Validity of the Cancer and Aging Research Group Predictive Tool in Older Japanese Patients
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Design
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
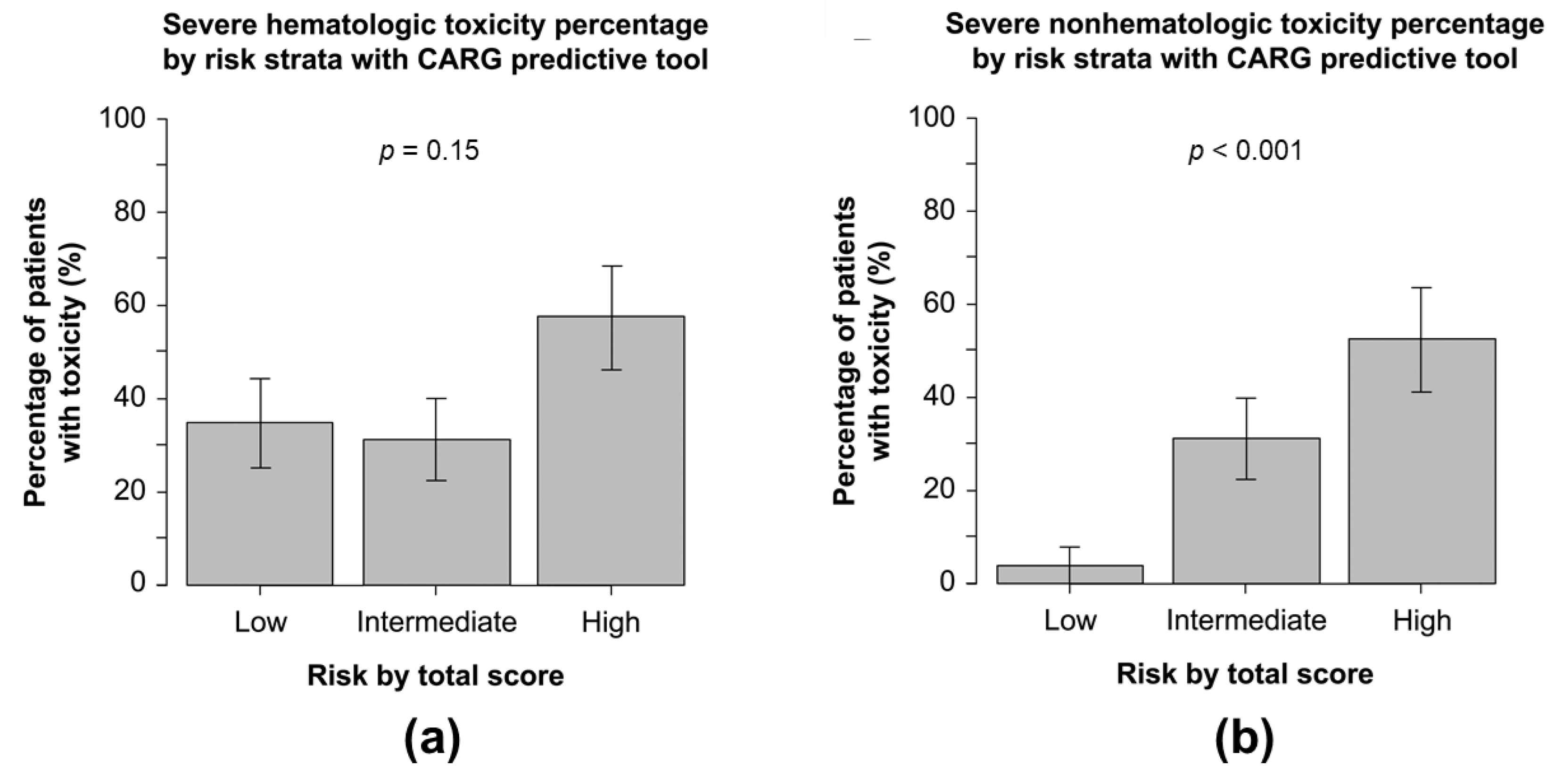
3.2. CRAEs
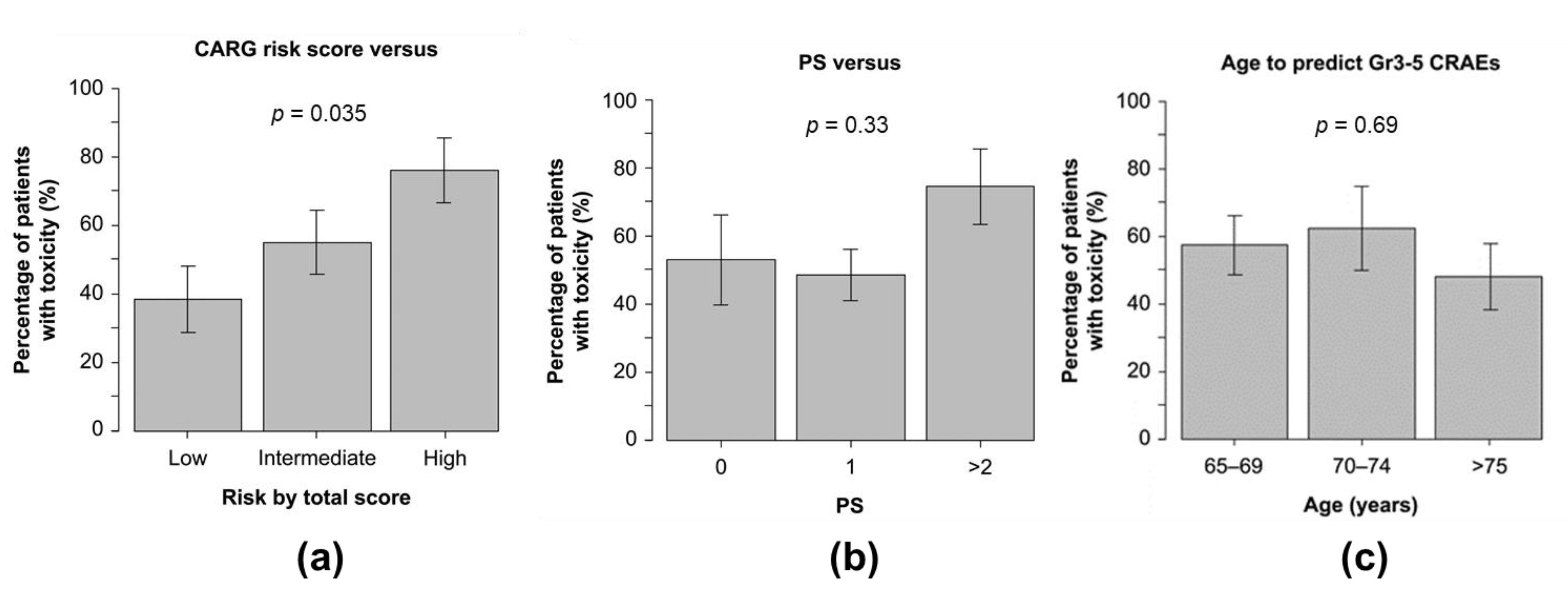
3.3. Ability of CARG Risk Score vs. ECOG PS vs. Age to Predict Grade 3–5 CRAEs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hori, M.; Matsuda, T.; Shibata, A.; Katanoda, K.; Sobue, T.; Nishimoto, H. Cancer incidence and incidence rates in Japan in 2009: A study of 32 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn. J. Clin. Oncol. 2015, 45, 884–891. [Google Scholar] [CrossRef] [PubMed]
- Langer, C.J.; Manola, J.; Bernardo, P.; Kugler, J.W.; Bonomi, P.; Cella, D.; Johnson, D.H. Cisplatin-based therapy for elderly patients with advanced non-small-cell lung cancer: Implications of Eastern Cooperative Oncology Group 5592, a randomized trial. J. Natl. Cancer Inst. 2002, 94, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Muss, H.B.; Berry, D.A.; Cirrincione, C.; Budman, D.R.; Henderson, I.C.; Citron, M.L.; Norton, L.; Winer, E.P.; Hudis, C.A. Toxicity of older and younger patients treated with adjuvant chemotherapy for node-positive breast cancer: The Cancer and Leukemia Group B Experience. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2007, 25, 3699–3704. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Soares, H.P.; Balducci, L.; Djulbegovic, B. Treatment tolerance and efficacy in geriatric oncology: A systematic review of phase III randomized trials conducted by five National Cancer Institute-sponsored cooperative groups. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2007, 25, 1272–1276. [Google Scholar] [CrossRef] [PubMed]
- Hurria, A.; Hurria, A.; Brogan, K.; Panageas, K.S.; Pearce, C.; Norton, L.; Jakubowski, A.; Howard, J.; Hudis, C. Effect of creatinine clearance on patterns of toxicity in older patients receiving adjuvant chemotherapy for breast cancer. Drugs Aging 2005, 22, 785–791. [Google Scholar] [CrossRef]
- Repetto, L. Greater risks of chemotherapy toxicity in elderly patients with cancer. J. Supportive Oncol. 2003, 1, 18–24. [Google Scholar]
- Chatta, G.S.; Price, T.H.; Stratton, J.R.; Dale, D.C. Aging and marrow neutrophil reserves. J. Am. Geriatr. Soc. 1994, 42, 77–81. [Google Scholar] [CrossRef]
- Vestal, R.E. Aging and pharmacology. Cancer 1997, 80, 1302–1310. [Google Scholar] [CrossRef]
- Williams, G.R.; Mackenzie, A.; Magnuson, A.; Olin, R.; Chapman, A.; Mohile, S.; Allore, H.; Somerfield, M.R.; Targia, V.; Extermann, M.; et al. Comorbidity in older adults with cancer. J. Geriatr. Oncol. 2016, 7, 249–257. [Google Scholar] [CrossRef] [Green Version]
- Nightingale, G.; Hajjar, E.; Swartz, K.; Andrel-Sendecki, J.; Chapman, A. Evaluation of a pharmacist-led medication assessment used to identify prevalence of and associations with polypharmacy and potentially inappropriate medication use among ambulatory senior adults with cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 1453–1459. [Google Scholar] [CrossRef]
- Hurria, A.; Togawa, K.; Mohile, S.G.; Owusu, C.; Klepin, H.D.; Gross, C.P.; Lichtman, S.M.; Gajra, A.; Bhatia, S.; Katheria, V.; et al. Predicting chemotherapy toxicity in older adults with cancer: A prospective multicenter study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2011, 29, 3457–3465. [Google Scholar] [CrossRef] [Green Version]
- Hurria, A.; Mohile, S.; Gajra, A.; Klepin, H.; Muss, H.; Chapman, A.; Feng, T.; Smith, D.; Sun, C.L.; De Glas, N.; et al. Validation of a Prediction Tool for Chemotherapy Toxicity in Older Adults With Cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2016, 34, 2366–2371. [Google Scholar] [CrossRef]
- Mohile, S.G.; Dale, W.; Somerfield, M.R.; Schonberg, M.A.; Boyd, C.M.; Burhenn, P.S.; Canin, B.; Cohen, H.J.; Holmes, H.M.; Hopkins, J.O.; et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy: ASCO Guideline for Geriatric Oncology. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2018, 36, 2326–2347. [Google Scholar] [CrossRef]
- Ling, W.H.; Lee, S.C. Inter-ethnic differences--how important is it in cancer treatment? Ann. Acad. Med. Singap. 2011, 40, 356–361. [Google Scholar]
- Iwamoto, M.; Nakamura, F.; Higashi, T. Estimated life expectancy and risk of death from cancer by quartiles in the older Japanese population: 2010 vital statistics. Cancer Epidemiol. 2014, 38, 511–514. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [Green Version]
- Lewis, J.H.; Kilgore, M.L.; Goldman, D.P.; Trimble, E.L.; Kaplan, R.; Montello, M.J.; Housman, M.G.; Escarce, J.J. Participation of patients 65 years of age or older in cancer clinical trials. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2003, 21, 1383–1389. [Google Scholar] [CrossRef]
- Murthy, V.H.; Krumholz, H.M.; Gross, C.P. Participation in cancer clinical trials: Race-, sex-, and age-based disparities. JAMA 2004, 291, 2720–2726. [Google Scholar] [CrossRef]
- Abbasi, J. Older Patients (Still) Left Out of Cancer Clinical Trials. JAMA 2019, 322, 1751–1753. [Google Scholar] [CrossRef]
- Nie, X.; Liu, D.; Li, Q.; Bai, C. Predicting chemotherapy toxicity in older adults with lung cancer. J. Geriatr. Oncol. 2013, 4, 334–339. [Google Scholar] [CrossRef]
- Kotzerke, D.; Moritz, F.; Mantovani, L.; Hambsch, P.; Hering, K.; Kuhnt, T.; Yahiaoui-Doktor, M.; Forstmeyer, D.; Lordick, F.; Knödler, M. The performance of three oncogeriatric screening tools—G8, optimised G8 and CARG—in predicting chemotherapy-related toxicity in older patients with cancer. A prospective clinical study. J. Geriatr. Oncol. 2019, 10, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Liao, X.; Feng, J.; Yin, T.; Liang, Y. Prospective comparison of the value of CRASH and CARG toxicity scores in predicting chemotherapy toxicity in geriatric oncology. Oncol. Lett. 2019, 18, 4947–4955. [Google Scholar] [CrossRef] [PubMed]
- Ortland, I.; Mendel Ott, M.; Kowar, M.; Sippel, C.; Jaehde, U.; Jacobs, A.H.; Ko, Y.D. Comparing the performance of the CARG and the CRASH score for predicting toxicity in older patients with cancer. J. Geriatr. Oncol. 2020, 11, 997–1005. [Google Scholar] [CrossRef]
- Yoshida, H.; Shintani, D.; Kawashima, N.; Fujiwara, K. Predicting toxicity of platinum and taxane-based chemotherapy in older patients with gynecologic cancer. J. BUON Off. J. Balk. Union Oncol. 2020, 25, 736–742. [Google Scholar]
- Ostwal, V.; Ramaswamy, A.; Bhargava, P.; Hatkhambkar, T.; Swami, R.; Rastogi, S.; Mandavkar, S.; Ghosh, J.; Bajpai, J.; Gulia, S.; et al. Cancer Aging Research Group (CARG) score in older adults undergoing curative intent chemotherapy: A prospective cohort study. BMJ Open 2021, 11, e047376. [Google Scholar] [CrossRef] [PubMed]
- Moth, E.B.; Kiely, B.E.; Stefanic, N.; Naganathan, V.; Martin, A.; Grimison, P.; Stockler, M.R.; Beale, P.; Blinman, P. Predicting chemotherapy toxicity in older adults: Comparing the predictive value of the CARG Toxicity Score with oncologists’ estimates of toxicity based on clinical judgement. J. Geriatr. Oncol. 2019, 10, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.L.; Ma, T.; Cheung, K.L.; Choi, H.; Wong, J.; Lam, K.O.; Yuen, K.K.; Luk, M.Y.; Kwong, D. The predictive value of G8 and the Cancer and aging research group chemotherapy toxicity tool in treatment-related toxicity in older Chinese patients with cancer. J. Geriatr. Oncol. 2021, 12, 557–562. [Google Scholar] [CrossRef]
- Alibhai, S.M.; Aziz, S.; Manokumar, T.; Timilshina, N.; Breunis, H. A comparison of the CARG tool, the VES-13, and oncologist judgment in predicting grade 3+ toxicities in men undergoing chemotherapy for metastatic prostate cancer. J. Geriatr. Oncol. 2017, 8, 31–36. [Google Scholar] [CrossRef]
- Ben Ayed, W.; Ben Said, A.; Hamdi, A.; Mokrani, A.; Masmoudi, Y.; Toukabri, I.; Limayem, I.; Yahyaoui, Y. Toxicity, risk factors and management of cisplatin-induced toxicity: A prospective study. J. Oncol. Pharm. Pract. Off. Publ. Int. Soc. Oncol. Pharm. Pract. 2020, 26, 1621–1629. [Google Scholar] [CrossRef]
- Kilpatrick, K.; Shaw, J.L.; Jaramillo, R.; Toler, A.; Eisen, M.; Sangaré, L.; Soff, G.A. Occurrence and Management of Thrombocytopenia in Metastatic Colorectal Cancer Patients Receiving Chemotherapy: Secondary Analysis of Data From Prospective Clinical Trials. Clin. Colorectal Cancer 2021, 20, 170–176. [Google Scholar] [CrossRef]
- Muro, K.; Oh, S.C.; Shimada, Y.; Lee, K.W.; Yen, C.J.; Chao, Y.; Cho, J.Y.; Cheng, R.; Carlesi, R.; Chandrawansa, K.; et al. Subgroup analysis of East Asians in RAINBOW: A phase 3 trial of ramucirumab plus paclitaxel for advanced gastric cancer. J. Gastroenterol. Hepatol. 2016, 31, 581–589. [Google Scholar] [CrossRef]
- Shitara, K.; Muro, K.; Shimada, Y.; Hironaka, S.; Sugimoto, N.; Komatsu, Y.; Nishina, T.; Yamaguchi, K.; Segawa, Y.; Omuro, Y.; et al. Subgroup analyses of the safety and efficacy of ramucirumab in Japanese and Western patients in RAINBOW: A randomized clinical trial in second-line treatment of gastric cancer. Gastric Cancer Off. J. Int. Gastric Cancer Assoc. Jpn. Gastric Cancer Assoc. 2016, 19, 927–938. [Google Scholar] [CrossRef]
- Park, K.; Kim, J.H.; Cho, E.K.; Kang, J.H.; Shih, J.Y.; Zimmermann, A.H.; Lee, P.; Alexandris, E.; Puri, T.; Orlando, M. East Asian Subgroup Analysis of a Randomized, Double-Blind, Phase 3 Study of Docetaxel and Ramucirumab Versus Docetaxel and Placebo in the Treatment of Stage IV Non-small Cell Lung Cancer Following Disease Progression after One Prior Platinum-Based Therapy (REVEL). Cancer Res. Treat. 2016, 48, 1177–1186. [Google Scholar] [CrossRef]
- Tabernero, J.; Hoff, P.M.; Shen, L.; Ohtsu, A.; Shah, M.A.; Cheng, K.; Song, C.; Wu, H.; Eng-Wong, J.; Kim, K.; et al. Pertuzumab plus trastuzumab and chemotherapy for HER2-positive metastatic gastric or gastro-oesophageal junction cancer (JACOB): Final analysis of a double-blind, randomised, placebo-controlled phase 3 study. Lancet. Oncol. 2018, 19, 1372–1384. [Google Scholar] [CrossRef]
- Shitara, K.; Hara, H.; Yoshikawa, T.; Fujitani, K.; Nishina, T.; Hosokawa, A.; Asakawa, T.; Kawakami, S.; Muro, K. Pertuzumab plus trastuzumab and chemotherapy for Japanese patients with HER2-positive metastatic gastric or gastroesophageal junction cancer: A subgroup analysis of the JACOB trial. Int. J. Clin. Oncol. 2020, 25, 301–311. [Google Scholar] [CrossRef] [Green Version]
- Kudo, M.; Finn, R.S.; Qin, S.; Han, K.H.; Ikeda, K.; Piscaglia, F.; Baron, A.; Park, J.W.; Han, G.; Jassem, J.; et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomised phase 3 non-inferiority trial. Lancet 2018, 391, 1163–1173. [Google Scholar] [CrossRef] [Green Version]
- Yamashita, T.; Kudo, M.; Ikeda, K.; Izumi, N.; Tateishi, R.; Ikeda, M.; Aikata, H.; Kawaguchi, Y.; Wada, Y.; Numata, K.; et al. REFLECT-a phase 3 trial comparing efficacy and safety of lenvatinib to sorafenib for the treatment of unresectable hepatocellular carcinoma: An analysis of Japanese subset. J. Gastroenterol. 2020, 55, 113–122. [Google Scholar] [CrossRef] [Green Version]
- Decoster, L.; Van Puyvelde, K.; Mohile, S.; Wedding, U.; Basso, U.; Colloca, G.; Rostoft, S.; Overcash, J.; Wildiers, H.; Steer, C.; et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: An update on SIOG recommendations. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2015, 26, 288–300. [Google Scholar] [CrossRef]
- Garcia, M.V.; Agar, M.R.; Soo, W.K.; To, T.; Phillips, J.L. Screening Tools for Identifying Older Adults With Cancer Who May Benefit From a Geriatric Assessment: A Systematic Review. JAMA Oncol. 2021, 7, 616–627. [Google Scholar] [CrossRef]
- Extermann, M.; Boler, I.; Reich, R.R.; Lyman, G.H.; Brown, R.H.; DeFelice, J.; Levine, R.M.; Lubiner, E.T.; Reyes, P.; Schreiber, F.J., 3rd; et al. Predicting the risk of chemotherapy toxicity in older patients: The Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer 2012, 118, 3377–3386. [Google Scholar] [CrossRef]
- Seymour, M.T.; Thompson, L.C.; Wasan, H.S.; Middleton, G.; Brewster, A.E.; Shepherd, S.F.; O’Mahony, M.S.; Maughan, T.S.; Parmar, M.; Langley, R.E. Chemotherapy options in elderly and frail patients with metastatic colorectal cancer (MRC FOCUS2): An open-label, randomised factorial trial. Lancet 2011, 377, 1749–1759. [Google Scholar] [CrossRef] [Green Version]
- Cunningham, D.; Lang, I.; Marcuello, E.; Lorusso, V.; Ocvirk, J.; Shin, D.B.; Jonker, D.; Osborne, S.; Andre, N.; Waterkamp, D.; et al. Bevacizumab plus capecitabine versus capecitabine alone in elderly patients with previously untreated metastatic colorectal cancer (AVEX): An open-label, randomised phase 3 trial. Lancet. Oncol. 2013, 14, 1077–1085. [Google Scholar] [CrossRef]
- Mohile, S.G.; Mohamed, M.R.; Xu, H.; Culakova, E.; Loh, K.P.; Magnuson, A.; Flannery, M.A.; Obrecht, S.; Gilmore, N.; Ramsdale, E.; et al. Evaluation of geriatric assessment and management on the toxic effects of cancer treatment (GAP70+): A cluster-randomised study. Lancet 2021, 398, 1894–1904. [Google Scholar] [CrossRef]
| Characteristics | No. | % |
|---|---|---|
| Age (years) | ||
| 65–69 | 33 | 43 |
| 70–74 | 16 | 21 |
| 75–79 | 20 | 26 |
| ≥80 | 7 | 9 |
| Sex | ||
| Male | 44 | 58 |
| Female | 32 | 42 |
| ECOG PS | ||
| 0 | 15 | 20 |
| 1 | 45 | 59 |
| ≥2 | 16 | 21 |
| Cancer type | ||
| Breast | 7 | 9 |
| Lung | 6 | 8 |
| GI | 41 | 54 |
| GYN | 3 | 4 |
| GU | 1 | 1 |
| Other | 18 | 24 |
| Stage | ||
| I | 2 | 3 |
| II | 2 | 3 |
| III | 8 | 10 |
| IV | 63 | 83 |
| Other | 1 | 1 |
| Treatment | ||
| Standard dose | ||
| Yes | 53 | 70 |
| No | 23 | 30 |
| No. of chemo drugs | ||
| Monochemotherapy | 40 | 53 |
| Polychemotherapy | 36 | 47 |
| Line of chemotherapy | ||
| First line | 25 | 33 |
| ≥Second line | 51 | 67 |
| Growth factor use | ||
| Yes | 11 | 14 |
| No | 65 | 86 |
| Hemoglobin | ||
| <10 g/dL (female) | 16 | 21 |
| ≥10 g/dL (female) | 16 | 21 |
| <11 g/dL (male) | 20 | 26 |
| ≥11 g/dL (male) | 24 | 32 |
| Creatinine clearance | ||
| <34 mL/min | 5 | 7 |
| ≥34 mL/min | 71 | 93 |
| Hearing | ||
| Fair, poor, or totally deaf | 4 | 5 |
| Excellent or good | 72 | 95 |
| No. of falls in the past 6 months | ||
| ≥1 | 1 | 1 |
| None | 75 | 99 |
| Taking medications | ||
| With some help/unable | 10 | 13 |
| Without help | 66 | 87 |
| Limited in walking 100 m | ||
| Somewhat limited/limited a lot | 24 | 32 |
| Not limited | 52 | 68 |
| Decreased social activity because of | ||
| health/emotional problems | ||
| Some, most, all of the time | 27 | 36 |
| A little, or none of the time | 49 | 64 |
| CCI | ||
| 0 (low) | 0 | 0 |
| 1–2 (medium) | 4 | 5 |
| 3–4 (high) | 7 | 9 |
| ≥5 (very high) | 65 | 86 |
| CARG | ||
| 0–5 (low) | 26 | 34 |
| 6–9 (intermediate) | 29 | 38 |
| ≥10 (high) | 21 | 28 |
| Grade 3–5 CRAEs | CARG Risk Score Low (0–5) No. % | CARG Risk Score Intermediate (6–9) No. % | CARG Risk Score High (≥10) No. % |
|---|---|---|---|
| Hematologic | |||
| Leukopenia | 6 23 | 4 14 | 4 19 |
| Neutropenia | 9 35 | 9 31 | 3 14 |
| Anemia | 1 4 | 1 3 | 9 43 |
| Thrombocytopenia | 1 4 | 0 0 | 1 5 |
| Febrile neutropenia | 2 8 | 0 0 | 1 5 |
| Non-hematologic | |||
| Fatigue | 1 4 | 1 3 | 10 48 |
| Nausea | 0 0 | 2 7 | 10 48 |
| Mucositis oral | 0 0 | 0 0 | 3 14 |
| Diarrhea | 0 0 | 1 3 | 0 0 |
| Hypertension | 0 0 | 1 3 | 0 0 |
| Proteinuria | 0 0 | 1 3 | 0 0 |
| Edema | 0 0 | 0 0 | 1 5 |
| Hyponatremia | 0 0 | 1 3 | 1 5 |
| Hyperkalemia | 0 0 | 1 3 | 1 5 |
| Hypomagnesemia | 0 0 | 1 3 | 0 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suto, H.; Inui, Y.; Okamura, A. Validity of the Cancer and Aging Research Group Predictive Tool in Older Japanese Patients. Cancers 2022, 14, 2075. https://doi.org/10.3390/cancers14092075
Suto H, Inui Y, Okamura A. Validity of the Cancer and Aging Research Group Predictive Tool in Older Japanese Patients. Cancers. 2022; 14(9):2075. https://doi.org/10.3390/cancers14092075
Chicago/Turabian StyleSuto, Hirotaka, Yumiko Inui, and Atsuo Okamura. 2022. "Validity of the Cancer and Aging Research Group Predictive Tool in Older Japanese Patients" Cancers 14, no. 9: 2075. https://doi.org/10.3390/cancers14092075
APA StyleSuto, H., Inui, Y., & Okamura, A. (2022). Validity of the Cancer and Aging Research Group Predictive Tool in Older Japanese Patients. Cancers, 14(9), 2075. https://doi.org/10.3390/cancers14092075





