The Patient’s Point of View: COVID-19 and Neuroendocrine Tumor Disease
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
3. Results
3.1. Patient and Tumor Characteristics
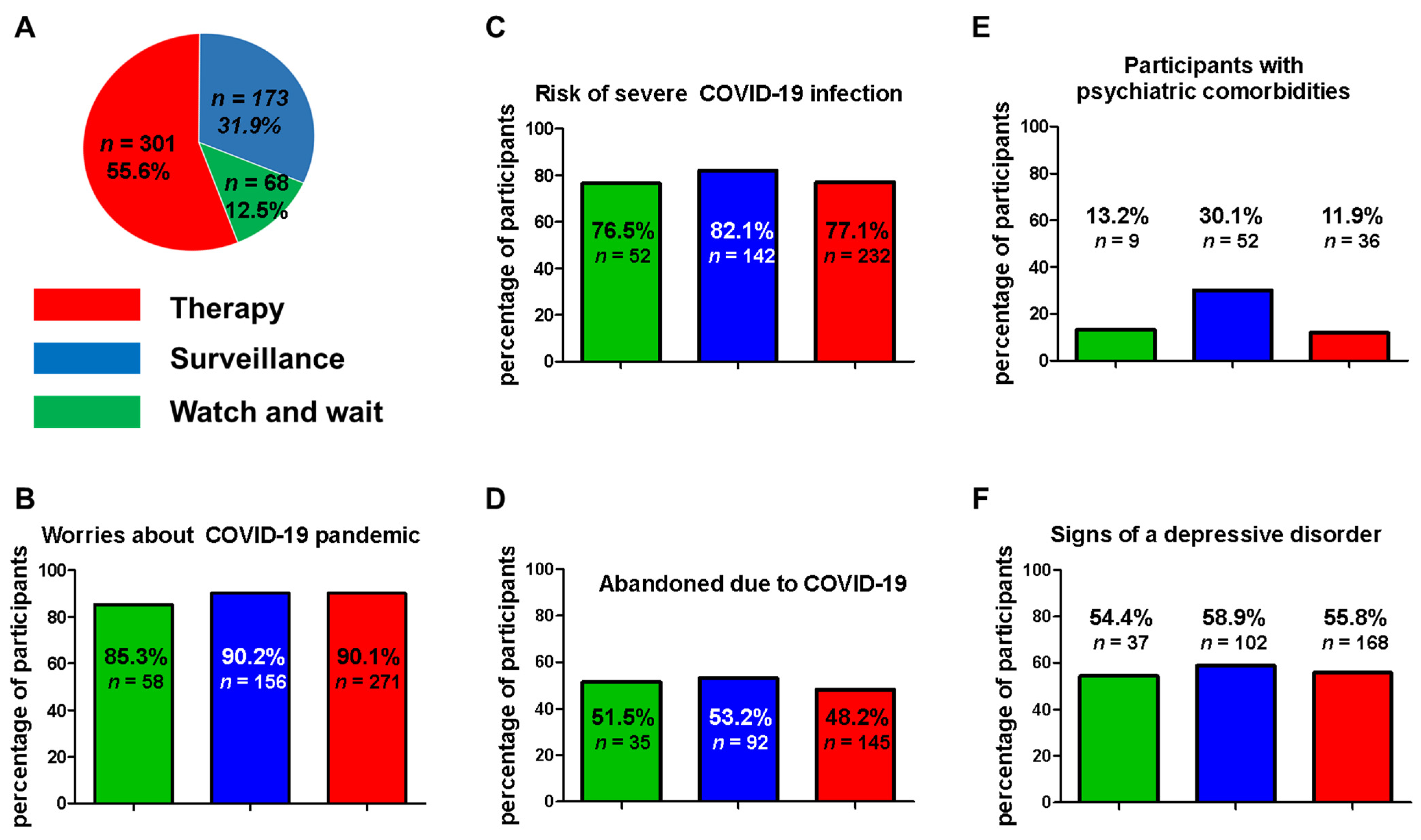
3.2. Treatment
3.3. Management of NET Patients during COVID-19
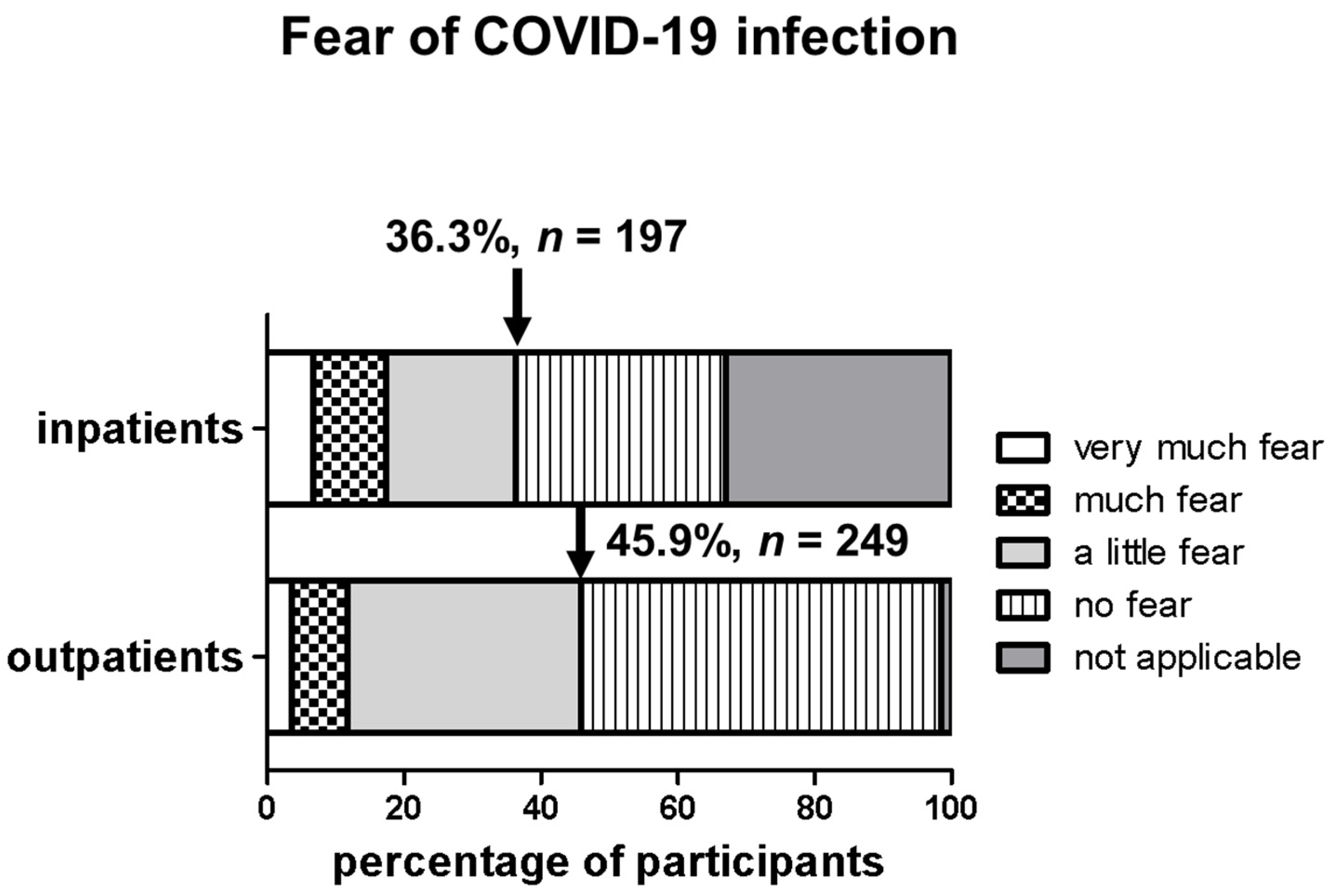
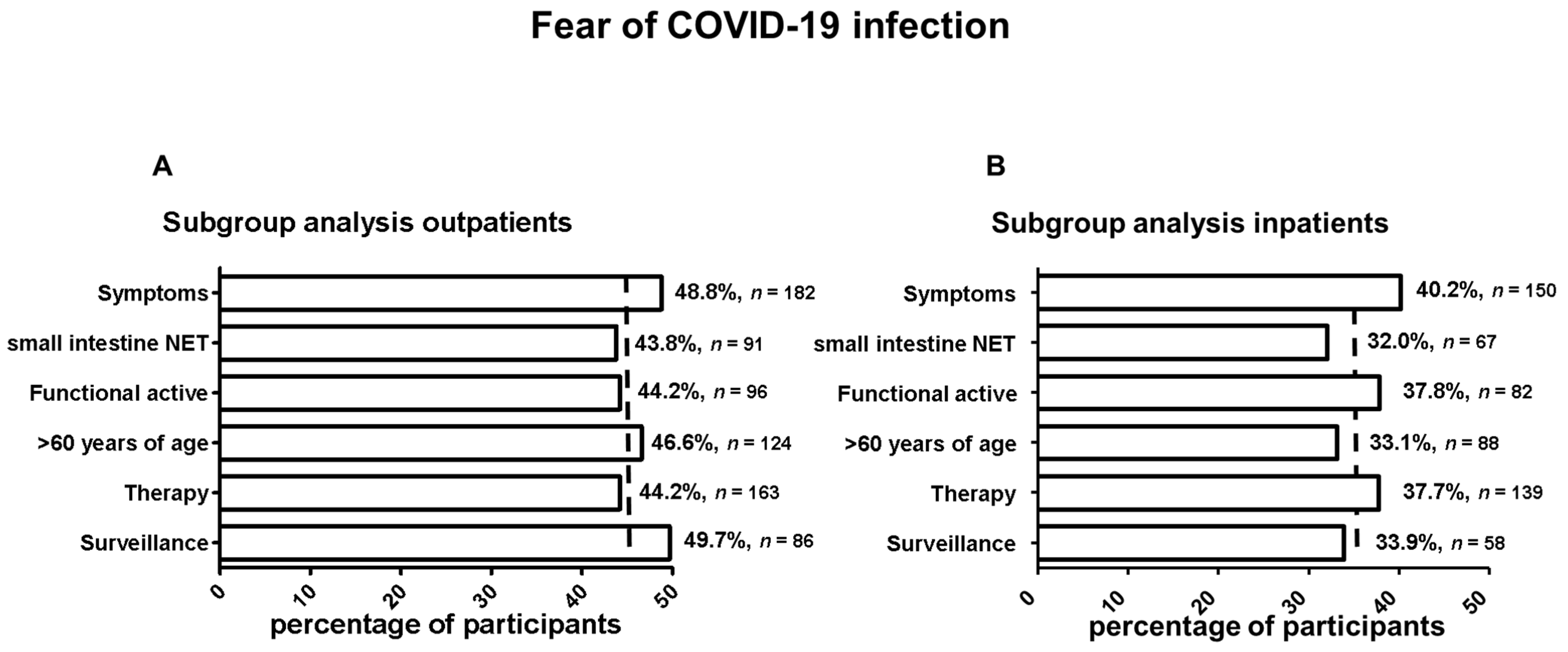
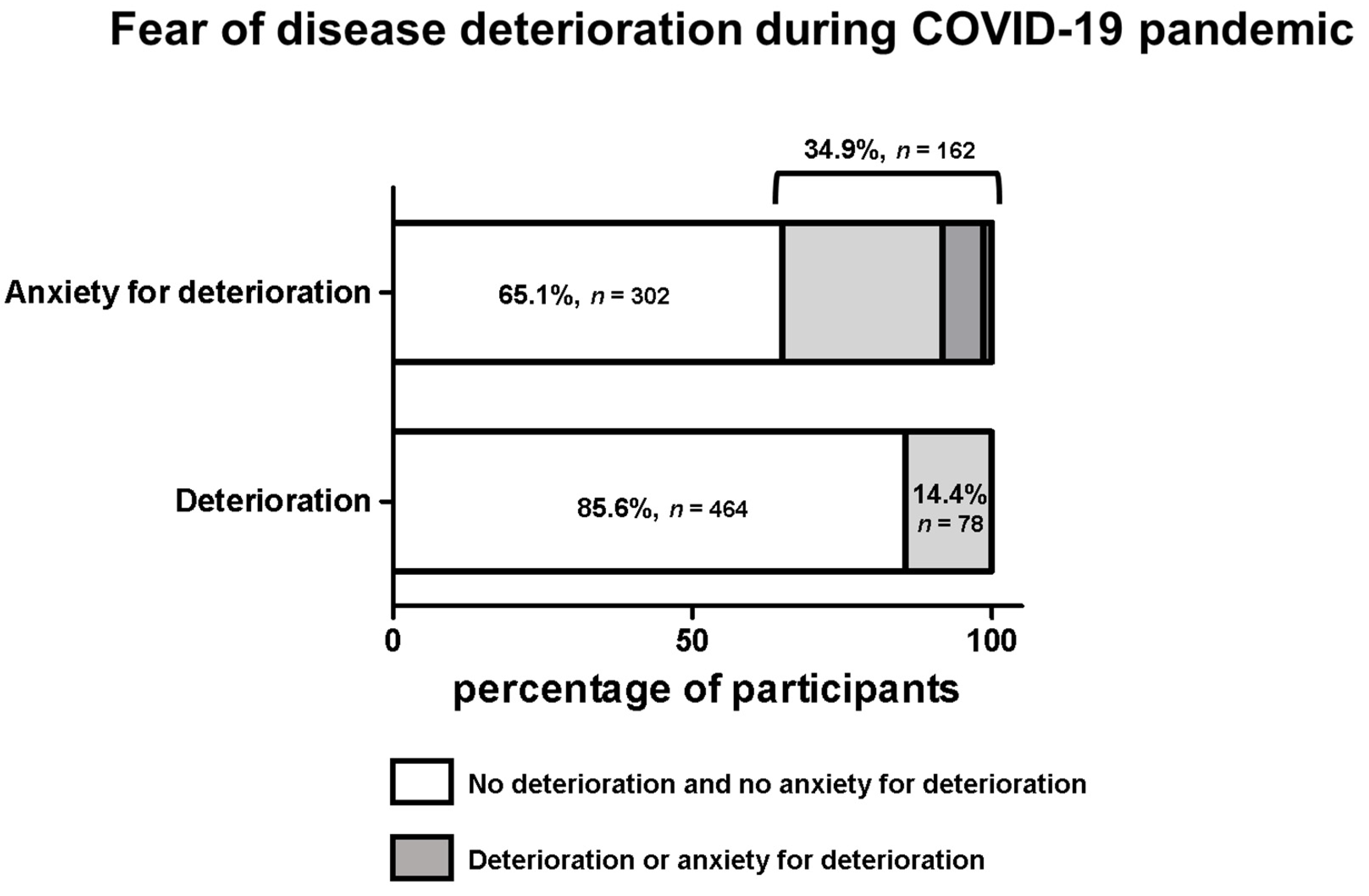
3.4. Anxieties and Concerns of Patients during COVID-19
3.5. Psychological Impact of the COVID-19 Pandemic for NET Patients
3.6. COVID-19 Positive Patients and Their Characteristics
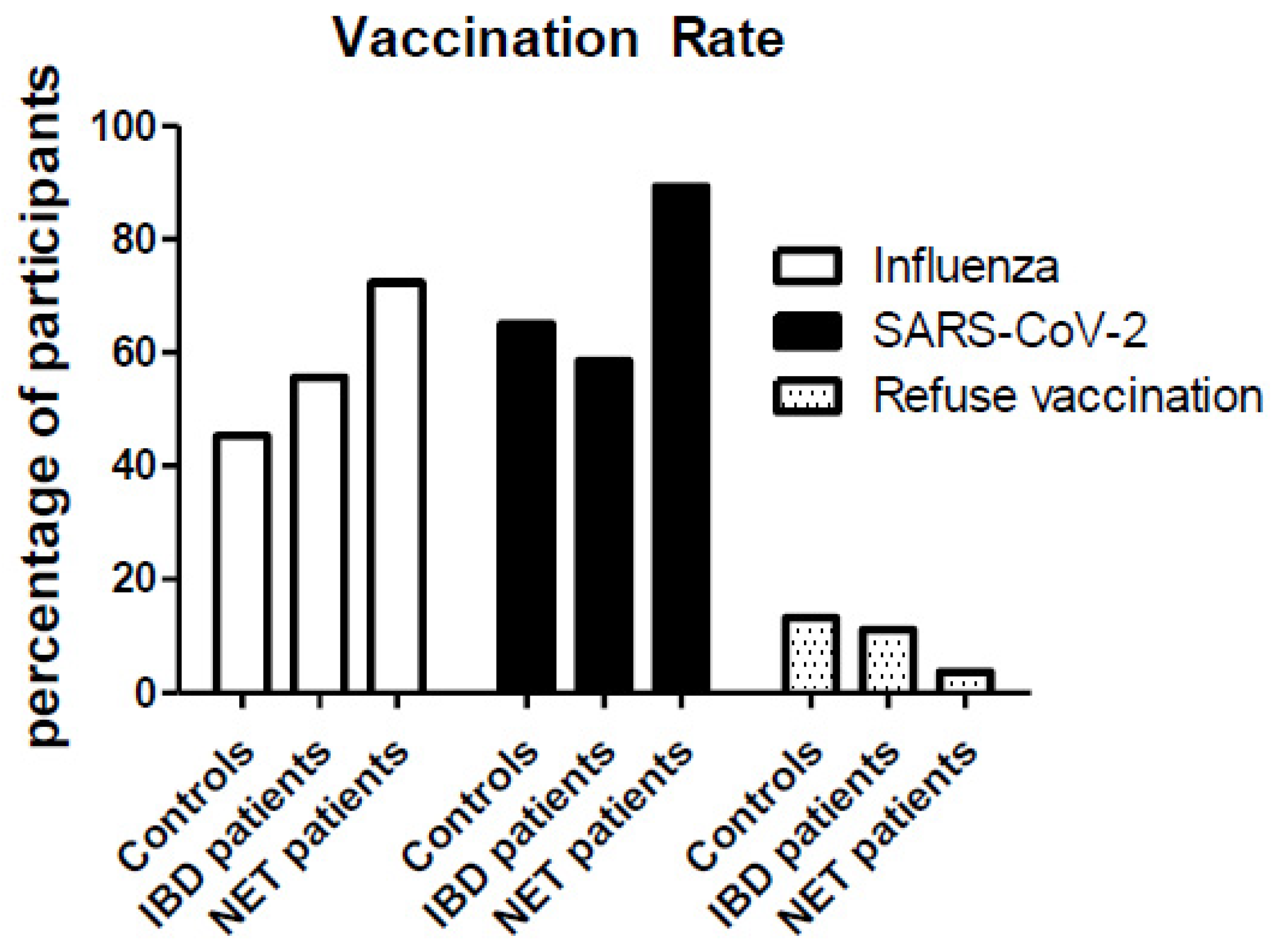
3.7. Opinions on Vaccination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Dasari, A.; Shen, C.; Halperin, D.M.; Zhao, B.; Zhou, S.; Xu, Y.; Shih, T.; Yao, J.C. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients with Neuroendocrine Tumors in the United States. JAMA Oncol. 2017, 3, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Brodziak, A.; Sigorski, D.; Osmola, M.; Wilk, M.; Gawlik-Urban, A.; Kiszka, J.; Machulska-Ciuraj, K.; Sobczuk, P. Attitudes of Patients with Cancer towards Vaccinations—Results of Online Survey with Special Focus on the Vaccination against COVID-19. Vaccines 2021, 9, 411. [Google Scholar] [CrossRef] [PubMed]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Bakouny, Z.; Hawley, J.E.; Choueiri, T.K.; Peters, S.; Rini, B.I.; Warner, J.L.; Painter, C.A. COVID-19 and Cancer: Current Challenges and Perspectives. Cancer Cell 2020, 38, 629–646. [Google Scholar] [CrossRef] [PubMed]
- RKI. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/nCoV.html (accessed on 30 November 2021).
- Rodriguez-Freixinos, V.; Capdevila, J.; Pavel, M.; Thawer, A.; Baudin, E.; O’Toole, D.; Herrmann, K.; Welin, S.; Grozinsky-Glasberg, S.; de Herder, W.W.; et al. Practical recommendations for the management of patients with gastroenteropancreatic and thoracic (carcinoid) neuroendocrine neoplasms in the COVID-19 era. Eur. J. Cancer 2021, 144, 200–214. [Google Scholar] [CrossRef]
- Panzuto, F.; Maccauro, M.; Campana, D.; Faggiano, A.; Massironi, S.; Pusceddu, S.; Spada, F.; Ferone, D.; Modica, R.; Grana, C.M.; et al. Impact of the SARS-CoV2 pandemic dissemination on the management of neuroendocrine neoplasia in Italy: A report from the Italian Association for Neuroendocrine Tumors (Itanet). J. Endocrinol. Investig. 2021, 44, 989–994. [Google Scholar] [CrossRef]
- Krug, S.; Garbe, J.; König, S.; Ungewiss, H.; Michl, P.; Rinke, A.; Schrader, J. Professional Assessment of the Impact of COVID-19 on Handling NET Patients. J. Clin. Med. 2020, 9, 3633. [Google Scholar] [CrossRef]
- Walldorf, J.; von Arnim, U.; Schmelz, R.; Riesner-Wehner, A.; Michl, P.; Grunert, P.C.; Stallmach, A.; Teich, N.; Reuken, P.A. SARS-CoV-2 Vaccination in Patients with Inflammatory Bowel Disease-Fear and Desire. Inflamm. Bowel Dis. 2021, 27, 1858–1861. [Google Scholar] [CrossRef]
- NET-Registers INaTiaD. Neuroendocrine Neoplasia within the German NET Registry. Z. Gastroenterol. 2018, 56, 1237–1246. [Google Scholar] [CrossRef]
- Niederle, M.B.; Hackl, M.; Kaserer, K.; Niederle, B. Gastroenteropancreatic neuroendocrine tumours: The current incidence and staging based on the WHO and European Neuroendocrine Tumour Society classification: An analysis based on prospectively collected parameters. Endocr.-Relat. Cancer 2010, 17, 909–918. [Google Scholar] [CrossRef]
- Halperin, D.M.; Shen, C.; Dasari, A.; Xu, Y.; Chu, Y.; Zhou, S.; Shih, Y.-C.T.; Yao, J.C. Frequency of carcinoid syndrome at neuroendocrine tumour diagnosis: A population-based study. Lancet Oncol. 2017, 18, 525–534. [Google Scholar] [CrossRef]
- Singh, S.; Granberg, D.; Wolin, E.; Warner, R.; Sissons, M.; Kolarova, T.; Goldstein, G.; Pavel, M.; Öberg, K.; Leyden, J. Patient-Reported Burden of a Neuroendocrine Tumor (NET) Diagnosis: Results from the First Global Survey of Patients with NETs. J. Glob. Oncol. 2017, 3, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Basuroy, R.; Bouvier, C.; Ramage, J.; Sissons, M.; Srirajaskanthan, R. Delays and routes to diagnosis of neuroendocrine tumours. BMC Cancer 2018, 18, 1122. [Google Scholar] [CrossRef] [PubMed]
- Curigliano, G.; Banerjee, S.; Cervantes, A.; Garassino, M.C.; Garrido, P.; Girard, N.; Haanen, J.; Jordan, K.; Lordick, F.; Machiels, J.P.; et al. Managing cancer patients during the COVID-19 pandemic: An ESMO multidisciplinary expert consensus. Ann. Oncol. 2020, 31, 1320–1335. [Google Scholar] [CrossRef]
- Aschele, C.; Negru, M.E.; Pastorino, A.; Cavanna, L.; Zagonel, V.; Barone-Adesi, F.; Blasi, L. Incidence of SARS-CoV-2 Infection Among Patients Undergoing Active Antitumor Treatment in Italy. JAMA Oncol. 2021, 7, 304–306. [Google Scholar] [CrossRef]
- Fazio, N.; Gervaso, L.; Halfdanarson, T.R.; La Salvia, A.; Hofland, J.; Hernando, J.; Sonbol, M.B.; Garcia-Carbonero, R.; Capdevila, J.; de Herder, W.W.; et al. Coronavirus disease 2019 in patients with neuroendocrine neoplasms: Preliminary results of the INTENSIVE study. Eur. J. Cancer 2021, 154, 246–252. [Google Scholar] [CrossRef]
- Dooling, K.; Marin, M.; Wallace, M.; McClung, N.; Chamberland, M.; Lee, G.M.; Talbot, H.K.; Romero, J.R.; Bell, B.P.; Oliver, S.E. The Advisory Committee on Immunization Practices’ Updated Interim Recommendation for Allocation of COVID-19 Vaccine—United States, December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 69, 1657–1660. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef]
- Chun, J.; Kim, S.; Park, E.; Park, S.-Y.; Koh, S.-J.; Cha, Y.; Yoo, H.; Joung, J.; Yoon, H.; Eom, B.; et al. Cancer Patients’ Willingness to Take COVID-19 Vaccination: A Nationwide Multicenter Survey in Korea. Cancers 2021, 13, 3883. [Google Scholar] [CrossRef]
- Barrière, J.; Gal, J.; Hoch, B.; Cassuto, O.; Leysalle, A.; Chamorey, E.; Borchiellini, D. Acceptance of SARS-CoV-2 vaccination among French patients with cancer: A cross-sectional survey. Ann. Oncol. 2021, 32, 673–674. [Google Scholar] [CrossRef]
- Fröjd, C.; Larsson, G.; Lampic, C.; Von Essen, L. Health related quality of life and psychosocial function among patients with carcinoid tumours. A longitudinal, prospective, and comparative study. Health Qual. Life Outcomes 2007, 5, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewis, A.R.; Wang, X.; Magdalani, L.; D’Arienzo, P.; Bashir, C.; Mansoor, W.; Hubner, R.; Valle, J.W.; McNamara, M.G. Health-related quality of life, anxiety, depression and impulsivity in patients with advanced gastroenteropancreatic neuroendocrine tumours. World J. Gastroenterol. 2018, 24, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Lauricella, E.; Cives, M.; Bracigliano, A.; Clemente, O.; Felici, V.; Lippolis, R.; Amoruso, B.; Pelle’, E.; Mandriani, B.; Esposto, C.; et al. The psychological impact of COVID-19 pandemic on patients with neuroendocrine tumors: Between resilience and vulnerability. J. Neuroendocr. 2021, 33, e13041. [Google Scholar] [CrossRef] [PubMed]

| n = 542 | Therapy n = 369 | (%) 68.1 | Surveillance n = 173 | (%) 31.9 | All | (%) |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18–40 | 14 | 3.8 | 8 | 4.6 | 22 | 4.1 |
| 41–60 | 169 | 45.8 | 85 | 49.1 | 254 | 46.9 |
| 61–80 and >80 | 186 | 50.4 | 80 | 46.3 | 266 | 49.0 |
| Tumor localization | ||||||
| small bowel | 148 | 40.1 | 60 | 34.7 | 212 | 39.1 |
| pancreas | 85 | 23.0 | 46 | 26.6 | 134 | 24.7 |
| duodenal | 36 | 9.8 | 14 | 8.1 | 50 | 9.2 |
| lung | 23 | 6.2 | 15 | 8.7 | 41 | 7.6 |
| CUP | 30 | 8.1 | 9 | 5.2 | 42 | 7.8 |
| others | 47 | 12.4 | 29 | 16.6 | 66 | 12.2 |
| Functional active | ||||||
| yes | 159 | 43.1 | 58 | 33.5 | 217 | 40.0 |
| no (+unknown) | 210 | 56.9 | 115 | 66.5 | 325 | 60.0 |
| Symptoms | ||||||
| yes | 269 | 72.9 | 104 | 60.1 | 373 | 68.8 |
| impaired resilience | 179 | 66.5 | 71 | 68.3 | 250 | 67.0 |
| diarrhea | 164 | 60.9 | 57 | 54.8 | 221 | 59.3 |
| flush | 91 | 33.8 | 18 | 17.3 | 109 | 29.2 |
| Time of diagnosis | ||||||
| >5 years | 170 | 46.1 | 80 | 46.2 | 250 | 46.1 |
| 1–5 years | 142 | 38.5 | 79 | 45.7 | 221 | 40.8 |
| <12 months | 57 | 15.4 | 14 | 8.1 | 71 | 13.1 |
| Period from symptoms to diagnosis | ||||||
| <3 months | 79 | 21.4 | 48 | 27.8 | 127 | 23.4 |
| 3–12 months | 79 | 21.4 | 44 | 25.4 | 123 | 22.7 |
| >12 months | 147 | 39.8 | 48 | 27.8 | 195 | 36.0 |
| Therapy | ||||||
| SSA | 201 | 54.5 | - | - | 201 | 54.5 |
| PRRT | 29 | 7.9 | - | - | 29 | 7.9 |
| CTx | 29 | 7.9 | - | - | 29 | 7.9 |
| TKI | 15 | 4.1 | - | - | 16 | 4.3 |
| W & W | 68 | 18.4 | - | - | 68 | 18.4 |
| Treatment setting | ||||||
| ENETS center | 122 | 33.1 | 56 | 32.4 | 178 | 32.8 |
| University Hospital (none ENETS) | 136 | 36.9 | 71 | 41.0 | 207 | 38.2 |
| Non-university Hospital | 49 | 13.3 | 15 | 8.7 | 64 | 11.8 |
| Specialist practice | 62 | 16.7 | 31 | 17.9 | 93 | 17.2 |
| n = 20 | Therapy n = 11 | (%) 55.0 | Surveillance n = 9 | (%) 45.0 | All | (%) |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18–40 | 2 | 18.2 | - | - | 2 | 10 |
| 41–60 | 4 | 36.4 | 6 | 66.6 | 10 | 50 |
| 61–80 | 5 | 45.4 | 3 | 33.3 | 8 | 40 |
| Tumor localization | ||||||
| small bowel | 5 | 45.4 | 1 | 11.1 | 6 | 30 |
| pancreas | 5 | 45.4 | 5 | 55.6 | 10 | 50 |
| others | 1 | 9.1 | 3 | 33.3 | 4 | |
| Functional active | ||||||
| yes | 3 | 27.3 | 1 | 11.1 | 4 | 20 |
| no (+unknown) | 8 | 72.7 | 8 | 88.9 | 16 | 80 |
| Symptoms | ||||||
| yes | 5 | 45.4 | 7 | 78.8 | 12 | 60 |
| no | 6 | 55.6 | 2 | 22.2 | 8 | 40 |
| Therapy | ||||||
| SSA | 5 | 45.4 | - | - | 5 | 25 |
| PRRT | 2 | 18.2 | - | - | 2 | 10 |
| CTx | 1 | 9.1 | - | - | 1 | 5 |
| TKI | 1 | 9.1 | - | - | 1 | 5 |
| W&W | 2 | 18.2 | - | - | 2 | 10 |
| Comorbidities | ||||||
| diabetes | 1 | 9.1 | 3 | 33.3 | 4 | 20 |
| hypertension | 6 | 55.6 | 5 | 55.6 | 11 | 55 |
| lung disease | 4 | 36.4 | - | - | 4 | 20 |
| chronic renal failure | - | - | 1 | 11.1 | 1 | 5 |
| liver cirrhosis | - | - | 1 | 11.1 | 1 | 5 |
| chronic infections | 1 | 9.1 | 1 | 11.1 | 2 | 10 |
| none | 2 | 18.2 | 1 | 11.1 | 3 | 15 |
| Attributed severe risk for COVID-19 infection | ||||||
| yes | 7 | 63.6 | 8 | 88.9 | 15 | 75 |
| no | 4 | 36.4 | 1 | 11.1 | 5 | 25 |
| COVID-19 disease course | ||||||
| mild | 5 | 45.4 | 4 | 44.4 | 9 | 45 |
| moderate | 5 | 45.4 | 5 | 55.6 | 10 | 50 |
| severe | 1 | 9.1 | - | - | 1 | 5 |
| Long-term effects of COVID-19 disease | ||||||
| fatigue | 5 | 45.4 | 4 | 44.4 | 9 | 45 |
| impaired concentration | 3 | 27.3 | 4 | 44.4 | 7 | 35 |
| impaired olfactory/ gustatory sense | 1 | 9.1 | 3 | 33.3 | 4 | 20 |
| insomnia | - | - | 2 | 22.2 | 2 | 10 |
| headaches | 2 | 18.2 | - | - | 2 | 10 |
| Vaccination planned | ||||||
| yes | 9 | 81.8 | 8 | 88.9 | 17 | 85 |
| undecided | 2 | 18.2 | 1 | 11.1 | 3 | 15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krug, S.; Khosravian, M.; Weissbach, J.; George, K.; Damm, M.; Garbe, J.; Walldorf, J.; Reuken, P.A.; Amin, T.; Siebenhüner, A.; et al. The Patient’s Point of View: COVID-19 and Neuroendocrine Tumor Disease. Cancers 2022, 14, 613. https://doi.org/10.3390/cancers14030613
Krug S, Khosravian M, Weissbach J, George K, Damm M, Garbe J, Walldorf J, Reuken PA, Amin T, Siebenhüner A, et al. The Patient’s Point of View: COVID-19 and Neuroendocrine Tumor Disease. Cancers. 2022; 14(3):613. https://doi.org/10.3390/cancers14030613
Chicago/Turabian StyleKrug, Sebastian, Maryam Khosravian, Julia Weissbach, Katharina George, Marko Damm, Jakob Garbe, Jens Walldorf, Philipp A. Reuken, Tania Amin, Alexander Siebenhüner, and et al. 2022. "The Patient’s Point of View: COVID-19 and Neuroendocrine Tumor Disease" Cancers 14, no. 3: 613. https://doi.org/10.3390/cancers14030613
APA StyleKrug, S., Khosravian, M., Weissbach, J., George, K., Damm, M., Garbe, J., Walldorf, J., Reuken, P. A., Amin, T., Siebenhüner, A., Rosendahl, J., Gress, T. M., Michl, P., Schrader, J., & Rinke, A. (2022). The Patient’s Point of View: COVID-19 and Neuroendocrine Tumor Disease. Cancers, 14(3), 613. https://doi.org/10.3390/cancers14030613







