Telemedicine in Neuro-Oncology—An Evaluation of Remote Consultations during the COVID-19 Pandemic
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Collection of Demographic Data
2.3. Statistical Analyses
3. Results
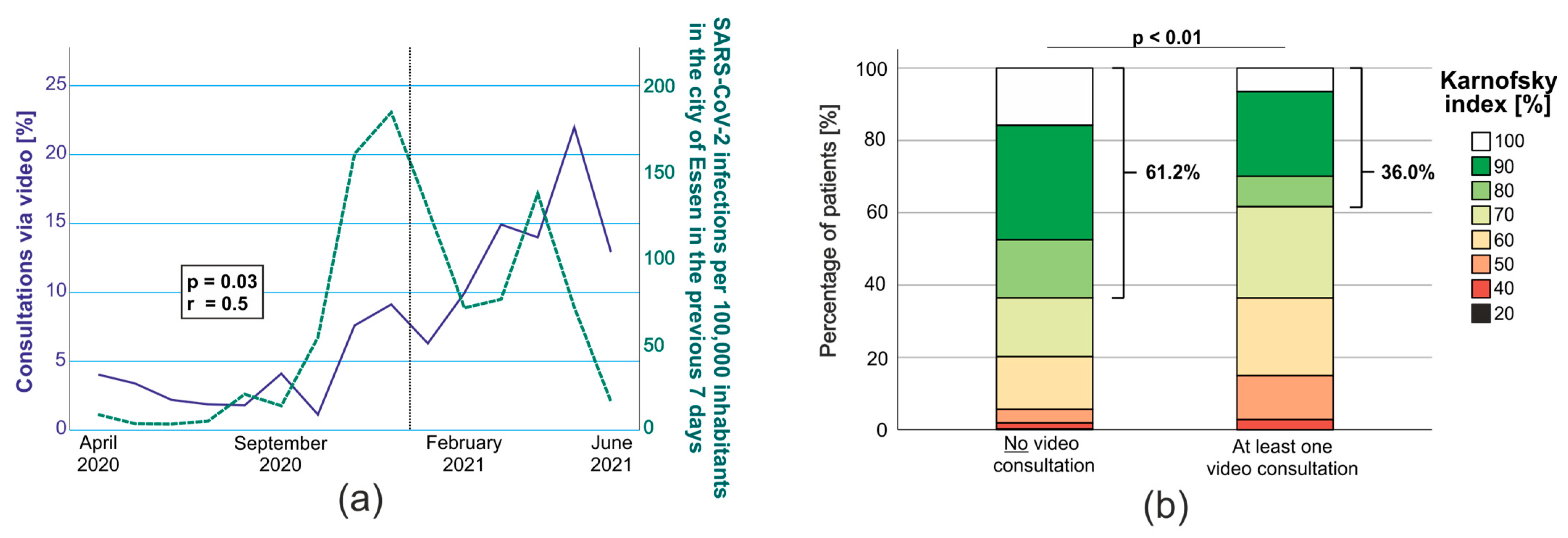
3.1. Patients with Glioblastoma, Long Travel Distance and Low Karnofsky Were More Likely to Choose VC
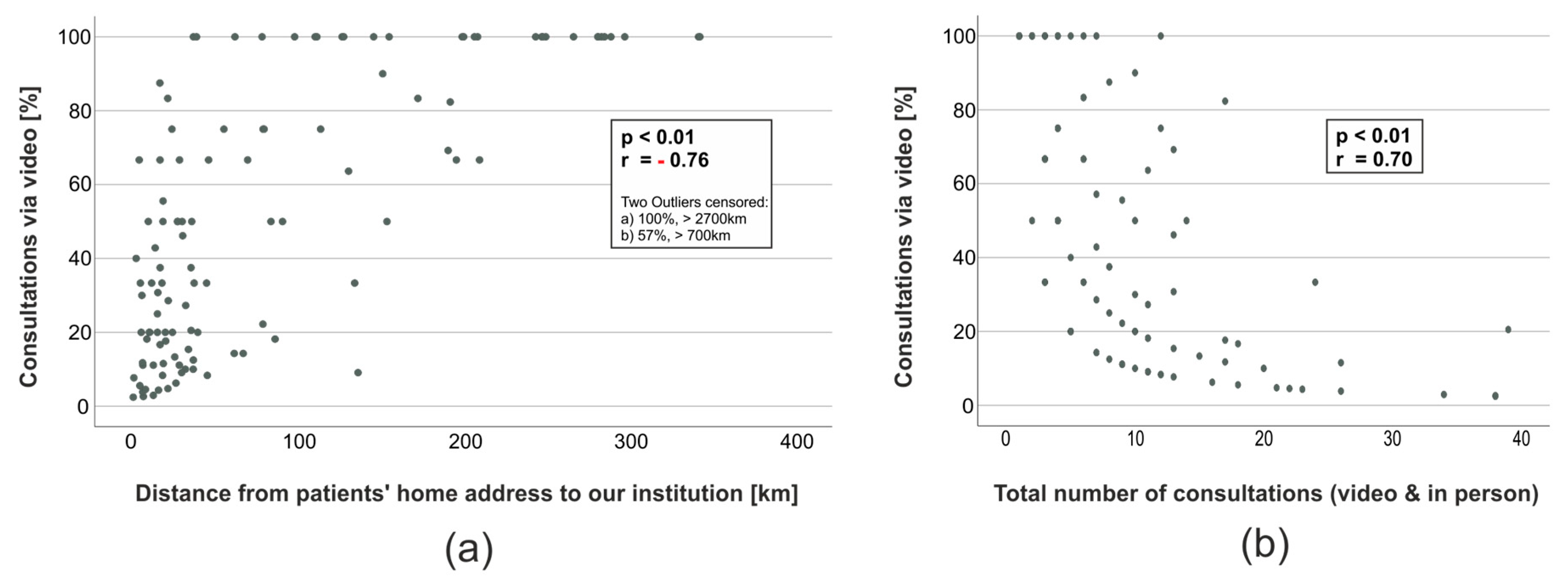
3.2. Ratio of VC Was Associated with the Travel Distance and the Number of Consultations in Total
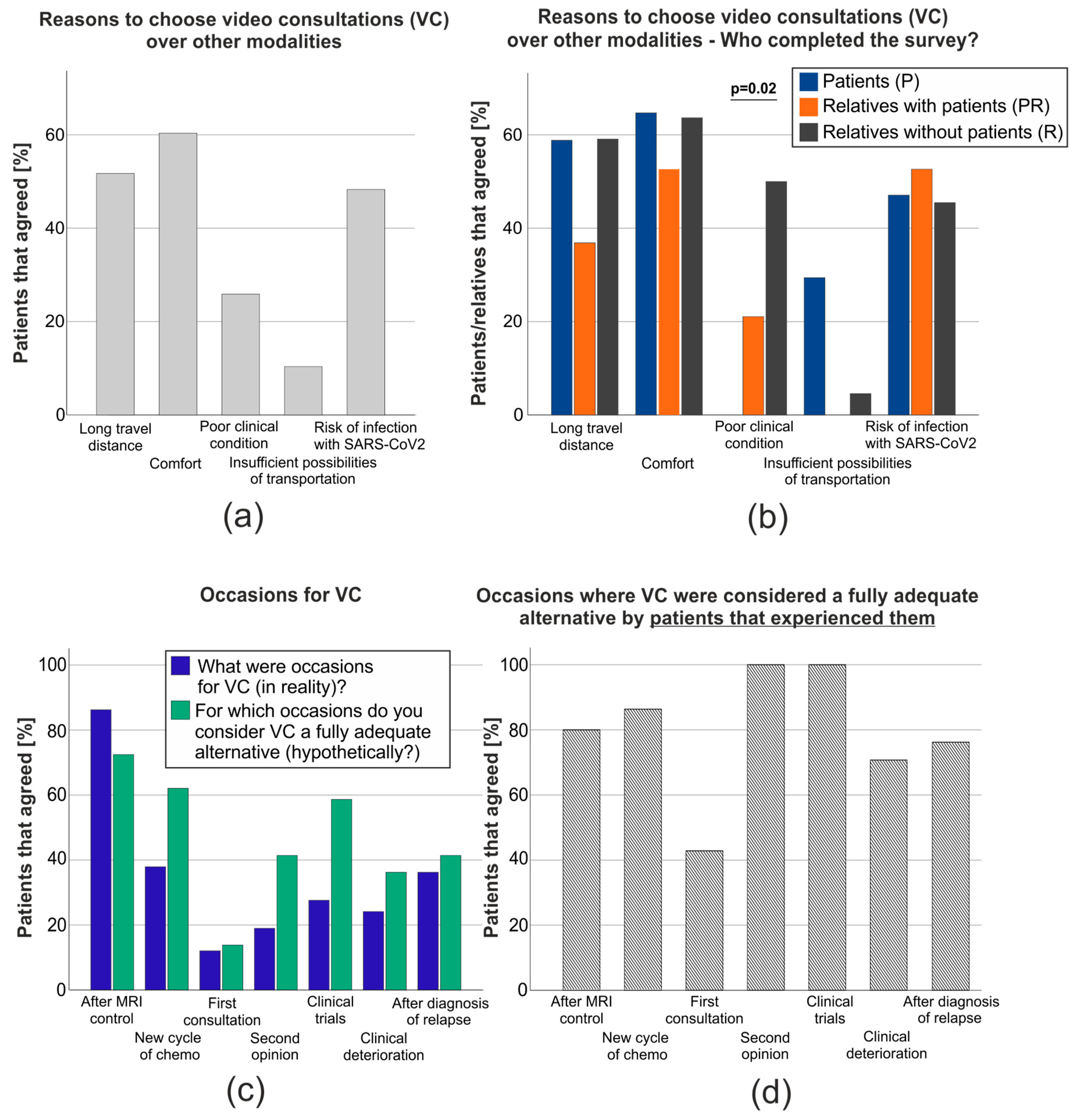
3.3. VC Were Considered an Adequate Alternative for Most Occasions but Not for the Initial Consultation
3.4. VC Had a Significantly Lower Expense yet Were Found to Be Slightly Less Personal Than Face-to-Face Consultations
3.5. The Offer of VC Made Patients Feel Safer
3.6. Patients Reported Interest in Implementing Further Telemedicine Modalities in Their Treatment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- John Hopkins UoM. 2022. Available online: https://coronavirus.jhu.edu/map.html (accessed on 10 July 2023).
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Kane-Gill, S.L.; Rincon, F. Expansion of Telemedicine Services: Telepharmacy, Telestroke, Teledialysis, Tele-Emergency Medicine. Crit. Care Clin. 2019, 35, 519–533. [Google Scholar] [CrossRef]
- Smith, A.C.; Gray, L.C. Telemedicine across the ages. Med. J. Aust. 2009, 190, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Richardson, E.; Aissat, D.; Williams, G.A.; Fahy, N. Keeping what works: Remote consultations during the COVID-19 pandemic. Eurohealth 2020, 26, 73–76. [Google Scholar]
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; He, J.; et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA 2020, 323, 1775–1776. [Google Scholar] [CrossRef] [PubMed]
- Shirke, M.M.; Shaikh, S.A.; Harky, A. Implications of Telemedicine in Oncology during the COVID-19 Pandemic. Acta Biomed. 2020, 91, e2020022. [Google Scholar]
- Clinical Management of COVID-19: Living Guideline, 13 January 2023; WHO/2019-nCoV/clinical/2023.1; World Health Organization: Geneva, Switzerland, 2023.
- Al-Shamsi, H.O.; Alhazzani, W.; Alhuraiji, A.; Coomes, E.A.; Chemaly, R.F.; Almuhanna, M.; Wolff, R.A.; Ibrahim, N.K.; Chua, M.L.; Hotte, S.J.; et al. A Practical Approach to the Management of Cancer Patients During the Novel Coronavirus Disease 2019 (COVID-19) Pandemic: An International Collaborative Group. Oncologist 2020, 25, e936–e945. [Google Scholar] [CrossRef]
- Nayak, L.; DeAngelis, L.M.; Brandes, A.A.; Peereboom, D.M.; Galanis, E.; Lin, N.U.; Soffietti, R.; Macdonald, D.R.; Chamberlain, M.; Perry, J.; et al. The Neurologic Assessment in Neuro-Oncology (NANO) scale: A tool to assess neurologic function for integration into the Response Assessment in Neuro-Oncology (RANO) criteria. Neuro-Oncol. 2017, 19, 625–635. [Google Scholar] [CrossRef]
- Coelho, J.J.; Arnold, A.; Nayler, J.; Tischkowitz, M.; MacKay, J. An assessment of the efficacy of cancer genetic counselling using real-time videoconferencing technology (telemedicine) compared to face-to-face consultations. Eur. J. Cancer 2005, 41, 2257–2261. [Google Scholar] [CrossRef]
- Allen, A.; Hayes, J. Patient satisfaction with telemedicine in a rural clinic. Am. J. Public Health 1994, 84, 1693. [Google Scholar] [CrossRef] [PubMed]
- Luz, P.L.D. Telemedicine and the Doctor/Patient Relationship. Arq. Bras. Cardiol. 2019, 113, 100–102. [Google Scholar] [CrossRef] [PubMed]
- Fonkem, E.; Gatson, N.T.N.; Tadipatri, R.; Cole, S.; Azadi, A.; Sanchez, M.; Stefanowicz, E. Telemedicine review in neuro-oncology: Comparative experiential analysis for Barrow Neurological Institute and Geisinger Health during the 2020 COVID-19 pandemic. Neurooncol. Pract. 2021, 8, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Strowd, R.E.; Dunbar, E.M.; Gan, H.K.; Kurz, S.; Jordan, J.T.; Mandel, J.J.; Mohile, N.A.; Nevel, K.S.; Taylor, J.W.; Ullrich, N.J.; et al. Practical guidance for telemedicine use in neuro-oncology. Neuro-Oncol. Pr. 2022, 9, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Qaddoumi, I.; Mansour, A.; Musharbash, A.; Drake, J.; Swaidan, M.; Tihan, T.; Bouffet, E. Impact of telemedicine on pediatric neuro-oncology in a developing country: The Jordanian-Canadian experience. Pediatr. Blood Cancer 2006, 48, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Qaddoumi, I.; Musharbash, A.; Elayyan, M.; Mansour, A.; Al-Hussaini, M.; Drake, J.; Swaidan, M.; Bartels, U.; Bouffet, E. Closing the survival gap: Implementation of medulloblastoma protocols in a low-income country through a twinning program. Int. J. Cancer 2007, 122, 1203–1206. [Google Scholar] [CrossRef]
- Al-Qudimat, M.R.; Day, S.; Almomani, T.; Odeh, D.; Qaddoumi, I. Clinical nurse coordinators: A new generation of highly specialized oncology nursing in Jordan. J. Pediatr. Hematol. Oncol. 2009, 31, 38–41. [Google Scholar] [CrossRef]
- Qaddoumi, I.; Bouffet, E. Supplementation of a successful pediatric neuro-oncology telemedicine-based twinning program by e-mails. Telemed. J. E Health 2009, 15, 975–982. [Google Scholar] [CrossRef]
- Boele, F.W.; van Uden-Kraan, C.F.; Hilverda, K.; Weimer, J.; Donovan, H.S.; Drappatz, J.; Lieberman, F.S.; Leeuw, I.V.-D.; Sherwood, P.R. Neuro-oncology family caregivers’ view on keeping track of care issues using eHealth systems: It’s a question of time. J. Neuro-Oncol. 2017, 134, 157–167. [Google Scholar] [CrossRef]
- Boele, F.W.; Klein, M.; Leeuw, I.M.V.-D.; Cuijpers, P.; Heimans, J.J.; Snijders, T.J.; Vos, M.; Bosma, I.; Tijssen, C.C.; Reijneveld, J.C.; et al. Internet-based guided self-help for glioma patients with depressive symptoms: A randomized controlled trial. J. Neuro-Oncol. 2017, 137, 191–203. [Google Scholar] [CrossRef]
- Hincapié, M.A.; Gallego, J.C.; Gempeler, A.; Piñeros, J.A.; Nasner, D.; Escobar, M.F. Implementation and Usefulness of Telemedicine During the COVID-19 Pandemic: A Scoping Review. J. Prim. Care Community Health 2020, 11, 2150132720980612. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.R.; Lawrence, J.; Williams, D., Jr.; Mainous, I.A. Population-Level Interest and Telehealth Capacity of US Hospitals in Response to COVID-19: Cross-Sectional Analysis of Google Search and National Hospital Survey Data. JMIR Public Health Surveill. 2020, 6, e18961. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.; Hayes, J. Patient satisfaction with teleoncology: A pilot study. Telemed. J. 1995, 1, 41–46. [Google Scholar] [CrossRef]
- Tudor, C. The Impact of the COVID-19 Pandemic on the Global Web and Video Conferencing SaaS Market. Electronics 2022, 11, 2633. [Google Scholar] [CrossRef]
- Czaja, S.J.; Charness, N.; Fisk, A.D.; Hertzog, C.; Nair, S.N.; Rogers, W.A.; Sharit, J. Factors predicting the use of technology: Findings from the center for research and education on aging and technology enhancement (create). Psychol. Aging 2006, 21, 333–352. [Google Scholar] [CrossRef]
- Ambroggi, M.; Biasini, C.; Del Giovane, C.; Fornari, F.; Cavanna, L. Distance as a Barrier to Cancer Diagnosis and Treatment: Review of the Literature. Oncologist 2015, 20, 1378–1385. [Google Scholar] [CrossRef] [PubMed]
- Tracey, E.; McCaughan, B.; Badgery-Parker, T.; Young, J.; Armstrong, B.K. Patients with localized non-small cell lung cancer miss out on curative surgery with distance from specialist care. ANZ J. Surg. 2015, 85, 658–663. [Google Scholar] [CrossRef]
- Nattinger, A.B.; Kneusel, R.T.; Hoffmann, R.G.; Gilligan, M.A. Relationship of distance from a radiotherapy facility and initial breast cancer treatment. J. Natl. Cancer Inst. 2001, 93, 1344–1346. [Google Scholar] [CrossRef]
- Voti, L.; Richardson, L.C.; Reis, I.M.; Fleming, L.E.; Mackinnon, J.; Coebergh, J.W. Treatment of local breast carcinoma in Florida: The role of the distance to radiation therapy facilities. Cancer 2006, 106, 201–207. [Google Scholar] [CrossRef]
- Dickinson, R.; Hall, S.; Sinclair, J.E.; Bond, C.; Murchie, P. Using technology to deliver cancer follow-up: A systematic review. BMC Cancer 2014, 14, 311. [Google Scholar] [CrossRef]
- Sirintrapun, S.J.; Lopez, A.M. Telemedicine in Cancer Care. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Gray, J.; Brain, K.; Iredale, R.; Alderman, J.; France, E.; Hughes, H. A pilot study of telegenetics. J. Telemed. Telecare 2000, 6, 245–247. [Google Scholar] [CrossRef]
- Triantafillou, V.; Rajasekaran, K. A Commentary on the Challenges of Telemedicine for Head and Neck Oncologic Patients during COVID-19. Otolaryngol. Head Neck Surg. 2020, 163, 81–82. [Google Scholar] [CrossRef] [PubMed]
- Levine, S.R.; Gorman, M. “Telestroke”: The application of telemedicine for stroke. Stroke 1999, 30, 464–469. [Google Scholar] [CrossRef]
- Wechsler, L.R.; Demaerschalk, B.M.; Schwamm, L.H.; Adeoye, O.M.; Audebert, H.J.; Fanale, C.V.; Hess, D.C.; Majersik, J.J.; Nystrom, K.V.; Reeves, M.J.; et al. Telemedicine Quality and Outcomes in Stroke: A Scientific Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2017, 48, e3–e25. [Google Scholar] [CrossRef]
- Ali, S.F.; Hubert, G.J.; Switzer, J.A.; Majersik, J.J.; Backhaus, R.; Shepard, L.W.; Vedala, K.; Schwamm, L.H. Validating the TeleStroke Mimic Score: A Prediction Rule for Identifying Stroke Mimics Evaluated Over Telestroke Networks. Stroke 2018, 49, 688–692. [Google Scholar] [CrossRef]
- Wood, J.; Wallin, M.; Finkelstein, J. Can a low-cost webcam be used for a remote neurological exam? Stud. Health Technol. Inform. 2013, 190, 30–32. [Google Scholar]
- Kane, R.L.; Bever, C.T.; Ehrmantraut, M.; Forte, A.; Culpepper, W.J.; Wallin, M.T. Teleneurology in patients with multiple sclerosis: EDSS ratings derived remotely and from hands-on examination. J. Telemed. Telecare 2008, 14, 190–194. [Google Scholar] [CrossRef]
- Hubble, J.P.; Pahwa, R.; Michalek, D.K.; Thomas, C.; Koller, W.C. Interactive video conferencing: A means of providing interim care to Parkinson’s disease patients. Mov. Disord. 1993, 8, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Bull, M.T.; Darwin, K.; Venkataraman, V.; Wagner, J.; Beck, C.A.; Dorsey, E.R.; Biglan, K.M. A Pilot Study of Virtual Visits in Huntington Disease. J. Huntingtons Dis. 2014, 3, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Amarendran, V.; George, A.; Gersappe, V.; Krishnaswamy, S.; Warren, C. The reliability of telepsychiatry for a neuropsychiatric assessment. Telemed. e-Health 2011, 17, 223–225. [Google Scholar] [CrossRef]
- Russell, T.G.; Jull, G.A.; Wootton, R. The diagnostic reliability of Internet-based observational kinematic gait analysis. J. Telemed. Telecare 2003, 9 (Suppl. S2), S48–S51. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, J.H.; Jhoo, J.H.; Lee, K.U.; Kim, K.W.; Lee, D.Y.; Woo, J.I. A Telemedicine System As a Care Modality for Dementia Patients in Korea. Alzheimer Dis. Assoc. Disord. 2000, 14, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Tsiakiri, A.; Koutzmpi, V.; Megagianni, S.; Toumaian, M.; Geronikola, N.; Despoti, A.; Kanellopoulou, S.; Arampatzi, X.; Margioti, E.; Davila, A.; et al. Remote neuropsychological evaluation of older adults. Appl. Neuropsychol. Adult 2022, 1–8. [Google Scholar] [CrossRef]
- Lindauer, A.; Seelye, A.; Lyons, B.; Dodge, H.H.; Mattek, N.; Mincks, K.; Kaye, J.; Erten-Lyons, D. Dementia Care Comes Home: Patient and Caregiver Assessment via Telemedicine. Gerontologist 2017, 57, e85–e93. [Google Scholar] [CrossRef] [PubMed]
- Müller, K.I.; Alstadhaug, K.B.; Bekkelund, S.I. Acceptability, Feasibility, and Cost of Telemedicine for Nonacute Headaches: A Randomized Study Comparing Video and Traditional Consultations. J. Med. Internet Res. 2016, 18, e140. [Google Scholar] [CrossRef]
- Müller, K.I.; Alstadhaug, K.B.; Bekkelund, S.I. Headache patients’ satisfaction with telemedicine: A 12-month follow-up randomized non-inferiority trial. Eur. J. Neurol. 2017, 24, 807–815. [Google Scholar] [CrossRef]
- Qubty, W.; Patniyot, I.; Gelfand, A. Telemedicine in a pediatric headache clinic: A prospective survey. Neurology 2018, 90, e1702–e1705. [Google Scholar] [CrossRef]
- Rasmusson, K.A.; Hartshorn, J.C. A comparison of epilepsy patients in a traditional ambulatory clinic and a telemedicine clinic. Epilepsia 2005, 46, 767–770. [Google Scholar] [CrossRef]
- Al Hussona, M.; Maher, M.; Chan, D.; Micieli, J.A.; Jain, J.D.; Khosravani, H.; Izenberg, A.; Kassardjian, C.D.; Mitchell, S.B. The Virtual Neurologic Exam: Instructional Videos and Guidance for the COVID-19 Era. Can. J. Neurol. Sci./J. Can. Sci. Neurol. 2020, 47, 598–603. [Google Scholar] [CrossRef]
- Sabesan, S.; Simcox, K.; Marr, I. Medical oncology clinics through videoconferencing: An acceptable telehealth model for rural patients and health workers. Intern. Med. J. 2012, 42, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Bunn, F.; Byrne, G.; Kendall, S. The effects of telephone consultation and triage on healthcare use and patient satisfaction: A systematic review. Br. J. Gen. Pract. 2005, 55, 956–961. [Google Scholar] [PubMed]
- Leibowitz, R.; Day, S.; Dunt, D. A systematic review of the effect of different models of after-hours primary medical care services on clinical outcome, medical workload, and patient and GP satisfaction. Fam. Pract. 2003, 20, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Turner, J.; O’Cathain, A.; Knowles, E.; Nicholl, J. Impact of the urgent care telephone service NHS 111 pilot sites: A controlled before and after study. BMJ Open 2013, 3, e003451. [Google Scholar] [CrossRef]
- McKinstry, B.; Watson, P.; Pinnock, H.; Heaney, D.; Sheikh, A. Telephone consulting in primary care: A triangulated qualitative study of patients and providers. Br. J. Gen. Pract. 2009, 59, e209–e218. [Google Scholar] [CrossRef]
- Hewitt, H.; Gafaranga, J.; McKinstry, B. Comparison of face-to-face and telephone consultations in primary care: Qualitative analysis. Br. J. Gen. Pract. 2010, 60, e201–e212. [Google Scholar] [CrossRef]
- Bell, K.R.; Temkin, N.R.; Esselman, P.C.; Doctor, J.N.; Bombardier, C.H.; Fraser, R.T.; Hoffman, J.M.; Powell, J.M.; Dikmen, S. The Effect of a Scheduled Telephone Intervention on Outcome After Moderate to Severe Traumatic Brain Injury: A Randomized Trial. Arch. Phys. Med. Rehabil. 2005, 86, 851–856. [Google Scholar] [CrossRef]
- Bell, K.R.; Hoffman, J.M.; Temkin, N.R.; Powell, J.M.; Fraser, R.T.; Esselman, P.C.; Barber, J.K.; Dikmen, S. The effect of telephone counselling on reducing post-traumatic symptoms after mild traumatic brain injury: A randomized trial. J. Neurol. Neurosurg. Psychiatry 2008, 79, 1275–1281. [Google Scholar] [CrossRef]
- Bombardier, C.H.; Bell, K.R.; Temkin, N.R.; Fann, J.R.; Hoffman, J.; Dikmen, S. The efficacy of a scheduled telephone intervention for ameliorating depressive symptoms during the first year after traumatic brain injury. J. Head Trauma Rehabil. 2009, 24, 230–238. [Google Scholar] [CrossRef]
- Dobkin, R.D.; Menza, M.; Allen, L.A.; Tiu, J.; Friedman, J.; Bienfait, K.L.; Gara, M.A.; Mark, M.H. Telephone-Based Cognitive–Behavioral Therapy for Depression in Parkinson Disease. J. Geriatr. Psychiatry Neurol. 2011, 24, 206–214. [Google Scholar] [CrossRef]
- Dobkin, R.D. The relationship between telephone-administered cognitive-behavioral therapy for depression and neuropsychological functioning in Parkinson’s disease. J. Neuropsychiatry Clin. Neurosci. 2014, 26, E10–E11. [Google Scholar] [CrossRef][Green Version]
- Calleo, J.S.; Amspoker, A.B.; Sarwar, A.I.; Kunik, M.E.; Jankovic, J.; Marsh, L.; York, M.; Stanley, M.A. A Pilot Study of a Cognitive–Behavioral Treatment for Anxiety and Depression in Patients With Parkinson Disease. J. Geriatr. Psychiatry Neurol. 2015, 28, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Shalowitz, D.I.; Smith, A.G.; Bell, M.C.; Gibb, R.K. Teleoncology for gynecologic cancers. Gynecol. Oncol. 2015, 139, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Salami, A.C.; Barden, G.M.; Castillo, D.L.; Hanna, M.; Petersen, N.J.; Davila, J.A.; Naik, A.D.; Anaya, D.A. Establishment of a Regional Virtual Tumor Board Program to Improve the Process of Care for Patients With Hepatocellular Carcinoma. J. Oncol. Pract. 2015, 11, e66–e74. [Google Scholar] [CrossRef]
- Russo, J.E.; McCool, R.R.; Davies, L. VA Telemedicine: An Analysis of Cost and Time Savings. Telemed. e-Health 2016, 22, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Waller, M.; Stotler, C. Telemedicine: A Primer. Curr. Allergy Asthma Rep. 2018, 18, 54. [Google Scholar] [CrossRef] [PubMed]


| Patients That Never Participated in VC (n = 498) | Patients That Participated in VC at Least Once (n = 114) | p-Value | |
|---|---|---|---|
| Sex | Male: 247 (49.6%) Female: 251 (50.4%) | Male: 63 (55.3%) Female: 51 (44.7%) | 0.16 (Fisher) |
| Age | 52.0 years (39–63 years) | 54.5 years (43–62 years) | 0.43 (MWU) |
| Karnofsky index | 20%: 1 (0.2%) 40%: 8 (1.6%) 50%: 18 (3.6%) 60%: 70 (14.1%) 70%: 78 (15.7%) 80%: 77 (15.5%) 90%: 152 (30.1%) 100%: 76 (15.3%) Not applicable: 18 (3.6%) | 20%: 0 (0%) 40%: 3 (2.6%) 50%: 13 (11.4%) 60%: 23 (20.2%) 70%: 27 (23.7%) 80%: 9 (7.9%) 90%: 25 (21.9%) 100%: 7 (6.1%) Not applicable: 7 (6.1%) | <0.01 (MWU) |
| CNS WHO grade of malignancy | Grade 1: 23 (4.6%) Grade 2: 96 (19.3%) Grade 3: 97 (19.5%) Grade 4: 212 (42.6%) No CNS WHO grade: 70 (14.1%) | Grade 1: 0 (0%) Grade 2: 9 (7.9%) Grade 3: 14 (12.2%) Grade 4: 80 (70.2%) No CNS WHO grade: 11 (9.6%) | <0.01 (Χ²) |
| Diagnosis | Glioblastoma/Gliosarcoma: 196 (39.4%) Astrocytoma IDHwt: 31 (6.2%) Astrocytoma IDHmut: 87 (17.5%) Oligodendroglioma: 51 (10.2%) Meningioma: 17 (3.4%) Metastasis: 18 (3.6%) Pilocytic Astrocytoma: 7 (1.4%) Craniopharyngioma: 2 (0.4%) Medulloblastoma: 7 (1.4%) Lymphoma: 2 (0.4%) Ependymoma: 9 (1.8%) Others: 71 (14.2%) | Glioblastoma/Gliosarcoma: 79 (69.2%) Astrocytoma IDHwt: 6 (5.3%) Astrocytoma IDHmut: 11 (9.6%) Oligodendroglioma: 3 (2.6%) Meningioma: 0 (0%) Metastasis: 3 (2.6%) Pilocytic Astrocytoma: 1 (0.9%) Craniopharyngioma: 0 (0%) Medulloblastoma: 0 (0%) Lymphoma: 0 (0%) Ependymoma: 0 (0%) Others: 11 (9.6%) | <0.01 (Χ2) |
| Distance | 14.4 km (6.3–25.6 km) | 37.5 km (17.2–138.9 km) | <0.01 (MWU) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feldheim, J.; Schmidt, T.; Oster, C.; Feldheim, J.; Stuschke, M.; Stummer, W.; Grauer, O.; Scheffler, B.; Hagemann, C.; Sure, U.; et al. Telemedicine in Neuro-Oncology—An Evaluation of Remote Consultations during the COVID-19 Pandemic. Cancers 2023, 15, 4054. https://doi.org/10.3390/cancers15164054
Feldheim J, Schmidt T, Oster C, Feldheim J, Stuschke M, Stummer W, Grauer O, Scheffler B, Hagemann C, Sure U, et al. Telemedicine in Neuro-Oncology—An Evaluation of Remote Consultations during the COVID-19 Pandemic. Cancers. 2023; 15(16):4054. https://doi.org/10.3390/cancers15164054
Chicago/Turabian StyleFeldheim, Jonas, Teresa Schmidt, Christoph Oster, Julia Feldheim, Martin Stuschke, Walter Stummer, Oliver Grauer, Björn Scheffler, Carsten Hagemann, Ulrich Sure, and et al. 2023. "Telemedicine in Neuro-Oncology—An Evaluation of Remote Consultations during the COVID-19 Pandemic" Cancers 15, no. 16: 4054. https://doi.org/10.3390/cancers15164054
APA StyleFeldheim, J., Schmidt, T., Oster, C., Feldheim, J., Stuschke, M., Stummer, W., Grauer, O., Scheffler, B., Hagemann, C., Sure, U., Kleinschnitz, C., Lazaridis, L., Kebir, S., & Glas, M. (2023). Telemedicine in Neuro-Oncology—An Evaluation of Remote Consultations during the COVID-19 Pandemic. Cancers, 15(16), 4054. https://doi.org/10.3390/cancers15164054









