Exploring Determinants of Interdisciplinary Collaboration within a Geriatric Oncology Setting: A Mixed-Method Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Procedure
2.3. Questionnaire
- Sociodemographic data: age, sex, profession, additional degree in geriatrics or oncology, workplace and years of professional experience.
- Relationship and perception of elderly cancer patients: this category of questions assessed physicians’ perceptions about the beginning of elderhood (e.g., “From what age do you consider a patient to be old?”), the number of elderly patients for each physician in the last month (“In the past month, how many elderly patients have you cared for?”), and the proportion of patients shared with the other specialty (“What is the proportion of your elderly patients currently under the care of a geriatrician?” or “What is the proportion of your elderly patients currently under the care of an oncologist?”).
- Medical decision criteria and treatment preference (e.g., “How do you make your medical decisions?”(in multidisciplinary meeting, after consulting other specialists, alone or other); “What are the factors that you take into consideration in your decision-making process for treatment choices?”(medical history, characteristics of the tumor, patient’s desire, age, psychosocial factors or impossibility of using treatment due to patient fragility); “What type of treatment do you usually prefer in the care of elderly cancer patients?” (surgery, hormone therapy, radiotherapy, chemotherapy or other).
- Presence and participation in interdisciplinary meetings (IDMs): two questions assessed the frequency of scheduled IDMs (e.g., “In your department, how often are interdisciplinary meetings with all doctors involved in the care of elderly patients and other professionals providing support for these patients held?” (weekly, bimonthly, monthly, less than once a month, there are no multidisciplinary meetings, do not know or no answer) and the frequency of participation for each physician (“How often do you participate?” (systematically, frequently (2 times out of 3), rarely (1 time out of 3), never, do not know or no answer).
- Physicians’ perceptions of older cancer patients’ needs (e.g., “What do you think are the specific needs of elderly patients treated for cancer?”);
- Use of GA tools (“Do you use geriatric assessment in your practice?”, “What kind of GA do you use?”);
- The perception of the interdisciplinary collaboration between oncology physicians and geriatricians (“What does working in collaboration with doctors working in oncology (oncologists, surgeons, anaesthetists and radiotherapists) bring to you?”, “What does working in collaboration with the geriatrician bring to you?”);
- The main obstacles of the collaboration between oncologists and geriatricians (e.g., “What, according to you, are the main obstacles to a full collaboration between oncologists and geriatricians or between your service and oncogeriatric care services?”).
2.4. Data Analysis
3. Results
3.1. Sample Characteristics
3.1.1. Geriatric Service
3.1.2. Oncology Service
3.2. Physicians’ Care of Elderly Cancer Patients
3.2.1. Oncogeriatric Care
3.2.2. Perceptions of Elderly Age
3.2.3. Medical Decision Criteria and Treatment Preference
3.2.4. Perceptions of the Specific Needs of Elderly Cancer Patients
3.3. Oncogeriatric Medical Practice and Interdisciplinarity
3.3.1. Use of Geriatric Screening Tools in the Oncology Setting
3.3.2. Interdisciplinary Meetings (IDMs)
3.3.3. Perceptions on Oncogeriatric Medical Practice
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yancik, R. Cancer in older persons: An international issue in an aging world. Semin. Oncol. 2004, 31, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Hurria, A.; Browner, I.S.; Cohen, H.J.; Denlinger, C.S.; DeShazo, M.; Extermann, M.; Ganti, A.K.P.; Holland, J.C.; Holmes, H.M.; Karlekar, M.B. Senior adult oncology. J. Natl. Compr. Cancer Netw. 2012, 10, 162–209. [Google Scholar] [CrossRef] [PubMed]
- Surbone, A.; Kagawa-Singer, M.; Terret, C.; Baider, L. The illness trajectory of elderly cancer patients across cultures: SIOG position paper. Ann. Oncol. 2007, 18, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Turner, N.J.; Haward, R.A.; Mulley, G.P.; Selby, P.J. Cancer in old age—Is it inadequately investigated and treated? BMJ 1999, 319, 309–312. [Google Scholar] [CrossRef] [PubMed]
- Bouchardy, C.; Rapiti, E.; Fioretta, G.; Laissue, P.; Neyroud-Caspar, I.; Schäfer, P.; Kurtz, J.; Sappino, A.-P.; Vlastos, G. Undertreatment Strongly Decreases Prognosis of Breast Cancer in Elderly Women. JCO 2003, 21, 3580–3587. [Google Scholar] [CrossRef] [PubMed]
- Talarico, L.; Chen, G.; Pazdur, R. Enrollment of Elderly Patients in Clinical Trials for Cancer Drug Registration: A 7-Year Experience by the US Food and Drug Administration. JCO 2004, 22, 4626–4631. [Google Scholar] [CrossRef]
- Terret, C.; Zulian, G.; Droz, J.-P. Statements on the interdependence between the oncologist and the geriatrician in geriatric oncology. Crit. Rev. Oncol./Hematol. 2004, 52, 127–133. [Google Scholar] [CrossRef]
- Birch, R.J.; Taylor, J.C.; Downing, A.; Spencer, K.; Finan, P.J.; Audisio, R.A.; Carrigan, C.M.; Selby, P.J.; Morris, E.J.A. Rectal cancer in old age—Is it appropriately managed? Evidence from population-based analysis of routine data across the English national health service. Eur. J. Surg. Oncol. 2019, 45, 1196–1204. [Google Scholar] [CrossRef]
- Giri, S.; Al-Obaidi, M.; Weaver, A.; Kenzik, K.M.; McDonald, A.; Clark, D.; Young-Smith, C.; Paluri, R.; Nandagopal, L.; Gbolahan, O.; et al. Association Between Chronologic Age and Geriatric Assessment–Identified Impairments: Findings From the CARE Registry. J. Natl. Compr. Cancer Netw. 2021, 19, 922–927. [Google Scholar] [CrossRef]
- Montroni, I.; Ugolini, G.; Saur, N.M.; Spinelli, A.; Rostoft, S.; Millan, M.; Wolthuis, A.; Daniels, I.R.; Hompes, R.; Penna, M.; et al. Personalized management of elderly patients with rectal cancer: Expert recommendations of the European Society of Surgical Oncology, European Society of Coloproctology, International Society of Geriatric Oncology, and American College of Surgeons Commission on Cancer. Eur. J. Surg. Oncol. 2018, 44, 1685–1702. [Google Scholar] [CrossRef]
- Balducci, L. Geriatric oncology: Challenges for the new century. Eur. J. Cancer 2000, 36, 1741–1754. [Google Scholar] [CrossRef]
- Balducci, L.; Extermann, M. Management of cancer in the older person: A practical approach. Oncology 2000, 5, 224–237. [Google Scholar] [CrossRef] [PubMed]
- Balducci, L. New paradigms for treating elderly patients with cancer: The comprehensive geriatric assessment and guidelines for supportive care. J. Support. Oncol. 2003, 1, 30–37. [Google Scholar]
- Schiphorst, A.H.W.; Ten Bokkel Huinink, D.; Breumelhof, R.; Burgmans, J.P.J.; Pronk, A.; Hamaker, M.E. Geriatric consultation can aid in complex treatment decisions for elderly cancer patients. Eur J. Cancer Care 2016, 25, 365–370. [Google Scholar] [CrossRef] [PubMed]
- de Vries, M.; van Weert, J.C.; Jansen, J.; Lemmens, V.E.; Maas, H.A. Step by step development of clinical care pathways for older cancer patients: Necessary or desirable? Eur. J. Cancer 2007, 43, 2170–2178. [Google Scholar] [CrossRef][Green Version]
- Wildiers, H.; Heeren, P.; Puts, M.; Topinkova, E.; Janssen-Heijnen, M.L.G.; Extermann, M.; Falandry, C.; Artz, A.; Brain, E.; Colloca, G.; et al. International Society of Geriatric Oncology Consensus on Geriatric Assessment in Older Patients with Cancer. JCO 2014, 32, 2595–2603. [Google Scholar] [CrossRef]
- Mohile, S.G.; Dale, W.; Somerfield, M.R.; Schonberg, M.A.; Boyd, C.M.; Burhenn, P.S.; Canin, B.; Cohen, H.J.; Holmes, H.M.; Hopkins, J.O.; et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy: ASCO Guideline for Geriatric Oncology. J. Clin. Oncol. 2018, 36, 2326–2347. [Google Scholar] [CrossRef]
- Magnuson, A.; Lemelman, T.; Pandya, C.; Goodman, M.; Noel, M.; Tejani, M.; Doughtery, D.; Dale, W.; Hurria, A.; Janelsins, M.; et al. Geriatric assessment with management intervention in older adults with cancer: A randomized pilot study. Support. Care Cancer 2018, 26, 605–613. [Google Scholar] [CrossRef]
- Caillet, P.; Canoui-Poitrine, F.; Vouriot, J.; Berle, M.; Reinald, N.; Krypciak, S.; Bastuji-Garin, S.; Culine, S.; Paillaud, E. Comprehensive Geriatric Assessment in the Decision-Making Process in Elderly Patients with. Cancer: ELCAPA Study. JCO 2011, 29, 3636–3642. [Google Scholar] [CrossRef]
- Hamaker, M.E.; te Molder, M.; Thielen, N.; van Munster, B.C.; Schiphorst, A.H.; van Huis, L.H. The effect of a geriatric evaluation on treatment decisions and outcome for older cancer patients—A systematic review. J. Geriatr. Oncol. 2018, 9, 430–440. [Google Scholar] [CrossRef]
- Hurria, A.; Togawa, K.; Mohile, S.G.; Owusu, C.; Klepin, H.D.; Gross, C.P.; Lichtman, S.M.; Gajra, A.; Bhatia, S.; Katheria, V.; et al. Predicting Chemotherapy Toxicity in Older Adults With Cancer: A Prospective Multicenter Study. J. Clin. Oncol. 2011, 29, 3457–3465. [Google Scholar] [CrossRef] [PubMed]
- Mohile, S.G.; Epstein, R.M.; Hurria, A.; Heckler, C.E.; Canin, B.; Culakova, E.; Duberstein, P.; Gilmore, N.; Xu, H.; Plumb, S.; et al. Communication With Older Patients With Cancer Using Geriatric Assessment: A Cluster-Randomized Clinical Trial From the National Cancer Institute Community Oncology Research Program. JAMA Oncol. 2020, 6, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Bellera, C.A.; Rainfray, M.; Mathoulin-Pélissier, S.; Mertens, C.; Delva, F.; Fonck, M.; Soubeyran, P.L. Screening older cancer patients: First evaluation of the G-8 geriatric screening tool. Ann. Oncol. 2012, 23, 2166–2172. [Google Scholar] [CrossRef] [PubMed]
- Soubeyran, P.; Bellera, C.; Goyard, J.; Heitz, D.; Curé, H.; Rousselot, H.; Albrand, G.; Servent, V.; Jean, O.S.; van Praagh, I. Screening for vulnerability in older cancer patients: The ONCODAGE Prospective Multicenter Cohort Study. PLoS ONE 2014, 9, e115060. [Google Scholar] [CrossRef] [PubMed]
- van Walree, I.C.; Scheepers, E.; van Huis-Tanja, L.; Emmelot-Vonk, M.H.; Bellera, C.; Soubeyran, P.; Hamaker, M.E. A systematic review on the association of the G8 with geriatric assessment, prognosis and course of treatment in older patients with cancer. J. Geriatr. Oncol. 2019, 10, 847–858. [Google Scholar] [CrossRef]
- Decoster, L.; Kenis, C.; Van Puyvelde, K.; Flamaing, J.; Conings, G.; De Grève, J.; Mets, T.; Milisen, K.; Lobelle, J.P.; Wildiers, H. The influence of clinical assessment (including age) and geriatric assessment on treatment decisions in older patients with cancer. J. Geriatr. Oncol. 2013, 4, 235–241. [Google Scholar] [CrossRef]
- Hamaker, M.E.; Jonker, J.M.; de Rooij, S.E.; Vos, A.G.; Smorenburg, C.H.; van Munster, B.C. Frailty screening methods for predicting outcome of a comprehensive geriatric assessment in elderly patients with cancer: A systematic review. Lancet Oncol. 2012, 13, e437–e444. [Google Scholar] [CrossRef]
- Decoster, L.; Van Puyvelde, K.; Mohile, S.; Wedding, U.; Basso, U.; Colloca, G.; Rostoft, S.; Overcash, J.; Wildiers, H.; Steer, C.; et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: An update on SIOG recommendations. Ann. Oncol. 2015, 26, 288–300. [Google Scholar] [CrossRef]
- Puts, M.T.E.; Hardt, J.; Monette, J.; Girre, V.; Springall, E.; Alibhai, S.M.H. Use of Geriatric Assessment for Older Adults in the Oncology Setting: A Systematic Review. J. Natl. Cancer Inst. 2012, 104, 1134–1164. [Google Scholar] [CrossRef]
- Tremblay, D.; Charlebois, K.; Terret, C.; Joannette, S.; Latreille, J. Integrated oncogeriatric approach: A systematic review of the literature using concept analysis. BMJ Open 2012, 2, e001483. [Google Scholar] [CrossRef]
- Puts, M.T.E.; Girre, V.; Monette, J.; Wolfson, C.; Monette, M.; Batist, G.; Bergman, H. Clinical experience of cancer specialists and geriatricians involved in cancer care of older patients: A qualitative study. Crit. Rev. Oncol. Hematol. 2010, 74, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Sifer-Rivière, L.; Girre, V.; Gisselbrecht, M.; Saint-Jean, O. Physicians’ perceptions of cancer care for elderly patients: A qualitative sociological study based on a pilot geriatric oncology program. Crit. Rev. Oncol. Hematol. 2010, 75, 58–69. [Google Scholar] [CrossRef] [PubMed]
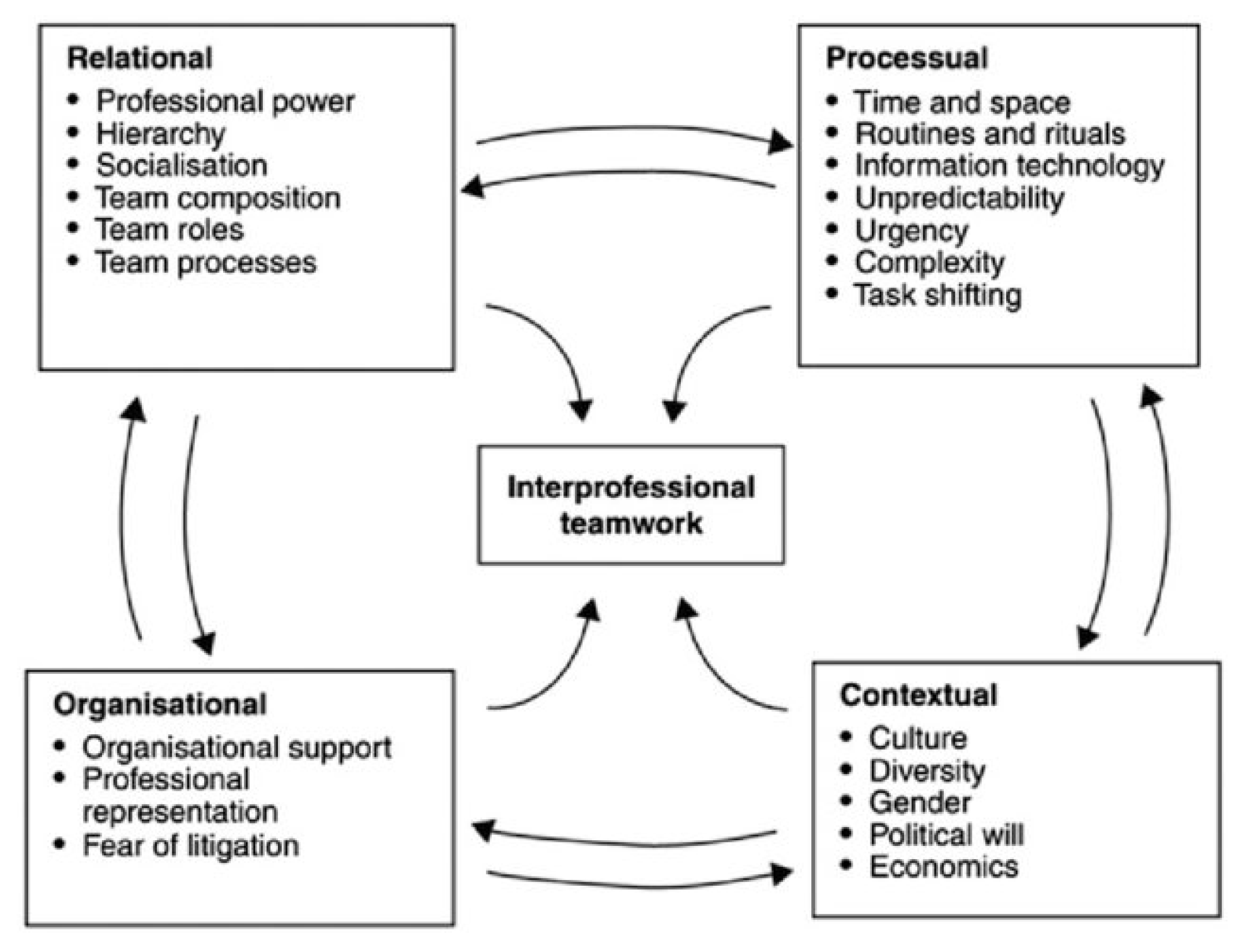
- Reeves, S.; Lewin, S.; Espin, S.; Zwarenstein, M. Interprofessional Teamwork for Health and Social Care; John Wiley & Sons: Hoboken, NJ, USA, 2011; Volume 8. [Google Scholar]
- Magnuson, A.; Dale, W.; Mohile, S. Models of Care in Geriatric Oncology. Curr. Geriatr. Rep. 2014, 3, 182. [Google Scholar] [CrossRef]
- Creamer, E.G.; Reeping, D. Advancing mixed methods in psychological research. Methods Psychol. 2020, 3, 100035. [Google Scholar] [CrossRef]
- Ritchie, J.; Spencer, L. Qualitative data analysis for applied policy research. In Analyzing Qualitative Data; Routledge: London, UK, 1994; ISBN 978-0-203-41308-1. [Google Scholar]
- Fusch, P.; Fusch, G.E.; Ness, L.R. Denzin’s paradigm shift: Revisiting triangulation in qualitative research. J. Soc. Chang. 2018, 10, 2. [Google Scholar] [CrossRef]
- Creswell, J.W.; Clark, V.L.P. Designing and Conducting Mixed Methods Research; Sage Publications: New York, NY, USA, 2017. [Google Scholar]
- Haverkamp, B.E.; Morrow, S.L.; Ponterotto, J.G. A time and place for qualitative and mixed methods in counseling psychology research. J. Couns. Psychol. 2005, 52, 123–125. [Google Scholar] [CrossRef]
- Extermann, M.; Aapro, M.; Bernabei, R.; Cohen, H.J.; Droz, J.-P.; Lichtman, S.; Mor, V.; Monfardini, S.; Repetto, L.; Sørbye, L. Use of comprehensive geriatric assessment in older cancer patients: Recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit. Rev. Oncol. Hematol. 2005, 55, 241–252. [Google Scholar] [CrossRef]
- Extermann, M. Integrating a geriatric evaluation in the clinical setting. Semin. Radiat. Oncol. 2012, 22, 272–276. [Google Scholar] [CrossRef]
- Protière, C.; Viens, P.; Rousseau, F.; Moatti, J.P. Prescribers’ attitudes toward elderly breast cancer patients. Discrimination or empathy? Crit. Rev. Oncol. Hematol. 2010, 75, 138–150. [Google Scholar] [CrossRef]
- Hurria, A.; Naeim, A.; Elkin, E.; Limaye, S.; Grover, A.; Hudis, C.; Pearce, C.; Robson, M. Adjuvant treatment recommendations in older women with breast cancer—A survey of oncologists. Crit. Rev. Oncol. Hematol. 2007, 61, 255–260. [Google Scholar] [CrossRef]
- Pryor, J. A nursing perspective on the relationship between nursing and allied health in inpatient rehabilitation. Disabil. Rehabil. 2008, 30, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Sifer-Riviere, L.; Saint-Jean, O.; Gisselbrecht, M.; Cudennec, T.; Girre, V. What the specific tools of geriatrics and oncology can tell us about the role and status of geriatricians in a pilot geriatric oncology program. Ann. Oncol. 2011, 22, 2325–2329. [Google Scholar] [CrossRef] [PubMed]
- Hall, P. Interprofessional teamwork: Professional cultures as barriers. J. Interprof. Care 2005, 19, 188–196. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Geriatricians (n = 7) | Oncology Physicians (n = 15) | Total (n = 22) |
|---|---|---|---|
| Age | 45.5 {9.6} | 43.7 {8.2} | 43.8 {8.2} |
| Sex | |||
| Female | (57%) | (53%) | - |
| Number of professionals with an additional degree: | |||
| -in oncology | 4 | - | 4 |
| -in geriatrics | - | 5 | 5 |
| Years practicing: | |||
| -oncology | - | 16.3 {8.9} | |
| -geriatrics | 11.7 {4.3} | - | 14.7 {7.9} |
| Care of Elderly Cancer Patients | Geriatricians (n = 7) | Oncology Physicians (n = 15) | Total (n = 22) |
|---|---|---|---|
| Elderly patients in active file | 75{20.4} | 31{19.5} | |
| Patients receiving: | |||
| -oncology care | 67% | - | |
| -geriatric care | - | 38% | |
| Perception of the beginning of elderly age | 75.2 (70–85) {6.1} | 72 (60–80) {4.5} | 73.5 (60–85) {5.1} |
| Processual Determinants | Geriatricians (n = 7) | Oncology Physicians (n = 15) |
|---|---|---|
| IDMs | ||
| -weekly | - | - |
| -less than once a month | 3 (50%) | 9 (60%) |
| -bimonthly | 1 (17%) | 1 (7%) |
| -no interdisciplinary meetings | 2 (33%) | 5 (33%) |
| -no answer | 1 (17%) | - |
| GA | 7 | 5 |
| -G8 | 2 | 3 |
| -other types of GA | 5 | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrault-Couchouron, M.; Micheli, N.; Soubeyran, P. Exploring Determinants of Interdisciplinary Collaboration within a Geriatric Oncology Setting: A Mixed-Method Study. Cancers 2022, 14, 1386. https://doi.org/10.3390/cancers14061386
Barrault-Couchouron M, Micheli N, Soubeyran P. Exploring Determinants of Interdisciplinary Collaboration within a Geriatric Oncology Setting: A Mixed-Method Study. Cancers. 2022; 14(6):1386. https://doi.org/10.3390/cancers14061386
Chicago/Turabian StyleBarrault-Couchouron, Marion, Noemi Micheli, and Pierre Soubeyran. 2022. "Exploring Determinants of Interdisciplinary Collaboration within a Geriatric Oncology Setting: A Mixed-Method Study" Cancers 14, no. 6: 1386. https://doi.org/10.3390/cancers14061386
APA StyleBarrault-Couchouron, M., Micheli, N., & Soubeyran, P. (2022). Exploring Determinants of Interdisciplinary Collaboration within a Geriatric Oncology Setting: A Mixed-Method Study. Cancers, 14(6), 1386. https://doi.org/10.3390/cancers14061386







