Early Prediction of Response Focused on Tumor Markers in Atezolizumab plus Bevacizumab Therapy for Hepatocellular Carcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
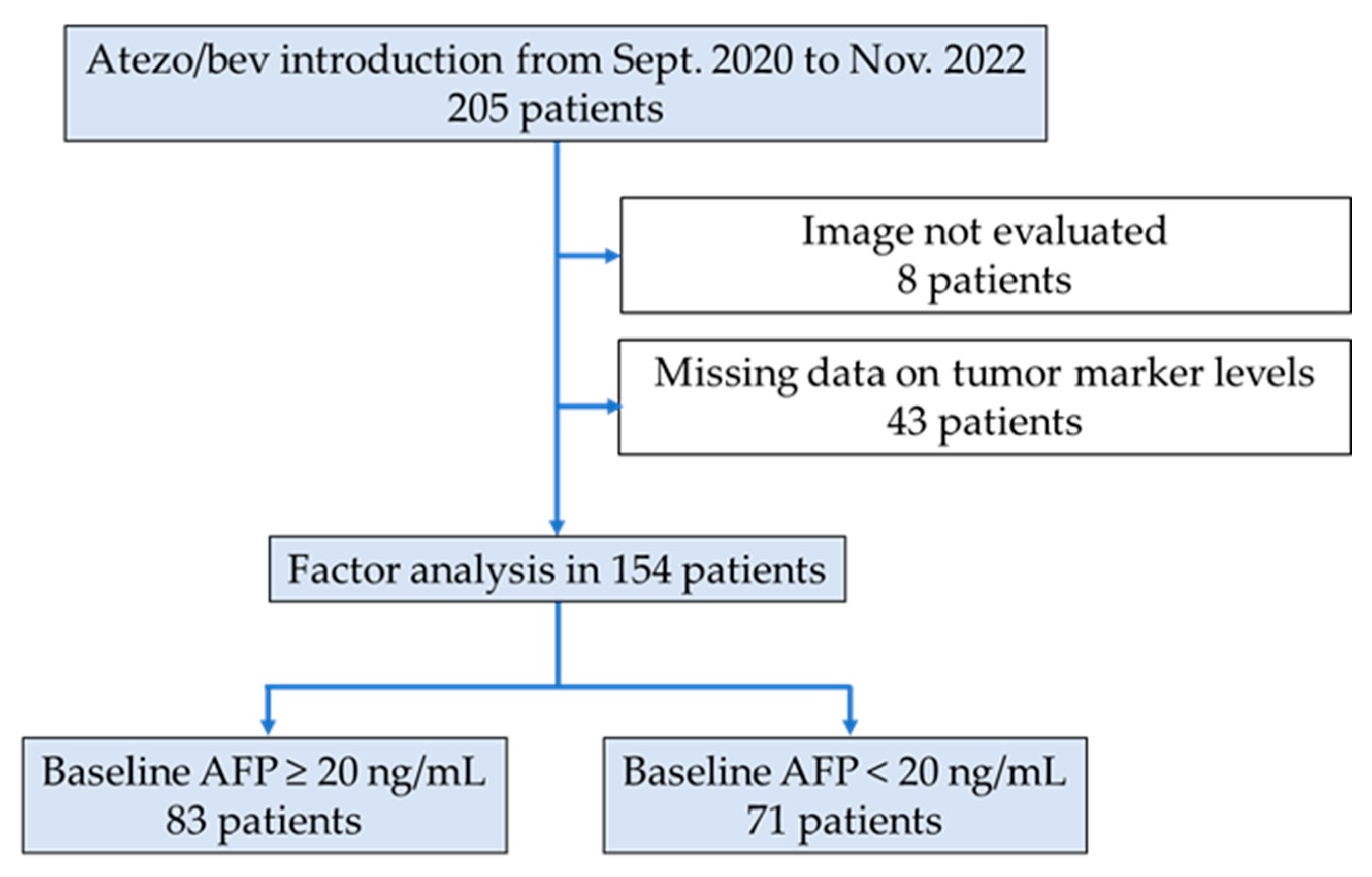
2.1. Study Design and Patients
2.2. Treatment Protocol and Evaluation of Treatment Response and Tumor Markers
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Relationship between Treatment Response and Change in AFP Levels
3.3. Predictor of OR Outcome in the High-AFP Group
3.4. Predictor of Early PD in the High-AFP Group
3.5. Predictor of OR Outcome in the Low-AFP Group
3.6. Predictor of Early PD in the Low-AFP Group
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Abou-Alfa, G.K.; Lau, G.; Kudo, M.; Chan, S.L.; Kelley, R.K.; Furuse, J.; Sukeepaisarnjaroen, W.; Kang, Y.-K.; Van Dao, T.; De Toni, E.N.; et al. Tremelimumab plus durvalumab in unresectable hepatocellular carcinoma. NEJM Evid. 2022, 1, 1–12. [Google Scholar] [CrossRef]
- Hasegawa, K.; Takemura, N.; Yamashita, T.; Watadani, T.; Kaibori, M.; Kubo, S.; Shimada, M.; Nagano, H.; Hatano, E.; Ai-kata, H.; et al. Clinical Practice Guidelines for Hepatocellular Carcinoma: The Japan Society of Hepatology 2021 version (5th JSH-HCC Guidelines). Hepatol. Res. 2023, 53, 383–390. [Google Scholar] [CrossRef]
- Llovet, J.M.; Villanueva, A.; Marrero, J.A.; Schwartz, M.; Meyer, T.; Galle, P.R.; Lencioni, R.; Greten, T.F.; Kudo, M.; Mandrekar, S.J.; et al. Trial design and endpoints in hepatocellular carcinoma: AASLD consensus conference. Hepatology 2021, 73, 158–191. [Google Scholar] [CrossRef]
- Gordan, J.D.; Kennedy, E.B.; Abou-Alfa, G.K.; Beg, M.S.; Brower, S.T.; Gade, T.P.; Goff, L.; Gupta, S.; Guy, J.; Harris, W.P.; et al. Systemic therapy for advanced hepatocellular carcinoma: ASCO guideline. J. Clin. Oncol. 2020, 38, 4317–4345. [Google Scholar] [CrossRef] [PubMed]
- Vogel, A.; Martinelli, E.; Vogel, A.; Cervantes, A.; Chau, I.; Daniele, B.; Llovet, J.M.; Meyer, T.; Nault, J.-C.; Neumann, U.; et al. Updated treatment recommendations for hepatocellular carcinoma (HCC) from the ESMO clinical practice guidelines. Ann. Oncol. 2021, 32, 801–805. [Google Scholar] [CrossRef]
- Himmelsbach, V.; Pinter, M.; Scheiner, B.; Venerito, M.; Sinner, F.; Zimpel, C.; Marquardt, J.U.; Trojan, J.; Waidmann, O.; Finkelmeier, F. Efficacy and safety of atezolizumab and bevacizumab in the real-world treatment of advanced hepatocellular carcinoma: Experience from four tertiary centers. Cancers 2022, 14, 1722. [Google Scholar] [CrossRef]
- Hiraoka, A.; Kumada, T.; Tada, T.; Hirooka, M.; Kariyama, K.; Tani, J.; Atsukawa, M.; Takaguchi, K.; Itobayashi, E.; Fukunishi, S.; et al. Atezolizumab plus bevacizumab treatment for unresectable hepatocellular carcinoma: Early clinical experience. Cancer Rep. 2022, 5, e1464. [Google Scholar] [CrossRef]
- Hayakawa, Y.; Tsuchiya, K.; Kurosaki, M.; Yasui, Y.; Kaneko, S.; Tanaka, Y.; Ishido, S.; Inada, K.; Kirino, S.; Yamashita, K.; et al. Early experience of atezolizumab plus bevacizumab therapy in Japanese patients with unresectable hepatocellular carcinoma in real-world practice. Investig. New Drugs 2022, 40, 392–402. [Google Scholar] [CrossRef]
- Ando, Y.; Kawaoka, T.; Kosaka, M.; Shirane, Y.; Johira, Y.; Miura, R.; Murakami, S.; Yano, S.; Amioka, K.; Naruto, K.; et al. Early tumor response and safety of atezolizumab plus bevacizumab for patients with unresectable hepatocellular carcinoma in real-world practice. Cancers 2021, 13, 3958. [Google Scholar] [CrossRef]
- Sharma, R.; Pillai, A.; Marron, T.U.; Fessas, P.; Saeed, A.; Jun, T.; Dharmapuri, S.; Szafron, D.; Naqash, R.A.; Gampa, A.; et al. Patterns and outcomes of subsequent therapy after immune checkpoint inhibitor discontinuation in HCC. Hepatol. Commun. 2022, 6, 1776–1785. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, L.H.; Seymour, L.; Litière, S.; Ford, R.; Gwyther, S.; Mandrekar, S.; Shankar, L.; Bogaerts, J.; Chen, A.; Dancey, J.; et al. RECIST 1.1–Standardisation and disease-specific adaptations: Perspectives from the RECIST working group. Eur. J. Cancer 2016, 62, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, A.; Michitaka, K.; Kumada, T.; Izumi, N.; Kadoya, M.; Kokudo, N.; Kubo, S.; Matsuyama, Y.; Nakashima, O.; Sakamoto, M.; et al. Validation and potential of albumin-bilirubin grade and prognostication in a nationwide survey of 46,681 hepatocellular carcinoma patients in Japan: The need for a more detailed evaluation of hepatic function. J. Liver Cancer 2017, 6, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Mazzaferro, V.; Llovet, J.M.; Miceli, R.; Bhoori, S.; Schiavo, M.; Mariani, L.; Camerini, T.; Roayaie, S.; Schwartz, M.E.; Grazi, G.L.; et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: A retrospective, exploratory analysis. Lancet Oncol. 2009, 10, 35–43. [Google Scholar] [CrossRef]
- Marrero, J.A.; Kulik, L.M.; Sirlin, C.B.; Zhu, A.X.; Finn, R.S.; Abecassis, M.M.; Roberts, L.R.; Heimbach, J.K. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American association for the study of liver diseases. Hepatology 2018, 68, 723–750. [Google Scholar] [CrossRef]
- Omata, M.; Cheng, A.-L.; Kokudo, N.; Kudo, M.; Lee, J.M.; Jia, J.; Tateishi, R.; Han, K.-H.; Chawla, Y.K.; Shiina, S.; et al. Asia–Pacific clinical practice guidelines on the management of hepatocellular carcinoma: A 2017 update. Hepatol. Int. 2017, 11, 317–370. [Google Scholar] [CrossRef]
- He, C.; Peng, W.; Liu, X.; Li, C.; Li, X.; Wen, T.F. Post-treatment alpha-fetoprotein response predicts prognosis of patients with hepatocellular carcinoma: A meta-analysis. Medicine 2019, 98, e16557. [Google Scholar] [CrossRef]
- Kuzuya, T.; Ishigami, M.; Ishizu, Y.; Honda, T.; Hayashi, K.; Katano, Y.; Hirooka, Y.; Ishikawa, T.; Nakano, I.; Goto, H. Early clinical response after 2 weeks of sorafenib therapy predicts outcomes and anti-tumor response in patients with advanced hepatocellular carcinoma. PLoS ONE 2015, 10, e0138776. [Google Scholar] [CrossRef]
- Kodama, K.; Kawaoka, T.; Namba, M.; Uchikawa, S.; Ohya, K.; Morio, K.; Nakahara, T.; Murakami, E.; Yamauchi, M.; Hiramatsu, A.; et al. Correlation between early tumor marker response and imaging response in patients with advanced hepatocellular carcinoma treated with lenvatinib. Oncology 2019, 97, 75–81. [Google Scholar] [CrossRef]
- Shao, Y.-Y.; Lin, Z.-Z.; Hsu, C.; Shen, Y.-C.; Hsu, C.-H.; Cheng, A.-L. Early alpha-fetoprotein response predicts treatment efficacy of antiangiogenic systemic therapy in patients with advanced hepatocellular carcinoma. Cancer 2010, 116, 4590–4596. [Google Scholar] [CrossRef]
- Saeki, I.; Yamasaki, T.; Yamashita, S.; Hanazono, T.; Urata, Y.; Furutani, T.; Yokoyama, Y.; Oishi, T.; Maeda, M.; Kimura, T.; et al. Early predictors of objective response in patients with hepatocellular carcinoma undergoing lenvatinib treatment. Cancers 2020, 12, 779. [Google Scholar] [CrossRef] [PubMed]
- Tamaki, N.; Tada, T.; Kurosaki, M.; Yasui, Y.; Ochi, H.; Mashiba, T.; Sakamoto, A.; Marusawa, H.; Narita, R.; Uchida, Y.; et al. Optimal threshold of alpha-fetoprotein response in patients with unresectable hepatocellular carcinoma treated with atezolizumab and bevacizumab. Investig. New Drugs 2022, 40, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Zhu, A.X.; Dayyani, F.; Yen, C.J.; Ren, Z.; Bai, Y.; Meng, Z.; Pan, H.; Dillon, P.; Mhatre, S.K.; Gaillard, V.E.; et al. Alpha-fetoprotein as a potential surrogate biomarker for atezolizumab + bevacizumab treatment of hepatocellular carcinoma. Clin. Cancer Res. 2022, 28, 3537–3545. [Google Scholar] [CrossRef]
- Iwamoto, H.; Shimose, S.; Noda, Y.; Shirono, T.; Niizeki, T.; Nakano, M.; Okamura, S.; Kamachi, N.; Suzuki, H.; Sakai, M.; et al. Initial experience of atezolizumab plus bevacizumab for unresectable hepatocellular carcinoma in real-world clinical practice. Cancers 2021, 13, 2786. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, N.; Hillan, K.J.; Gerber, H.P.; Novotny, W. Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat. Rev. Drug Discov. 2004, 3, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.F.; Bruno, R.; Eppler, S.; Novotny, W.; Lum, B.; Gaudreault, J. Clinical pharmacokinetics of bevacizumab in patients with solid tumors. Cancer Chemother. Pharmacol. 2008, 62, 779–786. [Google Scholar] [CrossRef] [PubMed]
- van der Kooij, M.K.; Suijkerbuijk, K.P.M.; Aarts, M.J.B.; van den Berkmortel, F.W.P.J.; Blank, C.U.; Boers-Sonderen, M.J.; van Breeschoten, J.; van den Eertwegh, A.J.M.; de Groot, J.W.B.; Haanen, J.B.A.G.; et al. Safety and efficacy of checkpoint inhibition in patients with melanoma and preexisting autoimmune disease: A cohort study. Ann. Intern. Med. 2021, 174, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Meserve, J.; Facciorusso, A.; Holmer, A.K.; Annese, V.; Sandborn, W.J.; Singh, S. Systematic review with meta-analysis: Safety and tolerability of immune checkpoint inhibitors in patients with pre-existing inflammatory bowel diseases. Aliment. Pharmacol. Ther. 2021, 53, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Eso, Y.; Takeda, H.; Taura, K.; Takai, A.; Takahashi, K.; Seno, H. Pretreatment neutrophil-to-lymphocyte ratio as a predictive marker of response to atezolizumab plus bevacizumab for hepatocellular carcinoma. Curr. Oncol. 2021, 28, 4157–4166. [Google Scholar] [CrossRef]
- Wu, Y.L.; Fulgenzi, C.A.M.; D’Alessio, A.; Cheon, J.; Nishida, N.; Saeed, A.; Wietharn, B.; Cammarota, A.; Pressiani, T.; Personeni, N.; et al. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios as prognostic biomarkers in unresectable hepatocellular carcinoma treated with atezolizumab plus bevacizumab. Cancers 2022, 14, 5834. [Google Scholar] [CrossRef]
- Wang, J.-H.; Chen, Y.-Y.; Kee, K.-M.; Wang, C.-C.; Tsai, M.-C.; Kuo, Y.-H.; Hung, C.-H.; Li, W.-F.; Lai, H.-L.; Chen, Y.-H. The prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with hepatocellular carcinoma receiving atezolizumab plus bevacizumab. Cancers 2022, 14, 343. [Google Scholar] [CrossRef] [PubMed]
- Ochi, H.; Kurosaki, M.; Joko, K.; Mashiba, T.; Tamaki, N.; Tsuchiya, K.; Marusawa, H.; Tada, T.; Nakamura, S.; Narita, R.; et al. Usefulness of neutrophil-to-lymphocyte ratio in predicting progression and survival outcomes after atezolizumab–bevacizumab treatment for hepatocellular carcinoma. Hepatol. Res. 2023, 53, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Myojin, Y.; Kodama, T.; Sakamori, R.; Maesaka, K.; Matsumae, T.; Sawai, Y.; Imai, Y.; Ohkawa, K.; Miyazaki, M.; Tanaka, S.; et al. Interleukin-6 is a circulating prognostic biomarker for hepatocellular carcinoma patients treated with combined immunotherapy. Cancers 2022, 14, 883. [Google Scholar] [CrossRef] [PubMed]




| Total | AFP ≥ 20 ng/mL | AFP < 20 ng/mL | ||
|---|---|---|---|---|
| Factor | n = 154 | n = 83 | n = 71 | |
| Age (years) | 75 (70–80) | 74 (68–80) | 76 (70–80) | |
| Sex | Male/female | 124/30 | 61/22 | 63/8 |
| ECOG-PS | 0/1/2/3 | 132/18/2/2 | 71/8/2/2 | 61/10/0/0 |
| Etiology | HBV/HCV/NBNC | 17/52/85 | 12/31/40 | 5/21/45 |
| Child-Pugh class | A/B | 145/9 | 75/8 | 70/1 |
| ALBI score | −2.32 (−2.65 to −2.09) | −2.31 (−2.68 to −1.99) | −2.33 (−2.64 to −2.17) | |
| mALBI grade | 1/2a/2b/3 | 46/38/68/2 | 26/17/38/2 | 20/21/30/0 |
| BCLC | A/B/C | 11/79/64 | 5/37/41 | 6/42/23 |
| MVI | Absence/presence | 109/45 | 51/32 | 58/13 |
| EHS | Absence/presence | 125/29 | 62/21 | 63/8 |
| Line | First/late | 99/55 | 56/27 | 43/28 |
| Tumor number | 4 (2–10) | 4 (2–10) | 4 (3–7) | |
| Tumor size | (mm) | 30 (18–61) | 43 (21–82) | 24 (15–40) |
| UT7 | IN/OUT | 56/98 | 25/58 | 31/40 |
| AFP | (ng/mL) | 31.1 (4.8–634.0) | 528.4 (136.7–6243.0) | 4.4 (2.4–8.8) |
| DCP | (mAU/mL) | 382.4 (51.7–4874.0) | 868.0 (160.8–12426.0) | 120.7 (29.2–1004.0) |
| Response | CR | PR | SD | PD | ORR | DCR |
|---|---|---|---|---|---|---|
| Total (n = 154) | 9 | 46 | 65 | 34 | 35.7% | 77.9% |
| High-AFP group (n = 83) | ||||||
| Decrease in AFP level > 30% | 2 | 14 | 5 | 2 | 69.6% * | 95.7% ** |
| Decrease in AFP level ≤ 30% | 1 | 16 | 24 | 19 | 28.3% | 68.3% |
| Low-AFP group (n = 71) | ||||||
| Baseline DCP < 40 mAU/mL | 2 | 10 | 9 | 1 | 54.6% † | 95.5% †† |
| Baseline DCP ≥ 40 mAU/mL | 4 | 6 | 26 | 13 | 20.4% | 73.5% |
| Factors | Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | p-Value | ||
| Age | <75/≥75 years | 0.471 | 0.192–1.153 | 0.0993 | |||
| Sex | Male/female | 0.726 | 0.271–1.947 | 0.5251 | |||
| ECOG-PS | 0/1–3 | 0.614 | 0.180–2.097 | 0.4360 | |||
| Etiology | Viral/non-viral | 1.806 | 0.740–4.410 | 0.1943 | 1.729 | 0.613–4.877 | 0.3004 |
| Line | First/late | 1.500 | 0.575–3.915 | 0.4075 | 1.756 | 0.558–5.526 | 0.3355 |
| mALBI | 1–2a/2b–3 | 0.655 | 0.271–1.585 | 0.3477 | 0.557 | 0.200–1.552 | 0.2634 |
| BCLC | A–B/C | 1.300 | 0.538–3.139 | 0.5597 | |||
| MVI | Absence/presence | 1.807 | 0.714–4.575 | 0.2119 | 2.096 | 0.691–6.356 | 0.1911 |
| EHS | Absence/presence | 1.444 | 0.512–4.079 | 0.4875 | 1.702 | 0.513–5.646 | 0.3848 |
| UT7 | IN/OUT | 1.014 | 0.389–2.643 | 0.9765 | 1.161 | 0.371–3.639 | 0.7975 |
| Decrease in AFP level >30% | Yes/no | 5.782 | 2.022–16.535 | 0.0011 | 5.517 | 1.773–17.165 | 0.0032 |
| Baseline AFP <400 ng/mL | Yes/no | 1.105 | 0.458–2.665 | 0.8243 | |||
| Baseline DCP <40 mAU/mL | Yes/no | 1.630 | 0.376–7.062 | 0.5139 | |||
| Factors | Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | p-Value | ||
| Age | ≥75/<75 years | 0.606 | 0.218–1.684 | 0.3369 | |||
| Sex | Female/male | 1.259 | 0.414–3.828 | 0.6848 | |||
| ECOG-PS | 1–3/0 | 1.719 | 0.458–6.454 | 0.4224 | |||
| Etiology | Non-viral/viral | 1.100 | 0.402–3.009 | 0.8527 | 1.390 | 0.430–4.493 | 0.5824 |
| Line | Late/first | 0.857 | 0.288–2.550 | 0.7817 | 0.656 | 0.171–2513 | 0.5385 |
| mALBI | 2b–3/1–2a | 0.646 | 0232–1.794 | 0.4017 | 0.606 | 0.187–1.969 | 0.4048 |
| BCLC | C/A–B | 2.321 | 0.817–6.598 | 0.1141 | |||
| MVI | Presence/absence | 1.864 | 0.673–5.159 | 0.2308 | 2.344 | 0.700–7.855 | 0.1673 |
| EHS | Presence/absence | 3.478 | 1.178–10.264 | 0.0240 | 3.682 | 1.106–12.262 | 0.0337 |
| UT7 | OUT/IN | 1.008 | 0.336–3.019 | 0.9892 | 0.741 | 0.202–2.719 | 0.6514 |
| Increase in AFP level ≥30% | Yes/no | 3.478 | 1.178–10.264 | 0.0240 | 4.077 | 1.180–14.092 | 0.0264 |
| Factors | Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | p-Value | ||
| Age | <75/≥75 years | 1.227 | 0.448–3.362 | 0.6904 | |||
| Sex | Male/female | 0.720 | 0.156–3.321 | 0.6733 | |||
| ECOG-PS | 0/1 | 1.951 | 0.379–10.050 | 0.4241 | |||
| Etiology | Viral/non-viral | 1.719 | 0.614–4.814 | 0.3027 | 1.600 | 0.487–5.232 | 0.4394 |
| Line | First/late | 1.607 | 0.556–4.642 | 0.3806 | 0.827 | 0.248–2.759 | 0.7567 |
| mALBI | 1–2a/2b–3 | 1.426 | 0.506–4.015 | 0.5017 | 1.053 | 0.326–3.402 | 0.9306 |
| BCLC | A–B/C | 0.578 | 0.695–4.955 | 0.3067 | |||
| MVI | Absence/presence | 2.895 | 0.584–14.352 | 0.1932 | 2.066 | 0.370–11.537 | 0.4085 |
| EHS | Absence/presence | 0.400 | 0.090–1.774 | 0.2280 | 0.352 | 0.063–1.952 | 0.2322 |
| UT7 | IN/OUT | 1.895 | 0.685–5.239 | 0.2181 | 1.221 | 0.379–3.927 | 0.9306 |
| Baseline DCP <40 mAU/mL | Yes/no | 4.680 | 1.574–13.912 | 0.0055 | 3.978 | 1.236–12.803 | 0.0206 |
| Factors | Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | p-Value | ||
| Age | ≥75/<75 years | 0.586 | 0.180–1.908 | 0.3749 | |||
| Sex | Female/male | 1.417 | 0.254–7.907 | 0.6913 | |||
| ECOG-PS | 1/0 | 1.021 | 0.192–5.440 | 0.9807 | |||
| Etiology | Non-viral/viral | 1.571 | 0.439–5.631 | 0.4876 | 1.279 | 0.218–7.502 | 0.7850 |
| Line | Late/first | 5.417 | 1.495–19.619 | 0.0101 | 4.720 | 0.040–1.115 | 0.0671 |
| mALBI | 2b–3/1–2a | 3.086 | 0.912–10.436 | 0.0699 | 2.924 | 0.579–14.773 | 0.1941 |
| BCLC | C/A–B | 1.765 | 0.531–5.865 | 0.3540 | |||
| MVI | Presence/absence | 5.357 | 1.429–20.082 | 0.0128 | 3.556 | 0.638–19.813 | 0.1477 |
| EHS | Presence/absence | 2.836 | 0.589–13.664 | 0.1937 | 9.806 | 0.572–167.988 | 0.1665 |
| UT7 | OUT/IN | 14.444 | 1.770–117.879 | 0.0127 | 15.756 | 1.398–177.499 | 0.0257 |
| Baseline DCP ≥40 mAU/mL | Yes/no | 7.583 | 0.925–62.172 | 0.0591 | 4.436 | 0.364–54.044 | 0.2428 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanabe, N.; Saeki, I.; Aibe, Y.; Matsuda, T.; Hanazono, T.; Nishi, M.; Hidaka, I.; Kuwashiro, S.; Shiratsuki, S.; Matsuura, K.; et al. Early Prediction of Response Focused on Tumor Markers in Atezolizumab plus Bevacizumab Therapy for Hepatocellular Carcinoma. Cancers 2023, 15, 2927. https://doi.org/10.3390/cancers15112927
Tanabe N, Saeki I, Aibe Y, Matsuda T, Hanazono T, Nishi M, Hidaka I, Kuwashiro S, Shiratsuki S, Matsuura K, et al. Early Prediction of Response Focused on Tumor Markers in Atezolizumab plus Bevacizumab Therapy for Hepatocellular Carcinoma. Cancers. 2023; 15(11):2927. https://doi.org/10.3390/cancers15112927
Chicago/Turabian StyleTanabe, Norikazu, Issei Saeki, Yuki Aibe, Takashi Matsuda, Tadasuke Hanazono, Maiko Nishi, Isao Hidaka, Shinya Kuwashiro, Shogo Shiratsuki, Keiji Matsuura, and et al. 2023. "Early Prediction of Response Focused on Tumor Markers in Atezolizumab plus Bevacizumab Therapy for Hepatocellular Carcinoma" Cancers 15, no. 11: 2927. https://doi.org/10.3390/cancers15112927
APA StyleTanabe, N., Saeki, I., Aibe, Y., Matsuda, T., Hanazono, T., Nishi, M., Hidaka, I., Kuwashiro, S., Shiratsuki, S., Matsuura, K., Egusa, M., Nishiyama, N., Fujioka, T., Kawamoto, D., Sasaki, R., Nishimura, T., Oono, T., Hisanaga, T., Matsumoto, T., ... Takami, T. (2023). Early Prediction of Response Focused on Tumor Markers in Atezolizumab plus Bevacizumab Therapy for Hepatocellular Carcinoma. Cancers, 15(11), 2927. https://doi.org/10.3390/cancers15112927







