Microsatellite Status Detection in Gastrointestinal Cancers: PCR/NGS Is Mandatory in Negative/Patchy MMR Immunohistochemistry
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimens
2.1.1. Series of Colorectal Cancers
2.1.2. Series of Gastric Cancers
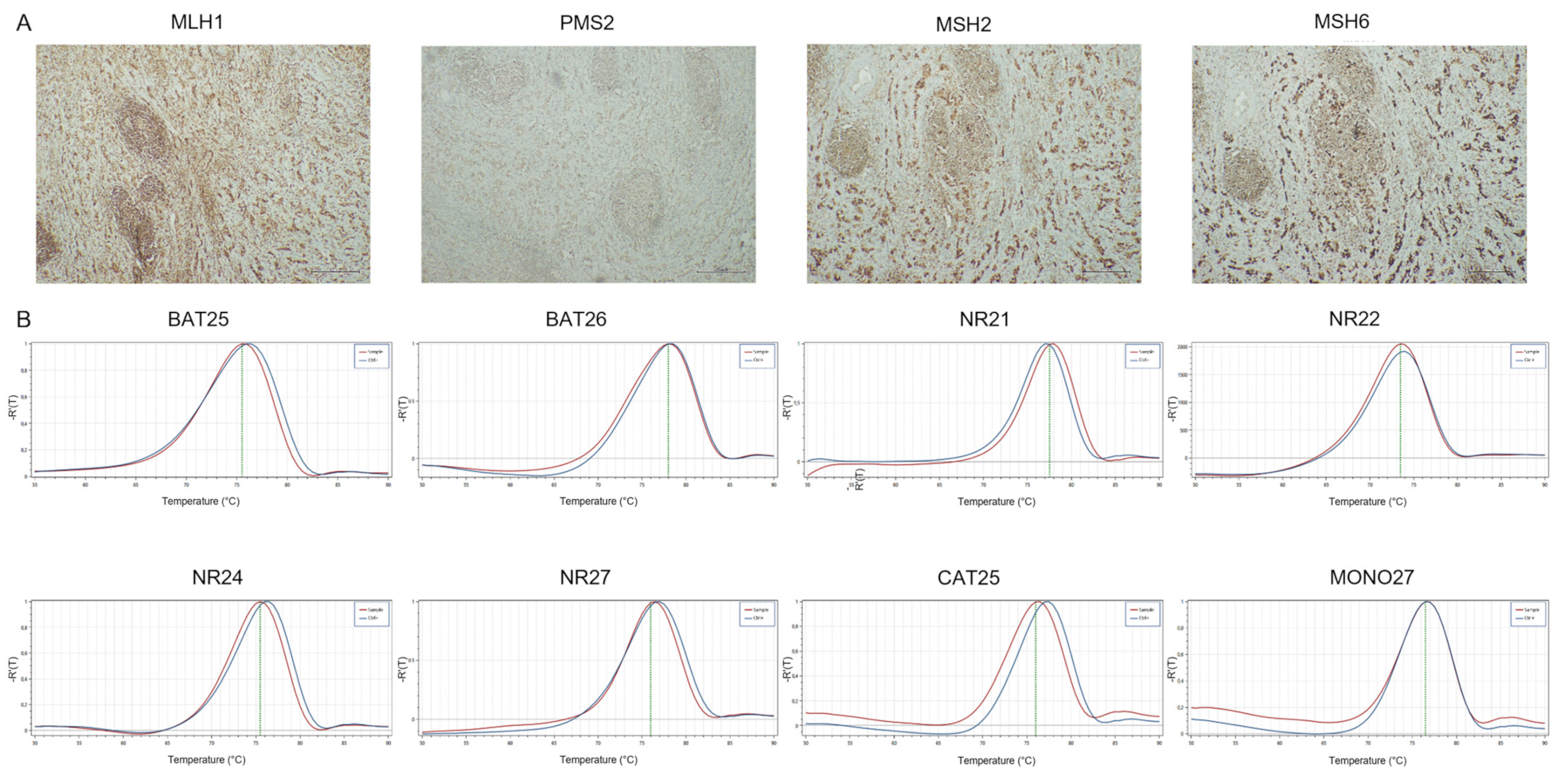
2.2. Immunohistochemical Analysis of MMR Protein Expression
2.3. PCR Detection for Microsatellite Status
2.4. NGS Detection for Microsatellite Status
2.5. Statistical Analysis
3. Results
3.1. Colon Cancer Series
3.1.1. Clinicopathological Features
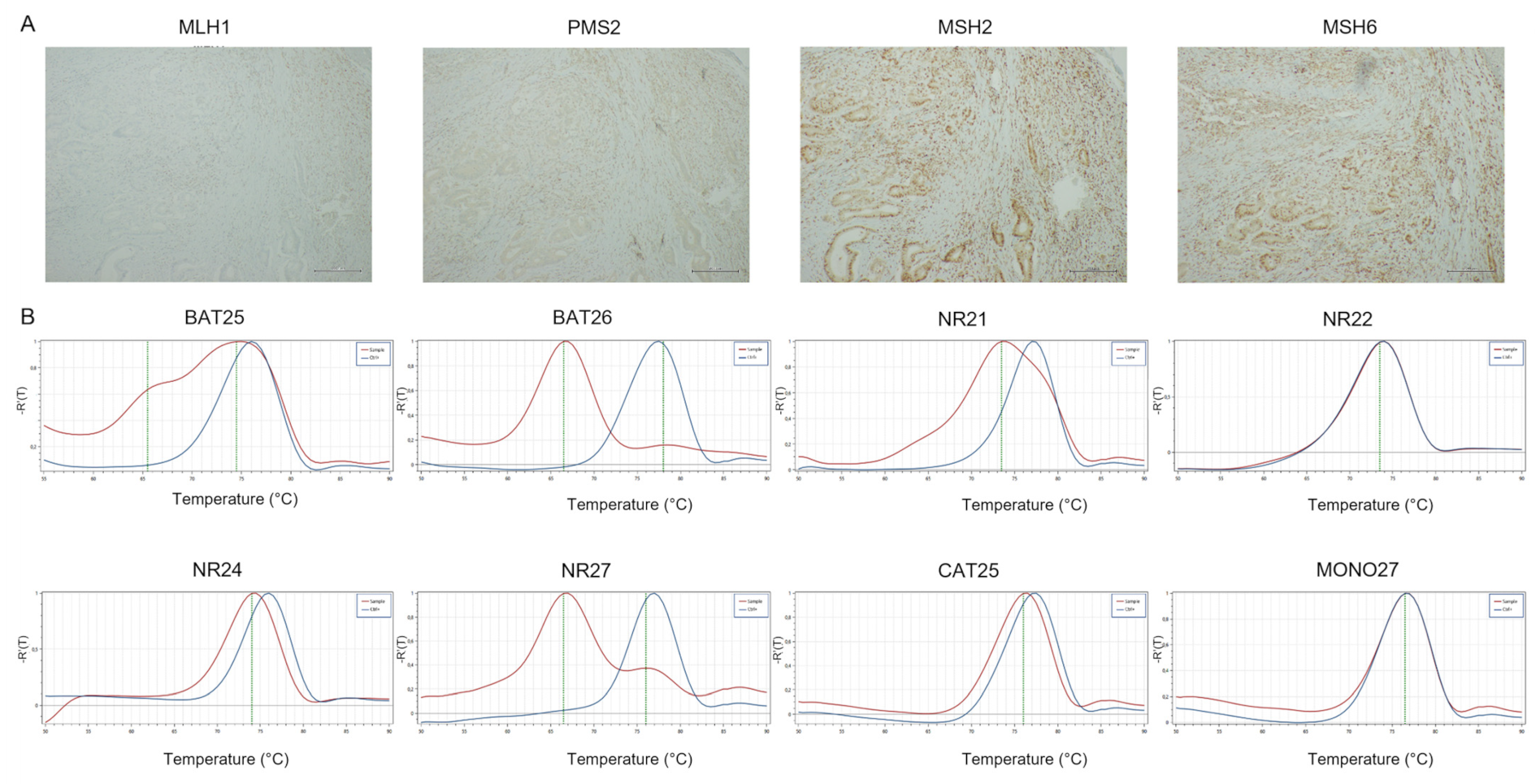
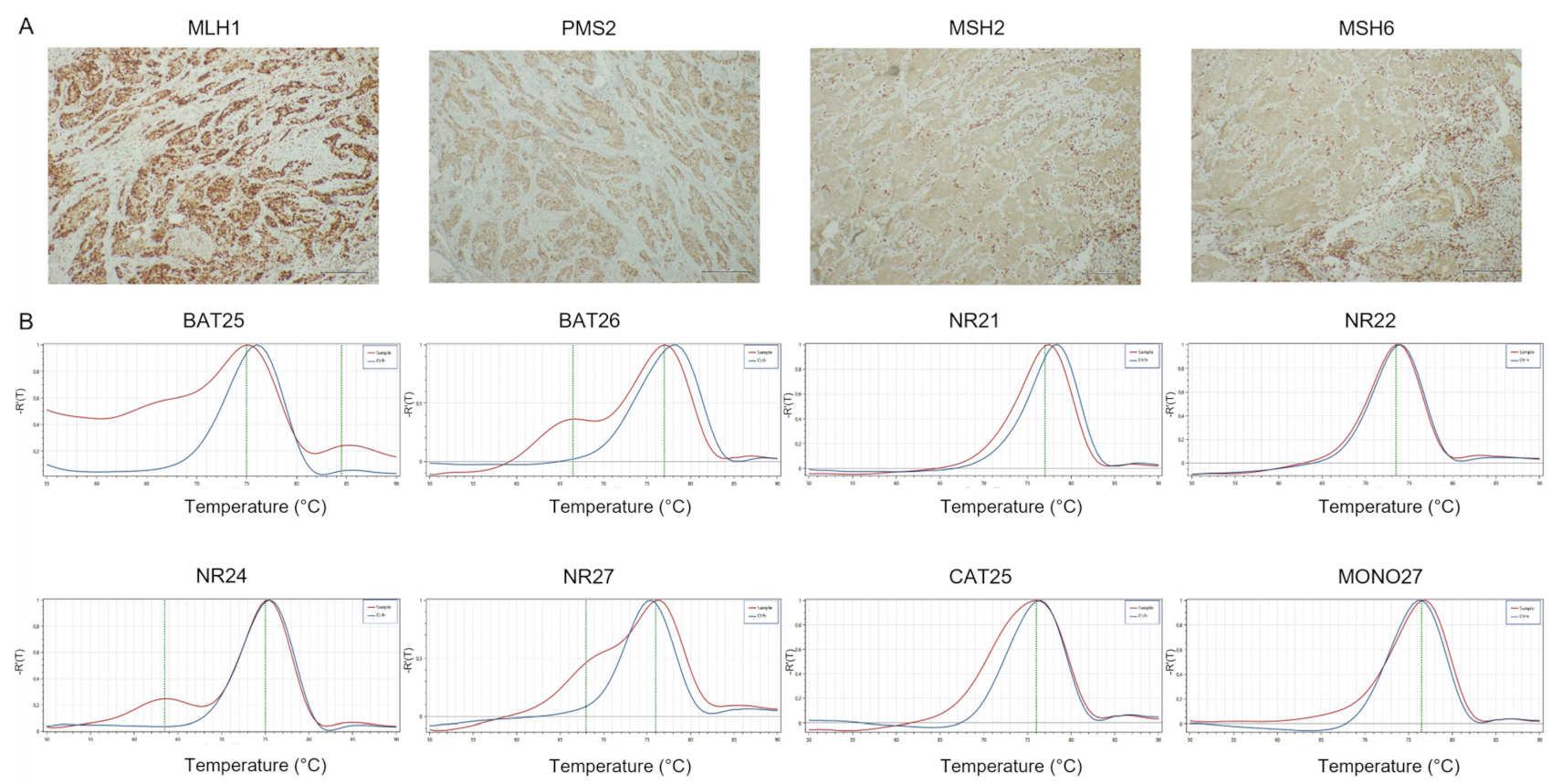
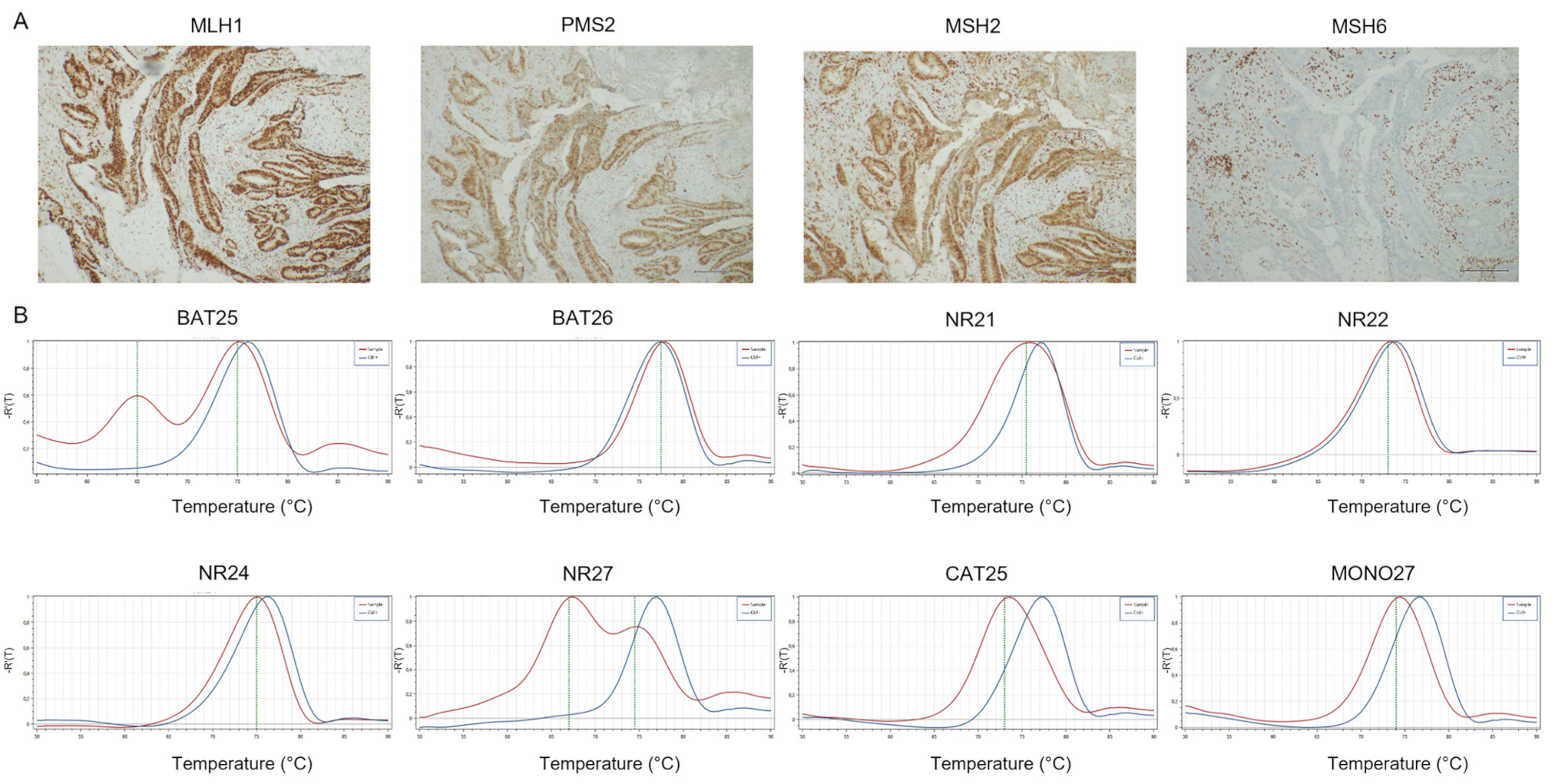
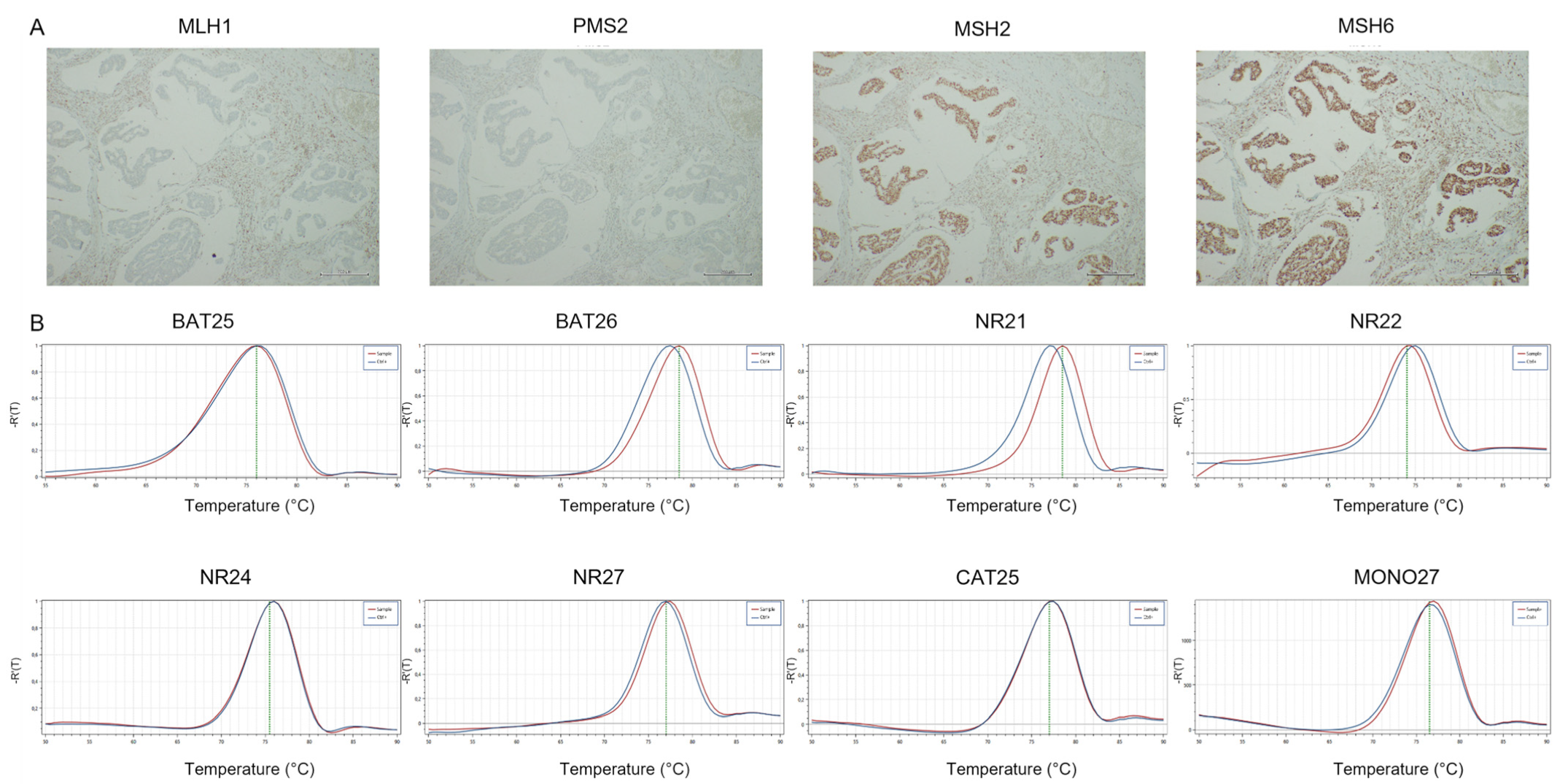
3.1.2. MMR-IHC Analysis
3.1.3. PCR Detection for Microsatellite Status
3.1.4. Comparison of MMR-IHC and MSI-PCR
3.1.5. Second Diagnostic Opinion of IHC and PCR
4. Gastric Cancer
4.1. Gastric Cancer Series
4.1.1. Clinical and Pathological Characteristics of Patients
4.1.2. MMR-IHC Analysis
4.1.3. PCR Detection for Microsatellite Status
4.1.4. Comparison of MMR-IHC and MSI Molecular Testing
4.1.5. Second Diagnostic Opinion of IHC and PCR
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boland, C.R.; Goel, A. Microsatellite instability in colorectal cancer. Gastroenterology 2010, 138, 2073–2087. [Google Scholar] [CrossRef] [PubMed]
- Collura, A.; Lefevre, J.H.; Svrcek, M.; Tougeron, D.; Zaanan, A.; Duval, A. Microsatellite instability and cancer: From genomic instability to personalized medicine. Med. Sci. 2019, 35, 535–543. [Google Scholar]
- Lefol, C.; Sohier, E.; Baudet, C.; Naïbo, P.; Ruano, E.; Grand-Masson, C.; Viari, A.; Wang, Q. Acquired somatic MMR deficiency is a major cause of MSI tumor in patients suspected for “Lynch-like syndrome” including young patients. Eur. J. Hum. Genet. 2021, 29, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Luo, H.; Huang, L.; Luo, H.; Zhu, X. Microsatellite instability: A review of what the oncologist should know. Cancer Cell Int. 2020, 20, 16. [Google Scholar] [CrossRef] [Green Version]
- Sahin, I.H.; Akce, M.; Alese, O.; Shaib, W.; Lesinski, G.B.; El-Rayes, B.; Wu, C. Immune checkpoint inhibitors for the treatment of MSI-H/MMR-D colorectal cancer and a perspective on resistance mechanisms. Br. J. Cancer 2019, 121, 809–818. [Google Scholar] [CrossRef]
- André, T.; Shiu, K.K.; Kim, T.W.; Jensen, B.V.; Jensen, L.H.; Punt, C.; Smith, D.; Garcia-Carbonero, R.; Benavides, M.; Gibbs, P.; et al. KEYNOTE-177 Investigators. Pembrolizumab in Microsatellite-Instability-High Advanced Colorectal Cancer. N. Engl. J. Med. 2020, 383, 2207–2218. [Google Scholar] [CrossRef]
- Puliga, E.; Corso, S.; Pietrantonio, F.; Giordano, S. Microsatellite instability in Gastric Cancer: Between lights and shadows. Cancer Treat. Rev. 2021, 95, 102175. [Google Scholar] [CrossRef]
- Pietrantonio, F.; Randon, G.; Di Bartolomeo, M.; Luciani, A.; Chao, J.; Smyth, E.C.; Petrelli, F. Predictive role of microsatellite instability for PD-1 blockade in patients with advanced gastric cancer: A meta-analysis of randomized clinical trials. ESMO Open 2021, 6, 100036. [Google Scholar] [CrossRef]
- Shitara, K.; Özgüroğlu, M.; Bang, Y.J.; Di Bartolomeo, M.; Mandalà, M.; Ryu, M.H.; Fornaro, L.; Olesiński, T.; Caglevic, C.; Chung, H.C.; et al. Pembrolizumab versus paclitaxel for previously treated, advanced gastric or gastro-oesophageal junction cancer (KEYNOTE-061): A randomised, open-label, controlled, phase 3 trial. Lancet 2018, 392, 123–133. [Google Scholar] [CrossRef]
- Shitara, K.; Van Cutsem, E.; Bang, Y.; Fuchs, C.S.; Wyrwicz, L.; Lee, K.W.; Kudaba, I.; Garrido, M.; Cheol Chung, H.; Castro, H.R.; et al. Pembrolizumab with or without chemotherapy vs. chemotherapy in patients with advanced G/GEJ cancer (GC) including outcomes according to Microsatellite Instability-High (MSI-H) status in KEYNOTE-062. Ann. Oncol. 2019, 30, v878–v879. [Google Scholar] [CrossRef]
- Shitara, K.; Van Cutsem, E.; Bang, Y.J.; Fuchs, C.; Wyrwicz, L.; Lee, K.W.; Kudaba, I.; Garrido, M.; Chung, H.C.; Lee, J.; et al. Efficacy and Safety of Pembrolizumab or Pembrolizumab Plus Chemotherapy vs. Chemotherapy Alone for Patients with First-line, Advanced Gastric Cancer: The KEYNOTE-062 Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020, 6, 1571–1580. [Google Scholar] [CrossRef] [PubMed]
- Chao, J.; Fuchs, C.S.; Shitara, K.; Tabernero, J.; Muro, K.; Van Cutsem, E.; Bang, Y.J.; De Vita, F.; Landers, G.A.; Yen, C.J.; et al. Pembrolizumab (pembro) in microsatellite instability-high (MSI-H) advanced gastric/gastroesophageal junction (G/GEJ) cancer by line of therapy. J. Clin. Oncol. 2020, 38 (Suppl. 4), 430. [Google Scholar] [CrossRef]
- Moehler, M.; Shitara, K.; Garrido, M.; Salman, P.; Shen, L.; Wyrwicz, L.; Yamaguchi, K.; Skoczylas, T.; Campos Bragagnoli, A.; Liu, T.; et al. LBA6_PR Nivolumab (nivo) plus chemotherapy (chemo) versus chemo as first-line (1L) treatment for advanced gastric cancer/gastroesophageal junction cancer (GC/GEJC)/esophageal adenocarcinoma (EAC): First results of the CheckMate 649 study. Ann. Oncol. 2020, 31, S1191. [Google Scholar] [CrossRef]
- Sepulveda, A.R.; Hamilton, S.R.; Allegra, C.J.; Grody, W.; Cushman-Vokoun, A.M.; Funkhouser, W.K.; Kopetz, S.E.; Lieu, C.; Lindor, N.M.; Minsky, B.D.; et al. Molecular Biomarkers for the Evaluation of Colorectal Cancer: Guideline from the American Society for Clinical Pathology, College of American Pathologists, Association for Molecular Pathology, and the American Society of Clinical Oncology. J. Clin. Oncol. 2017, 35, 1453–1486. [Google Scholar] [CrossRef]
- Battaglin, F.; Naseem, M.; Lenz, H.J.; Salem, M.E. Microsatellite instability in colorectal cancer: Overview of its clinical significance and novel perspectives. Clin. Adv. Hematol Oncol. 2018, 16, 735–745. [Google Scholar]
- De Salins, G.D.A.A.; Tachon, G.; Cohen, R.; Karayan-Tapon, L.; Junca, A.; Frouin, E.; Godet, J.; Evrard, C.; Randrian, V.; Duval, A.; et al. Discordance between immunochemistry of mismatch repair proteins and molecular testing of microsatellite instability in colorectal cancer. ESMO Open 2021, 6, 100–120. [Google Scholar]
- Kawakami, H.; Zaanan, A.; Sinicrope, F.A. Microsatellite instability testing and its role in the management of colorectal cancer. Curr. Treat. Options Oncol. 2015, 16, 30. [Google Scholar] [CrossRef]
- Suraweera, N.; Duval, A.; Reperant, M.; Vaury, C.; Furlan, D.; Leroy, K.; Seruca, R.; Iacopetta, B.; Hamelin, R. Evaluation of tumor microsatellite instability using five quasimonomorphic mononucleotide repeats and pentaplex PCR. Gastroenterology 2002, 123, 1804–1811. [Google Scholar] [CrossRef]
- Boland, C.R.; Thibodeau, S.N.; Hamilton, S.R.; Sidransky, D.; Eshleman, J.R.; Burt, R.W.; Meltzer, S.J.; Rodriguez-Bigas, M.A.; Fodde, R.; Ranzani, G.N.; et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: Development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998, 58, 5248–5257. [Google Scholar]
- Bonneville, R.; Krook, M.A.; Chen, H.Z.; Smith, A.; Samorodnitsky, E.; Wing, M.R.; Reeser, J.W.; Roychowdhury, S. Detection of Microsatellite Instability Biomarkers via Next-Generation Sequencing. Methods Mol. Biol. 2020, 2055, 119–132. [Google Scholar]
- Lindor, N.M.; Burgart, L.J.; Leontovich, O.; Goldberg, R.M.; Cunningham, J.M.; Sargent, D.J.; Walsh-Vockley, C.; Petersen, G.M.; Walsh, M.D.; Leggett, B.A.; et al. Immunohistochemistry versus microsatellite instability testing in phenotyping colorectal tumors. J. Clin. Oncol. 2002, 20, 1043–1048. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.; Grieu, F.; Morris, M.; Harvey, J.; Stewart, C.; Schofield, L.; Goldblatt, J.; Iacopetta, B. Heterogeneous staining for mismatch repair proteins during population-based prescreening for hereditary nonpolyposis colorectal cancer. J. Mol. Diagn. 2007, 9, 472–478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, M.L.; Chen, J.Y.; Hu, J.; Chen, Q.; Yu, L.X.; Liu, B.R.; Qian, X.P.; Yang, M. Comparison of microsatellite status detection methods in colorectal carcinoma. Int. J. Clin. Exp. Pathol. 2018, 11, 1431–1438. [Google Scholar] [PubMed]
- Cohen, R.; Hain, E.; Buhard, O. Assessment of local clinical practice for testing of mismatch repair deficiency in metastatic colorectal cancer: The need for new diagnostic guidelines prior to immunotherapy. Ann. Oncol. 2018, 29, 179–180. [Google Scholar] [CrossRef]
- Jaffrelot, M.; Selves, J.; Fares, N. Characterization of atypical dMMR (deficient MisMatch Repair) tumors: A study from a large cohort of 4948 cases. Ann. Oncol. 2019, 30, 870. [Google Scholar] [CrossRef]
- Ratti, M.; Lampis, A.; Hahne, J.C.; Passalacqua, R.; Valeri, N. Microsatellite instability in gastric cancer: Molecular bases, clinical perspectives, and new treatment approaches. Cell Mol. Life Sci. 2018, 75, 4151–4162. [Google Scholar] [CrossRef]
- Sugimoto, R.; Endo, M.; Osakabe, M.; Toya, Y.; Yanagawa, N.; Matsumoto, T.; Sugai, T. Immunohistochemical Analysis of Mismatch Repair Gene Proteins in Early Gastric Cancer Based on Microsatellite Status. Digestion 2021, 102, 691–700. [Google Scholar] [CrossRef]
- Illumina TruSight Oncology 500 Full Specification Information. Available online: https://www.illumina.com/content/dam/illumina/gcs/assembled-assets/marketing-literature/trusight-oncology-500-data-sheet-m-gl-00173/trusight-oncology-500-and-ht-data-sheet-m-gl-00173.pdf (accessed on 20 April 2022).
- Ronchi, A.; Pagliuca, F.; Zito Marino, F.; Argenziano, G.; Brancaccio, G.; Alfano, R.; Signoriello, G.; Moscarella, E.; Franco, R. Second Diagnostic Opinion by Experienced Dermatopathologists in the Setting of a Referral Regional Melanoma Unit Significantly Improves the Clinical Management of Patients with Cutaneous Melanoma. Front. Med. 2021, 7, 568946. [Google Scholar] [CrossRef]
- Inamura, K. Colorectal Cancers: An Update on Their Molecular Pathology. Cancers 2018, 10, 26. [Google Scholar] [CrossRef] [Green Version]
- Shia, J. Immunohistochemistry versus microsatellite instability testing for screening colorectal cancer patients at risk for hereditary nonpolyposis colorectal cancer syndrome. Part I. The utility of immunohistochemistry. J. Mol. Diagn. 2008, 10, 293–300. [Google Scholar] [CrossRef] [Green Version]
- Cicek, M.S.; Lindor, N.M.; Gallinger, S.; Bapat, B.; Hopper, J.L.; Jenkins, M.A.; Young, J.; Buchanan, D.; Walsh, M.D.; Le Marchand, L.; et al. Quality assessment and correlation of microsatellite instability and immunohistochemical markers among population- and clinic-based colorectal tumors results from the Colon Cancer Family Registry. J. Mol. Diagn. 2011, 13, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Karahan, B.; Argon, A.; Yıldırım, M.; Vardar, E. Relationship between MLH-1, MSH-2, PMS-2, MSH-6 expression and clinicopathological features in colorectal cancer. Int. J. Clin. Exp. Pathol. 2015, 8, 4044–4053. [Google Scholar] [PubMed]
- Wang, Q.; Liu, G.; Hu, C. Molecular Classification of Gastric Adenocarcinoma. Gastroenterol. Res. 2019, 12, 275–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alpert, L.; Pai, R.K.; Srivastava, A.; McKinnon, W.; Wilcox, R.; Yantiss, R.K.; Arcega, R.; Wang, H.L.; Robert, M.E.; Liu, X.; et al. Colorectal Carcinomas with Isolated Loss of PMS2 Staining by Immunohistochemistry. Arch. Pathol Lab. Med. 2018, 142, 523–528. [Google Scholar] [CrossRef]
- Stelloo, E.; Jansen, A.M.L.; Osse, E.M.; Nout, R.A.; Creutzberg, C.L.; Ruano, D.; Church, D.N.; Morreau, H.; Smit, V.T.H.B.M.; van Wezel, T.; et al. Practical guidance for mismatch repair-deficiency testing in endometrial cancer. Ann. Oncol. 2017, 28, 96–102. [Google Scholar] [CrossRef]
- Engel, K.B.; Moore, H.M. Effects of preanalytical variables on the detection of proteins by immunohistochemistry in formalin-fixed, paraffin-embedded tissue. Arch. Pathol. Lab. Med. 2011, 135, 537–543. [Google Scholar] [CrossRef]
- Chen, W.; Swanson, B.J.; Frankel, W.L. Molecular genetics of microsatellite-unstable colorectal cancer for pathologists. Diagn. Pathol. 2017, 12, 24. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Frankel, W.L. A practical guide to biomarkers for the evaluation of colorectal cancer. Mod. Pathol. 2019, 32 (Suppl. 1), 1–15. [Google Scholar] [CrossRef]
- Cohen, R.; Hain, E.; Buhard, O.; Guilloux, A.; Bardier, A.; Kaci, R.; Bertheau, P.; Renaud, F.; Bibeau, F.; Fléjou, J.F.; et al. Association of Primary Resistance to Immune Checkpoint Inhibitors in Metastatic Colorectal Cancer with Misdiagnosis of Microsatellite Instability or Mismatch Repair Deficiency Status. JAMA Oncol. 2019, 5, 551–555. [Google Scholar] [CrossRef]
- Zaanan, A.; Meunier, K.; Sangar, F.; Fléjou, J.F.; Praz, F. Microsatellite instability in colorectal cancer: From molecular oncogenic mechanisms to clinical implications. Cell Oncol. 2011, 34, 155–176. [Google Scholar] [CrossRef]
- Zaanan, A.; Taieb, J. How to better select patients with advanced gastric cancer for immunotherapy. Transl. Gastroenterol Hepatol. 2019, 4, 6. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | N. Cases (%) | pMMR | dMMR | lo-paMMR |
|---|---|---|---|---|
| 444 | 383 | 15 | 46 | |
| Age | ||||
| <67 | 181 (40.76%) | 156 (40.73%) | 8 (53.33%) | 17 (36.96%) |
| ≥67 | 263 (59.24%) | 227 (59.27%) | 7 (46.67%) | 29 (63.04%) |
| Sex | ||||
| male | 265 (59.68%) | 234 (61.1%) | 9 (60%) | 22 (47.83%) |
| female | 179 (40.32%) | 149 (38.9%) | 6 (40%) | 24 (52.17%) |
| Tumor site | ||||
| ascending colon | 123 (27.71%) | 91 (23.76%) | 8 (53.33%) | 24 (52.17%) |
| transverse colon | 7 (1.57%) | 4 (1.04%) | 0 | 3 (6.52%) |
| descending colon | 117 (26.36%) | 114 (29.76%) | 1 (6.67%) | 2 (4.35%) |
| sigma-rectum | 89 (20.04%) | 79 (20.63%) | 0 | 10 (21.74%) |
| metastatis | 24 (5.40%) | 20 (5.23%) | 2 (13.33%) | 2 (4.35%) |
| NA | 84 (18.92%) | 75 (19.58%) | 4 (26.67%) | 5 (10.87%) |
| Histological type | ||||
| adenocarcinoma | 407 (91.67%) | 366 (95.56%) | 11 (73.33%) | 30 (65.22%) |
| mucinous | 33 (7.21%) | 17 (4.44%) | 3 (20%) | 13 (28.26%) |
| signet ring cell | 4 (1.12%) | 0 | 1 (6.67%) | 3 (6.52%) |
| Grading | ||||
| G1 | 24 (5.40%) | 24 (5.40%) | 0 | 0 |
| G2 | 246 (55.41%) | 240 (62.66%) | 6 (40%) | 31 (67.39%) |
| G3 | 76 (17.12%) | 72 (18.80%) | 4 (26.67%) | 9 (19.57%) |
| NA | 98 (22.07%) | 93 (24.28%) | 5 (33.33%) | 6 (13.04%) |
| B-RAF status | ||||
| wt | 326 (73.42%) | 298 (77.80%) | 4 (26.67%) | 24 (52.17%) |
| mut | 26 (5.86%) | 12 (3.14%) | 5 (33.33%) | 9 (19.57%) |
| NA | 92 (20.72%) | 73 (19.06%) | 6 (40%) | 13 (28.26%) |
| K-RAS status | ||||
| wt | 199 (44.82%) | 170 (44.39%) | 7 (46.67%) | 22 (47.83%) |
| mut | 153 (34.46%) | 140 (36.55%) | 2 (13.33%) | 11 (23.91%) |
| NA | 92 (20.72%) | 73 (19.06%) | 6 (40%) | 13 (28.26%) |
| N-RAS status | ||||
| wt | 338 (76.13%) | 296 (77.29%) | 9 (60%) | 33 (71.74%) |
| mut | 14 (3.15%) | 14 (3.65%) | 0 | 0 |
| NA | 92 (20.72%) | 73 (19.06%) | 6 (40%) | 13 (28.26%) |
| dMMR-IHC | MSI-PCR | |||
|---|---|---|---|---|
| MSI-H | MSI-L | MSS | ||
| 15 dMMR | 13 | 2 | ||
| MLH1-PMS2 | 14 | 12 | 0 | 2 |
| MSH2-MSH6 | 1 | 1 | 0 | 0 |
| 46lo-paMMR | 13 | 3 | 30 | |
| 11 loss/1 MMR | ||||
| MLH1 | - | - | - | - |
| PMS2 | 9 | 6 | - | 3 |
| MSH2 | - | - | - | - |
| MSH6 | 2 | 2 | - | - |
| 31 patchy | ||||
| MLH1-PMS2 | 6 | 1 | - | 5 |
| MSH2-MSH6 | 1 | - | 1 | - |
| MLH1 | - | - | - | - |
| PMS2 | 23 | 2 | 2 | 19 |
| MSH2 | 1 | - | - | 1 |
| MSH6 | - | - | - | - |
| 4 loss/1 MMR patchy | ||||
| MLH1-PMS2 P and MSH6 lo | 1 | - | - | 1 |
| MLH1 P and PMS2 lo | 3 | 2 | - | 1 |
| Cases | MMR-IHC I OPINION | MMR-IHC II OPINION | MSI-PCR | Concordance of MMR-IHC I/II Opinion with PCR |
|---|---|---|---|---|
| 1 | PMS2 neg | MLH1-PMS2 neg | MSI-H | II |
| 2 | MLH1 patchy-PMS2 neg | MLH1-PMS2 neg | MSI-H | II |
| 3 | MLH1-PMS2 patchy | MLH1-PMS2 neg | MSS | I |
| 4 | PMS2 patchy | MLH1-PMS2 patchy | MSI-H | no |
| 5 | PMS2 patchy | PMS2 neg | MSS | I/II |
| 6 | PMS2 neg | PMS2 pos | MSS | I/II |
| Characteristics | N Cases (%) | pMMR | dMMR | lo-paMMR |
|---|---|---|---|---|
| 176 | 157 | 13 | 6 | |
| Age | ||||
| <65 | 95 (53.98%) | 92 (58.60%) | 3 (23.08%) | 0 |
| ≥65 | 81 (46.02%) | 65 (41.40%) | 10 (76.92%) | 6 (100%) |
| Sex | ||||
| male | 117 (66.48%) | 107 (68.15%) | 7 (53.85%) | 3 (50%) |
| female | 59 (33.52%) | 50 (31.85%) | 6 (46.15%) | 3 (50%) |
| Tumor site | ||||
| gastro-esophageal | 66 (37.49%) | 62 (39.49%) | 2 (15.38%) | 2 (33.33%) |
| junction | ||||
| antrum-body | 33 (18.19%) | 31 (19.74%) | 1 (7.69%) | 0 |
| body | 61 (34.66%) | 51 (32.49%) | 9 (69.24%) | 1 (16.67%) |
| metastasis | 4 (2.27%) | 4 (2.55%) | 0 | 0 |
| NA | 13 (7.39%) | 9 (5.73%) | 1 (7.69%) | 3 (50%) |
| Lauren typing | ||||
| intestinal type | 124 (70.45%) | 107 (68.15%) | 12 (92.31%) | 5 (83.33%) |
| diffuse type | 45 (25.57%) | 43 (27.39%) | 1 (7.69%) | 1 (16.67%) |
| mixed type | 7 (3.98%) | 7 (4.46%) | 0 | 0 |
| Grading | ||||
| G1 | 8 (4.54%) | 7 (4.46%) | 1 (7.69%) | 0 |
| G2 | 32 (18.18%) | 29 (18.47%) | 3 (23.07%) | 0 |
| G3 | 90 (51.14%) | 77 (49.04%) | 9 (69.24%) | 4 (66.66%) |
| NA | 46 (26.14%) | 44 (28.03%) | 0 | 2 (33.34%) |
| HER2 status | ||||
| negative | 135 (76.70%) | 120 (76.43%) | 10 (76.92%) | 5 (83.33%) |
| positive | 23 (13.07%) | 23 (14.65%) | 0 | 0 |
| NA | 18 (10.23%) | 14 (8.92%) | 3 (23.08%) | 1 (16.67%) |
| EBV status | ||||
| negative | 135 (76.70%) | 119 (75.80%) | 13 (100%) | 3 (50%) |
| positive | 1 (0.57%) | 0 | 0 | 1 (16.67%) |
| NA | 40 (22.73%) | 38 (24.20%) | 0 | 2 (33.33%) |
| PD-L1 status | ||||
| negative | 97 (55.11%) | 90 (57.32%) | 4 (30.77%) | 3 (50%) |
| positive | 48 (27.27%) | 42 (26.75%) | 4 (30.77%) | 2 (33.33%) |
| NA | 31 (17.62%) | 25 (15.93%) | 5 (38.46%) | 1 (16.67%) |
| dMMR-IHC | MSI-PCR | |||
|---|---|---|---|---|
| MSI-H | MSI-L | MSS | ||
| 13 dMMR | ||||
| MLH1-PMS2 | 13 | 12 | - | 1 |
| MSH2-MSH6 | - | - | - | - |
| 6 lo-paMMR | ||||
| 1 loss/1 MMR | ||||
| MLH1 | - | - | - | - |
| PMS2 | 1 | - | - | 1 |
| MSH2 | - | - | - | - |
| MSH6 | - | - | - | - |
| 5 patchy | ||||
| MLH1-PMS2 | 2 | - | - | 2 |
| MSH2-MSH6 | - | - | - | - |
| MLH1 | - | - | - | - |
| PMS2 | 3 | - | 1 | 2 |
| MSH2 | - | - | - | - |
| MSH6 | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zito Marino, F.; Amato, M.; Ronchi, A.; Panarese, I.; Ferraraccio, F.; De Vita, F.; Tirino, G.; Martinelli, E.; Troiani, T.; Facchini, G.; et al. Microsatellite Status Detection in Gastrointestinal Cancers: PCR/NGS Is Mandatory in Negative/Patchy MMR Immunohistochemistry. Cancers 2022, 14, 2204. https://doi.org/10.3390/cancers14092204
Zito Marino F, Amato M, Ronchi A, Panarese I, Ferraraccio F, De Vita F, Tirino G, Martinelli E, Troiani T, Facchini G, et al. Microsatellite Status Detection in Gastrointestinal Cancers: PCR/NGS Is Mandatory in Negative/Patchy MMR Immunohistochemistry. Cancers. 2022; 14(9):2204. https://doi.org/10.3390/cancers14092204
Chicago/Turabian StyleZito Marino, Federica, Martina Amato, Andrea Ronchi, Iacopo Panarese, Franca Ferraraccio, Ferdinando De Vita, Giuseppe Tirino, Erika Martinelli, Teresa Troiani, Gaetano Facchini, and et al. 2022. "Microsatellite Status Detection in Gastrointestinal Cancers: PCR/NGS Is Mandatory in Negative/Patchy MMR Immunohistochemistry" Cancers 14, no. 9: 2204. https://doi.org/10.3390/cancers14092204
APA StyleZito Marino, F., Amato, M., Ronchi, A., Panarese, I., Ferraraccio, F., De Vita, F., Tirino, G., Martinelli, E., Troiani, T., Facchini, G., Pirozzi, F., Perrotta, M., Incoronato, P., Addeo, R., Selvaggi, F., Lucido, F. S., Caraglia, M., Savarese, G., Sirica, R., ... Franco, R. (2022). Microsatellite Status Detection in Gastrointestinal Cancers: PCR/NGS Is Mandatory in Negative/Patchy MMR Immunohistochemistry. Cancers, 14(9), 2204. https://doi.org/10.3390/cancers14092204










