Different Oncologic Outcomes in Early-Onset and Late-Onset Sporadic Colorectal Cancer: A Regression Analysis on 2073 Patients
Abstract
Simple Summary
Abstract
1. Introduction
- It gives a contribution to the still-debated oncologic outcomes in EOCRC.
- It is the first report that early age of onset is a strong predictor for worse oncologic outcomes in CRC patients.
- It is the first report that EOCRC have a worse prognosis at earlier stages,
- It gives a contribution to the still limited comparative data on a large surgical population of sporadic early- and late-onset CRC.
- The results may be a starting point for further research on the topic.
2. Materials and Methods
2.1. Study Design and Patients’ Selection
2.2. Endpoints and Variables
2.3. Statistical Analysis
3. Results
3.1. Demographics and Clinical Presentation
3.2. Operative Data and Postoperative Outcomes
3.3. Pathological and Molecular Features
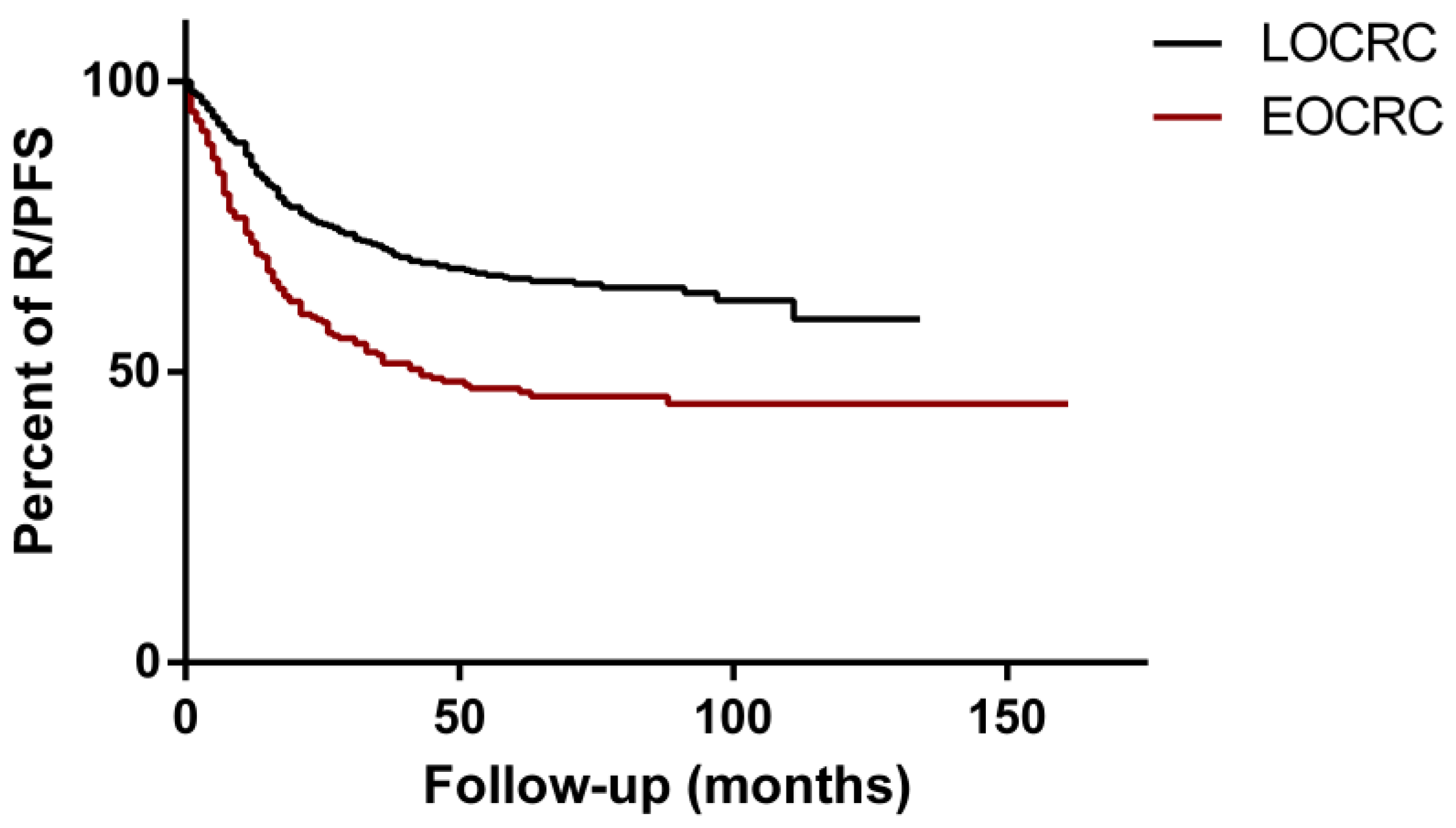
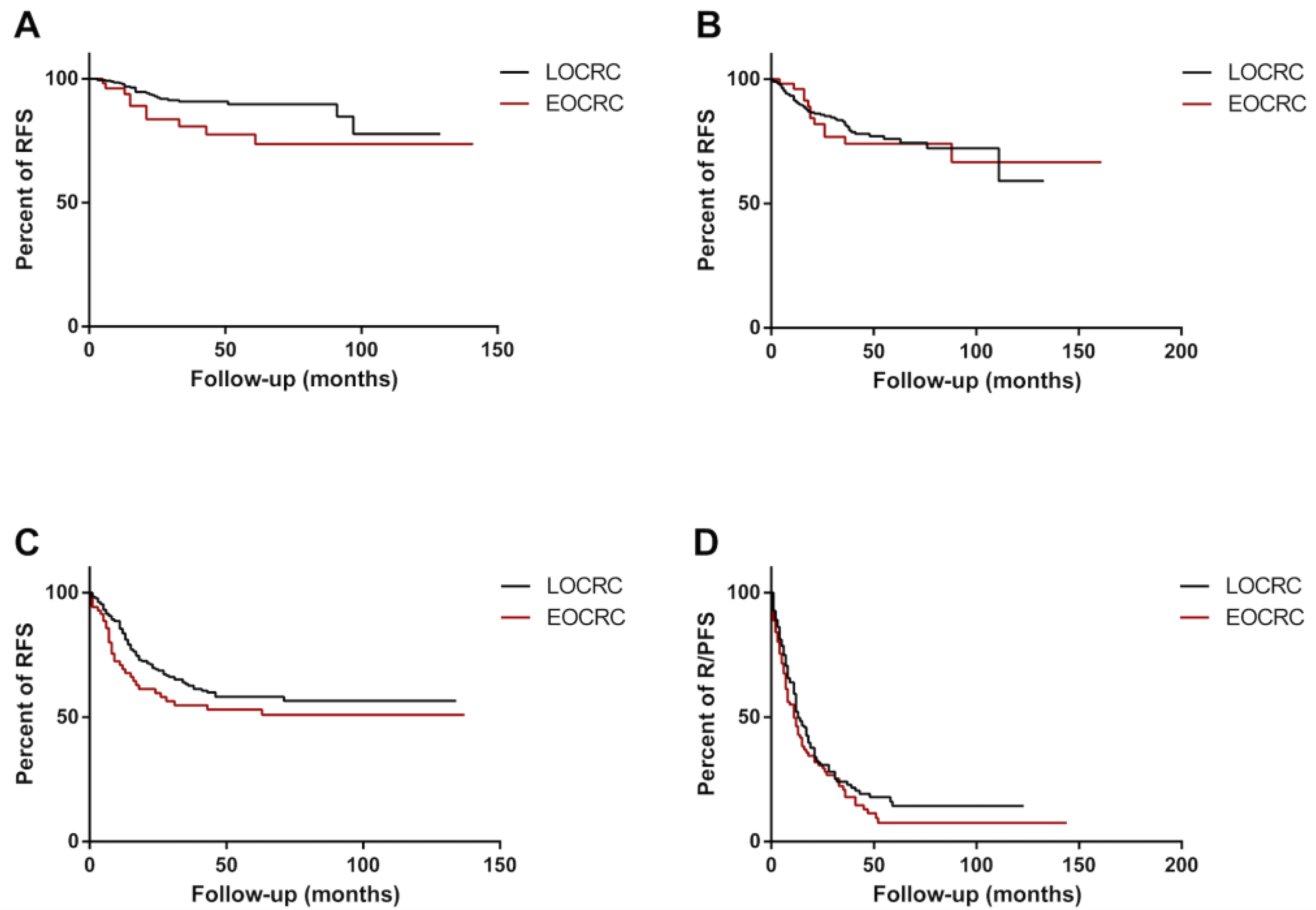
3.4. Oncological Outcomes
3.5. Univariable and Multivariable Analysis
3.6. Stage-Dependent R/PFS Analysis
4. Discussion
- The limitations of this study are inherent to its partially retrospective design and the wide time spanning, as therapies have changed. The monocentric nature can be both considered as a limitation and as one of the strengths, because the single institutional database allowed for a greater accuracy in data gathering and analysis. Another limitation relies on the high disproportion among the two samples, possibly leading to a random bias. This study has also some strong points: the very strict age-definition of EOCRC and the large surgical sample of sporadic EOCRC patients offers a significant amount of data. This is the first work reporting early age of onset as an independent risk factor for worse prognosis, particularly at early stages. Furthermore, our work gives a contribution to the still-debated topic of oncologic outcomes in EOCRC.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Collaborative, R.; Zaborowski, A.M.; Abdile, A.; Adamina, M.; Aigner, F.; d’Allens, L.; Allmer, C.; Alvarez, A.; Anula, R.; Andric, M.; et al. Characteristics of Early-Onset vs. Late-Onset Colorectal Cancer: A Review. JAMA Surg. 2021, 156, 865–874. [Google Scholar] [CrossRef] [PubMed]
- Himbert, C.; Figueiredo, J.C.; Shibata, D.; Ose, J.; Lin, T.; Huang, L.C.; Peoples, A.R.; Scaife, C.L.; Pickron, B.; Lambert, L.; et al. Clinical Characteristics and Outcomes of Colorectal Cancer in the ColoCare Study: Differences by Age of Onset. Cancers 2021, 13, 3817. [Google Scholar] [CrossRef] [PubMed]
- Alyabsi, M.; Algarni, M.; Alshammari, K. Trends in Colorectal Cancer Incidence Rates in Saudi Arabia (2001–2016) Using Saudi National Registry: Early- Versus Late-Onset Disease. Front. Oncol. 2021, 11, 730689. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.H.; Li, J.; Liu, L.J.; Zheng, N.X.; Zheng, K.; Mei, Z.; Bai, C.G.; Zhang, W. Trends, clinicopathological features, surgical treatment patterns and prognoses of early-onset versus late-onset colorectal cancer: A retrospective cohort study on 34067 patients managed from 2000 to 2021 in a Chinese tertiary center. Int. J. Surg. 2022, 104, 106780. [Google Scholar] [CrossRef]
- Saad El Din, K.; Loree, J.M.; Sayre, E.C.; Gill, S.; Brown, C.J.; Dau, H.; De Vera, M.A. Trends in the epidemiology of young-onset colorectal cancer: A worldwide systematic review. BMC Cancer 2020, 20, 288. [Google Scholar] [CrossRef]
- Wells, K.; Wise, P.E. Hereditary Colorectal Cancer Syndromes. Surg. Clin. N. Am. 2017, 97, 605–625. [Google Scholar] [CrossRef]
- Pearlman, R.; Frankel, W.L.; Swanson, B.; Zhao, W.; Yilmaz, A.; Miller, K.; Bacher, J.; Bigley, C.; Nelsen, L.; Goodfellow, P.J.; et al. Prevalence and Spectrum of Germline Cancer Susceptibility Gene Mutations Among Patients with Early-Onset Colorectal Cancer. JAMA Oncol. 2017, 3, 464–471. [Google Scholar] [CrossRef]
- You, Y.N.; Dozois, E.J.; Boardman, L.A.; Aakre, J.; Huebner, M.; Larson, D.W. Young-onset rectal cancer: Presentation, pattern of care and long-term oncologic outcomes compared to a matched older-onset cohort. Ann. Surg. Oncol. 2011, 18, 2469–2476. [Google Scholar] [CrossRef]
- Orsini, R.G.; Verhoeven, R.H.; Lemmens, V.E.; van Steenbergen, L.N.; de Hingh, I.H.; Nieuwenhuijzen, G.A.; Rutten, H.J. Comparable survival for young rectal cancer patients, despite unfavourable morphology and more advanced-stage disease. Eur. J. Cancer 2015, 51, 1675–1682. [Google Scholar] [CrossRef]
- Kolarich, A.; George, T.J., Jr.; Hughes, S.J.; Delitto, D.; Allegra, C.J.; Hall, W.A.; Chang, G.J.; Tan, S.A.; Shaw, C.M.; Iqbal, A. Rectal cancer patients younger than 50 years lack a survival benefit from NCCN guideline-directed treatment for stage II and III disease. Cancer 2018, 124, 3510–3519. [Google Scholar] [CrossRef]
- Foppa, C.; Francesca Bertuzzi, A.; Cianchi, F.; Carvello, M.; Maroli, A.; Wolthuis, A.M.; Rimassa, L.; Laghi, L.; Montorsi, M.; D’Hoore, A.J.L.; et al. Rectal Cancer in Adolescent and Young Adult Patients: Pattern of Clinical Presentation and Case-Matched Comparison of Outcomes. Dis. Colon. Rectum. 2021, 64, 1064–1073. [Google Scholar] [CrossRef] [PubMed]
- Foppa, C.; Tamburello, S.; Maroli, A.; Carvello, M.; Poliani, L.; Laghi, L.; Malesci, A.; Montorsi, M.; Perea, J.; Spinelli, A. Early age of onset is an independent predictor for worse disease-free survival in sporadic rectal cancer patients. A comparative analysis of 980 consecutive patients. Eur. J. Surg. Oncol. 2022, 48, 857–863. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Park, J.G.; Vasen, H.F.; Park, K.J.; Peltomaki, P.; Ponz de Leon, M.; Rodriguez-Bigas, M.A.; Lubinski, J.; Beck, N.E.; Bisgaard, M.L.; Miyaki, M.; et al. Suspected hereditary nonpolyposis colorectal cancer: International Collaborative Group on Hereditary Non-Polyposis Colorectal Cancer (ICG-HNPCC) criteria and results of genetic diagnosis. Dis. Colon. Rectum. 1999, 42, 710–715; discussion 715–716. [Google Scholar] [CrossRef] [PubMed]
- Gambella, A.; Falco, E.C.; Benazzo, G.; Osella-Abate, S.; Senetta, R.; Castellano, I.; Bertero, L.; Cassoni, P. The Importance of Being “That” Colorectal pT1: A Combined Clinico-Pathological Predictive Score to Improve Nodal Risk Stratification. Front. Med. 2022, 9, 837876. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.; Zheng, B.; Zheng, Q.; Chen, P. Influence of Old Age on Risk of Lymph Node Metastasis and Survival in Patients with T1 Colorectal Cancer: A Population-Based Analysis. Front. Oncol. 2021, 11, 706488. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, J.B.; Maggard, M.A.; Liu, J.H.; Etzioni, D.A.; Livingston, E.H.; Ko, C.Y. Do young colon cancer patients have worse outcomes? World J. Surg. 2004, 28, 558–562. [Google Scholar] [CrossRef]
- Saraste, D.; Jaras, J.; Martling, A. Population-based analysis of outcomes with early-age colorectal cancer. Br. J. Surg. 2020, 107, 301–309. [Google Scholar] [CrossRef]
- Zaborowski, A.M.; Murphy, B.; Creavin, B.; Rogers, A.C.; Kennelly, R.; Hanly, A.; Martin, S.T.; O’Connell, P.R.; Sheahan, K.; Winter, D.C. Clinicopathological features and oncological outcomes of patients with young-onset rectal cancer. Br. J. Surg. 2020, 107, 606–612. [Google Scholar] [CrossRef]
- Park, K.S.; Hong, Y.K.; Choi, Y.J.; Kang, J.G. Clinicopathologic characteristics of early-onset colorectal cancer. Ann. Coloproctol. 2022, 38, 362–369. [Google Scholar] [CrossRef]
- Bertocchi, A.; Carloni, S.; Ravenda, P.S.; Bertalot, G.; Spadoni, I.; Lo Cascio, A.; Gandini, S.; Lizier, M.; Braga, D.; Asnicar, F.; et al. Gut vascular barrier impairment leads to intestinal bacteria dissemination and colorectal cancer metastasis to liver. Cancer Cell 2021, 39, 708–724.e11. [Google Scholar] [CrossRef] [PubMed]
- Marx, O.M.; Mankarious, M.M.; Eshelman, M.A.; Ding, W.; Koltun, W.A.; Yochum, G.S. Transcriptome Analyses Identify Deregulated MYC in Early Onset Colorectal Cancer. Biomolecules 2022, 12, 1223. [Google Scholar] [CrossRef] [PubMed]
- Archambault, A.N.; Su, Y.R.; Jeon, J.; Thomas, M.; Lin, Y.; Conti, D.V.; Win, A.K.; Sakoda, L.C.; Lansdorp-Vogelaar, I.; Peterse, E.F.P.; et al. Cumulative Burden of Colorectal Cancer-Associated Genetic Variants Is More Strongly Associated with Early-Onset vs Late-Onset Cancer. Gastroenterology 2020, 158, 1274–1286.e12. [Google Scholar] [CrossRef] [PubMed]
- Berg, M.; Agesen, T.H.; Thiis-Evensen, E.; INFAC-study group; Merok, M.A.; Teixeira, M.R.; Vatn, M.H.; Nesbakken, A.; Skotheim, R.I.; Lothe, R.A. Distinct high resolution genome profiles of early onset and late onset colorectal cancer integrated with gene expression data identify candidate susceptibility loci. Mol. Cancer 2010, 9, 100. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | LOCRC | EOCRC | p |
|---|---|---|---|
| Number of patients | 1650 | 423 | |
| Age, years | 68.78 ± 10.07 | 42.44 ± 5.90 | <0.0001 |
| Gender, females | 41% (676) | 50% (212) | 0.003 |
| BMI, Kg/m2 | 25.21 ± 4.13 | 24.73 ± 4.40 | 0.055 |
| Obesity (BMI ≥ 30) | 17% (280) | 16% (68) | 0.528 |
| Smoking status | <0.0001 | ||
| Non-smokers | 60% (990) | 65% (275) | |
| Current smokers | 16% (264) | 23% (97) | |
| Ex-smokers | 24% (396) | 12% (51) | |
| Tumor location | <0.0001 | ||
| Right colon | 27% (445) | 22% (93) | |
| Left colon | 22% (363) | 32% (135) | |
| Rectum | 51% (842) | 46% (195) | |
| Relevant comorbidities | 80% (1320) | 21% (89) | <0.0001 |
| Preoperative treatment | 35% 585 | 49% 207 | <0.0001 |
| RT-CHT (RC patients) | 44% (375) | 51% (100) | |
| RT-CHT + systemic CHT (RC patients) | 6% (54) | 16% (32) | |
| Systemic CHT (RC or CRC patients) | 9% (156) | 18% (75) | |
| Synchronous tumors | 3% (50) | 2% (8) | 0.164 |
| Right colon | 38% (19) | 17% (1) | |
| Left colon | 43% (22) | 83% (7) | |
| Rectum | 19% (10) | -- | |
| Metastatic disease | 15% (248) | 34% (144) | <0.0001 |
| Family history of cancer | 48% (792) | 44% (186) | 0.285 |
| Family history of CRC | 20% (330) | 25% (106) | 0.048 |
| Outcome | LOCRC | EOCRC | p |
|---|---|---|---|
| Number of patients | 1650 | 423 | |
| Combined surgery on CRC and metastases (one or two stage) | 94% (233) | 90% (130) | 0.003 |
| Surgical setting | 0.002 | ||
| Elective surgery | 99% (1634) | 96% (406) | |
| Emergent surgery | 1% (16) | 4% (17) | |
| Surgical approach | <0.0001 | ||
| Minimally invasive surgery | 82% (1353) | 72% (305) | |
| Open surgery | 18% (297) | 28% (118) | |
| Operative time, minutes | 230.88 ± 93.23 | 239.92 ± 110.17 | 0.114 |
| Length of hospital stay, days | 5 [3–7] | 5 [5–8] | <0.0001 |
| Ninety-day postoperative complications | 29% (478) | 22% (93) | 0.010 |
| Clavien-Dindo I | 23% (110) | 12% (11) | |
| Clavien-Dindo II | 38% (182) | 43% (40) | |
| Clavien-Dindo IIIa | 11% (52) | 16% (15) | |
| Clavien-Dindo IIIb | 22% (105) | 27% (25) | |
| Clavien-Dindo IVa | 5% (23) | 1% (1) | |
| Clavien-Dindo IVb | 1% (6) | 1% (1) | |
| Clavien-Dindo V | -- | -- | |
| Ninety-day postoperative reoperations | 8% (132) | 7% (29) | 0.892 |
| Feature | LOCRC | EOCRC | p |
|---|---|---|---|
| Number of patients | 1650 | 423 | |
| Tumor regression (Dworak classification) | 0.019 | ||
| Dworak 0 | 4% (17) | 11% (14) | |
| Dworak 1 | 20% (86) | 23% (31) | |
| Dworak 2 | 24% (103) | 29% (38) | |
| Dworak 3 | 35% (150) | 25% (33) | |
| Dworak 4 | 17% (73) | 12% (16) | |
| Major or complete response to neoadjuvant therapy | 24% (103) | 34% (45) | 0.005 |
| Tumoral stage, AJCC 8th edition | <0.0001 | ||
| Stage 0 | 5% (70) | 5% (16) | |
| Stage I | 26% (428) | 18% (61) | |
| Stage II | 29% (476) | 19% (65) | |
| Stage III | 25% (414) | 25% (86) | |
| Stage IV | 15% (248) | 33% (116) | |
| Tumoral stage | 0.064 | ||
| 0 | 5% (82) | 6% (20) | |
| 1 | 14% (215) | 11% (39) | |
| 2 | 19% (319) | 14% (50) | |
| 3 | 50% (818) | 52% (178) | |
| 4 | 12% (202) | 17% (57) | |
| Node stage | <0.0001 | ||
| 0 | 61% (1002) | 48% (165) | |
| 1c | 2% (38) | 2% (6) | |
| 1 | 24% (385) | 25% (87) | |
| 2 | 13% (211) | 25% (86) | |
| Metastasis stage | <0.0001 | ||
| 0 | 85% (1388) | 66% (228) | |
| 1 | 15% (248) | 34% (116) | |
| Number of harvested lymph nodes | 22 [17–29] | 23 [19–34] | 0.0002 |
| Lymph nodes ratio | 0.10 [0.05–0.22] | 0.29 [0.07–1.00] | <0.0001 |
| Mucinous tumor | 15% (249) | 17% (57) | 0.513 |
| Signet-ring cells phenotype | 1% (25) | 3% (9) | 0.169 |
| Extramural invasion | 27% (441) | 22% (76) | 0.068 |
| Lymphovascular invasion | 33% (594) | 27% (93) | 0.026 |
| Perineural invasion | 12% (197) | 16% (54) | 0.074 |
| Tumor differentiation | <0.0001 | ||
| Grade 0 | 1% (18) | 1% (1) | |
| Grade 1 | 2% (30) | 1% (6) | |
| Grade 2 | 44% (726) | 38% (131) | |
| Grade 3 | 36% (586) | 28% (98) | |
| Grade 4 | 1% (17) | 1% (1) | |
| Not determinable | 16% (256) | 31% (107) | |
| Resection margins | 0.090 | ||
| R0 | 98% (1604) | 99% (343) | |
| R1 | 1.9% (31) | 1% (1) | |
| R2 | 0.1% (1) | -- | |
| Microsatellite Instability | 6% (99) | 4% (17) | 0.113 |
| Mutations ‡ | 13% (203) | 51% (78) | <0.0001 |
| Outcomes | LOCRC | EOCRC | p |
|---|---|---|---|
| Number of patients | 1650 | 423 | |
| Metachronous CRC tumors | 2% (33) | 0.2% (1) | 0.073 |
| Other neoplasms | 19% (314) | 4% (55) | <0.0001 |
| Adjuvant therapy | 48% (792) | 73% (309) | <0.0001 |
| Follow-up, months | 27 [7–60] | 28 [9–61] | 0.948 |
| Death | 12% (198) | 22% (93) | <0.0001 |
| Cancer-specific death | 8% (132) | 22% (93) | <0.0001 |
| Recurrence or progression | 21% (346) | 40% (169) | <0.0001 |
| Univariable Analysis | Multivariable Analysis | |||||
|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | p | HR | 95% CI | p |
| Age of onset (vs. LOCRC) | 1.89 | 1.72–2.75 | <0.0001 | 1.35 | 1.09–1.67 | 0.006 |
| Gender (vs. males) | 0.89 | 0.74–1.07 | 0.218 | -- | -- | -- |
| Obesity (BMI ≥ 30 Kg/m2) | 1.07 | 0.85–1.36 | 0.545 | -- | -- | -- |
| Smoking (vs. non-smokers) | 0.505 | -- | -- | -- | ||
| Current smokers | 1.04 | 0.81–1.33 | 0.779 | -- | -- | -- |
| Ex-smokers | 1.14 | 0.92–1.41 | 0.242 | -- | -- | -- |
| Tumor location (vs. right colon) | 0.146 | -- | -- | -- | ||
| Left colon | 1.10 | 0.86–1.41 | 0.448 | -- | -- | -- |
| Rectum | 0.89 | 0.71–1.11 | 0.294 | -- | -- | -- |
| Synchronous tumors | 1.40 | 0.87–2.24 | 0.163 | -- | -- | -- |
| Family history of CRC | 0.84 | 0.66–1.06 | 0.134 | -- | -- | -- |
| Preoperative radio/chemotherapy | 1.58 | 1.31–1.90 | <0.0001 | 1.34 | 1.09–1.63 | 0.005 |
| Surgery on CRC and metastases | 0.21 | 0.16–0.27 | <0.0001 | 0.87 | 0.65–1.16 | 0.337 |
| Postoperative reoperation | 0.98 | 0.66–1.45 | 0.925 | -- | -- | -- |
| Pathological stage AJCC 8th (vs. stage 0) | <0.0001 | <0.0001 | ||||
| Stage I | 2.21 | 0.68–7.16 | 0.187 | 2.82 | 0.86–9.27 | 0.087 |
| Stage II | 4.73 | 1.49–15.00 | 0.008 | 4.91 | 1.53–15.75 | 0.007 |
| Stage III | 9.69 | 3.08–30.42 | <0.0001 | 8.21 | 2.57–26.17 | <0.0001 |
| Stage IV | 31.97 | 10.23–99.96 | <0.0001 | 20.36 | 6.29–64.83 | <0.0001 |
| Mucinous tumors | 1.39 | 1.11–1.76 | 0.005 | 1.11 | 0.87–1.41 | 0.409 |
| Signet-ring cells phenotype | 2.58 | 1.48–4.47 | 0.001 | 2.24 | 1.26–3.98 | 0.006 |
| Extramural invasion | 2.64 | 2.19–3.18 | <0.0001 | 1.41 | 1.14–1.74 | 0.001 |
| Lymphovascular invasion | 2.68 | 2.24–3.21 | <0.0001 | 1.31 | 1.06–1.62 | 0.013 |
| Perineural invasion | 3.29 | 2.66–4.03 | <0.0001 | 1.44 | 1.14–1.81 | 0.002 |
| Univariable Analysis | Multivariable Analysis | |||||
|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | p | HR | 95% CI | p |
| Age of onset (vs. LOCRC) | 2.68 | 1.07–6.72 | 0.035 | 2.49 | 1.19–5.23 | 0.016 |
| Gender (vs. males) | 0.52 | 0.25–1.07 | 0.079 | -- | -- | -- |
| Obesity (BMI ≥ 30 Kg/m2) | 0.91 | 0.38–2.18 | 0.828 | -- | -- | -- |
| Smoking (vs. non-smokers) | 0.246 | -- | -- | -- | ||
| Current smokers | 1.23 | 0.49–3.08 | 0.656 | -- | -- | -- |
| Ex-smokers | 1.87 | 0.89–3.91 | 0.094 | -- | -- | -- |
| Tumor location (vs. right colon) | 0.452 | -- | -- | -- | ||
| Left colon | 0.54 | 0.18–1.65 | 0.277 | -- | -- | -- |
| Rectum | 0.98 | 0.44–2.19 | 0.964 | -- | -- | -- |
| Synchronous tumors | 3.08 | 0.74–12.88 | 0.123 | -- | -- | -- |
| Family history of CRC | 0.32 | 0.10–1.06 | 0.063 | -- | -- | -- |
| Postoperative reoperation | 0.62 | 0.13–3.00 | 0.551 | -- | -- | -- |
| Mucinous tumors | 0.84 | 0.26–2.74 | 0.775 | -- | -- | -- |
| Extramural invasion | 3.17 | 0.96–10.46 | 0.057 | -- | -- | -- |
| Lymphovascular invasion | 1.10 | 0.39–3.12 | 0.852 | -- | -- | -- |
| Perineural invasion | 3.01 | 0.41–22.08 | 0.277 | -- | -- | -- |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foppa, C.; Maroli, A.; Lauricella, S.; Luberto, A.; La Raja, C.; Bunino, F.; Carvello, M.; Sacchi, M.; De Lucia, F.; Clerico, G.; et al. Different Oncologic Outcomes in Early-Onset and Late-Onset Sporadic Colorectal Cancer: A Regression Analysis on 2073 Patients. Cancers 2022, 14, 6239. https://doi.org/10.3390/cancers14246239
Foppa C, Maroli A, Lauricella S, Luberto A, La Raja C, Bunino F, Carvello M, Sacchi M, De Lucia F, Clerico G, et al. Different Oncologic Outcomes in Early-Onset and Late-Onset Sporadic Colorectal Cancer: A Regression Analysis on 2073 Patients. Cancers. 2022; 14(24):6239. https://doi.org/10.3390/cancers14246239
Chicago/Turabian StyleFoppa, Caterina, Annalisa Maroli, Sara Lauricella, Antonio Luberto, Carlotta La Raja, Francesca Bunino, Michele Carvello, Matteo Sacchi, Francesca De Lucia, Giuseppe Clerico, and et al. 2022. "Different Oncologic Outcomes in Early-Onset and Late-Onset Sporadic Colorectal Cancer: A Regression Analysis on 2073 Patients" Cancers 14, no. 24: 6239. https://doi.org/10.3390/cancers14246239
APA StyleFoppa, C., Maroli, A., Lauricella, S., Luberto, A., La Raja, C., Bunino, F., Carvello, M., Sacchi, M., De Lucia, F., Clerico, G., Montorsi, M., & Spinelli, A. (2022). Different Oncologic Outcomes in Early-Onset and Late-Onset Sporadic Colorectal Cancer: A Regression Analysis on 2073 Patients. Cancers, 14(24), 6239. https://doi.org/10.3390/cancers14246239






