Multifaceted Pharmacological Potentials of Curcumin, Genistein, and Tanshinone IIA through Proteomic Approaches: An In-Depth Review
Abstract
Simple Summary
Abstract
1. Introduction
1.1. Brief Overview on the General Characteristics of Various Phytochemicals
1.1.1. Curcumin
1.1.2. Genistein
1.1.3. Tanshinone IIA (Tan IIA)
1.1.4. Allicin
1.1.5. Eugenol
1.1.6. Apigenin
1.1.7. Lycopene
1.1.8. Anthocyanins
1.1.9. Capsaicin
1.1.10. Shogaols
2. Proteomics-Based Interventions in Phytochemical Studies
| SI. No. | Target Tissue or Cells | Proteomic Strategies | Objective of the Study | Prospective Proteins Upregulated (↑) or Downregulated (↓) | Disease and/or Condition Studied | References |
|---|---|---|---|---|---|---|
| Proteomics studies to understand the molecular intricacies of Cur | ||||||
| 1 | Bacillus subtilis AH75 strain | 2D-DIGE, iTRAQ | To investigate the proteome alterations in Bacillus subtilis following Cur treatment and identification of its molecular/cellular targets to understand the mechanism of action | UDP-N-acetyl glucosamine 1-carboxy vinyl transferase 2—↓ Putative septation protein (SpoVG)—↑ ATP-dependent zinc metalloprotease (FtsH)—↑ | Antibacterial action | [142] |
| 2 | Escherichia coli (ATCC 25922) | LFQ, LC-MS/MS | To investigate the mechanistic aspects of the antibacterial effects of Cur in the dark and upon illumination | Chaperone SeqB—↑ Gro-P like protein E (GrpE)—↑ Elongation factor (Tu1)—↑ Universal stress protein F (UspF)—↑ Probable quinol monooxygenase (YgiN)—↑ Uncharacterized oxidoreductase (YajO)—↑ | Antibacterial action | [220] |
| 3 | Imipenem- resistant Acinetobacter baumannii | LFQ, LC-MS/MS | To investigate the alteration in protein profile following exposure to blue light combined with Cur treatment | Carbonylated Omp38—↑ Carbonylated elongation factor Tu and P—↑ Carbonylated ribosome releasing factor—↑ | Antimicrobial resistance | [221] |
| 4 | Fathead minnow epithelial cells (FHM) | LFQ, LC-MS/MS | To evaluate the effect of Cur pretreatment in fathead minnow cells infected with viral hemorrhagic septicemia virus (VHSV) | Fibronectin (FN) 1—↓ Heat shock cognate 71 (HSC71)—↓ F-actin—↑ | Viral Hemorrhagic Septicemia | [29] |
| 5 | Human liver carcinoma cells (HepG2 cells) | 2D-DIGE, MALDI-TOF/ TOF/MS | To understand the anticancer mechanism of natural borneol (NB) and Cur in combination | Heterogeneous nuclear ribonucleoprotein (hnRNPC1/C2)—↓ Nucleophosmin (NPM)—↓ Proteasome 20S Subunit Alpha 5 (PSMA5)—↓ | Liver cancer | [222] |
| 6 | Human glioblastoma cells (U87 cells) | 2D-DIGE, iTRAQ, LFQ LC-MS/MS | To understand the underlying intricacies of LLL12, a Cur derivative against glioblastoma multiforme | Triose phosphate isomerase (TPI)—↓ Phosphoglycerate mutase 1 (PGAM1)—↓ Adaptor molecule (CRK2)—↓ protein DJ-1 (PARK7) —↓ Basic transcription factor 3 (BTF3)—↓ | Glioblastoma multiforme | [223] |
| 7 | Human colorectal carcinoma cells (HCT116 cells) | iTRAQ (TM) | To understand the molecular mechanism of action of Cur against colon cancer and try to identify its exact molecular targets | Microtubule-associated proteins 1A/1B light chain 3B (LC3B)—↑ Lysosomal-associated membrane protein (Lamp1)—↑ Heat shock protein 70 (HSP70)—↑ | Colorectal cancer | [224] |
| 8 | Melanoma cells (LB24 Dagi cells) | LFQ LC-MS/MS | To investigate the changes in the protein profile of melanoma cells following treatment with D6 (Cur analog) | PolyUbiquitin-C—↑ Heat shock 70 kDa protein 1A/1B—↑ DnaJ homolog subfamily B member 1—↑ Heterogeneous nuclear ribonucleoprotein Q—↓ Histone-H2A type 1-C—↓ | Melanoma cancer | [225] |
| 9 | Human liver carcinoma cells (HepG2 cells) | MALDI- TOF/TOF/ MS | To understand the efficacy of Cur/β-cyclodextrin polymer (CUR/CDP) inclusion complex against HepG2 and its possible molecular mechanisms of action | Nucleophosmin (NPM1)—↓ Peroxiredoxin-6 (PRDX6)—↓ | Liver cancer | [226] |
| 10 | Human acute lymphocytic leukemia cells (MOLT-4 cells) | 2-DE, MALDI-TOF Pro | To understand the role of Siah- interacting protein (SIP) in Cur-based therapeutic intervention | Siah-interacting protein (SIP)—↓ | Leukemia | [227] |
| 11 | Human lung adenocarcinoma cells (A549 cells) | 2-DE, MALDI-TOF/ TOF MS | To understand the precise molecular mechanism of Cur against human lung cancer | Heat shock protein 90 (HSP-90)—↓ 14-3-3 protein—↓ | Lung cancer | [228] |
| 12 | Human colon adenocarcinoma cells (LOVO cells) | MALDI- TOF/TOF MS | To investigate the action of irinotecan and Cur against colorectal cancer (LOVO) cells | Peroxiredoxin-4—↑ Glutathione S-transferase Mu 5—↓ Translocon associated protein subunit delta—↓ Calpain small subunit 1—↓ Protein disulfide-isomerase—↑ (Cur + irinotecan treatment) | Colorectal cancer | [229] |
| 13 | Human colorectal cancer cells (SW480 and SW620 cells) | LFQ LC-MS/MS | To understand the anti-metastatic properties of the conventional chemotherapeutic drugs and the phytochemicals through comparative proteomic approach | Fatty acid synthase (FASN)—↓ Histone H4—↓ | Colorectal cancer | [230] |
| 14 | Human colon carcinoma cells (HCT-8/VCR cells) | 2-DE, MALDI- TOF/ MS | To explore the differential proteomic profile of vincristine-resistant HCT-8/VCR cells with and without Cur treatment | Glutathione S-transferase pi1 gene (GSTP1)—↓ | Colorectal cancer | [231] |
| 15 | Human colorectal cancer cells (SW480 and SW620 cells) | 2-DE, LC-MS/MS | To understand anticancer activity of Cur against colorectal cancer | Mitogen-activated protein kinase (MEK1/2)—↑ Extracellular signal-regulated kinases (ERK1)—↑ Histone deacetylase C1 (HDAC1)—↓ Tumor protein 53 (P53)—↓ AMP-activated protein kinase (AMPKβ1)—↓ | Colorectal cancer | [232] |
| 16 | Human gastric cancer cells (BGC-823, MKN-45 and SCG-7901 cells) | 2-DE, MALDI-TOF/ TOF MS | To investigate the potential of Cur as natural anticancer agent against gastric cancer | Annexin A1 (ANXA1)—↑ Apoptosis Inducing Factor Mitochondria Associated 1 protein (AIFM1)—↑ Proliferation associated protein (A2G4)—↑ Protein phosphatase PP1-alpha catalytic subunit (PP1A)—↑ Glucose-regulated protein 75 (GRP75)—↓ T-complex protein 1 subunit alpha isoform a (TCPA)—↓ Eukaryotic initiation factor 4A-III (IF4A3)—↓ Thioredoxin domain-containing protein 5 (TXND5)—↓ | Gastric cancer | [233,234] |
| 17 | Human breast cancer cells (MCF-7, ZR-75-1) and TGF-β1 pretreated fibroblasts | LFQ, LC-MS/MS | To investigate the effects of Cur against breast cancer | Heme Oxygenase-1 (HMOX1)—↑ Ras Related GTP Binding A (RRAGA)—↑ Ring Finger And CCCH-Type Domains 1 (RC3H1)—↓ (in MCF-7/CLC co-culture) Retrotransposon-derived protein (PEG10)—↓ (in ZR-75-1/CLC co-culture) | Breast cancer | [235] |
| 18 | Triple negative breast cancer (TNBC) cells (MDA-MB-231) | LFQ, LC-MS/MS | To gain insights into the molecular intricacies of the anticancer effects of combinatorial treatment of Cur and electrical pulses (Cur+EP) compared to solitary treatments | Aldolase, Fructose-Bisphosphate A (ALDOA)—↓ Enolase 2 (ENO2)—↓ Lactate dehydrogenase A (LDHA)—↓ Lactate dehydrogenase B (LDHB)—↓ Phosphofructokinase platelet (PFKP)—↓ Phosphoglucomutase 1 (PGM1)—↓ (PGAM1)—↓ Phosphoglycerate kinase 1 (PGK1)—↓ | Triple negative breast cancer | [236] |
| 19 | Human oral adenosquamous carcinoma cells (CAL 27 cells) | SILAC, LC-MS/MS | To investigate the underlying molecular intricacies of tyrosine signaling in response to Cur | Tyrosine-protein phosphatase non- receptor type 6 (PTPN6)—↑ Abelson tyrosine-protein kinase 2 (ABL2)—↑ Fyn-related Src family tyrosine kinase (FRK)—↓ Pseudopodium enriched atypical kinase (PEAK1)—↓ | Head and Neck cancer | [237] |
| 20 | Human Chronic myelogenous leukemia (CML) cells (K562 and LAMA84 cells) | SWATH MS | To investigate that how exosome proteins from Cur-treated K562 cells can mediate the anti-angiogenic effect on HUVECs | Myristoylated Alanine Rich C- Kinase Substrate (MARCKS)—↓ Ras Homolog Family Member B (RhoB)—↓ Vascular cell adhesion protein 1 (VCAM1)—↓ | Chronic myelogenous leukemia | [238] |
| 21 | Human chronic myelogenous leukemia (CML) cells (K562 and LAMA84 cells) | LFQ, LC-MS/MS | To understand the pharmacological potential of Cur as a safe anti-tumor agent that can function as a chemosensitizer and a multi-targeted inhibitor | Aldolase, Fructose-Bisphosphate A (ALDOA)—↓ pyruvate kinase muscle isozyme (PKM)—↓ Lactate dehydrogenase A (LDHA)—↓ Phosphoglycerate kinase 1 (PGK1)—↓ Importin-7 (IPO7)—↓ | Chronic myelogenous leukemia | [239] |
| 22 | Mouse macrophage cells (RAW264.7 cells) | 2-DE, MALDI-TOF/MS | To study the anti-atherosclerosis mechanism of action of Cur | ATP synthesis H+ transporting—↑ MHC class II—↑ Non-muscle myosin alkali light chain—↑ Cytochrome b5—↑ Phosphodiesterase 4D—↓ Eukaryotic initiation factor 3 (elF-3)—↓ Hnrpf protein—↓ Vimentin (VIME)—↓ Nucleophosmin—↓ Ran binding protein (Ranbp 1)—↓ | Atherosclerosis | [240] |
| 23 | Mouse fibroblast cells (3T3-L1) and Primary white adipocytes | 2-DE, MALDI-TOF/MS | To understand the proteomic changes in cultured white adipocytes in response to Cur treatment and to identify the target proteins responsible for the fat-browning effects of Cur | Hormone-sensitive lipase (HSL)—↑ | Weight management | [241] |
| 24 | C57BL/6 mice | LFQ, LC-MS/MS | To understand the therapeutic efficacy of Cur against pulmonary fibrosis | Tumor protein (p53)—↓ Urokinase-type Plasminogen Activator (Upa)—↑ Plasminogen activator inhibitor-1 (PAI-I protein)—↓ | Pulmonary fibrosis | [242] |
| 25 | Human neuroblastoma (NB) cells (SH-SY5Y cells) | LFQ, LC-MS/MS | To explore the anticancer activity of Cur against human neuroblastoma | Heat shock protein 70 (Hsp70)—↑ Peroxiredoxin 1 (PRDX1)—↓ Peroxiredoxin 6 (PRDX6)—↓ | Neuroblastoma | [243] |
| 26 | Human lens epithelial B3 cells (HLE- B3 cells) | SELDI-TOF/MS | To understand the effect of Cur on HLE-B3 cell proliferation | Chemotactic factor A17—↓ Chemotactic factor A22—↓ IL-8—↓ Neutrophil active peptide-2—↓ | Posterior capsular opacification post cataract complications | [244] |
| 27 | Human colorectal adenoma | LC-MS/MS | To evaluate the effect of Cur on intestinal Uridine diphosphate glucuronosy ltransferase (UGT) expression | Uridine diphosphate glucuronosyltransferase (UGTs)—not affected by oral Cur | Colorectal adenoma | [245] |
| 28 | Hepatic liver tissue and Murine hepatocyte cells (AML12 cells) | 2-DE, MALDI–TOF/MS | To investigate the underlying intricacies of the effect of Cur against non-alcoholic fatty liver disease (NAFLD) | Superoxide dismutase 1 (SOD1)—↑ Sirtuin 1 (SIRT1)—↑ | Non-alcoholic fatty liver disease | [246] |
| 29 | Male hamsters | LFQ, LC-MS/MS | To elucidate the potential use of Cur and to identify its novel molecular targets | S100A6—↓ Lumican—↓ Plastin-2—↓ 14-3-3 zeta/delta—↓ Vimentin (VIME)—↓ | Cholangiocarcinoma | [247] |
| 30 | Sprague Dawley rats | 2-DE, LC-MS/MS | To investigate whether Cur regulates γ- enolase expression in focal cerebral ischemic injury in rats | γ-enolase—attenuation of its decreased expression induced by ischemic injury | Cerebral Ischemia | [248] |
| 31 | Adult male rats | 2-DE; LC-MS/MS | To identify various proteins that are differentially expressed by Cur treatment in focal cerebral ischemia | Ubiquitin carboxy-terminal hydrolase L1 (UCH-L1)—↑ Isocitrate dehydrogenase (ICDH)—↑ Adenosyl homocysteinase (AHC)— ↑ Eukaryotic initiation factor 4A (eIF4A)— ↑ Pyridoxal phosphate phosphatase (PPP)—↓ | Cerebral Ischemia | [249] |
| 32 | Mouse models of human inflammtory bowel disease (IBD) | 2-DE, LC-MS/MS | To understand the role of nutrient–gene interactions in human inflammatory bowel disease (IBD) | Proteins involved in digestion, excretion, and metabolism—↓ Cellular stress and immune response proteins—↑ | Inflammatory bowel disease | [250] |
| Proteomics studies to understand the molecular intricacies of Gen | ||||||
| 33 | Triple negative breast cancer (TNBC) cells (MDA- MB-231 cells) | TMT | To elucidate anticancer effects of Gen against TNBC cells | Cyclin-dependent kinase inhibitor (p21WAF1)—↑ Bcl-2-associated X protein (Bax)—↑ B-cell lymphoma-2 (Bcl-2)—↓ Tumor p53 protein (p53)—↓ Cyclin-dependent kinase 1 (CDK1)—↓ | Breast cancer | [251] |
| 34 | Human breast cancer cells (T47D cells) | SILAC | To understand the effect of a varying intracellular ERα/ERβ ratio on Gen-induced genes and protein expression profile | Myosin (MYH10, MYH14, MYL12B, MYH9, and MYL6)—↑ S100 family Ca2+ binding proteins (S100A8, S100A9)—↓ Prolactin Induced Protein (PIP)—↓ | Breast cancer | [252] |
| 35 | Human hepatocellular carcinoma cells (SNU-449 cells) | 2-DE, LC-MS/MS | To understand the anticancer effects of Gen against SNU-449 cells | B-cell lymphoma-2 (Bcl-2)—↓ Thioredoxin 1 (Trx1)—↓ | Hepatocellular carcinoma | [253] |
| 36 | Human gastric cancer cells (SGC-7901 cells) | SDS-PAGE, LC- MS/MS | To understand Gen-induced protein alterations in gastric cancer cells and to investigate the molecular mechanism responsible for the anticancer actions | Kinesin family proteins (KIFs)—↓ KIF11, KIF20A, KIF22, KIF23—↓ Centromere Protein F (CENPF)—↓ | Gastric cancer | [254] |
| 37 | Human promyelocytic leukemia cells (HL-60 cells) | In-gel digestion, MALDI-TOF/TOF/MS | To elucidate the changes in protein profile following treatment with Gen in human leukemia cells | Hsp70 protein 8—↑ Heterogeneous nuclear ribonucleoprotein (hnRNP) H1—↑ Ras-related protein (Rab14)—↓ Heterogeneous nuclear ribonucleo protein C (hnRNP C)—↓ Stathmin-1—↓ | Leukemia | [17] |
| 38 | Human promyelocytic leukemia cells (HL-60 cells) and Human AML cells (MV4-11 cells) | iTRAQ | To investigate the prospect of using Gen as an effective alternative therapy for AML | Eukaryotic translation initiation factor 4E-binding protein 1 (4EBP-1)—↓ | Acute myeloid leukemia | [255] |
| 39 | Mouse Cardiomyocyte cells (HL-1 cells) | 2-DE, LC-MS/MS | To study the concentration-dependent effects of Gen treatments on cardiomyocytes | Heat shock protein 27 (HSP27)—↑ Cathepsin D—↑ Heat shock protein (HSP70)—↑ Glucose-regulated protein (GRP78)—↑ Voltage-dependent anion-selective channel protein 1 (VDAC-2)—↑ Preprotein translocase of the inner membrane of mitochondria (TIM50)—↑ Bcl-2-associated athanogene 2 (BAG2)—↓ N-Myc Downstream Regulated 1 (NDRG1)—↓ | Cardiac Ischemic stress | [256] |
| 40 | Human endothelial cells (EA. hy 926 cells) | 2-DE, LC-MS/MS | Gen, on changes in protein expression levels induced by the endothelial stressor homocysteine (Hcy) in EA.hy 926 endothelial cells | End binding 1 (EB1)—↓ Cathepsin B—↓ | Atherosclerosis | [257] |
| 41 | Rat Hepatic Stellate cells (HSC-T6 cells) | 2-DE, LC-MS/MS | To elucidate the antifibrotic mechanism of combinatorial treatment of Gen, Taurine, and epigallocatechin gallate (EGCG) | Hexokinase 2 (HK2)—↓ Lysosomal-associated membrane protein (LAMP1)—↑ Cathepsin D—↑ | Liver fibrosis | [258] |
| 42 | Rats | 2-DE, LC-MS/MS and/or MALDI-TOF/TOF | To understand the role of Gen in breast cancer prevention | Endoplasmic reticulum resident protein 29 (ERp29)—↑ Guanine deaminase—↑ Fetuin-B—↑ Annexin A1, A2—↓ | Breast cancer | [259] |
| 43 | Rats | 2-DE, LC-MS/MS | To investigate Gen mechanisms of action against chemically induced mammary cancer | GTP cyclohydrolase 1 (GTP-CH1)—↑ Tyrosine hydroxylase (TH)—↑ Vascular endothelial growth factor receptor 2 (VEGFR2)—↓ | Breast cancer | [260] |
| 44 | Prepubertal girls blood and urine | TMT | To identify protein biomarkers of the effect and susceptibility for cancer from the blood of girls exposed to select environmental chemicals | Endothelin-converting enzyme (ECE-1)—↓ Eukaryotic translation initiation factor 3 subunit J (EIF-3)—↓ Nucleolar 7—↑ PR domain zinc finger 5 (PRDM5)—↑ | Mammary cancer | [261] |
| 45 | Sprague Dawley rats | TMT | To identify protein biomarkers of susceptibility from blood sera of rats exposed prepubertally to Bisphenol A (BPA) or Gen | Neurosecretory protein VGF 8a (VGF)—↓ Rho-associated coiled-coil containing protein kinase 2 (ROCK2)—↓ Matrix metalloproteinase 3 (MMP3)—↓ Protein tyrosine phosphatase receptor type K (PTPRK)—↑ SET domain containing 2 (SETD2)—↑ Ubiquitin carboxyl-terminal hydrolase—↑ | Cancer | [262] |
| 46 | C57BL/6J female mice (INTACT) and castrated females (CAST) | 2-DE, LC-MS/MS | To assess the impact of Gen on the cardiac proteome in ovariectomized female mice | Myosin 6—↑ Myosin regulatory light chain 4 (MLC-4)—↑ Moesin—↑ | Cardiovascular disease | [263] |
| 47 | Mice | 2-DE, LC-MS/MS | To characterize an animal model for alternative hormone replacement with Gen as a natural estrogenic compound | LIM domain-binding protein—↑ Desmin—↑ | Animal model characterization | [264] |
| 48 | Sprague Dawley rat model of liver fibrosis | iTRAQ | To understand the anti-fibrotic mechanisms of combination therapy of Gen, taurine, and epigallocatechin gallate (EGCG) | Annexin A2 (Anxa2)—↑ Thioredoxin domain-containing protein (Txn1)—↑ Proteoglycan 4 (Prg4)—↑ polymeric immunoglobulin receptor (Pigr)—↑ fibulin-1 (Fbln1)—↑ Triosephosphate isomerase (Tpi1)—↑ | Liver fibrosis | [265] |
| 49 | Rat model of liver fibrosis | iTRAQ | To understand the possible therapeutic mechanism of combination therapy against liver fibrosis | Thioredoxin domain-containing protein (Txn1)—↑ DEAD box protein family (Ddx39a)—↑ 17-beta-hydroxysteroid dehydrogenase type 6 (Hsd17b6)—↑ Cysteine Conjugate-beta Lyase 2 (Ccbl2)—↑ Magnesium cation transporter protein (Magt1)—↑ Cytochrome P450 4A14 (Cyp4a14)—↑ Glutathione S-transferase A1 (Gsta1)—↑ | Liver fibrosis | [266] |
| 50 | Adults male Wistar rats | SDS-PAGE, LC- MS/MS | Morphological response of reactive astrocytes positive for glial fibrillary acidic protein (GFAP) in rats | Glial fibrillary acidic protein (GFAP)—↓ | Astrogliosis | [267] |
| Proteomics studies to understand the molecular intricacies of Tan IIA | ||||||
| 51 | Human cervical cancer cells (HeLa cells) | In-gel digestion, MALDI-TOF MS | To investigate the prospective potential of Tan IIA as a potential anti-tumor agent | Proliferating cell nuclear antigen (PCNA)—↓ Heat shock protein 27 (HSP27)—↓ Vimentin (VIME)—↓ β-tubulin—↑ Superoxide dismutase (MgSOD)—↑ Glucose-regulated protein 75 (GRP75)—↑ Prohibitin—↑ | Cervical cancer | [268] |
| 52 | Human hepatocellular carcinoma cells (MHCC97-H cells) and Chang liver cells | LFQ, LC-MS/MS | To elucidate the Tan IIA-induced protein profile alteration in MHCC97-H cells | Keratin, type II cytoskeletal 8—↓ Keratin, type I cytoskeletal 18, 19, and 20—↓ Cathespin D—↓ Profilin 1—↓ Nucleoside diphosphate kinase A—↑ Annexin A1, A2—↑ | Liver cancer | [269] |
| 53 | Human gastric cancer cells (AGS cells) | iTRAQ | To understand the mechanism of action of TanIIA against gastric cancer | Tumor p53 protein (P53)—↑ Serine/threonine-protein kinase (AKT)—↓ | Gastric cancer | [270] |
| 54 | Immortalized rat myofibroblast cells (HSC-T6 cells) and Human Hepatocellular carcinoma cells (HepG2 cells) | In-gel digestion, MALDI-TOF/ TOF/ MS | To explore the mechanism of apoptosis induced by Tan IIA on activated rat Hepatic Stellate Cells (HSCs) | Prohibitin—↑ Translational Controlled Tumor Protein–(TCTP)—↓ GDP-dissociation inhibitor 1 (GDIR1)—↓ 14-3-3ε—↓ | Liver fibrosis | [271] |
| 55 | Osteosarcoma cancer cells (MG-63 cells) | 2-DE, LC-MS/MS | To understand the molecular mechanisms of anticancer effects of Ginsenoside Rg1, Cinnamic acid, and Tan IIA and to know their targets | Prohibitin—↓ | Osteosarcoma | [272] |
| 56 | Human gastric cancer cells (AGS cells) | Phosphoproteomics LTQ LC-MS/MS | To understand the molecular signal transduction pathway associated with the anticancer potential of Tan IIA | Phosphorylation of heat shock protein 27 Heat shock factor 1 (HSF1)—↑ | Gastric cancer | [273] |
| 57 | Human papillomavirus type 16 (HPV-16)-positive cells (CaSki cells) and Human cervical cancer cells (HeLa and SiHa cells) | In-gel digestion, MALDI-TOF/ TOF MS | To evaluate the growth inhibitory effect of Tan IIA on CaSki cells | Protein disulfide-isomerase A1 (PDIA1)—↓ Glucose-regulated protein 78 (Grp78)—↓ Whey proteins (TERA)—↓ Glucose-regulated protein (Grp94)—↓ Vimentin (VIME)—↓ Glucosidase II Alpha Subunit (GANAB)—↑ Cytoskeletal protein (VINC)—↑ The Putative Coupling Protein (TCPA)—↑ The brucella effector protein B (TCPB)—↑ Keratin 2C7 (K2C7)—↑ | Cervical cancer | [274] |
| 58 | Bone marrow- derived mesenchymal cells (BM-MSC) and Wharton’s Jelly- derived mesenchymal cells (WJ- MSC) | LFQ, LC-MS/MS | To understand the ability of BM- and WJ-MSC to differentiate towards the osteogenic lineage | Proteins of BMP signaling—↑ | Orthopedic disease | [275] |
| 59 | Mice myocardial cells | LFQ, MALDI- TOF/TOF/MS | To investigate the effect of Tan IIA on transverse aortic constriction (TAC)-induced heart failure | NADPH Oxidase 4 (Nox4)—↓ P38—↓ Nuclear factor erythroid 2- Related factor 2 (Nrf2)—↑ | Myocardial apoptosis | [276] |
| 60 | Lung cancer Radioresistant cells (H358-IR and H157-IR cells) | SILAC MS | To evaluate the potential of Tan I as a potential radiation sensitizer in lung cancer | Phosphoribosyl Pyrophosphate Amidotransferase (PPAT)—↓ B-cell lymphoma-2 (BCL2)—↓ Caspase 8—↑ | Lung cancer | [277] |
| 61 | Adult male KM mice | 2-DE, LC-MS/MS | To understand the potentials of Tan II A sodium sulfonate (TSNIIA-SS) against Doxorubicin (DXR)-induced nephropathy | Myo-inositol oxygenase—↑ Glutathione peroxidases (GSH-Pxs)—↓ Proteasome alpha 5—↓ | Nephropathy | [278] |
2.1. Proteomic Approaches to Understand the Function of Curcumin as Therapeutic Intervention
2.1.1. Proteomic Studies to Explore Its Potential against Microbial Diseases
2.1.2. Proteomic Studies to Explore Its Potential against Cancer
2.1.3. Proteomic Studies to Explore Its Potential against Various Other Disease Pathologies
2.2. Proteomic Approaches to Understand the Function of Genistein as Therapeutic Intervention
2.3. Proteomic Approaches to Understand the Function of Tan IIA as Therapeutic Intervention
3. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ACTC1 | Alpha cardiac muscle protein |
| AEC | Alveolar epithelial cells |
| ALT | Alanine aminotransferase |
| AST | Aspartate transaminase |
| ATR | Ataxia telangiectasia serine/threonine-protein kinase |
| BLM | Bleomycin |
| BPA | Bisphenol A |
| BRCA1 | Breast cancer susceptibility gene 1 |
| BTF3 | Basic transcription factor 3 |
| CPT-1 | Carnitine palmitoyl transferase I |
| CRC | Colorectal cancer |
| CRK2 | Cysteine-rich receptor-like protein kinase |
| Cur-P | Curcumin probe |
| CUR/CDP | Curcumin/β-cyclodextrin polymer |
| 2-DE | Two-dimensional gel electrophoresis |
| 2D-DIGE | Two-dimensional differential gel electrophoresis |
| 2-DE/ESI-LC-MS | Two-dimensional liquid chromatography/electrospray ionization mass spectrometry |
| DJ-1 (PARK7) | Protein deglycase DJ-1, also known as Parkinson disease protein 7 |
| DMSO | Dimethyl sulfoxide |
| ECM | Extracellular matrix |
| eEF1 | Eukaryotic elongation factor 1 |
| EGF-R | Epidermal growth factor receptor |
| eIF2 | Eukaryotic Initiation Factor 2 |
| elF-3 | Eukaryotic initiation factor 3 |
| ER | Endoplasmic reticulum |
| FN-1 | Fibronectin-1 |
| FtsZ | Filamenting temperature-sensitive mutant Z |
| GBM | Glioblastoma multiforme |
| GLUT-4 | Glucose transporter type 4 |
| GSH-Px | Glutathione peroxidase |
| GSN | Gelsolin |
| GSTM5 | Glutathione S-transferase Mu 5 |
| HNRPF | Heterogeneous nuclear ribonucleoprotein F |
| HSC71 | Heat shock cognate 71 |
| HSL | Hormone-sensitive lipase |
| HSP27 | Heat shock protein 27 |
| IPA | Ingenuity pathways analysis |
| iTRAQ | Isobaric tags for relative and absolute quantitation |
| JNK | c-Jun N-terminal kinase |
| KM-mice | Kunming mice |
| LC-MALDI-MS | Liquid chromatography-matrix-assisted laser desorption/ionization mass spectrometry |
| LC-MS/MS | Liquid Chromatography with tandem mass spectrometry |
| LECs | Lens epithelial cells |
| LFQ | Label free quantitation |
| LTQ-Orbitrap | Linear ion trap-Orbitrap |
| MALDI-TOF/TOF-MS | Matrix-assisted laser desorption ionization tandem time-of-flight mass spectrometry |
| MBzP | Mono-benzyl phthalate |
| MEHP | Mono-ethyl hexyl phthalate |
| MLC | Myosin light chain |
| MLCK | Myosin light chain kinase |
| MMP3 | Matrix metalloproteinase-3 |
| MRM | Multiple reaction monitoring |
| MS | Mass spectrometry |
| mTOR | Mammalian target of rapamycin |
| NPM1 | Nucleophosmin |
| PCO | Posterior capsular opacification |
| PDI | Protein disulphide isomerase |
| PDIA3 | Protein disulfide isomerase A3 |
| PGAM1 | Phosphoglycerate mutase 1 |
| PGC-1α | Peroxisome proliferator-activated receptor gamma coactivator 1-alpha |
| PGK1 | Phosphoglycerate kinase-1 |
| PRDX4 | Peroxiredoxin-4 |
| PRDX6 | Peroxiredoxin-6 |
| Q-Orbitrap MS | Quadrupole-Orbitrap Mass Spectrometer |
| RanBP-1 | Ran binding protein-1 |
| rhbFGF | Recombinant human basic fibroblast growth factor |
| ROCK2 | Rho associated coiled-coil containing protein kinase 2 |
| ROS | Reactive oxygen species |
| SILAC | Stable isotope labeling by amino acids in cell culture |
| SOD | Superoxide dismutase |
| STAT3 | Signal transducer and activator of transcription 3 |
| SWATH-MS | Sequential window acquisition of all theoretical mass spectra |
| SDS-PAGE | Sodium dodecyl-sulfate polyacrylamide gel electrophoresis |
| T-AOC | Total antioxidant capacity |
| TAC | Transverse aortic constriction |
| Tan IIA | Tanshinone IIA |
| TGF-β1 | Transforming growth factor-β1 |
| TMT | Tandem mass tags |
| TNBC | Triple-negative breast cancer |
| TPI | Triosephosphate isomerase |
| UCP1 | Uncoupling protein 1 |
| UGT | Uridine diphosphate glucuronosyltransferase |
| VEGF-R2 | Vascular endothelial growth factor receptor 2 |
| VHSV | Viral hemorrhagic septicemia virus |
References
- Choudhary, N.; Tewari, D.; Nabavi, S.F.; Kashani, H.R.K.; Lorigooini, Z.; Filosa, R.; Khan, F.B.; Masoudian, N. Plant based food bioactives: A boon or bane for neurological disorders. Crit. Rev. Food Sci. Nutr. 2022, 1–47. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.B.; Ansari, M.A.; Uddin, S.; Palakott, A.R.; Anwar, I.; Almatroudi, A.; Alomary, M.N.; Alrumaihi, F.; Alkhayl, F.F.A.; Alghamdi, S.; et al. Prospective Role of Bioactive Molecules and Exosomes in the Therapeutic Potential of Camel Milk against Human Diseases: An Updated Perspective. Life 2022, 12, 990. [Google Scholar] [CrossRef] [PubMed]
- Patil, K.; Khan, F.B.; Akhtar, S.; Ahmad, A.; Uddin, S. The plasticity of pancreatic cancer stem cells: Implications in therapeutic resistance. Cancer Metastasis Rev. 2021, 40, 691–720. [Google Scholar] [CrossRef] [PubMed]
- Chiang, J.-T.; Badrealam, K.F.; Shibu, M.A.; Kuo, C.-H.; Huang, C.-Y.; Chen, B.-C.; Lin, Y.-M.; Viswanadha, V.P.; Kuo, W.-W. Eriobotrya japonica ameliorates cardiac hypertrophy in H9c2 cardiomyoblast and in spontaneously hypertensive rats. Environ. Toxicol. 2018, 33, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Chiang, J.-T.; Badrealam, K.F.; Shibu, M.A.; Cheng, S.-F.; Shen, C.-Y.; Chang, C.-F.; Lin, Y.-M.; Viswanadha, V.P.; Liao, S.-C.; Huang, C.-Y. Anti-Apoptosis and Anti-Fibrosis Effects of Eriobotrya Japonica in Spontaneously Hypertensive Rat Hearts. Int. J. Mol. Sci. 2018, 19, 1638. [Google Scholar] [CrossRef]
- Ansari, M.A.; Khan, F.B.; Safdari, H.A.; Almatroudi, A.; Alzohairy, M.A.; Safdari, M.; Amirizadeh, M.; Rehman, S.; Equbal, M.J.; Hoque, M. Prospective therapeutic potential of Tanshinone IIA: An updated overview. Pharmacol. Res. 2020, 164, 105364. [Google Scholar] [CrossRef]
- Forni, C.; Facchiano, F.; Bartoli, M.; Pieretti, S.; Facchiano, A.; D’Arcangelo, D.; Norelli, S.; Valle, G.; Nisini, R.; Beninati, S.; et al. Beneficial Role of Phytochemicals on Oxidative Stress and Age-Related Diseases. BioMed Res. Int. 2019, 2019, 8748253. [Google Scholar] [CrossRef]
- Ansari, M.A.; Badrealam, K.F.; Alam, A.; Tufail, S.; Khalique, G.; Equbal, M.J.; Alzohairy, M.A.; Almatroudi, A.; Alomary, M.N.; Pottoo, F.H. Recent Nano-based Therapeutic Intervention of Bioactive Sesquiterpenes: Prospects in Cancer Therapeutics. Curr. Pharm. Des. 2020, 26, 1138–1144. [Google Scholar] [CrossRef]
- Abdullah; Khan, M.A.; Ahmad, W.; Ahmad, M.; Adhikari, A.; Ibrar, M.; Rehman, M.U.; Asif, M.J.D.; Toxicology, C. Antioxidant, antinociceptive, anti-inflammatory, and hepatoprotective activities of pentacyclic triterpenes isolated from Ziziphus oxyphylla Edgew. Drug Chem. Toxicol. 2021, 45, 1796–1807. [Google Scholar] [CrossRef]
- Abdullah, M.A.K.; Ahmad, W.; Adhikari, A.; Ibrar, M.; ur Rehman, M.; Khan, M.; Kamil, A. Exploration of Hepatoprotective Potential and Phytochemicals of Ziziphus oxyphylla Edgew. Pak. Vet. J. 2020, 40, 431–436. [Google Scholar] [CrossRef]
- Alam, S.S.M.; Uddin, F.; Khan, F.B.; Kamal, M.A.; Hoque, M. Therapeutic and pharmacological potential of Tanshinones against lung cancer: A systematic review. Phytomed. Plus 2022, 2, 100202. [Google Scholar] [CrossRef]
- Chen, K.-J.; Hui, K.K.; Lee, M.S.; Xu, H. The Potential Benefit of Complementary/Alternative Medicine in Cardiovascular Diseases. Evid. -Based Complement. Altern. Med. 2012, 2012, 1. [Google Scholar] [CrossRef] [PubMed]
- Afendi, F.M.; Okada, T.; Yamazaki, M.; Hirai-Morita, A.; Nakamura, Y.; Nakamura, K.; Ikeda, S.; Takahashi, H.; Amin, A.U.; Darusman, L.K.; et al. KNApSAcK Family Databases: Integrated Metabolite–Plant Species Databases for Multifaceted Plant Research. Plant Cell Physiol. 2011, 53, e1. [Google Scholar] [CrossRef] [PubMed]
- Xue, R.; Fang, Z.; Zhang, M.; Yi, Z.; Wen, C.; Shi, T. TCMID: Traditional Chinese medicine integrative database for herb molecular mechanism analysis. Nucleic Acids Res. 2012, 41, D1089–D1095. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Gui, Y.; Chen, L.; Yuan, G.; Xu, X. CVDHD: A cardiovascular disease herbal database for drug discovery and network pharmacology. J. Chemin 2013, 5, 51. [Google Scholar] [CrossRef] [PubMed]
- Jensen, K.; Panagiotou, G.; Kouskoumvekaki, I. Integrated text mining and chemoinformatics analysis associates diet to health benefit at molecular level. PLoS Comput. Biol. 2014, 10, e1003432. [Google Scholar] [CrossRef]
- Zhang, D.; Tai, Y.-C.; Wong, C.-H.S.; Tai, L.-K.; Koay, E.S.-C.; Chen, C.-S. Molecular response of leukemia HL-60 cells to genistein treatment, a proteomics study. Leuk. Res. 2007, 31, 75–82. [Google Scholar] [CrossRef]
- Mohanraj, K.; Karthikeyan, B.S.; Vivek-Ananth, R.P.; Chand, R.P.B.; Aparna, S.R.; Mangalapandi, P.; Samal, A. IMPPAT: A curated database of Indian Medicinal Plants, Phytochemistry And Therapeutics. Sci. Rep. 2018, 8, 4329. [Google Scholar] [CrossRef]
- Newman, D.J.; Cragg, G.M. Natural products as sources of new drugs over the last 25 years. J. Nat. Prod. 2007, 70, 461–477. [Google Scholar] [CrossRef]
- Cutler, G.J.; Nettleton, J.A.; Ross, J.A.; Harnack, L.J.; Jacobs, D.R., Jr.; Scrafford, C.G.; Barraj, L.M.; Mink, P.J.; Robien, K. Dietary flavonoid intake and risk of cancer in postmenopausal women: The Iowa Women’s Health Study. Int. J. Cancer 2008, 123, 664–671. [Google Scholar] [CrossRef]
- Key, T.J.; Sharp, G.B.; Appleby, P.N.; Beral, V.; Goodman, M.T.; Soda, M.; Mabuchi, K. Soya foods and breast cancer risk: A prospective study in Hiroshima and Nagasaki, Japan. Br. J. Cancer 1999, 81, 1248–1256. [Google Scholar] [CrossRef]
- Hussain, Y.; Abdullah; Alsharif, K.F.; Aschner, M.; Theyab, A.; Khan, F.; Saso, L.; Khan, H. Therapeutic Role of Carotenoids in Blood Cancer: Mechanistic Insights and Therapeutic Potential. Nutrients 2022, 14, 1949. [Google Scholar] [CrossRef] [PubMed]
- Le Marchand, L.; Murphy, S.P.; Hankin, J.H.; Wilkens, L.R.; Kolonel, L.N. Intake of Flavonoids and Lung Cancer. Gynecol. Oncol. 2000, 92, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Su, L.J.; Arab, L.J. Tea consumption and the reduced risk of colon cancer–results from a national prospective cohort study. Public Health Nutr. 2002, 5, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Jakubczyk, K.; Drużga, A.; Katarzyna, J.; Skonieczna-Żydecka, K. Antioxidant Potential of Curcumin—A Meta-Analysis of Randomized Clinical Trials. Antioxidants 2020, 9, 1092. [Google Scholar] [CrossRef]
- Peng, Y.; Ao, M.; Dong, B.; Jiang, Y.; Yu, L.; Chen, Z.; Hu, C.; Xu, R. Anti-Inflammatory Effects of Curcumin in the Inflammatory Diseases: Status, Limitations and Countermeasures. Drug Des. Dev. Ther. 2021, ume 15, 4503–4525. [Google Scholar] [CrossRef]
- Adamczak, A.; Ożarowski, M.; Karpiński, T.M. Curcumin, a Natural Antimicrobial Agent with Strain-Specific Activity. Pharmaceuticals 2020, 13, 153. [Google Scholar] [CrossRef]
- Moghadamtousi, S.Z.; Kadir, H.A.; Hassandarvish, P.; Tajik, H.; Abubakar, S.; Zandi, K. A Review on Antibacterial, Antiviral, and Antifungal Activity of Curcumin. BioMed Res. Int. 2014, 2014, 186864. [Google Scholar] [CrossRef]
- Jeong, E.-H.; Vaidya, B.; Cho, S.-Y.; Park, M.-A.; Kaewintajuk, K.; Kim, S.R.; Oh, M.-J.; Choi, J.-S.; Kwon, J.; Kim, D. Identification of regulators of the early stage of viral hemorrhagic septicemia virus infection during curcumin treatment. Fish Shellfish Immunol. 2015, 45, 184–193. [Google Scholar] [CrossRef]
- Tomeh, M.A.; Hadianamrei, R.; Zhao, X. A Review of Curcumin and Its Derivatives as Anticancer Agents. Int. J. Mol. Sci. 2019, 20, 1033. [Google Scholar] [CrossRef]
- Ribeiro, A.P.D.; Pavarina, A.C.; Dovigo, L.N.; Brunetti, I.L.; Bagnato, V.S.; Vergani, C.E.; Costa, C.A.D.S. Phototoxic effect of curcumin on methicillin-resistant Staphylococcus aureus and L929 fibroblasts. Lasers Med. Sci. 2012, 28, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Hegge, A.B.; Nielsen, T.T.; Larsen, K.L.; Bruzell, E.; Tønnesen, H.H. Impact of Curcumin Supersaturation in Antibacterial Photodynamic Therapy—Effect of Cyclodextrin Type and Amount: Studies on Curcumin and Curcuminoides XLV. J. Pharm. Sci. 2012, 101, 1524–1537. [Google Scholar] [CrossRef] [PubMed]
- Santezi, C.; Reina, B.D.; de Annunzio, S.R.; Calixto, G.; Chorilli, M.; Dovigo, L.N. Photodynamic potential of curcumin in bioadhesive formulations: Optical characteristics and antimicrobial effect against biofilms. Photodiagnosis Photodyn. Ther. 2021, 35, 102416. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.; Boland, C.; Chauhan, D.P. Specific inhibition of cyclooxygenase-2 (COX-2) expression by dietary curcumin in HT-29 human colon cancer cells. Cancer Lett. 2001, 172, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Bezáková, L.; Košťálová, D.; Obložinský, M.; Hoffman, P.; Pekárová, M.; Kollárová, R.; Holková, I.; Mošovská, S.; Sturdík, E.S. Inhibition of 12/15 lipoxygenase by curcumin and an extract from Curcuma longa L. Ceska Slov. Farm. 2014, 63, 26–31. [Google Scholar]
- Rainey, N.E.; Moustapha, A.; Saric, A.; Nicolas, G.; Sureau, F.; Petit, P.X. Iron chelation by curcumin suppresses both curcumin-induced autophagy and cell death together with iron overload neoplastic transformation. Cell Death Discov. 2019, 5, 150. [Google Scholar] [CrossRef] [PubMed]
- Catanzaro, M.; Corsini, E.; Rosini, M.; Racchi, M.; Lanni, C. Immunomodulators Inspired by Nature: A Review on Curcumin and Echinacea. Molecules 2018, 23, 2778. [Google Scholar] [CrossRef] [PubMed]
- Lim, G.P.; Chu, T.; Yang, F.; Beech, W.; Frautschy, S.A.; Cole, G.M. The Curry Spice Curcumin Reduces Oxidative Damage and Amyloid Pathology in an Alzheimer Transgenic Mouse. J. Neurosci. 2001, 21, 8370–8377. [Google Scholar] [CrossRef]
- McClure, R.; Ong, H.; Janve, V.; Barton, S.; Zhu, M.; Li, B.; Dawes, M.; Jerome, W.G.; Anderson, A.; Massion, P.; et al. Aerosol Delivery of Curcumin Reduced Amyloid-β Deposition and Improved Cognitive Performance in a Transgenic Model of Alzheimer’s Disease. J. Alzheimer’s Dis. 2016, 55, 797–811. [Google Scholar] [CrossRef]
- Del Tredici, K.; Braak, H. Sporadic Parkinson’s disease: Development and distribution of α-synuclein pathology. Neuropathol. Appl. Neurobiol. 2016, 42, 33–50. [Google Scholar] [CrossRef]
- El Nebrisi, E.; Javed, H.; Ojha, S.K.; Oz, M.; Shehab, S. Neuroprotective Effect of Curcumin on the Nigrostriatal Pathway in a 6-Hydroxydopmine-Induced Rat Model of Parkinson’s Disease is Mediated by α7-Nicotinic Receptors. Int. J. Mol. Sci. 2020, 21, 7329. [Google Scholar] [CrossRef]
- Sharifi-Rad, J.; Quispe, C.; Imran, M.; Rauf, A.; Nadeem, M.; Gondal, T.A.; Ahmad, B.; Atif, M.; Mubarak, M.S.; Sytar, O.; et al. Genistein: An Integrative Overview of Its Mode of Action, Pharmacological Properties, and Health Benefits. Oxidative Med. Cell. Longev. 2021, 2021, 150. [Google Scholar] [CrossRef] [PubMed]
- Goh, Y.X.; Jalil, J.; Lam, K.W.; Husain, K.; Premakumar, C.M. Genistein: A Review on its Anti-Inflammatory Properties. Front. Pharmacol. 2022, 13, 820969. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.; Landauer, M.R.; Foriska, M.A.; Ledney, G.D. Antibacterial activity of the soy isoflavone genistein. J. Basic Microbiol. 2006, 46, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Tuli, H.S.; Tuorkey, M.J.; Thakral, F.; Sak, K.; Kumar, M.; Sharma, A.K.; Sharma, U.; Jain, A.; Aggarwal, V.; Bishayee, A. Molecular Mechanisms of Action of Genistein in Cancer: Recent Advances. Front. Pharmacol. 2019, 10, 1336. [Google Scholar] [CrossRef]
- Tanjak, P.; Thiantanawat, A.; Watcharasit, P.; Satayavivad, J. Genistein reduces the activation of AKT and EGFR, and the production of IL6 in cholangiocarcinoma cells involving estrogen and estrogen receptors. Int. J. Oncol. 2018, 53, 177–188. [Google Scholar] [CrossRef]
- Polkowski, K.; Mazurek, A.P. Biological properties of genistein. A review of in vitro and in vivo data. Acta Pol. Pharm. -Drug Res. 2000, 57, 30–38. [Google Scholar]
- Li, R.; He, P.; Cui, J.; Staufenbiel, M.; Harada, N.; Shen, Y. Brain Endogenous Estrogen Levels Determine Responses to Estrogen Replacement Therapy via Regulation of BACE1 and NEP in Female Alzheimer’s Transgenic Mice. Mol. Neurobiol. 2012, 47, 857–867. [Google Scholar] [CrossRef]
- Youn, K.; Park, J.-H.; Lee, S.; Lee, S.; Lee, J.; Yun, E.-Y.; Jeong, W.-S.; Jun, M. BACE1 Inhibition by Genistein: Biological Evaluation, Kinetic Analysis, and Molecular Docking Simulation. J. Med. Food 2018, 21, 416–420. [Google Scholar] [CrossRef]
- Arbabi, E.; Hamidi, G.; Talaei, S.A.; Salami, M. Estrogen agonist genistein differentially influences the cognitive and motor disorders in an ovariectomized animal model of Parkinsonism. Iran. J. Basic Med. Sci. 2016, 19, 1285–1290. [Google Scholar] [CrossRef]
- Rhiu, S.; Chae, M.K.; Lee, E.J.; Lee, J.B.; Yoon, J.S.; Huang, W.; Zhang, X. Effect of Tanshinone IIA in an In Vitro Model of Graves’ Orbitopathy. Investig. Opthalmol. Vis. Sci. 2014, 55, 5900–5910. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, Z.; Xu, H. Anti-Inflammatory and Immunomodulatory Mechanism of Tanshinone IIA for Atherosclerosis. Evid. -Based Complement. Altern. Med. 2014, 2014, 267976. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Zhang, W.; Wang, T.; Li, N.; Mu, H.; Zhang, J.; Duan, J. Unveiling the Mode of Action of Two Antibacterial Tanshinone Derivatives. Int. J. Mol. Sci. 2015, 16, 17668–17681. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.; Zhang, M.; Liu, J.-N.; Zhao, X.; Zhang, Y.-Q.; Fang, L. Tanshinone IIA: A Review of its Anticancer Effects. Front. Pharmacol. 2021, 11, 611087. [Google Scholar] [CrossRef]
- Xing, Y.; Tu, J.; Zheng, L.; Guo, L.; Xi, T. Anti-angiogenic effect of tanshinone IIA involves inhibition of the VEGF/VEGFR2 pathway in vascular endothelial cells. Oncol. Rep. 2014, 33, 163–170. [Google Scholar] [CrossRef]
- Park, Y.-K.; Obiang-Obounou, B.W.; Lee, J.; Lee, T.-Y.; Bae, M.-A.; Hwang, K.-S.; Lee, K.-B.; Choi, J.-S.; Jang, B.-C. Anti-Adipogenic Effects on 3T3-L1 Cells and Zebrafish by Tanshinone IIA. Int. J. Mol. Sci. 2017, 18, 2065. [Google Scholar] [CrossRef]
- Ozhan Kocakaya, Ş.; Ertaş, A.; Yener, I.; Ercan, B.; Oral, E.; Akdeniz, M.; Kaplaner, E.; Topcu, G.; Kolak, U. Selective in-vitro enzymes’ inhibitory activities of fingerprints compounds of Salvia species and molecular docking simulations. Iran. J. Pharm. Res. 2020, 19, 187–198. [Google Scholar]
- Ślusarczyk, S.; Senol Deniz, F.S.; Abel, R.; Pecio, Ł.; Pérez-Sánchez, H.; Cerón-Carrasco, J.P.; den-Haan, H.; Banerjee, P.; Preissner, R.; Krzyżak, E.; et al. Norditerpenoids with Selective Anti-Cholinesterase Activity from the Roots of Perovskia atriplicifolia Benth. Int. J. Mol. Sci. 2020, 21, 4475. [Google Scholar] [CrossRef]
- Ding, B.; Lin, C.; Liu, Q.; He, Y.; Ruganzu, J.B.; Jin, H.; Peng, X.; Ji, S.; Ma, Y.; Yang, W. Tanshinone IIA attenuates neuroinflammation via inhibiting RAGE/NF-κB signaling pathway in vivo and in vitro. J. Neuroinflamm. 2020, 17, 302. [Google Scholar] [CrossRef]
- Zhang, X.S.; Ha, S.; Wang, X.L.; Shi, Y.L.; Duan, S.S.; Li, Z.A. Tanshinone IIA protects dopaminergic neurons against 6-hydroxydopamine-induced neurotoxicity through miR-153/NF-E2-related factor 2/antioxidant response element signaling pathway. Neuroscience 2015, 303, 489–502. [Google Scholar] [CrossRef]
- Chung, L.Y. The antioxidant properties of garlic compounds: Allyl cysteine, alliin, allicin, and allyl disulfide. J. Med. Food 2006, 9, 205–213. [Google Scholar] [CrossRef]
- Ankri, S.; Mirelman, D. Antimicrobial properties of allicin from garlic. Microbes Infect. 1999, 1, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-S.; Kim, K.S.; Han, I.; Kim, M.-H.; Jung, M.H.; Park, H.-K. Quantitative and Qualitative Analysis of the Antifungal Activity of Allicin Alone and in Combination with Antifungal Drugs. PLoS ONE 2012, 7, e38242. [Google Scholar] [CrossRef]
- Cutler, R.R.; Wilson, P. Antibacterial activity of a new, stable, aqueous extract of allicin against methicillin-resistant Staphylococcus aureus. Br. J. Biomed. Sci. 2004, 61, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Rouf, R.; Uddin, S.J.; Sarker, D.K.; Islam, M.T.; Ali, E.S.; Shilpi, J.A.; Nahar, L.; Tiralongo, E.; Sarker, S.D. Antiviral potential of garlic (Allium sativum) and its organosulfur compounds: A systematic update of pre-clinical and clinical data. Trends Food Sci. Technol. 2020, 104, 219–234. [Google Scholar] [CrossRef] [PubMed]
- Benavides, G.A.; Squadrito, G.L.; Mills, R.W.; Patel, H.D.; Isbell, T.S.; Patel, R.P.; Darley-Usmar, V.M.; Doeller, J.E.; Kraus, D.W. Hydrogen sulfide mediates the vasoactivity of garlic. Proc. Natl. Acad. Sci. USA 2007, 104, 17977–17982. [Google Scholar] [CrossRef]
- Li, X.-H.; Li, C.-Y.; Lu, J.-M.; Tian, R.-B.; Wei, J. Allicin ameliorates cognitive deficits ageing-induced learning and memory deficits through enhancing of Nrf2 antioxidant signaling pathways. Neurosci. Lett. 2012, 514, 46–50. [Google Scholar] [CrossRef]
- Eilat, S.; Oestraicher, Y.; Rabinkov, A.; Ohad, D.; Mirelman, D.; Battler, A.; Eldar, M.; Vered, Z. Alteration of lipid profile in hyperlipidemic rabbits by allicin, an active constituent of garlic. Coron. Artery Dis. 1995, 6, 985–990. [Google Scholar]
- Gebhardt, R.; Beck, H.; Wagner, K.G.; Metabolism, L. Inhibition of cholesterol biosynthesis by allicin and ajoene in rat hepatocytes and HepG2 cells. Biochim. Et Biophys. Acta (BBA) Lipids Lipid Metab. 1994, 1213, 57–62. [Google Scholar] [CrossRef]
- Oommen, S.; Anto, R.J.; Srinivas, G.; Karunagaran, D. Allicin (from garlic) induces caspase-mediated apoptosis in cancer cells. Eur. J. Pharmacol. 2003, 485, 97–103. [Google Scholar] [CrossRef]
- Park, S.-Y.; Cho, S.-J.; Kwon, H.-C.; Lee, K.-R.; Rhee, D.-K.; Pyo, S. Caspase-independent cell death by allicin in human epithelial carcinoma cells: Involvement of PKA. Cancer Lett. 2005, 224, 123–132. [Google Scholar] [CrossRef]
- Bat-Chen, W.; Golan, T.; Peri, I.; Ludmer, Z.; Schwartz, B. Allicin Purified From Fresh Garlic Cloves Induces Apoptosis in Colon Cancer Cells Via Nrf2. Nutr. Cancer 2010, 62, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Gülçin, I. Antioxidant Activity of Eugenol: A Structure–Activity Relationship Study. J. Med. Food 2011, 14, 975–985. [Google Scholar] [CrossRef] [PubMed]
- Barboza, J.N.; Da Silva Maia Bezerra Filho, C.; Silva, R.O.; Medeiros, J.V.R.; de Sousa, D.P. An Overview on the Anti-inflammatory Potential and Antioxidant Profile of Eugenol. Oxidative Med. Cell. Longev. 2018, 2018, 3957262. [Google Scholar] [CrossRef] [PubMed]
- Marchese, A.; Barbieri, R.; Coppo, E.; Orhan, I.E.; Daglia, M.; Nabavi, S.M.; Izadi, M.; Abdollahi, M.; Ajami, M. Antimicrobial activity of eugenol and essential oils containing eugenol: A mechanistic viewpoint. Crit. Rev. Microbiol. 2017, 43, 668–689. [Google Scholar] [CrossRef] [PubMed]
- Zari, A.T.; Zari, T.A.; Hakeem, K.R. Anticancer Properties of Eugenol: A Review. Molecules 2021, 26, 7407. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.; Brahmbhatt, K.; Priyani, A.; Ahmed, M.; Rizvi, T.A.; Sharma, C. Eugenol Enhances the Chemotherapeutic Potential of Gemcitabine and Induces Anticarcinogenic and Anti-inflammatory Activity in Human Cervical Cancer Cells. Cancer Biother. Radiopharm. 2011, 26, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Kaur, G.; Athar, M.; Alam, M.S. Eugenol precludes cutaneous chemical carcinogenesis in mouse by preventing oxidative stress and inflammation and by inducing apoptosis. Mol. Carcinog. 2009, 49, 290–301. [Google Scholar] [CrossRef]
- Vidhya, N.; Devaraj, S.N. Induction of apoptosis by eugenol in human breast cancer cells. J. Pharmacol. Exp. Ther. 2011, 49, 871–878. [Google Scholar]
- Pramod, K.; Ansari, S.H.; Ali, J. Eugenol: A Natural Compound with Versatile Pharmacological Actions. Nat. Prod. Commun. 2010, 5, 1999–2006. [Google Scholar] [CrossRef]
- Brodin, P.; Røed, A. Effects of eugenol on rat phrenic nerve and phrenic nerve-diaphragm preparations. Arch. Oral Biol. 1984, 29, 611–615. [Google Scholar] [CrossRef] [PubMed]
- Venkadeswaran, K.; Muralidharan, A.R.; Annadurai, T.; Ruban, V.V.; Sundararajan, M.; Anandhi, R.; Thomas, P.A.; Geraldine, P. Antihypercholesterolemic and Antioxidative Potential of an Extract of the Plant, Piper betle, and Its Active Constituent, Eugenol, in Triton WR-1339-Induced Hypercholesterolemia in Experimental Rats. Evid. -Based Complement. Altern. Med. 2014, 2014, 478973. [Google Scholar] [CrossRef]
- Khalil, A.A.; Rahman, U.U.; Khan, M.R.; Sahar, A.; Mehmood, T.; Khan, M. Essential oil eugenol: Sources, extraction techniques and nutraceutical perspectives. RSC Adv. 2017, 7, 32669–32681. [Google Scholar] [CrossRef]
- El-Kady, A.M.; Ahmad, A.A.; Hassan, T.M.; El-Deek, H.E.M.; Fouad, S.S.; Al-Thaqfan, S.S. Eugenol, a potential schistosomicidal agent with anti-inflammatory and antifibrotic effects against Schistosoma mansoni, induced liver pathology. Infect. Drug Resist. 2019, ume 12, 709–719. [Google Scholar] [CrossRef]
- Ueda-Nakamura, T.; Mendonça-Filho, R.R.; Morgado-Díaz, J.A.; Maza, P.K.; Filho, B.P.D.; Cortez, D.A.G.; Alviano, D.S.; Rosa, M.D.S.S.; Lopes, A.H.C.; Alviano, C.S.; et al. Antileishmanial activity of Eugenol-rich essential oil from Ocimum gratissimum. Parasitol. Int. 2005, 55, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.K.; Park, S.U.J. Recent insights into the biological functions of apigenin. Indian J. Exp. Biol. 2020, 19, 984–991. [Google Scholar]
- Lee, J.-H.; Zhou, H.Y.; Cho, S.Y.; Kim, Y.S.; Lee, Y.S.; Jeong, C.S. Anti-inflammatory mechanisms of apigenin: Inhibition of cyclooxygenase-2 expression, adhesion of monocytes to human umbilical vein endothelial cells, and expression of cellular adhesion molecules. Arch. Pharmacal Res. 2007, 30, 1318–1327. [Google Scholar] [CrossRef]
- Escande, C.; Nin, V.; Price, N.L.; Capellini, V.; Gomes, A.P.; Barbosa, M.T.; O’Neil, L.; White, T.A.; Sinclair, D.A.; Chini, E.N. Flavonoid apigenin is an inhibitor of the NAD+ ase CD38: Implications for cellular NAD+ metabolism, protein acetylation, and treatment of metabolic syndrome. Diabetes 2013, 62, 1084–1093. [Google Scholar] [CrossRef]
- Cardenas, H.; Arango, D.; Nicholas, C.; Duarte, S.; Nuovo, G.J.; He, W.; Voss, O.H.; Gonzalez-Mejia, M.E.; Guttridge, D.C.; Grotewold, E.; et al. Dietary apigenin exerts immune-regulatory activity in vivo by reducing NF-κB activity, halting leukocyte infiltration and restoring normal metabolic function. Int. J. Mol. Sci. 2016, 17, 323. [Google Scholar] [CrossRef]
- Kim, S.; Woo, E.-R.; Lee, D.G. Apigenin promotes antibacterial activity via regulation of nitric oxide and superoxide anion production. J. Basic Microbiol. 2020, 60, 862–872. [Google Scholar]
- Shibata, C.; Ohno, M.; Otsuka, M.; Kishikawa, T.; Goto, K.; Muroyama, R.; Kato, N.; Yoshikawa, T.; Takata, A.; Koike, K. The flavonoid apigenin inhibits hepatitis C virus replication by decreasing mature microRNA122 levels. Virology 2014, 462–463, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Qi, M.; Li, P.; Zhan, Y.; Shao, H. Apigenin in cancer therapy: Anti-cancer effects and mechanisms of action. Cell Biosci. 2017, 7, 50. [Google Scholar] [CrossRef] [PubMed]
- Ashrafizadeh, M.; Bakhoda, M.R.; Bahmanpour, Z.; Ilkhani, K.; Zarrabi, A.; Makvandi, P.; Khan, H.; Mazaheri, S.; Darvish, M.; Mirzaei, H. Apigenin as Tumor Suppressor in Cancers: Biotherapeutic Activity, Nanodelivery, and Mechanisms With Emphasis on Pancreatic Cancer. Front. Chem. 2020, 8, 829. [Google Scholar] [CrossRef] [PubMed]
- Osigwe, C.C.; Akah, P.A.; Nworu, C.S.; Okoye, F.B.C. Apigenin: A methanol fraction component of Newbouldia laevis leaf, as a potential antidiabetic agent. J. Phytopharm. 2017, 6, 38–44. [Google Scholar] [CrossRef]
- Kalra, S.; Mukherjee, J.J.; Venkataraman, S.; Bantwal, G.; Shaikh, S.; Saboo, B.; Das, A.K.; Ramachandran, A. Hypoglycemia: The neglected complication. Indian J. Endocrinol. Metab. 2013, 17, 819–834. [Google Scholar] [CrossRef]
- Cazarolli, L.H.; Folador, P.; Moresco, H.H.; Brighente, I.M.C.; Pizzolatti, M.G.; Silva, F.R.M.B. Mechanism of action of the stimulatory effect of apigenin-6-C-(2″-O-α-l-rhamnopyranosyl)-β-l-fucopyranoside on 14C-glucose uptake. Chem. Interact. 2009, 179, 407–412. [Google Scholar] [CrossRef]
- Balez, R.; Steiner, N.; Engel, M.; Sanz Muñoz, S.; Lum, J.S.; Wu, Y.; Wang, D.; Vallotton, P.; Sachdev, P.; O’Connor, M.; et al. Neuroprotective effects of apigenin against inflammation, neuronal excitability and apoptosis in an induced pluripotent stem cell model of Alzheimer’s disease. Sci. Rep. 2016, 6, 31450. [Google Scholar] [CrossRef]
- Ali, F.; Rahul; Naz, F.; Jyoti, S.; Siddique, Y.H. Health functionality of apigenin: A review. Int. J. Food Prop. 2017, 20, 1197–1238. [Google Scholar] [CrossRef]
- Imran, M.; Ghorat, F.; Ul-Haq, I.; Ur-Rehman, H.; Aslam, F.; Heydari, M.; Shariati, M.A.; Okuskhanova, E.; Yessimbekov, Z.; Thiruvengadam, M.; et al. Lycopene as a Natural Antioxidant Used to Prevent Human Health Disorders. Antioxidants 2020, 9, 706. [Google Scholar] [CrossRef]
- Campos, K.K.D.; Araújo, G.R.; Martins, T.L.; Bandeira, A.C.B.; Costa, G.D.P.; Talvani, A.; Garcia, C.C.M.; Oliveira, L.A.M.; Costa, D.C.; Bezerra, F.S. The antioxidant and anti-inflammatory properties of lycopene in mice lungs exposed to cigarette smoke. J. Nutr. Biochem. 2017, 48, 9–20. [Google Scholar] [CrossRef]
- Alshahrani, M.Y.; Ibrahim, E.H.; Asiri, M.; Kilany, M.; Alkhathami, A.G.; Chandramoorthy, H.C. Lycopene augments and enhances anti-oxidant/antibacterial efficiency of ethanolic leaf extract of Helianthus annuus over multidrug-resistant bacterial isolates. J. King Saud Univ. -Sci. 2022, 34, 102250. [Google Scholar] [CrossRef]
- Ono, M.; Takeshima, M.; Nakano, S. Mechanism of the Anticancer Effect of Lycopene (Tetraterpenoids). Enzymes 2015, 37, 139–166. [Google Scholar] [CrossRef] [PubMed]
- Islamian, J.P.; Mehrali, H. Lycopene as A Carotenoid Provides Radioprotectant and Antioxidant Effects by Quenching Radiation-Induced Free Radical Singlet Oxygen: An Overview. Cell J. 2015, 16, 386–391. [Google Scholar] [CrossRef]
- Jacques, P.F.; Lyass, A.; Massaro, J.M.; Vasan, R.S.; D’Agostino Sr, R.B. Relationship of lycopene intake and consumption of tomato products to incident CVD. Br. J. Nutr. 2013, 110, 545–551. [Google Scholar] [CrossRef]
- Chen, D.; Huang, C.; Chen, Z. A review for the pharmacological effect of lycopene in central nervous system disorders. Biomed. Pharmacother. 2019, 111, 791–801. [Google Scholar] [CrossRef]
- Kähkönen, M.P.; Heinonen, M. Antioxidant Activity of Anthocyanins and Their Aglycons. J. Agric. Food Chem. 2003, 51, 628–633. [Google Scholar] [CrossRef]
- Ma, Z.; Du, B.; Li, J.; Yang, Y.; Zhu, F. An Insight into Anti-Inflammatory Activities and Inflammation Related Diseases of Anthocyanins: A Review of Both In Vivo and In Vitro Investigations. Int. J. Mol. Sci. 2021, 22, 11076. [Google Scholar] [CrossRef]
- Cisowska, A.; Wojnicz, D.; Hendrich, A.B. Anthocyanins as Antimicrobial Agents of Natural Plant Origin. Nat. Prod. Commun. 2011, 6, 149–156. [Google Scholar] [CrossRef]
- Palungwachira, P.; Tancharoen, S.; Phruksaniyom, C.; Klungsaeng, S.; Srichan, R.; Kikuchi, K.; Nararatwanchai, T. Erratum to “Antioxidant and Anti-Inflammatory Properties of Anthocyanins Extracted from Oryza sativa L. in Primary Dermal Fibroblasts”. Oxidative Med. Cell. Longev. 2020, 2020, 1. [Google Scholar] [CrossRef]
- Fragoso, M.F.; Romualdo, G.R.; Vanderveer, L.A.; Franco-Barraza, J.; Cukierman, E.; Clapper, M.L.; Carvalho, R.F.; Barbisan, L.F. Lyophilized açaí pulp (Euterpe oleracea Mart) attenuates colitis-associated colon carcinogenesis while its main anthocyanin has the potential to affect the motility of colon cancer cells. Food Chem. Toxicol. 2018, 121, 237–245. [Google Scholar] [CrossRef]
- Qian, X.; Wang, X.; Luo, J.; Liu, Y.; Pang, J.; Zhang, H.; Xu, Z.; Xie, J.; Jiang, X.; Ling, W. Hypouricemic and nephroprotective roles of anthocyanins in hyperuricemic mice. Food Funct. 2019, 10, 867–878. [Google Scholar] [CrossRef] [PubMed]
- Aboonabi, A.; Singh, I.; Meyer, R.R. Cytoprotective effects of berry anthocyanins against induced oxidative stress and inflammation in primary human diabetic aortic endothelial cells. Chem. Interact. 2020, 317, 108940. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, R.; Francioso, A.; Mosca, L.; Silva, P. Anthocyanins: A Comprehensive Review of Their Chemical Properties and Health Effects on Cardiovascular and Neurodegenerative Diseases. Molecules 2020, 25, 3809. [Google Scholar] [CrossRef] [PubMed]
- Joshi, R.; Gangabhagirathi, R. Antioxidant activity of capsaicin on radiation-induced oxidation of murine hepatic mitochondrial membrane preparation. Res. Rep. Biochem. 2015, 5, 163–171. [Google Scholar] [CrossRef]
- Kim, C.-S.; Kawada, T.; Kim, B.-S.; Han, I.-S.; Choe, S.-Y.; Kurata, T.; Yu, R. Capsaicin exhibits anti-inflammatory property by inhibiting IkB-a degradation in LPS-stimulated peritoneal macrophages. Cell. Signal. 2002, 15, 299–306. [Google Scholar] [CrossRef]
- Füchtbauer, S.; Mousavi, S.; Bereswill, S.; Heimesaat, M.M. Antibacterial properties of capsaicin and its derivatives and their potential to fight antibiotic resistance—A literature survey. Eur. J. Microbiol. Immunol. 2021, 11, 10–17. [Google Scholar] [CrossRef]
- Veloso, J.; Prego, C.; Varela, M.M.; Carballeira, R.; Bernal, A.; Merino, F.; Díaz, J. Properties of capsaicinoids for the control of fungi and oomycetes pathogenic to pepper. Plant Biol. 2014, 16, 85–177. [Google Scholar] [CrossRef]
- Tang, K.; Zhang, X.; Guo, Y. Identification of the dietary supplement capsaicin as an inhibitor of Lassa virus entry. Acta Pharm. Sin. B 2020, 10, 789–798. [Google Scholar] [CrossRef]
- Clark, R.; Lee, S.-H. Anticancer Properties of Capsaicin Against Human Cancer. Anticancer Res. 2016, 36, 837–843. [Google Scholar]
- Fattori, V.; Hohmann, M.S.N.; Rossaneis, A.C.; Pinho-Ribeiro, F.A.; Verri, W.A. Capsaicin: Current understanding of its mechanisms and therapy of pain and other pre-clinical and clinical uses. Molecules 2016, 21, 844. [Google Scholar] [CrossRef]
- Holzer, P.; Lippe, I. Stimulation of afferent nerve endings by intragastric capsaicin protects against ethanol-induced damage of gastric mucosa. Neuroscience 1988, 27, 981–987. [Google Scholar] [CrossRef]
- Kawada, T.; Hagihara, K.-I.; Iwai, K. Effects of Capsaicin on Lipid Metabolism in Rats Fed a High Fat Diet. J. Nutr. 1986, 116, 1272–1278. [Google Scholar] [CrossRef] [PubMed]
- Andersen, H.H.; Marker, J.B.; Hoeck, E.A.; Elberling, J.; Arendt-Nielsen, L. Antipruritic effect of pretreatment with topical capsaicin 8% on histamine-and cowhage-evoked itch in healthy volunteers: A randomized, vehicle-controlled, proof-of-concept trial. Br. J. Dermatol. 2017, 177, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Caetano, B.F.R.; Tablas, M.B.; Pereira, N.E.F.; de Moura, N.A.; Carvalho, R.F.; Rodrigues, M.A.M.; Barbisan, L.F. Capsaicin reduces genotoxicity, colonic cell proliferation and preneoplastic lesions induced by 1,2-dimethylhydrazine in rats. Toxicol. Appl. Pharmacol. 2018, 338, 93–102. [Google Scholar] [CrossRef]
- Chrubasik, S.; Pittler, M.; Roufogalis, B. Zingiberis rhizoma: A comprehensive review on the ginger effect and efficacy profiles. Phytomedicine 2005, 12, 684–701. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-K.; Jang, H.-D. 6-shogaol attenuates H2O2-induced oxidative stress via upregulation of Nrf2-mediated γ-glutamylcysteine synthetase and heme oxygenase expression in HepG2 cells. Food Sci. Biotechnol. 2016, 25, 319–327. [Google Scholar] [CrossRef]
- Bak, M.-J.; Ok, S.; Jun, M.; Jeong, W.-S. 6-Shogaol-Rich Extract from Ginger Up-Regulates the Antioxidant Defense Systems in Cells and Mice. Molecules 2012, 17, 8037–8055. [Google Scholar] [CrossRef]
- Dugasani, S.; Pichika, M.R.; Nadarajah, V.D.; Balijepalli, M.K.; Tandra, S.; Korlakunta, J.N. Comparative antioxidant and anti-inflammatory effects of [6]-gingerol, [8]-gingerol, [10]-gingerol and [6]-shogaol. J. Ethnopharmacol. 2010, 127, 515–520. [Google Scholar] [CrossRef]
- Han, Q.; Yuan, Q.; Meng, X.; Huo, J.; Bao, Y.; Xie, G. 6-Shogaol attenuates LPS-induced inflammation in BV2 microglia cells by activating PPAR-γ. Oncotarget 2017, 8, 42001. [Google Scholar] [CrossRef]
- Chen, F.; Tang, Y.; Sun, Y.; Veeraraghavan, V.P.; Mohan, S.K.; Cui, C. 6-shogaol, a active constiuents of ginger prevents UVB radiation mediated inflammation and oxidative stress through modulating NrF2 signaling in human epidermal keratinocytes (HaCaT cells). J. Photochem. Photobiol. B Biol. 2019, 197, 111518. [Google Scholar] [CrossRef]
- Annamalai, G.; Suresh, K. [6]-Shogaol attenuates inflammation, cell proliferation via modulate NF-κB and AP-1 oncogenic signaling in 7, 12-dimethylbenz [a] anthracene induced oral carcinogenesis. Biomed. Pharmacother. 2018, 98, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Rampogu, S.; Baek, A.; Gajula, R.G.; Zeb, A.; Bavi, R.S.; Kumar, R.; Kim, Y.; Kwon, Y.J.; Lee, K.W. Ginger (Zingiber officinale) phytochemicals—Gingerenone-A and shogaol inhibit SaHPPK: Molecular docking, molecular dynamics simulations and in vitro approaches. Ann. Clin. Microbiol. Antimicrob. 2018, 17, 16. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Eom, Y. Antifungal and anti-biofilm effects of 6-shogaol against Candida auris. J. Appl. Microbiol. 2020, 130, 1142–1153. [Google Scholar] [CrossRef] [PubMed]
- Hayati, R.F.; Better, C.D.; Denis, D.; Komarudin, A.G.; Bowolaksono, A.; Yohan, B.; Sasmono, R.T. [6]-Gingerol Inhibits Chikungunya Virus Infection by Suppressing Viral Replication. BioMed Res. Int. 2021, 2021, 6623400. [Google Scholar] [CrossRef] [PubMed]
- Zadorozhna, M.; Mangieri, D. Mechanisms of chemopreventive and therapeutic proprieties of ginger extracts in cancer. Int. J. Mol. Sci. 2021, 22, 6599. [Google Scholar] [CrossRef]
- Khaki, A.; Fathiazad, F.; Nouri, M.; Afshin Khaki, A.; Ozanci, C.C.; Ghafari-Novin, M.; Hamadeh, M. The effects of Ginger on spermatogenesis and sperm parameters of rat. Int. J. Reprod. BioMed. 2009, 7, 7. [Google Scholar] [CrossRef]
- Smith, M.R.; Gangireddy, S.R.; Narala, V.R.; Hogaboam, C.M.; Standiford, T.J.; Christensen, P.J.; Kondapi, A.K.; Reddy, R.C. Curcumin inhibits fibrosis-related effects in IPF fibroblasts and in mice following bleomycin-induced lung injury. Am. J. Physiol. Cell. Mol. Physiol. 2010, 298, L616–L625. [Google Scholar] [CrossRef]
- Stanić, Z. Curcumin, a Compound from Natural Sources, a True Scientific Challenge—A Review. Plant Foods Hum. Nutr. 2017, 72, 1–12. [Google Scholar] [CrossRef]
- López-Malo, D.; Villarón-Casares, C.A.; Alarcón-Jiménez, J.; Miranda, M.; Díaz-Llopis, M.; Romero, F.J.; Villar, V.M. Curcumin as a Therapeutic Option in Retinal Diseases. Antioxidants 2020, 9, 48. [Google Scholar] [CrossRef]
- Rainey, N.E.; Moustapha, A.; Petit, P.X. Curcumin, a Multifaceted Hormetic Agent, Mediates an Intricate Crosstalk between Mitochondrial Turnover, Autophagy, and Apoptosis. Oxidative Med. Cell. Longev. 2020, 2020, 3656419. [Google Scholar] [CrossRef]
- De, R.; Kundu, P.; Swarnakar, S.; Ramamurthy, T.; Chowdhury, A.; Nair, G.B.; Mukhopadhyay, A.K. Antimicrobial Activity of Curcumin against Helicobacter pylori Isolates from India and during Infections in Mice. Antimicrob. Agents Chemother. 2009, 53, 1592–1597. [Google Scholar] [CrossRef] [PubMed]
- Reddy, P.J.; Sinha, S.; Ray, S.; Sathe, G.J.; Chatterjee, A.; Prasad, T.K.; Dhali, S.; Srikanth, R.; Panda, D.; Srivastava, S. Comprehensive analysis of temporal alterations in cellular proteome of Bacillus subtilis under curcumin treatment. PLoS ONE 2015, 10, e0120620. [Google Scholar] [CrossRef]
- Sharma, O. Antioxidant activity of curcumin and related compounds. Biochem. Pharmacol. 1976, 25, 1811–1812. [Google Scholar] [CrossRef] [PubMed]
- Ragunathan, I.; Panneerselvam, N. Antimutagenic potential of curcumin on chromosomal aberrations in Allium cepa. J. Zhejiang Univ. Sci. B 2007, 8, 470–475. [Google Scholar] [CrossRef][Green Version]
- Sun, D.; Zhuang, X.; Xiang, X.; Liu, Y.; Zhang, S.; Liu, C.; Barnes, S.; Grizzle, W.; Miller, D.; Zhang, H.-G. A Novel Nanoparticle Drug Delivery System: The Anti-inflammatory Activity of Curcumin Is Enhanced When Encapsulated in Exosomes. Mol. Ther. 2010, 18, 1606–1614. [Google Scholar] [CrossRef]
- Hatcher, H.; Planalp, R.; Cho, J.; Torti, F.M.; Torti, S.V. Curcumin: From ancient medicine to current clinical trials. Cell Mol. Life Sci. 2008, 65, 1631–1652. [Google Scholar] [CrossRef]
- Ronis, M.J.J. Effects of soy containing diet and isoflavones on cytochrome P450 enzyme expression and activity. Drug Metab. Rev. 2016, 48, 331–341. [Google Scholar] [CrossRef]
- Dixon, R.A.; Ferreira, D. Genistein. Phytochemistry 2002, 60, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Sak, K. Current epidemiological knowledge about the role of flavonoids in prostate carcinogenesis. Exp. Oncol. 2017, 39, 98–105. [Google Scholar] [CrossRef]
- Kim, I.-S. Current Perspectives on the Beneficial Effects of Soybean Isoflavones and Their Metabolites for Humans. Antioxidants 2021, 10, 1064. [Google Scholar] [CrossRef]
- Ganai, A.A.; Farooqi, H. Bioactivity of genistein: A review of in vitro and in vivo studies. Biomed. Pharmacother. 2015, 76, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Uifălean, A.; Schneider, S.; Ionescu, C.; Lalk, M.; Iuga, C.A. Soy Isoflavones and Breast Cancer Cell Lines: Molecular Mechanisms and Future Perspectives. Molecules 2015, 21, 13. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Kim, C.-W.; Jeon, S.-Y.; Go, R.-E.; Hwang, K.-A.; Choi, K.-C. Chemopreventive and chemotherapeutic effects of genistein, a soy isoflavone, upon cancer development and progression in preclinical animal models. Lab. Anim. Res. 2014, 30, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Malloy, K.M.; Wang, J.; Clark, L.H.; Fang, Z.; Sun, W.; Yin, Y.; Kong, W.; Zhou, C.; Bae-Jump, V.L. Novasoy and genistein inhibit endometrial cancer cell proliferation through disruption of the AKT/mTOR and MAPK signaling pathways. Am. J. Transl. Res. 2018, 10, 784–795. [Google Scholar] [PubMed]
- Yu, Y.; Xing, Y.; Zhang, Q.; Zhang, Q.; Huang, S.; Li, X.; Gao, C. Soy isoflavone genistein inhibits hsa_circ_0031250/miR -873-5p/FOXM1 axis to suppress non-small-cell lung cancer progression. IUBMB Life 2020, 73, 92–107. [Google Scholar] [CrossRef] [PubMed]
- Alorda-Clara, M.; Torrens-Mas, M.; Morla-Barcelo, P.M.; Roca, P.; Sastre-Serra, J.; Pons, D.G.; Oliver, J. High Concentrations of Genistein Decrease Cell Viability Depending on Oxidative Stress and Inflammation in Colon Cancer Cell Lines. Int. J. Mol. Sci. 2022, 23, 7526. [Google Scholar] [CrossRef]
- Nie, Z.-Y.; Zhao, M.-H.; Cheng, B.-Q.; Pan, R.-F.; Wang, T.-R.; Qin, Y.; Zhang, X.-J. Tanshinone IIA regulates human AML cell proliferation, cell cycle, and apoptosis through miR-497-5p/AKT3 axis. Cancer Cell Int. 2020, 20, 379. [Google Scholar] [CrossRef]
- Liu, Z.; Zhu, W.; Kong, X.; Chen, X.; Sun, X.; Zhang, W.; Zhang, R. Tanshinone IIA inhibits glucose metabolism leading to apoptosis in cervical cancer. Oncol. Rep. 2019, 42, 1893–1903. [Google Scholar] [CrossRef]
- Curtis, H.; Noll, U.; Störmann, J.; Slusarenko, A.J. Broad-spectrum activity of the volatile phytoanticipin allicin in extracts of garlic (Allium sativum L.) against plant pathogenic bacteria, fungi and Oomycetes. Physiol. Mol. Plant Pathol. 2004, 65, 79–89. [Google Scholar] [CrossRef]
- Gruhlke, M.C.; Nwachwukwu, I.; Arbach, M.; Anwar, A.; Noll, U.; Slusarenko, A.J. Allicin from garlic, effective in controlling several plant diseases, is a reactive sulfur species (RSS) that pushes cells into apoptosis. In Proceedings of the Modern Fungicides and Antifungal Compounds VI, 16th International Reinhardsbrunn Symposium, Friedrichroda, Germany, 25–29 April 2010; pp. 325–330. [Google Scholar]
- Ried, K.; Toben, C.; Fakler, P. Effect of garlic on serum lipids: An updated meta-analysis. Nutr. Rev. 2013, 71, 282–299. [Google Scholar] [CrossRef]
- Warshafsky, S.; Kamer, R.S.; Sivak, S.L. Effect of garlic on total serum cholesterol. A meta-analysis. Ann. Intern. Med. 1993, 119, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Focke, M.; Feld, A.; Lichtenthaler, H.K. Allicin, a naturally occurring antibiotic from garlic, specifically inhibits acetyl-CoA synthetase. FEBS Lett. 1990, 261, 106–108. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Porter, T.D. Garlic and garlic-derived compounds inhibit human squalene monooxygenase. J. Nutr. 2001, 131, 1662–1667. [Google Scholar] [CrossRef] [PubMed]
- Barceloux, D.G. Medical Toxicology of Natural Substances: Foods, Fungi, Medicinal Herbs, Plants, and Venomous Animals; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2008. [Google Scholar]
- Basch, E.; Gasparyan, A.; Giese, N.; Hashmi, S.; Miranda, M.; Sollars, D.; Seamon, E.; Tanguay-Colucci, S.; Ulbricht, C.; Varghese, M.; et al. Clove (Eugenia aromatica) and clove oil (eugenol). Natural standard monograph (www. naturalstandard. com) copyright© 2008. J. Diet Suppl. 2008, 5, 117–146. [Google Scholar] [CrossRef]
- Leite, A.M.; Lima, E.D.O.; Souza, E.L.D.; Diniz, M.D.F.F.M.; Trajano, V.N.; de Medeiros, I.A. Inhibitory effect of beta-pinene, alpha-pinene and eugenol on the growth of potential infectious endocarditis causing Gram-positive bacteria. Rev. Bras. Cienc. Farm. 2007, 43, 121–126. [Google Scholar] [CrossRef]
- Ali, S.M.; A Khan, A.; Ahmed, I.; Musaddiq, M.; Ahmed, K.S.; Polasa, H.; Rao, L.V.; Habibullah, C.M.; A Sechi, L.; Ahmed, N. Antimicrobial activities of Eugenol and Cinnamaldehyde against the human gastric pathogen Helicobacter pylori. Ann. Clin. Microbiol. Antimicrob. 2005, 4, 20. [Google Scholar] [CrossRef]
- Leem, H.-H.; Kim, E.-O.; Seo, M.-J.; Choi, S.-W. Antioxidant and Anti-Inflammatory Activities of Eugenol and Its Derivatives from Clove (Eugenia caryophyllata Thunb.). J. Korean Soc. Food Sci. Nutr. 2011, 40, 1361–1370. [Google Scholar] [CrossRef]
- Kabuto, H.; Yamanushi, T.T. Effects of zingerone [4-(4-hydroxy-3-methoxyphenyl)-2-butanone] and eugenol [2-methoxy-4-(2-propenyl) phenol] on the pathological progress in the 6-hydroxydopamine-induced parkinson’s disease mouse model. Neurochem. Res. 2011, 36, 2244–2249. [Google Scholar] [CrossRef]
- Harikumar, K.B.; Kunnumakkara, A.B.; Sethi, G.; Diagaradjane, P.; Anand, P.; Pandey, M.K.; Gelovani, J.; Krishnan, S.; Guha, S.; Aggarwal, B.B. Resveratrol, a multitargeted agent, can enhance antitumor activity of gemcitabine in vitro and in orthotopic mouse model of human pancreatic cancer. Int. J. Cancer 2010, 127, 257–268. [Google Scholar]
- Hume, W. Effect of Eugenol on Constrictor Responses in Blood Vessels of the Rabbit Ear. J. Dent. Res. 1983, 62, 1013–1015. [Google Scholar] [CrossRef]
- Markowitz, K.; Moynihan, M.; Liu, M.; Kim, S. Biologic properties of eugenol and zinc oxide-eugenol: A clinically oriented review. Oral Surg. Oral Med. Oral Pathol. 1992, 73, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Bhagwat, S.; Haytowitz, D.B.; Holden, J.M. USDA Database for the Flavonoid Content of Selected Foods. J.U.D.o.A.B Release 3. Volume 159. 2011. Available online: https://www.ars.usda.gov/ARSUserFiles/80400525/data/flav/flav_r03.pdf (accessed on 8 September 2022).
- Jack, C.R., Jr.; Bennett, D.A.; Blennow, K.; Carrillo, M.C.; Dunn, B.; Haeberlein, S.B.; Holtzman, D.M.; Jagust, W.; Jessen, F.; Karlawish, J.J.; et al. NIA-AA research framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018, 14, 535–562. [Google Scholar] [CrossRef]
- Takagaki, N.; Sowa, Y.; Oki, T.; Nakanishi, R.; Yogosawa, S.; Sakai, T. Apigenin induces cell cycle arrest and p21/WAF1 expression in a p53-independent pathway. Int. J. Oncol. 2005, 26, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Maggioni, D.; Garavello, W.; Rigolio, R.; Pignataro, L.; Gaini, R.; Nicolini, G. Apigenin impairs oral squamous cell carcinoma growth in vitro inducing cell cycle arrest and apoptosis. Int. J. Oncol. 2013, 43, 1675–1682. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Dia, V.P.; Baek, S.J.; Zhong, Q. Nanoencapsulation of apigenin with whey protein isolate: Physicochemical properties, in vitro activity against colorectal cancer cells, and bioavailability. LWT 2021, 154, 112751. [Google Scholar] [CrossRef]
- Seo, H.-S.; Jo, J.K.; Ku, J.M.; Choi, H.-S.; Choi, Y.K.; Woo, J.-K.; Kim, H.I.; Kang, S.-Y.; Lee, K.M.; Nam, K.W.; et al. Induction of caspase-dependent extrinsic apoptosis by apigenin through inhibition of signal transducer and activator of transcription 3 (STAT3) signalling in HER2-overexpressing BT-474 breast cancer cells. Biosci. Rep. 2015, 35, e00276. [Google Scholar] [CrossRef]
- Kashyap, D.; Sharma, A.; Tuli, H.S.; Sak, K.; Garg, V.K.; Buttar, H.S.; Setzer, W.N.; Sethi, G. Apigenin: A natural bioactive flavone-type molecule with promising therapeutic function. J. Funct. Foods 2018, 48, 457–471. [Google Scholar] [CrossRef]
- Seo, H.-S.; Ku, J.M.; Choi, H.-S.; Woo, J.-K.; Jang, B.-H.; Shin, Y.C.; Ko, S.-G. Induction of caspase-dependent apoptosis by apigenin by inhibiting STAT3 signaling in HER2-overexpressing MDA-MB-453 breast cancer cells. Anticancer Res. 2014, 34, 2869–2882. [Google Scholar]
- Choudhari, S.M.; Ananthanarayan, L. Enzyme aided extraction of lycopene from tomato tissues. Food Chem. 2007, 102, 77–81. [Google Scholar] [CrossRef]
- Li, N.; Wu, X.; Zhuang, W.; Xia, L.; Chen, Y.; Wu, C.; Rao, Z.; Du, L.; Zhao, R.; Yi, M.; et al. Tomato and lycopene and multiple health outcomes: Umbrella review. Food Chem. 2020, 343, 128396. [Google Scholar] [CrossRef]
- Durairajanayagam, D.; Agarwal, A.; Ong, C.; Prashast, P. Lycopene and male infertility. Asian J. Androl. 2014, 16, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Rao, A.V. Tomato lycopene and low density lipoprotein oxidation: A human dietary intervention study. Lipids 1998, 33, 981–984. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Rao, A.V. Tomato lycopene and its role in human health and chronic diseases. Can. Med. Assoc. J. 2000, 163, 739–744. [Google Scholar]
- Zou, J.; Feng, D.; Ling, W.-H.; Duan, R.-D. Lycopene suppresses proinflammatory response in lipopolysaccharide-stimulated macrophages by inhibiting ROS-induced trafficking of TLR4 to lipid raft-like domains. J. Nutr. Biochem. 2013, 24, 1117–1122. [Google Scholar] [CrossRef] [PubMed]
- Göncü, T.; Oğuz, E.; Sezen, H.; Koçarslan, S.; Oğuz, H.; Akal, A.; Adıbelli, F.M.; Çakmak, S.; Aksoy, N. Anti-inflammatory effect of lycopene on endotoxin-induced uveitis in rats. Arq. Bras. Oftalmol. 2016, 79, 357–362. [Google Scholar] [CrossRef]
- Moia, V.M.; Portilho, F.L.; Pádua, T.A.; Corrêa, L.B.; Ricci-Junior, E.; Rosas, E.C.; Alencar, L.M.R.; Sinfronio, F.S.M.; Sampson, A.; Iram, S.H.; et al. Lycopene used as Anti-inflammatory Nanodrug for the Treatment of Rheumathoid Arthritis: Animal assay, Pharmacokinetics, ABC Transporter and Tissue Deposition. Colloids Surf. B Biointerfaces 2020, 188, 110814. [Google Scholar] [CrossRef]
- Thies, F.; Masson, L.F.; Rudd, A.; Vaughan, N.; Tsang, C.; Brittenden, J.; Simpson, W.G.; Duthie, S.; Horgan, G.W.; Duthie, G. Effect of a tomato-rich diet on markers of cardiovascular disease risk in moderately overweight, disease-free, middle-aged adults: A randomized controlled trial. Am. J. Clin. Nutr. 2012, 95, 1013–1022. [Google Scholar] [CrossRef]
- Kelkel, M.; Schumacher, M.; Dicato, M.; Diederich, M. Antioxidant and anti-proliferative properties of lycopene. Free. Radic. Res. 2011, 45, 925–940. [Google Scholar] [CrossRef]
- Riaz, M.; Zia-Ul-Haq, M.; Saad, B. Anthocyanins and Human Health: Biomolecular and Therapeutic Aspects; Springer: Berlin/Heidelberg, Germany, 2016; Volume 10. [Google Scholar]
- Mazza, G.; Miniati, E. Anthocyanins in Fruits, Vegetables, and Grains; CRC Press: Boca Raton, FL, USA, 2018. [Google Scholar]
- de Pascual-Teresa, S.; Moreno, D.A.; García-Viguera, C. Flavanols and anthocyanins in cardiovascular health: A review of current evidence. Int. J. Mol. Sci. 2010, 11, 1679–1703. [Google Scholar] [CrossRef]
- Wang, L.S.; Kuo, C.T.; Peiffer, D.; Seguin, C.; Stoner, K.; Huang, Y.W.; Huang, T.H.; Salzman, N.; Liu, Z.; Rosenberg, D. Anthocyanins, anthocyanin derivatives, and colorectal cancer. In Anthocyanins in Health and Disease; CRC Press: Boca Raton, FL, USA, 2013; pp. 225–243. [Google Scholar]
- Pour, P.M.; Fakhri, S.; Asgary, S.; Farzaei, M.H.; Echeverría, J. The Signaling Pathways, and Therapeutic Targets of Antiviral Agents: Focusing on the Antiviral Approaches and Clinical Perspectives of Anthocyanins in the Management of Viral Diseases. Front. Pharmacol. 2019, 10, 1207. [Google Scholar] [CrossRef]
- Rice-Evans, C.; Miller, N.; Paganga, G. Antioxidant properties of phenolic compounds. Trends Plant Sci. 1997, 2, 152–159. [Google Scholar] [CrossRef]
- Jomova, K.; Valko, M. Advances in metal-induced oxidative stress and human disease. Toxicology 2011, 283, 65–87. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, T.; Horio, F.; Osawa, T. Cyanidin 3-O-β-D-glucoside suppresses nitric oxide production during a zymosan treatment in rats. J. Nutr. Sci. Vitaminol. 2002, 48, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Polychronopoulos, P.; Magiatis, P.; Skaltsounis, A.; Myrianthopoulos, V.; Mikros, E.; Tarricone, A.; Musacchio, A.; Roe, S.; Pearl, L.; Leost, M.J.; et al. Anthocyanin-rich acai (Euterpe oleracea Mart.) fruit pulp fractions attenuate inflammatory stress signaling in mouse brain BV-2 microglial cells. J. Agric. Food Chem. 2004, 47, 1084–1093. [Google Scholar]
- Medda, R.; Lyros, O.; Schmidt, J.L.; Jovanovic, N.; Nie, L.; Link, B.J.; Otterson, M.F.; Stoner, G.D.; Shaker, R.; Rafiee, P. Anti inflammatory and anti angiogenic effect of black raspberry extract on human esophageal and intestinal microvascular endothelial cells. Microvasc. Res. 2015, 97, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-S.; Choi, M.-A.; Kim, B.-S.; Han, I.-S.; Kurata, T.; Yu, R. Capsaicin protects against ethanol-induced oxidative injury in the gastric mucosa of rats. Life Sci. 2000, 67, 3087–3093. [Google Scholar] [CrossRef]
- Amna, T.; Hwang, I.; Shang, K.; Amina, M.; Al-Musayeib, N.M.; Al-Deyab, S.S. Influence of capsaicin on inflammatory cytokines induced by lipopolysaccharide in myoblast cells under in vitro environment. Pharmacogn. Mag. 2017, 13, S26–S32. [Google Scholar] [CrossRef]
- Gram, D.X.; Hansen, A.J.; Wilken, M.; Elm, T.; Svendsen, O.; Carr, R.D.; Ahrén, B.; Brand, C.L. Plasma calcitonin gene-related peptide is increased prior to obesity, and sensory nerve desensitization by capsaicin improves oral glucose tolerance in obese Zucker rats. Eur. J. Endocrinol. 2005, 153, 963–969. [Google Scholar] [CrossRef]
- Chen, H.Y.; Lee, Y.H.; Chen, H.Y.; Yeh, C.A.; Chueh, P.J.; Lin, Y.-M.J. Capsaicin Inhibited Aggressive Phenotypes through Downregulation of Tumor-Associated NADH Oxidase (tNOX) by POU Domain Transcription Factor POU3F2. Molecules 2016, 21, 733. [Google Scholar] [CrossRef]
- Meral, O.; Alpay, M.; Kismali, G.; Kosova, F.; Cakir, D.U.; Pekcan, M.; Yigit, S.; Sel, T. Capsaicin inhibits cell proliferation by cytochrome c release in gastric cancer cells. Tumor Biol. 2014, 35, 6485–6492. [Google Scholar] [CrossRef]
- Amantini, C.; Mosca, M.; Nabissi, M.; Lucciarini, R.; Caprodossi, S.; Arcella, A.; Giangaspero, F.; Santoni, G. Capsaicin-induced apoptosis of glioma cells is mediated by TRPV1 vanilloid receptor and requires p38 MAPK activation. J. Neurochem. 2007, 102, 977–990. [Google Scholar] [CrossRef] [PubMed]
- Backonja, M.M.; Malan, T.P.; Vanhove, G.F.; Tobias, J. NGX-4010, a High-Concentration Capsaicin Patch, for the Treatment of Postherpetic Neuralgia: A Randomized, Double-Blind, Controlled Study with an Open-Label Extension. Pain Med. 2010, 11, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Tesfaye, S. Advances in the management of diabetic peripheral neuropathy. Curr. Opin. Support. Palliat. Care 2009, 3, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Hoeks, M.; Bagguley, T.; van Marrewijk, C.; Smith, A.; Bowen, D.; Culligan, D.; Kolade, S.; Symeonidis, A.; Garelius, H.; Spanoudakis, M.; et al. Toxic iron species in lower-risk myelodysplastic syndrome patients: Course of disease and effects on outcome. Leukemia 2020, 35, 1745–1750. [Google Scholar] [CrossRef]
- Kim, E.-C.; Min, J.-K.; Kim, T.-Y.; Lee, S.-J.; Yang, H.-O.; Han, S.; Kim, Y.-M.; Kwon, Y.-G. [6]-Gingerol, a pungent ingredient of ginger, inhibits angiogenesis in vitro and in vivo. Biochem. Biophys. Res. Commun. 2005, 335, 300–308. [Google Scholar] [CrossRef]
- Schirle, M.; Bantscheff, M.; Kuster, B. Mass Spectrometry-Based Proteomics in Preclinical Drug Discovery. Chem. Biol. 2012, 19, 72–84. [Google Scholar] [CrossRef]
- Thomford, N.E.; Senthebane, D.A.; Rowe, A.; Munro, D.; Seele, P.; Maroyi, A.; Dzobo, K. Natural Products for Drug Discovery in the 21st Century: Innovations for Novel Drug Discovery. Int. J. Mol. Sci. 2018, 19, 1578. [Google Scholar] [CrossRef]
- Rix, U.; Superti-Furga, G. Target profiling of small molecules by chemical proteomics. Nat. Chem. Biol. 2009, 5, 616–624. [Google Scholar] [CrossRef]
- Aslam, B.; Basit, M.; Nisar, M.A.; Khurshid, M.; Rasool, M.H. Proteomics: Technologies and Their Applications. J. Chromatogr. Sci. 2017, 55, 182–196. [Google Scholar] [CrossRef]
- de Souza, L.P.; Alseekh, S.; Scossa, F.; Fernie, A.R. Ultra-high-performance liquid chromatography high-resolution mass spectrometry variants for metabolomics research. Nat. Methods 2021, 18, 733–746. [Google Scholar] [CrossRef]
- Chanukuppa, V.; Taware, R.; Chatterjee, T.; Sharma, S.; More, T.H.; Taunk, K.; Kumar, S.; Santra, M.K.; Rapole, S. Current Understanding of the Potential of Proteomics and Metabolomics Approaches in Cancer Chemoresistance: A Focus on Multiple Myeloma. Curr. Top. Med. Chem. 2019, 18, 2584–2598. [Google Scholar] [CrossRef] [PubMed]
- Beck, M.; Claassen, M.; Aebersold, R. Comprehensive proteomics. Curr. Opin. Biotechnol. 2011, 22, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Domon, B.; Aebersold, R. Mass Spectrometry and Protein Analysis. Science 2006, 312, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Shlar, I.; Droby, S.; Rodov, V. Modes of antibacterial action of curcumin under dark and light conditions: A toxicoproteomics approach. J. Proteom. 2017, 160, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.; Cheng, Y.; Lai, M.; Hu, A. Identification of carbonylated proteins in a bactericidal process induced by curcumin with blue light irradiation on imipenem-resistant Acinetobacter baumannii. Rapid Commun. Mass Spectrom. 2019, 34, e8548. [Google Scholar] [CrossRef]
- Chen, J.; Li, L.; Su, J.; Li, B.; Zhang, X.; Chen, T. Proteomic analysis of G2/M arrest triggered by natural borneol/curcumin in HepG2 cells, the importance of the reactive oxygen species-p53 pathway. J. Agric. Food Chem. 2015, 63, 6440–6449. [Google Scholar] [CrossRef]
- Jain, R.; Kulkarni, P.; Dhali, S.; Rapole, S.; Srivastava, S. Quantitative proteomic analysis of global effect of LLL12 on U87 cell’s proteome: An insight into the molecular mechanism of LLL12. J. Proteom. 2015, 113, 127–142. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, J.; Zhang, C.-J.; Wong, Y.K.; Lim, T.K.; Hua, Z.-C.; Liu, B.; Tannenbaum, S.R.; Shen, H.-M.; Lin, Q. In situ Proteomic Profiling of Curcumin Targets in HCT116 Colon Cancer Cell Line. Sci. Rep. 2016, 6, 22146. [Google Scholar] [CrossRef]
- Pisano, M.; Palomba, A.; Tanca, A.; Pagnozzi, D.; Uzzau, S.; Addis, M.F.; Dettori, M.A.; Fabbri, D.; Palmieri, G.; Rozzo, C. Protein expression changes induced in a malignant melanoma cell line by the curcumin analogue compound D6. BMC Cancer 2016, 16, 317. [Google Scholar] [CrossRef]
- Chen, J.; Cao, X.; Qin, X.; Liu, H.; Chen, S.; Zhong, S.; Li, Y. Proteomic analysis of the molecular mechanism of curcumin/β-cyclodextrin polymer inclusion complex inhibiting HepG2 cells growth. J. Food Biochem. 2019, 44, e13119. [Google Scholar] [CrossRef]
- Luo, J.; Yang, J.; Yu, B.-Y.; Liu, W.; Li, M.; Zhuang, S.-M. Identification of Siah-interacting protein as a potential regulator of apoptosis and curcumin resistance. Oncogene 2010, 29, 6357–6366. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Liu, Y.-Z.; Zhang, F.; Wang, H.-S.; Zhang, G.; Zhou, B.-H.; Zuo, Y.-L.; Cai, S.-H.; Bu, X.-Z.; Du, J. Identification of potential pathways involved in the induction of cell cycle arrest and apoptosis by a new 4-arylidene curcumin analogue T63 in lung cancer cells: A comparative proteomic analysis. Mol. BioSyst. 2014, 10, 1320–1331. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.-J.; Chen, X.-W.; Wang, J.-Z.; Ju, Y.-L.; Ou Yang, M.-Z.; Zhang, W.-J. Proteomic analysis identifies proteins associated with curcumin-enhancing efficacy of irinotecan-induced apoptosis of colorectal cancer LOVO cell. Int. J. Clin. Exp. Pathol. 2014, 7, 1–15. [Google Scholar] [PubMed]
- Lee, J.-G.; McKinney, K.Q.; Pavlopoulos, A.J.; Park, J.-H.; Hwang, S. Identification of anti-metastatic drug and natural compound targets in isogenic colorectal cancer cells. J. Proteom. 2015, 113, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Li, L. Relationship of GSTP1 lower expression and multidrug resistance reversing of curcumin on human colon carcinoma cells. Zhonghua Yi Xue Za Zhi 2015, 95, 2478–2482. [Google Scholar]
- Sato, T.; Higuchi, Y.; Shibagaki, Y.; Hattori, S. Phosphoproteomic Analysis Identifies Signaling Pathways Regulated by Curcumin in Human Colon Cancer Cells. Anticancer Res. 2017, 37, 4789–4798. [Google Scholar] [CrossRef]
- Cai, X.; Huang, W.; Qiao, Y.; Du, S.; Chen, Y.; Chen, D.; Yu, S.; Che, R.; Liu, N.; Jiang, Y. Inhibitory effects of curcumin on gastric cancer cells: A proteomic study of molecular targets. Phytomedicine 2013, 20, 495–505. [Google Scholar] [CrossRef]
- Maioli, E.; Torricelli, C.; Valacchi, G. Rottlerin and curcumin: A comparative analysis. Ann. N. Y. Acad. Sci. 2012, 1259, 65–76. [Google Scholar] [CrossRef]
- Kreutz, D.; Sinthuvanich, C.; Bileck, A.; Janker, L.; Muqaku, B.; Slany, A.; Gerner, C. Curcumin exerts its antitumor effects in a context dependent fashion. J. Proteom. 2018, 182, 65–72. [Google Scholar] [CrossRef]
- Mittal, L.; Aryal, U.K.; Camarillo, I.G.; Raman, V.; Sundararajan, R. Effective electrochemotherapy with curcumin in MDA-MB-231-human, triple negative breast cancer cells: A global proteomics study. Bioelectrochemistry 2019, 131, 107350. [Google Scholar] [CrossRef]
- Sathe, G.; Pinto, S.M.; Syed, N.; Nanjappa, V.; Solanki, H.S.; Renuse, S.; Chavan, S.; Khan, A.A.; Patil, A.H.; Nirujogi, R.S.; et al. Phosphotyrosine profiling of curcumin-induced signaling. Clin. Proteom. 2016, 13, 13. [Google Scholar] [CrossRef] [PubMed]
- Taverna, S.; Fontana, S.; Monteleone, F.; Pucci, M.; Saieva, L.; De Caro, V.; Cardinale, V.G.; Giallombardo, M.; Vicario, E.; Rolfo, C.; et al. Curcumin modulates chronic myelogenous leukemia exosomes composition and affects angiogenic phenotype via exosomal miR-21. Oncotarget 2016, 7, 30420. [Google Scholar] [CrossRef] [PubMed]
- Monteleone, F.; Taverna, S.; Alessandro, R.; Fontana, S. SWATH-MS based quantitative proteomics analysis reveals that curcumin alters the metabolic enzyme profile of CML cells by affecting the activity of miR-22/IPO7/HIF-1α axis. J. Exp. Clin. Cancer Res. 2018, 37, 170. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; Lin, T.; Wo, X.; Wang, P.; Zhou, Y.; Yang, Z. Proteomic research on anti-atherosclerosis mechanism of curcumin in RAW264.7. China J. Chin. Mater. Medica 2011, 36, 1207–1211. [Google Scholar]
- Kim, S.W.; Choi, J.H.; Mukherjee, R.; Hwang, K.-C.; Yun, J.W. Proteomic identification of fat-browning markers in cultured white adipocytes treated with curcumin. Mol. Cell. Biochem. 2016, 415, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Gouda, M.M.; Rex, D.A.B.; Es, S.P.; Modi, P.K.; Chanderasekaran, J.; Bhandary, Y.P. Proteomics Analysis Revealed the Importance of Inflammation-Mediated Downstream Pathways and the Protective Role of Curcumin in Bleomycin-Induced Pulmonary Fibrosis in C57BL/6 Mice. J. Proteome Res. 2020, 19, 2950–2963. [Google Scholar] [CrossRef] [PubMed]
- D’Aguanno, S.; D’Agnano, I.; De Canio, M.; Rossi, C.; Bernardini, S.; Federici, G.; Urbani, A. Shotgun proteomics and network analysis of neuroblastoma cell lines treated with curcumin. Mol. Biosyst. 2012, 8, 1068–1077. [Google Scholar] [CrossRef]
- Hu, Y.-H.; Huang, X.-R.; Qi, M.-X.; Hou, B.-Y. Curcumin inhibits proliferation of human lens epithelial cells: A proteomic analysis. J. Zhejiang Univ. B 2012, 13, 402–407. [Google Scholar] [CrossRef]
- Asher, G.N.; Fallon, J.K.; Smith, P.C. UGT concentrations in human rectal tissue after multidose, oral curcumin. Pharmacol. Res. Perspect. 2016, 4, e00222. [Google Scholar] [CrossRef]
- Lee, D.E.; Lee, S.J.; Kim, S.J.; Lee, H.-S.; Kwon, O.-S. Curcumin ameliorates nonalcoholic fatty liver disease through inhibition of O-GlcNAcylation. Nutrients 2019, 11, 2702. [Google Scholar] [CrossRef]
- Khoontawad, J.; Intuyod, K.; Rucksaken, R.; Hongsrichan, N.; Pairojkul, C.; Pinlaor, P.; Boonmars, T.; Wongkham, C.; Jones, A.; Plieskatt, J.; et al. Discovering proteins for chemoprevention and chemotherapy by curcumin in liver fluke infection-induced bile duct cancer. PLoS ONE 2018, 13, e0207405. [Google Scholar] [CrossRef] [PubMed]
- Gim, S.-A.; Lee, S.-R.; Shah, F.-A.; Koh, P.-O. Curcumin attenuates the middle cerebral artery occlusion-induced reduction in γ-enolase expression in an animal model. Lab. Anim. Res. 2015, 31, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Shah, F.-A.; Gim, S.-A.; Sung, J.-H.; Jeon, S.-J.; Kim, M.-O.; Koh, P.-O. Identification of proteins regulated by curcumin in cerebral ischemia. J. Surg. Res. 2015, 201, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Barnett, M.; Young, W.; Cooney, J.; Roy, N. Metabolomics and Proteomics, and What to Do with All These ‘Omes’: Insights from Nutrigenomic Investigations in New Zealand. Lifestyle Genom. 2014, 7, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Zhang, Q.; Wang, X.; Yang, X.; Wang, X.; Huang, Z.; Jiao, Y.; Wang, J. Quantitative phosphoproteomics reveals genistein as a modulator of cell cycle and DNA damage response pathways in triple-negative breast cancer cells. Int. J. Oncol. 2016, 48, 1016–1028. [Google Scholar] [CrossRef]
- Sotoca, A.M.; Gelpke, M.D.S.; Boeren, S.; Ström, A.; Gustafsson, J.; Murk, A.J.; Rietjens, I.; Vervoort, J. Quantitative Proteomics and Transcriptomics Addressing the Estrogen Receptor Subtype-mediated Effects in T47D Breast Cancer Cells Exposed to the Phytoestrogen Genistein. Mol. Cell. Proteom. 2011, 10. [Google Scholar] [CrossRef]
- Roh, T.; Kim, S.W.; Moon, S.H.; Nam, M.J. Genistein induces apoptosis by down-regulating thioredoxin-1 in human hepatocellular carcinoma SNU-449 cells. Food Chem. Toxicol. 2016, 97, 127–134. [Google Scholar] [CrossRef]
- Yan, G.R.; Zou, F.Y.; Dang, B.L.; Zhang, Y.; Yu, G.; Liu, X.; He, Q.Y. Genistein-induced mitotic arrest of gastric cancer cells by downregulating KIF 20 A, a proteomics study. Proteomics 2012, 12, 2391–2399. [Google Scholar] [CrossRef]
- Narasimhan, K.; Lee, Y.M.; Lim, T.K.; A Port, S.; Han, J.-H.; Chen, C.-S.; Lin, Q. Genistein exerts anti-leukemic effects on genetically different acute myeloid leukemia cell lines by inhibiting protein synthesis and cell proliferation while inducing apoptosis–molecular insights from an iTRAQ™ quantitative proteomics study. Oncoscience 2015, 2, 111–124. [Google Scholar] [CrossRef]
- Sun, Z.; Biela, L.M.; Hamilton, K.L.; Reardon, K.F. Concentration-dependent effects of the soy phytoestrogen genistein on the proteome of cultured cardiomyocytes. J. Proteom. 2012, 75, 3592–3604. [Google Scholar] [CrossRef]
- Fuchs, D.; de Pascual-Teresa, S.; Rimbach, G.; Virgili, F.; Ambra, R.; Turner, R.; Daniel, H.; Wenzel, U. Proteome analysis for identification of target proteins of genistein in primary human endothelial cells stressed with oxidized LDL or homocysteine. Eur. J. Nutr. 2004, 44, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhu, M.; Huo, Y.; Zhang, X.; Liao, M. Anti-fibrosis activity of combination therapy with epigallocatechin gallate, taurine and genistein by regulating glycolysis, gluconeogenesis, and ribosomal and lysosomal signaling pathways in HSC-T6 cells. Exp. Ther. Med. 2018, 16, 4329–4338. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Betancourt, A.M.; Mobley, J.A.; Lamartiniere, C.A. Proteomic Discovery of Genistein Action in the Rat Mammary Gland. J. Proteome Res. 2011, 10, 1621–1631. [Google Scholar] [CrossRef] [PubMed]
- Rowell, C.; Carpenter, D.M.; Lamartiniere, C.A. Chemoprevention of Breast Cancer, Proteomic Discovery of Genistein Action in the Rat Mammary Gland. J. Nutr. 2005, 135, 2953S–2959S. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Betancourt, A.; Jenkins, S.; Biro, F.; Pinney, S.M.; Chen, D.; Russo, J.; Lamartiniere, C.A. Altered blood proteome in girls with high urine concentrations of bisphenol A, genistein, mono-ethyl hexylphthalate and mono-benzyl phthalate. MOJ Proteom. Bioinform. 2015, 2, 44. [Google Scholar] [CrossRef] [PubMed]
- Betancourt, A.; Mobley, J.A.; Wang, J.; Jenkins, S.; Chen, N.; Kojima, K.; Russo, J.; Lamartiniere, C.A. Alterations in the Rat Serum Proteome Induced by Prepubertal Exposure to Bisphenol A and Genistein. J. Proteome Res. 2014, 13, 1502–1514. [Google Scholar] [CrossRef] [PubMed]
- Schwab, K.; Stein, R.; Scheler, C.; Theuring, F. Dietary genistein enhances phosphorylation of regulatory myosin light chain in the myocardium of ovariectomized mice. Electrophoresis 2012, 33, 1795–1803. [Google Scholar] [CrossRef]
- Schwab, K.; Neumann, B.; Vignon-Zellweger, N.; Fischer, A.; Stein, R.; Jungblut, P.R.; Scheler, C.; Theuring, F. Dietary phytoestrogen supplementation induces sex differences in the myocardial protein pattern of mice: A comparative proteomics study. Proteomics 2011, 11, 3887–3904. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Zhou, Y.; Li, Y.; Zhang, X.; He, M.; Zang, N.; Zhou, Y.; Liao, M. iTRAQ-based proteomic analysis of combination therapy with taurine, epigallocatechin gallate, and genistein on carbon tetrachloride-induced liver fibrosis in rats. Toxicol. Lett. 2015, 232, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Li, Y.; Li, M.; Zhang, X.; Liao, M. Txn1, Ctsd and Cdk4 are key proteins of combination therapy with taurine, epigallocatechin gallate and genistein against liver fibrosis in rats. Biomed. Pharmacother. 2017, 85, 611–619. [Google Scholar] [CrossRef]
- Bagheri, M.; Rezakhani, A.; Nyström, S.; Turkina, M.V.; Roghani, M.; Hammarström, P.; Mohseni, S. Amyloid Beta1-40-Induced Astrogliosis and the Effect of Genistein Treatment in Rat: A Three-Dimensional Confocal Morphometric and Proteomic Study. PLoS ONE 2013, 8, e76526. [Google Scholar] [CrossRef] [PubMed]
- Pan, T.-L.; Hung, Y.-C.; Wang, P.-W.; Chen, S.-T.; Hsu, T.-K.; Sintupisut, N.; Cheng, C.-S.; Lyu, P.-C. Functional proteomic and structural insights into molecular targets related to the growth inhibitory effect of tanshinone IIA on HeLa cells. Proteomics 2010, 10, 914–929. [Google Scholar] [CrossRef] [PubMed]
- Long, X.; Zhang, J.; Zhang, Y.; Yao, J.; Cai, Z.; Yang, P. Nano-LC-MS/MS based proteomics of hepatocellular carcinoma cells compared to Chang liver cells and tanshinone IIA induction. Mol. BioSyst. 2011, 7, 1728–1741. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.-L.; Hsia, C.-R.; Hsu, C.-L.; Huang, H.-C.; Juan, H.-F. Integrating transcriptomics and proteomics to show that tanshinone IIA suppresses cell growth by blocking glucose metabolism in gastric cancer cells. BMC Genom. 2015, 16, 41. [Google Scholar] [CrossRef] [PubMed]
- Pan, T.-L.; Wang, P.-W. Explore the Molecular Mechanism of Apoptosis Induced by Tanshinone IIA on Activated Rat Hepatic Stellate Cells. Evid. -Based Complement. Altern. Med. 2012, 2012, 734987. [Google Scholar] [CrossRef]
- Shi, S.L.; Li, Q.F.; Liu, Q.R.; Xu, D.H.; Tang, J.; Liang, Y.; Zhao, Z.L.; Yang, L.M. Nuclear matrix protein, prohibitin, was down-regulated and translocated from nucleus to cytoplasm during the differentiation of osteosarcoma MG-63 cells induced by ginsenoside Rg1, cinnamic acid, and tanshinone IIA (RCT). J. Cell Biochem. 2009, 108, 926–934. [Google Scholar] [CrossRef]
- Yin, C.-F.; Kao, S.-C.; Hsu, C.-L.; Chang, Y.-W.; Cheung, C.H.Y.; Huang, H.-C.; Juan, H.-F. Phosphoproteome Analysis Reveals Dynamic Heat Shock Protein 27 Phosphorylation in Tanshinone IIA-Induced Cell Death. J. Proteome Res. 2020, 19, 1620–1634. [Google Scholar] [CrossRef]
- Pan, T.L.; Wang, P.W.; Hung, Y.C.; Huang, C.H.; Rau, K.M. Proteomic analysis reveals tanshinone IIA enhances apoptosis of advanced cervix carcinoma CaSki cells through mitochondria intrinsic and endoplasmic reticulum stress pathways. Proteomics 2013, 13, 3411–3423. [Google Scholar] [CrossRef]
- Cabrera-Pérez, R.; Monguió-Tortajada, M.; Gámez-Valero, A.; Rojas-Márquez, R.; Borràs, F.E.; Roura, S.; Vives, J. Osteogenic commitment of Wharton’s jelly mesenchymal stromal cells: Mechanisms and implications for bioprocess development and clinical application. Stem Cell Res. Ther. 2019, 10, 356. [Google Scholar] [CrossRef]
- Yan, S.-H.; Zhao, N.-W.; Geng, Z.-R.; Shen, J.-Y.; Liu, F.-M.; Yan, D.; Zhou, J.; Nie, C.; Huang, C.-C.; Fang, Z.-Y. Modulations of Keap1-Nrf2 signaling axis by TIIA ameliorated the oxidative stress-induced myocardial apoptosis. Free Radic. Biol. Med. 2018, 115, 191–201. [Google Scholar] [CrossRef]
- Yan, Y.; Su, W.; Zeng, S.; Qian, L.; Chen, X.; Wei, J.; Chen, N.; Gong, Z.; Xu, Z. Effect and Mechanism of Tanshinone I on the Radiosensitivity of Lung Cancer Cells. Mol. Pharm. 2018, 15, 4843–4853. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, Y.; Ma, C.; Zhang, L.; Wu, W.; Guan, S.; Yang, M.; Wang, J.; Jiang, B.; Guo, D.-A. Proteomic Assessment of Tanshinone II A Sodium Sulfonate on Doxorubicin Induced Nephropathy. Am. J. Chin. Med. 2011, 39, 395–409. [Google Scholar] [CrossRef] [PubMed]
- Weng, W.; Goel, A. Curcumin and colorectal cancer: An update and current perspective on this natural medicine. Semin. Cancer Biol. 2020, 80, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Anand, P.; Kunnumakkara, A.B.; Newman, R.A.; Aggarwal, B.B. Bioavailability of curcumin: Problems and promises. Mol. Pharm. 2007, 4, 807–818. [Google Scholar] [CrossRef]
- Huang, Y.-F.; Zhu, D.-J.; Chen, X.-W.; Chen, Q.-K.; Luo, Z.-T.; Liu, C.-C.; Wang, G.-X.; Zhang, W.-J.; Liao, N.-Z. Curcumin enhances the effects of irinotecan on colorectal cancer cells through the generation of reactive oxygen species and activation of the endoplasmic reticulum stress pathway. Oncotarget 2017, 8, 40264–40275. [Google Scholar] [CrossRef]
- Singh, L.; Sharma, S.; Xu, S.; Tewari, D.; Fang, J. Curcumin as a Natural Remedy for Atherosclerosis: A Pharmacological Review. Molecules 2021, 26, 4036. [Google Scholar] [CrossRef]
- Silvestro, S.; Sindona, C.; Bramanti, P.; Mazzon, E. A State of the Art of Antioxidant Properties of Curcuminoids in Neurodegenerative Diseases. Int. J. Mol. Sci. 2021, 22, 3168. [Google Scholar] [CrossRef]
- Gregory, J.; Vengalasetti, Y.; Bredesen, D.; Rao, R. Neuroprotective Herbs for the Management of Alzheimer’s Disease. Biomolecules 2021, 11, 543. [Google Scholar] [CrossRef]
- Simeonova, R.; Zheleva, D.; Valkova, I.; Stavrakov, G.; Philipova, I.; Atanasova, M.; Doytchinova, I. A Novel Galantamine-Curcumin Hybrid as a Potential Multi-Target Agent against Neurodegenerative Disorders. Molecules 2021, 26, 1865. [Google Scholar] [CrossRef]
- Goedert, M.; Spillantini, M.G.; Del Tredici, K.; Braak, H. 100 years of Lewy pathology. Nat. Rev. Neurol. 2012, 9, 13–24. [Google Scholar] [CrossRef]
- Vallés, S.L.; Borrás, C.; Gambini, J.; Furriol, J.; Ortega, A.; Sastre, J.; Pallardó, F.V.; Viña, J. Oestradiol or genistein rescues neurons from amyloid beta-induced cell death by inhibiting activation of p38. Aging Cell 2008, 7, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Cai, Q.; Wei, H. Effect of dietary genistein on antioxidant enzyme activities in SENCAR mice. Nutr. Cancer 1996, 25, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hao, H.; Wang, G.; Cui, N.; Li, J.; Xie, L.; Ding, Z. Pharmacokinetics, Absorption and Tissue Distribution of Tanshinone IIA Solid Dispersion. Planta Medica 2006, 72, 1311–1317. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Zuo, Z.; Chow, M.S.S. Danshen: An Overview of Its Chemistry, Pharmacology, Pharmacokinetics, and Clinical Use. J. Clin. Pharmacol. 2005, 45, 1345–1359. [Google Scholar] [CrossRef]
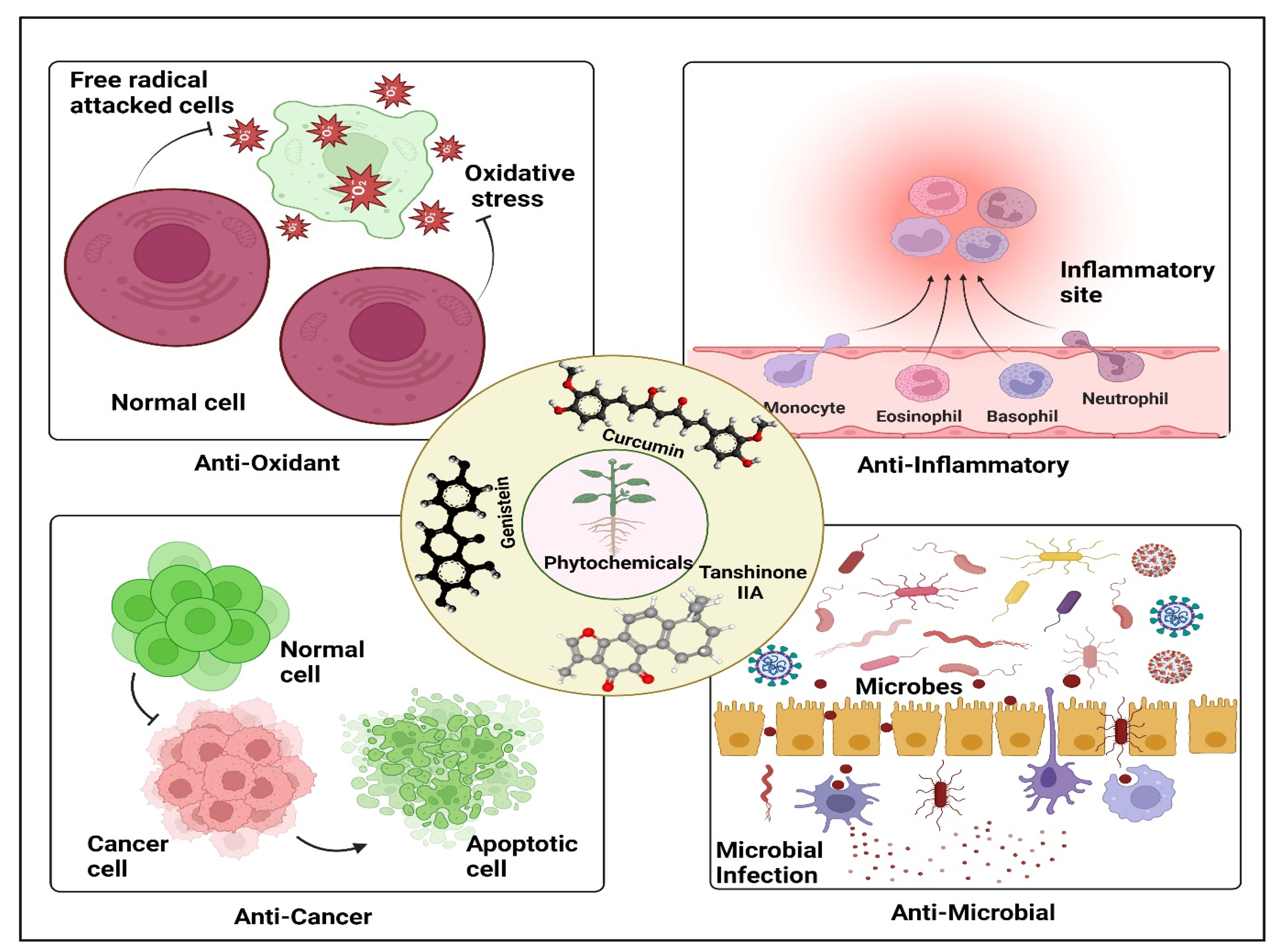
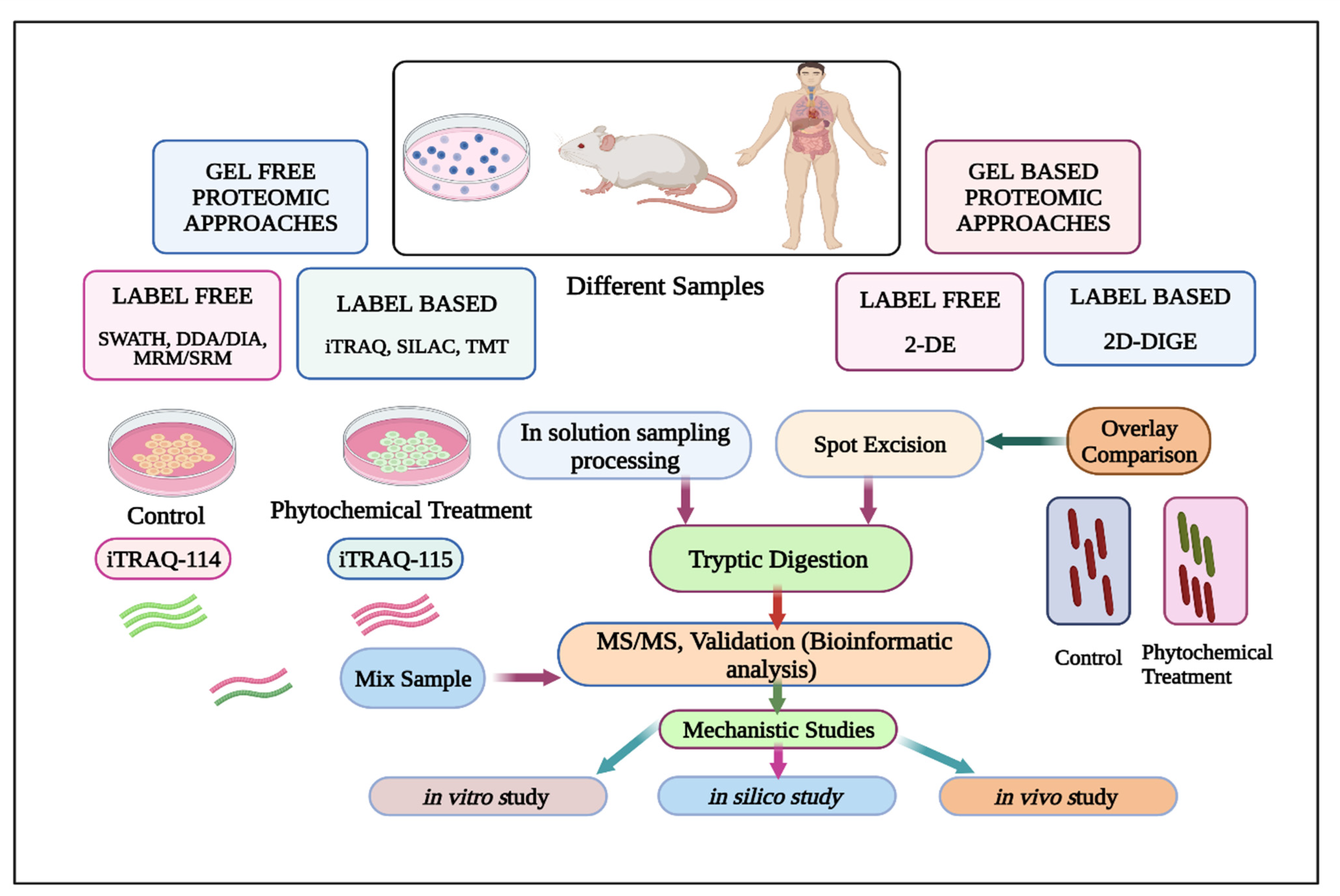
| S. No. | PhytochemicalName | Appearance | Chemical Structure | Molecular Weight, Chemical Formula, Pubchem CID, and IUPAC Name | Prospective Pharmacological Properties |
|---|---|---|---|---|---|
| 1. | Curcumin | Bright yellow-orange | 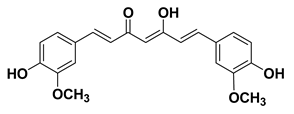 | Mol wt: 368.38 g/mol Chemical formula: C21H20O6 Pubchem CID:969516 IUPAC name: 1,7-Bis(4-hydroxy-3-methoxyphenyl)hepta-1,6-diene-3,5-dione | It acts as an antioxidant [25], anti-inflammatory [26] anti-bacterial [27], anti-fungal [28] antiviral [29], and anti-neoplastic agent [30]. It exhibits phototoxic and photodynamic activities [31,32,33], acts as a cyclo-oxygenase inhibitor [34], lipoxygenase inhibitor [35], iron chelator [36], immunomodulator [37], and neuroprotective agents [38,39,40,41]. |
| 2. | Genistein | Yellow | 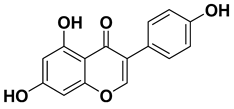 | Mol wt: 270.24 g/mol Chemical formula: C15H10O5 Pubchem CID: 5280961 IUPAC name: 5,7-dihydroxy-3-(4-hydroxyphenyl)chromen-4-one | It has antioxidant [42], anti-inflammatory and immunosuppressive activities [43]; it acts as anti-microbial agent [44], it embodies anti-carcinogenic and anti-metastatic properties [45]. It also acts as a phytoestrogen and a protein tyrosine kinase inhibitor [46], and neuroprotective agent [47,48,49,50]. |
| 3. | Tanshinone IIA | Red | 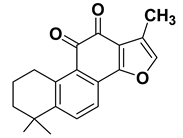 | Mol wt: 294.3 g/mol Chemical formula: C19H18O3 Pubchem CID: 164676 IUPAC name: 1,6,6-trimethyl-8,9-dihydro-7H-naphtho [1,2-g] [1]benzofuran-10,11-dione | It embodies antioxidant [51], anti -inflammatory [52], anti-microbial [53], anti-cancer [54], anti-angiogenic [55], and anti-adipogenic properties [56], and embodies neuroprotective properties [57,58,59,60]. |
| 4. | Allicin | Slightly yellow | 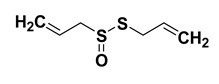 | Mol wt: 162.3 g/mol Chemical formula: C6H10OS2, Pubchem CID: 65036 IUPAC name: 3-prop-2-enyl sulfinyl sulfanyl prop-1-ene | It embodies free radical scavenging properties, viz., anti-oxidant [61], anti-bacterial [62,63,64], anti-fungal [63], and anti-viral properties [65]. It exhibits antihypertensive [66] and neuroprotective properties [67] and acts as hypo-lipidemic and hypo-glycemic [68,69] and anti-cancer agent [70,71,72]. |
| 5. | Eugenol | Pale yellow | 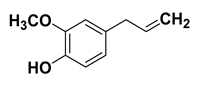 | Mol wt: 164.2 g/mol Chemical formula: C10H12O2 Pubchem CID: 3314 IUPAC name: 2-methoxy-4-prop-2-enyl phenol | It embodies antioxidant [73], anti-inflammatory [74], anti-microbial [75], anti-tumor [76,77,78,79], anti-mutagenic [76,77,78,79], anti-allergic [80], antipyretic [81] and analgesic characteristics [80]. It is a 5-lipoxygenase inhibitor [76], anti-hypercholesterolemic, and anti-atherogenic potential [82], antidiabetic [83], antiparasitic [84], and anti-leishmanial agent [85]. |
| 6. | Apigenin | Yellow | 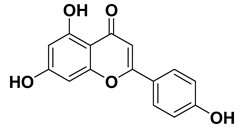 | Mol wt: 270.24 g/mol Chemical formula: C15H10O5 Pubchem CID: 5280443 IUPAC name: 5,7-dihydroxy-2-(4-hydroxyphenyl) chromen-4-one | It is an antioxidant [86], anti-inflammatory [87,88,89], anti-bacterial [90], anti-viral [91], anti-cancer [92], chemo-preventive agent, anti-invasive [92,93], and antidiabetic agent [94,95,96] and embodies neuroprotective [97] and vasodilatory action [98]. |
| 7. | Lycopene | Bright Red | 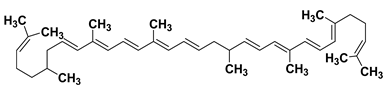 | Mol wt: 536.873 g/mol Chemical formula: C40H56, Pubchem CID: 446925 IUPAC name: 2,6,10,14,19,23,27,31-octamethyldotriaconta-2,6,8,10,12,14,16,18,20,22,24,26,30-tridecaene | It is an antioxidant [99], anti-inflammatory [100], anti-microbial [101], anticancer [102], radiation-protective agent [103], and embodies cardioprotective [104] and neuroprotective properties [105]. |
| 8. | Anthocyanin | Red, purple, and blue | 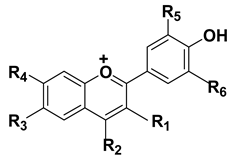 | Mol wt: 207.24724 g/mol, Chemical formula: C15H11O+, Pubchem CID: 145858 IUPAC name: 2-phenylchromenylium | It embodies antioxidant [106], anti-inflammatory [107], anti-microbial [108], antiviral [109], and anticancer properties [110]; it embodies hypouricemic and nephroprotective effects [111]. It acts as a cyto-protective [112] and neuroprotective agent [113]. |
| 9. | Capsaicin | Crystalline white | 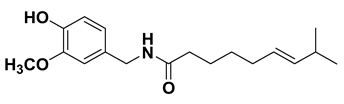 | Mol wt: 305.4 g/mol, Chemical formula: C18H27NO3 Pubchem CID:1548943 IUPAC name: (E)-N-[(4-hydroxy-3-methoxyphenyl) methyl]-8-methylnon-6-enamide | It act as an antioxidant [114], anti-inflammatory [115], anti-bacterial [116], anti-fungal [117], anti-viral [118], and anticancer agent [119]. It act as an analgesic [120], gastroprotective [121], anti-obesity [122], and antipruritic agent [123]. It embodies anti-proliferative and pro-apoptotic properties against cancer [124]. |
| 10. | Shogaols | Bright yellow | 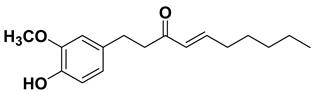 | Mol wt: 276.376 g·mol−1, Chemical formula: C17H24O3, Pubchem CID: 5281794 IUPAC name: (E)-1-(4-hydroxy-3-methoxyphenyl)dec-4-en-3-one | It has been found as an antioxidant [125,126,127], anti-inflammatory [128,129,130,131], anti-bacterial [132], anti-fungal [133], anti-viral [134], anticancer, and chemo-preventive agent [135] with anti-emetic and anti-thrombotic properties [136]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, F.B.; Singh, P.; Jamous, Y.F.; Ali, S.A.; Abdullah; Uddin, S.; Zia, Q.; Jena, M.K.; Khan, M.; Owais, M.; et al. Multifaceted Pharmacological Potentials of Curcumin, Genistein, and Tanshinone IIA through Proteomic Approaches: An In-Depth Review. Cancers 2023, 15, 249. https://doi.org/10.3390/cancers15010249
Khan FB, Singh P, Jamous YF, Ali SA, Abdullah, Uddin S, Zia Q, Jena MK, Khan M, Owais M, et al. Multifaceted Pharmacological Potentials of Curcumin, Genistein, and Tanshinone IIA through Proteomic Approaches: An In-Depth Review. Cancers. 2023; 15(1):249. https://doi.org/10.3390/cancers15010249
Chicago/Turabian StyleKhan, Farheen Badrealam, Parul Singh, Yahya F. Jamous, Syed Azmal Ali, Abdullah, Shahab Uddin, Qamar Zia, Manoj Kumar Jena, Mohsina Khan, Mohammad Owais, and et al. 2023. "Multifaceted Pharmacological Potentials of Curcumin, Genistein, and Tanshinone IIA through Proteomic Approaches: An In-Depth Review" Cancers 15, no. 1: 249. https://doi.org/10.3390/cancers15010249
APA StyleKhan, F. B., Singh, P., Jamous, Y. F., Ali, S. A., Abdullah, Uddin, S., Zia, Q., Jena, M. K., Khan, M., Owais, M., Huang, C. Y., Chanukuppa, V., Ardianto, C., Ming, L. C., Alam, W., Khan, H., & Ayoub, M. A. (2023). Multifaceted Pharmacological Potentials of Curcumin, Genistein, and Tanshinone IIA through Proteomic Approaches: An In-Depth Review. Cancers, 15(1), 249. https://doi.org/10.3390/cancers15010249











