Principles of Molecular Utility for CMS Classification in Colorectal Cancer Management
Abstract
Simple Summary
Abstract
1. Introduction
2. CRC Management Based on Staging Systems
2.1. TNM Staging, a Pathological Evaluation of CRC
2.2. Molecular Staging, Genetic and Epigenetic Characteristics of CRC
- (i)
- CRC development from benign to malignant lesions, induced by some key driver genes, acquires a series of mutations over time. Among the key driver genes that play role in carcinogenesis, the adenomatous polyposis coli (APC), accompanied by its mutations, regulates growth advantages in epithelial cells and results in the formation of a small adenoma. Later, the generation of mutations in KRAS and BRAF provides a second round of expansion for cells, involving transformation to a large adenoma. Finally, the occurrence of PIK3CA, SMAD4, and p53 mutations develops a malignant tumor that has the potential for invasion and metastasis. It remains unclear which mutations of these key driver genes are involved in the metastasis of CRC [15].
- (ii)
- MSI is caused by mutations in DNA mismatch repair genes (MLH1, MSH2, MSH6, and PMS2) and EPCAM. The occurrence of mutations in MLH1 or MSH2 genes leads to an increased risk (70–80%) of developing cancer, while mutations in the MSH6 or PMS2 genes have a comparatively lower risk (25–60%) of cancer development [16]. Nearly 15–20% of primary CRCs have the MSI phenotype, whereas the remainders are microsatellite stable (MSS). MSI tumors demonstrate multiple single nucleotide variants (SNVs) and insertion/deletions (indels). The five microsatellite markers were used as a standard panel to access the MSI status of cancer, including BAT26 and BAT25 as mononucleotide repeats, plus three dinucleotide repeats (D2S123, D5S346, and D17S250), as defined by the Bethesda Guidelines [17]. A subset of tumors with unstable loci in ≥30% markers are defined as “microsatellite high” (MSI-H), a subset of tumors with 10–29% unstable loci are classified as “microsatellite low” (MSI-L), and “microsatellite stable” (MSS) tumors are marked with no unstable markers [16]. In a study conducted by Mori et al. [18], a comprehensive genomic screening of microsatellite coding regions was performed, revealing the presence of mutations in nine loci (TGF-βR2, Bax, MSH3, ActRIIB, SEC63, AIM2, NADH–ubiquinone oxidoreductase, COBLL1, and EBP1) in over 20% of tumors. It has been observed that the presence of MSI-H in CRC is associated with superior anti-tumor immune response, inhibition of tumor cell growth, and an improved prognosis when compared to patients displaying MSI-L or MSS status. MSI status is a conceivable predictor for the treatment decision strategy method in MSI-H and MSI-L tumors. Furthermore, MSI tumors are more frequently located in the proximal colon, and present as more poorly differentiated cancers [19]. MSI is rarely found in polyps, except in Lynch syndrome, due to germline mutations in one of the MMR genes. MSI is the hallmark of HNPCC or Lynch syndrome and occurs in >95% of HNPCC cases [16].
- (iii)
- CIN nominated as the suppressor pathway phenotype is observed in 70–85% of CRC tumors and is often considered equal to MSS status [20]. CIN is induced by the occasional gain or loss of the whole chromosome during mitosis. Accordingly, CIN tumors are often aneuploid with structural or numerical aberrations. Furthermore, numerous significant events contribute to the development of the CIN, such as encompassing mutations in some oncogenes, such as APC, KRAS, TP53, CTNNB1, and PIK3CA, and loss of heterozygosity (LOH) chromosome in 18q with some of the tumor suppressor genes, such as SMAD2, SMAD4, and DCC, in the location. Traditionally, CRC develops through the adenoma to carcinoma pathway. APC gene mutation and inactivation are early events that are followed by the activation of KRAS as an oncogene due to mutation appearance in the adenomatous stage, followed by the inactivation of TP53 on chromosome 17p and the deletion of chromosome 18q, leading to metastatic carcinoma [21]. APC mutations are present at the preliminary stages of neoplasia and are majorly linked with the classic tubular adenoma pathway and CIN cancers [22].
- (iv)
- CIMP is an epigenetic event that has been observed to precede the onset of cancer. The process involves an increase in methylation levels within the promoter region, which can lead to the silencing of tumor-suppressor genes. Conversely, global hypomethylation has been linked to genomic instability and chromosomal abnormalities. In CRC, epigenetic instability manifests as hypermethylation of CpG islands, often in tandem with global DNA hypomethylation. In CIMP-positive CRC, promoter regions of tumor suppressor genes are frequently hypermethylated, resulting in loss-of-function in these genes.
2.3. Supervised Gene Expression Profiles for Prognosis Prediction of Early Stages CRC
- The Oncotype DX colon cancer assay (Genomic Health, Redwood City, CA, USA, http://www.genomichealth.com (accessed on 27 February 2023) predicts recurrence in stage II colon cancer patients after surgical resection [27,28]. Oncotype DX includes a 12-gene expression assay (7 cancer-related—BGN, C-MYC, FAP, GADD45B, INHBA, Ki-67, MYBL2—and 5 reference genes—ATP5E, GPX1, PGK1, UBB, VDAC2 [29]—based on reverse transcriptase-polymerase chain reaction (RT-PCR). It has been tested on archival formalin-fixed and paraffin-embedded (FFPE) tumor tissue specimens in the QUASAR trial [14].
- Coloprint (Agendia, Amsterdam, The Netherlands, http://www.agendia.com (accessed on 27 February 2023) is a test based on an 18-mRNA signature that predicts CRC relapse in the early stages of the disease. Furthermore, Coloprint uses whole-genome expression data analysis and has been validated in several independent cohorts. In addition, ColoPrint can predict the development of distant metastasis in stage II CRC patients and facilitates treatment strategy decisions for patients who may be safely managed without chemotherapy [30].
- A further prognostic gene expression microarray-based assay, ColDx, commercially administered as GeneFx Colon, was developed by Almac (Almac Group Ltd., Craigavon, UK) [31]. It is based on a 634-gene signature panel [32] and performed on FFPE tumor samples [33]. This assay differentiates stage II tumors into low- and high-risk for disease recurrence [14].
- CologuideEX (Oslo University Hospital, Oslo, Norway) stratifies CRC patients into high- and low-recurrence risk groups based on molecular markers. It contains a small panel of 13 genes (PIGR, CXCL13, MMP3, TUBA1B, SESN1, AZGP1, KLK6, EPHA7, SEMA3A, DSC3, CXCL10, ENPP3, and BNIP3) optimally combined for robust risk stratification of CRC stage II patients using a consecutive Norwegian test series [34] by Affymetrix exon-based microarrays (Affymetrix, Santa Clara, CA, USA). The test was performed on fresh-frozen samples [35].
- The OncoDefender-CRC test investigates the expression profiles of 5 genes (BMI1, ETV6, H3F3B, RPS10, and VEGFA) on archival FFPE tumor tissue by RT-PCR using the custom 384-well TaqMan low-density arrays. This dichotomous 5-gene prognostic signature is able to differentiate between patients with lymph node-negative, invasive CRCs at “high risk” from those at “low risk” of recurrence within 3 years after curative resection [36].
- The ColoGuidePro was also created at Oslo University Hospital (Norway) to predict good or poor prognosis in stages II and III of CRC patients. This assay includes a panel of seven genes, and it is based on Affymetrix exon-based microarrays to determine the expression signature of fresh-frozen tissue samples [37].
| Assay | Company | Gene Signature | Specimen Used | Technique for GEP | Actual Status | Refs. |
|---|---|---|---|---|---|---|
| ColoPrint colon cancer recurrence assay | Agendia, Inc. | 18-gene expression profile | Fresh tissue or fresh, frozen tissue | Agendia customized whole-genome high-density microarrays | Not FDA approved | [38,39,40] |
| GeneFx Colon | Licensed by Precision Therapeutics (originally developed by Almac Diagnostics as the ColDX assay) | 634 probe-set signatures | Formalin-fixed paraffin-embedded tissue | Amplified product hybridized to Almac Colorectal Cancer DSA on Affymetrix 7G scanner | Not FDA approved | [32] |
| OncoDefender-CRC (colon and rectal cancer) | Everist Genomics | 5 genes | Formalin-fixed paraffin-embedded tissue | TaqMan Array | Not FDA approved | [36] |
| Oncotype DX colon cancer assay | Genomic Health, Inc. | 12 genes (7 prognostics and 5 reference genes) | Formalin-fixed paraffin-embedded tissue | Reverse transcription-quantitative PCR (RT-qPCR) | Not FDA approved | [27,28,29] |
| ColoGuideEx | Oslo University Hospital, Norway | 13 genes | Fresh, frozen biopsies | Exon-based microarray | Unknown status | [34] |
| ColoGuidePro (Derived from ColoGuideEx) | Oslo University Hospital, Norway | 7 genes | Fresh, frozen biopsies | Exon-based microarray | Unknown status | [37] |
2.4. The Consensus Molecular Subtyping as a Transcriptome-Based Staging
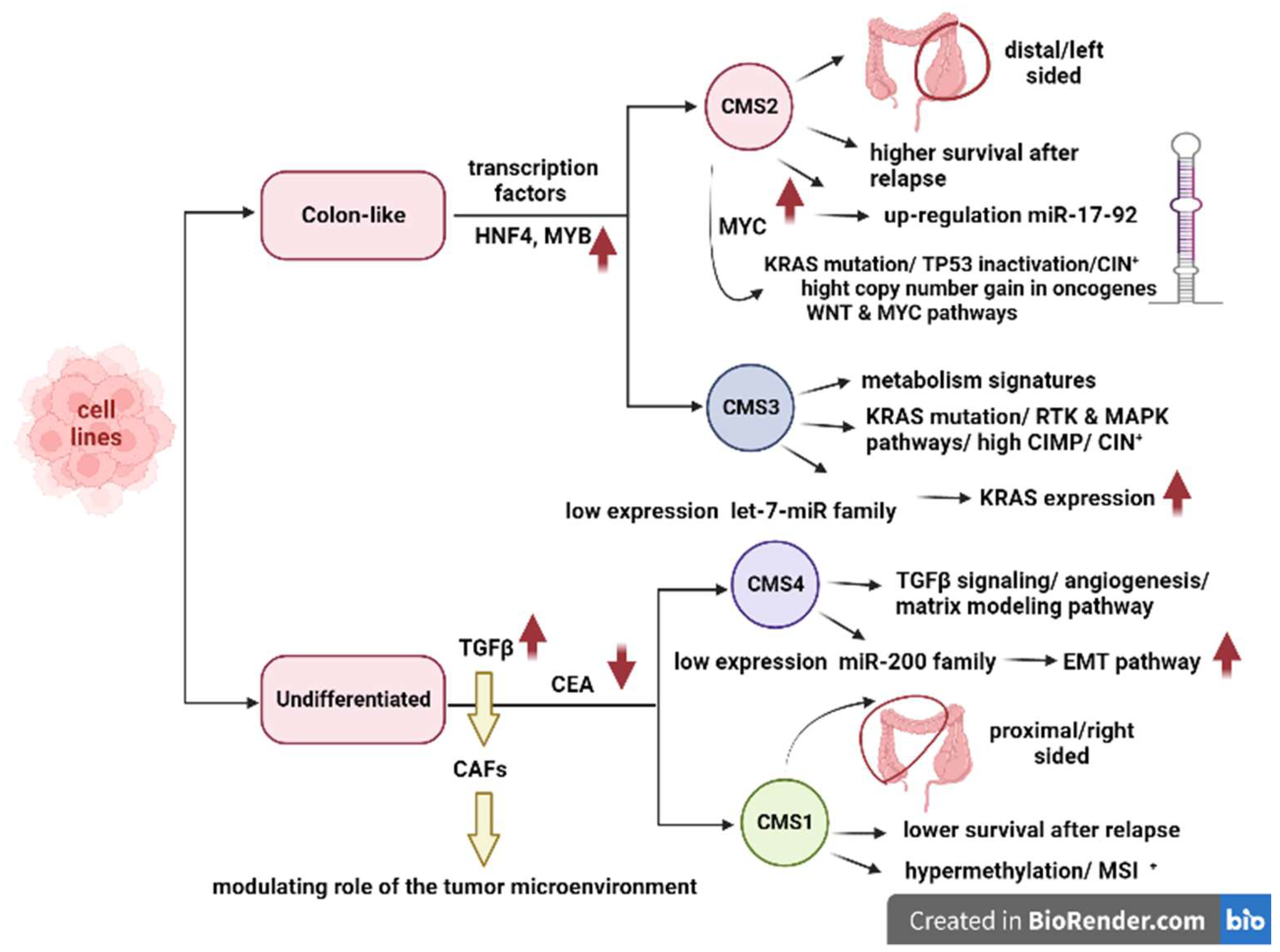
3. CMS Classification and Regulatory Networks
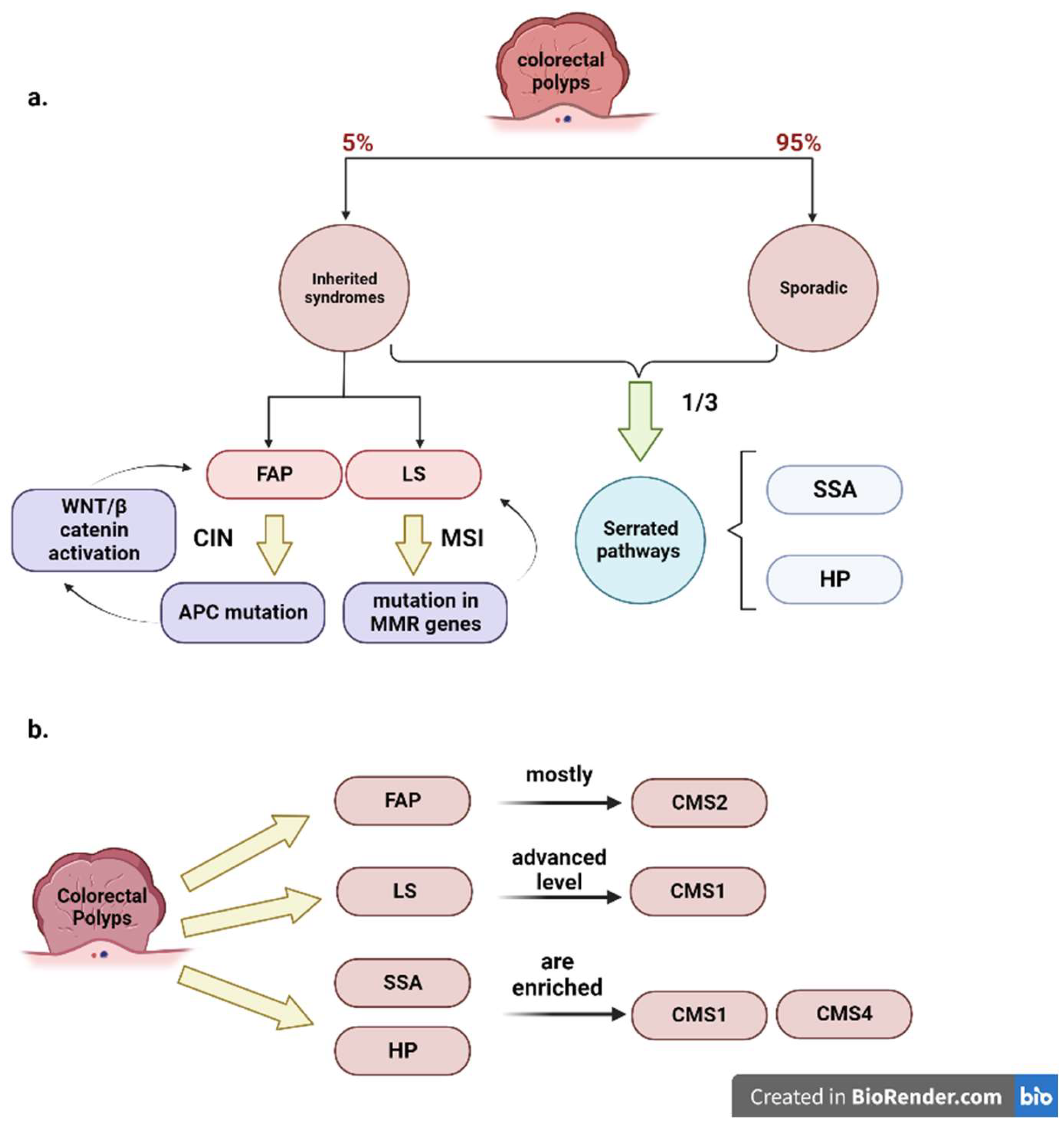
4. CMS and Polyps
5. Role of CMS in the Prediction of CRC Prognosis
6. In Vitro and In Vivo CMS-Based Studies for Tailoring Treatments in CRC
7. Role of CMS in the Prediction of Drug Response in CRC
8. CMS and Immunoscore
9. CMS and Immunotherapy
10. CMS and Gut Microbiome
11. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Goding Sauer, A.; Fedewa, S.A.; Butterly, L.F.; Anderson, J.C.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Luo, D.; Cai, S.; Li, Q.; Li, X. Real-World Implications of Nonbiological Factors with Staging, Prognosis and Clinical Management in Colon Cancer. Cancers 2018, 10, 263. [Google Scholar] [CrossRef]
- Benson, A.B. 2023 NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Colon Cancer Version 3.2022–January 25, 2023. J. Natl. Compr. Cancer Netw. 2023. Available online: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1428 (accessed on 27 February 2023).
- Vogelstein, B.; Fearon, E.R.; Hamilton, S.R.; Kern, S.E.; Preisinger, A.C.; Leppert, M.; Nakamura, Y.; White, R.; Smits, A.M.; Bos, J.L. Genetic alterations during colorectal-tumor development. N. Engl. J. Med. 1988, 319, 525–532. [Google Scholar] [CrossRef]
- Weiser, M.R. AJCC 8th Edition: Colorectal Cancer. Ann. Surg. Oncol. 2018, 25, 1454–1455. [Google Scholar] [CrossRef] [PubMed]
- Purcell, R.V.; Schmeier, S.; Lau, Y.C.; Pearson, J.F.; Frizelle, F.A. Molecular subtyping improves prognostication of Stage 2 colorectal cancer. BMC Cancer 2019, 19, 1155. [Google Scholar] [CrossRef]
- Rosen, R.D.; Sapra, A. TNM Classification. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2022. [Google Scholar]
- Lea, D.; Håland, S.; Hagland, H.R.; Søreide, K. Accuracy of TNM staging in colorectal cancer: A review of current culprits, the modern role of morphology and stepping-stones for improvements in the molecular era. Scand. J. Gastroenterol. 2014, 49, 1153–1163. [Google Scholar] [CrossRef]
- Wang, W.; Kandimalla, R.; Huang, H.; Zhu, L.; Li, Y.; Gao, F.; Goel, A.; Wang, X. Molecular subtyping of colorectal cancer: Recent progress, new challenges and emerging opportunities. Semin. Cancer Biol. 2019, 55, 37–52. [Google Scholar] [CrossRef]
- Soldevilla, B.; Carretero-Puche, C.; Gomez-Lopez, G.; Al-Shahrour, F.; Riesco, M.C.; Gil-Calderon, B.; Alvarez-Vallina, L.; Espinosa-Olarte, P.; Gomez-Esteves, G.; Rubio-Cuesta, B.; et al. The correlation between immune subtypes and consensus molecular subtypes in colorectal cancer identifies novel tumour microenvironment profiles, with prognostic and therapeutic implications. Eur. J. Cancer 2019, 123, 118–129. [Google Scholar] [CrossRef]
- Vivas, C.S.; Sanz-Pamplona, R.; Grasselli, J.; Mulet-Margalef, N.; Soler, R.S. Are Gene Signatures Ready for Use in the Selection of Patients for Adjuvant Treatment? Curr. Color. Cancer Rep. 2016, 12, 18–26. [Google Scholar] [CrossRef]
- Qian, Y.; Daza, J.; Itzel, T.; Betge, J.; Zhan, T.; Marmé, F.; Teufel, A. Prognostic cancer gene expression signatures: Current status and challenges. Cells 2021, 10, 648. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Sun, W.; Zhou, Y.; Li, P.; Chen, F.; Chen, H.; Xia, D.; Xu, E.; Lai, M.; Wu, Y. Mutations of key driver genes in colorectal cancer progression and metastasis. Cancer Metastasis Rev. 2018, 37, 173–187. [Google Scholar] [CrossRef]
- Malki, A.; ElRuz, R.A.; Gupta, I.; Allouch, A.; Vranic, S.; Al Moustafa, A.E. Molecular Mechanisms of Colon Cancer Progression and Metastasis: Recent Insights and Advancements. Int. J. Mol. Sci. 2020, 22, 130. [Google Scholar] [CrossRef] [PubMed]
- Boland, C.R.; Thibodeau, S.N.; Hamilton, S.R.; Sidransky, D.; Eshleman, J.R.; Burt, R.W.; Meltzer, S.J.; Rodriguez-Bigas, M.A.; Fodde, R.; Ranzani, G.N.; et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: Development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998, 58, 5248–5257. [Google Scholar] [PubMed]
- Mori, Y.; Yin, J.; Rashid, A.; Leggett, B.A.; Young, J.; Simms, L.; Kuehl, P.M.; Langenberg, P.; Meltzer, S.J.; Stine, O.C. Instabilotyping: Comprehensive identification of frameshift mutations caused by coding region microsatellite instability. Cancer Res. 2001, 61, 6046–6049. [Google Scholar]
- Kang, S.; Na, Y.; Joung, S.Y.; Lee, S.I.; Oh, S.C.; Min, B.W. The significance of microsatellite instability in colorectal cancer after controlling for clinicopathological factors. Medicine. 2018, 97, e0019. [Google Scholar] [CrossRef]
- Requena, D.O.; Garcia-Buitrago, M. Molecular Insights Into Colorectal Carcinoma. Arch. Med. Res. 2020, 51, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, R.; Singh, J.K.; Wunnava, A.; Al-Obeed, O.; Abdulla, M.; Srivastava, S.K. Emerging trends in colorectal cancer: Dysregulated signaling pathways (Review). Int. J. Mol. Med. 2021, 47, 1. [Google Scholar] [CrossRef]
- Zhang, Z.H.; Jhaveri, D.J.; Marshall, V.M.; Bauer, D.C.; Edson, J.; Narayanan, R.K.; Robinson, G.J.; Lundberg, A.E.; Bartlett, P.F.; Wray, N.R.; et al. A Comparative Study of Techniques for Differential Expression Analysis on RNA-Seq Data. PLoS ONE 2014, 9, e103207. [Google Scholar] [CrossRef]
- Toyota, M.; Ahuja, N.; Ohe-Toyota, M.; Herman, J.G.; Baylin, S.B.; Issa, J.-P.J. CpG island methylator phenotype in colorectal cancer. Proc. Natl. Acad. Sci. USA 1999, 96, 8681–8686. [Google Scholar] [CrossRef]
- Zong, L.; Abe, M.; Ji, J.; Zhu, W.G.; Yu, D. Tracking the Correlation Between CpG Island Methylator Phenotype and Other Molecular Features and Clinicopathological Features in Human Colorectal Cancers: A Systematic Review and Meta-Analysis. Clin. Transl. Gastroenterol. 2016, 7, e151. [Google Scholar] [CrossRef] [PubMed]
- Advani, S.M.; Advani, P.; DeSantis, S.M.; Brown, D.; VonVille, H.M.; Lam, M.; Loree, J.M.; Mehrvarz Sarshekeh, A.; Bressler, J.; Lopez, D.S.; et al. Clinical, Pathological, and Molecular Characteristics of CpG Island Methylator Phenotype in Colorectal Cancer: A Systematic Review and Meta-analysis. Transl. Oncol. 2018, 11, 1188–1201. [Google Scholar] [CrossRef]
- Russell, M.C.; Chang, G.J. Molecular profiling for stage II colon cancer. Color. Cancer 2012, 1, 479–490. [Google Scholar] [CrossRef]
- Marisa, L.; de Reyniès, A.; Duval, A.; Selves, J.; Gaub, M.P.; Vescovo, L.; Etienne-Grimaldi, M.C.; Schiappa, R.; Guenot, D.; Ayadi, M.; et al. Gene expression classification of colon cancer into molecular subtypes: Characterization, validation, and prognostic value. PLoS Med. 2013, 10, e1001453. [Google Scholar] [CrossRef]
- Clark-Langone, K.M.; Sangli, C.; Krishnakumar, J.; Watson, D. Translating tumor biology into personalized treatment planning: Analytical performance characteristics of the Oncotype DX®Colon Cancer Assay. BMC Cancer 2010, 10, 691. [Google Scholar] [CrossRef] [PubMed]
- Yau, T.O. Precision treatment in colorectal cancer: Now and the future. JGH Open 2019, 3, 361–369. [Google Scholar] [CrossRef]
- Maak, M.; Simon, I.; Nitsche, U.; Roepman, P.; Snel, M.; Glas, A.M.; Schuster, T.; Keller, G.; Zeestraten, E.; Goossens, I. Independent validation of a prognostic genomic signature (ColoPrint) for patients with stage II colon cancer. Ann. Surg. 2013, 257, 1053–1058. [Google Scholar] [CrossRef]
- Sharif, S.; O’Connell, M.J. Gene signatures in stage II colon cancer: A clinical review. Curr. Color. Cancer Rep. 2012, 8, 225–231. [Google Scholar] [CrossRef]
- Fang, S.H.; Efron, J.E.; Berho, M.E.; Wexner, S.D. Dilemma of stage II colon cancer and decision making for adjuvant chemotherapy. J. Am. Coll. Surg. 2014, 219, 1056–1069. [Google Scholar] [CrossRef]
- Graham, D.M.; Coyle, V.M.; Kennedy, R.D.; Wilson, R.H. Molecular subtypes and personalized therapy in metastatic colorectal cancer. Curr. Color. Cancer Rep. 2016, 12, 141–150. [Google Scholar] [CrossRef]
- Ågesen, T.H.; Sveen, A.; Merok, M.A.; Lind, G.E.; Nesbakken, A.; Skotheim, R.I.; Lothe, R.A. ColoGuideEx: A robust gene classifier specific for stage II colorectal cancer prognosis. Gut 2012, 61, 1560–1567. [Google Scholar] [CrossRef]
- Lopez, N.E.; Weiss, A.C.; Robles, J.; Fanta, P.; Ramamoorthy, S.L. A systematic review of clinically available gene expression profiling assays for stage II colorectal cancer: Initial steps toward genetic staging. Am. J. Surg. 2016, 212, 700–714. [Google Scholar] [CrossRef]
- Lenehan, P.F.; Boardman, L.A.; Riegert-Johnson, D.; De Petris, G.; Fry, D.W.; Ohrnberger, J.; Heyman, E.R.; Gerard, B.; Almal, A.A.; Worzel, W.P. Generation and external validation of a tumor-derived 5-gene prognostic signature for recurrence of lymph node-negative, invasive colorectal carcinoma. Cancer 2012, 118, 5234–5244. [Google Scholar] [CrossRef] [PubMed]
- Sveen, A.; Ågesen, T.H.; Nesbakken, A.; Meling, G.I.; Rognum, T.O.; Liestøl, K.; Skotheim, R.I.; Lothe, R.A. ColoGuidePro: A Prognostic 7-Gene Expression Signature for Stage III Colorectal Cancer PatientsPrognostic Gene Expression Classifier of Colorectal Cancer. Clin. Cancer Res. 2012, 18, 6001–6010. [Google Scholar] [CrossRef]
- Salazar, R.; Roepman, P.; Capella, G.; Moreno, V.; Simon, I.; Dreezen, C.; Lopez-Doriga, A.; Santos, C.; Marijnen, C.; Westerga, J. Gene expression signature to improve prognosis prediction of stage II and III colorectal cancer. J. Clin. Oncol. 2011, 29, 17–24. [Google Scholar] [CrossRef]
- Tan, I.B.; Tan, P. An 18-gene signature (ColoPrint®) for colon cancer prognosis. Nat. Rev. Clin. Oncol. 2011, 8, 131–133. [Google Scholar] [CrossRef] [PubMed]
- Kopetz, S.; Tabernero, J.; Rosenberg, R.; Jiang, Z.-Q.; Moreno, V.; Bachleitner-Hofmann, T.; Lanza, G.; Stork-Sloots, L.; Maru, D.; Simon, I. Genomic classifier ColoPrint predicts recurrence in stage II colorectal cancer patients more accurately than clinical factors. Oncol. 2015, 20, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Guinney, J.; Dienstmann, R.; Wang, X.; de Reyniès, A.; Schlicker, A.; Soneson, C.; Marisa, L.; Roepman, P.; Nyamundanda, G.; Angelino, P.; et al. The consensus molecular subtypes of colorectal cancer. Nat. Med. 2015, 21, 1350–1356. [Google Scholar] [CrossRef]
- Llosa, N.J.; Cruise, M.; Tam, A.; Wicks, E.C.; Hechenbleikner, E.M.; Taube, J.M.; Blosser, R.L.; Fan, H.; Wang, H.; Luber, B.S. The Vigorous Immune Microenvironment of Microsatellite Instable Colon Cancer Is Balanced by Multiple Counter-Inhibitory CheckpointsImmune Checkpoints in Human Colorectal Cancer. Cancer Discov. 2015, 5, 43–51. [Google Scholar] [CrossRef]
- Anitei, M.-G.; Zeitoun, G.; Mlecnik, B.; Marliot, F.; Haicheur, N.; Todosi, A.-M.; Kirilovsky, A.; Lagorce, C.; Bindea, G.; Ferariu, D. Prognostic and predictive values of the immunoscore in patients with rectal cancer. Clin. Cancer Res. 2014, 20, 1891–1899. [Google Scholar] [CrossRef] [PubMed]
- Eide, P.W.; Bruun, J.; Lothe, R.A.; Sveen, A. CMScaller: An R package for consensus molecular subtyping of colorectal cancer pre-clinical models. Sci. Rep. 2017, 7, 16618. [Google Scholar] [CrossRef]
- Mooi, J.K.; Wirapati, P.; Asher, R.; Lee, C.K.; Savas, P.; Price, T.J.; Townsend, A.; Hardingham, J.; Buchanan, D.; Williams, D.; et al. The prognostic impact of consensus molecular subtypes (CMS) and its predictive effects for bevacizumab benefit in metastatic colorectal cancer: Molecular analysis of the AGITG MAX clinical trial. Ann. Oncol. 2018, 29, 2240–2246. [Google Scholar] [CrossRef]
- Haasnoot, K.J.C.; Backes, Y.; Moons, L.M.G.; Kranenburg, O.; Trinh, A.; Vermeulen, L.; Noë, M.; Tuynman, J.B.; van Lent, A.U.G.; van Ginneken, R.; et al. Associations of non-pedunculated T1 colorectal adenocarcinoma outcome with consensus molecular subtypes, immunoscore, and microsatellite status: A multicenter case-cohort study. Mod. Pathol. 2020, 33, 2626–2636. [Google Scholar] [CrossRef]
- Ubink, I.; van Eden, W.J.; Snaebjornsson, P.; Kok, N.F.M.; van Kuik, J.; van Grevenstein, W.M.U.; Laclé, M.M.; Sanders, J.; Fijneman, R.J.A.; Elias, S.G.; et al. Histopathological and molecular classification of colorectal cancer and corresponding peritoneal metastases. Br. J. Surg. 2018, 105, e204–e211. [Google Scholar] [CrossRef] [PubMed]
- Rajamäki, K.; Taira, A.; Katainen, R.; Välimäki, N.; Kuosmanen, A.; Plaketti, R.M.; Seppälä, T.T.; Ahtiainen, M.; Wirta, E.V.; Vartiainen, E.; et al. Genetic and Epigenetic Characteristics of Inflammatory Bowel Disease-Associated Colorectal Cancer. Gastroenterology 2021, 161, 592–607. [Google Scholar] [CrossRef]
- Müller, M.F.; Ibrahim, A.E.; Arends, M.J. Molecular pathological classification of colorectal cancer. Virchows Arch. 2016, 469, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Fessler, E.; Jansen, M.; De Sousa, E.M.F.; Zhao, L.; Prasetyanti, P.R.; Rodermond, H.; Kandimalla, R.; Linnekamp, J.F.; Franitza, M.; van Hooff, S.R.; et al. A multidimensional network approach reveals microRNAs as determinants of the mesenchymal colorectal cancer subtype. Oncogene 2016, 35, 6026–6037. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Choi, P.; Casey, S.C.; Dill, D.L.; Felsher, D.W. MYC through miR-17-92 Suppresses Specific Target Genes to Maintain Survival, Autonomous Proliferation, and a Neoplastic State. Cancer Cell. 2014, 26, 262–272. [Google Scholar] [CrossRef]
- Paz-Cabezas, M.; Calvo-López, T.; Romera-Lopez, A.; Tabas-Madrid, D.; Ogando, J.; Fernández-Aceñero, M.J.; Sastre, J.; Pascual-Montano, A.; Mañes, S.; Díaz-Rubio, E.; et al. Molecular Classification of Colorectal Cancer by microRNA Profiling: Correlation with the Consensus Molecular Subtypes (CMS) and Validation of miR-30b Targets. Cancers 2022, 14, 5175. [Google Scholar] [CrossRef]
- Stoffel, E.M.; Murphy, C.C. Epidemiology and mechanisms of the increasing incidence of colon and rectal cancers in young adults. Gastroenterology 2020, 158, 341–353. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.; Willis, J.A.; Reumers, J.; Taggart, M.W.; San Lucas, F.A.; Thirumurthi, S.; Kanth, P.; Delker, D.A.; Hagedorn, C.H.; Lynch, P.M.; et al. Colorectal premalignancy is associated with consensus molecular subtypes 1 and 2. Ann. Oncol. 2018, 29, 2061–2067. [Google Scholar] [CrossRef] [PubMed]
- Fearon, E.R. Molecular genetics of colorectal cancer. Annu. Rev. Pathol. 2011, 6, 479–507. [Google Scholar] [CrossRef] [PubMed]
- Fessler, E.; Drost, J.; van Hooff, S.R.; Linnekamp, J.F.; Wang, X.; Jansen, M.; De Sousa, E.M.F.; Prasetyanti, P.R.; JE, I.J.; Franitza, M.; et al. TGFβ signaling directs serrated adenomas to the mesenchymal colorectal cancer subtype. EMBO Mol. Med. 2016, 8, 745–760. [Google Scholar] [CrossRef]
- Komor, M.A.; Bosch, L.J.; Bounova, G.; Bolijn, A.S.; Delis-van Diemen, P.M.; Rausch, C.; Hoogstrate, Y.; Stubbs, A.P.; de Jong, M.; Jenster, G.; et al. Consensus molecular subtype classification of colorectal adenomas. J. Pathol. 2018, 246, 266–276. [Google Scholar] [CrossRef]
- Lenz, H.J.; Argiles, G.; Yoshino, T.; Tejpar, S.; Ciardiello, F.; Braunger, J.; Salnikov, A.V.; Gabrielyan, O.; Schmid, R.; Höfler, J.; et al. Association of Consensus Molecular Subtypes and Molecular Markers with Clinical Outcomes in Patients with Metastatic Colorectal Cancer: Biomarker Analyses From LUME-Colon 1. Clin. Color. Cancer 2021, 20, 84–95.e8. [Google Scholar] [CrossRef]
- Li, Y.; Mo, S.; Zhang, L.; Ma, X.; Hu, X.; Huang, D.; Lu, B.; Luo, C.; Peng, H.; Cai, S.; et al. Postoperative circulating tumor DNA combined with consensus molecular subtypes can better predict outcomes in stage III colon cancers: A prospective cohort study. Eur. J. Cancer 2022, 169, 198–209. [Google Scholar] [CrossRef]
- Tarazona, N.; Gimeno-Valiente, F.; Gambardella, V.; Huerta, M.; Roselló, S.; Zuniga, S.; Calon, A.; Carbonell-Asins, J.A.; Fontana, E.; Martinez-Ciarpaglini, C.; et al. Detection of postoperative plasma circulating tumour DNA and lack of CDX2 expression as markers of recurrence in patients with localised colon cancer. ESMO Open. 2020, 5, e000847. [Google Scholar] [CrossRef]
- Becht, E.; de Reyniès, A.; Giraldo, N.A.; Pilati, C.; Buttard, B.; Lacroix, L.; Selves, J.; Sautès-Fridman, C.; Laurent-Puig, P.; Fridman, W.H. Immune and Stromal Classification of Colorectal Cancer Is Associated with Molecular Subtypes and Relevant for Precision Immunotherapy. Clin. Cancer Res. 2016, 22, 4057–4066. [Google Scholar] [CrossRef]
- Bonaventura, P.; Shekarian, T.; Alcazer, V.; Valladeau-Guilemond, J.; Valsesia-Wittmann, S.; Amigorena, S.; Caux, C.; Depil, S. Cold tumors: A therapeutic challenge for immunotherapy. Front. Immunol. 2019, 10, 168. [Google Scholar] [CrossRef]
- Smeby, J.; Sveen, A.; Merok, M.A.; Danielsen, S.A.; Eilertsen, I.A.; Guren, M.; Dienstmann, R.; Nesbakken, A.; Lothe, R.A. CMS-dependent prognostic impact of KRAS and BRAFV600E mutations in primary colorectal cancer. Ann. Oncol. 2018, 29, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Li, L.; Xu, R. Association of Epigenetic Clock with Consensus Molecular Subtypes and Overall Survival of Colorectal Cancer. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1720–1724. [Google Scholar] [CrossRef] [PubMed]
- Linnekamp, J.F.; Hooff, S.R.v.; Prasetyanti, P.R.; Kandimalla, R.; Buikhuisen, J.Y.; Fessler, E.; Ramesh, P.; Lee, K.A.S.T.; Bochove, G.G.W.; de Jong, J.H.; et al. Consensus molecular subtypes of colorectal cancer are recapitulated in in vitro and in vivo models. Cell. Death Differ. 2018, 25, 616–633. [Google Scholar] [CrossRef]
- Berg, K.C.G.; Eide, P.W.; Eilertsen, I.A.; Johannessen, B.; Bruun, J.; Danielsen, S.A.; Bjørnslett, M.; Meza-Zepeda, L.A.; Eknæs, M.; Lind, G.E.; et al. Multi-omics of 34 colorectal cancer cell lines - a resource for biomedical studies. Mol. Cancer 2017, 16, 116. [Google Scholar] [CrossRef]
- Ludwig, N.; Leidinger, P.; Becker, K.; Backes, C.; Fehlmann, T.; Pallasch, C.; Rheinheimer, S.; Meder, B.; Stähler, C.; Meese, E.; et al. Distribution of miRNA expression across human tissues. Nucleic Acids Res. 2016, 44, 3865–3877. [Google Scholar] [CrossRef]
- Calon, A.; Lonardo, E.; Berenguer-Llergo, A.; Espinet, E.; Hernando-Momblona, X.; Iglesias, M.; Sevillano, M.; Palomo-Ponce, S.; Tauriello, D.V.F.; Byrom, D.; et al. Stromal gene expression defines poor-prognosis subtypes in colorectal cancer. Nat. Genet. 2015, 47, 320–329. [Google Scholar] [CrossRef]
- Mo, S.; Tang, P.; Luo, W.; Zhang, L.; Li, Y.; Hu, X.; Ma, X.; Chen, Y.; Bao, Y.; He, X.; et al. Patient-Derived Organoids from Colorectal Cancer with Paired Liver Metastasis Reveal Tumor Heterogeneity and Predict Response to Chemotherapy. Adv. Sci. 2022, 9, 2204097. [Google Scholar] [CrossRef] [PubMed]
- Laoukili, J.; Constantinides, A.; Wassenaar, E.C.E.; Elias, S.G.; Raats, D.A.E.; van Schelven, S.J.; van Wettum, J.; Volckmann, R.; Koster, J.; Huitema, A.D.R.; et al. Peritoneal metastases from colorectal cancer belong to Consensus Molecular Subtype 4 and are sensitised to oxaliplatin by inhibiting reducing capacity. Br. J. Cancer 2022, 126, 1824–1833. [Google Scholar] [CrossRef] [PubMed]
- Michels, B.E.; Mosa, M.H.; Grebbin, B.M.; Yepes, D.; Darvishi, T.; Hausmann, J.; Urlaub, H.; Zeuzem, S.; Kvasnicka, H.M.; Oellerich, T.; et al. Human colon organoids reveal distinct physiologic and oncogenic Wnt responses. J. Exp. Med. 2019, 216, 704–720. [Google Scholar] [CrossRef] [PubMed]
- Mazzeschi, M.; Sgarzi, M.; Romaniello, D.; Gelfo, V.; Cavallo, C.; Ambrosi, F.; Morselli, A.; Miano, C.; Laprovitera, N.; Girone, C.; et al. The autocrine loop of ALK receptor and ALKAL2 ligand is an actionable target in consensus molecular subtype 1 colon cancer. J. Exp. Clin. Cancer Res. 2022, 41, 113. [Google Scholar] [CrossRef]
- Ramzy, G.M.; Koessler, T.; Ducrey, E.; McKee, T.; Ris, F.; Buchs, N.; Rubbia-Brandt, L.; Dietrich, P.-Y.; Nowak-Sliwinska, P. Patient-Derived In Vitro Models for Drug Discovery in Colorectal Carcinoma. Cancers 2020, 12, 1423. [Google Scholar] [CrossRef]
- Brown, K.M.; Xue, A.; Mittal, A.; Samra, J.S.; Smith, R.; Hugh, T.J. Patient-derived xenograft models of colorectal cancer in pre-clinical research: A systematic review. Oncotarget 2016, 7, 66212–66225. [Google Scholar] [CrossRef] [PubMed]
- Isella, C.; Brundu, F.; Bellomo, S.E.; Galimi, F.; Zanella, E.; Porporato, R.; Petti, C.; Fiori, A.; Orzan, F.; Senetta, R.; et al. Selective analysis of cancer-cell intrinsic transcriptional traits defines novel clinically relevant subtypes of colorectal cancer. Nat. Commun. 2017, 8, 15107. [Google Scholar] [CrossRef]
- Buikhuisen, J.Y.; Torang, A.; Medema, J.P. Exploring and modelling colon cancer inter-tumour heterogeneity: Opportunities and challenges. Oncogenesis 2020, 9, 66. [Google Scholar] [CrossRef]
- Aparicio, J.; Esposito, F.; Serrano, S.; Falco, E.; Escudero, P.; Ruiz-Casado, A.; Manzano, H.; Fernandez-Montes, A. Metastatic colorectal cancer. First line therapy for unresectable disease. J. Clin. Med. 2020, 9, 3889. [Google Scholar] [CrossRef] [PubMed]
- Okita, A.; Takahashi, S.; Ouchi, K.; Inoue, M.; Watanabe, M.; Endo, M.; Honda, H.; Yamada, Y.; Ishioka, C. Consensus molecular subtypes classification of colorectal cancer as a predictive factor for chemotherapeutic efficacy against metastatic colorectal cancer. Oncotarget 2018, 9, 18698–18711. [Google Scholar] [CrossRef] [PubMed]
- Ragulan, C.; Eason, K.; Fontana, E.; Nyamundanda, G.; Tarazona, N.; Patil, Y.; Poudel, P.; Lawlor, R.T.; Del Rio, M.; Koo, S.-L. Analytical validation of multiplex biomarker assay to stratify colorectal cancer into molecular subtypes. Sci. Rep. 2019, 9, 7665. [Google Scholar] [CrossRef]
- Van Cutsem, E.; Cervantes, A.; Adam, R.; Sobrero, A.; Van Krieken, J.; Aderka, D.; Aguilar, E.A.; Bardelli, A.; Benson, A.; Bodoky, G. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann. Oncol. 2016, 27, 1386–1422. [Google Scholar] [CrossRef] [PubMed]
- Gómez-España, M.; Gallego, J.; González-Flores, E.; Maurel, J.; Páez, D.; Sastre, J.; Aparicio, J.; Benavides, M.; Feliu, J.; Vera, R. SEOM clinical guidelines for diagnosis and treatment of metastatic colorectal cancer (2018). Clin. Transl. Oncol. 2019, 21, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Martini, G.; Dienstmann, R.; Ros, J.; Baraibar, I.; Cuadra-Urteaga, J.L.; Salva, F.; Ciardiello, D.; Mulet, N.; Argiles, G.; Tabernero, J.; et al. Molecular subtypes and the evolution of treatment management in metastatic colorectal cancer. Adv. Med. Oncol. 2020, 12, 1758835920936089. [Google Scholar] [CrossRef]
- Dienstmann, R.; Villacampa, G.; Sveen, A.; Mason, M.J.; Niedzwiecki, D.; Nesbakken, A.; Moreno, V.; Warren, R.S.; Lothe, R.A.; Guinney, J. Relative contribution of clinicopathological variables, genomic markers, transcriptomic subtyping and microenvironment features for outcome prediction in stage II/III colorectal cancer. Ann. Oncol. 2019, 30, 1622–1629. [Google Scholar] [CrossRef] [PubMed]
- Duschinsky, R.; Pleven, E.; Heidelberger, C. The synthesis of 5-fluoropyrimidines. J. Am. Chem. Soc. 1957, 79, 4559–4560. [Google Scholar] [CrossRef]
- Gustavsson, B.; Carlsson, G.; Machover, D.; Petrelli, N.; Roth, A.; Schmoll, H.-J.; Tveit, K.-M.; Gibson, F. A review of the evolution of systemic chemotherapy in the management of colorectal cancer. Clin. Color. Cancer 2015, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Stintzing, S.; Wirapati, P.; Lenz, H.J.; Neureiter, D.; Fischer von Weikersthal, L.; Decker, T.; Kiani, A.; Kaiser, F.; Al-Batran, S.; Heintges, T.; et al. Consensus molecular subgroups (CMS) of colorectal cancer (CRC) and first-line efficacy of FOLFIRI plus cetuximab or bevacizumab in the FIRE3 (AIO KRK-0306) trial. Ann. Oncol. 2019, 30, 1796–1803. [Google Scholar] [CrossRef]
- Lenz, H.-J.; Ou, F.-S.; Venook, A.; Hochster, H.; Niedzwiecki, D.; Goldberg, R.; Mayer, R.; Bertagnolli, M.; Blanke, C.; Zemla, T.; et al. Impact of consensus molecular subtyping (CMS) on overall survival (OS) and progression free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): Analysis of CALGB/SWOG 80405 (Alliance). J. Clin. Oncol. 2017, 35, 3511. [Google Scholar] [CrossRef]
- Song, N.; Pogue-Geile, K.L.; Gavin, P.G.; Yothers, G.; Kim, S.R.; Johnson, N.L.; Lipchik, C.; Allegra, C.J.; Petrelli, N.J.; O’Connell, M.J.; et al. Clinical Outcome From Oxaliplatin Treatment in Stage II/III Colon Cancer According to Intrinsic Subtypes: Secondary Analysis of NSABP C-07/NRG Oncology Randomized Clinical Trial. JAMA Oncol. 2016, 2, 1162–1169. [Google Scholar] [CrossRef]
- Del Rio, M.; Mollevi, C.; Bibeau, F.; Vie, N.; Selves, J.; Emile, J.F.; Roger, P.; Gongora, C.; Robert, J.; Tubiana-Mathieu, N.; et al. Molecular subtypes of metastatic colorectal cancer are associated with patient response to irinotecan-based therapies. Eur. J. Cancer 2017, 76, 68–75. [Google Scholar] [CrossRef]
- Tebbutt, N.C.; Wilson, K.; Gebski, V.J.; Cummins, M.M.; Zannino, D.; van Hazel, G.A.; Robinson, B.; Broad, A.; Ganju, V.; Ackland, S.P.; et al. Capecitabine, bevacizumab, and mitomycin in first-line treatment of metastatic colorectal cancer: Results of the Australasian Gastrointestinal Trials Group Randomized Phase III MAX Study. J. Clin. Oncol. 2010, 28, 3191–3198. [Google Scholar] [CrossRef]
- Roepman, P.; Tabernero, J.; Schlicker, A.; Majewski, I.; Tian, S.; Moreno, V.; Snel, M.H.; Chresta, C.M.; Rosenberg, R.; Nitsche, U.; et al. Colorectal cancer intrinsic subtypes predict chemotherapy benefit, deficient mismatch repair and epithelial-to-mesenchymal transition. Int. J. Cancer 2014, 134, 552–562. [Google Scholar] [CrossRef]
- De Sousa, E.M.F.; Jansen, M.; Wang, X.; Fessler, E.; Trinh, A.; De Rooij, L.P.M.H.; De Jong, J.H.; De Boer, O.J.; Van Leersum, R.; Bijlsma, M.F.; et al. Poor-prognosis colon cancer is defined by a molecularly distinct subtype and develops from serrated precursor lesions. Nat. Med. 2013, 19, 614–618. [Google Scholar] [CrossRef]
- Taieb, J.; André, T.; Auclin, E. Refining adjuvant therapy for non-metastatic colon cancer, new standards and perspectives. Cancer Treat. Rev. 2019, 75, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Allen, W.L.; Dunne, P.D.; McDade, S.; Scanlon, E.; Loughrey, M.; Coleman, H.; McCann, C.; McLaughlin, K.; Nemeth, Z.; Syed, N.; et al. Transcriptional subtyping and CD8 immunohistochemistry identifies poor prognosis stage II/III colorectal cancer patients who benefit from adjuvant chemotherapy. JCO Precis. Oncol. 2018, 2018, 1–15. [Google Scholar] [CrossRef] [PubMed]
- ten Hoorn, S.; de Back, T.R.; Sommeijer, D.W.; Vermeulen, L. Clinical Value of Consensus Molecular Subtypes in Colorectal Cancer: A Systematic Review and Meta-Analysis. JNCI J. Natl. Cancer Inst. 2021, 114, 503–516. [Google Scholar] [CrossRef] [PubMed]
- Alderdice, M.; Richman, S.D.; Gollins, S.; Stewart, J.P.; Hurt, C.; Adams, R.; McCorry, A.M.; Roddy, A.C.; Vimalachandran, D.; Isella, C.; et al. Prospective patient stratification into robust cancer-cell intrinsic subtypes from colorectal cancer biopsies. J. Pathol. 2018, 245, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Dunne, P.D.; McArt, D.G.; Bradley, C.A.; O’Reilly, P.G.; Barrett, H.L.; Cummins, R.; O’Grady, T.; Arthur, K.; Loughrey, M.B.; Allen, W.L.; et al. Challenging the Cancer Molecular Stratification Dogma: Intratumoral Heterogeneity Undermines Consensus Molecular Subtypes and Potential Diagnostic Value in Colorectal Cancer. Clin. Cancer Res. 2016, 22, 4095–4104. [Google Scholar] [CrossRef] [PubMed]
- Maleckar, J.; Sherman, L. The composition of the T cell receptor repertoire in nude mice. J. Immunol. 1987, 138, 3873–3876. [Google Scholar] [CrossRef]
- Fridman, W.H.; Sautès-Fridman, C.; Galon, J. The immune contexture in human tumours: Impact on clinical outcome. Nat. Rev. Cancer 2012, 12, 298–306. [Google Scholar] [CrossRef]
- Galon, J.; Mlecnik, B.; Bindea, G.; Angell, H.K.; Berger, A.; Lagorce, C.; Lugli, A.; Zlobec, I.; Hartmann, A.; Bifulco, C.; et al. Towards the introduction of the ‘Immunoscore’ in the classification of malignant tumours. J. Pathol. 2014, 232, 199–209. [Google Scholar] [CrossRef]
- Angell, H.; Galon, J. From the immune contexture to the Immunoscore: The role of prognostic and predictive immune markers in cancer. Curr. Opin. Immunol. 2013, 25, 261–267. [Google Scholar] [CrossRef]
- Pagès, F.; Mlecnik, B.; Marliot, F.; Bindea, G.; Ou, F.S.; Bifulco, C.; Lugli, A.; Zlobec, I.; Rau, T.T.; Berger, M.D.; et al. International validation of the consensus Immunoscore for the classification of colon cancer: A prognostic and accuracy study. Lancet 2018, 391, 2128–2139. [Google Scholar] [CrossRef]
- Galon, J.; Costes, A.; Sanchez-Cabo, F.; Kirilovsky, A.; Mlecnik, B.; Lagorce-Pagès, C.; Tosolini, M.; Camus, M.; Berger, A.; Wind, P.; et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 2006, 313, 1960–1964. [Google Scholar] [CrossRef] [PubMed]
- Ossendorp, F.; Mengedé, E.; Camps, M.; Filius, R.; Melief, C.J. Specific T helper cell requirement for optimal induction of cytotoxic T lymphocytes against major histocompatibility complex class II negative tumors. J. Exp. Med. 1998, 187, 693–702. [Google Scholar] [CrossRef]
- Quezada, S.A.; Simpson, T.R.; Peggs, K.S.; Merghoub, T.; Vider, J.; Fan, X.; Blasberg, R.; Yagita, H.; Muranski, P.; Antony, P.A. Tumor-reactive CD4+ T cells develop cytotoxic activity and eradicate large established melanoma after transfer into lymphopenic hosts. J. Exp. Med. 2010, 207, 637–650. [Google Scholar] [CrossRef] [PubMed]
- Kreiter, S.; Vormehr, M.; Van de Roemer, N.; Diken, M.; Löwer, M.; Diekmann, J.; Boegel, S.; Schrörs, B.; Vascotto, F.; Castle, J.C. Mutant MHC class II epitopes drive therapeutic immune responses to cancer. Nature 2015, 520, 692–696. [Google Scholar] [CrossRef]
- Topalian, S.L.; Drake, C.G.; Pardoll, D.M. Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell. 2015, 27, 450–461. [Google Scholar] [CrossRef] [PubMed]
- Lal, N.; White, B.S.; Goussous, G.; Pickles, O.; Mason, M.J.; Beggs, A.D.; Taniere, P.; Willcox, B.E.; Guinney, J.; Middleton, G.W. KRAS Mutation and Consensus Molecular Subtypes 2 and 3 Are Independently Associated with Reduced Immune Infiltration and Reactivity in Colorectal Cancer. Clin. Cancer Res. 2018, 24, 224. [Google Scholar] [CrossRef] [PubMed]
- Loupakis, F.; Biason, P.; Prete, A.A.; Cremolini, C.; Pietrantonio, F.; Pella, N.; Dell’Aquila, E.; Sperti, E.; Zichi, C.; Intini, R.; et al. CK7 and consensus molecular subtypes as major prognosticators in (V600E)BRAF mutated metastatic colorectal cancer. Br. J. Cancer 2019, 121, 593–599. [Google Scholar] [CrossRef]
- Borelli, B.; Antoniotti, C.; Carullo, M.; Germani, M.M.; Conca, V.; Masi, G. Immune-Checkpoint Inhibitors (ICIs) in Metastatic Colorectal Cancer (mCRC) Patients beyond Microsatellite Instability. Cancers 2022, 14, 4974. [Google Scholar] [CrossRef]
- Bittoni, A.; Sotte, V.; Meletani, T.; Cantini, L.; Giampieri, R.; Berardi, R. Immunotherapy in colorectal cancer treatment: Actual landscape and future perspectives. J. Cancer Metastasis Treat. 2018, 4, 55. [Google Scholar] [CrossRef]
- Calu, V.; Ionescu, A.; Stanca, L.; Geicu, O.I.; Iordache, F.; Pisoschi, A.M.; Serban, A.I.; Bilteanu, L. Key biomarkers within the colorectal cancer related inflammatory microenvironment. Sci. Rep. 2021, 11, 7940. [Google Scholar] [CrossRef] [PubMed]
- Thorsson, V.; Gibbs, D.L.; Brown, S.D.; Wolf, D.; Bortone, D.S.; Ou Yang, T.H.; Porta-Pardo, E.; Gao, G.F.; Plaisier, C.L.; Eddy, J.A.; et al. The Immune Landscape of Cancer. Immunity 2018, 48, 812–830.e14. [Google Scholar] [CrossRef] [PubMed]
- Sveen, A.; Bruun, J.; Eide, P.W.; Eilertsen, I.A.; Ramirez, L.; Murumägi, A.; Arjama, M.; Danielsen, S.A.; Kryeziu, K.; Elez, E.; et al. Colorectal Cancer Consensus Molecular Subtypes Translated to Preclinical Models Uncover Potentially Targetable Cancer Cell Dependencies. Clin. Cancer Res. 2018, 24, 794–806. [Google Scholar] [CrossRef] [PubMed]
- Picard, E.; Verschoor, C.P.; Ma, G.W.; Pawelec, G. Relationships between immune landscapes, genetic subtypes and responses to immunotherapy in colorectal cancer. Front. Immunol. 2020, 11, 369. [Google Scholar] [CrossRef]
- Karpinski, P.; Rossowska, J.; Sasiadek, M.M. Immunological landscape of consensus clusters in colorectal cancer. Oncotarget 2017, 8, 105299. [Google Scholar] [CrossRef]
- Kroemer, G.; Zitvogel, L. Cancer immunotherapy in 2017: The breakthrough of the microbiota. Nat. Rev. Immunol. 2018, 18, 87–88. [Google Scholar] [CrossRef]
- Chung, L.; Thiele Orberg, E.; Geis, A.L.; Chan, J.L.; Fu, K.; DeStefano Shields, C.E.; Dejea, C.M.; Fathi, P.; Chen, J.; Finard, B.B.; et al. Bacteroides fragilis Toxin Coordinates a Pro-carcinogenic Inflammatory Cascade via Targeting of Colonic Epithelial Cells. Cell. Host Microbe 2018, 23, 203–214.e5. [Google Scholar] [CrossRef] [PubMed]
- Long, X.; Wong, C.C.; Tong, L.; Chu, E.S.H.; Ho Szeto, C.; Go, M.Y.Y.; Coker, O.O.; Chan, A.W.H.; Chan, F.K.L.; Sung, J.J.Y.; et al. Peptostreptococcus anaerobius promotes colorectal carcinogenesis and modulates tumour immunity. Nat. Microbiol. 2019, 4, 2319–2330. [Google Scholar] [CrossRef] [PubMed]
- Mima, K.; Nishihara, R.; Qian, Z.R.; Cao, Y.; Sukawa, Y.; Nowak, J.A.; Yang, J.; Dou, R.; Masugi, Y.; Song, M.; et al. Fusobacterium nucleatum in colorectal carcinoma tissue and patient prognosis. Gut 2016, 65, 1973–1980. [Google Scholar] [CrossRef]
- Fong, W.; Li, Q.; Yu, J. Gut microbiota modulation: A novel strategy for prevention and treatment of colorectal cancer. Oncogene 2020, 39, 4925–4943. [Google Scholar] [CrossRef]
- Purcell, R.V.; Visnovska, M.; Biggs, P.J.; Schmeier, S.; Frizelle, F.A. Distinct gut microbiome patterns associate with consensus molecular subtypes of colorectal cancer. Sci. Rep. 2017, 7, 11590. [Google Scholar] [CrossRef]
- Mouradov, D.; Greenfield, P.; Li, S.; In, E.J.; Storey, C.; Sakthianandeswaren, A.; Georgeson, P.; Buchanan, D.D.; Ward, R.L.; Hawkins, N.J.; et al. Oncomicrobial Community Profiling Identifies Clinicomolecular and Prognostic Subtypes of Colorectal Cancer. Gastroenterology 2023, in press. [Google Scholar] [CrossRef]
- Guo, P.; Tian, Z.; Kong, X.; Yang, L.; Shan, X.; Dong, B.; Ding, X.; Jing, X.; Jiang, C.; Jiang, N. FadA promotes DNA damage and progression of Fusobacterium nucleatum-induced colorectal cancer through up-regulation of chk2. J. Exp. Clin. Cancer Res. 2020, 39, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.A.; Liu, F.; Riordan, S.M.; Lee, C.S.; Zhang, L. Global Investigations of Fusobacterium nucleatum in Human Colorectal Cancer. Front. Oncol. 2019, 9, 566. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.S.; Nishihara, R.; Cao, Y.; Song, M.; Mima, K.; Qian, Z.R.; Nowak, J.A.; Kosumi, K.; Hamada, T.; Masugi, Y.; et al. Association of Dietary Patterns with Risk of Colorectal Cancer Subtypes Classified by Fusobacterium nucleatum in Tumor Tissue. JAMA Oncol. 2017, 3, 921–927. [Google Scholar] [CrossRef]
- Mima, K.; Cao, Y.; Chan, A.T.; Qian, Z.R.; Nowak, J.A.; Masugi, Y.; Shi, Y.; Song, M.; Da Silva, A.; Gu, M. Fusobacterium nucleatum in colorectal carcinoma tissue according to tumor location. Clin. Transl. Gastroenterol. 2016, 7, e200. [Google Scholar] [CrossRef] [PubMed]
| CMS1 | CMS2 | CMS3 | CMS4 | Unclassified/Mixed | |
|---|---|---|---|---|---|
| Distribution |  |  |  |  |  |
| Biological features | Immune subtype MSI Tumors BRAFV600E mutation Hypermutated CIMP  DNA damage repair genes  | CIN  Epithelial differentiation Tumor suppressor genes  TP53 mutation | KRAS mutation 30% hypermutated CIMP  | SCNA  EMT  | |
| Pathways activation | MAPK RTK JAK-STAT | WNT MYC | MAPK RTK Epithelial and metabolism signatures | TGFβ signaling Angiogenesis Matrix remodeling Stromal infiltration Complement inflammatory system | |
| MicroRNA | MiR-17–92  | Let 7-miR family  | miR-200 family associated with EMT regulation  | ||
| Cell line | Undifferentiated | Colon-like | Colon-like | Undifferentiated | |
| Prognostic value | Good prognosis in early stage  Cytotoxic lymphocytes genes overexpression Poor prognosis after recurrence | Stage 2 tumors:  Highest OS | Stage 2 tumors:  Lowest OS | Poorer prognosis | Adequate nintedanib therapy response |
| Predict value | Bevacizumab may be more efficient than cetuximab | Sensitivity to oxaliplatin  Addition of bevacizumab to capecitabine-based chemotherapy is beneficial | Addition of bevacizumab to capecitabine-based chemotherapy is beneficial  | Stage III resistant to anti-EGFR therapy/no benefit from adjuvant therapy IRI-based regimen is highly beneficial Cetuximab may be more effective than Bevacizumab | |
| Polyps and adenomas | Same in both sexes Mostly right colon Mostly HP and SSA polyps Immune and stromal infiltration Activation of JAK-STAT and MAPK signaling BRAFV600E mutation | Same in both sexes Mostly left colon Significant enrichment for WNT and MYC pathways and E2F transcription factors/G2/M checkpoint/ mitotic spindle assembly/PI3K/ mTOR genes Most of the FAP, LS, and sporadic polyps Most of AP polyps | Chang et al. study: a small proportion of polyps in Komor et al. study: metabolism-associated Most prevalent (73%) Low risk of developing CRC Enrichment in haem, fatty acid, and sugar metabolism genes | Mesenchymal and stromal signatures TGFβ activation Mostly in SSA and HP polyps Low frequency | |
| Immunoscore | In non-pedunculated T1 CRC: I-low | In non-pedunculated T1 CRC: I-high | |||
| Immunotherapy and Immune Subtypes | C1 wound healing IS (46%) C2 IFN-g dominant IS (53%) Other IS rare The most likely to profit from immunotherapy | C1 wound healing IS (91%) C2 IFN-g dominant IS (8%) Other IS rare Immunity in KRAS mutant CMS2 is more suppressed | C1 wound healing IS (77–78%) C2 IFN-g dominant (11–13%) C3 inflammatory IS (7%) C4 lymphocyte-depleted IS (4%) | C1 wound healing IS (77–78%) C2 IFN-g dominant (11–13%) C3 inflammatory IS (6%) TGF-β dominant phenotype (2.3%) exclusively for CMS4 | |
| Gut microbiome | Fusobacteria  Bacteroidetes  Fusobacterium Hwasookii  Porphyromonas Gingivalis  Fusobacterium nucleatum  Parvimonas micra  Peptostreptococcus stomatis  Firmicutes  Proteobacteria  | Selenomas  Prevotella  Bacteroides  | Selenomas  Prevotella  |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rejali, L.; Seifollahi Asl, R.; Sanjabi, F.; Fatemi, N.; Asadzadeh Aghdaei, H.; Saeedi Niasar, M.; Ketabi Moghadam, P.; Nazemalhosseini Mojarad, E.; Mini, E.; Nobili, S. Principles of Molecular Utility for CMS Classification in Colorectal Cancer Management. Cancers 2023, 15, 2746. https://doi.org/10.3390/cancers15102746
Rejali L, Seifollahi Asl R, Sanjabi F, Fatemi N, Asadzadeh Aghdaei H, Saeedi Niasar M, Ketabi Moghadam P, Nazemalhosseini Mojarad E, Mini E, Nobili S. Principles of Molecular Utility for CMS Classification in Colorectal Cancer Management. Cancers. 2023; 15(10):2746. https://doi.org/10.3390/cancers15102746
Chicago/Turabian StyleRejali, Leili, Romina Seifollahi Asl, Fatemeh Sanjabi, Nayeralsadat Fatemi, Hamid Asadzadeh Aghdaei, Mahsa Saeedi Niasar, Pardis Ketabi Moghadam, Ehsan Nazemalhosseini Mojarad, Enrico Mini, and Stefania Nobili. 2023. "Principles of Molecular Utility for CMS Classification in Colorectal Cancer Management" Cancers 15, no. 10: 2746. https://doi.org/10.3390/cancers15102746
APA StyleRejali, L., Seifollahi Asl, R., Sanjabi, F., Fatemi, N., Asadzadeh Aghdaei, H., Saeedi Niasar, M., Ketabi Moghadam, P., Nazemalhosseini Mojarad, E., Mini, E., & Nobili, S. (2023). Principles of Molecular Utility for CMS Classification in Colorectal Cancer Management. Cancers, 15(10), 2746. https://doi.org/10.3390/cancers15102746








