Cost-Effectiveness Analysis of Axicabtagene Ciloleucel vs. Tisagenlecleucel for the Management of Relapsed/Refractory Diffuse Large B-Cell Lymphoma in Spain
Abstract
:Simple Summary
Abstract
1. Introduction
2. Results
2.1. Base Case
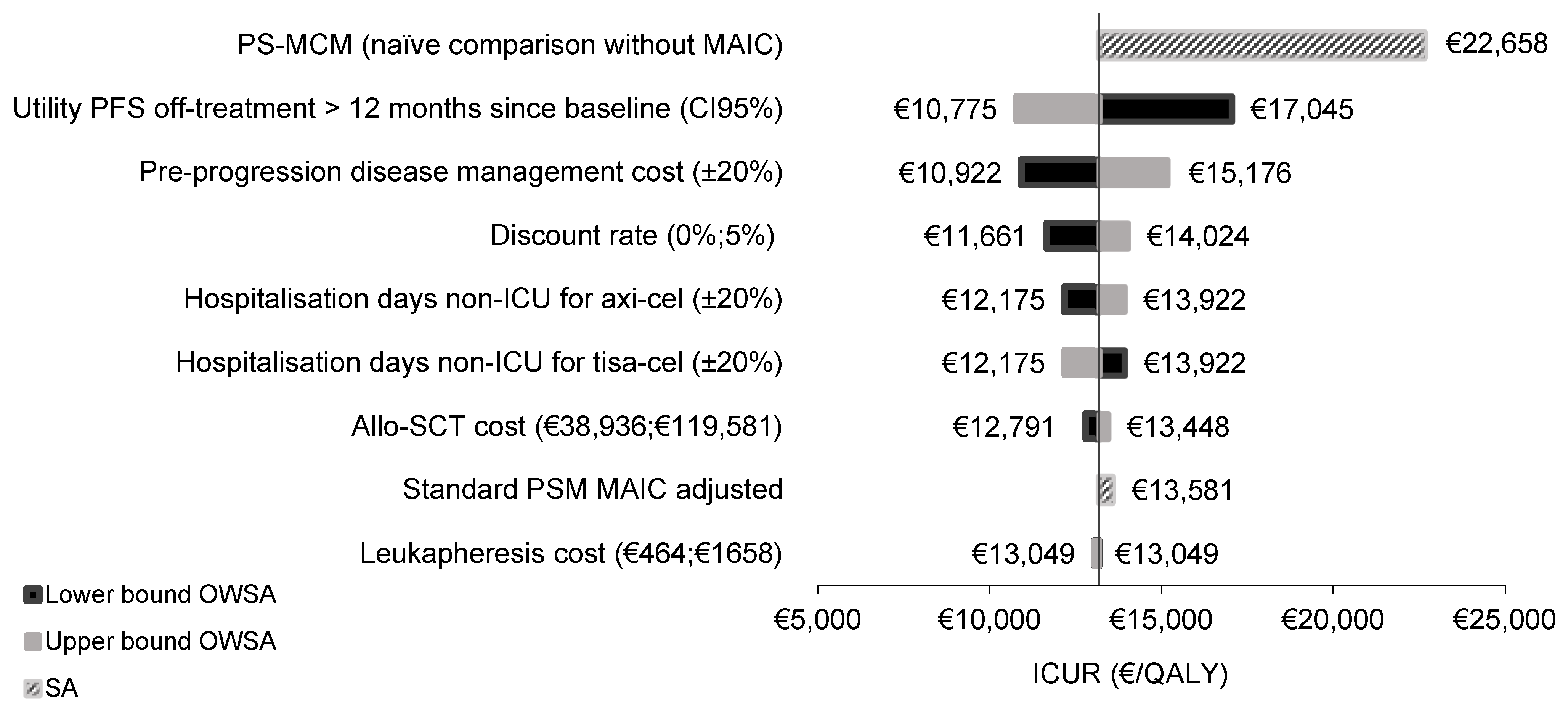
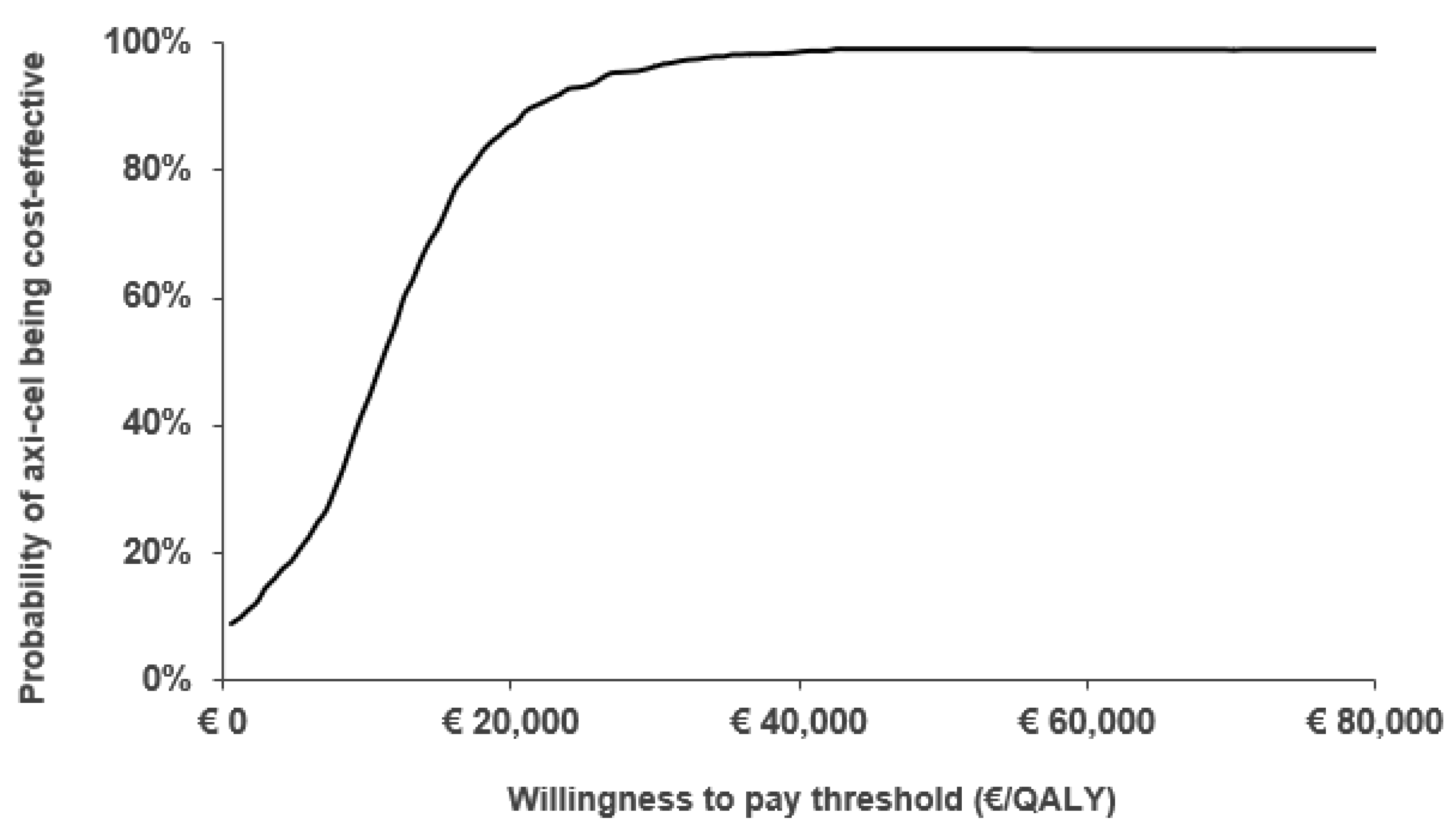
2.2. Sensitivity Analysis
3. Discussion
4. Materials and Methods
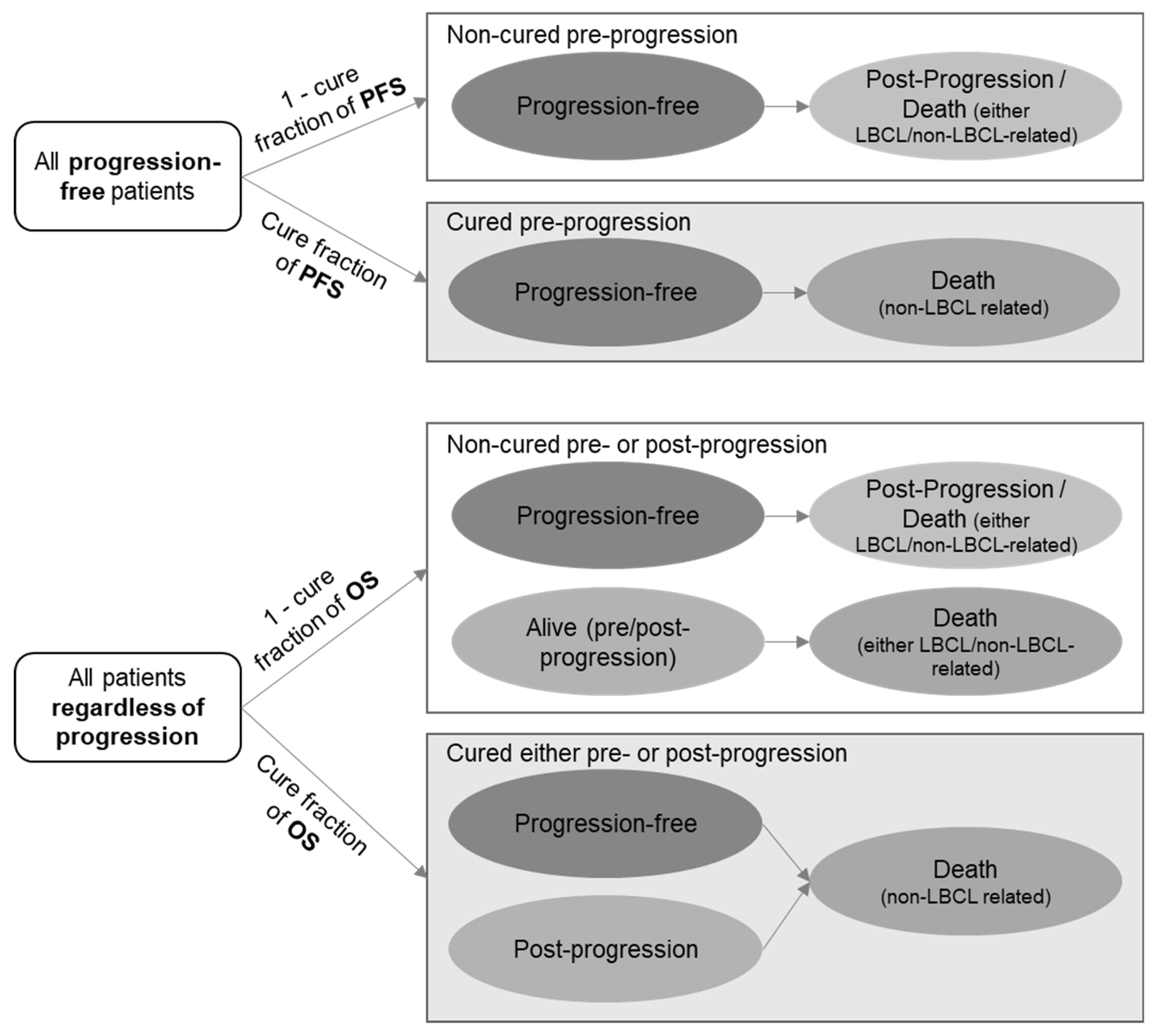
4.1. Model Structure
4.2. Population
4.3. Treatment Strategies
4.4. Clinical Data
4.5. Utilities
4.6. Resource Use and Costs
4.7. Outcomes
4.8. Sensitivity Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Cancer Institute. Adult Non-Hodgkin Lymphoma Treatment (PDQ®)—Professional Version; National Cancer Institute: London, UK, 2019. Available online: www.cancer.gov/types/lymphoma/hp/adult-nhl-treatment-pdq (accessed on 20 October 2019).
- Tilly, H.; Gomes da Silva, M.; Vitolo, U.; Jack, A.; Meignan, M.; Lopez-Guillermo, A.; Walewski, J.; André, M.; Johnson, P.W.; Pfreundschuh, M.; et al. Diffuse large B-cell lymphoma (DLBCL): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Bastos-Oreiro, M.; Muntañola, A.; Panizo, C.; Gonzalez-Barca, E.; de Villambrosia, S.G.; Córdoba, R.; López, J.L.B.; González-Sierra, P.; Terol, M.J.; Gutierrez, A.; et al. RELINF: Prospective epidemiological registry of lymphoid neoplasms in Spain. A project from the GELTAMO group. Ann Hematol. 2020, 99, 799–808. [Google Scholar] [CrossRef]
- Friedberg, J.W. Relapsed/Refractory Diffuse Large B-cell Lymphoma; Hematology, American Society of Hematology Education Program: Washington, DC, USA, 2011; pp. 498–505. [Google Scholar] [CrossRef] [Green Version]
- Crump, M.; Neelapu, S.S.; Farooq, U.; Van Den Neste, E.; Kuruvilla, J.; Westin, J.; Link, B.K.; Hay, A.; Cerhan, J.R.; Zhu, L.; et al. Outcomes in refractory diffuse large B-cell lymphoma: Results from the international SCHOLAR-1 study. Blood 2017, 130, 1800–1808. [Google Scholar] [CrossRef]
- Hopfinger, G.; Worel, N. CAR T-cell therapy in diffuse large B-cell lymphoma. MEMO 2020, 13, 32–35. [Google Scholar] [CrossRef] [Green Version]
- Locke, F.L.; Ghobadi, A.; Jacobson, C.A.; Miklos, D.B.; Lekakis, L.J.; Oluwole, O.O.; Lin, Y.; Braunschweig, I.; Hill, B.T.; Timmerman, J.M.; et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): A single-arm, multicentre, phase 1-2 trial. Lancet Oncol. 2019, 20, 31–42. [Google Scholar] [CrossRef]
- Schuster, S.J.; Bishop, M.R.; Tam, C.S.; Waller, E.K.; Borchmann, P.; McGuirk, J.P.; Jäger, U.; Jaglowski, S.; Andreadis, C.; Westin, J.R.; et al. Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N. Engl. J. Med. 2019, 380, 45–56. [Google Scholar] [CrossRef]
- Oluwole, O.O.; Jansen, J.P.; Lin, V.W.; Chan, K.; Keeping, S.; Navale, L.; Locke, F.L. Comparing Efficacy, Safety, and Preinfusion Period of Axicabtagene Ciloleucel versus Tisagenlecleucel in Relapsed/Refractory Large B Cell Lymphoma. Biol. Blood Marrow Transplant. 2020, 26, 1581–1588. [Google Scholar] [CrossRef]
- Jørgensen, J.; Hanna, E.; Kefalas, P. Outcomes-based reimbursement for gene therapies in practice: The experience of recently launched CAR-T cell therapies in major European countries. J. Mark. Access Health Policy 2020, 8, 1715536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vallejo-Torres, L.; García-Lorenzo, B.; Serrano-Aguilar, P. Estimating a cost-effectiveness threshold for the Spanish NHS. Health Econ. 2018, 27, 746–761. [Google Scholar] [CrossRef]
- Sacristán, J.A.; Oliva, J.; Campillo-Artero, C.; Puig-Junoy, J.; Pinto-Prades, J.L.; Dilla, T.; Rubio-Terrés, C.; Ortún, V. What is an efficient health intervention in Spain in 2020? Gac Sanit. 2020, 34, 189–193. [Google Scholar] [CrossRef]
- Informe de seguimiento de la Dirección General de Cartera Común de Servicios del Sistema Nacional de Salud (SNS) y Farmacia sobre el Plan para el Abordaje de las Terapias Avanzadas en el SNS; Ministry of Health: Madrid, Spain, 2020; Available online: https://www.mscbs.gob.es/profesionales/farmacia/pdf/20201201.Informe_MS_seguimiento_Plan_terapias_avanzadas_SNS.pdf (accessed on 23 February 2021).
- Liu, R.; Oluwole, O.O.; Diakite, I.; Botteman, M.F.; Snider, J.T.; Locke, F.L. Cost effectiveness of axicabtagene ciloleucel versus tisagenlecleucel for adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy in the United States. J. Med. Econ. 2021, 24, 458–468. [Google Scholar] [CrossRef]
- Marchetti, M.; Martelli, E.; Zinzani, P.L. Cost-effectiveness of axicabtagene ciloleucel for relapsed or refractory diffuse large B-cell lymphoma in Italy. Blood 2018, 132, 4779. [Google Scholar] [CrossRef]
- Roth, J.A.; Sullivan, S.D.; Lin, V.W.; Bansal, A.; Purdum, A.G.; Navale, L.; Cheng, P.; Ramsey, S.D. Cost-effectiveness of axicabtagene ciloleucel for adult patients with relapsed or refractory large B-cell lymphoma in the United States. J. Med. Econ. 2018, 21, 1238–1245. [Google Scholar] [CrossRef]
- Yang, H.; Qi, C.; Zhang, J.; El Ouagari, K. Cost-effectiveness of tisagenlecleucel for adults with relapsed or refractory diffuse large b-cell lymphoma: A canadian societal perspective. Value Health 2018, 21, S44. [Google Scholar] [CrossRef] [Green Version]
- Moradi-Lakeh, M.; Yaghoubi, M.; Seitz, P.; Javanbakht, M.; Brock, E. Cost-Effectiveness of Tisagenlecleucel in Paediatric Acute Lymphoblastic Leukaemia (pALL) and Adult Diffuse Large B-Cell Lymphoma (DLBCL) in Switzerland. Adv Ther. 2021, 38, 3427–3443. [Google Scholar] [CrossRef]
- Ministry of Health. Ministerio de Sanidad Consumo y Bienestar Social (MSCBS)—Dirección General de Cartera Básica de Servicios del SNS y Farmacia (DGCYF). 2019. Available online: https://www.mscbs.gob.es/profesionales/farmacia/valtermed/docs/VALTERMED_Preguntas_y_Respuestas.pdf (accessed on 22 February 2021).
- Phillippo, D.M.; Ades, A.E.; Dias, S.; Palmer, S.; Abrams, K.R.; Welton, K.J. NICE DSU Technical Support Document 18: Methods for Population-Adjusted Indirect Comparisons in Submissions to NICE; National Institute for Health and Care Excellence: Sheffield, UK, 2016; Available online: https://www.nice.org.uk/guidance/ta306 (accessed on 17 February 2021).
- National Institute for Health and Care Excellence. Tisagenlecleucel for Treating Relapsed or Refractory Diffuse Large B-Cell Lymphoma after 2 or More Systemic Therapies; Technology Appraisal Guidance [TA567]; National Institute for Health and Care Excellence: Sheffield, UK, 2019; Available online: https://www.nice.org.uk/guidance/ta567 (accessed on 18 February 2021).
- National Institute for Health and Care Excellence. Axicabtagene ciloleucel for Treating Diffuse Large B-cell Lymphoma and Primary Mediastinal Large B-cell Lymphoma after 2 or More Systemic Therapies; Technology Appraisal Guidance [TA559]; National Institute for Health and Care Excellence: Sheffield, UK, 2019; Available online: https://www.nice.org.uk/guidance/ta559 (accessed on 18 February 2021).
- Whittington, M.D.; McQueen, R.B.; Ollendorf, D.A.; Kumar, V.M.; Chapman, R.H.; Tice, J.A.; Pearson, S.D.; Campbell, J.D. Long-term Survival and Cost-effectiveness Associated with Axicabtagene Ciloleucel vs. Chemotherapy for Treatment of B-Cell Lymphoma. JAMA Netw. Open. 2019, 2, e190035. [Google Scholar] [CrossRef]
- Zhang, J.; Li, J.; Ma, Q.; Yang, H.; Signorovitch, J.; Wu, E. Letter to the Editor Regarding “Comparing Efficacy, Safety, and Preinfusion Period of Axicabtagene Ciloleucel versus Tisagenlecleucel in Relapsed/Refractory Large B Cell Lymphoma”. Biol. Blood Marrow. Transplant. 2020, 26, e333–e334. [Google Scholar] [CrossRef]
- Bansal, A.; Sullivan, S.D.; Lin, V.W.; Purdum, A.G.; Navale, L.; Cheng, P.; Ramsey, S.D. Estimating Long-Term Survival for Patients with Relapsed or Refractory Large B-Cell Lymphoma Treated with Chimeric Antigen Receptor Therapy: A Comparison of Standard and Mixture Cure Models. Med. Decis. Mak. 2019, 39, 294–298. [Google Scholar] [CrossRef]
- Othus, M.; Barlogie, B.; Leblanc, M.L.; Crowley, J.J. Cure models as a useful statistical tool for analyzing survival. Clin. Cancer Res. 2012, 18, 3731–3736. [Google Scholar] [CrossRef] [Green Version]
- Othus, M.; Bansal, A.; Koepl, L.; Wagner, S.; Ramsey, S. Accounting for cured patients in cost-effectiveness analysis. Value Health 2017, 20, 705–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López-Bastida, J.; Oliva, J.; Antoñanzas, F.; García-Altés, A.; Gisbert, R.; Mar, J.; Puig-Junoy, J. Spanish recommendations on economic evaluation of health technologies. Eur. J. Health Econ. 2010, 11, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Ortega, A.; Marín, R.; Fraga, M.D.; López-Briz, E.; Puigventós, F. (GENESIS-SEFH). Guía de evaluación económica e impacto presupuestario en los informes de evaluación de medicamentos. Guía práctica asociada al programa MADRE v 4.0; Sociedad Española de Farmacia Hospitalaria: Madrid, Spain, 2017; Available online: http://gruposdetrabajo.sefh.es/genesis (accessed on 23 February 2021).
- Instituto Nacional de Estadística. Tablas de Mortalidad proyectadas 2016–2065: Esperanza de Vida por edad y sexo; Instituto Nacional de Estadística: Madrid, Spain, 2020; Available online: www.ine.es (accessed on 10 December 2021).
- Lin, V.; Jiang, Y.; Chuang, L.H.; Navale, L.; Cheng, P.; Purdum, A. Poster B439: Health Utilities for Patients With Relapsed or Refractory Large B Cell Lymphoma (R/R-LBCL) Ad Hoc Analysis From an Axicabtagene Ciloleucel (Axi-Cel) Safety Management Study. In Proceedings of the 44th Annual Meeting of the European Society for Blood and Marrow Transplantation, Lisbon, Portugal, 18–21 March 2018. [Google Scholar]
- Chen, Q.; Staton, A.D.; Ayer, T.; Goldstein, D.A.; Koff, J.L.; Flowers, C.R. Exploring the potential cost-effectiveness of precision medicine treatment strategies for diffuse large B-cell lymphoma. Leukemia Lymphoma 2018, 59, 1700–1709. [Google Scholar] [CrossRef] [PubMed]
- Base de datos del Conocimiento Sanitario—Bot Plus 2.0. Consejo General de Colegios Oficiales de Farmacéuticos. 2020. Available online: https://botplusweb.portalfarma.com/ (accessed on 10 December 2020).
- Relación Informativa de Medicamentos Afectados por las Deducciones Establecidas en el Real Decreto Ley 8/2010 de 20 de Mayo por el que se Adoptan Medidas Extraordinarias para la Reducción del Déficit Público; Ministry of Health: Madrid, Spain, 2021; Available online: https://www.mscbs.gob.es/profesionales/farmacia/pdf/DeduccionesFebrero2021.pdf (accessed on 23 February 2021).
- Oblikue Consulting. Base de datos de Costes Sanitarios eSalud. Oblikue Consulting, 2020. Available online: http://www.oblikue.com/bddcostes/ (accessed on 10 December 2020).
- Instituto Nacional de Estadística. Cálculo de Variaciones Del Índice de Precios de Consumo [Internet]; Instituto Nacional de Estadística: Madrid, Spain, 2020; Available online: https://www.ine.es/calcula/calcula.do (accessed on 15 December 2020).
| Health Outcomes | Axicabtagene Ciloleucel | Tisagenlecleucel | Incremental |
|---|---|---|---|
| Overall survival | |||
| % alive at 1 year | 75.3% | 47.3% | 28.0% |
| % alive at 2 years | 61.2% | 38.3% | 22.8% |
| % alive at 5 years | 50.1% | 34.4% | 15.7% |
| % alive at 10 years | 45.2% | 32.5% | 12.7% |
| % alive at 20 years | 36.8% | 27.0% | 9.8% |
| % alive at 30 years | 19.8% | 14.6% | 5.2% |
| % alive at 40 years | 2.2% | 1.6% | 0.6% |
| Total LYG per patient | 9.45 | 6.71 | 2.74 |
| LYG in pre-progression state | 8.87 | 5.97 | 2.90 |
| LYG in post-progression state | 0.58 | 0.75 | −0.16 |
| Total QALY per patient | 7.47 | 5.16 | 2.31 |
| QALYs in pre-progression state | 7.25 | 4.87 | 2.37 |
| QALYs in post-progression state | 0.23 | 0.29 | −0.06 |
| Costs | |||
| Total costs per patient | €430,746.52 | €400,611.79 | €30,134.73 |
| Drug acquisition costs † | €313,920.00 | €307,200.00 | €6720.00 |
| Leukapheresis costs | €1030.68 | €1030.68 | €0.00 |
| Conditioning chemotherapy costs | €4270.89 | €4234.24 | €36.65 |
| CAR T administration and monitoring costs ‡ | €20,257.42 | €20,257.42 | €0.00 |
| SCT costs | €5574.17 | €4247.66 | €1326.51 |
| Health state medical costs: pre-progression state | €75,035.09 | €50,473.64 | €24,561.45 |
| Health state medical costs: post-progression state | €8065.4 | €10,333.30 | −€2267.76 |
| End-of-life care costs | €2299.85 | €2548.29 | −€248.44 |
| AEs costs | €292.88 | €286.56 | €6.32 |
| ICER (axi-cel vs. tisa-cel) | €10,998.64/LYG | ||
| ICUR (axi-cel vs. tisa-cel) | €13,048.58/QALY | ||
| Health State | Utility Value |
| Pre-progression [31] | |
| Pre-progression: CAR T on treatment (1st month) | 0.740 |
| Pre-progression: off-treatment ≤12 months | 0.782 |
| Pre-progression: off-treatment >12 months | 0.820 |
| Post-progression [32] | 0.390 |
| Treatment Related Costs | Cost |
| Drug acquisition costs [33,34] | |
| Axi-cel: 0.4–2.0 × 108 cells/kg | €313,920.00 † |
| Tisa-cel: 1.2 × 106−6.0 × 108 cells/kg | €307,200.00 † |
| Leukapheresis [35] | €1064.79 |
| Lymphodepleting chemotherapy: axi-cel [33,34] | €174.84 |
| Lymphodepleting chemotherapy: tisa-cel [33,34] | €138.18 |
| CAR T administration and monitoring [35] | €8767.73 |
| Allo-SCT [35] | €70,559.14 |
| Auto-SCT [35] | €48,591.37 |
| ICU hospitalisation (per day) [35] | €1338.45 |
| Non-ICU hospitalisation (per day) [35] | €722.89 |
| End-of-life care [35] | €3132.52 |
| Health states medical resource costs | |
| Pre-progression health state (€/month) [33,34,35] | €704.89 |
| Post-progression health state (€/month) [33,34,35] | €1153.43 |
| AE management cost | |
| Cytokine release syndrome [33,34,35] | €1073.59 |
| Neurological events [33,34,35] | €713.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bastos-Oreiro, M.; de las Heras, A.; Presa, M.; Casado, M.A.; Pardo, C.; Martín-Escudero, V.; Sureda, A. Cost-Effectiveness Analysis of Axicabtagene Ciloleucel vs. Tisagenlecleucel for the Management of Relapsed/Refractory Diffuse Large B-Cell Lymphoma in Spain. Cancers 2022, 14, 538. https://doi.org/10.3390/cancers14030538
Bastos-Oreiro M, de las Heras A, Presa M, Casado MA, Pardo C, Martín-Escudero V, Sureda A. Cost-Effectiveness Analysis of Axicabtagene Ciloleucel vs. Tisagenlecleucel for the Management of Relapsed/Refractory Diffuse Large B-Cell Lymphoma in Spain. Cancers. 2022; 14(3):538. https://doi.org/10.3390/cancers14030538
Chicago/Turabian StyleBastos-Oreiro, Mariana, Ana de las Heras, María Presa, Miguel A. Casado, Carlos Pardo, Victoria Martín-Escudero, and Anna Sureda. 2022. "Cost-Effectiveness Analysis of Axicabtagene Ciloleucel vs. Tisagenlecleucel for the Management of Relapsed/Refractory Diffuse Large B-Cell Lymphoma in Spain" Cancers 14, no. 3: 538. https://doi.org/10.3390/cancers14030538
APA StyleBastos-Oreiro, M., de las Heras, A., Presa, M., Casado, M. A., Pardo, C., Martín-Escudero, V., & Sureda, A. (2022). Cost-Effectiveness Analysis of Axicabtagene Ciloleucel vs. Tisagenlecleucel for the Management of Relapsed/Refractory Diffuse Large B-Cell Lymphoma in Spain. Cancers, 14(3), 538. https://doi.org/10.3390/cancers14030538






