Tas-102 for Refractory Metastatic Colorectal Cancer: A Multicenter Retrospective Cohort Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Study Population
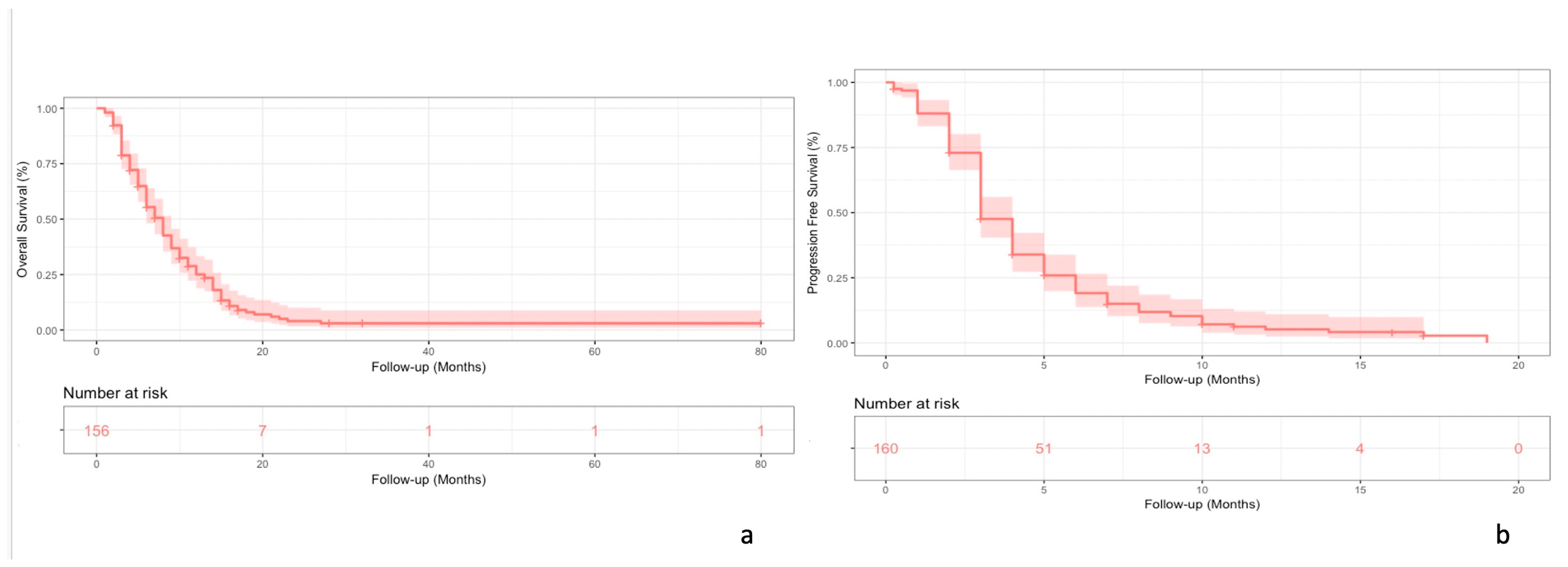
3.2. Effectiveness
3.3. Safety
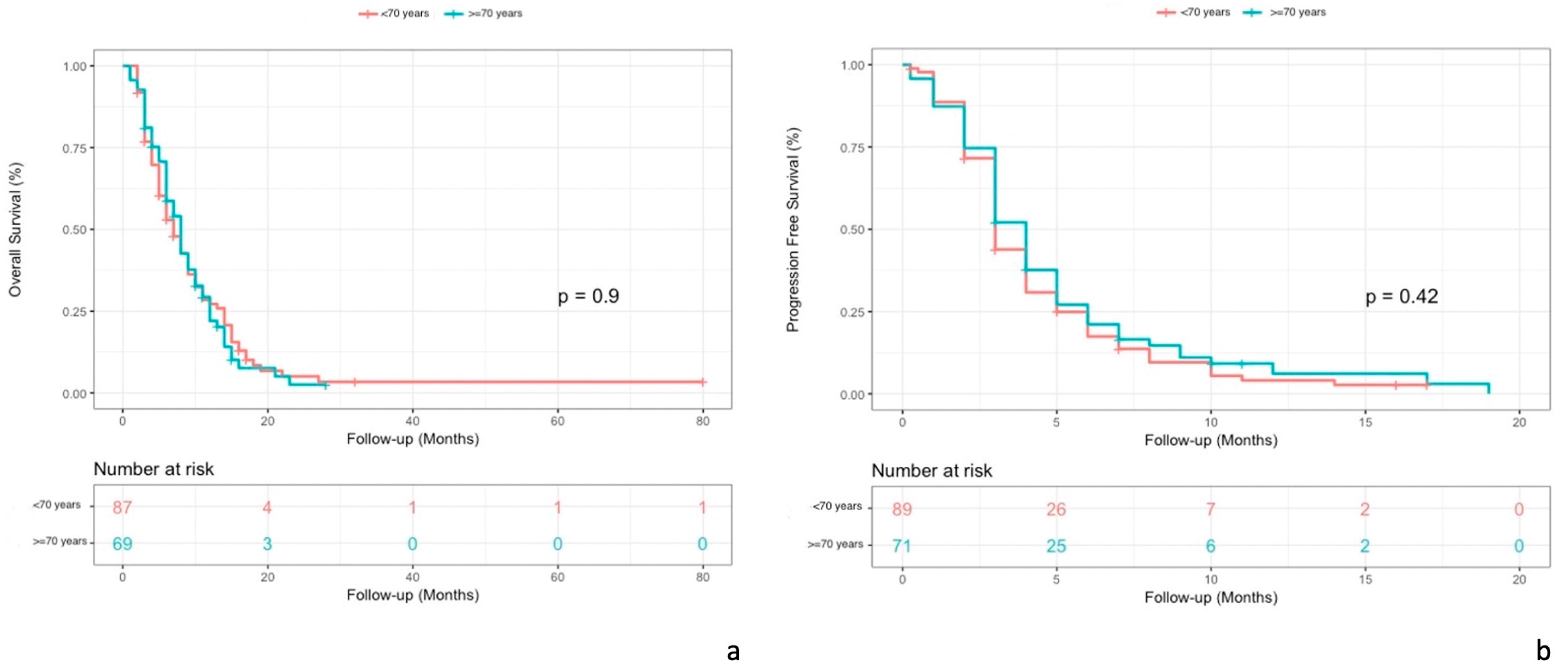
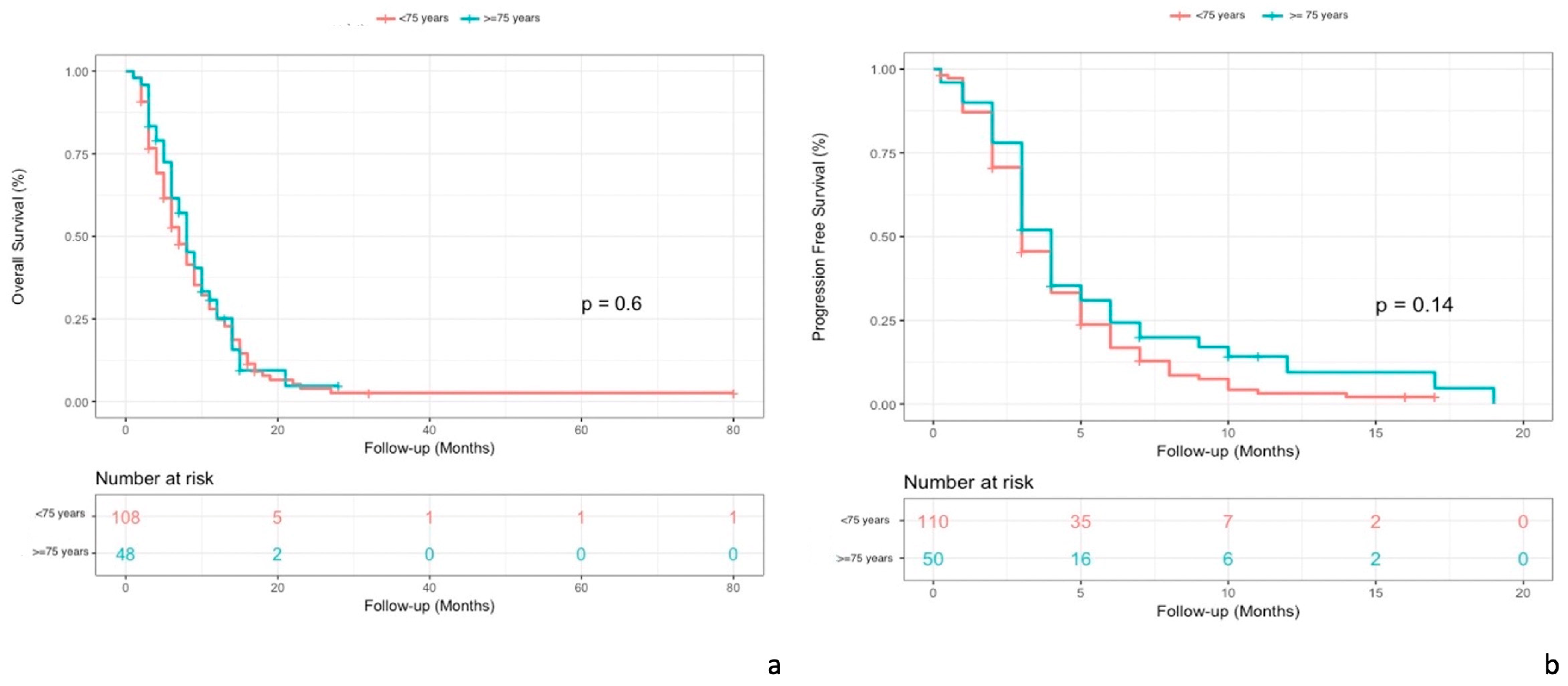
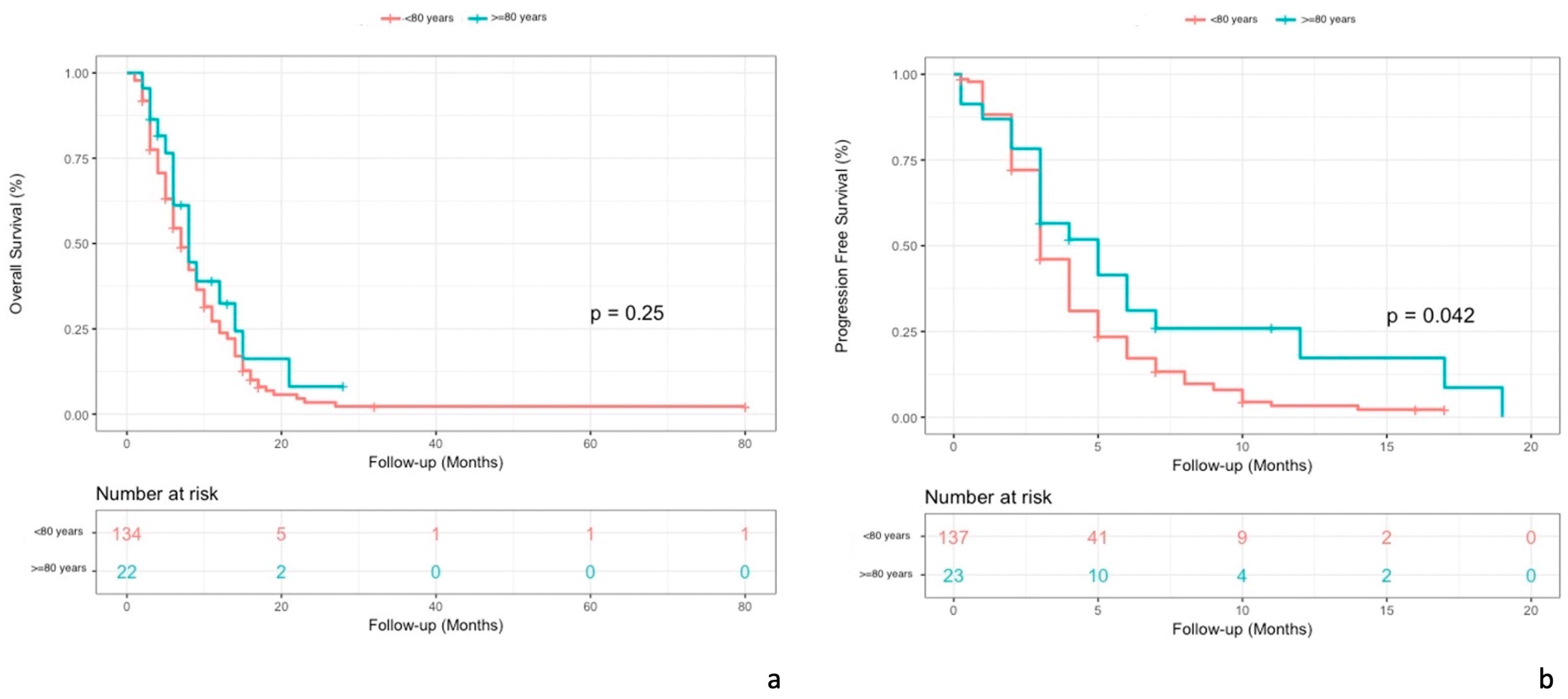
3.4. Elderly Patients
3.5. Special Subgroups
3.5.1. Heart Disease
3.5.2. HIV+
3.5.3. DPYD Gene Polymorphism
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cancer Today 2022. Available online: https://gco.iarc.fr/today/online-analysis-pie?v=2020&mode=cancer&mode_population=continents&population=900&populations=900&key=total&sex=0&cancer=39&type=2&statistic=5&prevalence=1&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&nb_items=7&group_cancer=1&include_nmsc=1&include_nmsc_other=1&half_pie=0&donut=0#collapse-group-0-4 (accessed on 1 April 2023).
- Van Cutsem, E.; Cervantes, A.; Adam, R.; Sobrero, A.; Van Krieken, J.H.; Aderka, D.; Aranda Aguilar, E.; Bardelli, A.; Benson, A.; Bodoky, G.; et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann. Oncol. 2016, 27, 1386–1422. [Google Scholar] [CrossRef] [PubMed]
- Lenz, H.J.; Stintzing, S.; Loupakis, F. TAS-102, a novel antitumor agent: A review of the mechanism of action. Cancer Treat. Rev. 2015, 41, 777–783. [Google Scholar] [CrossRef]
- Mayer, R.J.; Van Cutsem, E.; Falcone, A.; Yoshino, T.; Garcia-Carbonero, R.; Mizunuma, N.; Yamazaki, K.; Shimada, Y.; Tabernero, J.; Komatsu, Y.; et al. Randomized Trial of TAS-102 for Refractory Metastatic Colorectal Cancer. New Engl. J. Med. 2015, 372, 1909–1919. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, F.; Barni, S.; Bertocchi, P.; Zaniboni, A. TAS-102, the first “cardio-gentle” fluoropyrimidine in the colorectal cancer landscape? BMC Cancer 2016, 16, 386. [Google Scholar] [CrossRef] [PubMed]
- Bachet, J.B.; Wyrwicz, L.; Price, T.; Cremolini, C.; Phelip, J.M.; Portales, F.; Ozet, A.; Cicin, I.; Atlan, D.; Becquart, M.; et al. Safety, efficacy and patient-reported outcomes with trifluridine/tipiracil in pretreated metastatic colorectal cancer: Results of the PRECONNECT study. ESMO Open 2020, 5, e000698. [Google Scholar] [CrossRef]
- Carriles, C.; Jimenez-Fonseca, P.; Sánchez-Cánovas, M.; Pimentel, P.; Carmona-Bayonas, A.; García, T.; Carbajales-Álvarez, M.; Lozano-Blázquez, A. Trifluridine/Tipiracil (TAS-102) for refractory metastatic colorectal cancer in clinical practice: A feasible alternative for patients with good performance status. Clin. Transl. Oncol. 2019, 21, 1781–1785. [Google Scholar] [CrossRef]
- Kwakman, J.J.M.; Vink, G.; Vestjens, J.H.; Beerepoot, L.V.; de Groot, J.W.; Jansen, R.L.; Opdam, F.L.; Boot, H.; Creemers, G.J.; van Rooijen, J.M.; et al. Feasibility and effectiveness of trifluridine/tipiracil in metastatic colorectal cancer: Real-life data from The Netherlands. Int. J. Clin. Oncol. 2018, 23, 482–489. [Google Scholar] [CrossRef]
- Stavraka, C.; Pouptsis, A.; Synowiec, A.; Angelis, V.; Satterthwaite, L.; Khan, S.; Chauhan, M.; Holden, C.; Young, S.; Karampera, C.; et al. Trifluridine/Tipiracil in Metastatic Colorectal Cancer: A UK Multicenter Real-world Analysis on Efficacy, Safety, Predictive and Prognostic Factors. Clin. Colorectal. Cancer 2021, 20, 342–349. [Google Scholar] [CrossRef]
- Van Cutsem, E.; Mayer, R.J.; Laurent, S.; Winkler, R.; Grávalos, C.; Benavides, M.; Longo-Munoz, F.; Portales, F.; Ciardiello, F.; Siena, S.; et al. The subgroups of the phase III RECOURSE trial of trifluridine/tipiracil (TAS-102) versus placebo with best supportive care in patients with metastatic colorectal cancer. Eur. J. Cancer 2018, 90, 63–72. [Google Scholar] [CrossRef]
- Cicero, G.; Addeo, R.; De Luca, R.; Lo Re, G.; Gulotta, L.; Marchesa, P.; Gulotta, G. TAS-102 in metastatic colorectal cancer (mCRC): Efficacy, tolerability, and quality of life in heavily pretreated elderly patients: A real-life study. Drugs Context 2020, 9, 2020-6-3. [Google Scholar] [CrossRef]
- Bolzacchini, E.; Luchena, G.; Giordano, M. Safety Report of TAS-102 in a Patient with Reduced DPD Activity. Clin. Colorectal. Cancer 2019, 18, 310–312. [Google Scholar] [CrossRef] [PubMed]
- Schouten, J.F.; Willems, J.; Sanders, S.J.W.J.; Creemers, G.J.; Deenen, M.J. Standard-Dose Trifluridine/Tipiracil as Safe Treatment Alternative in Metastatic Colorectal Cancer Patients with DPD Deficiency. Clin. Colorectal. Cancer 2021, 20, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Sforza, V.; Martinelli, E.; Cardone, C.; Martini, G.; Napolitano, S.; Vitiello, P.P.; Vitale, P.; Zanaletti, N.; Reginelli, A.; Bisceglie, M.D.; et al. Clinical outcome of patients with chemorefractory metastatic colorectal cancer treated with trifluridine/tipiracil (TAS-102): A single Italian institution compassionate use programme. ESMO Open 2017, 2, e000229. [Google Scholar] [CrossRef] [PubMed]
- Longo-Muñoz, F.; Argiles, G.; Tabernero, J.; Cervantes, A.; Gravalos, C.; Pericay, C.; Gil-Calle, S.; Mizuguchi, H.; Carrato-Mena, A.; Limón, M.L.; et al. Efficacy of trifluridine and tipiracil (TAS-102) versus placebo, with supportive care, in a randomized, controlled trial of patients with metastatic colorectal cancer from Spain: Results of a subgroup analysis of the phase 3 RECOURSE trial. Clin. Transl. Oncol. 2017, 19, 227–235. [Google Scholar] [CrossRef] [PubMed]
- U.S Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE) Common Terminology Criteria for Adverse Events (CTCAE) v5.0 [Internet]. 2017. Available online: https://www.meddra.org/ (accessed on 1 January 2023).
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Wallander, M.; Rolander, B.; Åvall-Lundqvist, E.; Elander, N.O. Real world aspects of palliative trifluridine plus tiperacil (TAS-102) in refractory metastatic colorectal cancer. J. Gastrointest. Oncol. 2020, 11, 616–625. [Google Scholar] [CrossRef]
- Cremolini, C.; Rossini, D.; Martinelli, E.; Pietrantonio, F.; Lonardi, S.; Noventa, S.; Tamburini, E.; Frassineti, G.L.; Mosconi, S.; Nichetti, F.; et al. Trifluridine/Tipiracil (TAS-102) in Refractory Metastatic Colorectal Cancer: A Multicenter Register in the Frame of the Italian Compassionate Use Program. Oncologist 2018, 23, 1178–1187. [Google Scholar] [CrossRef]
- Pietrantonio, F.; Miceli, R.; Rimassa, L.; Lonardi, S.; Aprile, G.; Mennitto, A.; Marmorino, F.; Bozzarelli, S.; Antonuzzo, L.; Tamburini, E.; et al. Estimating 12-week death probability in patients with refractory metastatic colorectal cancer: The Colon Life nomogram. Ann. Oncol. 2017, 28, 555–561. [Google Scholar] [CrossRef]
- Köhne, C.H.; Cunningham, D.; Di Costanzo, F.; Glimelius, B.; Blijham, G.; Aranda, E.; Scheithauer, W.; Rougier, P.; Palmer, M.; Wils, J.; et al. Clinical determinants of survival in patients with 5-fluorouracil-based treatment for metastatic colorectal cancer: Results of a multivariate analysis of 3825 patients. Ann. Oncol. 2002, 13, 308–317. [Google Scholar] [CrossRef]
- Xu, J.; Kim, T.W.; Shen, L.; Sriuranpong, V.; Pan, H.; Xu, R.; Guo, W.; Han, S.W.; Liu, T.; Park, Y.S.; et al. Results of a Randomized, Double-Blind, Placebo-Controlled, Phase III Trial of Trifluridine/Tipiracil (TAS-102) Monotherapy in Asian Patients with Previously Treated Metastatic Colorectal Cancer: The TERRA Study. J. Clin. Oncol. 2018, 36, 350–358. [Google Scholar] [CrossRef]
- Zaniboni, A.; Barone, C.A.; Banzi, M.C.; Bergamo, F.; Blasi, L.; Bordonaro, R.; Bartolomeo, M.D.; Costanzo, F.D.; Frassineti, G.L.; Garufi, C.; et al. Italian results of the PRECONNECT study: Safety and efficacy of trifluridine/tipiracil in metastatic colorectal cancer. Future Oncol. 2021, 17, 2315–2324. [Google Scholar] [CrossRef]
- Yoshino, T.; Uetake, H.; Funato, Y.; Yamaguchi, Y.; Koyama, T.; Ozawa, D.; Tajiri, M.; Muro, K. Post-marketing surveillance study of trifluridine/tipiracil in patients with metastatic colorectal cancer. Jpn. J. Clin. Oncol. 2021, 51, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Bendell, J.C.; Patel, M.R.; Yoshida, K.; Seraj, J.; Weaver, R.; Lemech, C.; Todaro, T.G.; Pant, S.; Arkenau, H.T. Phase 1 study of cardiac safety of TAS-102 in patients with advanced solid tumors. Cancer Chemother. Pharmacol. 2016, 77, 1275–1283. [Google Scholar] [CrossRef]
- Polk, A.; Vaage-Nilsen, M.; Vistisen, K.; Nielsen, D.L. Cardiotoxicity in cancer patients treated with 5-fluorouracil or capecitabine: A systematic review of incidence, manifestations and predisposing factors. Cancer Treat. Rev. 2013, 39, 974–984. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.C.; Calis, K.A.; Burke, L.B.; Walawander, C.A.; Grasela, T.H. Symptomatic cardiotoxicity associated with 5-fluorouracil. Pharmacotherapy 1997, 17, 729–736. [Google Scholar] [PubMed]
| Value | Patients (n.) | Patients (%) | |
|---|---|---|---|
| Age | |||
| Median | 68 years | ||
| Range | 38–89 years | ||
| <70 years | 89 | 56% | |
| ≥70 years | 71 | 44% | |
| <75 years | 110 | 69% | |
| ≥75 years | 50 | 31% | |
| <80 years | 137 | 86% | |
| ≥80 years | 23 | 14% | |
| Gender | |||
| Male | 103 | 64% | |
| Female | 57 | 36% | |
| ECOG PS | |||
| 0 | 47 | 29% | |
| 1 | 100 | 63% | |
| 2+ | 13 | 8% | |
| Sidedness | |||
| Right colon | 45 | 28% | |
| Left colon | 71 | 44% | |
| Rectum | 44 | 28% | |
| RAS | |||
| Mutated | 90 | 56% | |
| Wild Type | 63 | 40% | |
| ND | 7 | 4% | |
| BRAF | |||
| Mutated | 5 | 3% | |
| Wild Type | 134 | 84% | |
| ND | 21 | 13% | |
| MSS/MSI | |||
| MSS | 102 | 64% | |
| MSI | 4 | 3% | |
| ND | 54 | 33% | |
| Time between diagnosis and metastases | |||
| >18 months | 113 | 71% | |
| <=18 months | 38 | 24% | |
| ND | 9 | 6% | |
| Metastatic sites n. | |||
| 1 | 44 | 27% | |
| 2 or more | 116 | 73% | |
| Previous treatment lines | |||
| 0 | 2 | 1% | |
| 1 | 11 | 7% | |
| 2 | 115 | 72% | |
| 3 | 25 | 16% | |
| 4 or more | 7 | 4% | |
| Previous therapies | |||
| Fluoropirimidines | 158 | 99% | |
| Oxaliplatin | 146 | 91% | |
| Irinotecan | 147 | 92% | |
| Bevacizumab | 122 | 76% | |
| Aflibercept | 30 | 19% | |
| Anti-EGFR | 53 | 33% | |
| Regorafenib | 10 | 6% | |
| Cardiac disease | |||
| Yes | 19 | 12% | |
| No | 134 | 84% | |
| ND | 7 | 4% | |
| DPYD | |||
| Mutated | 1 | <1% | |
| Wild Type | 21 | 13% | |
| ND | 138 | 86% | |
| HIV | |||
| HIV+ | 3 | 2% | |
| HIV- | 108 | 68% | |
| ND | 49 | 31% | |
| Staging at diagnosis | |||
| Stage IV | 85 | 53% | |
| Stages I–II–III | 75 | 47% | |
| TOTAL | 160 |
| HR | 95% CI | p-Value | ||
|---|---|---|---|---|
| Gender | Female | 1.00 | reference | |
| Male | 1.02 | 0.71–1.45 | 0.92 | |
| Age | 0.99 | 0.98–.02 | 0.93 | |
| <70 | 1.00 | reference | ||
| >=70 | 1.02 | 0.73–1.44 | 0.91 | |
| <75 | 1.00 | reference | ||
| >=75 | 0.91 | 0.63–1.32 | 0.62 | |
| <80 | 1.00 | reference | ||
| >=80 | 0.75 | 0.45–1.27 | 0.28 | |
| Sidedness | Rectum | 1.00 | reference | |
| Right colon | 0.98 | 0.62–1.53 | 0.91 | |
| Left colon | 0.82 | 0.54–1.24 | 0.35 | |
| PS ECOG | 0 | 1.00 | reference | |
| 1 | 1.73 | 1.17–2.55 | 0.01 | |
| >=2 | 2.12 | 1.10–4.09 | 0.02 | |
| RASstatus | Wild type | 1.00 | reference | |
| Mutated | 0.97 | 0.69–1.37 | 0.86 | |
| BRAFstatus | Wild type | 1.00 | reference | |
| Mutated | 1.39 | 0.51–3.78 | 0.52 | |
| MSS/MSI | MSS | 1.00 | reference | |
| MSI | 0.66 | 0.21–2.12 | 0.49 | |
| Staging at diagnosis | I-II-III | 1.00 | reference | |
| IV | 1.26 | 0.89–1.78 | 0.19 | |
| Previous treatment lines | <=2 | 1.00 | reference | |
| >2 | 0.92 | 0.59–1.43 | 0.71 | |
| Regorafenib | No | 1.00 | reference | |
| Sì | 0.84 | 0.44–1.61 | 0.60 | |
| Metastatic sites n. | 1 | 1.00 | reference | |
| >1 | 1.38 | 0.93–2.04 | 0.11 | |
| Time between metastases and TAS-102 treatment | <=18 months | 1.00 | reference | |
| >18 months | 0.93 | 0.63–1.38 | 0.73 | |
| Liver metastases | No | 1.00 | reference | |
| Yes | 1.37 | 0.92–2.05 | 0.13 | |
| Lung metastases | No | 1.00 | reference | |
| Yes | 0.86 | 0.61–1.20 | 0.37 | |
| Peritoneal metastases | No | 1.00 | reference | |
| Yes | 1.25 | 0.84–1.87 | 0.27 |
| Adverse EvenT (AE) | Any Grade | G1–G2 | G3–G4 | N. Grade NA |
|---|---|---|---|---|
| Leukopenia | 46 (29%) | 15 (9%) | 4 (3%) | 27 (17%) |
| Neutropenia | 78 (49%) | 14 (9%) | 30 (19%) | 34 (21%) |
| Anemia | 36 (23%) | 16 (10%) | 7 (4%) | 13 (8%) |
| Thrombocytopenia | 5 (3%) | 4 (3%) | 0 | 1 (<1%) |
| Febrile neutropenia | 5 (3%) | 0 | 5 (3%) | 0 |
| Asthenia | 67 (42%) | 21 (13%) | 3 (2%) | 43 (27%) |
| Nausea | 19 (12%) | 4 (3%) | 0 | 15 (9%) |
| Vomiting | 10 (6%) | 2 (1%) | 0 | 8 (5%) |
| Diarrhea | 23 (14%) | 11 (7%) | 1 (<1%) | 11 (7%) |
| Hepatotoxicity | 6 (4%) | 0 | 1 (<1%) | 5 (3%) |
| Nephrotoxicity (>crea) | 1 (<1%) | 0 | 0 | 1 (<1%) |
| Skin rash | 2 (1%) | 0 | 0 | 2 (1%) |
| Itching | 1 (<1%) | 0 | 0 | 1 (<1%) |
| Mucositis | 3 (2%) | 0 | 0 | 3 (2%) |
| Declivuos edema | 2 (1%) | 0 | 0 | 2 (1%) |
| Gastrointestinal bleeding | 2 (1%) | 0 | 0 | 2 (1%) |
| Alopecia | 1 (<1%) | 1 (<1%) | 0 | 0 |
| Anorexia | 1 (<1%) | 0 | 0 | 1 (<1%) |
| Dysgeusia | 1 (<1%) | 0 | 0 | 1 (<1%) |
| Pneumonia | 1 (<1%) | 0 | 0 | 1 (<1%) |
| Hypoglycemia | 1 (<1%) | 0 | 0 | 1 (<1%) |
| Constipation | 2 (1%) | 0 | 0 | 2 (1%) |
| Paresthesias | 1 (<1%) | 0 | 0 | 1 (<1%) |
| Headhache | 1 (<1%) | 0 | 0 | 1 (<1%) |
| Hypotension | 1 (<1%) | 0 | 0 | 1 (<1%) |
| No AE | 19 |
| Neutropenia | G3–G4 Neutropenia * | Leukopenia | Anemia | Thrombocytopenia | Febrile Neutropenia | Asthenia | Diarrhea | Nausea | Vomiting | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No/G1–G2 | G3–G4 | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | |
| <70 years | 48 (53.9) | 41 (46.1) | 55 (77.5) | 16 (22.5) | 60 (67.4) | 29 (32.3) | 67 (75.3) | 22 (24.7) | 84 (94.4) | 5 (5.6) | 88 (98.9) | 1 (1.1) | 49 (55.1) | 40 (44.9) | 75 (84.3) | 14 (15.7) | 75 (84.3) | 14 (15.7) | 81 (91.0) | 8 (9.0) |
| >=70 years | 34 (47.9) | 37 (52.1) | 41 (74.6) | 14 (25.4) | 54 (76.1) | 17 (23.9) | 57 (80.3) | 14 (19.7) | 71 (100.0) | 0 (0.0) | 67 (94.4) | 4 (5.6) | 44 (62.0) | 27 (38.0) | 62 (87.3) | 9 (12.7) | 66 (93.0) | 5 (7.0) | 69 (97.2) | 2 (2.8) |
| p-value | 0.45 | 0.70 | 0.23 | 0.45 | 0.07 | 0.17 | 0.38 | 0.58 | 0.09 | 0.19 | ||||||||||
| <75 years | 63 (57.3) | 47 (42.7) | 72 (80.0) | 18 (20.0) | 78 (70.9) | 32 (29.1) | 84 (76.4) | 26 (23.6) | 105 (95.5) | 5 (4.6) | 109 (99.1) | 1 (0.9) | 58 (52.7) | 52 (47.3) | 95 (86.4) | 15 (13.6) | 95 (86.4) | 15 (13.6) | 102 (92.7) | 8 (7.3) |
| >=75 years | 19 (38.0) | 31 (62.0) | 24 (66.7) | 12 (33.3) | 36 (72.0) | 14 (28.0) | 40 (80.0) | 10 (20.0) | 50 (100.0) | 0 (0.0) | 46 (92.0) | 4 (8.0) | 35 (70.0) | 15 (30.0) | 42 (84.0) | 8 (16.0) | 46 (92.0) | 4 (8.0) | 48 (96.0) | 2 (4.0) |
| p-value | 0.02 | 0.11 | 0.89 | 0.61 | 0.33 | 0.04 | 0.04 | 0.69 | 0.31 | 0.73 | ||||||||||
| <80 years | 73 (53.3) | 64 (46.7) | 86 (79.6) | 22 (20.4) | 99 (72.3) | 38 (27.7) | 106 (77.4) | 31 (22.6) | 132 (96.4) | 5 (3.7) | 134 (97.8) | 3 (2.2) | 75 (54.7) | 62 (45.3) | 118 (86.2) | 19 (13.9) | 121 (88.3) | 16 (11.7) | 129 (94.2) | 8 (5.8) |
| >=80 years | 9 (39.1) | 14 (60.9) | 10 (55.6) | 8 (44.4) | 15 (65.2) | 8 (34.8) | 18 (78.3) | 5 (21.7) | 23 (100.0) | 0 (0.0) | 21 (91.3) | 2 (8.7) | 18 (78.3) | 5 (21.7) | 19 (82.6) | 4 (17.4) | 20 (87.0) | 3 (13.0) | 21 (91.3) | 2 (8.7) |
| p-value | 0.21 | 0.03 | 0.49 | 0.92 | 0.99 | 0.15 | 0.03 | 0.75 | 0.74 | 0.64 | ||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conti, M.; Bolzacchini, E.; Luchena, G.; Bertu’, L.; Tagliabue, P.; Aglione, S.; Ardizzoia, A.; Arnoffi, J.; Guida, F.M.; Bertolini, A.; et al. Tas-102 for Refractory Metastatic Colorectal Cancer: A Multicenter Retrospective Cohort Study. Cancers 2023, 15, 3465. https://doi.org/10.3390/cancers15133465
Conti M, Bolzacchini E, Luchena G, Bertu’ L, Tagliabue P, Aglione S, Ardizzoia A, Arnoffi J, Guida FM, Bertolini A, et al. Tas-102 for Refractory Metastatic Colorectal Cancer: A Multicenter Retrospective Cohort Study. Cancers. 2023; 15(13):3465. https://doi.org/10.3390/cancers15133465
Chicago/Turabian StyleConti, Matteo, Elena Bolzacchini, Giovanna Luchena, Lorenza Bertu’, Paola Tagliabue, Stefania Aglione, Antonio Ardizzoia, Jessica Arnoffi, Francesco Maria Guida, Alessandro Bertolini, and et al. 2023. "Tas-102 for Refractory Metastatic Colorectal Cancer: A Multicenter Retrospective Cohort Study" Cancers 15, no. 13: 3465. https://doi.org/10.3390/cancers15133465
APA StyleConti, M., Bolzacchini, E., Luchena, G., Bertu’, L., Tagliabue, P., Aglione, S., Ardizzoia, A., Arnoffi, J., Guida, F. M., Bertolini, A., Pastorini, A., Duro, M., Bettega, D., Roda’, G., Artale, S., Squizzato, A., & Giordano, M. (2023). Tas-102 for Refractory Metastatic Colorectal Cancer: A Multicenter Retrospective Cohort Study. Cancers, 15(13), 3465. https://doi.org/10.3390/cancers15133465







