How Timely Is Diagnosis of Lung Cancer? Cohort Study of Individuals with Lung Cancer Presenting in Ambulatory Care in the United States
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection
2.4. Sociodemographic Variables & Comorbidity
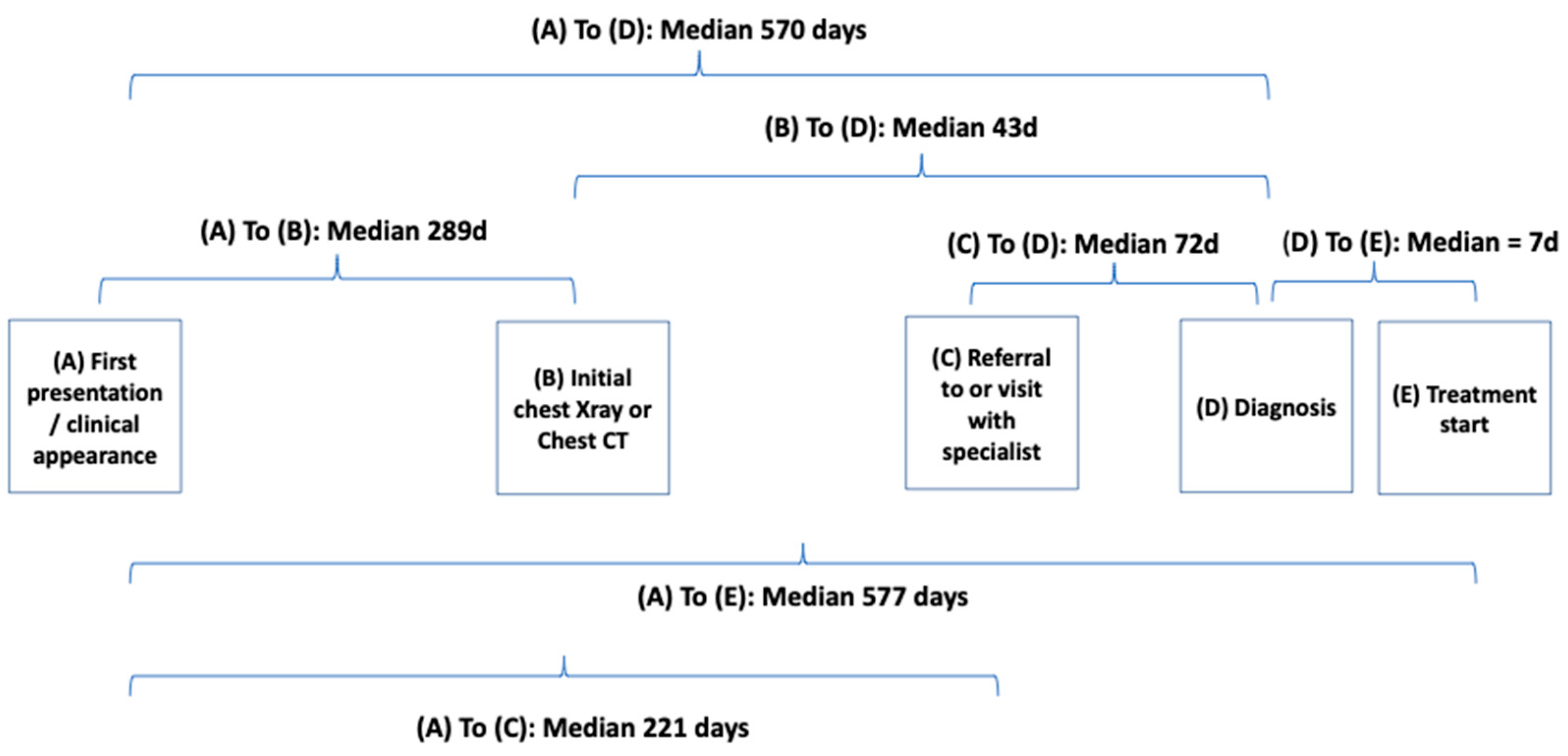
2.5. Time Point Definitions
2.6. Lung Cancer Histology and Stage
2.7. Data Analysis
3. Results
3.1. Selection of Cohort
3.2. Description of the Cohort
3.3. Symptoms and Signs Prior to Diagnosis
3.4. Impact of Definition of Initial Symptomatic Presentation on Time to Diagnosis
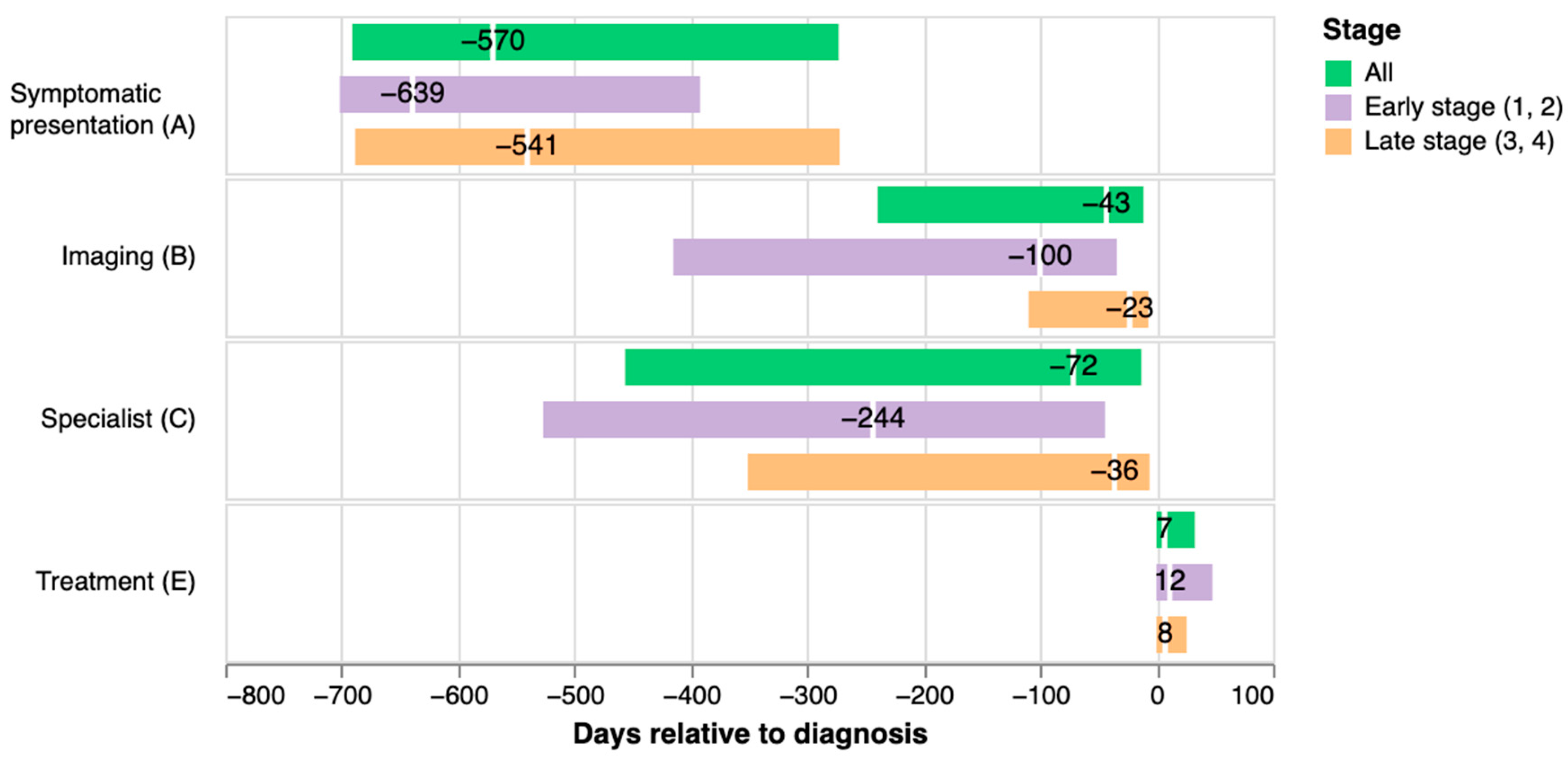
3.5. Duration of Illness and Length of Key Time Intervals Prior to Diagnosis
4. Discussion
4.1. Summary
4.2. Comparison to Current Literature
4.3. Strengths and Limitations
4.4. Study Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| (A) Date of first symptomatic presentation | Date of first in-person clinical encounter in the 24 months prior to the diagnosis date where at least one symptom or sign previously associated with lung cancer was recorded. Patients with no recorded signs or symptoms prior to their diagnosis date were considered asymptomatic and did not have a date of first symptomatic presentation designated. |
| (B) Date of referral to or date of receipt of initial chest imaging procedure (chest X-ray or chest CT) | Earliest of either the date of first referral for, or date of receipt of chest imaging (i.e., chest X-ray or chest CT), following initial symptomatic presentation with a linked reason for referral related to suspicion of lung cancer and occurring within 14 days after date of diagnosis (to account for delays of documentation or billing). |
| (C) Date of referral to or encounter with lung cancer specialist | Earliest date of either first referral to, or encounter with a specialty care department (including Ambulatory Surgery, General Surgery, Hematology, Hematology and Oncology, Interventional Radiology, Medical Oncology, Neuro Oncology, Oncology, Palliative Care, Pulmonary Diagnostic Testing, Pulmonary Medicine, Radiation Oncology, Radiation Therapy, Respiratory Disease, Sarcoma, Special Procedures, Surgery, Thoracic, Thoracic Medicine, Thoracic Surgery) for a lung related ICD diagnostic code (lung cancer diagnosis, lung cancer symptoms, lung related diagnoses, abnormal imaging, other diagnoses that may present with lung cancer symptoms) in the two years prior to diagnosis and the 14 days after diagnosis (to account for delay in recording in the medical record). |
| (D) Date of diagnosis | Date of first pathology report that provided pathologic confirmation of lung cancer closest to the first recorded lung cancer diagnosis code. If there was no pathologic confirmation or was >30-day difference between pathologic date and first recorded lung cancer diagnosis code then a manual chart review was conducted to confirm the date of diagnosis. |
| (E) Date of first treatment | Date of initiation of the first course of any medical or surgical treatment identified from SEER. |
Appendix B
| Patient Characteristics | All (n = 711) n (%) | Small Cell Lung Cancer (n = 63) n (%) | Non-Small Cell Lung Cancer (n = 556) n (%) | Other (n = 44) n (%) |
|---|---|---|---|---|
| Age (years) | ||||
| 18–49 | 36 (5.1) | 4 (6.3) | 25 (4.5) | 4 (9.1) |
| 50–59 | 129 (18.1) | 16 (25.4) | 96 (17.3) | 3 (6.8) |
| 60–69 | 261 (36.7) | 21 (33.3) | 212 (38.1) | 10 (22.7) |
| 70–79 | 185 (26.0) | 11 (17.5) | 152 (27.3) | 13 (29.5) |
| 80+ | 100 (14.1) | 11 (17.5) | 71 (12.8) | 14 (31.8) |
| Sex | ||||
| Male | 355 (49.9) | 37 (58.7) | 277 (49.8) | 20 (45.5) |
| Race/Ethnicity | ||||
| Asian or Pacific Islander | 80 (11.3) | 2 (3.2) | 69 (12.4) | 4 (9.1) |
| Hispanic or Latino | 23 (3.2) | 2 (3.2) | 18 (3.2) | 1 (2.3) |
| Non-Hispanic Black | 58 (8.2) | 0 (0.0) | 52 (9.4) | 5 (11.4) |
| Non-Hispanic White | 492 (69.2) | 52 (82.5) | 377 (67.8) | 28 (63.6) |
| Other | 58 (8.2) | 7 (11.1) | 40 (7.2) | 6 (13.6) |
| Smoking status | ||||
| Ever smoker | 531 (74.7) | 58 (92.1) | 410 (73.7) | 34 (77.3) |
| Never smoker | 122 (17.2) | 0 (0.0) | 109 (19.6) | 8 (18.2) |
| Unknown | 58 (8.2) | 5 (7.9) | 37 (6.7) | 2 (4.5) |
| Insurance | ||||
| Medicaid | 117 (16.5) | 19 (26.8) | 90 (15.4) | 8 (14.5) |
| Medicare | 437 (61.5) | 40 (56.3) | 365 (62.4) | 32 (58.2) |
| Military | 13 (1.8) | 1 (1.4) | 12 (0.1) | 0 (0.0) |
| Not Insured | 7 (1.0) | 0 (0.0) | 6 (1.0) | 1 (1.8) |
| Private | 130 (18.3) | 11 (15.5) | 108 (18.5) | 11 (20.0) |
| Unknown | 7 (1.0) | 0 (0.0) | 4 (0.7) | 3 (5.5) |
| Census Tract Poverty Indicator | ||||
| 0–10% poverty | 383 (53.9) | 36 (57.1) | 299 (53.8) | 21 (47.7) |
| 10–20% poverty | 222 (31.2) | 15 (23.8) | 177 (31.8) | 13 (29.5) |
| ≥20% poverty | 106 (14.9) | 12 (19.0) | 80 (14.4) | 10 (22.7) |
| Comorbidity—Elixhauser van Walraven Weighted Score ** mean (SD) | 17.36 (11.8) | 22.40 (11.98) | 16.92 (11.68) | 16.59 (11.30) |
Appendix C
| All (n = 711) | Early Stage (n = 238) | Late Stage (n = 385) | p Value | ||
|---|---|---|---|---|---|
| Age (years) | 18–49 | 36 (5.1%) | 9 (3.8%) | 23 (6.0%) | 0.5478 |
| 50–59 | 129 (18.1%) | 37 (15.5%) | 72 (18.7%) | ||
| 60–69 | 261 (36.7%) | 90 (37.8%) | 141 (36.6%) | ||
| 70–79 | 185 (26.0%) | 66 (27.7%) | 100 (26.0%) | ||
| 80+ | 100 (14.1%) | 36 (15.1%) | 49 (12.7%) | ||
| Sex | Female | 356 (50.1%) | 136 (57.1%) | 179 (46.5%) | 0.0124 |
| Male | 355 (49.9%) | 102 (42.9%) | 206 (53.5%) | ||
| Race/Ethnicity | Asian or Pacific Islander | 80 (11.3%) | 25 (10.5%) | 44 (11.4%) | 0.9514 |
| Hispanic or Latino | 23 (3.2%) | 9 (3.8%) | 12 (3.1%) | ||
| Non-Hispanic Black | 68 (9.6%) | 26 (10.9%) | 39 (10.1%) | ||
| Non-Hispanic White | 524 (73.7%) | 174 (73.1%) | 281 (73.0%) | ||
| Other | 16 (2.3%) | 4 (1.7%) | 9 (2.3%) | ||
| Smoking status | Current or former | 531 (74.7%) | 191 (80.3%) | 278 (72.2%) | 0.0015 |
| Never | 122 (17.2%) | 42 (17.6%) | 71 (18.4%) | ||
| No data | 58 (8.2%) | 5 (2.1%) | 36 (9.4%) | ||
| Insurance | No insurance or Unknown | 14 (2.0%) | 2 (0.8%) | 9 (2.3%) | 0.2257 |
| Private Insurance | 130 (18.3%) | 38 (16.0%) | 73 (19.0%) | ||
| Public Insurance | 567 (79.7%) | 198 (83.2%) | 303 (78.7%) | ||
| Census Tract Poverty Indicator | 0–<10% poverty | 383 (53.9%) | 129 (54.2%) | 207 (53.8%) | 0.5021 |
| 10–<20% poverty | 222 (31.2%) | 68 (28.6%) | 123 (31.9%) | ||
| ≥20–100% poverty | 106 (14.9%) | 41 (17.2%) | 55 (14.3%) | ||
| Comorbidity—Elixhauser van Walraven Weighted Score | Mean (SD) | 17.4 (11.8) | 13.9 (10.2) | 19.8 (12.2) | <0.0001 |
Appendix D
| All Patients (n = 711) | Early and Late Stages (n = 623) | Early Stage (n = 238) | Late Stage (n = 385) | p-Value | |
|---|---|---|---|---|---|
| Cough | 573 (80.59%) | 504 (80.90%) | 209 (87.82%) | 295 (76.62%) | 0.0008 |
| Shortness of breath | 515 (72.43%) | 450 (72.23%) | 184 (77.31%) | 266 (69.09%) | 0.0329 |
| Fatigue | 476 (66.95%) | 418 (67.09%) | 161 (67.65%) | 257 (66.75%) | 0.8863 |
| Chest Pain | 403 (56.68%) | 360 (57.78%) | 145 (60.92%) | 215 (55.84%) | 0.2444 |
| Chest crackles or wheeze | 397 (55.84%) | 344 (55.22%) | 148 (62.18%) | 196 (50.91%) | 0.0077 |
| Back pain | 350 (49.23%) | 306 (49.12%) | 125 (52.52%) | 181 (47.01%) | 0.2099 |
| Weight loss | 308 (43.32%) | 269 (43.18%) | 108 (45.38%) | 161 (41.82%) | 0.4305 |
| Bone pain | 270 (37.97%) | 245 (39.33%) | 114 (47.90%) | 131 (34.03%) | 0.0008 |
| Lymphadenopathy | 151 (21.24%) | 133 (21.35%) | 28 (11.76%) | 105 (27.27%) | 0.0000 |
| Hemoptysis | 118 (16.60%) | 97 (15.57%) | 43 (18.07%) | 54 (14.03%) | 0.2157 |
| Finger clubbing | 39 (5.49%) | 33 (5.30%) | 17 (7.14%) | 16 (4.16%) | 0.1518 |
Appendix E
| All Patients (n = 711) | NSCLC and SCLC (n = 609) | NSLCL (n = 546) | SCLC (n = 63) | p-Value | |
|---|---|---|---|---|---|
| Cough | 573 (80.59%) | 505 (82.9%) | 450 (82.4%) | 55 (87.3%) | 0.4245 |
| Shortness of breath | 515 (72.43%) | 445 (73.1%) | 398 (72.9%) | 47 (74.6%) | 0.8889 |
| Fatigue | 476 (66.95%) | 412 (67.7%) | 368 (67.4%) | 44 (69.8%) | 0.8025 |
| Chest Pain | 403 (56.68%) | 356 (58.5%) | 316 (57.9%) | 40 (63.5%) | 0.4706 |
| Chest crackles or wheeze | 397 (55.84%) | 342 (56.2%) | 302 (55.3%) | 40 (63.5%) | 0.2692 |
| Back pain | 350 (49.23%) | 301 (49.4%) | 271 (49.6%) | 30 (47.6%) | 0.8652 |
| Weight loss | 308 (43.32%) | 260 (42.7%) | 237 (43.4%) | 23 (36.5%) | 0.3609 |
| Bone pain | 270 (37.97%) | 244 (40.1%) | 222 (40.7%) | 22 (34.9%) | 0.4567 |
| Lymphadenopathy | 151 (21.24%) | 131 (21.5%) | 110 (20.1%) | 21 (33.3%) | 0.0244 |
| Hemoptysis | 118 (16.60%) | 98 (16.1%) | 88 (16.1%) | 10 (15.9%) | 1.0000 |
| Finger clubbing | 39 (5.49%) | 33 (5.4%) | 32 (5.9%) | 1 (1.6%) | 0.2607 |
References
- American Cancer Society. Lung Cancer Survival Rates. Available online: https://www.cancer.org/cancer/lung-cancer/detection-diagnosis-staging/survival-rates.html (accessed on 11 May 2022).
- Moyer, V.A. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2014, 160, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Wood, D.E.; Eapen, G.A.; Ettinger, D.S.; Hou, L.; Jackman, D.; Kazerooni, E.; Klippenstein, D.; Lackner, R.P.; Leard, L.; Leung, A.N.; et al. Lung cancer screening. Natl. Compr. Cancer Netw. 2012, 10, 240–265. [Google Scholar] [CrossRef]
- Fedewa, S.A.; Bandi, P.; Smith, R.A.; Silvestri, G.A.; Jemal, A. Lung Cancer Screening Rates During the COVID-19 Pandemic. Chest 2021, 161, 586–589. [Google Scholar] [CrossRef]
- Sarma, E.A.; Kobrin, S.C.; Thompson, M.J. A Proposal to Improve the Early Diagnosis of Symptomatic Cancers in the United States. Cancer Prev. Res. 2020, 13, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, W.; Peters, T.J.; Round, A.; Sharp, D. What are the clinical features of lung cancer before the diagnosis is made? A population based case-control study. Thorax 2005, 60, 1059–1065. [Google Scholar] [CrossRef]
- Lyratzopoulos, G.; Wardle, J.; Rubin, G. Rethinking diagnostic delay in cancer: How difficult is the diagnosis? BMJ 2014, 349, g7400. [Google Scholar] [CrossRef] [PubMed]
- Walter, F.M.; Rubin, G.; Bankhead, C.; Morris, H.C.; Hall, N.; Mills, K.; Dobson, C.; Rintoul, R.C.; Hamilton, W.; Emery, J. Symptoms and other factors associated with time to diagnosis and stage of lung cancer: A prospective cohort study. Br. J. Cancer 2015, 112, S6–S13. [Google Scholar] [CrossRef]
- Nadpara, P.A.; Madhavan, S.S.; Tworek, C.; Sambamoorthi, U.; Hendryx, M.; Almubarak, M. Guideline-concordant lung cancer care and associated health outcomes among elderly patients in the United States. J. Geriatr. Oncol. 2015, 6, 101–110. [Google Scholar] [CrossRef]
- Myers, L.C.; Skillings, J.; Heard, L.; Metlay, J.P.; Mort, E. Medical Malpractice Involving Pulmonary/Critical Care Physicians. Chest 2019, 156, 907–914. [Google Scholar] [CrossRef]
- Schacht, K.; Furst, W.; Jimbo, M.; Chavey, W.E. A Malpractice Claims Study of a Family Medicine Department: A 20-Year Review. J. Am. Board Fam. Med. 2022, 35, 380–386. [Google Scholar] [CrossRef]
- World Health Organization. Guide to Cancer Early Diagnosis; World Health Organization: Geneva, Switzerland, 2017; ISBN 978-92-4-151194-0. [Google Scholar]
- Luciani, S.; Berman, N.J. Status report. Canadian strategy for cancer control. Chronic Dis. Cent. 2000, 21, 23–25. [Google Scholar]
- Kim, J.O.A.; Davis, F.; Butts, C.; Winget, M. Waiting Time Intervals for Non-small Cell Lung Cancer Diagnosis and Treatment in Alberta: Quantification of Intervals and Identification of Risk Factors Associated with Delays. Clin. Oncol. 2016, 28, 750–759. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, E.; Green, A.; Oesterlind, K.; Rasmussen, T.R.; Iachina, M.; Palshof, T. Nationwide Quality Improvement in Lung Cancer Care: The Role of the Danish Lung Cancer Group and Registry. J. Thorac. Oncol. 2013, 8, 1238–1247. [Google Scholar] [CrossRef]
- Singh, H.; Graber, M. Reducing diagnostic error through medical home-based primary care reform. JAMA 2010, 304, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Prado, M.G.; Kessler, L.G.; Au, M.A.; Burkhardt, H.A.; Zigman Suchsland, M.; Kowalski, L.; Stephens, K.A.; Yetisgen, M.; Walter, F.M.; Neal, R.D.; et al. Symptoms and signs of lung cancer prior to diagnosis: Comparative study using electronic health records. medRxiv 2022. [Google Scholar] [CrossRef]
- National Cancer Institute Surveillance Epidemiology and End Results (SEER) Program. SEER Data Reporting Tools—Site Recode ICD-O-3 (1/27/2003) Definition. Available online: https://seer.cancer.gov/siterecode/icdo3_d01272003/ (accessed on 30 June 2021).
- Elixhauser, A.; Steiner, C.; Harris, D.R.; Coffey, R.M. Comorbidity measures for use with administrative data. Med. Care 1998, 36, 8–27. [Google Scholar] [CrossRef] [PubMed]
- van Walraven, C.; Austin, P.C.; Jennings, A.; Quan, H.; Forster, A.J. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med. Care 2009, 47, 626–633. [Google Scholar] [CrossRef] [PubMed]
- Thompson, N.R.; Fan, Y.; Dalton, J.E.; Jehi, L.; Rosenbaum, B.P.; Vadera, S.; Griffith, S.D. A New Elixhauser-based Comorbidity Summary Measure to Predict In-Hospital Mortality. Med. Care 2015, 53, 374–379. [Google Scholar] [CrossRef]
- Hansen, R.P.; Vedsted, P.; Sokolowski, I.; Søndergaard, J.; Olesen, F. Time intervals from first symptom to treatment of cancer: A cohort study of 2,212 newly diagnosed cancer patients. BMC Health Serv. Res. 2011, 11, 284. [Google Scholar] [CrossRef]
- Weller, D.; Vedsted, P.; Rubin, G.; Walter, F.M.; Emery, J.; Scott, S.; Campbell, C.; Andersen, R.S.; Hamilton, W.; Olesen, F.; et al. The Aarhus statement: Improving design and reporting of studies on early cancer diagnosis. Br. J. Cancer 2012, 106, 1262–1267. [Google Scholar] [CrossRef]
- Tørring, M.L.; Falborg, A.Z.; Jensen, H.; Neal, R.D.; Weller, D.; Reguilon, I.; ICBP Working Group; Menon, U.; Vedsted, P. Advanced-stage cancer and time to diagnosis: An International Cancer Benchmarking Partnership (ICBP) cross-sectional study. Eur. J. Cancer Care 2019, 28, e13100. [Google Scholar] [CrossRef] [PubMed]
- Lybarger, K.; Ostendorf, M.; Thompson, M.; Yetisgen, M. Extracting COVID-19 diagnoses and symptoms from clinical text: A new annotated corpus and neural event extraction framework. J. Biomed. Inform. 2021, 117, 103761. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) Program. ICD-O-3 Coding Materials. Available online: https://seer.cancer.gov/icd-o-3/ (accessed on 2 July 2021).
- Travis, W.D.; Brambilla, E.; Noguchi, M.; Nicholson, A.G.; Geisinger, K.R.; Yatabe, Y.; Beer, D.G.; Powell, C.A.; Riely, G.J.; Van Schil, P.E.; et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J. Thorac. Oncol. 2011, 6, 244–285. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M. Classification and Pathology of Lung Cancer. Surg. Oncol. Clin. N. Am. 2016, 25, 447–468. [Google Scholar] [CrossRef] [PubMed]
- American College of Surgeons. Cancer Staging Systems. Available online: https://www.facs.org/quality-programs/cancer-programs/american-joint-committee-on-cancer/cancer-staging-systems/ (accessed on 2 July 2021).
- Seabold, S.; Perktold, J. Statsmodels: Econometric and Statistical Modeling with Python. In Proceedings of the 9th Python in Science Conference, Austin, TX, USA, 28 June–3 July 2010; pp. 92–96. [Google Scholar] [CrossRef]
- Launay, E.; Cohen, J.F.; Bossuyt, P.M.; Buekens, P.; Deeks, J.; Dye, T.; Feltbower, R.; Ferrari, A.; Kramer, M.; Leeflang, M.; et al. Reporting studies on time to diagnosis: Proposal of a guideline by an international panel (REST). BMC Med. 2016, 14, 146. [Google Scholar] [CrossRef] [PubMed]
- Ellis, P.M.; Vandermeer, R. Delays in the diagnosis of lung cancer. J. Thorac. Dis. 2011, 3, 183–188. [Google Scholar] [CrossRef]
- Koyi, H.; Hillerdal, G.; Brandén, E. Patient’s and doctors’ delays in the diagnosis of chest tumors. Lung Cancer 2002, 35, 53–57. [Google Scholar] [CrossRef]
- Romine, P.E.; Sun, Q.; Fedorenko, C.; Li, L.; Tang, M.; Eaton, K.D.; Goulart, B.H.L.; Martins, R.G. Impact of Diagnostic Delays on Lung Cancer Survival Outcomes: A Population Study of the US SEER-Medicare Database. JCO Oncol. Pract. 2022, 18, e877–e885. [Google Scholar] [CrossRef]
- Walter, F.M.; Webster, A.; Scott, S.; Emery, J. The Andersen Model of Total Patient Delay: A systematic review of its application in cancer diagnosis. J. Health Serv. Res. Policy 2012, 17, 110–118. [Google Scholar] [CrossRef]
- Al Achkar, M.; Zigman Suchsland, M.; Walter, F.M.; Neal, R.D.; Goulart, B.H.L.; Thompson, M.J. Experiences along the diagnostic pathway for patients with advanced lung cancer in the USA: A qualitative study. BMJ Open 2021, 11, e045056. [Google Scholar] [CrossRef]
- Corner, J.; Hopkinson, J.; Roffe, L. Experience of health changes and reasons for delay in seeking care: A UK study of the months prior to the diagnosis of lung cancer. Soc. Sci. Med. 2006, 62, 1381–1391. [Google Scholar] [CrossRef] [PubMed]
- Corner, J.; Hopkinson, J.; Fitzsimmons, D.; Barclay, S.; Muers, M. Is late diagnosis of lung cancer inevitable? Interview study of patients’ recollections of symptoms before diagnosis. Thorax 2005, 60, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Tod, A.M.; Craven, J.; Allmark, P. Diagnostic delay in lung cancer: A qualitative study. J. Adv. Nurs. 2008, 61, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Vidaver, R.M.; Shershneva, M.B.; Hetzel, S.J.; Holden, T.R.; Campbell, T.C. Typical Time to Treatment of Patients With Lung Cancer in a Multisite, US-Based Study. J. Oncol. Pract. 2016, 12, e643–e653. [Google Scholar] [CrossRef] [PubMed]
- Gould, M.K.; Ghaus, S.J.; Olsson, J.K.; Schultz, E.M. Timeliness of care in Veterans with non-small cell lung cancer. Chest 2008, 133, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, M.M.; Silverstein, S.C.; Quinn, M.; Waterston, L.B.; Thomas, C.A.; Benneyan, J.C.; Han, P.K.J. Timeliness of access to lung cancer diagnosis and treatment: A scoping literature review. Lung Cancer 2017, 112, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Schultz, E.M.; Powell, A.A.; McMillan, A.; Olsson, J.K.; Enderle, M.A.; Graham, B.A.; Ordin, D.L.; Gould, M.K. Hospital characteristics associated with timeliness of care in veterans with lung cancer. Am. J. Respir. Crit. Care Med. 2009, 179, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Seda, G.; Stafford, C.M.; Parrish, J.S.; Praske, S.P.; Daheshia, M. Population characterization, histological evaluation, and timeliness of care of surgical nonsmall cell lung cancer patients in a military academic medical center. Mil. Med. 2012, 177, 748–751. [Google Scholar] [CrossRef]
- Walters, S.; Maringe, C.; Coleman, M.P.; Peake, M.D.; Butler, J.; Young, N.; Bergström, S.; Hanna, L.; Jakobsen, E.; Kölbeck, K.; et al. Lung cancer survival and stage at diagnosis in Australia, Canada, Denmark, Norway, Sweden and the UK: A population-based study, 2004–2007. Thorax 2013, 68, 551–564. [Google Scholar] [CrossRef]
- Jemal, A.; Fedewa, S.A. Lung Cancer Screening With Low-Dose Computed Tomography in the United States—2010 to 2015. JAMA Oncol. 2017, 3, 1278–1281. [Google Scholar] [CrossRef]
- Duggan, K.J.; Descallar, J.; Vinod, S.K. Application of Guideline Recommended Treatment in Routine Clinical Practice: A Population-based Study of Stage I-IIIB Non-small Cell Lung Cancer. Clin. Oncol. 2016, 28, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Tolwin, Y.; Gillis, R.; Peled, N. Gender and lung cancer-SEER-based analysis. Ann. Epidemiol. 2020, 46, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Freeman, H.P.; Chu, K.C. Determinants of cancer disparities: Barriers to cancer screening, diagnosis, and treatment. Surg. Oncol. Clin. North Am. 2005, 14, 655–669. [Google Scholar] [CrossRef]
- Overhage, J.M.; Overhage, L.M. Sensible use of observational clinical data. Stat. Methods Med. Res. 2013, 22, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Koo, M.M.; Hamilton, W.; Walter, F.M.; Rubin, G.P.; Lyratzopoulos, G. Symptom Signatures and Diagnostic Timeliness in Cancer Patients: A Review of Current Evidence. Neoplasia 2018, 20, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Guldbrandt, L.M.; Fenger-Grøn, M.; Rasmussen, T.R.; Rasmussen, F.; Meldgaard, P.; Vedsted, P. The effect of direct access to CT scan in early lung cancer detection: An unblinded, cluster-randomised trial. BMC Cancer 2015, 15, 934. [Google Scholar] [CrossRef]
- Iyer, S.; Roughley, A.; Rider, A.; Taylor-Stokes, G. The symptom burden of non-small cell lung cancer in the USA: A real-world cross-sectional study. Support. Care Cancer 2014, 22, 181–187. [Google Scholar] [CrossRef]


| Patient Characteristics | All (n = 711) n (%) * | Stage 1 (n = 193) n (%) | Stage 2 (n = 45) n (%) | Stage 3 (n = 109) n (%) | Stage 4 (n = 276) n (%) | Stage Not Known (n = 80) n (%) |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18–49 | 36 (5.1) | 7 (3.6) | 2 (4.4) | 4 (3.7) | 19 (6.9) | 4 (5.0) |
| 50–59 | 129 (18.1) | 30 (15.5) | 7 (15.6) | 23 (21.1) | 49 (17.8) | 17 (21.2) |
| 60–69 | 261 (36.7) | 74 (38.3) | 16 (35.6) | 43 (39.4) | 98 (35.5) | 26 (32.5) |
| 70–79 | 185 (26.0) | 51 (26.4) | 15 (33.3) | 28 (25.7) | 72 (26.1) | 19 (23.8) |
| 80+ | 100 (14.1) | 31 (16.1) | 5 (11.1) | 11 (10.1) | 38 (13.8) | 14 (17.5) |
| Sex | ||||||
| Male | 355 (49.9) | 73 (37.8) | 29 (64.4) | 61 (56.0) | 145 (52.5) | 43 (53.8) |
| Race/Ethnicity | ||||||
| Asian or Pacific Islander | 80 (11.3) | 17 (8.8) | 8 (17.8) | 11 (10.1) | 33 (12.0) | 11 (13.8) |
| Hispanic or Latino | 23 (3.2) | 6 (3.1) | 3 (6.7) | 5 (4.6) | 7 (2.5) | 2 (2.5) |
| Non-Hispanic Black | 58 (8.2) | 21 (10.9) | 3 (6.7) | 8 (7.3) | 23 (8.3) | 3 (3.8) |
| Non-Hispanic White | 492 (69.2) | 144 (74.6) | 27 (60.0) | 80 (73.4) | 179 (64.9) | 56 (70.0) |
| Other | 58 (8.2) | 5 (2.6) | 4 (8.9) | 5 (4.6) | 34 (12.3) | 8 (10.0) |
| Smoking status | ||||||
| Ever smoker | 531 (74.7) | 152 (78.8) | 39 (86.7) | 94 (86.2) | 184 (66.7) | 56 (70.0) |
| Never smoker | 122 (17.2) | 38 (19.7) | 4 (8.9) | 8 (7.3) | 63 (22.8) | 8 (10.0) |
| Unknown | 58 (8.2) | 3 (1.6) | 2 (4.4) | 7 (6.4) | 29 (10.5) | 16 (20.0) |
| Insurance | ||||||
| Medicaid | 117 (16.5) | 25 (13.0) | 3 (6.7) | 25 (22.9) | 49 (17.8) | 15 (18.8) |
| Medicare | 437 (61.5) | 133 (68.9) | 32 (71.1) | 58 (53.2) | 164 (59.4) | 45 (56.2) |
| Military | 13 (1.8) | 5 (2.6) | 0 (0.0) | 3 (2.8) | 4 (1.4) | 1 (1.2) |
| Not Insured | 7 (1.0) | 1 (0.5) | 0 (0.0) | 3 (2.8) | 3 (1.1) | 0 (0.0) |
| Private | 130 (18.3) | 28 (14.5) | 10 (22.2) | 19 (17.4) | 54 (19.6) | 17 (21.2) |
| Unknown | 7 (1.0) | 1 (0.5) | 0 (0.0) | 1 (0.9) | 2 (0.7) | 2 (2.5) |
| Census Tract Poverty Indicator | ||||||
| 0–10% poverty | 383 (53.9) | 108 (56.0) | 21 (46.7) | 56 (51.4) | 151 (54.7) | 41 (51.2) |
| 10–20% poverty | 222 (31.2) | 53 (27.5) | 15 (33.3) | 31 (28.4) | 92 (33.3) | 29 (36.2) |
| ≥20% poverty | 106 (14.9) | 32 (16.6) | 9 (20.0) | 22 (20.2) | 33 (12.0) | 10 (12.5) |
| Comorbidity: Elixhauser van Walraven Weighted Score mean (SD) | 17.36 (11.8) | 13.53 (9.8) | 15.76 (11.8) | 16.27 (12.1) | 21.19 (11.9) | 16.16 (12.0) |
| Number of Symptoms/Signs Present within 30-Day Window * | Number of Patients | Mean (SD) | Range (Shortest, Longest Interval) | Median (IQR) |
|---|---|---|---|---|
| ≥1 | 647 | 481 (228) | 0, 731 | 570 (273–691) |
| ≥2 | 570 | 412 (233) | 0, 731 | 396 (213–653) |
| ≥3 | 396 | 377 (230) | 0, 731 | 322 (176–607) |
| ≥4 | 233 | 355 (225) | 5, 731 | 297 (165–587) |
| ≥5 | 122 | 314 (217) | 7, 731 | 264 (148–445) |
| All | Cancer Type | Stage | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NSCLC | SCLC | Stages 1,2 | Stages 3,4 | |||||||
| n | Median (IQR) | n | Median (IQR) | * | Median (IQR) | n | Median (IQR) | n | Median (IQR) | |
| Interval | ||||||||||
| A to D (Presentation to diagnosis) | 647 | 570 (273–691) | 504 | 584 (305–691) | 57 | 605 (314–709) | 211 | 639 (392–702) | 356 | 540 (272–688) |
| A to B (Presentation to chest imaging †) | 635 | 291 (144–552) | 497 | 313 (149–559) | 57 | 307 (183–627) | 209 | 286 (134–536) | 348 | 324 (176–586) |
| A to C (Presentation to specialist visit) | 640 | 236 (118–467) | 499 | 250 (123–491) | 57 | 203 (93–488) | 210 | 216 (114–480) | 352 | 261 (129–522) |
| B to D (Chest imaging to diagnosis) | 635 | 43 (11–240) | 497 | 44 (14–255) | 57 | 43 (10–150) | 209 | 100 (34–415) | 348 | 23 (7–110) |
| C to D (Specialist visit to diagnosis) | 640 | 72 (13–456) | 499 | 87 (15–468) | 57 | 84 (7–429) | 210 | 244 (44–527) | 352 | 36 (7–351) |
| D to E (Diagnosis to treatment initiation) ** | 525 | 12 (0–36) | 425 | 13 (0–40) | 51 | 3 (0–13) | 188 | 19 (0–49) | 282 | 9 (0–28) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zigman Suchsland, M.; Kowalski, L.; Burkhardt, H.A.; Prado, M.G.; Kessler, L.G.; Yetisgen, M.; Au, M.A.; Stephens, K.A.; Farjah, F.; Schleyer, A.M.; et al. How Timely Is Diagnosis of Lung Cancer? Cohort Study of Individuals with Lung Cancer Presenting in Ambulatory Care in the United States. Cancers 2022, 14, 5756. https://doi.org/10.3390/cancers14235756
Zigman Suchsland M, Kowalski L, Burkhardt HA, Prado MG, Kessler LG, Yetisgen M, Au MA, Stephens KA, Farjah F, Schleyer AM, et al. How Timely Is Diagnosis of Lung Cancer? Cohort Study of Individuals with Lung Cancer Presenting in Ambulatory Care in the United States. Cancers. 2022; 14(23):5756. https://doi.org/10.3390/cancers14235756
Chicago/Turabian StyleZigman Suchsland, Monica, Lesleigh Kowalski, Hannah A. Burkhardt, Maria G. Prado, Larry G. Kessler, Meliha Yetisgen, Maggie A. Au, Kari A. Stephens, Farhood Farjah, Anneliese M. Schleyer, and et al. 2022. "How Timely Is Diagnosis of Lung Cancer? Cohort Study of Individuals with Lung Cancer Presenting in Ambulatory Care in the United States" Cancers 14, no. 23: 5756. https://doi.org/10.3390/cancers14235756
APA StyleZigman Suchsland, M., Kowalski, L., Burkhardt, H. A., Prado, M. G., Kessler, L. G., Yetisgen, M., Au, M. A., Stephens, K. A., Farjah, F., Schleyer, A. M., Walter, F. M., Neal, R. D., Lybarger, K., Thompson, C. A., Achkar, M. A., Sarma, E. A., Turner, G., & Thompson, M. (2022). How Timely Is Diagnosis of Lung Cancer? Cohort Study of Individuals with Lung Cancer Presenting in Ambulatory Care in the United States. Cancers, 14(23), 5756. https://doi.org/10.3390/cancers14235756







