The Impact of Metastasectomy on Survival Outcomes of Renal Cell Carcinoma: A 10-Year Single Center Experience
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Data Collection and Follow-Up
2.3. Statistical Methods
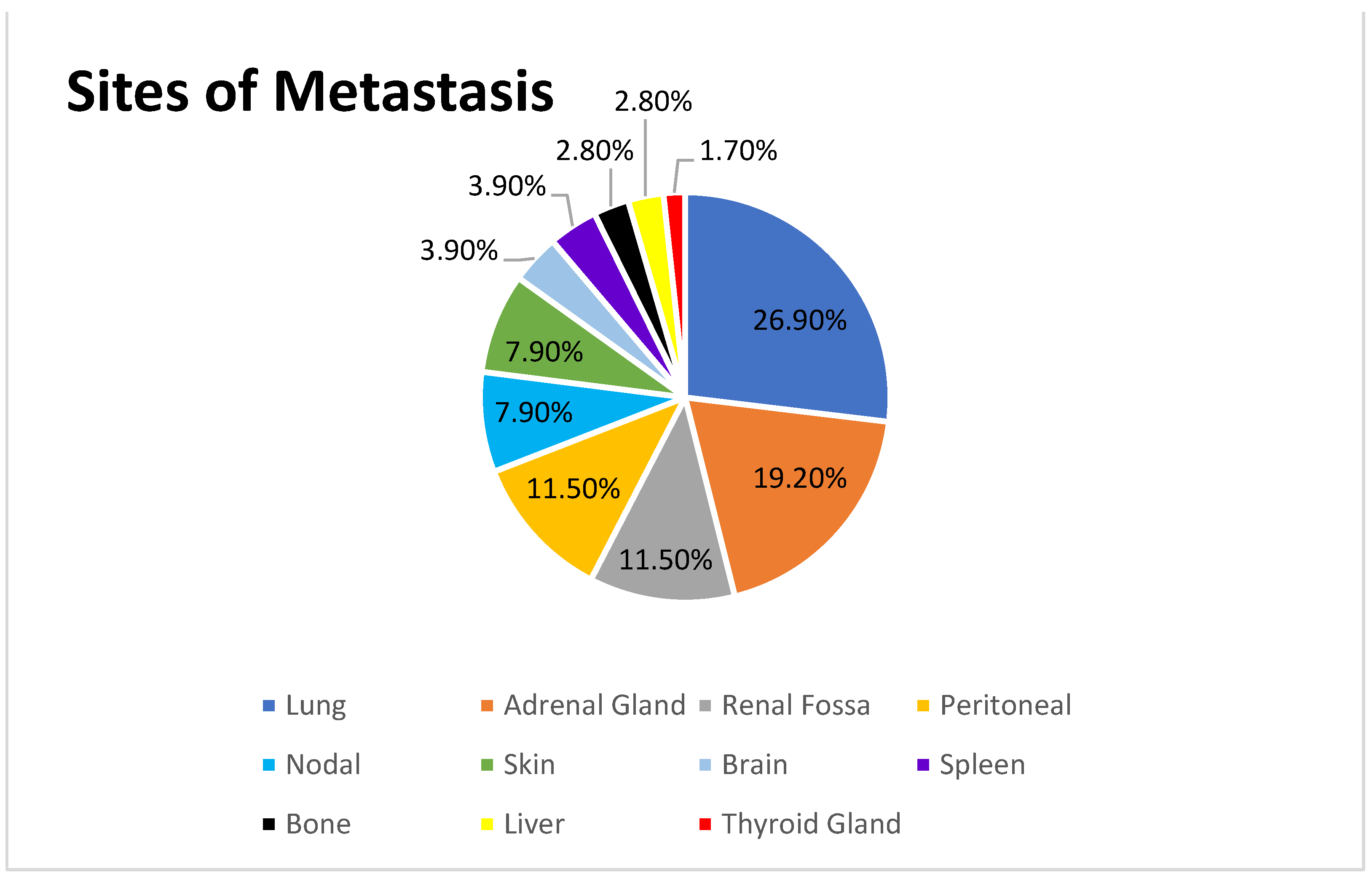
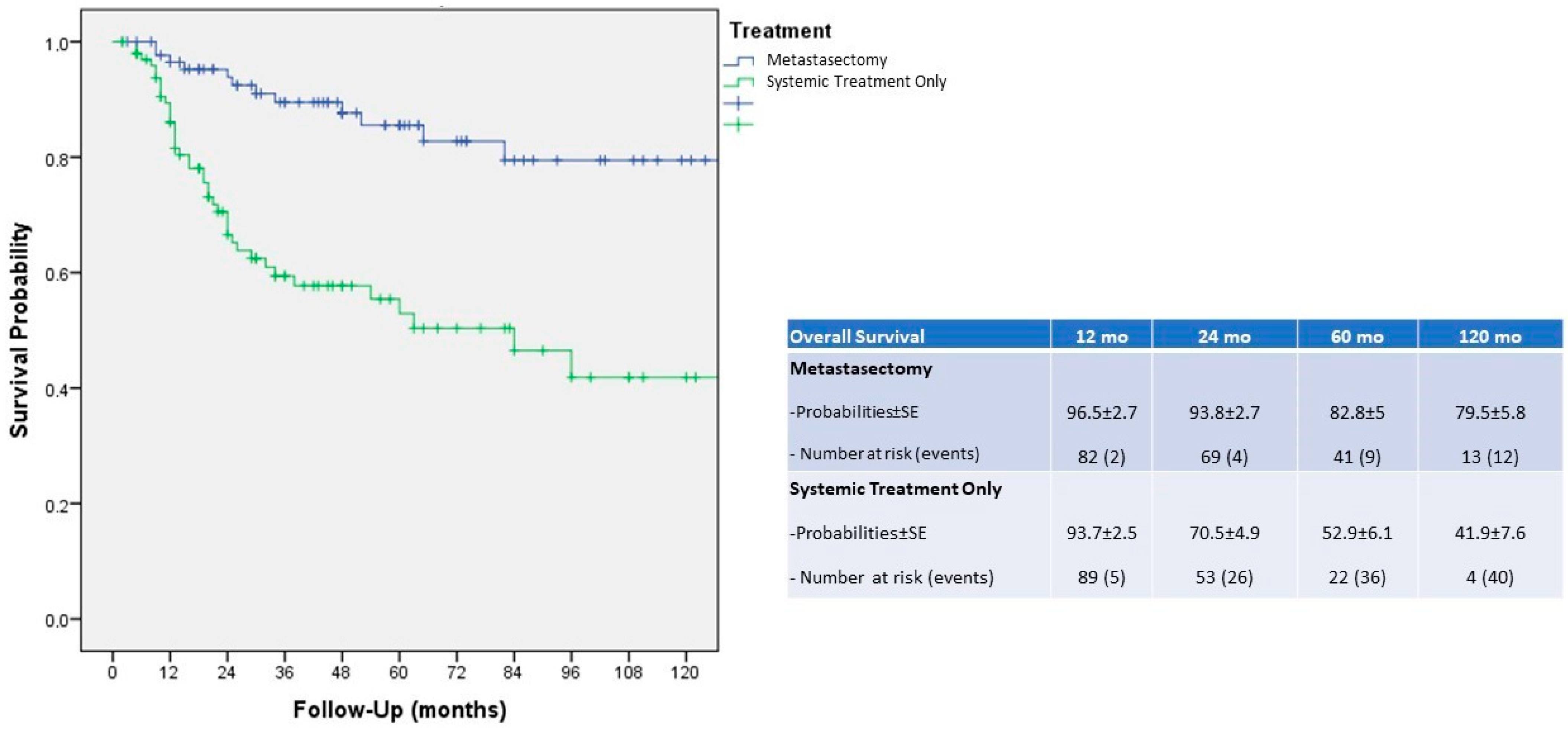
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ljungberg, B.; Albiges, L.; Abu-Ghanem, Y.; Bedke, J.; Capitanio, U.; Dabestani, S.; Fernández-Pello, S.; Giles, R.H.; Hofmann, F.; Hora, M.; et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2022 Update. Eur. Urol. 2022, 82, 399–410. [Google Scholar] [CrossRef] [PubMed]
- Dabestani, S.; Thorstenson, A.; Lindblad, P.; Harmenberg, U.; Ljungberg, B.; Lundstam, S. Renal Cell Carcinoma Recurrences and Metastases in Primary Non-Metastatic Patients: A Population-Based Study. World J. Urol. 2016, 34, 1081–1086. [Google Scholar] [CrossRef] [PubMed]
- Breda, A.; Konijeti, R.; Lam, J.S. Patterns of Recurrence and Surveillance Strategies for Renal Cell Carcinoma Following Surgical Resection. Expert Rev. Anticancer Ther. 2007, 7, 847–862. [Google Scholar] [CrossRef]
- Ferriero, M.; Prata, F.; Mastroianni, R.; De Nunzio, C.; Tema, G.; Tuderti, G.; Bove, A.M.; Anceschi, U.; Brassetti, A.; Misuraca, L.; et al. The Impact of Locoregional Treatments for Metastatic Castration Resistant Prostate Cancer on Disease Progression: Real Life Experience from a Multicenter Cohort. Prostate Cancer Prostatic Dis. 2022. [Google Scholar] [CrossRef]
- Kulaylat, M.N.; Gibbs, J.F. Thermoablation of Colorectal Liver Metastasis. J. Surg. Oncol. 2010, 101, 699–705. [Google Scholar] [CrossRef]
- Bailleux, C.; Eberst, L.; Bachelot, T. Treatment Strategies for Breast Cancer Brain Metastases. Br. J. Cancer 2021, 124, 142–155. [Google Scholar] [CrossRef]
- Kotecha, R.; Ahluwalia, M.S.; Siomin, V.; McDermott, M.W. Surgery, Stereotactic Radiosurgery, and Systemic Therapy in the Management of Operable Brain Metastasis. Neurol. Clin. 2022, 40, 421–436. [Google Scholar] [CrossRef]
- Bang, H.J.; Littrup, P.J.; Goodrich, D.J.; Currier, B.P.; Aoun, H.D.; Heilbrun, L.K.; Vaishampayan, U.; Adam, B.; Goodman, A.C. Percutaneous Cryoablation of Metastatic Renal Cell Carcinoma for Local Tumor Control: Feasibility, Outcomes, and Estimated Cost-Effectiveness for Palliation. J. Vasc. Interv. Radiol. 2012, 23, 770–777. [Google Scholar] [CrossRef]
- Kothari, G.; Foroudi, F.; Gill, S.; Corcoran, N.M.; Siva, S. Outcomes of Stereotactic Radiotherapy for Cranial and Extracranial Metastatic Renal Cell Carcinoma: A Systematic Review. Acta Oncol. 2015, 54, 148–157. [Google Scholar] [CrossRef]
- Zaid, H.B.; Parker, W.P.; Safdar, N.S.; Gershman, B.; Erwin, P.J.; Murad, M.H.; Boorjian, S.A.; Costello, B.A.; Thompson, R.H.; Leibovich, B.C. Outcomes Following Complete Surgical Metastasectomy for Patients with Metastatic Renal Cell Carcinoma: A Systematic Review and Meta-Analysis. J. Urol. 2017, 197, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Matuszczak, M.; Kiljańczyk, A.; Salagierski, M. Surgical Approach in Metastatic Renal Cell Carcinoma: A Literature Review. Cancers 2023, 15, 1804. [Google Scholar] [CrossRef] [PubMed]
- Méjean, A.; Ravaud, A.; Thezenas, S.; Colas, S.; Beauval, J.-B.; Bensalah, K.; Geoffrois, L.; Thiery-Vuillemin, A.; Cormier, L.; Lang, H.; et al. Sunitinib Alone or after Nephrectomy in Metastatic Renal-Cell Carcinoma. N. Engl. J. Med. 2018, 379, 417–427. [Google Scholar] [CrossRef]
- Kavolius, J.P.; Mastorakos, D.P.; Pavlovich, C.; Russo, P.; Burt, M.E.; Brady, M.S. Resection of Metastatic Renal Cell Carcinoma. J. Clin. Oncol. 1998, 16, 2261–2266. [Google Scholar] [CrossRef] [PubMed]
- Dragomir, A.; Nazha, S.; Wood, L.A.; Rendon, R.A.; Finelli, A.; Hansen, A.; So, A.I.; Kollmannsberger, C.; Basappa, N.S.; Pouliot, F.; et al. Outcomes of Complete Metastasectomy in Metastatic Renal Cell Carcinoma Patients: The Canadian Kidney Cancer Information System Experience. Urol. Oncol. 2020, 38, 799.e1–799.e10. [Google Scholar] [CrossRef]
- Alt, A.L.; Boorjian, S.A.; Lohse, C.M.; Costello, B.A.; Leibovich, B.C.; Blute, M.L. Survival after Complete Surgical Resection of Multiple Metastases from Renal Cell Carcinoma. Cancer 2011, 117, 2873–2882. [Google Scholar] [CrossRef]
- Samsel, R.; Cichocki, A.; Roszkowska-Purska, K.; Papierska, L.; Koalasińska-Ćwikła, A.; Karpeta, E.; Ostrowski, T.; Nowak, K. Adrenal Metastases—Long-Term Results of Surgical Treatment, Single-Centre Experience. Współczesna Onkol. 2020, 24, 29–33. [Google Scholar] [CrossRef]
- Thomas, A.Z.; Adibi, M.; Borregales, L.D.; Hoang, L.N.; Tamboli, P.; Jonasch, E.; Tannir, N.M.; Matin, S.F.; Wood, C.G.; Karam, J.A. Surgical Management of Local Retroperitoneal Recurrence of Renal Cell Carcinoma after Radical Nephrectomy. J. Urol. 2015, 194, 316–322. [Google Scholar] [CrossRef]
- Romeo, A.; Garcia Marchiñena, P.; Jurado, A.M.; Gueglio, G. Renal Fossa Recurrence after Radical Nephrectomy: Current Management, and Oncological Outcomes. Urol. Oncol. Semin. Orig. Investig. 2020, 38, 42.e7–42.e12. [Google Scholar] [CrossRef]
- Meyer, C.P.; Sun, M.; Karam, J.A.; Leow, J.J.; de Velasco, G.; Pal, S.K.; Chang, S.L.; Trinh, Q.-D.; Choueiri, T.K. Complications After Metastasectomy for Renal Cell Carcinoma—A Population-Based Assessment. Eur. Urol. 2017, 72, 171–174. [Google Scholar] [CrossRef]
- Paparel, P.; Bigot, P.; Matillon, X.; Bensalah, K.; Salomon, L.; Baumert, H.; Bastide, C.; Thuret, R.; Karsenty, G.; Long, J.A.; et al. Local Recurrence after Radical Nephrectomy for Kidney Cancer: Management and Prediction of Outcomes. A Multi-Institutional Study: Local Recurrence After Radical Nephrectomy. J. Surg. Oncol. 2014, 109, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Vatansever, S.; Nordenström, E.; Raffaelli, M.; Brunaud, L.; Makay, Ö.; EUROCRINE Council. Robot-Assisted versus Conventional Laparoscopic Adrenalectomy: Results from the EUROCRINE Surgical Registry. Surgery 2022, 171, 1224–1230. [Google Scholar] [CrossRef]
- Lyon, T.D.; Thompson, R.H.; Shah, P.H.; Lohse, C.M.; Boorjian, S.A.; Costello, B.A.; Cheville, J.C.; Leibovich, B.C. Complete Surgical Metastasectomy of Renal Cell Carcinoma in the Post-Cytokine Era. J. Urol. 2020, 203, 275–282. [Google Scholar] [CrossRef]
- Ferriero, M.C.; Brassetti, A.; Mastroianni, R.; Costantini, M.; Tuderti, G.; Anceschi, U.; Bove, A.M.; Misuraca, L.; Guaglianone, S.; Gallucci, M.; et al. Off-clamp robot-assisted partial nephrectomy for purely hilar tumors: Technique, perioperative, oncologic and functional outcomes from a single center series. Eur. J. Surg. Oncol. 2022, 48, 1848–1853. [Google Scholar] [CrossRef]
- Simone, G.; Tuderti, G.; Anceschi, U.; Ferriero, M.; Costantini, M.; Minisola, F.; Vallati, G.; Pizzi, G.; Guaglianone, S.; Misuraca, L.; et al. “Ride the Green Light”: Indocyanine Green-marked Off-clamp Robotic Partial Nephrectomy for Totally Endophytic Renal Masses. Eur. Urol. 2019, 75, 1008–1014. [Google Scholar] [CrossRef] [PubMed]
- Sharp, E.; Guduru, A.; May, A.M.; Lombardo, L.; Siddiqui, S.A.; Hamilton, Z.A. The Distribution of Metastatic Renal Cell Carcinoma by Presenting Tumor Stage in the Modern Era. Clin. Genitourin. Cancer 2022, 20, e296–e302. [Google Scholar] [CrossRef]
- Leibovich, B.C.; Lohse, C.M.; Cheville, J.C.; Zaid, H.B.; Boorjian, S.A.; Frank, I.; Thompson, R.H.; Parker, W.P. Predicting Oncologic Outcomes in Renal Cell Carcinoma after Surgery. Eur. Urol. 2018, 73, 772–780. [Google Scholar] [CrossRef]
- Cindolo, L.; Patard, J.-J.; Chiodini, P.; Schips, L.; Ficarra, V.; Tostain, J.; de La Taille, A.; Altieri, V.; Lobel, B.; Zigeuner, R.E.; et al. Comparison of Predictive Accuracy of Four Prognostic Models for Nonmetastatic Renal Cell Carcinoma after Nephrectomy: A Multicenter European Study. Cancer 2005, 104, 1362–1371. [Google Scholar] [CrossRef]
- Kattan, M.W.; Reuter, V.; Motzer, R.J.; Katz, J.; Russo, P. A Postoperative Prognostic Nomogram for Renal Cell Carcinoma. J. Urol. 2001, 166, 63–67. [Google Scholar] [CrossRef]
- Lam, J.S.; Shvarts, O.; Leppert, J.T.; Pantuck, A.J.; Figlin, R.A.; Belldegrun, A.S. Postoperative Surveillance Protocol for Patients with Localized and Locally Advanced Renal Cell Carcinoma Based on a Validated Prognostic Nomogram and Risk Group Stratification System. J. Urol. 2005, 174, 466–472; discussion 472; quiz 801. [Google Scholar] [CrossRef]
- Parker, W.P.; Cheville, J.C.; Frank, I.; Zaid, H.B.; Lohse, C.M.; Boorjian, S.A.; Leibovich, B.C.; Thompson, R.H. Application of the Stage, Size, Grade, and Necrosis (SSIGN) Score for Clear Cell Renal Cell Carcinoma in Contemporary Patients. Eur. Urol. 2017, 71, 665–673. [Google Scholar] [CrossRef]
- Kim, J.K.; Lee, H.; Oh, J.J.; Lee, S.; Hong, S.K.; Lee, S.E.; Byun, S.-S. Synchronous Bilateral RCC Is Associated with Poor Recurrence-Free Survival Compared with Unilateral RCC: A Single-Center Study with Propensity Score Matching Analysis. Clin. Genitourin. Cancer 2019, 17, e570–e580. [Google Scholar] [CrossRef]
- Tellini, R.; Antonelli, A.; Tardanico, R.; Fisogni, S.; Veccia, A.; Furlan, M.C.; Carobbio, F.; Cozzoli, A.; Zanotelli, T.; Simeone, C. Positive Surgical Margins Predict Progression-Free Survival After Nephron-Sparing Surgery for Renal Cell Carcinoma: Results from a Single Center Cohort of 459 Cases with a Minimum Follow-up of 5 Years. Clin. Genitourin. Cancer 2019, 17, e26–e31. [Google Scholar] [CrossRef]
- Bai, R.; Gao, L.; Wang, J.; Jiang, Q. Positive Surgical Margins May Not Affect the Survival of Patients with Renal Cell Carcinoma after Partial Nephrectomy: A Meta-Analysis Based on 39 Studies. Front. Oncol. 2022, 12, 945166. [Google Scholar] [CrossRef]
- Abdel-Rahman, O. Clinical correlates and prognostic value of different metastatic sites in metastatic renal cell carcinoma. Future Oncol. 2017, 13, 1967–1980. [Google Scholar] [CrossRef]
- Motzer, R.J.; Tannir, N.M.; McDermott, D.F.; Arén Frontera, O.; Melichar, B.; Choueiri, T.K.; Plimack, E.R.; Barthélémy, P.; Porta, C.; George, S.; et al. Nivolumab plus Ipilimumab versus Sunitinib in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2018, 378, 1277–1290. [Google Scholar] [CrossRef]
- Marchioni, M.; Amparore, D.; Pecoraro, A.; Bertolo, R.; Campi, R.; EAU Young Academic Urologists (YAU) Renal Cancer Working Group. Morbidity and mortality of metastasectomy for renal cell carcinoma: Is centralization of care the way forward? Minerva Urol. Nephrol. 2023, 75, 413–416. [Google Scholar] [CrossRef]
| Clinical Features | Median or N (IQR or %) |
|---|---|
| Age (years) | 61 (47–70) |
| Gender | |
| F | 48 (30.2) |
| M | 111 (69.8) |
| ECOG | |
| 0 | 148 (93.1) |
| 1 | 11 (6.9) |
| Bilateral disease | 5 (3.1) |
| Primary Treatment | |
| Radical Nephrectomy | 108 (67.9) |
| Partial Nephrectomy | 51 (32.1) |
| pT | |
| x | 4 (2.5) |
| 1a | 25 (15.7) |
| 1b | 46 (28.9) |
| 2a | 18 (11.3) |
| 2b | 10 (6.3) |
| 3a | 34 (21.4) |
| 3b | 18 (11.3) |
| 3c | 2 (1.3) |
| 4 | 2 (1.3) |
| pN | |
| 0 | 144 (90.5) |
| 1 | 6 (3.8) |
| 2 | 8 (5.1) |
| 3 | 1 (0.6) |
| AJCC stage | |
| I | 69 (43.4) |
| II | 27 (16.9) |
| III | 61 (38.3) |
| IV | 2 (1.3) |
| Histology | |
| ccRCC | 134 (84.3) |
| Other than ccRCC | 25 (15.7) |
| Positive Surgical Margins Rate | 2 (1.3) |
| Follow-up time (months) | 16 (9–42) |
| Treatment | |
| MST | 77 (48.4) |
| ST | 82 (51.2) |
| COX Regression Analysis for Overall Survival | ||||||||
|---|---|---|---|---|---|---|---|---|
| Univariable | Multivariable | |||||||
| Variable | p | OR | 95% CIs | p | OR | 95% CIs | ||
| Low | High | Low | High | |||||
| Age | 0.838 | 1.00 | 0.96 | 1.05 | - | - | - | - |
| Gender | 0.647 | 1.07 | 0.79 | 1.45 | - | - | - | - |
| Bilaterality | 0.471 | 2.07 | 0.28 | 14.23 | - | - | - | - |
| ccRCC histology | 0.052 | 1.87 | 0.99 | 3.49 | - | - | - | - |
| AJCC stage (I ref.) | 0.003 | 0.035 | ||||||
| II vs. I | 0.138 | 1.95 | 0.81 | 4.71 | 0.146 | 1.93 | 0.79 | 4.68 |
| III vs. II | 0.001 | 3.47 | 1.71 | 7.03 | 0.036 | 2.31 | 1.06 | 5.07 |
| IV vs. I | 0.016 | 6.52 | 1.42 | 30.01 | 0.018 | 13.22 | 1.56 | 111.77 |
| Positive Surgical Margins | 0.953 | 1.02 | 0.51 | 2.06 | - | - | - | - |
| Metastasectomy | <0.001 | 3.89 | 2.07 | 7.32 | 0.019 | 2.77 | 1.18 | 6.47 |
| Local Metastasis (renal fossa, peritoneal, skin) | 0.031 | 4.80 | 1.16 | 19.91 | 0.257 | 2.50 | 0.51 | 12.23 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferriero, M.; Cacciatore, L.; Ochoa, M.; Mastroianni, R.; Tuderti, G.; Costantini, M.; Anceschi, U.; Misuraca, L.; Brassetti, A.; Guaglianone, S.; et al. The Impact of Metastasectomy on Survival Outcomes of Renal Cell Carcinoma: A 10-Year Single Center Experience. Cancers 2023, 15, 3332. https://doi.org/10.3390/cancers15133332
Ferriero M, Cacciatore L, Ochoa M, Mastroianni R, Tuderti G, Costantini M, Anceschi U, Misuraca L, Brassetti A, Guaglianone S, et al. The Impact of Metastasectomy on Survival Outcomes of Renal Cell Carcinoma: A 10-Year Single Center Experience. Cancers. 2023; 15(13):3332. https://doi.org/10.3390/cancers15133332
Chicago/Turabian StyleFerriero, Mariaconsiglia, Loris Cacciatore, Mario Ochoa, Riccardo Mastroianni, Gabriele Tuderti, Manuela Costantini, Umberto Anceschi, Leonardo Misuraca, Aldo Brassetti, Salvatore Guaglianone, and et al. 2023. "The Impact of Metastasectomy on Survival Outcomes of Renal Cell Carcinoma: A 10-Year Single Center Experience" Cancers 15, no. 13: 3332. https://doi.org/10.3390/cancers15133332
APA StyleFerriero, M., Cacciatore, L., Ochoa, M., Mastroianni, R., Tuderti, G., Costantini, M., Anceschi, U., Misuraca, L., Brassetti, A., Guaglianone, S., Bove, A. M., Papalia, R., Gallucci, M., & Simone, G. (2023). The Impact of Metastasectomy on Survival Outcomes of Renal Cell Carcinoma: A 10-Year Single Center Experience. Cancers, 15(13), 3332. https://doi.org/10.3390/cancers15133332







