Activation of Investigator-Initiated Clinical Trials with a Pharmaceutical for Cancer Patients before and after Post-Millennial Changes of Regulations in Germany and Europe
Abstract
:Simple Summary
Abstract
1. Trial Activation and Conduct before 2004
2. Changes in the Legislation around 2000
- In Germany, university hospitals (UH) had to adopt a new legal status. Before 1998, UH were non-independent operations of the German Federal States. In particular, they had no legal independence and relied on small administrations, which simultaneously operated for the corresponding medical faculties of the universities. With the new legal status, most university hospitals became corporations under public law [8] which induced a dualism between the medical faculty and university hospital with areas of conflict and legal independence of the university hospital, resulting in considerable workforce expansion in the legal divisions and changes in responsibilities. Physician–scientists were no longer able to activate an IIT in their own responsibility but depended on complicated decision pathways by the legal department of the hospital with time and cost consequences, as outlined below.
- In 2003, the legal basis of hospital financing was switched to a German adaption of the Australian Disease-Related Group (G-DRG) system. The aim of G-DRG was to limit the “cost explosion” in the health system. It is not the topic of this opinion paper to judge whether such a “cost explosion” ever existed or whether this objective was reached. However, today roughly two-thirds of German UH are in deep financial deficit and the annual deficit accumulated to EUR >500 million in 2020 [9]. At the same time, the dual system of financing for the UH, with insurance reimbursement for standard of care and with state grants for research and teaching activities, are by no means sufficient to cover the dramatic cost increases for clinical IITs, and an adequate build-up of public grants or grants by charity organizations for the conduct of clinical trials, in particular IITs, is lacking behind. Thus, today many IITs are financed or co-financed by the pharmaceutical industry, which changes the meaning of the term IIT.
- Good Clinical Practice (GCP) Guidelines were issued by the European Union as Clinical Trials Directive 2001 (EU CTD 2001/20) throughout Europe, which was followed by national changes in Drug Laws (2004, in Germany 12. Novelle, AMG). Whereas the two structural and legal changes mentioned above are more or less Germany-specific, the GCP-guidelines have an impact in Europe and the US. This legal framework, implemented with the objective to be a quality standard for the design, conduct, performance, monitoring, auditing, recording, analysis and reporting of clinical trials, and hereby to improve trial quality and patient safety, has caused tremendous difficulties and delays in the activation and conduct of clinical trials. An important example of the new bureaucratic hurdles is the institution of a “sponsor”. A sponsor is responsible for initiation, management and/or financing of a clinical trial, and its institution has transferred the legal responsibility for a trial from the investigators and clinicians to a central legal institution (or individual). The EU CTD 2001/20 has resulted in a cost explosion in the performance of academic clinical trials designed to develop optimized standards of care, which have to comply with the same regulatory and administrative requirements as commercial drug development through clinical phases I to III.
3. Trial Activation after 2004
4. Emergence and Consequences of Change in UH Legal Status, G-DRG, and EU-CTD 2001/20 for the Activation of an IIT after 2004
5. Conclusions and Recommendations
Author Contributions
Funding
Conflicts of Interest
References
- Berdel, W.E. Membrane-Active Lipids as Experimental Anticancer Drugs. Br. J. Cancer 1991, 64, 208–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berdel, W.E.; Schlehe, H.; Fink, U.; Emmerich, B.; Maubach, P.A.; Emslander, H.P.; Daum, S.; Rastetter, J. Early Tumor and Leukemia Response to Alkyl-Lysophospholipids in a Phase I Study. Cancer 1982, 50, 2011–2015. [Google Scholar] [CrossRef] [Green Version]
- Hilgard, P.; Klenner, T.; Stekar, J.; Unger, C. Alkylphosphocholines: A New Class of Membrane-Active Anticancer Agents. Cancer Chemother. Pharmacol. 1993, 32, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Mitrou, P.S.; Fischer, M.; Weissenfels, I.; Diehl, V.; Gropp, C.; Liesenfeld, A.; Schmidt, M.; Berdel, W.E.; Fink, U.; Graubner, M. Treatment of Inoperable Non-Small-Cell Bronchogenic Carcinoma with Etoposide and Cis-Platinum. Cancer Treat. Rev. 1982, 9 (Suppl. A), 139–142. [Google Scholar] [CrossRef]
- Rossig, C.; Juergens, H.; Schrappe, M.; Moericke, A.; Henze, G.; von Stackelberg, A.; Reinhardt, D.; Burkhardt, B.; Woessmann, W.; Zimmermann, M.; et al. Effective Childhood Cancer Treatment: The Impact of Large Scale Clinical Trials in Germany and Austria. Pediatr. Blood Cancer 2013, 60, 1574–1581. [Google Scholar] [CrossRef]
- Kreuser, E.D.; Fiebig, H.H.; Scheulen, M.E.; Hanauske, A.; Keppler, B.K.; Mross, K.; Schalhorn, A.; Eisenbrand, G.; Edler, L.; Höffken, K.; et al. Standard Operating Procedures and Organization of German Phase I, II, and III Study Groups, New Development Group (AWO), and Study Group of Pharmacology in Oncology and Hematology (APOH) of the Association of Medical Oncology (AIO) of the German Cancer Society. Onkologie 1998, 21 (Suppl. 3), 1–70. [Google Scholar]
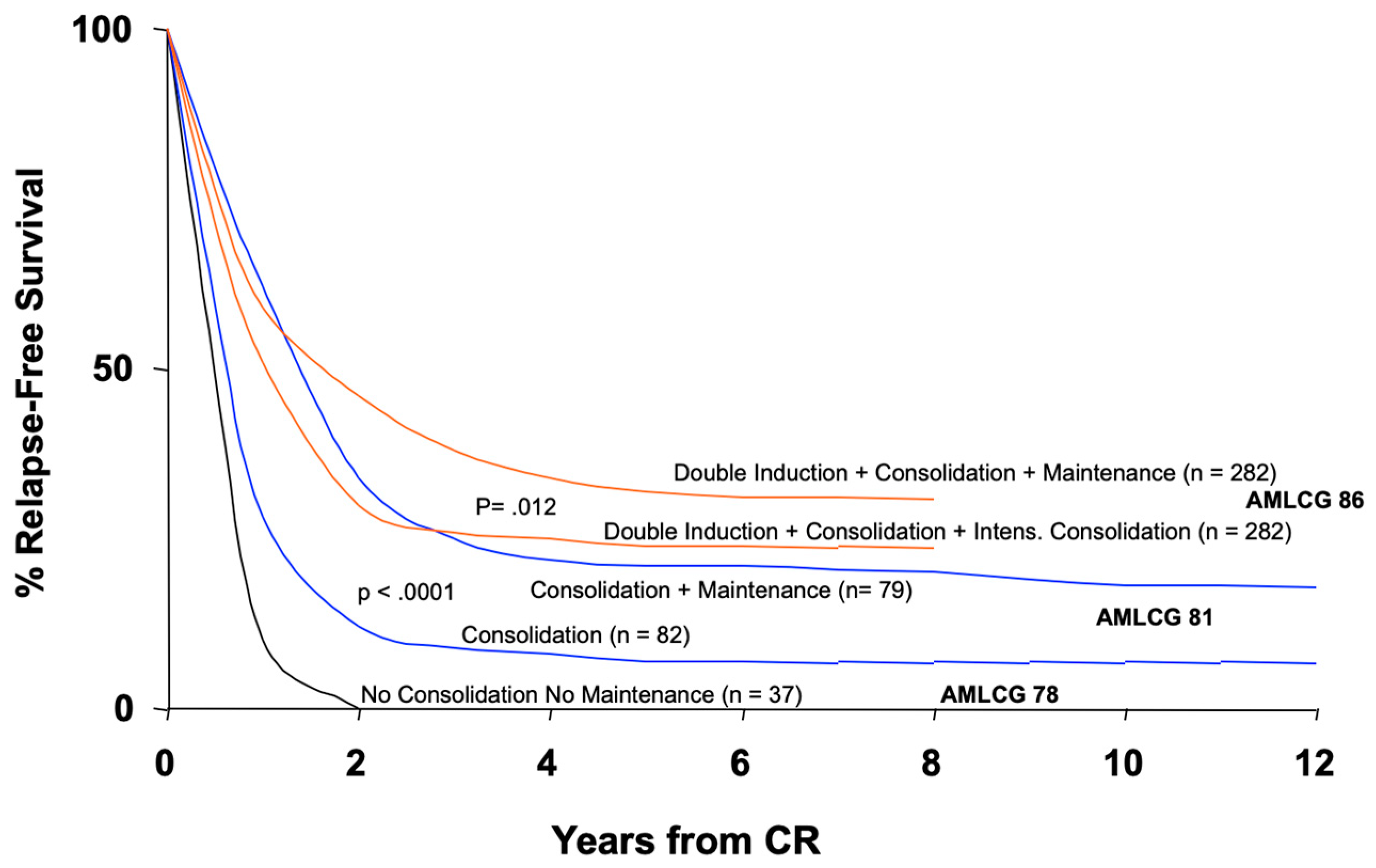
- Büchner, T.; Krug, U.; Berdel, W.E.; Heinecke, A.; Sauerland, M.C.; Wörmann, B.; Hiddemann, W. Maintenance for acute myeloid leukemia revisited. Curr. Treat. Options Oncol. 2007, 8, 296–304. [Google Scholar] [CrossRef]
- Wissenschaftlicher Dienst—Deutscher Bundestag. Begriff, Rechtsreformen und Finanzierung der Universitätskliniken in Deutschland; Deutscher Bundestag: Bonn, Germany, 2016; WD 9-3000-007/16. Available online: www.bundestag.de (accessed on 16 January 2022).
- Verband der Universitätsklinika Deutschlands (VUD). Uniklinika in Finanznot–Neuausrichtung der Krankenhausversorgung dringend notwendig. Pressemitteilung. 21 October 2021. Available online: www.uniklinika.de (accessed on 16 January 2022).
- Opinion of the European Economic and Social Committee on Cooperation and Transfer of Knowledge between Research Organisations, Industry and SMEs—An Important Prerequisite for Innovation (Own-Initiative Opinion) (2009/C 218/02). Available online: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ/C/2009/218/0008/0014/EN/PDF (accessed on 16 January 2022).
- Tallen, G.; Dworzak, M.; Gadner, H.; Masera, G.; Schrappe, M.; Biondi, A.; Vassal, G.; Pieters, R.; Jazbec, J.; Morland, B.; et al. Imperative of Continual Support by the European Community for Future Advances in Paediatric Oncology in Europe: Meeting Report of the EC-Funded Science-Communication Project DIRECT “Overcoming Cancer with Research”. memo-Mag. Eur. Med Oncol. 2009, 2, 234–245. [Google Scholar] [CrossRef]
- Hartmann, M. Impact Assessment of the European Clinical Trials Directive: A Longitudinal, Prospective, Observational Study Analyzing Patterns and Trends in Clinical Drug Trial Applications Submitted since 2001 to Regulatory Agencies in six EU Countries. Trials 2012, 13, 53. [Google Scholar] [CrossRef] [Green Version]
- Stewart, D.J.; Whitney, S.N.; Kurzrock, R. Equipoise Lost: Ethics, Costs, and the Regulation of Cancer Clinical Research. J. Clin. Oncol. 2010, 28, 2925–2935. [Google Scholar] [CrossRef] [Green Version]
- Kearns, P. The Need for Proportionate Regulation of Clinical Trials. Lancet Oncol. 2013, 14, 454–455. [Google Scholar] [CrossRef]
- Piccart-Gebhart, M.J. The 41st David A. Karnofsky Memorial Award Lecture: Academic Research Worldwide—Quo Vadis? J. Clin. Oncol. 2014, 32, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Steensma, D.P.; Kantarjian, H.M. Impact of Cancer Research Bureaucracy on Innovation, Costs, and Patient Care. J. Clin. Oncol. 2014, 32, 376–378. [Google Scholar] [CrossRef] [PubMed]
- Stewart, D.J.; Batist, G.; Kantarjian, H.M.; Bradford, J.P.; Schiller, J.H.; Kurzrock, R. The Urgent Need for Clinical Research Reform to Permit Faster, Less Expensive Access to New Therapies for Lethal Diseases. Clin. Cancer Res. 2015, 21, 4561–4568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berdel, W.E. Unintended Regulatory Caused Early Death—A Difficult Endpoint in Cancer Patient Care and Treatment. Cancers 2021, 13, 1457. [Google Scholar] [CrossRef] [PubMed]
- Sekeres, M. Contract Research Agonizations–advocating for a return to common sense in clinical research. Editorial. ASH Clinical News, 15 June 2017. [Google Scholar]
- Ehninger, G.; Overkamp, F.; Freund, M. (Eds.) Zur Situation Klinischer Studien in Deutschland; Karger: Berlin, Germany, 2013; Volume 36, pp. 1–44. [Google Scholar] [CrossRef]
- Deutsche Gesellschaft für Hämatologie und Medizinische Onkologie e.V. Available online: www.dgho.de (accessed on 16 January 2022).
- Rule, S.; LeGuill, S. Bureaucracy is Strangling Clinical Research. BMJ 2019, 364, 1097. [Google Scholar] [CrossRef]
- Grimes, D.A.; Hubacher, D.; Nanda, K.; Schulz, K.F.; Moher, D.; Altman, D.G. The Good Clinical Practice Guideline: A Bronze Standard for Clinical Research. Lancet 2005, 366, 172–174. [Google Scholar] [CrossRef]
- Reith, C.; Landray, M.; Deveraux, P.J.; Bosch, J.; Granger, C.B.; Baigent, C.; Califf, R.M.; Collins, R.; Yusuf, S. Randomized Clinical Trials-Removing Unnecessary Obstacles. N. Engl. J. Med. 2013, 369, 1061–1065. [Google Scholar] [CrossRef] [Green Version]
- Opinion of the European Economic and Social Committee on the ‘Proposal for a Regulation of the European Parliament and of the Council on Clinical Trials on Medicinal Products for Human Use, and Repealing Directive 2001/20/EC’. Official Journal of the European Union, Document COM (2021) 369 Final—2012/0192 (COD). Available online: https/www.eur-lex.europa.eu (accessed on 16 January 2022).
- Senior, K. European Commission Proposals Do Not Impress Researchers. Lancet Oncol. 2012, 13, 864. [Google Scholar] [CrossRef]
- Knaapen, M.; Ploem, M.C.; Kruijt, M.; Oudijk, M.A.; Van Der Graaf, R.; Bet, P.M.; Bakx, R.; Van Heurn, L.W.E.; Gorter, R.R.; Van Der Lee, J.H. Low-Risk Trials for Children and Pregnant Women Threatened by Unnecessary Strict Regulations. Does the Coming EU Clinical Trial Regulation Offer a Solution? Eur. J. Pediatr. 2020, 179, 1205–1211. [Google Scholar] [CrossRef]
- Klinische Prüfung–Genehmigungsverfahren. Available online: www.bfarm.de (accessed on 16 January 2022).
- Klinische Prüfung–Bearbeitungsstatistik. Available online: www.PEI.de (accessed on 16 January 2022).
- Klingebiel, T.; Jürgens, H.; Glauche, I.; Gnekow, A.; Kandels, D.; Woessmann, W.; Schneider, D.T.; Suttorp, M. Registries and Studies in the Society for Pediatric Oncology and Hematology (GPOH)–What Contribution Do They Make to Progress. Klin. Padiatr. 2020, 232, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Hemminki, A.; Kellokumpu-Lehtinen, P.-L. Harmful Impact of EU Clinical Trials Directive. BMJ 2006, 332, 501–502. [Google Scholar] [CrossRef] [PubMed]
- Klingmann, I. (coord.) Impact on Clinical Research of European Legislation. In HEALTH-F1-2007-201002, Project Final Report; European Forum for Good Clinical Practice: Brussels, Belgium, 2009; Available online: https/www.eortc.org/app/uploads/2020/01/FINAL_REPORT_ICREL (accessed on 16 January 2022).
- Karlberg, J.P.E.; Speers, M.A. Reviewing Clinical Trials: A Guide for the Ethics Committee. Available online: https://www.clinicaltrialmagnifier.org/wp-content/uploads/2015/10/ECGuide-English.pdf (accessed on 16 January 2022).
- McMahon, A.D.; Conway, D.I.; MacDonald, T.M.; McInnes, G.T. The Unintended Consequences of Clinical Trials Regulations. PLoS Med. 2009, 6, e1000131. [Google Scholar] [CrossRef] [Green Version]
- Vose, J.M.; Levit, L.A.; Hurley, P.; Lee, C.; Thompson, M.A.; Stewart, T.; Hofacker, J.; Bruinooge, S.S.; Hayes, D.F. Addressing Administrative and Regulatory Burden in Cancer Clinical Trials: Summary of a Stakeholder Survey and Workshop Hosted by the American Society of Clinical Oncology and the Association of American Cancer Institutes. J. Clin. Oncol. 2016, 34, 3796–3802. [Google Scholar] [CrossRef] [PubMed]
- Cagnazzo, C. The Thin Border between Individual and Collective Ethics: The Downside of GDPR. Lancet Oncol. 2021, 22, 1494–1496. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berdel, W.E. Activation of Investigator-Initiated Clinical Trials with a Pharmaceutical for Cancer Patients before and after Post-Millennial Changes of Regulations in Germany and Europe. Cancers 2022, 14, 1308. https://doi.org/10.3390/cancers14051308
Berdel WE. Activation of Investigator-Initiated Clinical Trials with a Pharmaceutical for Cancer Patients before and after Post-Millennial Changes of Regulations in Germany and Europe. Cancers. 2022; 14(5):1308. https://doi.org/10.3390/cancers14051308
Chicago/Turabian StyleBerdel, Wolfgang E. 2022. "Activation of Investigator-Initiated Clinical Trials with a Pharmaceutical for Cancer Patients before and after Post-Millennial Changes of Regulations in Germany and Europe" Cancers 14, no. 5: 1308. https://doi.org/10.3390/cancers14051308
APA StyleBerdel, W. E. (2022). Activation of Investigator-Initiated Clinical Trials with a Pharmaceutical for Cancer Patients before and after Post-Millennial Changes of Regulations in Germany and Europe. Cancers, 14(5), 1308. https://doi.org/10.3390/cancers14051308





