Cost–Utility Analysis of Open Radical Hysterectomy Compared to Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
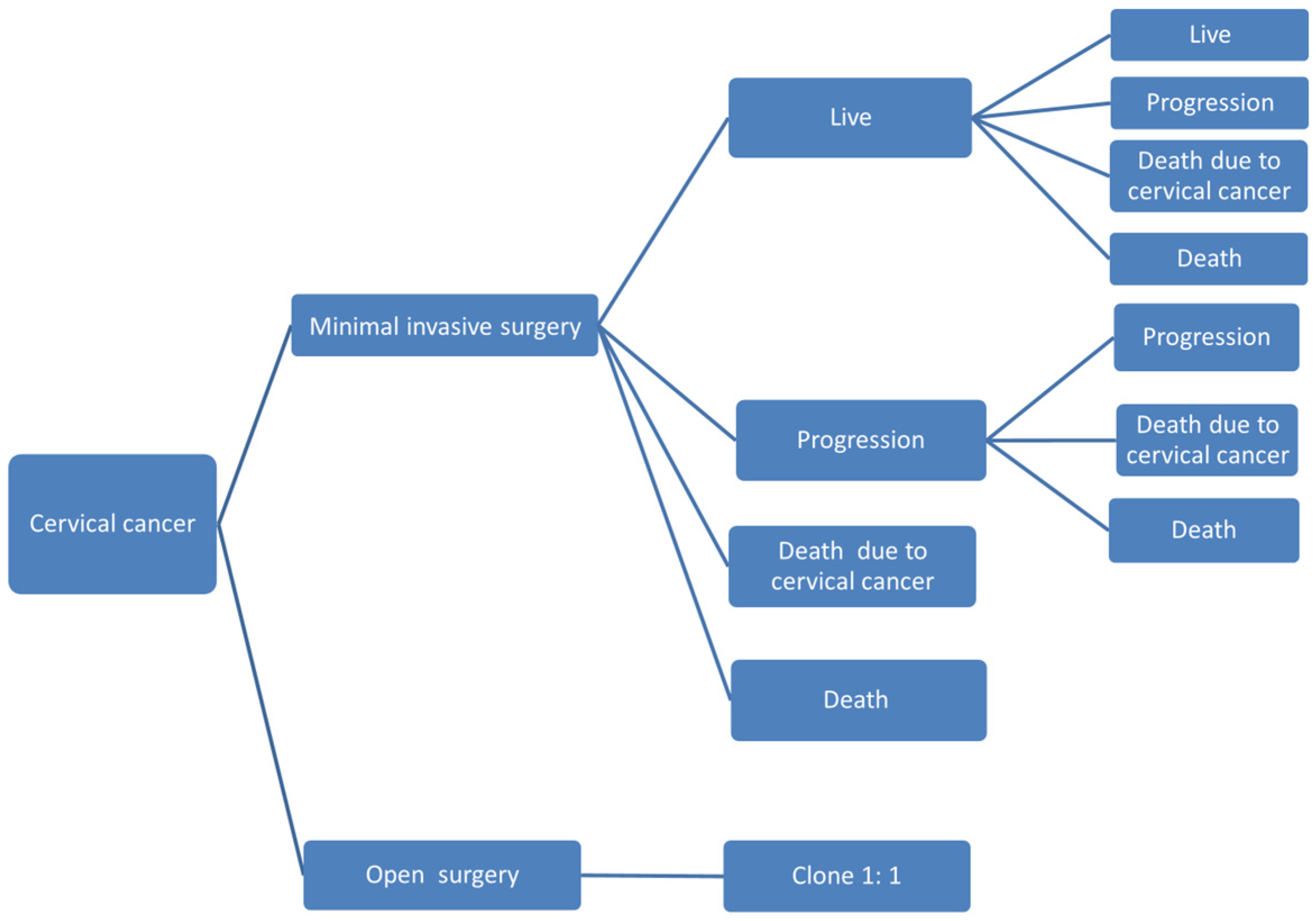
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wright, J.D.; Herzog, T.J.; Neugut, A.I.; Burke, W.M.; Lu, Y.S.; Lewin, S.N.; Hershman, D.L. Comparative effectiveness of minimally invasive and abdominal radical hysterectomy for cervical cancer. Gynecol. Oncol. 2012, 127, 11–17. [Google Scholar] [CrossRef]
- Piedimonte, S.; Czuzoj-Shulman, N.; Gotlieb, W.; Abenhaim, H.A. Robotic Radical Hysterectomy for Cervical Cancer: A Population-Based Study of Adoption and Immediate Postoperative Outcomes in the United States. J. Minim. Invasive Gynecol. 2019, 26, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Melamed, A.; Ramirez, P.T. Changing treatment landscape for early cervical cancer: Outcomes reported with minimally invasive surgery compared with an open approach. Curr. Opin. Obstet. Gynecol. 2020, 32, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Kang, H.; Kim, D.H. A comparative study of laparoscopic radical hysterectomy with radical abdominal hysterectomy for early-stage cervical cancer: A long-term follow-up study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 156, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Paik, E.S.; Lim, M.C.; Kim, M.H.; Kim, Y.H.; Song, E.S.; Seong, S.J.; Suh, D.H.; Lee, J.M.; Lee, C.; Choi, C.H. Comparison of laparoscopic and abdominal radical hysterectomy in early stage cervical cancer patients without adjuvant treatment: Ancillary analysis of a Korean Gynecologic Oncology Group Study (KGOG 1028). Gynecol. Oncol. 2019, 154, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Diver, E.; Hinchcliff, E.; Gockley, A.; Melamed, A.; Contrino, L.; Feldman, S.; Growdon, W. Minimally Invasive Radical Hysterectomy for Cervical Cancer Is Associated with Reduced Morbidity and Similar Survival Outcomes Compared With Laparotomy. J. Minim. Invasive Gynecol. 2017, 24, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Sert, B.M.; Boggess, J.F.; Ahmad, S.; Jackson, A.L.; Stavitzski, N.M.; Dahl, A.A.; Holloway, R.W. Robot-assisted versus open radical hysterectomy: A multi-institutional experience for early-stage cervical cancer. Eur. J. Surg. Oncol. 2016, 42, 513–522. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, S.; Lv, A.; Huang, S. Laparoscopically Assisted Radical Vaginal Hysterectomy for Early-Stage Cervical Cancer: A Systemic Review and Meta-Analysis. Int. J. Gynecol. Cancer 2016, 26, 1497–1502. [Google Scholar] [CrossRef]
- Park, D.A.; Yun, J.E.; Kim, S.W.; Lee, S.H. Surgical and clinical safety and effectiveness of robot-assisted laparoscopic hysterectomy compared to conventional laparoscopy and laparotomy for cervical cancer: A systematic review and meta-analysis. Eur. J. Surg. Oncol. 2017, 43, 994–1002. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, P.T.; Frumovitz, M.; Pareja, R.; Lopez, A.; Vieira, M.; Ribeiro, R.; Buda, A.; Yan, X.; Shuzhong, Y.; Chetty, N.; et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N. Engl. J. Med. 2018, 379, 1895–1904. [Google Scholar] [CrossRef] [PubMed]
- Melamed, A.; Margul, D.J.; Chen, L.; Keating, N.L.; Del Carmen, M.G.; Yang, J.; Seagle, B.L.L.; Alexander, A.; Barber, E.L.; Rice, L.W.; et al. Survival after Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. N. Engl. J. Med. 2018, 379, 1905–1914. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Dai, W.; Si, Y.; Shi, Y.; Li, X.; Jiang, K.; Shen, J.; Ying, L. Comparison of Minimally Invasive Versus Abdominal Radical Hysterectomy for Early-Stage Cervical Cancer: An Updated Meta-Analysis. Front. Oncol. 2022, 11, 762921. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Cai, J.; Li, R.; Wang, Y.; Zhao, J.; Huang, Y.; Xu, L.; Yang, Q.; Wang, Z. A meta-analysis of survival after minimally invasive radical hysterectomy versus abdominal radical hysterectomy in cervical cancer: Center-associated factors matter. Arch. Gynecol. Obstet. 2022, 306, 623–637. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Deng, T.; Gu, S. Minimally invasive surgery and abdominal radical hysterectomy in patients with early-stage cervical cancer: A meta-analysis. Int. J. Gynaecol. Obstet. 2022, 157, 255–264. [Google Scholar] [CrossRef]
- Rodriguez, J.; Rauh-Hain, J.A.; Saenz, J.; Isla, D.O.; Rendon Pereira, G.J.; Odetto, D.; Martinelli, F.; Villoslada, V.; Zapardiel, I.; Trujillo, L.M.; et al. Oncological outcomes of laparoscopic radical hysterectomy versus radical abdominal hysterectomy in patients with early-stage cervical cancer: A multicenter analysis. Int. J. Gynecol. Cancer 2021, 31, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, B.; Ren, F.; Song, Z.; Ouyang, L.; Liu, K. Survival After Minimally Invasive vs. Open Radical Hysterectomy for Cervical Cancer: A Meta-Analysis. Front. Oncol. 2020, 10, 1236. [Google Scholar] [CrossRef] [PubMed]
- Nitecki, R.; Ramirez, P.T.; Frumovitz, M.; Krause, K.J.; Tergas, A.I.; Wright, J.D.; Rauh-Hain, J.A.; Melamed, A. Survival After Minimally Invasive vs. Open Radical Hysterectomy for Early-Stage Cervical Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2020, 6, 1019–1027. [Google Scholar] [CrossRef]
- Cusimano, M.C.; Baxter, N.N.; Gien, L.T.; Moineddin, R.; Liu, N.; Dossa, F.; Willows, K.; Ferguson, S.E. Impact of surgical approach on oncologic outcomes in women undergoing radical hysterectomy for cervical cancer. Am. J. Obstet. Gynecol. 2019, 221, 619.e1–619.e24. [Google Scholar] [CrossRef]
- Kim, S.I.; Cho, J.H.; Seol, A.; Kim, Y.I.; Lee, M.; Kim, H.S.; Chung, H.H.; Kim, J.W.; Park, N.H.; Song, Y.S. Comparison of survival outcomes between minimally invasive surgery and conventional open surgery for radical hysterectomy as primary treatment in patients with stage IB1-IIA2 cervical cancer. Gynecol. Oncol. 2019, 153, 3–12. [Google Scholar] [CrossRef]
- Piedimonte, S.; Pond, G.R.; Plante, M.; Nelson, G.; Kwon, J.; Altman, A.; Feigenberg, T.; Elit, L.; Lau, S.; Sabourin, J.; et al. Comparison of outcomes between abdominal, minimally invasive and combined vaginal-laparoscopic hysterectomy in patients with stage IAI/IA2 cervical cancer: 4C (Canadian Cervical Cancer Collaborative) study. Gynecol. Oncol. 2022, 166, 230–235. [Google Scholar] [CrossRef]
- Hayek, J.; Mowzoon, M.; Demissie, S.; Palileo, A.; Serur, E.; Goldberg, G.L.; Alagkiozidis, I. Minimally invasive versus open surgery for women with stage 1A1 and stage 1A2 cervical cancer: A retrospective database cohort study. Ann. Med. Surg. 2022, 77, 103507. [Google Scholar] [CrossRef]
- Basaran, D.; Leitao, M.M. The Landmark Series: Minimally Invasive Surgery for Cervical Cancer. Ann. Surg. Oncol. 2021, 28, 204–211. [Google Scholar] [CrossRef]
- Uppal, S.; Rebecca Liu, J.; Kevin Reynolds, R.; Rice, L.W.; Spencer, R.J. Trends and comparative effectiveness of inpatient radical hysterectomy for cervical cancer in the United States (2012–2015). Gynecol. Oncol. 2019, 152, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Graves, N.; Janda, M.; Merollini, K.; Gebski, V.; Obermair, A. The cost-effectiveness of total laparoscopic hysterectomy compared to total abdominal hysterectomy for the treatment of early stage endometrial cancer. BMJ Open 2013, 3, e001884. [Google Scholar] [CrossRef] [PubMed]
- Lundin, E.S.; Carlsson, P.; Wodlin, N.B.; Nilsson, L.; Kjölhede, P. Cost-effectiveness of robotic hysterectomy versus abdominal hysterectomy in early endometrial cancer. Int. J. Gynecol. Cancer 2020, 30, 1719–1725. [Google Scholar] [CrossRef]
- Close, A.; Robertson, C.; Rushton, S.; Shirley, M.; Vale, L.; Ramsay, C.; Pickard, R. Comparative cost-effectiveness of robot-assisted and standard laparoscopic prostatectomy as alternatives to open radical prostatectomy for treatment of men with localised prostate cancer: A health technology assessment from the perspective of the UK National Health Service. Eur. Urol. 2013, 64, 361–369. [Google Scholar] [CrossRef]
- Pourrahmat, M.M.; Kim, A.; Kansal, A.R.; Hux, M.; Pushkarna, D.; Fazeli, M.S.; Chung, K.C. Health state utility values by cancer stage: A systematic literature review. Eur. J. Health Econ. 2021, 22, 1275–1288. [Google Scholar] [CrossRef]
- Garabedian, C.; Merlot, B.; Bresson, L.; Tresch, E.; Narducci, F.; Leblanc, E. Minimally invasive surgical management of early-stage cervical cancer: An analysis of the risk factors of surgical complications and of oncologic outcomes. Int. J. Gynecol. Cancer 2015, 25, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Mendivil, A.A.; Rettenmaier, M.A.; Abaid, L.N.; Brown, J.V.; Micha, J.P.; Lopez, K.L.; Goldstein, B.H. Survival rate comparisons amongst cervical cancer patients treated with an open, robotic-assisted or laparoscopic radical hysterectomy: A five year experience. Surg. Oncol. 2016, 25, 66–71. [Google Scholar] [CrossRef]
- Sobiczewski, P.; Bidzinski, M.; Derlatka, P.; Panek, G.; Danska-Bidzinska, A.; Gmyrek, L.; Michalski, W. Early cervical cancer managed by laparoscopy and conventional surgery: Comparison of treatment results. Int. J. Gynecol. Cancer 2009, 19, 1390–1395. [Google Scholar] [CrossRef]
- Wang, Y.; Deng, L.; Xu, H.C.; Zhang, Y.; Liang, Z.Q. Laparoscopy versus laparotomy for the management of early stage cervical cancer. BMC Cancer 2015, 15, 928. [Google Scholar] [CrossRef] [PubMed]
- Cao, T.; Feng, Y.; Huang, Q.; Wan, T.; Liu, J. Prognostic and Safety Roles in Laparoscopic Versus Abdominal Radical Hysterectomy in Cervical Cancer: A Meta-analysis. J. Laparoendosc. Adv. Surg. Tech. A 2015, 25, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Frumovitz, M.; Dos Reis, R.; Sun, C.C.; Milam, M.R.; Bevers, M.W.; Brown, J.; Slomovitz, B.M.; Ramirez, P.T. Comparison of total laparoscopic and abdominal radical hysterectomy for patients with early-stage cervical cancer. Obstet. Gynecol. 2007, 110, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Nam, J.H.; Park, J.Y.; Kim, D.Y.; Kim, J.H.; Kim, Y.M.; Kim, Y.T. Laparoscopic versus open radical hysterectomy in early-stage cervical cancer: Long-term survival outcomes in a matched cohort study. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2012, 23, 903–911. [Google Scholar] [CrossRef]
- Lewicki, P.J.; Basourakos, S.P.; Qiu, Y.; Hu, J.C.; Sheyn, D.; Hijaz, A.; Shoag, J.E. Effect of a Randomized, Controlled Trial on Surgery for Cervical Cancer. N. Engl. J. Med. 2021, 384, 1669–1671. [Google Scholar] [CrossRef]
- Frumovitz, M.; Obermair, A.; Coleman, R.L.; Pareja, R.; Lopez, A.; Ribero, R.; Isla, D.; Rendon, G.; Bernadini, M.Q.; Buda, A.; et al. Quality of life in patients with cervical cancer after open versus minimally invasive radical hysterectomy (LACC): A secondary outcome of a multicentre, randomised, open-label, phase 3, non-inferiority trial. Lancet. Oncol. 2020, 21, 851–860. [Google Scholar] [CrossRef]
- Galaal, K.; Bryant, A.; Fisher, A.D.; Al-Khaduri, M.; Kew, F.; Lopes, A.D. Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane database Syst. Rev. 2012, 2012, CD006655. [Google Scholar] [CrossRef]
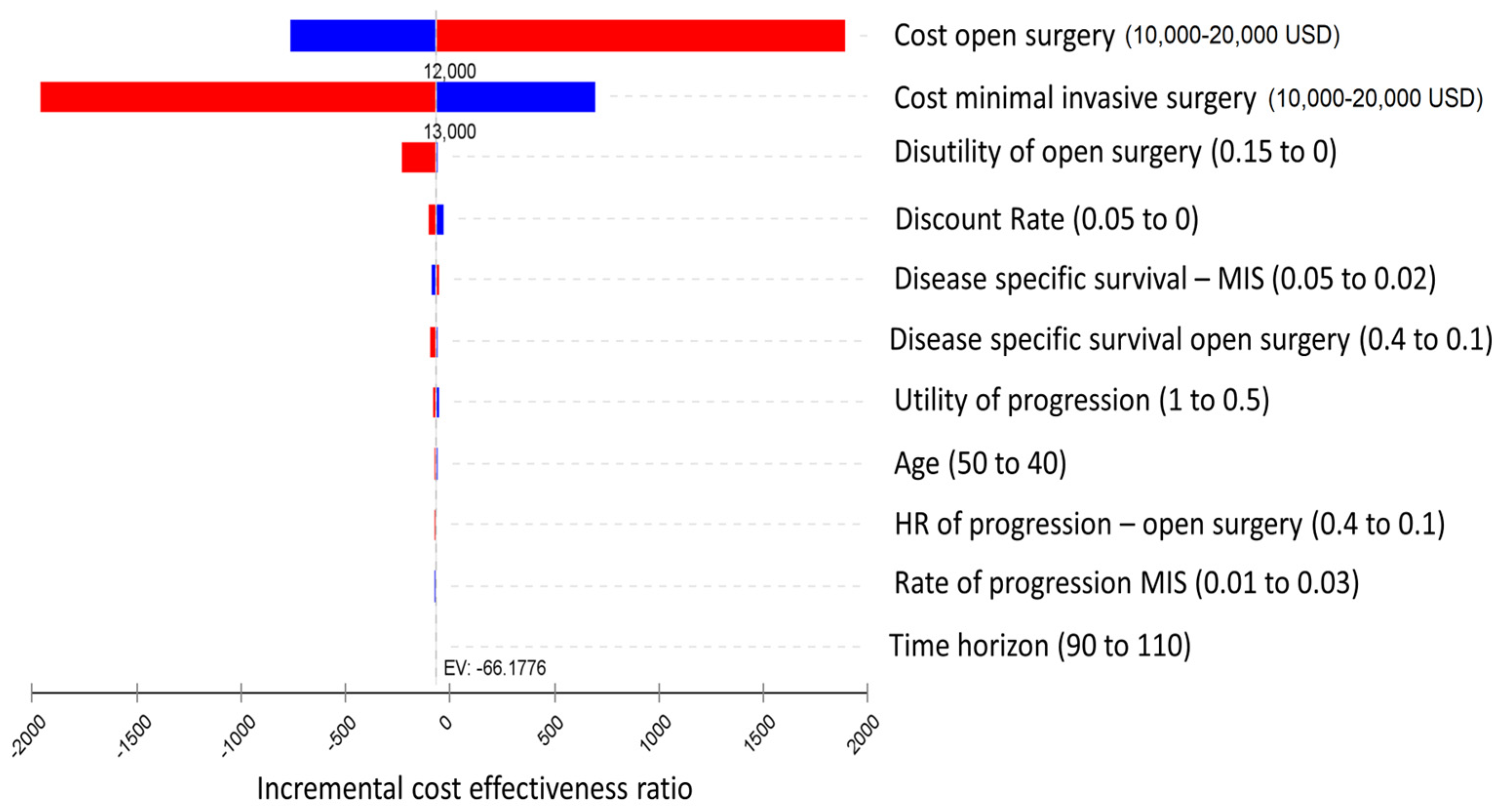
| Description | Base | Low | High | Ref. |
|---|---|---|---|---|
| Age | 45 | 40 | 50 | assumption |
| disutility of Open surgery | 0.02 | 0 | 0.4 | [27] |
| HR of Disease-Specific Survival—Open Surgery | 0.152 | 0.1 | 0.4 | [10] |
| HR of Progression—Open Surgery | 0.235 | 0.1 | 0.4 | [10] |
| Discount Rate | 0.03 | 0 | 0.05 | assumption |
| Rate of Disease-Specific Survival—Minimally Invasive | 0.015 | 0.01 | 0.02 | [10] |
| Rate of Progression—Minimally Invasive | 0.0216 | 0.01 | 0.03 | [10] |
| Time Horizon—Until age | 100 | 90 | 110 | assumption |
| Utility of Progression | 0.8 | 0.5 | 1 | [27] |
| Cost of Laparotomy (Open Surgery) | 12,624 | 10,000 | 20,000 | [23] |
| Cost of laparoscopic surgery | 12,873 | 10,000 | 20,000 | [23] |
| Cost of Robotic surgery | 14,029 | 10,000 | 20,000 | [23] |
| Strategy | Cost | Incremental Cost | Effect | Incremental Effect | Incremental Cost-Effectiveness Ratio |
| Open radical hysterectomy | 12,624 | 20.88 | |||
| Laparoscopic radical hysterectomy | 12,873 | 249 | 17.12 | −3.76 | −66.18 |
| Strategy | Cost | Incremental Cost | Effect | Incremental Effect | Incremental Cost-Effectiveness Ratio |
| Open radical hysterectomy | 12,624 | 20.88 | |||
| Robotic radical hysterectomy | 14,029 | 1405 | 17.12 | −3.76 | −373.41 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michaan, N.; Leshno, M.; Fire, G.; Safra, T.; Rosenberg, M.; Peleg-Hasson, S.; Grisaru, D.; Laskov, I. Cost–Utility Analysis of Open Radical Hysterectomy Compared to Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. Cancers 2023, 15, 4325. https://doi.org/10.3390/cancers15174325
Michaan N, Leshno M, Fire G, Safra T, Rosenberg M, Peleg-Hasson S, Grisaru D, Laskov I. Cost–Utility Analysis of Open Radical Hysterectomy Compared to Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. Cancers. 2023; 15(17):4325. https://doi.org/10.3390/cancers15174325
Chicago/Turabian StyleMichaan, Nadav, Moshe Leshno, Gil Fire, Tamar Safra, Michal Rosenberg, Shira Peleg-Hasson, Dan Grisaru, and Ido Laskov. 2023. "Cost–Utility Analysis of Open Radical Hysterectomy Compared to Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer" Cancers 15, no. 17: 4325. https://doi.org/10.3390/cancers15174325
APA StyleMichaan, N., Leshno, M., Fire, G., Safra, T., Rosenberg, M., Peleg-Hasson, S., Grisaru, D., & Laskov, I. (2023). Cost–Utility Analysis of Open Radical Hysterectomy Compared to Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. Cancers, 15(17), 4325. https://doi.org/10.3390/cancers15174325





