Cost-Effectiveness of Artificial Intelligence Support in Computed Tomography-Based Lung Cancer Screening
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
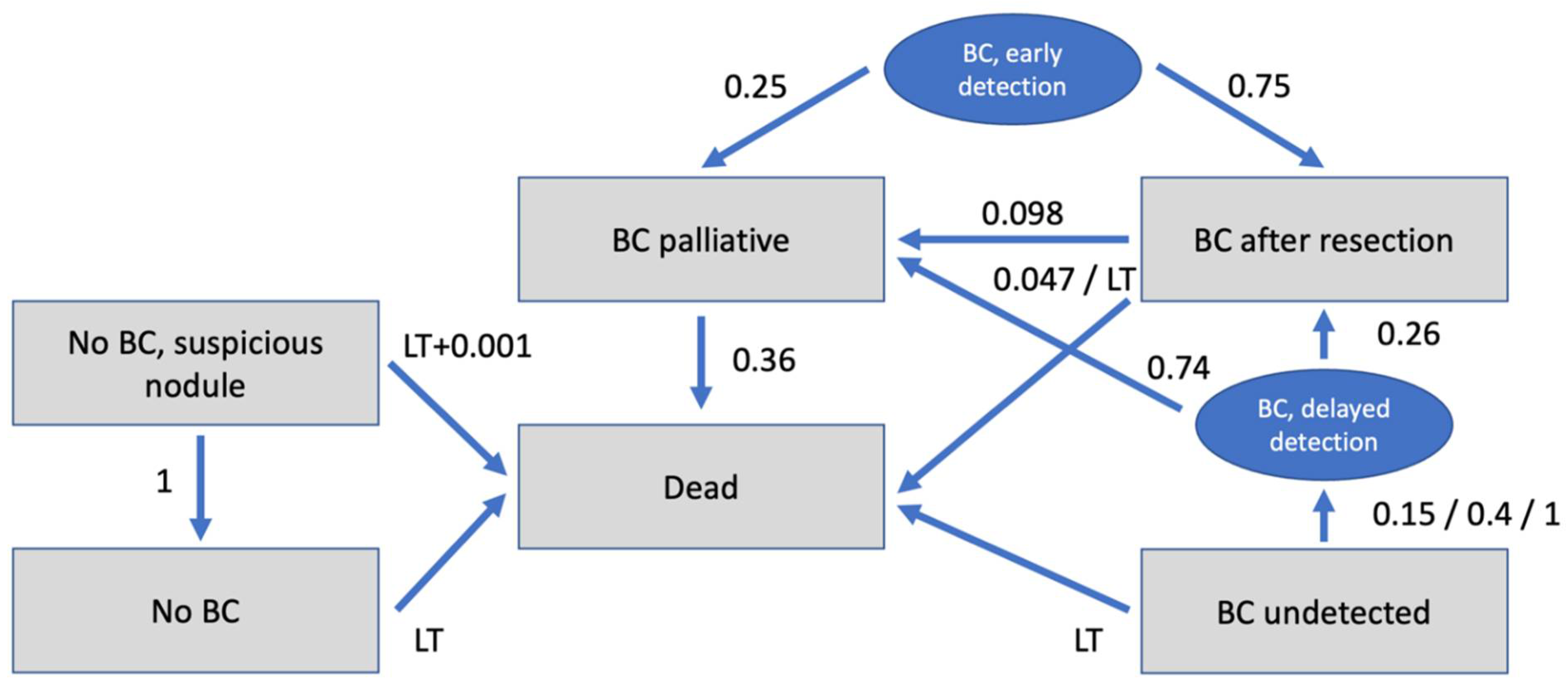
2.1. Model Structure
- No BC (patients without BC = true negative);
- No BC, Suspicious nodule (patients without BC but suspicious nodule = false positive);
- BC undetected (patients with undetected BC = false negative);
- BC after resection (patients with BC after resection);
- BC palliative (patients with BC which is unresectable/palliative);
- Dead.
2.2. Input Parameters
2.3. Diagnostic Test Performances
2.4. Costs
2.5. Utilities
2.6. Transition Probabilities
2.7. Cost-Effectiveness Analysis
3. Results
3.1. Cost-Effectiveness Analysis
3.2. Sensitivity Analysis
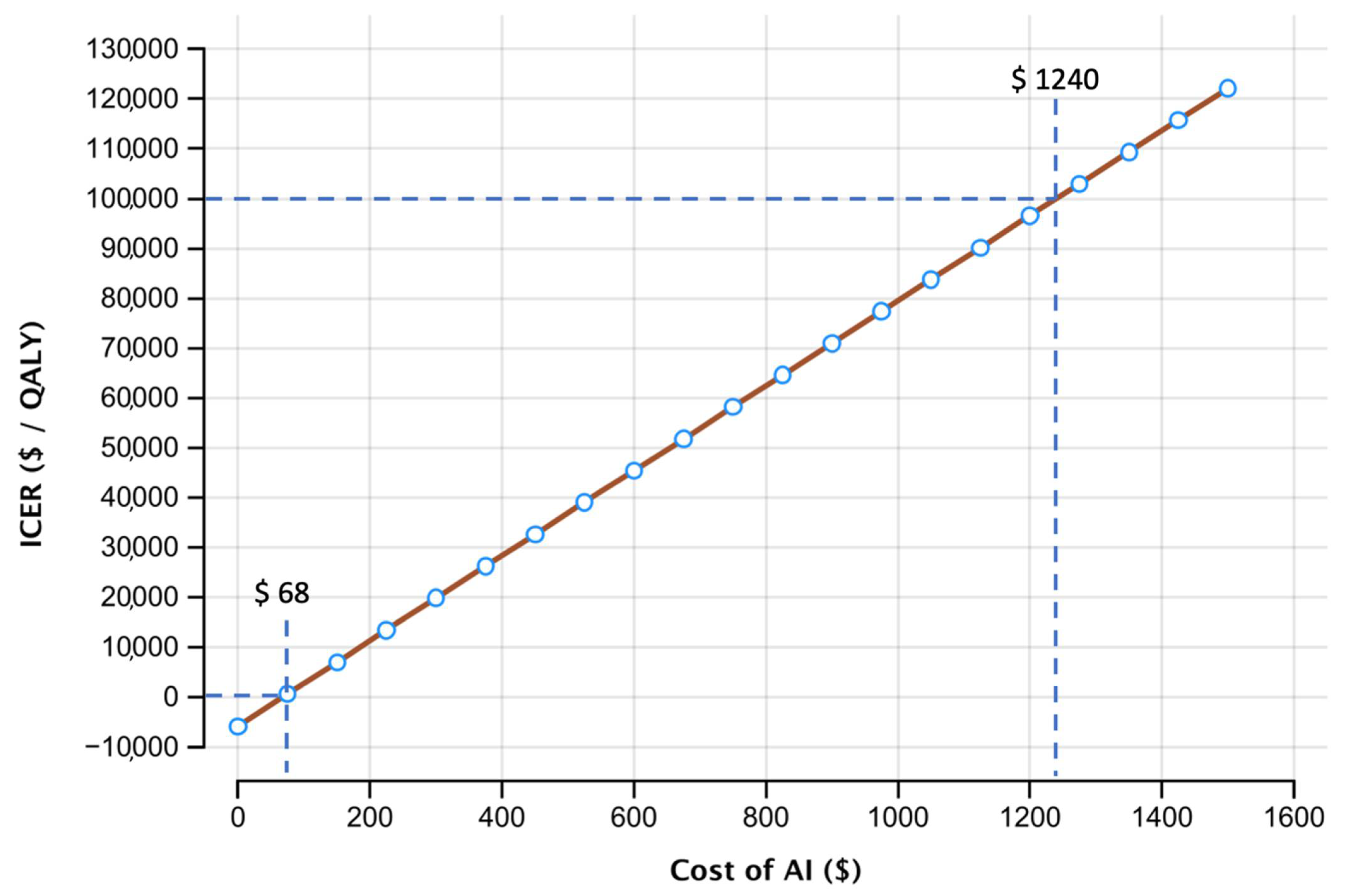
3.3. Threshold Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moyer Virginia, A. On behalf of the us preventive services task force screening for lung cancer: Us preventive services task force recommendation statement. Ann. Intern. Med. 2014, 160, 330–338. [Google Scholar]
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef] [PubMed]
- Oudkerk, M.; Devaraj, A.; Vliegenthart, R.; Henzler, T.; Prosch, H.; Heussel, C.P.; Bastarrika, G.; Sverzellati, N.; Mascalchi, M.; Delorme, S. European position statement on lung cancer screening. Lancet Oncol. 2017, 18, e754–e766. [Google Scholar] [PubMed]
- De Koning, H.J.; van der Aalst, C.M.; de Jong, P.A.; Scholten, E.T.; Nackaerts, K.; Heuvelmans, M.A.; Lammers, J.-W.J.; Weenink, C.; Yousaf-Khan, U.; Horeweg, N. Reduced lung-cancer mortality with volume ct screening in a randomized trial. N. Engl. J. Med. 2020, 382, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, J.F.; Siersma, V.; Pedersen, J.H.; Heleno, B.; Saghir, Z.; Brodersen, J. Healthcare costs in the danish randomised controlled lung cancer ct-screening trial: A registry study. Lung Cancer 2014, 83, 347–355. [Google Scholar] [CrossRef]
- Wiener, R.S.; Schwartz, L.M.; Woloshin, S.; Welch, H.G. Population-based risk for complications after transthoracic needle lung biopsy of a pulmonary nodule: An analysis of discharge records. Ann. Intern. Med. 2011, 155, 137–144. [Google Scholar] [CrossRef]
- Kastner, J.; Hossain, R.; Jeudy, J.; Dako, F.; Mehta, V.; Dalal, S.; Dharaiya, E.; White, C. Lung-rads version 1.0 versus lung-rads version 1.1: Comparison of categories using nodules from the national lung screening trial. Radiology 2021, 300, 203704. [Google Scholar]
- McKee, B.J.; Regis, S.M.; McKee, A.B.; Flacke, S.; Wald, C. Performance of acr lung-rads in a clinical ct lung screening program. J. Am. Coll. Radiol. 2016, 13, R25–R29. [Google Scholar] [CrossRef]
- Mehta, H.J.; Mohammed, T.-L.; Jantz, M.A. The american college of radiology lung imaging reporting and data system: Potential drawbacks and need for revision. Chest 2017, 151, 539–543. [Google Scholar] [CrossRef]
- Singh, S.; Pinsky, P.; Fineberg, N.S.; Gierada, D.S.; Garg, K.; Sun, Y.; Nath, P.H. Evaluation of reader variability in the interpretation of follow-up ct scans at lung cancer screening. Radiology 2011, 259, 263–270. [Google Scholar] [CrossRef]
- McKinney, S.M.; Sieniek, M.; Godbole, V.; Godwin, J.; Antropova, N.; Ashrafian, H.; Back, T.; Chesus, M.; Corrado, G.S.; Darzi, A. International evaluation of an ai system for breast cancer screening. Nature 2020, 577, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.S.; Goldin, J.G.; Rogers, S.; Kim, H.J.; Suh, R.D.; McNitt-Gray, M.F.; Shah, S.K.; Truong, D.; Brown, K.; Sayre, J.W. Computer-aided lung nodule detection in ct: Results of large-scale observer test1. Acad. Radiol. 2005, 12, 681–686. [Google Scholar] [CrossRef] [PubMed]
- De Hoop, B.; de Boo, D.W.; Gietema, H.A.; van Hoorn, F.; Mearadji, B.; Schijf, L.; van Ginneken, B.; Prokop, M.; Schaefer-Prokop, C. Computer-aided detection of lung cancer on chest radiographs: Effect on observer performance. Radiology 2010, 257, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Jeon, K.N.; Goo, J.M.; Lee, C.H.; Lee, Y.; Choo, J.Y.; Lee, N.K.; Shim, M.-S.; Lee, I.S.; Kim, K.G.; Gierada, D.S. Computer-aided nodule detection and volumetry to reduce variability between radiologists in the interpretation of lung nodules at low-dose screening ct. Investig. Radiol. 2012, 47, 457. [Google Scholar] [CrossRef]
- Ardila, D.; Kiraly, A.P.; Bharadwaj, S.; Choi, B.; Reicher, J.J.; Peng, L.; Tse, D.; Etemadi, M.; Ye, W.; Corrado, G. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 2019, 25, 954–961. [Google Scholar] [CrossRef]
- Arias, E.; Xu, J.; Kochanek, K.D. United states life tables, 2016. Natl. Vital Stat. Rep. 2019, 68, 4. [Google Scholar]
- Cameron, D.; Ubels, J. Norstr öm f: On what basis are medical cost-effectiveness thresholds set. Clashing Opin. Absence Data A Syst. Rev. Glob. Health Action 2018, 11, 1447828. [Google Scholar] [CrossRef]
- Sanders, G.D.; Neumann, P.J.; Basu, A.; Brock, D.W.; Feeny, D.; Krahn, M.; Kuntz, K.M.; Meltzer, D.O.; Owens, D.K.; Prosser, L.A. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: Second panel on cost-effectiveness in health and medicine. JAMA 2016, 316, 1093–1103. [Google Scholar] [CrossRef]
- Jacob, L.; Freyn, M.; Kalder, M.; Dinas, K.; Kostev, K. Impact of tobacco smoking on the risk of developing 25 different cancers in the uk: A retrospective study of 422,010 patients followed for up to 30 years. Oncotarget 2018, 9, 17420. [Google Scholar] [CrossRef]
- Procedure Price Lookup for Outpatient Services. Medicare.gov 71275. 2021. Available online: https://www.medicare.gov/procedure-price-lookup/cost/71275/ (accessed on 9 January 2022).
- Ten Haaf, K.; Tammemägi, M.C.; Bondy, S.J.; van der Aalst, C.M.; Gu, S.; McGregor, S.E.; Nicholas, G.; de Koning, H.J.; Paszat, L.F. Performance and cost-effectiveness of computed tomography lung cancer screening scenarios in a population-based setting: A microsimulation modeling analysis in Ontario, Canada. PLoS Med. 2017, 14, e1002225. [Google Scholar] [CrossRef]
- Cowper, P.A.; Feng, L.; Kosinski, A.S.; Tong, B.C.; Habib, R.H.; Putnam, J.B., Jr.; Onaitis, M.W.; Furnary, A.P.; Wright, C.D.; Jacobs, J.P. Initial and longitudinal cost of surgical resection for lung cancer. Ann. Thorac. Surg. 2021, 111, 1827–1833. [Google Scholar] [CrossRef] [PubMed]
- Gareen, I.F.; Duan, F.; Greco, E.M.; Snyder, B.S.; Boiselle, P.M.; Park, E.R.; Fryback, D.; Gatsonis, C. Impact of lung cancer screening results on participant health-related quality of life and state anxiety in the national lung screening trial. Cancer 2014, 120, 3401–3409. [Google Scholar] [CrossRef] [PubMed]
- Grutters, J.P.; Joore, M.A.; Wiegman, E.M.; Langendijk, J.A.; de Ruysscher, D.; Hochstenbag, M.; Botterweck, A.; Lambin, P.; Pijls-Johannesma, M. Health-related quality of life in patients surviving non-small cell lung cancer. Thorax 2010, 65, 903–907. [Google Scholar] [CrossRef]
- Möller, A.; Sartipy, U. Long-term health-related quality of life following surgery for lung cancer. Eur. J. Cardio-Thorac. Surg. 2012, 41, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Doyle, S.; Lloyd, A.; Walker, M. Health state utility scores in advanced non-small cell lung cancer. Lung Cancer 2008, 62, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Green, A.; Hauge, J.; Iachina, M.; Jakobsen, E. The mortality after surgery in primary lung cancer: Results from the danish lung cancer registry. Eur. J. Cardio-Thorac. Surg. 2016, 49, 589–594. [Google Scholar] [CrossRef]
- Toker, A.; Dilege, S.; Ziyade, S.; Eroglu, O.; Tanju, S.; Yilmazbayhan, D.; Kilicarslan, Z.; Kalayci, G. Causes of death within 1 year of resection for lung cancer. Early mortality after resection. Eur. J. Cardio-Thorac. Surg. 2004, 25, 515–519. [Google Scholar] [CrossRef][Green Version]
- Lou, F.; Huang, J.; Sima, C.S.; Dycoco, J.; Rusch, V.; Bach, P.B. Patterns of recurrence and second primary lung cancer in early-stage lung cancer survivors followed with routine computed tomography surveillance. J. Thorac. Cardiovasc. Surg. 2013, 145, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Scholten, E.T.; Horeweg, N.; de Koning, H.J.; Vliegenthart, R.; Oudkerk, M.; Willem, P.T.M.; de Jong, P.A. Computed tomographic characteristics of interval and post screen carcinomas in lung cancer screening. Eur. Radiol. 2015, 25, 81–88. [Google Scholar] [CrossRef]
- Thorsteinsson, H.; Alexandersson, A.; Oskarsdottir, G.N.; Skuladottir, R.; Isaksson, H.J.; Jonsson, S.; Gudbjartsson, T. Resection rate and outcome of pulmonary resections for non–small-cell lung cancer: A nationwide study from iceland. J. Thorac. Oncol. 2012, 7, 1164–1169. [Google Scholar] [CrossRef]
- Cancer Stat Facts: Lung and Bronchus Cancer. 2021. Available online: https://seer.cancer.gov/statfacts/html/lungb.html (accessed on 9 January 2022).
- Goldstein, I.M.; Lawrence, J.; Miner, A.S. Human-machine collaboration in cancer and beyond: The centaur care model. JAMA Oncol. 2017, 3, 1303–1304. [Google Scholar] [CrossRef] [PubMed]
- Liang, M.; Tang, W.; Xu, D.M.; Jirapatnakul, A.C.; Reeves, A.P.; Henschke, C.I.; Yankelevitz, D. Low-dose ct screening for lung cancer: Computer-aided detection of missed lung cancers. Radiology 2016, 281, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.; Pauling, J.; Keck, A.; Baumbach, J. Systematic review of economic impact studies of artificial intelligence in health care. J. Med. Internet Res. 2020, 22, e16866. [Google Scholar] [CrossRef] [PubMed]
- Pastorino, U.; Rossi, M.; Rosato, V.; Marchianò, A.; Sverzellati, N.; Morosi, C.; Fabbri, A.; Galeone, C.; Negri, E.; Sozzi, G. Annual or biennial ct screening versus observation in heavy smokers: 5-year results of the mild trial. Eur. J. Cancer Prev. 2012, 21, 308–315. [Google Scholar] [CrossRef]
- Van Klaveren, R.J.; Oudkerk, M.; Prokop, M.; Scholten, E.T.; Nackaerts, K.; Vernhout, R.; van Iersel, C.A.; van den Bergh, K.A.; Westeinde, S.V.; van der Aalst, C. Management of lung nodules detected by volume ct scanning. N. Engl. J. Med. 2009, 361, 2221–2229. [Google Scholar] [CrossRef]
- Van den Bergh, K.A.; Essink-Bot, M.-L.; Borsboom, G.J.; Scholten, E.T.; Prokop, M.; de Koning, H.J.; van Klaveren, R.J. Short-term health-related quality of life consequences in a lung cancer ct screening trial (nelson). Br. J. Cancer 2010, 102, 27–34. [Google Scholar] [CrossRef]
- Jonas, D.E.; Reuland, D.S.; Reddy, S.M.; Nagle, M.; Clark, S.D.; Weber, R.P.; Enyioha, C.; Malo, T.L.; Brenner, A.T.; Armstrong, C. Screening for lung cancer with low-dose computed tomography: Updated evidence report and systematic review for the us preventive services task force. JAMA 2021, 325, 971–987. [Google Scholar] [CrossRef]
- Audelan, B.; Lopez, S.; Fillard, P.; Diascorn, Y.; Padovani, B.; Delingette, H. Validation of Lung Nodule Detection a Year before Diagnosis in Nlst Dataset Based on a Deep Learning System; European Respiratory Society: Lausanne, Switzerland, 2021. [Google Scholar]
- Hoverman, J.R.; Klein, I.; Harrison, D.W.; Hayes, J.E.; Garey, J.S.; Harrell, R.; Sipala, M.; Houldin, S.; Jameson, M.D.; Abdullahpour, M. Opening the black box: The impact of an oncology management program consisting of level i pathways and an outbound nurse call system. J. Oncol. Pract. 2014, 10, 63–67. [Google Scholar] [CrossRef][Green Version]
- Peng, S.; Liu, Y.; Lv, W.; Liu, L.; Zhou, Q.; Yang, H.; Ren, J.; Liu, G.; Wang, X.; Zhang, X. Deep learning-based artificial intelligence model to assist thyroid nodule diagnosis and management: A multicentre diagnostic study. Lancet Digit. Health 2021, 3, e250–e259. [Google Scholar] [CrossRef]
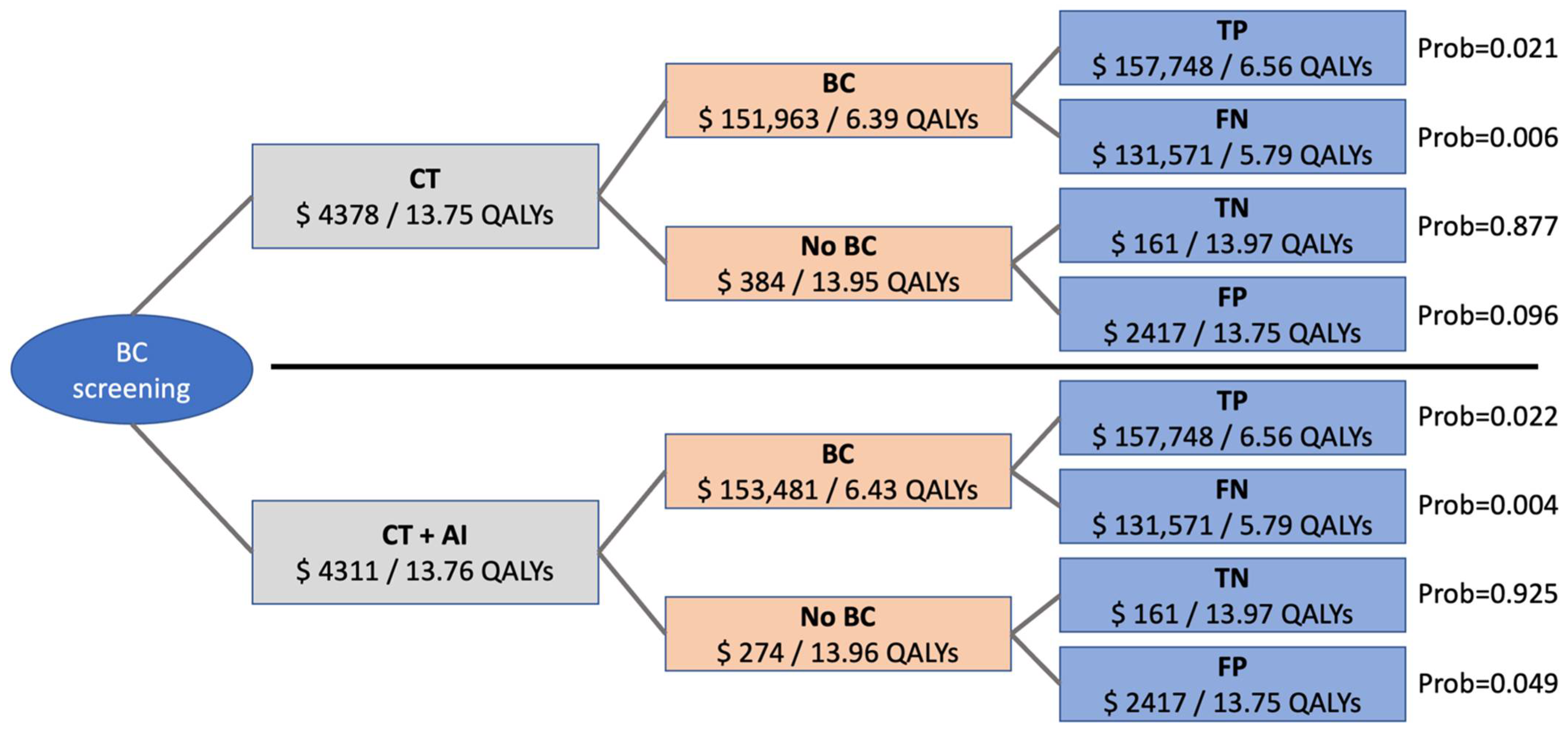


| Pre-test-Probability of BC | 2.635 | Jacob et al. [19] |
| Age at diagnostic procedure | 60 years | US Preventive Services Task Force [1] |
| Assumed WTP | USD 100,000,00 | Assumption |
| Discount rate | 3.00% | Assumption |
| Markov model time | 20 years | Assumption |
| Diagnostic Test Performances | ||
| Sensitivity for BC CT | 77.9% | Ardila et al. [15] |
| Specificity for BC CT | 87.7% | Ardila et al. [15] |
| Sensitivity for BC CT + AI | 97.7% | Ardila et al. [15] |
| Specificity for BC CT + AI | 98.4% | Ardila et al. [15] |
| Costs (Acute) | ||
| CT | USD 161.00 | Medicare (71,250) [20] |
| Costs (Long Term) | ||
| No BC | USD 0.00 | |
| Follow up if false positive | USD 2256.00 | ten Haaf et al. [21] |
| Curative therapy BC/resection cost | USD 36,305.00 | Cowper et al. [22] |
| BC undetected | USD 0 | Assumption |
| BC after resection | USD 4283.00 | ten Haaf et al. [21] |
| Therapy BC, palliative | USD 60,000.00 | ten Haaf et al. [21] |
| Dead | USD 0 | Assumption |
| Utilities | ||
| No BC | 1 | Assumption |
| Follow up if false positive | 0.98 | Gareen et al. [23] |
| Curative therapy BC/resection | 0.79 | Grutters et al. [24] |
| BC undetected | 1 | Assumption |
| BC after resection | 0.933 | Möller et al. [25] |
| BC palliative | 0.63 | Doyle et al. [26] |
| Dead | 0 | Assumption |
| Transition Probabilities | ||
| Verification of suspicious nodule as no BC | 100% | Assumption |
| Death if no BC but suspicious nodule | 0.001 (invasive diagnostics) + life tables | The National Lung Screening Trial Research Team [2] |
| Resection rate of BC after early detection | 75% | The National Lung Screening Trial Research Team [2] |
| Death after curative resection | 4.70% | Green et al./Toker et al. [27,28] |
| Recurrence after resection | 9.80% | Lou et al. [29] |
| Detection of initially undetected BC | 15% 1st, 40% 2nd, 100% 3rd year | Scholten et al. [30] |
| Death with undetected BC | life tables | |
| Resection rate of BC after delayed detection | 26% | Hunbogi et al. [31] |
| Death with palliative care | 36% | Cancer Stat Facts: Lung and Bronchus Cancer, National Cancer Institute [32] |
| Death without BC | life tables | |
| WTP (USD/QALY) | 0 | 20,000 | 40,000 | 60,000 | 80,000 | 100,000 | 120,000 | 150,000 | 200,000 |
| Cost of AI (USD) | 68 | 302 | 537 | 771 | 1006 | 1240 | 1475 | 1826 | 2412 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziegelmayer, S.; Graf, M.; Makowski, M.; Gawlitza, J.; Gassert, F. Cost-Effectiveness of Artificial Intelligence Support in Computed Tomography-Based Lung Cancer Screening. Cancers 2022, 14, 1729. https://doi.org/10.3390/cancers14071729
Ziegelmayer S, Graf M, Makowski M, Gawlitza J, Gassert F. Cost-Effectiveness of Artificial Intelligence Support in Computed Tomography-Based Lung Cancer Screening. Cancers. 2022; 14(7):1729. https://doi.org/10.3390/cancers14071729
Chicago/Turabian StyleZiegelmayer, Sebastian, Markus Graf, Marcus Makowski, Joshua Gawlitza, and Felix Gassert. 2022. "Cost-Effectiveness of Artificial Intelligence Support in Computed Tomography-Based Lung Cancer Screening" Cancers 14, no. 7: 1729. https://doi.org/10.3390/cancers14071729
APA StyleZiegelmayer, S., Graf, M., Makowski, M., Gawlitza, J., & Gassert, F. (2022). Cost-Effectiveness of Artificial Intelligence Support in Computed Tomography-Based Lung Cancer Screening. Cancers, 14(7), 1729. https://doi.org/10.3390/cancers14071729






