Association of Smoking and Respiratory Disease History with Pancreatic Pathologies Requiring Surgical Resection
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Cohort Selection
2.3. Statistical Analysis
2.4. Ethical Approval
3. Results
3.1. Cohort Description
3.2. Distribution of Respiratory Diseases
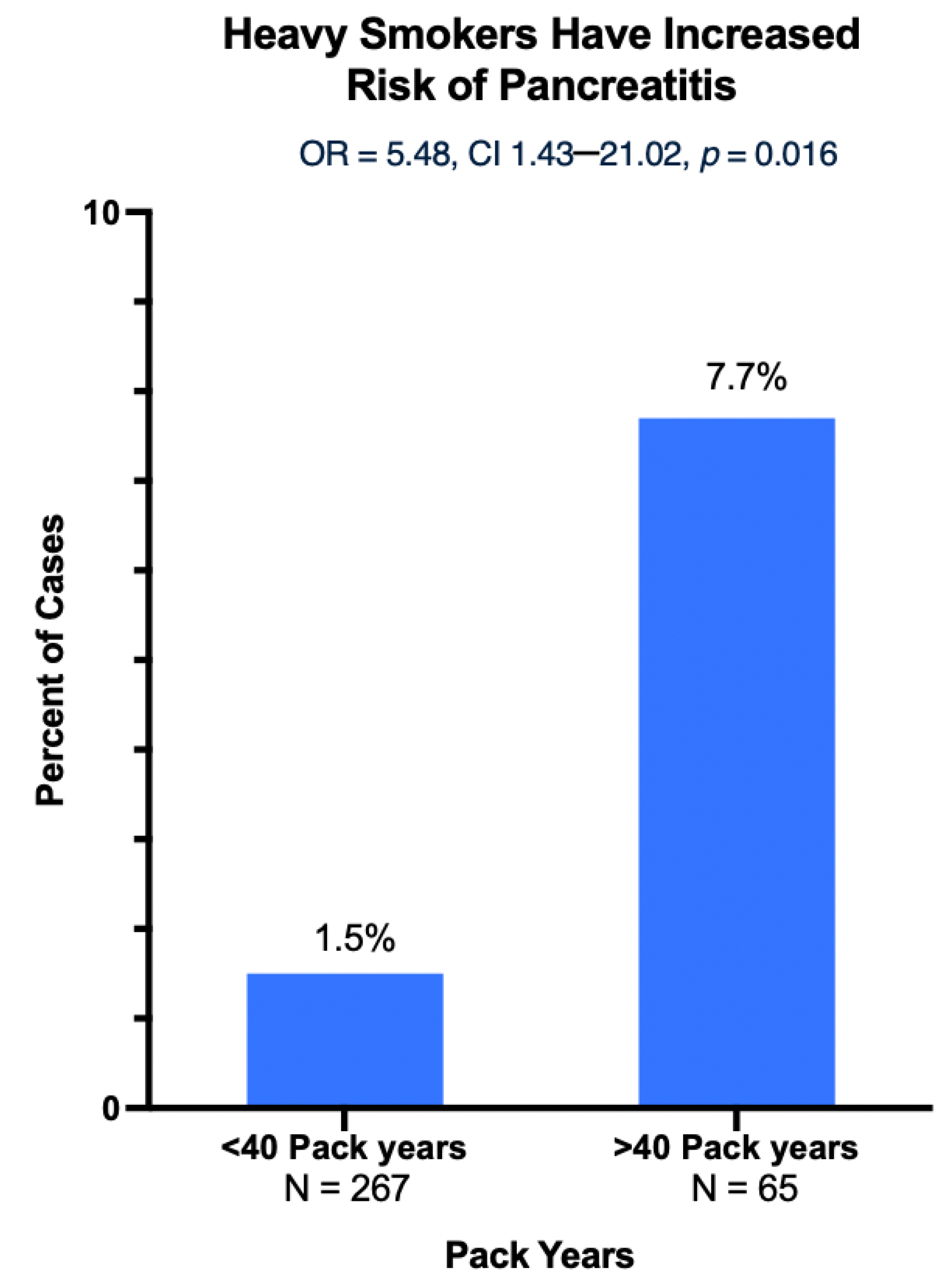
3.3. Smoking Is Linked with Pancreatic Pathologies
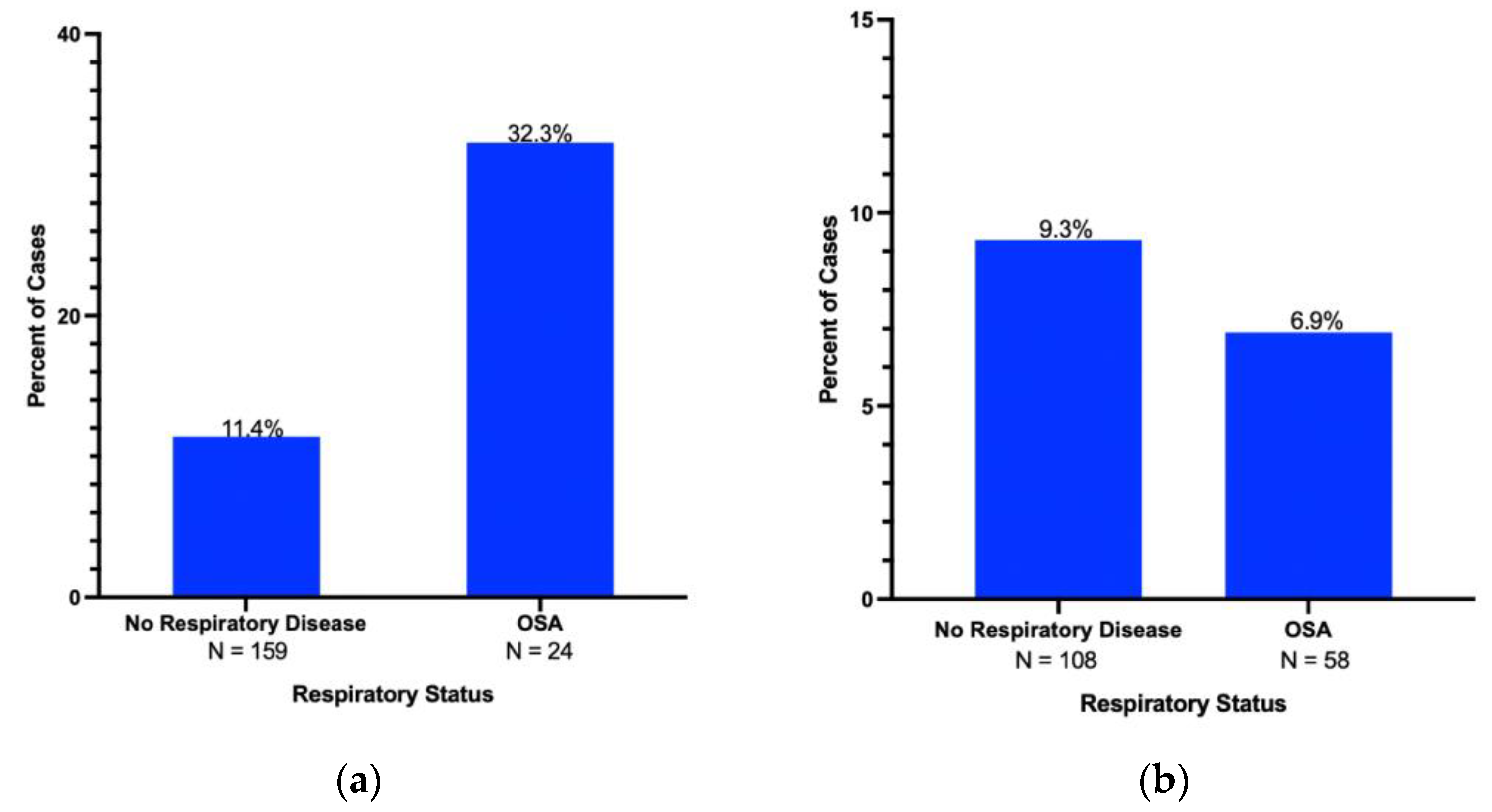
3.4. Respiratory Diseases and Linkage to Pancreatic Lesions
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, Y.; Hai, B.; Niu, X.; Ai, L.; Cao, Y.; Li, R.; Li, Y. Chronic intermittent hypoxia disturbs insulin secretion and causes pancreatic injury via the MAPK signaling pathway. Biochem. Cell Biol. 2017, 95, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Nevler, A.; Khalilieh, S.; Lavu, H.; Bowne, W.; Yeo, C.J. Hypercapnic Tissue Gene Expression and Survival in Early-Stage Pancreatic Ductal Adenocarcinoma. J. Am. Coll. Surg. 2023, 236, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Emami Nejad, A.; Najafgholian, S.; Rostami, A.; Sistani, A.; Shojaeifar, S.; Esparvarinha, M.; Nedaeinia, R.; Javanmard, S.H.; Taherian, M.; Ahmadlou, M.; et al. The role of hypoxia in the tumor microenvironment and development of cancer stem cell: A novel approach to developing treatment. Cancer Cell Int. 2021, 21, 62. [Google Scholar] [CrossRef]
- Muz, B.; de la Puente, P.; Azab, F.; Azab, A.K. The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Hypoxia 2015, 3, 83–92. [Google Scholar] [CrossRef]
- Iodice, S.; Gandini, S.; Maisonneuve, P.; Lowenfels, A.B. Tobacco and the risk of pancreatic cancer: A review and meta-analysis. Langenbecks Arch. Surg. 2008, 393, 535–545. [Google Scholar] [CrossRef]
- Heinen, M.M.; Verhage, B.A.; Goldbohm, R.A.; van den Brandt, P.A. Active and passive smoking and the risk of pancreatic cancer in the Netherlands Cohort Study. Cancer Epidemiol. Biomark. 2010, 19, 1612–1622. [Google Scholar] [CrossRef] [PubMed]
- Molina-Montes, E.; Van Hoogstraten, L.; Gomez-Rubio, P.; Löhr, M.; Sharp, L.; Molero, X.; Márquez, M.; Michalski, C.W.; Farré, A.; Perea, J.; et al. Pancreatic cancer risk in relation to lifetime smoking patterns, tobacco type, and dose-response relationships. Cancer Epidemiol. Biomark. 2020, 29, 1009–1018. [Google Scholar] [CrossRef]
- Kornum, J.B.; Svaerke, C.; Thomsen, R.W.; Lange, P.; Sørensen, H.T. Chronic obstructive pulmonary disease and cancer risk: A Danish nationwide cohort study. Respir. Med. 2012, 106, 845–852. [Google Scholar] [CrossRef]
- Chiang, C.L.; Hu, Y.W.; Wu, C.H.; Chen, Y.-T.; Liu, C.-J.; Luo, Y.-H.; Chen, Y.-M.; Chen, T.-J.; Su, K.-C.; Chou, K.-T. Spectrum of cancer risk among Taiwanese with chronic obstructive pulmonary disease. Int. J. Clin. Oncol. 2016, 21, 1014–1020. [Google Scholar] [CrossRef]
- Kamata, K.; Takenaka, M.; Nakai, A.; Omoto, S.; Miyata, T.; Minaga, K.; Matsuda, T.; Yamao, K.; Imai, H.; Chiba, Y.; et al. Association between the risk factors for pancreatic ductal adenocarcinoma and those for malignant intraductal papillary mucinous neoplasm. Oncology 2017, 93 (Suppl. S1), 102–106. [Google Scholar] [CrossRef]
- Carr, R.A.; Roch, A.M.; Shaffer, K.; Aboudi, S.; Schmidt CM 2nd DeWitt, J.; Ceppa, E.P.; House, M.G.; Zyromski, N.J.; Nakeeb, A.; Schmidt, C.M. Smoking and IPMN malignant progression. Am. J. Surg. 2017, 213, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, T.; Masuda, A.; Toyama, H.; Shiomi, H.; Zen, Y.; Sofue, K.; Takenaka, M.; Kobayashi, T.; Yagi, Y.; Yamanaka, K.; et al. Smoking status and the incidence of pancreatic cancer concomitant with intraductal papillary mucinous neoplasm. Pancreas 2017, 46, 582–588. [Google Scholar] [CrossRef]
- Xiong, H.; Lao, M.; Wang, L.; Xu, Y.; Pei, G.; Lu, B.; Shi, Q.; Chen, J.; Zhang, S.; Ou, Q. The incidence of cancer is increased in hospitalized adult patients with obstructive sleep apnea in China: A retrospective cohort study. Front. Oncol. 2022, 12, 856121. [Google Scholar] [CrossRef] [PubMed]
- Nieto, F.J.; Peppard, P.E.; Young, T.; Finn, L.; Hla, K.M.; Farré, R. Sleep-disordered breathing and cancer mortality: Results from the Wisconsin Sleep Cohort Study. Am. J. Respir. Crit. Care Med. 2012, 186, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Brenner, R.; Kivity, S.; Peker, M.; Reinhorn, D.; Keinan-Boker, L.; Silverman, B.; Liphsitz, I.; Kolitz, T.; Levy, C.; Shlomi, D.; et al. Increased risk for cancer in young patients with severe obstructive sleep apnea. Respiration 2019, 97, 15–23. [Google Scholar] [CrossRef]
- Masoero, G.; Spinaci, S.; Arossa, W.; Andriulli, A.; Gaia, E.; De Pretis, G.; Dobrilla, G.; De la Pierre, M. Pulmonary involvement in chronic pancreatitis. Dig. Dis. Sci. 1984, 29, 896–901. [Google Scholar] [CrossRef]
- Jung, J.H.; Sosnowska, D.; Weaver, J.; Parson, H.K.; Casellini, C.M.; Vinik, A.I. Expression of Hypoxia-Inducible Factors in Different Stages of Pancreatic Tumor Progression. Reports 2020, 3, 30. [Google Scholar] [CrossRef]
- Jang, J.H.; Cotterchio, M.; Borgida, A.; Gallinger, S.; Cleary, S.P. Genetic variants in carcinogen-metabolizing enzymes, cigarette smoking and pancreatic cancer risk. Carcinogenesis 2012, 33, 818–827. [Google Scholar] [CrossRef]
- Polonikov, A.V.; Samgina, T.A.; Nazarenko, P.M.; Bushueva, O.Y.; Ivanov, V.P. Alcohol Consumption and Cigarette Smoking are Important Modifiers of the Association Between Acute Pancreatitis and the PRSS1-PRSS2 Locus in Men. Pancreas 2017, 46, 230–236. [Google Scholar] [CrossRef]
- Alahmari, A.A.; Sreekumar, B.; Patel, V.; Ashat, M.; Alexandre, M.; Uduman, A.K.; Akinbiyi, E.O.; Ceplenski, A.; Shugrue, C.A.; Kolodecik, T.R.; et al. Cigarette toxin 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) induces experimental pancreatitis through α7 nicotinic acetylcholine receptors (nAChRs) in mice. PLoS ONE 2018, 13, e0197362. [Google Scholar] [CrossRef]
- Coté, G.A.; Yadav, D.; Slivka, A.; Hawes, R.H.; Anderson, M.A.; Burton, F.R.; Brand, R.E.; Banks, P.A.; Lewis, M.D.; Disario, J.A.; et al. Alcohol and smoking as risk factors in an epidemiology study of patients with chronic pancreatitis. Clin. Gastroenterol. Hepatol. 2011, 9, 266–273; quiz e27. [Google Scholar] [CrossRef] [PubMed]
- Abelson, H.; Cohen, R.; Schrayer, D.; Rappaport, M. Drug Use in America: Problem in Perspective: Volume 1. In The Technical Papers of the Second Report of the National Commission on Marihuana and Drug Abuse; Drug experience, attitudes and related behavior among adolescents and adults; US Government Printing Office: Washington, DC, USA, 1973; pp. 488–871. [Google Scholar]
- Friedman, G.D.; Siegelaub, A.B.; Seltzer, C.C. Cigarettes, alcohol, coffee and peptic ulcer. N. Engl. J. Med. 1974, 290, 469–473. [Google Scholar] [CrossRef] [PubMed]
- Maisonneuve, P.; Lowenfels, A.B.; Müllhaupt, B.; Cavallini, G.; Lankisch, P.G.; Andersen, J.R.; Dimagno, E.P.; Andrén-Sandberg, A.; Domellöf, L.; Frulloni, L.; et al. Cigarette smoking accelerates progression of alcoholic chronic pancreatitis. Gut 2005, 54, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Rebours, V.; Vullierme, M.P.; Hentic, O.; Maire, F.; Hammel, P.; Ruszniewski, P.; Lévy, P. Smoking and the course of recurrent acute and chronic alcoholic pancreatitis: A dose-dependent relationship. Pancreas 2012, 41, 1219–1224. [Google Scholar] [CrossRef]
- Yuhara, H.; Ogawa, M.; Kawaguchi, Y.; Igarashi, M.; Mine, T. Smoking and risk for acute pancreatitis: A systematic review and meta-analysis. Pancreas 2014, 43, 1201–1207. [Google Scholar] [CrossRef]
- Yadav, D.; Hawes, R.H.; Brand, R.E.; Anderson, M.A.; Money, M.E.; Banks, P.A.; Bishop, M.D.; Baillie, J.; Sherman, S.; DiSario, J.; et al. Alcohol consumption, cigarette smoking, and the risk of recurrent acute and chronic pancreatitis. Arch. Intern. Med. 2009, 169, 1035–1045. [Google Scholar] [CrossRef]
- Yadav, D.; Slivka, A.; Sherman, S.; Hawes, R.H.; Anderson, M.A.; Burton, F.R.; Brand, R.E.; Lewis, M.D.; Gardner, T.B.; Gelrud, A.; et al. Smoking is underrecognized as a risk factor for chronic pancreatitis. Pancreatology 2010, 10, 713–719. [Google Scholar] [CrossRef]
- Ye, X.; Lu, G.; Huai, J.; Ding, J. Impact of smoking on the risk of pancreatitis: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0124075. [Google Scholar] [CrossRef]
- Singhvi, A.; Yadav, D. Myths and realities about alcohol and smoking in chronic pancreatitis. Curr. Opin. Gastroenterol. 2018, 34, 355–361. [Google Scholar] [CrossRef]
- Georgiadou, D.; Sergentanis, T.N.; Sakellariou, S.; Filippakis, G.M.; Zagouri, F.; Psaltopoulou, T.; Lazaris, A.C.; Patsouris, E.; Gounaris, A.; Zografos, G.C. Immunohistochemical expression of sex steroid hormone receptors, cell cycle regulators and angiogenesis factors in intraductal papillary mucinous neoplasms: An explorative study. Anticancer Res. 2015, 35, 1049–1056. [Google Scholar]
- Celli, B.R.; Halbert, R.J.; Nordyke, R.J.; Schau, B. Airway obstruction in never smokers: Results from the Third National Health and Nutrition Examination Survey. Am. J. Med. 2005, 118, 1364–1372. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.L.; Chan, M.C.; Wang, C.C.; Lin, C.H.; Wang, H.C.; Hsu, J.Y.; Hang, L.-W.; Chang, C.-J.; Perng, S.D.-W. COPD in Taiwan: A National Epidemiology Survey. Int. J. Chron. Obstruct. Pulmon Dis. 2015, 10, 2459–2467. [Google Scholar] [PubMed]
- Hagstad, S.; Ekerljung, L.; Lindberg, A.; Backman, H.; Ronmark, E.; Lundback, B. COPD among non-smokers—Report from the obstructive lung disease in Northern Sweden (OLIN) studies. Respir. Med. 2012, 106, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.S.; Kim, K.J.; Rhee, C.K.; Yoo, K.H.; Jung, K.S.; Park, Y.B. Prevalence, characteristics, and risk of exacerbation in young patients with chronic obstructive pulmonary disease. Respir. Res. 2022, 23, 212. [Google Scholar] [CrossRef]
- Lamprecht, B.; Schirnhofer, L.; Kaiser, B.; Buist, S.; Studnicka, M. Non-reversible airway obstruction in never smokers: Results from the Austrian BOLD study. Respir. Med. 2008, 102, 1833–1838. [Google Scholar] [CrossRef]
- Palamaner Subash Shantha, G.; Kumar, A.A.; Cheskin, L.J.; Pancholy, S.B. Association between sleep-disordered breathing, obstructive sleep apnea, and cancer incidence: A systematic review and meta-analysis. Sleep Med. 2015, 16, 1289–1294. [Google Scholar] [CrossRef]
- Chang, W.P.; Liu, M.E.; Chang, W.C.; Yang, A.C.; Ku, Y.C.; Pai, J.T.; Lin, Y.W.; Tsai, S.J. Sleep apnea and the subsequent risk of breast cancer in women: A nationwide population-based cohort study. Sleep Med. 2014, 15, 1016–1020. [Google Scholar] [CrossRef]
- Chen, J.C.; Hwang, J.H. Sleep apnea increased incidence of primary central nervous system cancers: A nationwide cohort study. Sleep Med. 2014, 15, 749–754. [Google Scholar] [CrossRef]
- Dal Molin, M.; Brant, A.; Blackford, A.L.; Griffin, J.F.; Shindo, K.; Barkley, T.; Rezaee, N.; Hruban, R.H.; Wolfgang, C.L.; Goggins, M. Obstructive Sleep Apnea and Pathological Characteristics of Resected Pancreatic Ductal Adenocarcinoma. PLoS ONE 2016, 11, e0164195. [Google Scholar] [CrossRef]
- Bhat, T.A.; Panzica, L.; Kalathil, S.G.; Thanavala, Y. Immune dysfunction in patients with chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. 2015, 12 (Suppl. S2), S169–S175. [Google Scholar] [CrossRef]
- Cruz, T.; López-Giraldo, A.; Noell, G.; Casas-Recasens, S.; Garcia, T.; Molins, L.; Juan, M.; Fernandez, A.M.; Agustí, A.; Faner, R. Multi-level immune response network in mild-moderate Chronic Obstructive Pulmonary Disease (COPD). Respir. Res. 2019, 20, 152. [Google Scholar] [CrossRef] [PubMed]
- Oudijk, E.J.; Lammers, J.W.; Koenderman, L. Systemic inflammation in chronic obstructive pulmonary disease. Eur. Respir. J. 2003, 46, 5s–13s. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, K.; Huppertz, T.; Radsak, M.; Gouveris, H. Cellular immune dysfunction in obstructive sleep apnea. Front. Surg. 2022, 9, 890377. [Google Scholar] [CrossRef] [PubMed]
- Fujino, M.; Aishima, S.; Shindo, K.; Oda, Y.; Morimatsu, K.; Tsutsumi, K.; Otsuka, T.; Tanaka, M.; Oda, Y. Expression of glucose transporter-1 is correlated with hypoxia-inducible factor 1α and malignant potential in pancreatic neuroendocrine tumors. Oncol. Lett. 2016, 12, 3337–3343. [Google Scholar] [CrossRef] [PubMed]
- Semenza, G.L. Targeting HIF-1 for cancer therapy. Nat. Rev. Cancer 2003, 3, 721–732. [Google Scholar] [CrossRef]
- Koh, M.Y.; Lemos, R.; Jr Liu, X.; Powis, G. The hypoxia-associated factor switches cells from HIF-1alpha- to HIF-2alpha-dependent signaling promoting stem cell characteristics, aggressive tumor growth and invasion. Cancer Res. 2011, 71, 4015–4027. [Google Scholar] [CrossRef]
- Carmeliet, P.; Dor, Y.; Herbert, J.M.; Fukumura, D.; Brusselmans, K.; Dewerchin, M.; Neeman, M.; Bono, F.; Abramovitch, R.; Maxwell, P.; et al. Role of HIF-1alpha in hypoxia-mediated apoptosis, cell proliferation and tumour angiogenesis. Nature 1998, 394, 485–490. [Google Scholar] [CrossRef]
- Luo, D.; Wang, Z.; Wu, J.; Jiang, C.; Wu, J. The role of hypoxia inducible factor-1 in hepatocellular carcinoma. Biomed. Res. Int. 2014, 2014, 409272. [Google Scholar] [CrossRef]
- Nagaraju, G.P.; Bramhachari, P.V.; Raghu, G.; El-Rayes, B.F. Hypoxia inducible factor-1alpha: Its role in colorectal carcinogenesis and metastasis. Cancer Lett. 2015, 366, 11–18. [Google Scholar] [CrossRef]
- Parks, S.K.; Cormerais, Y.; Marchiq, I.; Pouyssegur, J. Hypoxia optimises tumour growth by controlling nutrient import and acidic metabolite export. Mol. Aspects Med. 2016, 47–48, 3–14. [Google Scholar] [CrossRef]
- Xie, J.; Xiao, Y.; Zhu, X.Y.; Ning, Z.Y.; Xu, H.F.; Wu, H.M. Hypoxia regulates stemness of breast cancer MDA-MB-231 cells. Med. Oncol. 2016, 33, 42. [Google Scholar] [CrossRef] [PubMed]
- Maharjan, C.K.; Ear, P.H.; Tran, C.G.; Howe, J.R.; Chandrasekharan, C.; Quelle, D.E. Pancreatic neuroendocrine tumors: Molecular mechanisms and therapeutic targets. Cancers 2021, 13, 5117. [Google Scholar] [CrossRef] [PubMed]
- Obata, S.; Goi, T.; Nakazawa, T.; Kimura, Y.; Katayama, K.; Yamaguchi, A. Changes in CO2 concentration increase the invasive ability of colon cancer cells. Anticancer Res. 2013, 33, 1881–1885. [Google Scholar]
- Kikuchi, R.; Iwai, Y.; Tsuji, T.; Watanabe, Y.; Koyama, N.; Yamaguchi, K.; Nakamura, H.; Aoshiba, K. Hypercapnic tumor microenvironment confers chemoresistance to lung cancer cells by reprogramming mitochondrial metabolism in vitro. Free Radic Biol. Med. 2019, 134, 200–214. [Google Scholar] [CrossRef]
- Nevler, A.; Brown, S.Z.; Nauheim, D.; Portocarrero, C.; Rodeck, U.; Bassig, J.; Schultz, C.W.; McCarthy, G.A.; Lavu, H.; Yeo, T.P.; et al. Effect of hypercapnia, an element of obstructive respiratory disorder, on pancreatic cancer chemoresistance and progression. J. Am. Coll. Surg. 2020, 230, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Woo, A.; Lee, S.W.; Koh, H.Y.; Kim, M.A.; Han, M.Y.; Yon, D.K. Incidence of cancer after asthma development: 2 independent population-based cohort studies. J. Allergy Clin. Immunol. 2021, 147, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Bian, J.; Chen, Z.; Fishe, J.N.; Zhang, D.; Braithwaite, D.; George, T.J.; Shenkman, E.A.; Licht, J.D. Cancer incidence after asthma diagnosis: Evidence from a large clinical research network in the United States. Cancer Med. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Wang, H.; Diepgen, T.L. Is atopy a protective or a risk factor for cancer? A review of epidemiological studies. Allergy 2005, 60, 1098–1111. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Rubio, P.; Zock, J.P.; Rava, M.; Marquez, M.; Sharp, L.; Hidalgo, M.; Carrato, A.; Ilzarbe, L.; Michalski, C.; Molero, X.; et al. Reduced risk of pancreatic cancer associated with asthma and nasal allergies. Gut 2017, 66, 314–322. [Google Scholar] [CrossRef]
- Gomez-Rubio, P.; Rosato, V.; Márquez, M.; Bosetti, C.; Molina-Montes, E.; Rava, M.; Piñero, J.; Michalski, C.W.; Farré, A.; Molero, X.; et al. A systems approach identifies time-dependent associations of multimorbidities with pancreatic cancer risk. Ann. Oncol. 2017, 28, 1618–1624. [Google Scholar] [CrossRef]
- Wroblewski, M.; Velthaus, J.L.; Bauer, R.; Müller, V.; Schem, C.; Fasching, P.A.; Karn, T.; Fehm, T.N.; Kühn, T.; Rack, B.K.; et al. Effect of mast cells on efficacy of anti-angiogenic therapy by secreting matrix-degrading granzyme b. J. Clin. Oncol. 2017, 15, 11522. [Google Scholar] [CrossRef]
- Cotterchio, M.; Lowcock, E.; Bider-Canfield, Z.; Lemire, M.; Greenwood, C.; Gallinger, S.; Hudson, T. Association between variants in atopy-related immunologic candidate genes and pancreatic cancer risk. PLoS ONE 2015, 10, e0125273. [Google Scholar] [CrossRef] [PubMed]


| Total Cases N = 723 | No Respiratory Disease (NRD) N = 267 | Smoking History N = 382 | COPD N = 59 | OSA N = 82 | Asthma N = 78 | Overall N (%)/Mean (SD) |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male (N=, %) | 108 (40.4%) | 213 (55.8%) | 34 (57.6%) | 58 (70.7%) | 31 (39.7%) | 363 (50.2%) |
| Female (N=, %) | 159 (59.6%) | 169 (44.2%) | 25 (42.4%) | 24 (29.3%) | 47 (60.3%) | 360 (49.8%) |
| Age (Mean, SD) | 66.3 (±12.8) | 67.5 (±9.82) | 69.9 (±6.80) | 66.6 (±8.48) | 64.6 (±11.9) | 66.8 (±11.25) |
| BMI (Mean, SD) | 26.3 (±5.26) | 27.0 (±5.44) | 26.2 (±5.03) | 29.9 (±5.95) | 27.1 (±5.01) | 27 (±5.6) |
| No Respiratory Disease (N=, %) | 267 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 267 (36.9%) |
| Smoking Data | ||||||
| Positive Smoking History (N=, %) | 0 (0%) | 382 (100%) | 51 (86.4%) | 48 (58.2%) | 37 (47.4%) | 382 (52.8%) |
| Current Smokers (N=, %) | 0 (0%) | 63 (16.5%) | 16 (27.1%) | 9 (11.0%) | 8 (10.3%) | 63 (8.7%) |
| Pack Years (Mean, SD) | 0 (±0) | 26.1 (±21.0) | 33.3 (±24.6) | 15.1 (±20.0) | 10.4 (±15.4) | 23.2 (±20.1) |
| Years Since Quitting (Mean, SD) | 0 (±0) | 22.9 (±17.5) | 15.92 (±16.6) | 27.4 (±14.0) | 23.4 (±15.2) | 22 (±18.1) |
| Lung Diseases | ||||||
| Any Lung Disease (N=, %) | 0 (0%) | 108 (28.3%) | 59 (100%) | 82 (100%) | 78 (100%) | 182 (25.2%) |
| COPD (N=, %) | 0 (0%) | 51 (13.4%) | 59 (100%) | 16 (19.5%) | 13 (16.7%) | 59 (8.2%) |
| Asthma (N=, %) | 0 (0%) | 37 (9.7%) | 13 (22%) | 15 (18.3%) | 78 (100%) | 78 (10.8%) |
| OSA (N=, %) | 0 (0%) | 48 (12.7%) | 16 (27.1%) | 82 (100%) | 15 (19.2%) | 82 (11.3%) |
| Pathology | Number of Cases (N=, %) |
|---|---|
| Pancreatic Ductal Adenocarcinoma (PDAC) | 374 (51.73%) |
| Intraductal Papillary Mucinous Neoplasm (IPMN) | 79 (10.93%) |
| Ampullary Adenocarcinoma | 53 (7.33%) |
| Pancreatic Neuroendocrine Tumor (PNET) | 50 (6.92%) |
| Other Benign | 49 (6.78%) |
| Duodenal Adenocarcinoma | 43 (5.95%) |
| Cholangiocarcinoma | 20 (2.77%) |
| Histologically Proven Chronic Pancreatitis | 21 (2.90%) |
| Adenosquamous Carcinoma | 11 (1.52%) |
| Other Malignant | 11 (1.52%) |
| Solid Pseudopapillary Neoplasm (SPN) | 6 (0.83%) |
| Gastrointestinal Stromal Tumor (GIST) | 5 (0.69%) |
| Sarcomatoid Carcinoma | 2 (0.28%) |
| Acinar Cell Carcinoma | 1 (0.14%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ream, C.; Sabitsky, M.; Huang, R.; Hammelef, E.; Yeo, T.P.; Lavu, H.; Yeo, C.J.; Bowne, W.; Nevler, A. Association of Smoking and Respiratory Disease History with Pancreatic Pathologies Requiring Surgical Resection. Cancers 2023, 15, 2935. https://doi.org/10.3390/cancers15112935
Ream C, Sabitsky M, Huang R, Hammelef E, Yeo TP, Lavu H, Yeo CJ, Bowne W, Nevler A. Association of Smoking and Respiratory Disease History with Pancreatic Pathologies Requiring Surgical Resection. Cancers. 2023; 15(11):2935. https://doi.org/10.3390/cancers15112935
Chicago/Turabian StyleReam, Carolyn, Matthew Sabitsky, Rachel Huang, Emma Hammelef, Theresa P. Yeo, Harish Lavu, Charles J. Yeo, Wilbur Bowne, and Avinoam Nevler. 2023. "Association of Smoking and Respiratory Disease History with Pancreatic Pathologies Requiring Surgical Resection" Cancers 15, no. 11: 2935. https://doi.org/10.3390/cancers15112935
APA StyleReam, C., Sabitsky, M., Huang, R., Hammelef, E., Yeo, T. P., Lavu, H., Yeo, C. J., Bowne, W., & Nevler, A. (2023). Association of Smoking and Respiratory Disease History with Pancreatic Pathologies Requiring Surgical Resection. Cancers, 15(11), 2935. https://doi.org/10.3390/cancers15112935






