Selection Criteria and Treatment Outcome for Advanced Non-Small Cell Lung Cancer (NSCLC) Patients Unfit for Platinum-Based First-Line Therapy: Results of the MOON-OSS Observational Trial
Simple Summary
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Population
2.2. Endpoints and Assessment
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
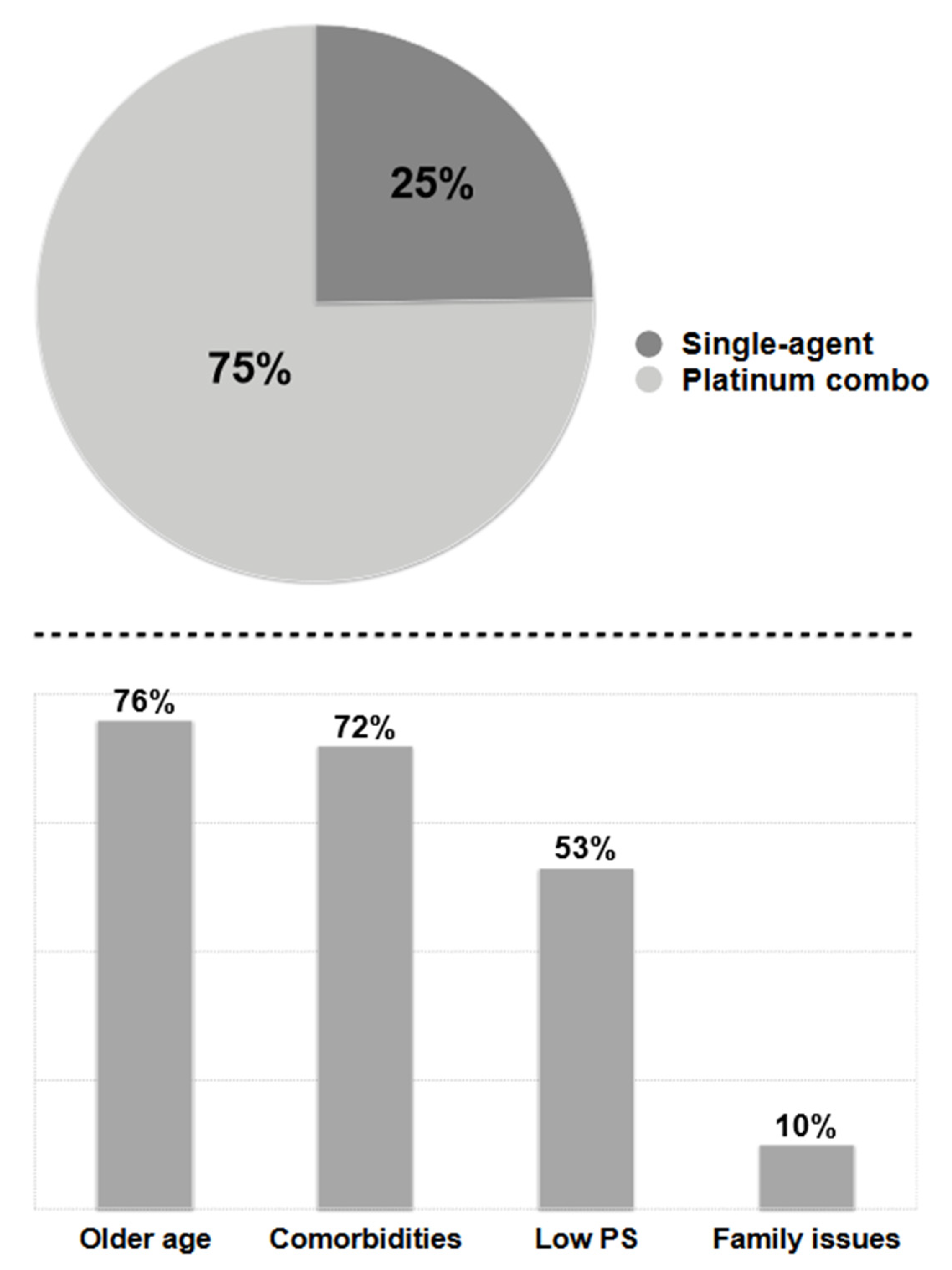
3.2. Selection Criteria, Treatment Disposition and Outcome
3.3. Safety
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- IARC. Globocan 2018. 2018. Available online: http://gco.iarc.fr/ (accessed on 7 June 2019).
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Weir, H.K.; Thun, M.J.; Hankey, B.F.; Ries, L.A.; Howe, H.L.; Wingo, P.A.; Jemal, A.; Ward, E.; Anderson, R.N.; Edwards, B.K. Annual report to the nation on the status of cancer, 1975–2000, featuring the uses of surveillance data for cancer prevention and control. J. Natl. Cancer Inst. 2003, 95, 1276–1299, Erratum in J. Natl. Cancer Inst. 2003, 95, 1641. [Google Scholar] [CrossRef] [PubMed]
- Howlader, N.; Noone, A.M.; Krapcho, M.; Garshell, J.; Neyman, N.; Altekruse, S.F.; Kosary, C.L.; Yu, M.; Ruhl, J.; Tatalovich, Z.; et al. (Eds.) SEER Cancer Statistics Review, 1975–2010; National Cancer Institute: Bethesda, MD, USA, 2013. Available online: https://seer.cancer.gov/archive/csr/1975_2010/ (accessed on 6 December 2022).
- Planchard, D.; Popat, S.; Kerr, K.; Novello, S.; Smit, E.F.; Faivre-Finn, C.; Mok, T.S.; Reck, M.; Van Schil, P.E.; Hellmann, M.D.; et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2018, 29 (Suppl. 4), iv192–iv237. Available online: https://www.esmo.org/guidelines/lung-and-chest-tumours/clinical-practice-living-guidelines-metastatic-non-small-cell-lung-cancer (accessed on 1 June 2020). [CrossRef] [PubMed]
- De Giglio, A.; Nuvola, G.; Baldini, C. Clinical consideration for choosing combination therapies in advanced non-small-cell lung cancer: Age, Eastern Cooperative Organization performance status 2, steroids and antibiotics. Future Oncol. 2020, 16, 1683–1690. [Google Scholar] [CrossRef] [PubMed]
- Friedlaender, A.; Banna, G.L.; Buffoni, L.; Addeo, A. Poor-performance status assessment of patients with non-small cell lung cancer remains vague and blurred in the immunotherapy era. Curr. Oncol. Rep. 2019, 21, 107. [Google Scholar] [CrossRef]
- De Marinis, F.; Bria, E.; Baas, P.; Tiseo, M.; Camerini, A.; Favaretto, A.G.; Gridelli, C. Treatment of unfit patients with advanced non-small-cell lung cancer: Definition criteria according an expert panel. Clin. Lung Cancer 2015, 16, 399–405. [Google Scholar] [CrossRef]
- Corre, R.; Greillier, L.; Le Caër, H.; Audigier-Valette, C.; Baize, N.; Bérard, H.; Falchero, L.; Monnet, I.; Dansin, E.; Vergnenègre, A.; et al. Use of a Comprehensive Geriatric Assessment for the Management of Elderly Patients With Advanced Non-Small-Cell Lung Cancer: The Phase III Randomized ESOGIA-GFPC-GECP 08-02 Study. J. Clin. Oncol. 2016, 34, 1476–1483. [Google Scholar] [CrossRef]
- Radzikowska, E.; Głaz, P.; Roszkowski, K. Lung cancer in women: Age, smoking, histology, performance status, stage, initial treatment and survival. Population-based study of 20561 cases. Ann. Oncol. 2002, 13, 1087–1093. [Google Scholar] [CrossRef]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2016, 375, 1823–1833. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0; National Institutes of Health National Cancer Institute: Bethesda, MD, USA, 2010; 28 May 2009 (v4.03: 14 June 2010).
- Seto, Y.; Kaneko, Y.; Mouri, T.; Fujii, H.; Tanaka, S.; Shiotsu, S.; Hiranuma, O.; Morimoto, Y.; Iwasaku, M.; Yamada, T.; et al. Prognostic factors in older patients with wild-type epidermal growth factor receptor advanced non-small cell lung cancer: A multicenter retrospective study. Transl. Lung Cancer Res. 2021, 10, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Kitazawa, H.; Takeda, Y.; Naka, G.; Sugiyama, H. Decision-making factors for best supportive care alone and prognostic factors after best supportive care in non-small cell lung cancer patients. Sci. Rep. 2019, 9, 19872. [Google Scholar] [CrossRef] [PubMed]
- Sacher, A.G.; Le, L.W.; Lau, A.; Earle, C.C.; Leighl, N.B. Real-world chemotherapy treatment patterns in metastatic non-small cell lung cancer: Are patients undertreated? Cancer 2015, 121, 2562–2569. [Google Scholar] [CrossRef] [PubMed]
- Ganti, A.K.; Wang, X.; Stinchcombe, T.E.; Wang, Y.; Bradley, J.; Cohen, H.J.; Kelly, K.; Paulus, R.; Ramalingam, S.S.; Vokes, E.E.; et al. Clinical prognostic model for older patients with advanced non-small cell lung cancer. J. Geriatr. Oncol. 2019, 10, 555–559. [Google Scholar] [CrossRef]
- Cacicedo, J.; Casquero, F.; Navarro, A.; Martinez-Indart, L.; Del Hoyo, O.; Frías, A.; de Zarate, R.O.; Büchser, D.; Gómez-Iturriaga, A.; San Miguel, I.; et al. Prospective multicentre analysis of the therapeutic approach and prognostic factors determining overall survival in elderly patients with non-small-cell lung carcinoma treated with curative intent. BJR Open 2022, 4, 20210058. [Google Scholar] [CrossRef]
- Mathur, S.; Prince, L.; Bucher, O.; Xue, L.; Banerji, S.; Dawe, D.E. The impact of the modified frailty index on clinical outcomes for patients with stage IV non-small cell lung cancer receiving chemotherapy. J. Geriatr. Oncol. 2022, 13, 654–661. [Google Scholar] [CrossRef]
- Noda-Narita, S.; Kawachi, A.; Okuyama, A.; Sadachi, R.; Hirakawa, A.; Goto, Y.; Fujiwara, Y.; Higashi, T.; Yonemori, K. First-line treatment for lung cancer among Japanese older patients: A real-world analysis of hospital-based cancer registry data. PLoS ONE 2021, 16, e0257489. [Google Scholar] [CrossRef]
- Camerini, A.; Puccetti, C.; Donati, S.; Valsuani, C.; Petrella, M.C.; Tartarelli, G.; Puccinelli, P.; Amoroso, D. Metronomic oral vinorelbine as first-line treatment in elderly patients with advanced non-small cell lung cancer: Results of a phase II trial (MOVE trial). BMC Cancer 2015, 15, 359. [Google Scholar] [CrossRef]
- Camerini, A.; Banna, G.L.; Cinieri, S.; Pezzuto, A.; Mencoboni, M.; Rosetti, F.; Figueiredo, A.; Rizzo, P.; Ricci, A.; Langenhoven, L.; et al. Metronomic oral vinorelbine for the treatment of advanced non-small cell lung cancer: A multicenter international retrospective analysis. Clin. Transl. Oncol. 2019, 21, 790–795. [Google Scholar] [CrossRef]
- Camerini, A.; Morabito, A.; Montanino, A.; Bernabé, R.; Grossi, F.; Ramlau, R.; Ciuleanu, T.E.; Ceresoli, G.L.; Pasello, G.; de Marinis, F.; et al. Metronomic oral vinorelbine in previously untreated advanced non-small-cell lung cancer patients unfit for platinum-based chemotherapy: Results of the randomized phase II Tempo Lung trial. ESMO Open 2021, 6, 100051. [Google Scholar] [CrossRef]
- Lee, S.M.; Schulz, C.; Prabhash, K.; Han, B.; Szczesna, A.; Cortinovis, D.L.; Rittmeyer, A.; Vicente Baz, D.; Califano, R.; Tuan Anh, L.; et al. IPSOS: Results from a phase III study of first-line atezolizumab vs single-agent chemotherapy in patients with NSCLC not eligible for a platinum-containing regimen. Ann. Oncol. 2022, 33 (Suppl. 7), S808–S869. [Google Scholar] [CrossRef]
- Lena, H.; Monnet, I.; Bylicki, O.; Audigier-Valette, C.; Falchero, L.; Vergnenegre, A.; Demontrond, P.; Greillier, L.; Geier, M.; Guisier, F.; et al. Randomized phase III study of nivolumab and ipilimumab versus carboplatin-based doublet in first-line treatment of PS 2 or elderly (≥70 years) patients with advanced non–small cell lung cancer (Energy-GFPC 06-2015 study). J. Clin. Oncol. 2022, 40, 9011. [Google Scholar] [CrossRef]
- Paz-Ares, L.; Luft, A.; Vicente, D.; Tafreshi, A.; Gümüş, M.; Mazières, J.; Hermes, B.; Çay Şenler, F.; Csőszi, T.; Fülöp, A.; et al. Pembrolizumab plus Chemotherapy for Squamous Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 379, 2040–2051. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, L.; Rodríguez-Abreu, D.; Gadgeel, S.; Esteban, E.; Felip, E.; De Angelis, F.; Domine, M.; Clingan, P.; Hochmair, M.J.; Powell, S.F.; et al. embrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 2078–2092. [Google Scholar] [CrossRef]
- Yang, Z.; Chen, Y.; Wang, Y.; Hu, M.; Qian, F.; Zhang, Y.; Zhang, B.; Zhang, W.; Han, B. Pembrolizumab Plus Chemotherapy Versus Chemotherapy Monotherapy as a First-Line Treatment in Elderly Patients (≥75 Years Old) with Non-Small-Cell Lung Cancer. Front. Immunol. 2022, 13, 807575. [Google Scholar] [CrossRef]
- Vergnenegre, A.; Monnet, I.; Bizieux, A.; Bernardi, M.; Chiapa, A.M.; Léna, H.; Chouaïd, C.; Robinet, G. Open-label Phase II trial to evaluate safety and efficacy of second-line metronomic oral vinorelbine-atezolizumab combination for stage-IV non-small-cell lung cancer—VinMetAtezo trial, (GFPC‡ 04-2017). Future Oncol. 2020, 16, 5–10. [Google Scholar] [CrossRef]
- Barlesi, F.; Deyme, L.; Imbs, D.C.; Cousin, E.; Barbolosi, M.; Bonnet, S.; Tomasini, P.; Greillier, L.; Galloux, M.; Testot-Ferry, A.; et al. Revisiting metronomic vinorelbine with mathematical modelling: A Phase I trial in lung cancer. Cancer Chemother. Pharmacol. 2022, 90, 149–160. [Google Scholar] [CrossRef]
- Elharrar, X.; Barbolosi, D.; Ciccolini, J.; Meille, C.; Faivre, C.; Lacarelle, B.; André, N.; Barlesi, F. A phase Ia/Ib clinical trial of metronomic chemotherapy based on a mathematical model of oral vinorelbine in metastatic non-small cell lung cancer and malignant pleural mesothelioma: Rationale and study protocol. BMC Cancer 2016, 16, 278. [Google Scholar] [CrossRef]
| Characteristics (Total n = 221) | n (%) |
|---|---|
| Age median (range) | 79 (56–92) years |
| Sex | |
| Female | 56 (25.5%) |
| Male | 165 (74.5%) |
| Smoker status | |
| Current smokers | 60 (27.1%) |
| Former smokers | 128 (62.5%) |
| Never smokers | 33 (10.4%) |
| Disease stage | |
| IIIB | 62 (28.1%) |
| IV | 159 (71.9%) |
| ECOG PS | |
| 0 | 23 (10.9%) |
| 1 | 94 (42.5%) |
| ≥2 | 103 (46.6%) |
| Histology | |
| Adenocarcinoma | 107 (48.4%) |
| Squamous cell carcinoma | 94 (42.5%) |
| Large-cell carcinoma | 9 (4.1%) |
| NOS carcinoma | 11 (5%) |
| Comorbid illnesses median (range) | 2 (0–6) |
| Comorbid illnesses * | |
| Hypertension | 166 (75.1%) |
| COPD | 141 (63.8%) |
| Heart disease | 120 (54.3%) |
| Cerebral or peripheral vascular disease | 95 (43%) |
| Diabetes | 66 (29.9%) |
| Chronic renal failure | 52 (23.5%) |
| Hepatitis and/or cirrhosis | 24 (10.9%) |
| Severe auto-immune disorders | 15 (6.8%) |
| Disease sites median (range) | 3 (1–5) |
| Disease sites * | |
| Lung ° | 138 (62.4%) |
| Lymph nodes | 112 (50.7%) |
| Pleura | 108 (48.9%) |
| Bone | 95 (43%) |
| Adrenal | 88 (39.8%) |
| Liver | 35 (15.8%) |
| Brain | 22 (9.9%) |
| Other | 15 (6.8%) |
| Single-agent treatment | |
| Gemcitabine | 22 (10%) |
| Oral standard vinorelbine | 18 (8.2%) |
| Metronomic vinorelbine | 174 (78.6%) |
| Others * | 7 (3.2%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camerini, A.; Del Conte, A.; Pezzuto, A.; Scotti, V.; Facchinetti, F.; Ciccone, L.P.; Perna, M.; Sartori, G.; Puccetti, C.; Ricci, A.; et al. Selection Criteria and Treatment Outcome for Advanced Non-Small Cell Lung Cancer (NSCLC) Patients Unfit for Platinum-Based First-Line Therapy: Results of the MOON-OSS Observational Trial. Cancers 2022, 14, 6074. https://doi.org/10.3390/cancers14246074
Camerini A, Del Conte A, Pezzuto A, Scotti V, Facchinetti F, Ciccone LP, Perna M, Sartori G, Puccetti C, Ricci A, et al. Selection Criteria and Treatment Outcome for Advanced Non-Small Cell Lung Cancer (NSCLC) Patients Unfit for Platinum-Based First-Line Therapy: Results of the MOON-OSS Observational Trial. Cancers. 2022; 14(24):6074. https://doi.org/10.3390/cancers14246074
Chicago/Turabian StyleCamerini, Andrea, Alessandro Del Conte, Aldo Pezzuto, Vieri Scotti, Francesco Facchinetti, Lucia Pia Ciccone, Marco Perna, Giulia Sartori, Cheti Puccetti, Alberto Ricci, and et al. 2022. "Selection Criteria and Treatment Outcome for Advanced Non-Small Cell Lung Cancer (NSCLC) Patients Unfit for Platinum-Based First-Line Therapy: Results of the MOON-OSS Observational Trial" Cancers 14, no. 24: 6074. https://doi.org/10.3390/cancers14246074
APA StyleCamerini, A., Del Conte, A., Pezzuto, A., Scotti, V., Facchinetti, F., Ciccone, L. P., Perna, M., Sartori, G., Puccetti, C., Ricci, A., Santo, A., Tiseo, M., & Amoroso, D. (2022). Selection Criteria and Treatment Outcome for Advanced Non-Small Cell Lung Cancer (NSCLC) Patients Unfit for Platinum-Based First-Line Therapy: Results of the MOON-OSS Observational Trial. Cancers, 14(24), 6074. https://doi.org/10.3390/cancers14246074







