2.14 (1.89–2.42) | <0.001 |
| Primary cancer site | ||||
| Left | Reference | Reference | ||
| Right | 1.40 (1.26–1.56) | <0.001 | 1.35 (1.22–1.51) | <0.001 |
| Liver metastases timing | ||||
| Synchronous | Reference | Reference | ||
| Metachronous | 1.14 (1.04–1.24) | 0.007 | 1.26 (1.14–1.39) | <0.001 |
| Extrahepatic metastasis | ||||
| No | Reference | Reference | ||
| Yes | 2.10 (1.91–2.30) | <0.001 | 1.46 (1.33–1.60) | <0.001 |
| Systemic therapy | ||||
| No | Reference | Reference | ||
| Yes | 0.71 (0.63–0.80) | <0.001 | 0.70 (0.62–0.79) | <0.001 |
| Liver metastases treatment methods | ||||
| Hepatectomy + RFA | 0.25 (0.19–0.34) | <0.001 | 0.28 (0.21–0.37) | <0.001 |
| Hepatectomy only | 0.22 (0.20–0.26) | <0.001 | 0.24 (0.21–0.27) | <0.001 |
| RFA only | 0.29 (0.29–0.41) | <0.001 | 0.33 (0.24–0.45) | <0.001 |
| Non local therapy | Reference | Reference |
| Variable | Hepatectomy/RFA | Non-Aggressive | p-Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Total | 597 | 597 | |||
| Sex | 1.00 | ||||
| Female | 205 | (34.3) | 205 | (34.3) | |
| Male | 392 | (65.7) | 392 | (65.7) | |
| Age (years) | 1.00 | ||||
| <60 | 272 | (45.6) | 272 | (45.6) | |
| ≥60 | 325 | (54.4) | 325 | (54.4) | |
| Mean (SD) | 61.6 | (11.5) | 61.6 | (11.5) | 1.00 |
| DM | 0.512 | ||||
| No | 475 | (79.6) | 484 | (81.1) | |
| Yes | 122 | (20.4) | 113 | (18.9) | |
| BMI (kg/m2), mean (SD) | 24.4 | (3.7) | 23.5 | (3.9) | <0.001 |
| CEA (ng/mL), mean (SD) | 99 | (490) | 528 | (2028) | <0.001 |
| Primary cancer site | 0.360 | ||||
| Left | 475 | (79.6) | 462 | (77.4) | |
| Right | 122 | (20.4) | 135 | (22.6) | |
| Clinical staging | 0.006 | ||||
| I | 35 | (5.9) | 31 | (5.2) | |
| II | 54 | (9.1) | 41 | (6.9) | |
| III | 148 | (24.8) | 108 | (18.1) | |
| IV | 360 | (60.3) | 417 | (69.9) | |
| Clinical T staging | <0.001 | ||||
| 1 | 6 | (1.0) | 5 | (0.8) | |
| 2 | 79 | (13.2) | 64 | (10.7) | |
| 3 | 336 | (56.3) | 293 | (49.1) | |
| 4 | 145 | (24.3) | 155 | (26.0) | |
| Missing | 31 | (5.2) | 80 | (13.4) | |
| Clinical N staging | <0.001 | ||||
| 0 | 146 | (24.5) | 127 | (21.3) | |
| 1 | 211 | (35.3) | 171 | (28.6) | |
| 2 | 202 | (33.8) | 210 | (35.2) | |
| Missing | 38 | (6.4) | 89 | (14.9) | |
| Clinical M staging | <0.001 | ||||
| 0 | 237 | (39.7) | 180 | (30.2) | |
| 1 | 360 | (60.3) | 417 | (69.9) | |
| Missing | 0 | (0) | 3 | (0.2) | |
| Liver metastases timing * | 1.00 | ||||
| Synchronous | 301 | (50.4) | 301 | (50.4) | |
| Metachronous | 296 | (49.6) | 296 | (49.6) | |
| Extrahepatic metastasis | 1.00 | ||||
| No | 431 | (72.2) | 431 | (72.2) | |
| Yes | 166 | (27.8) | 166 | (27.8) | |
| Systemic therapy | 1.00 | ||||
| No | 56 | (9.4) | 56 | (9.4) | |
| Yes | 541 | (90.6) | 541 | (90.6) | |
| Neoadjuvant (Pre HR) | |||||
| No | 371 | (62.1) | - | - | |
| Yes | 226 | (37.9) | - | - | |
| Adjuvant (Post HR) | |||||
| No | 160 | (26.8) | - | - | |
| Yes | 437 | (73.2) | - | - | |
| Treatment | |||||
| Hepatectomy + RFA | 66 | (11.1) | - | - | |
| Hepatectomy only | 462 | (77.4) | - | - | |
| RFA only | 69 | (11.6) | - | - | |
| Treatment | HR (95% CI) * | p-Value |
|---|---|---|
| Full data | ||
| Hepatectomy + RFA | 0.18 (0.08–0.39) | <0.001 |
| Hepatectomy only | 0.15 (0.11–0.21) | <0.001 |
| RFA only | 0.10 (0.04–0.25) | <0.001 |
| Non | Reference | |
| Female | ||
| Hepatectomy + RFA | 0.32 (0.08–1.22) | 0.095 |
| Hepatectomy only | 0.12 (0.06–0.22) | <0.001 |
| RFA only | 0.11 (0.02–0.56) | 0.008 |
| Non | Reference | |
| Male | ||
| Hepatectomy + RFA | 0.15 (0.06–0.38) | <0.001 |
| Hepatectomy only | 0.15 (0.10–0.22) | <0.001 |
| RFA only | 0.08 (0.02–0.26) | <0.001 |
| Non | Reference | |
| Age < 60 years | ||
| Hepatectomy + RFA | 0.22 (0.08–0.59) | 0.003 |
| Hepatectomy only | 0.19 (0.12–0.29) | <0.001 |
| RFA only | 0.08 (0.02–0.37) | 0.001 |
| Non | Reference | |
| Age ≥ 60 years | ||
| Hepatectomy + RFA | 0.12 (0.03–0.46) | 0.002 |
| Hepatectomy only | 0.12 (0.07–0.19) | <0.001 |
| RFA only | 0.10 (0.03–0.36) | <0.001 |
| Non | Reference |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Canseco, L.M.; Liu, Y.-W.; Lu, C.-C.; Lee, K.-C.; Chen, H.-H.; Hu, W.-H.; Tsai, K.-L.; Yang, Y.-H.; Wang, C.-C.; Hung, C.-H. Survival Evidence of Local Control for Colorectal Cancer Liver Metastases by Hepatectomy and/or Radiofrequency Ablation. Cancers 2023, 15, 4434. https://doi.org/10.3390/cancers15184434
Canseco LM, Liu Y-W, Lu C-C, Lee K-C, Chen H-H, Hu W-H, Tsai K-L, Yang Y-H, Wang C-C, Hung C-H. Survival Evidence of Local Control for Colorectal Cancer Liver Metastases by Hepatectomy and/or Radiofrequency Ablation. Cancers. 2023; 15(18):4434. https://doi.org/10.3390/cancers15184434
Chicago/Turabian StyleCanseco, Lariza Marie, Yueh-Wei Liu, Chien-Chang Lu, Ko-Chao Lee, Hong-Hwa Chen, Wan-Hsiang Hu, Kai-Lung Tsai, Yao-Hsu Yang, Chih-Chi Wang, and Chao-Hung Hung. 2023. "Survival Evidence of Local Control for Colorectal Cancer Liver Metastases by Hepatectomy and/or Radiofrequency Ablation" Cancers 15, no. 18: 4434. https://doi.org/10.3390/cancers15184434
APA StyleCanseco, L. M., Liu, Y.-W., Lu, C.-C., Lee, K.-C., Chen, H.-H., Hu, W.-H., Tsai, K.-L., Yang, Y.-H., Wang, C.-C., & Hung, C.-H. (2023). Survival Evidence of Local Control for Colorectal Cancer Liver Metastases by Hepatectomy and/or Radiofrequency Ablation. Cancers, 15(18), 4434. https://doi.org/10.3390/cancers15184434








