Reduction of Blood Loss by Means of the Cavitron Ultrasonic Surgical Aspirator for Thoracoscopic Salvage Anatomic Lung Resections
Abstract
Simple Summary
Abstract
1. Introduction
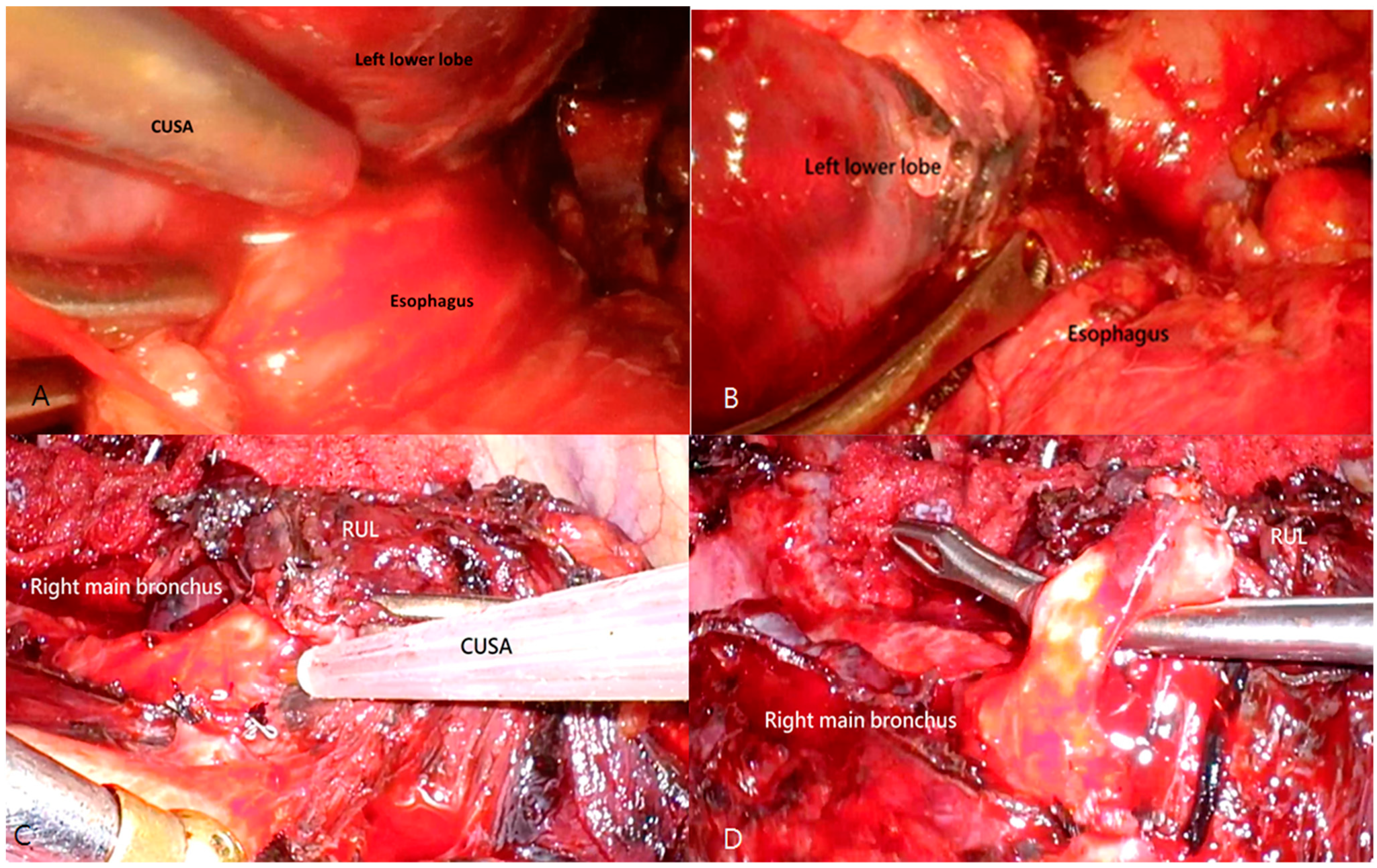
2. Materials and Methods
2.1. Patient Inclusion
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Patient and Treatment Parameters in Salvage Anatomic Lung Resections with and without CUSA
3.2. Factors Affecting Complications in Thoracoscopic Salvage Anatomic Lung Resections
3.3. Factors Affecting Intraoperative Blood Loss in Thoracoscopic Salvage Anatomic Lung Resections
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chang, Y.-J.; Huang, J.-Y.; Lin, C.-H.; Wang, B.-Y. Survival and treatment of lung cancer in Taiwan between 2010 and 2016. J. Clin. Med. 2021, 10, 4675. [Google Scholar] [CrossRef] [PubMed]
- Postmus, P.; Kerr, K.; Oudkerk, M.; Senan, S.; Waller, D.; Vansteenkiste, J.; Escriu, C.; Peters, S. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv1–iv21. [Google Scholar] [CrossRef] [PubMed]
- Ettinger, D.S.; Wood, D.E.; Aggarwal, C.; Aisner, D.L.; Akerley, W.; Bauman, J.R.; Bharat, A.; Bruno, D.S.; Chang, J.Y.; Chirieac, L.R. NCCN guidelines insights: Non–small cell lung cancer, version 1.2020: Featured updates to the NCCN guidelines. J. Natl. Compr. Cancer Netw. 2019, 17, 1464–1472. [Google Scholar] [CrossRef]
- Kuzmik, G.A.; Detterbeck, F.C.; Decker, R.H.; Boffa, D.J.; Wang, Z.; Oliva, I.B.; Kim, A.W. Pulmonary resections following prior definitive chemoradiation therapy are associated with acceptable survival. Eur. J. Cardio-Thorac. Surg. 2013, 44, e66–e70. [Google Scholar] [CrossRef]
- Schreiner, W.; Dudek, W.; Lettmaier, S.; Fietkau, R.; Sirbu, H. Should salvage surgery be considered for local recurrence after definitive chemoradiation in locally advanced non-small cell lung cancer? J. Cardiothorac. Surg. 2016, 11, 9. [Google Scholar] [CrossRef] [PubMed]
- Bauman, J.E.; Mulligan, M.S.; Martins, R.G.; Kurland, B.F.; Eaton, K.D.; Wood, D.E. Salvage lung resection after definitive radiation (>59 Gy) for non-small cell lung cancer: Surgical and oncologic outcomes. Ann. Thorac. Surg. 2008, 86, 1632–1639. [Google Scholar] [CrossRef]
- Adachi, K.; Kuroda, H.; Tanahashi, M.; Takao, M.; Ohde, Y.; Yokoi, K.; Tarukawa, T. Survival benefits of salvage surgery for primary lung cancer based on routine clinical practice. Thorac. Cancer 2021, 12, 1716–1720. [Google Scholar] [CrossRef]
- Kouritas, V.K.; Kefaloyannis, E.; Tcherveniakov, P.; Milton, R.; Chaudhuri, N.; Brunelli, A.; Papagiannopoulos, K. Do pleural adhesions influence the outcome of patients undergoing major lung resection? Interact. Cardiovasc. Thorac. Surg. 2017, 25, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Kaba, E.; Ozyurtkan, M.O.; Ayalp, K.; Cosgun, T.; Alomari, M.R.; Toker, A. Salvage thoracic surgery in patients with lung cancer: Potential indications and benefits. J. Cardiothorac. Surg. 2018, 13, 13. [Google Scholar] [CrossRef] [PubMed]
- Hamada, A.; Soh, J.; Mitsudomi, T. Salvage surgery after definitive chemoradiotherapy for patients with non-small cell lung cancer. Transl. Lung Cancer Res. 2021, 10, 555. [Google Scholar] [CrossRef]
- Mizobuchi, T.; Yamamoto, N.; Nakajima, M.; Baba, M.; Miyoshi, K.; Nakayama, H.; Watanabe, S.-I.; Katoh, R.; Kohno, T.; Kamiyoshihara, M. Salvage surgery for local recurrence after carbon ion radiotherapy for patients with lung cancer. Eur. J. Cardio-Thorac. Surg. 2015, 49, 1503–1509. [Google Scholar] [CrossRef] [PubMed]
- Sawada, S.; Suehisa, H.; Ueno, T.; Yamashita, M. Eight cases of salvage pulmonary resection for residual disease or isolated local recurrence detected after definitive chemoradiotherapy for N2 Stage-IIIA lung cancer. Asian J. Surg. 2017, 40, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Furrer, K.; Weder, W.; Eboulet, E.I.; Betticher, D.; Pless, M.; Stupp, R.; Krueger, T.; Perentes, J.Y.; Schmid, R.A.; Lardinois, D. Extended resection for potentially operable patients with stage III non-small cell lung cancer after induction treatment. J. Thorac. Cardiovasc. Surg. 2022, 164, 1587–1602. [Google Scholar] [CrossRef] [PubMed]
- Cerfolio, R.J.; Bryant, A.S.; Jones, V.L.; Cerfolio, R.M. Pulmonary resection after concurrent chemotherapy and high dose (60 Gy) radiation for non-small cell lung cancer is safe and may provide increased survival. Eur. J. Cardio-Thorac. Surg. 2009, 35, 718–723. [Google Scholar] [CrossRef]
- Goudie, E.; Tahiri, M.; Liberman, M. Present and future application of energy devices in thoracic surgery. Thorac. Surg. Clin. 2016, 26, 229–236. [Google Scholar] [CrossRef]
- Rau, H.; Duessel, A.; Wurzbacher, S. The use of water-jet dissection in open and laparoscopic liver resection. HPB 2008, 10, 275–280. [Google Scholar] [CrossRef]
- Williams, J. Histologic evaluation of tissues sectioned by ultrasonically powered instruments (a preliminary report). Mt. Sinai J. Med. 1979, 46, 105–106. [Google Scholar]
- Huang, K.-W.; Lee, P.-H.; Kusano, T.; Reccia, I.; Jayant, K.; Habib, N. Impact of cavitron ultrasonic surgical aspirator (CUSA) and bipolar radiofrequency device (Habib-4X) based hepatectomy for hepatocellular carcinoma on tumour recurrence and disease-free survival. Oncotarget 2017, 8, 93644. [Google Scholar] [CrossRef]
- Moggia, E.; Rouse, B.; Simillis, C.; Li, T.; Vaughan, J.; Davidson, B.R.; Gurusamy, K.S. Methods to decrease blood loss during liver resection: A network meta-analysis. Cochrane Database Syst. Rev. 2016, 10, CD010683. [Google Scholar]
- Simillis, C.; Li, T.; Vaughan, J.; Becker, L.A.; Davidson, B.R.; Gurusamy, K.S. Methods to decrease blood loss during liver resection: A network meta-analysis. Cochrane Database Syst. Rev. 2014, 4, CD010683. [Google Scholar]
- Eisenberg, M.; Deboever, N.; Antonoff, M.B. Salvage surgery in lung cancer following definitive therapies. J. Surg. Oncol. 2023, 127, 319–328. [Google Scholar] [CrossRef]
- Timmerman, R.; McGarry, R.; Yiannoutsos, C.; Papiez, L.; Tudor, K.; DeLuca, J.; Ewing, M.; Abdulrahman, R.; DesRosiers, C.; Williams, M. Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. J. Clin. Oncol. 2006, 24, 4833–4839. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Li, X.; Tang, W.; Xie, P.; Tan, X. Primary tumor location in lung cancer: The evaluation and administration. Chin. Med. J. 2022, 135, 127–136. [Google Scholar]
- Brunelli, A.; Kim, A.W.; Berger, K.I.; Addrizzo-Harris, D.J. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143, e166S–e190S. [Google Scholar] [PubMed]
- Charlson, M.E.; Carrozzino, D.; Guidi, J.; Patierno, C. Charlson comorbidity index: A critical review of clinimetric properties. Psychother. Psychosom. 2022, 91, 8–35. [Google Scholar]
- Clavien, P.A.; Barkun, J.; De Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; De Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [PubMed]
- Socinski, M.A.; Obasaju, C.; Gandara, D.; Hirsch, F.R.; Bonomi, P.; Bunn, P.A., Jr.; Kim, E.S.; Langer, C.J.; Natale, R.B.; Novello, S.; et al. Current and Emergent Therapy Options for Advanced Squamous Cell Lung Cancer. J. Thorac. Oncol. 2018, 13, 165–183. [Google Scholar] [CrossRef] [PubMed]
- Sonobe, M.; Yutaka, Y.; Nakajima, D.; Hamaji, M.; Menju, T.; Ohsumi, A.; Chen-Yoshikawa, T.F.; Sato, T.; Date, H. Salvage surgery after chemotherapy or chemoradiotherapy for initially unresectable lung carcinoma. Ann. Thorac. Surg. 2019, 108, 1664–1670. [Google Scholar]
- Yang, C.-F.J.; Meyerhoff, R.R.; Stephens, S.J.; Singhapricha, T.; Toomey, C.B.; Anderson, K.L.; Kelsey, C.; Harpole, D.; D’Amico, T.A.; Berry, M.F. Long-term outcomes of lobectomy for non-small cell lung cancer after definitive radiation treatment. Ann. Thorac. Surg. 2015, 99, 1914–1920. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, E.K.; Vauthey, J.-N.; Ellis, L.M.; Ellis, V.; Pollock, R.; Broglio, K.R.; Hess, K.; Curley, S.A. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann. Surg. 2004, 239, 818. [Google Scholar] [CrossRef]
- Finch, R.; Malik, H.; Hamady, Z.; Al-Mukhtar, A.; Adair, R.; Prasad, K.; Lodge, J.; Toogood, G. Effect of type of resection on outcome of hepatic resection for colorectal metastases. J. Br. Surg. 2007, 94, 1242–1248. [Google Scholar] [CrossRef]
- Storck, B.; Rutgers, E.; Gortzak, E.; Zoetmulder, F. The impact of the CUSA ultrasonic dissection device on major liver resections. Neth. J. Surg. 1991, 43, 99–101. [Google Scholar]
- Hardy, K.; Martin, J.; Fletcher, D.; Maclellan, D.; Jones, R. Hepatic resection: Value of operative ultrasound and ultrasonic dissection. Aust. N. Z. J. Surg. 1989, 59, 621–623. [Google Scholar] [CrossRef] [PubMed]
- Zwart, M.J.; Görgec, B.; Arabiyat, A.; Nota, C.L.; van der Poel, M.J.; Fichtinger, R.S.; Berrevoet, F.; van Dam, R.M.; Aldrighetti, L.; Fuks, D.J.H. Pan-European survey on the implementation of robotic and laparoscopic minimally invasive liver surgery. HPB 2022, 24, 322–331. [Google Scholar] [CrossRef]
- Cheng, Y.K.; Qin, Q.Y.; Huang, X.Y.; Lan, P.; Wang, L.; Gao, X.; Ma, T.H. Effect of interval between preoperative radiotherapy and surgery on clinical outcome and radiation proctitis in rectal cancer from FOWARC trial. Cancer Med. 2020, 9, 912–919. [Google Scholar] [CrossRef]
- Bergamini, C.; Ferris, R.L.; Xie, J.; Mariani, G.; Ali, M.; Holmes, W.C.; Harrington, K.; Psyrri, A.; Cavalieri, S.; Licitra, L.J.H.; et al. Bleeding complications in patients with squamous cell carcinoma of the head and neck. Head Neck 2021, 43, 2844–2858. [Google Scholar] [CrossRef]
- Kim, H.K.; Cho, J.H.; Choi, Y.S.; Zo, J.I.; Shim, Y.M.; Park, K.; Ahn, M.-J.; Ahn, Y.C.; Kim, K.; Kim, J. Outcomes of neoadjuvant concurrent chemoradiotherapy followed by surgery for non-small-cell lung cancer with N2 disease. Lung Cancer 2016, 96, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Mayer, M.; Kann, R.; Weder, W.; Zouhair, A.; Betticher, D.C.; Roth, A.D.; Stahel, R.A.; Majno, S.B.; Peters, S. Neoadjuvant chemotherapy and radiotherapy followed by surgery in selected patients with stage IIIB non-small-cell lung cancer: A multicentre phase II trial. Lancet Oncol. 2009, 10, 785–793. [Google Scholar]
- Dickhoff, C.; Dahele, M.; Paul, M.; van de Ven, P.; de Langen, A.; Senan, S.; Smit, E.; Hartemink, K. Salvage surgery for locoregional recurrence or persistent tumor after high dose chemoradiotherapy for locally advanced non-small cell lung cancer. Lung Cancer 2016, 94, 108–113. [Google Scholar] [CrossRef]
- Bograd, A.J.; Mann, C.; Gorden, J.A.; Gilbert, C.R.; Farivar, A.S.; Aye, R.W.; Louie, B.E.; Vallières, E. Salvage lung resections after definitive chemoradiotherapy: A safe and effective oncologic option. Ann. Thorac. Surg. 2020, 110, 1123–1130. [Google Scholar] [CrossRef]
- Antonoff, M.B.; Correa, A.M.; Sepesi, B.; Nguyen, Q.-N.; Walsh, G.L.; Swisher, S.G.; Vaporciyan, A.A.; Mehran, R.J.; Hofstetter, W.L.; Rice, D.C. Salvage pulmonary resection after stereotactic body radiotherapy: A feasible and safe option for local failure in selected patients. J. Thorac. Cardiovasc. Surg. 2017, 154, 689–699. [Google Scholar] [PubMed]
- Lin, M.-W.; Yu, S.-L.; Hsu, Y.-C.; Chen, Y.-M.; Lee, Y.-H.; Hsiao, Y.-J.; Lin, J.-W.; Su, T.-J.; Yang, C.-F.J.; Chiang, X.-H. Salvage Surgery for Advanced Lung Adenocarcinoma after EGFR Tyrosine Kinase Inhibitor Treatment. Ann. Thorac. Surg. 2023, 116, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Yen, Y.T.; Lai, W.W.; Huang, W.L.; Chang, C.C.; Tseng, Y.L. Outcomes of salvage lung resections in advanced EGFR-mutant lung adenocarcinomas under EGFR TKIs. Thorac. Cancer 2021, 12, 2655–2665. [Google Scholar] [CrossRef] [PubMed]
- Berry, M.F.; Hanna, J.; Tong, B.C.; Burfeind, W.R., Jr.; Harpole, D.H.; D’Amico, T.A.; Onaitis, M. Risk factors for morbidity after lobectomy for lung cancer in elderly patients. Ann. Thorac. Surg. 2009, 88, 1093–1099. [Google Scholar] [CrossRef]
- Sui, X.; Zhao, H.; Wang, J.; Yang, F.; Yang, F.; Li, Y.; Surgery, C. Outcome of VATS lobectomy for elderly non-small cell lung cancer: A propensity score-matched study. Ann. Thorac. Cardiovasc. Surg. 2015, 21, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, A.K.; Nakagawa, K.; Nakayama, Y.; Ohe, Y.; Yotsukura, M.; Uchida, S.; Asakura, K.; Yoshida, Y.; Watanabe, S.-I. Salvage Surgery Compared to Surgery After Induction Chemoradiation Therapy for Advanced Lung Cancer. Ann. Thorac. Surg. 2022, 114, 2087–2092. [Google Scholar] [CrossRef] [PubMed]
- Mitsuyoshi, A.; Inoguchi, K.; Yokoyama, D. The Cavitron ultrasonic surgical aspirator with a low amplitude is a useful dissection device for surgical procedures: Application to vascular detachment and lymph node dissection. Updates Surg. 2016, 68, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Casal, R.F.; Vial, M.R.; Miller, R.; Mudambi, L.; Grosu, H.B.; Eapen, G.A.; Jimenez, C.A.; Morice, R.C.; Cornwell, L.; Ost, D.J. What exactly is a centrally located lung tumor? Results of an online survey. Ann. Am. Thorac. Soc. 2017, 14, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Forde, P.M.; Chaft, J.E.; Smith, K.N.; Anagnostou, V.; Cottrell, T.R.; Hellmann, M.D.; Zahurak, M.; Yang, S.C.; Jones, D.R.; Broderick, S. Neoadjuvant PD-1 blockade in resectable lung cancer. N. Engl. J. Med. 2018, 378, 1976–1986. [Google Scholar] [CrossRef]
- Li, N.; Ying, J.; Tao, X.; Zhang, F.; Zhao, Z.; Ling, Y.; Gao, Y.; Zhao, J.; Xue, Q.; Mao, Y. Efficacy and safety of neoadjuvant PD-1 blockade with sintilimab in resectable squamous non-small cell lung cancer (sqNSCLC). J. Clin. Oncol. 2019, 37, 8531. [Google Scholar] [CrossRef]
- Provencio, M.; Nadal, E.; Insa, A.; García-Campelo, M.R.; Casal-Rubio, J.; Dómine, M.; Majem, M.; Rodríguez-Abreu, D.; Martínez-Martí, A.; Carpeño, J.D.C. Neoadjuvant chemotherapy and nivolumab in resectable non-small-cell lung cancer (NADIM): An open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020, 21, 1413–1422. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Fu, F.; Hu, H.; Wang, S.; Li, Y.; Hu, H.; Chen, H. Gefitinib as neoadjuvant therapy for resectable stage II-IIIA non–small cell lung cancer: A phase II study. J. Thorac. Cardiovasc. Surg. 2021, 161, 434–442.e2. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Guo, Y.-J.; Song, J.; Wang, Y.-R.; Zhang, S.-L.; Huang, L.-T.; Zhao, J.-Z.; Jing, W.; Han, C.-B.; Ma, J.-T. Neoadjuvant EGFR-TKI therapy for EGFR-mutant NSCLC: A systematic review and pooled analysis of five prospective clinical trials. Front. Oncol. 2021, 10, 586596. [Google Scholar] [CrossRef] [PubMed]

| Non-CUSA | CUSA | p | |
|---|---|---|---|
| N = 15 | N = 7 | ||
| Age, median (IQR) | 62 (56–69) | 67 (58–74) | 0.447 |
| Sex | |||
| Female | 3 (20.0) | 2 (28.6) | 0.739 |
| Male | 12 (80.0) | 5 (71.4) | |
| Morbidity score | 5.0 (3–9) | 5.0 (4–8) | 0.837 |
| Smokers | 10 (67.7) | 5 (71.4) | 0.999 |
| Pathology | 0.227 | ||
| Adenocarcinoma | 7 (46.7) | 3 (42.9) | |
| Squamous cell carcinoma | 5 (33.3) | 2 (28.6) | |
| Others | 3 (20.0) | 2 (28.6) | |
| Differentiation | 0.999 | ||
| Moderately differentiated | 10 (66.7) | 4 (57.1) | |
| Poorly differentiated | 4 (26.7) | 2 (28.6) | |
| Tumor size (mm, IQR) | 40.0 (30–70) | 44.0 (28–60) | 0.891 |
| Stage | 0.273 | ||
| IIIB+C | 9 (60.0) | 5 (71.4) | |
| IV | 6 (40.0) | 2 (28.6) | |
| FEV1, Median (IQR) | 84.0 (73.0–89.0) | 71.0 (58.0–100.0) | 0.332 |
| DLCO, Median (IQR) | 75.0 (65.0–90.0) | 71.0 (55.0–79.0) | 0.298 |
| ACCP risk grade | 0.334 | ||
| Low risk | 12 (80.0) | 4 (57.1) | |
| Moderate risk | 3 (20.0) | 3 (42.9) | |
| Immunotherapy | 3 (20.0) | 3 (42.9) | 0.334 |
| Targeted therapy | 6 (40.0) | 3 (42.9) | 0.999 |
| Radiotherapy | 4 (26.7) | 4 (57.1) | 0.343 |
| Chemotherapy | 14 (93.3) | 5 (71.4) | 0.227 |
| Operation | 0.445 | ||
| Lobectomy | 12 (80.0) | 7 (100) | |
| Bilobectomy | 2 (13.3) | 0 (0.0) | |
| Pneumonectomy | 1 (6.7) | 0 (0.0) | |
| pCR | 3 (20.0) | 3 (42.9) | 0.334 |
| ALL Type | Non-CUSA | CUSA | p-Value |
|---|---|---|---|
| N = 15 | N = 7 | ||
| Blood loss, median (IQR) | 250 (150–450) | 100 (100–200) | 0.014 * |
| Surgical duration, median (IQR) | 3.8 (3.5–4.5) | 6.0 (4.0–7.0) | 0.021 * |
| Duration of hospitalization, days, median (IQR) | 9.0 (8.0–12.0) | 11 (8–13) | 0.731 |
| ICU admission | 4.0 (26.7) | 4.0 (57.1) | 0.343 |
| Length of ICU admission (days), median (IQR) | 2.0 (1.0–5.0) | 2.5 (1.5–5.5) | 0.368 |
| Period of chest tube insertion, days, median (IQR) | 6.0 (5.0–9.0) | 7.0 (4.0–9.0) | >0.999 |
| Persistent air leak, n (%) | 4.0 (26.7) | 1.0 (14.3) | >0.999 |
| All complications | 6.0 (40.0) | 3.0 (42.9) | >0.999 |
| Grade III complications | 2.0 (13.3) | 0.0 (0.0) | >0.999 |
| Complication | With | Without | p | |
|---|---|---|---|---|
| N = 9 (100) | N = 13 (100) | |||
| Sex | ||||
| Male | n (%) | 7 (77.8) | 10 (76.9) | 0.962 |
| Female | n (%) | 2 (22.2) | 3 (23.1) | |
| Age | median (IQR) | 70 (68, 73) | 58 (56, 62) | 0.001 * |
| OR (95% CI) | 1.355 | (1.065, 1.724) | 0.013 ** | |
| Smoker | n (%) | 7 (77.8) | 8 (61.5) | 0.648 |
| Charlson comorbidity index | median (IQR) | 8 (5, 9) | 4(3, 8) | 0.071 |
| ACCP low risk | n (%) | 5 (55.6) | 11 (84.6) | 0.178 |
| Pathology | 0.021 * | |||
| Adenocarcinoma | n (%) | 1 (11.1) | 9 (69.2) | |
| Squamous cell carcinoma | n (%) | 4 (44.4) | 3 (23.0) | |
| Others | n (%) | 4 (44.4) | 1 (7.7) | |
| Tumor stage | ||||
| IIIB+C | n (%) | 5 (55.6) | 9 (69.2) | 0.147 |
| IV | n (%) | 4 (44.4) | 4 (3.08) | |
| Tumor size | n (%) | 49 (40, 70) | 39(30, 45) | 0.235 |
| Radiotherapy | n (%) | 6 (66.7) | 2 (15.4) | 0.026 * |
| Chemotherapy | n (%) | 9 (100) | 10 (76.9) | 0.204 |
| Target Therapy | n (%) | 2 (22.2) | 7 (53.8) | 0.203 |
| Immunotherapy | n (%) | 4 (44.4) | 2 (15.4) | 0.178 |
| CUSA | n (%) | 3 (33.3) | 4 (30.8) | 0.899 |
| Blood Loss, mL | ||||
|---|---|---|---|---|
| n | Median (IQR) | p | ||
| Age | year | 22 | −210.4 (−494.4, 73.5) † | 0.583 |
| Gender | male | 17 | 150 (150, 350) | 0.401 |
| female | 5 | 100 (100, 350) | ||
| Smoker | yes | 15 | 200 (150, 350) | 0.237 |
| no | 7 | 150 (100, 250) | ||
| ACCP | Low | 16 | 150 (125, 135) | 0.999 |
| Moderate | 6 | 175 (100, 350) | ||
| Morbidity score | 22 | 37.8 (−6.9, 82.4) † | 0.093 | |
| Tumor size | mm | 22 | 0.06 (−7.1, 7.3) † | 0.121 |
| Tumor stage | IIIB+C | 14 | 150 (100, 350) | 0.224 |
| IV | 8 | 225 (200, 250) | ||
| Pathology | AdenoCa | 10 | 150 (100, 350) | 0.611 |
| SCC | 7 | 150 (150, 350) | ||
| Others | 5 | 350 (150, 350) | ||
| Radiotherapy | yes | 8 | 275 (200, 350) | 0.330 |
| no | 14 | 150 (150, 250) | ||
| 282.9 (19.7, 546.3) †,‡ | 0.037 ** | |||
| Chemotherapy | yes | 19 | 150 (100, 350) | 0.160 |
| no | 3 | 100 (50, 250) | ||
| Target therapy | yes | 9 | 150 (100, 250) | 0.556 |
| no | 13 | 150 (150, 350) | ||
| Immunotherapy | yes | 6 | 250 (150, 350) | 0.910 |
| no | 16 | 150 (150, 350) | ||
| CUSA | yes | 7 | 100 (100, 200) | 0.014 * |
| no | 15 | 250 (150, 450) | ||
| −296.7 (−568.6, −24.8) †,‡ | 0.034 ** | |||
| pCR | yes | 6 | 150 (100, 350) | 0.541 |
| no | 16 | 175 (125, 400) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.-H.; Tsai, S.C.-S.; Lin, F.C.-F. Reduction of Blood Loss by Means of the Cavitron Ultrasonic Surgical Aspirator for Thoracoscopic Salvage Anatomic Lung Resections. Cancers 2023, 15, 4069. https://doi.org/10.3390/cancers15164069
Wang Y-H, Tsai SC-S, Lin FC-F. Reduction of Blood Loss by Means of the Cavitron Ultrasonic Surgical Aspirator for Thoracoscopic Salvage Anatomic Lung Resections. Cancers. 2023; 15(16):4069. https://doi.org/10.3390/cancers15164069
Chicago/Turabian StyleWang, Yu-Hsiang, Stella Chin-Shaw Tsai, and Frank Cheau-Feng Lin. 2023. "Reduction of Blood Loss by Means of the Cavitron Ultrasonic Surgical Aspirator for Thoracoscopic Salvage Anatomic Lung Resections" Cancers 15, no. 16: 4069. https://doi.org/10.3390/cancers15164069
APA StyleWang, Y.-H., Tsai, S. C.-S., & Lin, F. C.-F. (2023). Reduction of Blood Loss by Means of the Cavitron Ultrasonic Surgical Aspirator for Thoracoscopic Salvage Anatomic Lung Resections. Cancers, 15(16), 4069. https://doi.org/10.3390/cancers15164069









