Thiazolidinedione Use Is Associated with a Borderline Lower Risk of Multiple Myeloma and a Significantly Lower Risk of Death in Patients with Type 2 Diabetes Mellitus in Taiwan
Abstract
Simple Summary
Abstract
1. Introduction
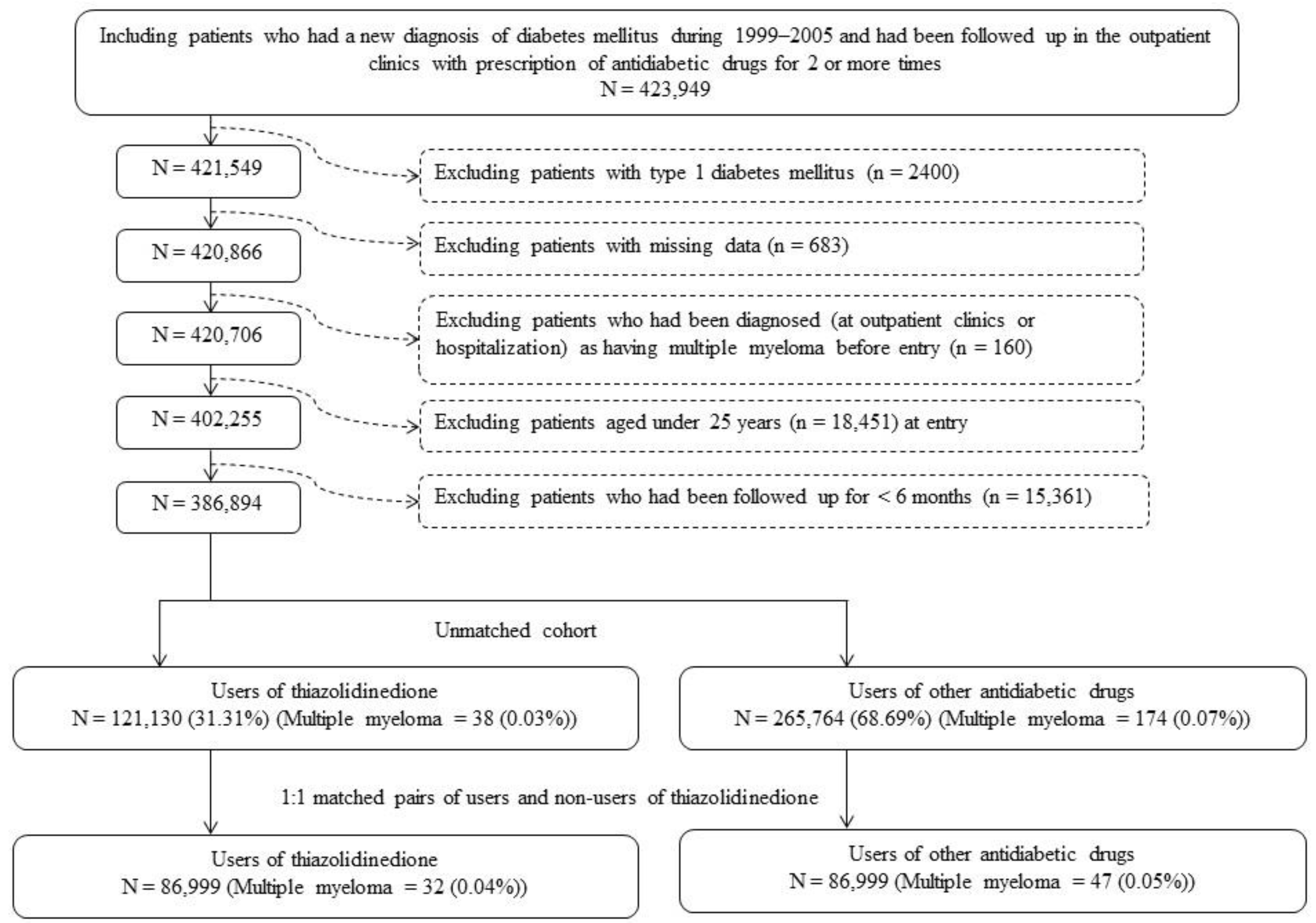
2. Materials and Methods
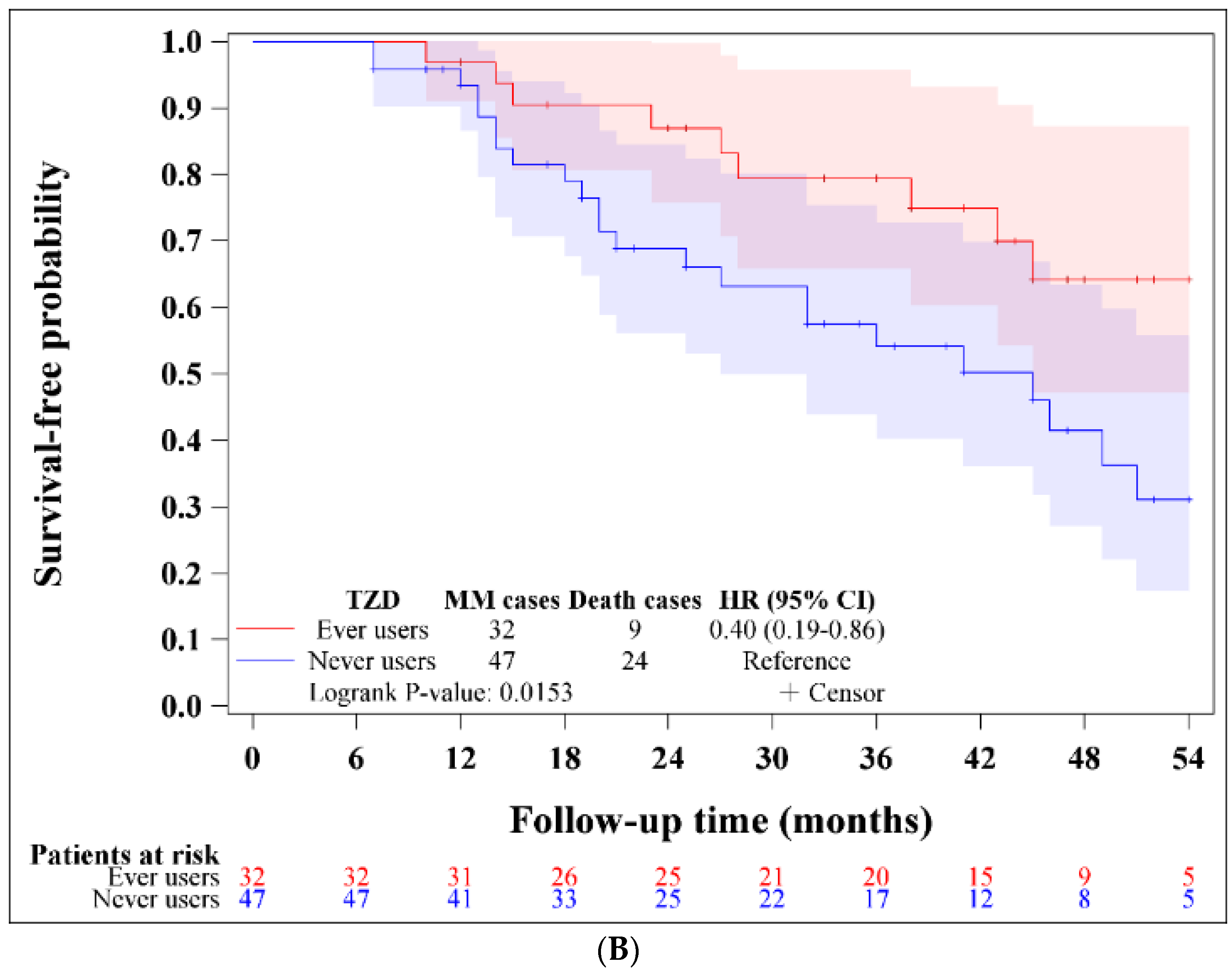
3. Results
4. Discussion
4.1. Main Findings
4.2. Explanations for an Attenuated Effect of TZD in Humans
4.3. Implications
4.4. Strengths
4.5. Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rajkumar, S.V. Multiple myeloma: 2022 update on diagnosis, risk stratification, and management. Am. J. Hematol. 2022, 97, 1086–1107. [Google Scholar] [CrossRef]
- Kazandjian, D. Multiple myeloma epidemiology and survival: A unique malignancy. Semin. Oncol. 2016, 43, 676–681. [Google Scholar] [CrossRef]
- Castaneda, O.; Baz, R. Multiple myeloma genomics—A concise review. Acta Med. Acad. 2019, 48, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Brigle, K.; Rogers, B. Pathobiology and diagnosis of multiple myeloma. Semin. Oncol. Nurs. 2017, 33, 225–236. [Google Scholar] [CrossRef] [PubMed]
- Cowan, A.J.; Green, D.J.; Kwok, M.; Lee, S.; Coffey, D.G.; Holmberg, L.A.; Tuazon, S.; Gopal, A.K.; Libby, E.N. Diagnosis and management of multiple myeloma: A review. JAMA 2022, 327, 464–477. [Google Scholar] [CrossRef]
- Tentolouris, A.; Ntanasis-Stathopoulos, I.; Eleftheriadou, I.; Malandrakis, P.; Tzeravini, E.; Gavriatopoulou, M. Diabetes mellitus and multiple myeloma; common features of two distinct entities. Diabetes Metab. Res. Rev. 2022, 38, e3535. [Google Scholar] [CrossRef] [PubMed]
- Ragbourne, S.C.; Maghsoodi, N.; Streetly, M.; Crook, M.A. The association between metabolic syndrome and multiple myeloma. Acta Haematol. 2021, 144, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.; Dossus, L.; Kaaks, R. Obesity related hyperinsulinaemia and hyperglycaemia and cancer development. Arch. Physiol. Biochem. 2009, 115, 86–96. [Google Scholar] [CrossRef] [PubMed]
- Wallin, A.; Larsson, S.C. Body mass index and risk of multiple myeloma: A meta-analysis of prospective studies. Eur. J. Cancer 2011, 47, 1606–1615. [Google Scholar] [CrossRef]
- Bertazzi, P.A.; Zocchetti, C.; Guercilena, S.; Consonni, D.; Tironi, A.; Landi, M.T.; Pesatori, A.C. Dioxin exposure and cancer risk: A 15-year mortality study after the “Seveso accident”. Epidemiology 1997, 8, 646–652. [Google Scholar] [CrossRef]
- Fracchiolla, N.S.; Annaloro, C.; Guidotti, F.; Fattizzo, B.; Cortelezzi, A. 2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) role in hematopoiesis and in hematologic diseases: A critical review. Toxicology 2016, 374, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Harbron, R.W.; Pasqual, E. Ionising radiation as a risk factor for lymphoma: A review. J. Radiol. Prot. 2020, 40, R151. [Google Scholar] [CrossRef] [PubMed]
- Andreotti, G.; Birmann, B.M.; Cozen, W.; De Roos, A.J.; Chiu, B.C.; Costas, L.; de Sanjosé, S.; Moysich, K.; Camp, N.J.; Spinelli, J.J.; et al. A pooled analysis of cigarette smoking and risk of multiple myeloma from the international multiple myeloma consortium. Cancer Epidemiol. Biomark. Prev. 2015, 24, 631–634. [Google Scholar] [CrossRef] [PubMed]
- Landgren, O.; Zeig-Owens, R.; Giricz, O.; Goldfarb, D.; Murata, K.; Thoren, K.; Ramanathan, L.; Hultcrantz, M.; Dogan, A.; Nwankwo, G.; et al. Multiple myeloma and its precursor disease among firefighters exposed to the World Trade Center disaster. JAMA Oncol. 2018, 4, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Mateos, M.V.; Landgren, O. MGUS and smoldering multiple myeloma: Diagnosis and epidemiology. Plasma Cell Dyscrasias 2016, 169, 3–12. [Google Scholar]
- Sundararajan, S.; Kumar, A.; Korde, N.; Agarwal, A. Smoldering multiple myeloma: Emerging concepts and therapeutics. Curr. Hematol. Malig. Rep. 2016, 11, 102–110. [Google Scholar] [CrossRef]
- Mateos, M.V.; González-Calle, V. Smoldering multiple myeloma: Who and when to treat. Clin. Lymphoma Myeloma Leuk. 2017, 17, 716–722. [Google Scholar] [CrossRef]
- Thorsteinsdóttir, S.; Gíslason, G.K.; Aspelund, T.; Rögnvaldsson, S.; Óskarsson, J.Þ.; Sigurðardóttir, G.Á.; Þórðardóttir, Á.R.; Viðarsson, B.; Önundarson, P.T.; Agnarsson, B.A.; et al. Prevalence of smoldering multiple myeloma based on nationwide screening. Nat. Med. 2023, 29, 467–472. [Google Scholar] [CrossRef]
- Huang, S.Y.; Yao, M.; Tang, J.L.; Lee, W.C.; Tsay, W.; Cheng, A.L.; Wang, C.H.; Chen, Y.C.; Shen, M.C.; Tien, H.F. Epidemiology of multiple myeloma in Taiwan: Increasing incidence for the past 25 years and higher prevalence of extramedullary myeloma in patients younger than 55 years. Cancer 2007, 110, 896–905. [Google Scholar] [CrossRef]
- Tang, C.H.; Liu, H.Y.; Hou, H.A.; Qiu, H.; Huang, K.C.; Siggins, S.; Rothwell, L.A.; Liu, Y. Epidemiology of multiple myeloma in Taiwan, a population based study. Cancer Epidemiol. 2018, 55, 136–141. [Google Scholar] [CrossRef]
- Tzeng, H.E.; Lin, C.L.; Tsai, C.H.; Tang, C.H.; Hwang, W.L.; Cheng, Y.W.; Sung, F.C.; Chung, C.J. Time trend of multiple myeloma and associated secondary primary malignancies in Asian patients: A Taiwan population-based study. PLoS ONE 2013, 8, e68041. [Google Scholar]
- Chen, J.H.; Chung, C.H.; Wang, Y.C.; Hsu, S.N.; Huang, W.Y.; Chien, W.C. Prevalence and mortality-related factors of multiple myeloma in Taiwan. PLoS ONE 2016, 11, e0167227. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ugai, T.; Ito, H.; Oze, I.; Saito, E.; Rahman, M.S.; Boffetta, P.; Gupta, P.C.; Sawada, N.; Tamakoshi, A.; Shu, X.O.; et al. Association of BMI smoking, and alcohol with multiple myeloma mortality in Asians: A pooled analysis of more than 800,000 participants in the Asia Cohort Consortium. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1861–1867. [Google Scholar] [CrossRef]
- Chou, Y.S.; Yang, C.F.; Chen, H.S.; Yang, S.H.; Yu, Y.B.; Hong, Y.C.; Liu, C.Y.; Gau, J.P.; Liu, J.H.; Chen, P.M.; et al. Pre-existing diabetes mellitus in patients with multiple myeloma. Eur. J. Haematol. 2012, 89, 320–327. [Google Scholar] [CrossRef]
- Hsu, P.; Lin, T.W.; Gau, J.P.; Yu, Y.B.; Hsiao, L.T.; Tzeng, C.H.; Chen, P.M.; Chiou, T.J.; Liu, J.H.; Liu, Y.C.; et al. Risk of early mortality in patients with newly diagnosed multiple myeloma. Medicine 2015, 94, e2305. [Google Scholar] [CrossRef]
- Tseng, C.H.; Tseng, F.H. Peroxisome proliferator-activated receptor agonists and bladder cancer: Lessons from animal studies. J. Environ. Sci. Health C Environ. Carcinog. Ecotoxicol. Rev. 2012, 30, 368–402. [Google Scholar] [CrossRef] [PubMed]
- Kumar, H.; Aggarwal, N.; Marwaha, M.G.; Deep, A.; Chopra, H.; Matin, M.M.; Roy, A.; Emran, T.B.; Mohanta, Y.K.; Ahmed, R.; et al. Thiazolidin-2,4-dione scaffold: An insight into recent advances as antimicrobial, antioxidant, and hypoglycemic agents. Molecules 2022, 27, 6763. [Google Scholar] [CrossRef]
- Kajal, K.; Singh, G.; Pradhan, T.; Bhurta, D.; Monga, V. The medicinal perspective of 2,4-thiazolidinediones based ligands as antimicrobial, antitumor and antidiabetic agents: A review. Arch. Pharm. 2022, 355, e2100517. [Google Scholar] [CrossRef]
- Tseng, C.H. A review on thiazolidinediones and bladder cancer in human studies. J. Environ. Sci. Health C Environ. Carcinog. Ecotoxicol. Rev. 2014, 32, 1–45. [Google Scholar] [CrossRef]
- Chi, T.; Wang, M.; Wang, X.; Yang, K.; Xie, F.; Liao, Z.; Wei, P. PPAR-γ modulators as current and potential cancer treatments. Front. Oncol. 2021, 11, 737776. [Google Scholar] [CrossRef]
- Ray, D.M.; Bernstein, S.H.; Phipps, R.P. Human multiple myeloma cells express peroxisome proliferator-activated receptor gamma and undergo apoptosis upon exposure to PPARgamma ligands. Clin. Immunol. 2004, 113, 203–213. [Google Scholar] [PubMed]
- Eucker, J.; Bängeroth, K.; Zavrski, I.; Krebbel, H.; Zang, C.; Heider, U.; Jakob, C.; Elstner, E.; Possinger, K.; Sezer, O. Ligands of peroxisome proliferator-activated receptor gamma induce apoptosis in multiple myeloma. Anti-Cancer Drugs 2004, 15, 955–960. [Google Scholar] [PubMed]
- Garcia-Bates, T.M.; Bernstein, S.H.; Phipps, R.P. Peroxisome proliferator-activated receptor gamma overexpression suppresses growth and induces apoptosis in human multiple myeloma cells. Clin. Cancer Res. 2008, 14, 6414–6425. [Google Scholar] [PubMed]
- Rui, M.; Huang, Z.; Liu, Y.; Wang, Z.; Liu, R.; Fu, J.; Huang, H. Rosiglitazone suppresses angiogenesis in multiple myeloma via downregulation of hypoxia-inducible factor-1α and insulin-like growth factor-1 mRNA expression. Mol. Med. Rep. 2014, 10, 2137–2143. [Google Scholar] [PubMed]
- Wang, L.H.; Yang, X.Y.; Zhang, X.; Huang, J.; Hou, J.; Li, J.; Xiong, H.; Mihalic, K.; Zhu, H.; Xiao, W.; et al. Transcriptional inactivation of STAT3 by PPARgamma suppresses IL-6-responsive multiple myeloma cells. Immunity 2004, 20, 205–218. [Google Scholar] [PubMed]
- Wang, L.H.; Yang, X.Y.; Zhang, X.; Farrar, W.L. Inhibition of adhesive interaction between multiple myeloma and bone marrow stromal cells by PPARgamma cross talk with NF-kappaB and C/EBP. Blood J. Am. Soc. Hematol. 2007, 110, 4373–4384. [Google Scholar]
- Kurtoglu, M.; Philips, K.; Liu, H.; Boise, L.H.; Lampidis, T.J. High endoplasmic reticulum activity renders multiple myeloma cells hypersensitive to mitochondrial inhibitors. Cancer Chemother. Pharmacol. 2010, 66, 129–140. [Google Scholar]
- Lessard, S.J.; Chen, Z.P.; Watt, M.J.; Hashem, M.; Reid, J.J.; Febbraio, M.A.; Kemp, B.E.; Hawley, J.A. Chronic rosiglitazone treatment restores AMPKalpha2 activity in insulin-resistant rat skeletal muscle. Am. J. Physiol. Endocrinol. Metab. 2006, 290, E251–E257. [Google Scholar]
- LeBrasseur, N.K.; Kelly, M.; Tsao, T.S.; Farmer, S.R.; Saha, A.K.; Ruderman, N.B.; Tomas, E. Thiazolidinediones can rapidly activate AMP-activated protein kinase in mammalian tissues. Am. J. Physiol. Endocrinol. Metab. 2006, 291, E175–E181. [Google Scholar]
- Baumann, P.; Mandl-Weber, S.; Emmerich, B.; Straka, C.; Schmidmaier, R. Activation of adenosine monophosphate activated protein kinase inhibits growth of multiple myeloma cells. Exp. Cell Res. 2007, 313, 3592–3603. [Google Scholar]
- Tseng, C.H. Pioglitazone and bladder cancer in human studies: Is it diabetes itself, diabetes drugs, flawed analyses or different ethnicities? J. Formos. Med. Assoc. 2012, 111, 123–131. [Google Scholar]
- Tseng, C.H. Use of metformin and risk of kidney cancer in patients with type 2 diabetes. Eur. J. Cancer 2016, 52, 19–25. [Google Scholar]
- Tseng, C.H. The risk of multiple myeloma is reduced in metformin initiators: A retrospective cohort study in Taiwanese patients with type 2 diabetes mellitus. Cancers 2022, 14, 5637. [Google Scholar]
- Tseng, C.H. Pioglitazone has a null association with inflammatory bowel disease in patients with type 2 diabetes mellitus. Pharmaceuticals 2022, 15, 1538. [Google Scholar]
- Parsons, L.S. Performing a 1:N Case-Control Match on Propensity Score. Available online: https://support.sas.com/resources/papers/proceedings/proceedings/sugi29/165-29.pdf (accessed on 19 June 2023).
- Tseng, C.H. Diabetes, insulin use and Helicobacter pylori eradication: A retrospective cohort study. BMC Gastroenterol. 2012, 12, 46. [Google Scholar]
- Chang, L. A Study of Validation on Comorbidity Derived from Claims Data. Master’s Thesis, National Yang-Ming University, Taiwan, China, 2004. Available online: http://140.113.39.130/cgi-bin/gs32/ymgsweb.cgi/ccd=V8yNvb/search#result (accessed on 19 June 2023).
- Austin, P.C.; Stuart, E.A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat. Med. 2015, 34, 3661–3679. [Google Scholar]
- Ranganathan, P.; Pramesh, C.S.; Aggarwal, R. Common pitfalls in statistical analysis: Absolute risk reduction, relative risk reduction, and number needed to treat. Perspect. Clin. Res. 2016, 7, 51–53. [Google Scholar] [CrossRef]
- Tseng, C.H.; Chong, C.K.; Chan, T.T.; Bai, C.H.; You, S.L.; Chiou, H.Y.; Su, T.C.; Chen, C.J. Optimal anthropometric factor cutoffs for hyperglycemia, hypertension and dyslipidemia for the Taiwanese population. Atherosclerosis 2010, 210, 585–589. [Google Scholar] [PubMed]
- Tseng, C.H.; Huang, T.S. Pioglitazone with sulfonylurea: Glycemic and lipid effects in Taiwanese diabetic patients. Diabetes Res. Clin. Pract. 2005, 70, 193–194. [Google Scholar] [PubMed]
- Roman-Trufero, M.; Auner, H.W.; Edwards, C.M. Multiple myeloma metabolism—A treasure trove of therapeutic targets? Front. Immunol. 2022, 13, 897862. [Google Scholar] [PubMed]
- Otley, M.O.C.; Sinal, C.J. Adipocyte-cancer cell interactions in the bone microenvironment. Front. Endocrinol. 2022, 13, 903925. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.D.; Ferrara, A.; Peng, T.; Hedderson, M.; Bilker, W.B.; Quesenberry, C.P., Jr.; Vaughn, D.J.; Nessel, L.; Selby, J.; Strom, B.L. Risk of bladder cancer among diabetic patients treated with pioglitazone: Interim report of a longitudinal cohort study. Diabetes Care 2011, 34, 916–922. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.H. Pioglitazone and bladder cancer: A population-based study of Taiwanese. Diabetes Care 2012, 35, 278–280. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tseng, C.H. Rosiglitazone is not associated with an increased risk of bladder cancer. Cancer Epidemiol. 2013, 37, 385–389. [Google Scholar] [CrossRef]
- Tseng, C.H. Pioglitazone and prostate cancer risk in Taiwanese male patients with type 2 diabetes: A retrospective cohort study. World J. Men’s Health 2023, 41, 119–128. [Google Scholar] [CrossRef]
- Kao, L.T.; Xirasagar, S.; Lin, H.C.; Huang, C.Y. Association between pioglitazone use and prostate cancer: A population-based case-control study in the Han population. J. Clin. Pharmacol. 2019, 59, 344–349. [Google Scholar] [CrossRef]
- Boxall, N.; Bennett, D.; Hunger, M.; Dolin, P.; Thompson, P.L. Evaluation of exposure to pioglitazone and risk of prostate cancer: A nested case-control study. BMJ Open Diabetes Res. Care 2016, 4, e000303. [Google Scholar] [CrossRef]
- Wen, W.; Wu, P.; Gong, J.; Zhao, M.; Zhang, Z.; Chen, R.; Chen, H.; Sun, J. Association of pioglitazone with increased risk of prostate cancer and pancreatic cancer: A functional network study. Diabetes Ther. 2018, 9, 2229–2243. [Google Scholar] [CrossRef]
- Nissen, S.E.; Wolski, K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N. Engl. J. Med. 2007, 356, 2457–2471. [Google Scholar] [CrossRef]
- Tseng, C.H. Pioglitazone reduces dementia risk in patients with type 2 diabetes mellitus: A retrospective cohort analysis. J. Clin. Med. 2018, 7, 306. [Google Scholar] [CrossRef]
- Zhong, H.; Geng, R.; Zhang, Y.; Ding, J.; Liu, M.; Deng, S.; Tu, Q. Effects of peroxisome proliferator-activated receptor-gamma agonists on cognitive function: A systematic review and meta-analysis. Biomedicines 2023, 11, 246. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, R.B.; Kendall, D.M.; Deeg, M.A.; Buse, J.B.; Zagar, A.J.; Pinaire, J.A.; Tan, M.H.; Khan, M.A.; Perez, A.T.; Jacober, S.J.; et al. A comparison of lipid and glycemic effects of pioglitazone and rosiglitazone in patients with type 2 diabetes and dyslipidemia. Diabetes Care 2005, 28, 1547–1554. [Google Scholar] [CrossRef] [PubMed]
- Deeg, M.A.; Buse, J.B.; Goldberg, R.B.; Kendall, D.M.; Zagar, A.J.; Jacober, S.J.; Khan, M.A.; Perez, A.T.; Tan, M.H.; GLAI Study Investigators. Pioglitazone and rosiglitazone have different effects on serum lipoprotein particle concentrations and sizes in patients with type 2 diabetes and dyslipidemia. Diabetes Care 2007, 30, 2458–2464. [Google Scholar] [CrossRef]
- Ndakotsu, A.; Vivekanandan, G. The role of thiazolidinediones in the amelioration of nonalcoholic fatty liver disease: A systematic review. Cureus 2022, 14, e25380. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.S.; Lee, B.W. Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease. Clin. Mol. Hepatol. 2020, 26, 430–443. [Google Scholar] [CrossRef]
- An, J.; Sohn, J.H. Pharmacological advances in the treatment of nonalcoholic fatty liver diseases: Focused on global results of randomized controlled trials. Clin. Mol. Hepatol. 2023, 29, S268–S275. [Google Scholar] [CrossRef] [PubMed]
- Kernan, W.N.; Viscoli, C.M.; Furie, K.L.; Young, L.H.; Inzucchi, S.E.; Gorman, M.; Guarino, P.D.; Lovejoy, A.M.; Peduzzi, P.N.; Conwit, R.; et al. Pioglitazone after ischemic stroke or transient ischemic attack. N. Engl. J. Med. 2016, 374, 1321–1331. [Google Scholar] [CrossRef]
- Nesti, L.; Tricò, D.; Mengozzi, A.; Natali, A. Rethinking pioglitazone as a cardioprotective agent: A new perspective on an overlooked drug. Cardiovasc. Diabetol. 2021, 20, 109. [Google Scholar] [CrossRef]
- Giglio, R.V.; Papanas, N.; Rizvi, A.A.; Ciaccio, M.; Patti, A.M.; Ilias, I.; Pantea Stoian, A.; Sahebkar, A.; Janez, A.; Rizzo, M. An update on the current and emerging use of thiazolidinediones for type 2 diabetes. Medicina 2022, 58, 1475. [Google Scholar] [CrossRef]
- Aouali, N.; Palissot, V.; El-Khoury, V.; Moussay, E.; Janji, B.; Pierson, S.; Brons, N.H.; Kellner, L.; Bosseler, M.; Van Moer, K.; et al. Peroxisome proliferator-activated receptor gamma agonists potentiate the cytotoxic effect of valproic acid in multiple myeloma cells. Br. J. Haematol. 2009, 147, 662–671. [Google Scholar] [CrossRef]
- Huang, H.; Wu, D.; Fu, J.; Chen, G.; Chang, W.; Chow, H.C.; Leung, A.Y.; Liang, R. All-trans retinoic acid can intensify the growth inhibition and differentiation induction effect of rosiglitazone on multiple myeloma cells. Eur. J. Haematol. 2009, 83, 191–202. [Google Scholar] [CrossRef]
- Kumagai, T.; Ikezoe, T.; Gui, D.; O’Kelly, J.; Tong, X.J.; Cohen, F.J.; Said, J.W.; Koeffler, H.P. RWJ-241947 (MCC-555), a unique peroxisome proliferator-activated receptor-gamma ligand with antitumor activity against human prostate cancer in vitro and in beige/nude/X-linked immunodeficient mice and enhancement of apoptosis in myeloma cells induced by arsenic trioxide. Clin. Cancer Res. 2004, 10, 1508–1520. [Google Scholar]
- Benova, A.; Ferencakova, M.; Bardova, K.; Funda, J.; Prochazka, J.; Spoutil, F.; Cajka, T.; Dzubanova, M.; Balcaen, T.; Kerckhofs, G.; et al. Novel thiazolidinedione analog reduces a negative impact on bone and mesenchymal stem cell properties in obese mice compared to classical thiazolidinediones. Mol. Metab. 2022, 65, 101598. [Google Scholar] [CrossRef]
- Harrison, S.A.; Alkhouri, N.; Davison, B.A.; Sanyal, A.; Edwards, C.; Colca, J.R.; Lee, B.H.; Loomba, R.; Cusi, K.; Kolterman, O.; et al. Insulin sensitizer MSDC-0602K in non-alcoholic steatohepatitis: A randomized, double-blind, placebo-controlled phase IIb study. J. Hepatol. 2020, 72, 613–626. [Google Scholar] [CrossRef]
- Fujii, S.; Nakamura, S.; Oda, A.; Miki, H.; Tenshin, H.; Teramachi, J.; Hiasa, M.; Bat-Erdene, A.; Maeda, Y.; Oura, M.; et al. Unique anti-myeloma activity by thiazolidine-2,4-dione compounds with Pim inhibiting activity. Br. J. Haematol. 2018, 180, 246–258. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, Y.; Guo, Y.; Wang, H.; Fu, R. An overview of pim kinase as a target in multiple myeloma. Cancer Med. 2023, 12, 11746–11759. [Google Scholar] [CrossRef]
- Liu, Z.; Guo, Y.; Liu, X.; Cao, P.; Liu, H.; Dong, X.; Ding, K.; Fu, R. Pim-2 kinase regulates energy metabolism in multiple myeloma. Cancers 2022, 15, 67. [Google Scholar] [CrossRef]
- Burton, J.D.; Castillo, M.E.; Goldenberg, D.M.; Blumenthal, R.D. Peroxisome proliferator-activated receptor-gamma antagonists exhibit potent antiproliferative effects versus many hematopoietic and epithelial cancer cell lines. Anti-Cancer Drugs 2007, 18, 525–534. [Google Scholar] [CrossRef] [PubMed]
- Musto, P.; Anderson, K.C.; Attal, M.; Richardson, P.G.; Badros, A.; Hou, J.; Comenzo, R.; Du, J.; Durie, B.G.M.; San Miguel, J.; et al. Second primary malignancies in multiple myeloma: An overview and IMWG consensus. Ann. Oncol. 2017, 28, 228–245. [Google Scholar] [CrossRef] [PubMed]
- Poh, C.; Keegan, T.; Rosenberg, A.S. Second primary malignancies in multiple myeloma: A review. Blood Rev. 2021, 46, 100757. [Google Scholar] [CrossRef]
- Wang, J.; Lv, C.; Zhou, M.; Xu, J.Y.; Chen, B.; Wan, Y. Second. primary malignancy risk in multiple myeloma from 1975 to 2018. Cancers 2022, 14, 4919. [Google Scholar] [CrossRef]
- Liu, Y.; Hou, H.A.; Qiu, H.; Tang, C.H. Is the risk of second primary malignancy increased in multiple myeloma in the novel therapy era? A population-based, retrospective cohort study in Taiwan. Sci. Rep. 2020, 10, 14393. [Google Scholar] [CrossRef] [PubMed]
- Nien, F.J.; Tseng, C.H. A review on the clinical safety of thiazolidinediones. Formos. J. Endocrinol. Metab. 2014, 5, 2–14. [Google Scholar]
- Pearce, N.; Checkoway, H.; Kriebel, D. Bias in occupational epidemiology studies. Occup. Environ. Med. 2007, 64, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.Y.; Wu, M.Y.; Kuo, Y.H.; Tou, S.I.; Yen, H.R. Chinese herbal medicine is helpful for survival improvement in patients with multiple myeloma in Taiwan: A nationwide retrospective matched-cohort study. Integr. Cancer Ther. 2020, 19, 1534735420943280. [Google Scholar] [CrossRef]
- Mirhosseini, N.; Psihogios, A.; McLaren, M.D.; Seely, D. Vitamin D and multiple myeloma: A scoping review. Curr. Oncol. 2023, 30, 3263–3276. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.H.; Lee, K.Y.; Tseng, F.H. An updated review on cancer risk associated with incretin mimetics and enhancers. J. Environ. Sci. Health Part C 2015, 33, 67–124. [Google Scholar] [CrossRef] [PubMed]
- Busek, P.; Duke-Cohan, J.S.; Sedo, A. Does DPP-IV inhibition offer new avenues for therapeutic intervention in malignant disease? Cancers 2022, 14, 2072. [Google Scholar] [CrossRef]
- Arvanitakis, K.; Koufakis, T.; Kotsa, K.; Germanidis, G. How far beyond diabetes can the benefits of glucagon-like peptide-1 receptor agonists go? A review of the evidence on their effects on hepatocellular carcinoma. Cancers 2022, 14, 4651. [Google Scholar] [CrossRef]
- Hendryx, M.; Dong, Y.; Ndeke, J.M.; Luo, J. Sodium-glucose cotransporter 2 (SGLT2) inhibitor initiation and hepatocellular carcinoma prognosis. PLoS ONE 2022, 17, e0274519. [Google Scholar] [CrossRef]
- Luo, J.; Hendryx, M.; Dong, Y. Sodium-glucose cotransporter 2 (SGLT2) inhibitors and non-small cell lung cancer survival. Br. J. Cancer 2023, 128, 1541–1547. [Google Scholar] [CrossRef] [PubMed]
- Dutka, M.; Bobiński, R.; Francuz, T.; Garczorz, W.; Zimmer, K.; Ilczak, T.; Ćwiertnia, M.; Hajduga, M.B. SGLT-2 inhibitors in cancer treatment-mechanisms of action and emerging new perspectives. Cancers 2022, 14, 5811. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Ever Users (n = 86,999) | Never Users (n = 86,999) | Standardized Difference | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Basic data | |||||
| Age * (years) | 59.32 | 12.3 | 59.08 | 11.72 | −1.85 |
| Diabetes duration * (years) | 5.57 | 2.48 | 5.53 | 5.53 | −2.55 |
| Sex (men) | 45,907 | 52.77 | 45,835 | 52.68 | −0.07 |
| Occupation | |||||
| I | 34,333 | 39.46 | 34,394 | 39.53 | |
| II | 18,635 | 21.42 | 18,864 | 21.68 | 0.62 |
| III | 17,510 | 20.13 | 17,605 | 20.24 | 0.39 |
| IV | 16,521 | 18.99 | 16,136 | 18.55 | −1.13 |
| Living region | |||||
| Taipei | 31,203 | 35.87 | 31,090 | 35.74 | |
| Northern | 9601 | 11.04 | 9513 | 10.93 | −0.34 |
| Central | 16,908 | 19.43 | 16,981 | 19.52 | 0.29 |
| Southern | 12,060 | 13.86 | 12,151 | 13.97 | 0.23 |
| Kao-Ping and Eastern | 17,227 | 19.8 | 17,264 | 19.84 | 0.21 |
| Major comorbidities of diabetes mellitus | |||||
| Obesity | 4011 | 4.61 | 3977 | 4.57 | −0.29 |
| Hypertension | 64,495 | 74.13 | 64,187 | 73.78 | −0.72 |
| Dyslipidemia | 63,152 | 72.59 | 63,362 | 72.83 | 0.55 |
| Major complications of diabetes mellitus | |||||
| Hypoglycemia | 1367 | 1.57 | 1351 | 1.55 | −0.01 |
| Eye diseases | 15,892 | 18.27 | 15,562 | 17.89 | −0.70 |
| Nephropathy | 17,747 | 20.4 | 17,747 | 20.4 | −0.95 |
| Diabetic polyneuropathy | 17,523 | 20.14 | 17,214 | 19.79 | −0.55 |
| Peripheral arterial disease | 16,722 | 19.22 | 16,538 | 19.01 | −0.42 |
| Stroke | 20,546 | 23.62 | 20,012 | 23 | −1.37 |
| Ischemic heart disease | 34,784 | 39.98 | 34,287 | 39.41 | −1.14 |
| Comorbidities/clinical symptoms that might affect exposure or outcome | |||||
| Tobacco abuse | 1948 | 2.24 | 1930 | 2.22 | −0.10 |
| Alcohol-related diagnoses | 4676 | 5.37 | 4699 | 5.4 | 0.11 |
| Chronic obstructive pulmonary disease | 37,410 | 43 | 36,851 | 42.36 | −1.31 |
| Valvular heart disease | 6855 | 7.88 | 6715 | 7.72 | −0.67 |
| Heart failure | 12,187 | 14.01 | 11,822 | 13.59 | −1.18 |
| Head injury | 1228 | 1.41 | 1190 | 1.37 | −0.41 |
| Dementia | 4238 | 4.87 | 4014 | 4.61 | −1.21 |
| Parkinson’s disease | 1694 | 1.95 | 1609 | 1.85 | −0.69 |
| Helicobacter pylori infection | 641 | 0.74 | 628 | 0.72 | −0.20 |
| Hepatitis B virus infection | 602 | 0.69 | 1722 | 1.98 | −0.07 |
| Hepatitis C virus infection | 3192 | 3.67 | 3172 | 3.65 | −0.10 |
| Cirrhosis of liver without mention of alcohol | 3361 | 3.86 | 3370 | 3.87 | 0.07 |
| Other chronic nonalcoholic liver disease | 8434 | 9.69 | 8472 | 9.74 | 0.12 |
| Epstein-Barr virus infection | 602 | 0.69 | 605 | 0.7 | 0.05 |
| Human immunodeficiency virus disease | 53 | 0.06 | 41 | 0.05 | −0.65 |
| Autoimmune diseases | 6815 | 7.83 | 6734 | 7.74 | −0.35 |
| Organ transplantation | 234 | 0.27 | 224 | 0.26 | −0.20 |
| Immunosuppressants | 3099 | 3.56 | 3014 | 3.46 | −0.52 |
| Insomnia | 21,631 | 24.86 | 21,228 | 24.4 | −1.07 |
| Malaise and fatigue | 4411 | 5.07 | 4301 | 4.94 | −0.63 |
| History of some disorders of the central nervous system | 18,264 | 20.99 | 18,013 | 20.7 | −0.70 |
| Ocular pterygium | 3621 | 4.16 | 3661 | 4.21 | 0.25 |
| Disorders of thyroid gland | 9010 | 10.36 | 8876 | 10.2 | −0.66 |
| Nutritional deficiencies | 2194 | 2.52 | 2150 | 2.47 | −0.30 |
| Depression | 5953 | 6.84 | 5865 | 6.74 | −0.43 |
| Bone fractures | 17,997 | 20.69 | 17,693 | 20.34 | −0.87 |
| Benign neoplasm of bone and articular cartilage | 385 | 0.44 | 340 | 0.39 | −0.85 |
| Antidiabetic drugs | |||||
| Insulin | 2751 | 3.16 | 2697 | 3.1 | −0.63 |
| Sulfonylurea | 56,575 | 65.03 | 58,437 | 67.17 | 4.23 |
| Metformin | 56,695 | 65.17 | 56,695 | 65.17 | 0.92 |
| Meglitinide | 5205 | 5.98 | 5182 | 5.96 | −0.19 |
| Acarbose | 7518 | 8.64 | 7466 | 8.58 | −0.52 |
| Drugs commonly used by diabetes patients | |||||
| Aspirin | 45,717 | 52.55 | 45,375 | 52.16 | −0.73 |
| Statin | 44,908 | 51.62 | 44,915 | 51.63 | 0.04 |
| Fibrate | 30,913 | 35.53 | 31,122 | 35.77 | 0.58 |
| Angiotensin converting enzyme inhibitor/angiotensin receptor blocker | 55,466 | 63.75 | 55,366 | 63.64 | −0.10 |
| Calcium channel blocker | 46,946 | 53.96 | 46,636 | 53.61 | −0.61 |
| Thiazolidinedione Use | Incident Case Number | Cases Followed | Person-Years | Incidence Rate (per 100,000 Person-Years) | Hazard Ratio | 95% Confidence Interval | p Value |
|---|---|---|---|---|---|---|---|
| Never users | 47 | 86,999 | 358,126.16 | 13.12 | 1.000 | ||
| Ever users | 32 | 86,999 | 368,026.76 | 8.70 | 0.652 | (0.416–1.023) | 0.0625 |
| Median of cumulative duration of thiazolidinedione therapy (months) | |||||||
| Never users | 47 | 86,999 | 358,126.16 | 13.12 | 1.000 | ||
| <15.5 | 15 | 43,491 | 160,490.73 | 9.35 | 0.706 | (0.394–1.264) | 0.2417 |
| ≥15.5 | 17 | 43,508 | 207,536.04 | 8.19 | 0.603 | (0.346–1.051) | 0.0743 |
| Cumulative duration of thiazolidinedione therapy treated as a continuous variable | 0.980 | (0.963–0.997) | 0.0185 | ||||
| Models | Incident Case Number | Cases Followed | Person-Years | Incidence Rate (per 100,000 Person-Years) | Hazard Ratio | 95% Confidence Interval | p Value |
|---|---|---|---|---|---|---|---|
| 1. Excluding ever users of rosiglitazone | |||||||
| Never users | 47 | 86,999 | 358,126.16 | 13.12 | 1.000 | ||
| Ever users | 11 | 34,914 | 123,073.04 | 8.94 | 0.673 | (0.348–1.300) | 0.2380 |
| 2. Excluding ever users of pioglitazone | |||||||
| Never users | 47 | 86,999 | 358,126.16 | 13.12 | 1.000 | ||
| Ever users | 10 | 20,109 | 89,453.24 | 11.18 | 0.832 | (0.420–1.646) | 0.5966 |
| 3. Age < 65 years | |||||||
| Never users | 15 | 58,267 | 247,605.60 | 6.06 | 1.000 | ||
| Ever users | 15 | 59,680 | 262,621.53 | 5.71 | 0.927 | (0.543–1.898) | 0.8362 |
| 4. Age ≥ 65 years | |||||||
| Never users | 32 | 28,732 | 110,520.56 | 28.95 | 1.000 | ||
| Ever users | 17 | 27,319 | 105,405.24 | 16.13 | 0.550 | (0.305–0.992) | 0.0468 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tseng, C.-H. Thiazolidinedione Use Is Associated with a Borderline Lower Risk of Multiple Myeloma and a Significantly Lower Risk of Death in Patients with Type 2 Diabetes Mellitus in Taiwan. Cancers 2023, 15, 4276. https://doi.org/10.3390/cancers15174276
Tseng C-H. Thiazolidinedione Use Is Associated with a Borderline Lower Risk of Multiple Myeloma and a Significantly Lower Risk of Death in Patients with Type 2 Diabetes Mellitus in Taiwan. Cancers. 2023; 15(17):4276. https://doi.org/10.3390/cancers15174276
Chicago/Turabian StyleTseng, Chin-Hsiao. 2023. "Thiazolidinedione Use Is Associated with a Borderline Lower Risk of Multiple Myeloma and a Significantly Lower Risk of Death in Patients with Type 2 Diabetes Mellitus in Taiwan" Cancers 15, no. 17: 4276. https://doi.org/10.3390/cancers15174276
APA StyleTseng, C.-H. (2023). Thiazolidinedione Use Is Associated with a Borderline Lower Risk of Multiple Myeloma and a Significantly Lower Risk of Death in Patients with Type 2 Diabetes Mellitus in Taiwan. Cancers, 15(17), 4276. https://doi.org/10.3390/cancers15174276





