Structural and Socio-Spatial Determinants Influencing Care and Survival of Patients with a Pancreatic Adenocarcinoma: Results of the PANDAURA Cohort
Abstract
Simple Summary
Abstract
1. Introduction
2. Patients and Method
2.1. Study Objective
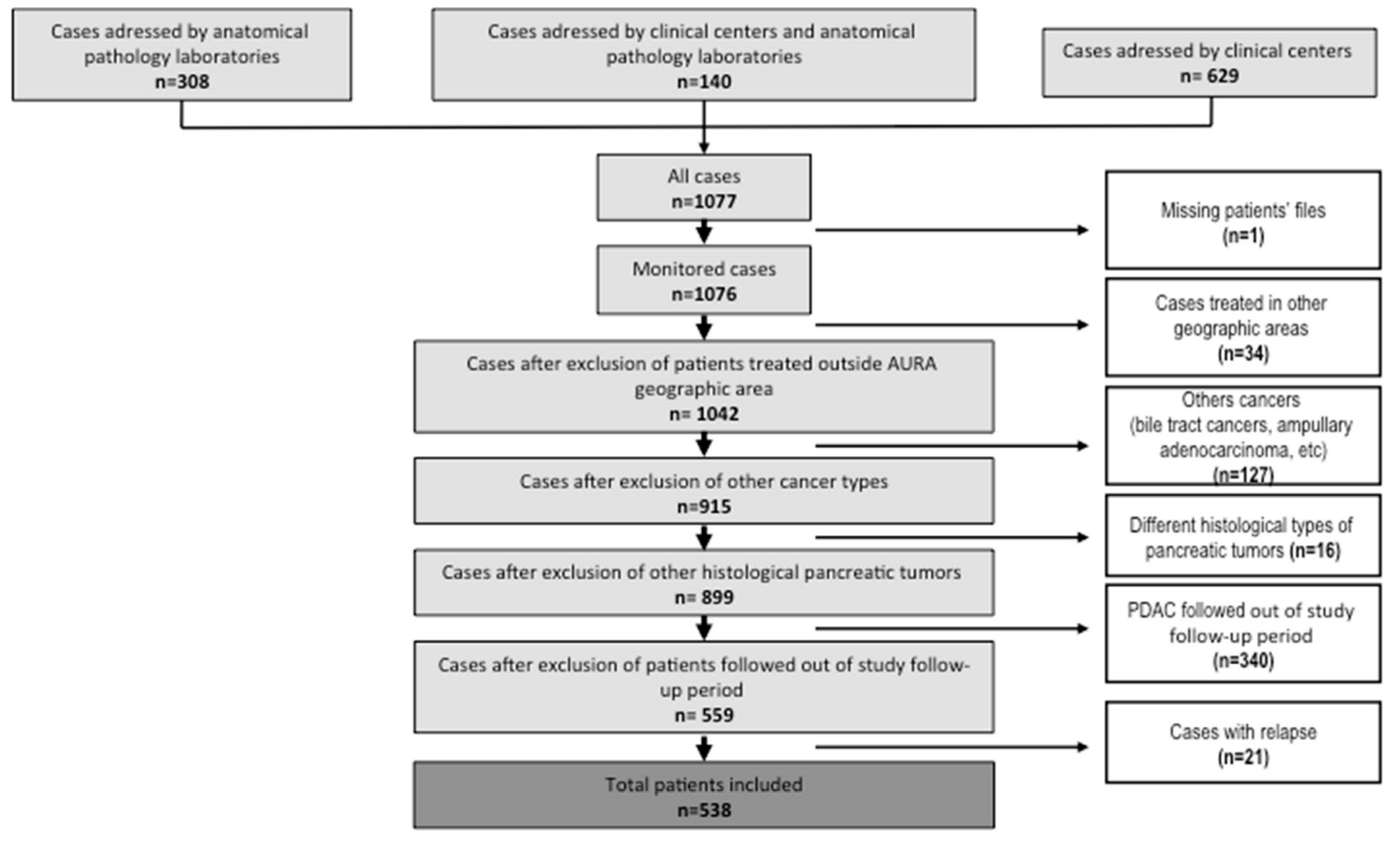
2.2. Population
2.3. Ethical Approval
2.4. Socio-Spatial Indices
2.5. Statistics
3. Results
3.1. Patient and Treatment Characteristics
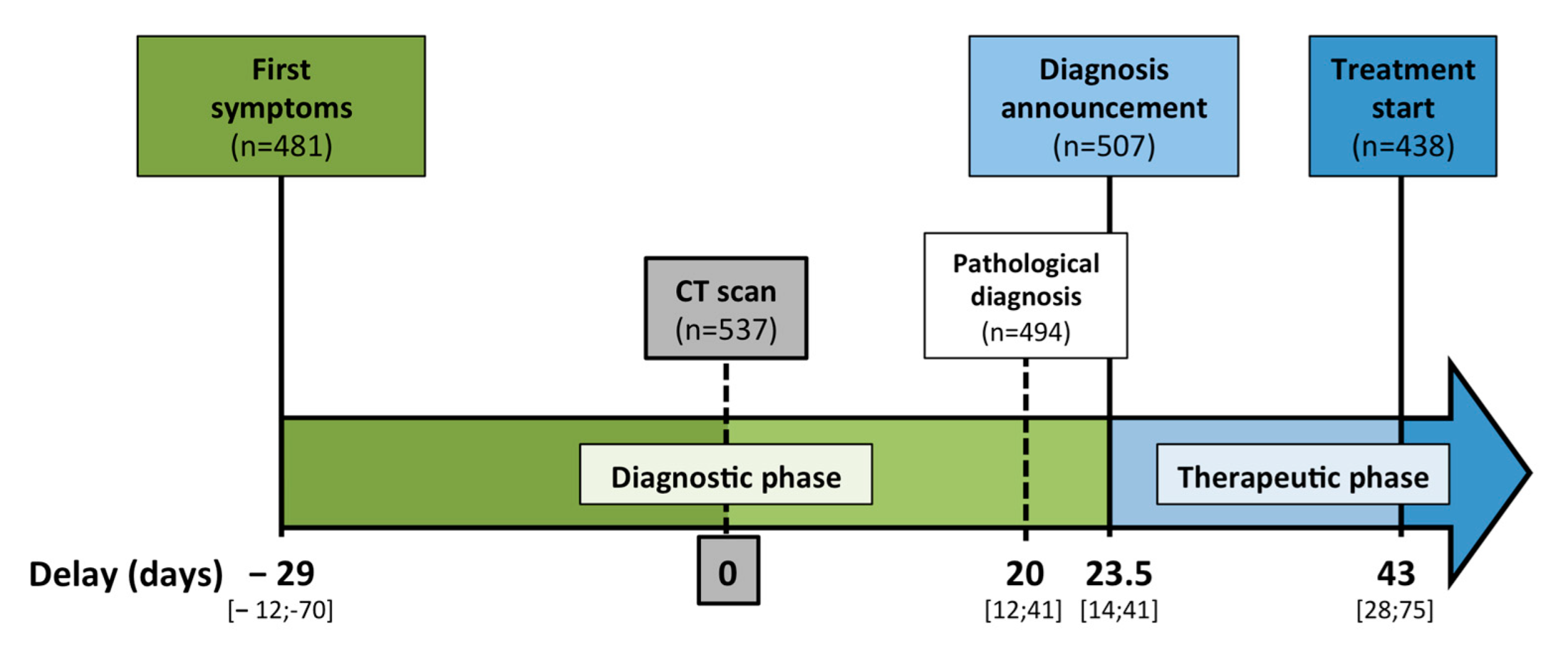
3.2. Care Pathway and Delays
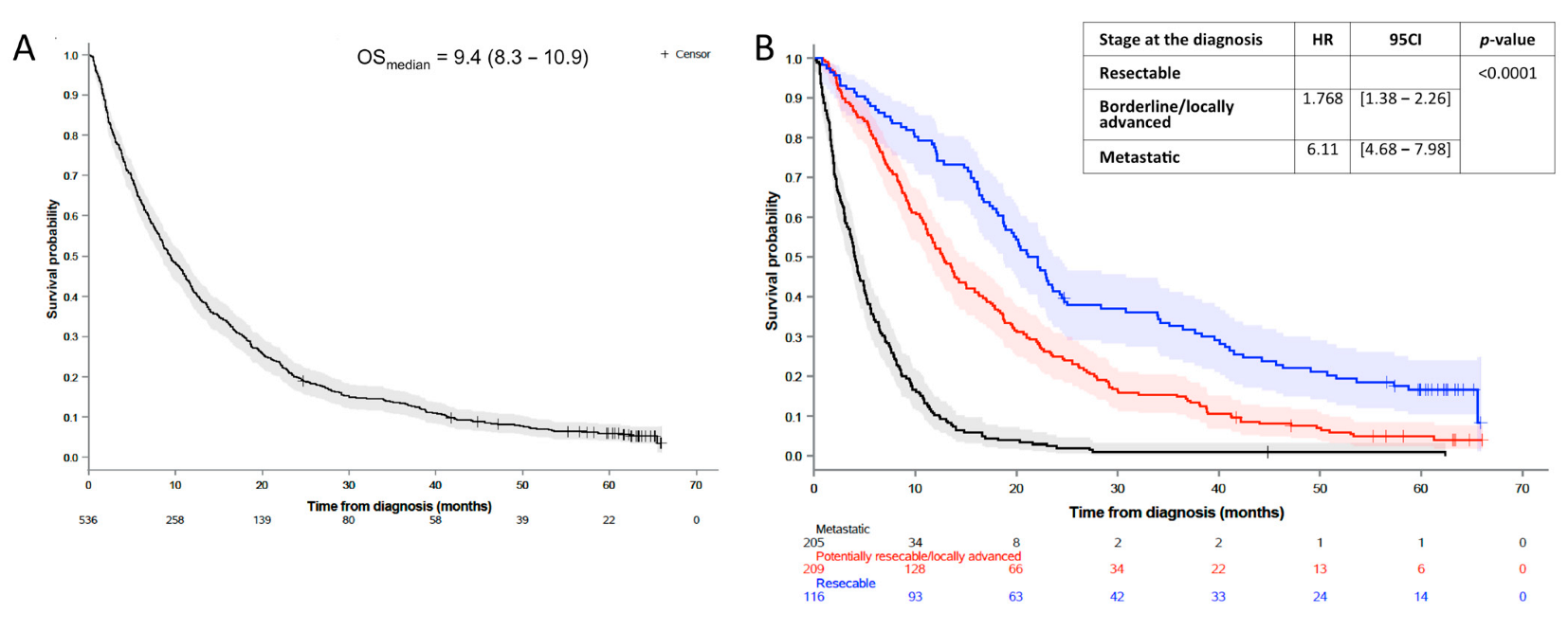
3.3. Survival Outcomes and Predictive Markers of Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Park, W.; Chawla, A.; O’Reilly, E.M. Pancreatic cancer: A review. JAMA 2021, 326, 851–862. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.P.; Hong, T.S.; Bardeesy, N. Pancreatic adenocarcinoma. N. Engl. J. Med. 2014, 371, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the united states. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef] [PubMed]
- Carioli, G.; Malvezzi, M.; Bertuccio, P.; Boffetta, P.; Levi, F.; La Vecchia, C.; Negri, E. European cancer mortality predictions for the year 2021 with focus on pancreatic and female lung cancer. Ann. Oncol. 2021, 32, 478–487. [Google Scholar] [CrossRef]
- Raptis, D.A.; Fessas, C.; Belasyse-Smith, P.; Kurzawinski, T.R. Clinical presentation and waiting time targets do not affect prognosis in patients with pancreatic cancer. Surgeon 2010, 8, 239–246. [Google Scholar] [CrossRef]
- Brugel, M.; Bouché, O.; Kianmanesh, R.; Teuma, L.; Tashkandi, A.; Regimbeau, J.M.; Pessaux, P.; Royer, B.; Rhaiem, R.; Perrenot, C.; et al. Time from first seen in specialist care to surgery does not influence survival outcome in patients with upfront resected pancreatic adenocarcinoma. BMC Surg. 2021, 21, 413. [Google Scholar] [CrossRef]
- Sanjeevi, S.; Ivanics, T.; Lundell, L.; Kartalis, N.; Andrén-Sandberg, Å.; Blomberg, J.; Del Chiaro, M.; Ansorge, C. Impact of delay between imaging and treatment in patients with potentially curable pancreatic cancer. Br. J. Surg. 2016, 103, 267–275. [Google Scholar] [CrossRef]
- Papageorge, M.V.; Evans, D.B.; Tseng, J.F. Health care disparities and the future of pancreatic cancer care. Surg. Oncol. Clin. N. Am. 2021, 30, 759–771. [Google Scholar] [CrossRef]
- Mehta, V.V.; Friedmann, P.; McAuliffe, J.C.; Muscarella, P.; In, H. Pancreatic cancer surgery following emergency department admission: Understanding poor outcomes and disparities in care. J. Gastrointest. Surg. 2020, 25, 1261–1270. [Google Scholar] [CrossRef]
- Barreto, S.G. Pancreatic cancer in australia: Is not it time we address the inequitable resource problem? Future Oncol. 2020, 16, 1385–1392. [Google Scholar] [CrossRef]
- Diaz, A.; Paredes, A.Z.; Hyer, J.M.; Pawlik, T.M. Variation in value among hospitals performing complex cancer operations. Surgery 2020, 168, 106–112. [Google Scholar] [CrossRef] [PubMed]
- de la Fouchardière, C.; Adham, M.; Marion-Audibert, A.-M.; Duclos, A.; Darcha, C.; Berthelet, O.; Hervieu, V.; Artru, P.; Labrosse, H.; Fayet, Y.; et al. Management of patients with pancreatic ductal adenocarcinoma in the real-life setting: Lessons from the french national hospital database. Cancers 2021, 13, 3515. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Qi, Y. An enhanced two-step floating catchment area (e2sfca) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 1100–1107. [Google Scholar] [CrossRef] [PubMed]
- Fayet, Y.; Praud, D.; Fervers, B.; Ray-Coquard, I.; Blay, J.-Y.; Ducimetiere, F.; Fagherazzi, G.; Faure, E. Beyond the map: Evidencing the spatial dimension of health inequalities. Int. J. Health Geogr. 2020, 19, 46. [Google Scholar] [CrossRef] [PubMed]
- Stathis, A.; Moore, M.J. Advanced pancreatic carcinoma: Current treatment and future challenges. Nat. Rev. Clin. Oncol. 2010, 7, 163–172. [Google Scholar] [CrossRef]
- Exarchakou, A.; Kipourou, D.-K.; Belot, A.; Rachet, B. Socio-economic inequalities in cancer survival: How do they translate into number of life-years lost? Br. J. Cancer 2022, 126, 1490–1498. [Google Scholar] [CrossRef]
- Acuna, S.A.; Kirkegård, J.; Ladekarl, M.; Fristrup, C.W.; Hansen, C.P.; Sall, M.; Mortensen, F.V. Urban versus rural residency and pancreatic cancer survival: A danish nationwide population-based cohort study. PLoS ONE 2018, 13, e0202486. [Google Scholar]
- Kuhn, Y.; Koscielny, A.; Glowka, T.; Hirner, A.; Kalff, J.C.; Standop, J. Postresection survival outcomes of pancreatic cancer according to demographic factors and socio-economic status. Eur. J. Surg. Oncol. (EJSO) 2010, 36, 496–500. [Google Scholar] [CrossRef]
- Thobie, A.; Mulliri, A.; Dolet, N.; Eid, Y.; Bouvier, V.; Launoy, G.; Alves, A.; Dejardin, O. Socioeconomic status impacts survival and access to resection in pancreatic adenocarcinoma: A high-resolution population-based cancer registry study. Surg. Oncol. 2018, 27, 759–766. [Google Scholar] [CrossRef]
- Murage, P.; Crawford, S.M.; Bachmann, M.; Jones, A. Geographical disparities in access to cancer management and treatment services in england. Health Place 2016, 42, 11–18. [Google Scholar] [CrossRef]
- Green, T.; Atkin, K.; Macleod, U. Cancer detection in primary care: Insights from general practitioners. Br. J. Cancer 2015, 112, S41–S49. [Google Scholar] [CrossRef] [PubMed]
- Lucas-Gabrielli, V.; Mangeney, C. How can accessibility measures be improved to better target underserved areas? Rev. D’epidemiologie Sante Publique 2019, 67, S25–S32. [Google Scholar] [CrossRef] [PubMed]
- Virgilsen, L.F.; Møller, H.; Vedsted, P. Travel distance to cancer-diagnostic facilities and tumour stage. Health Place 2019, 60, 102208. [Google Scholar] [CrossRef] [PubMed]
- Hata, T.; Motoi, F.; Ishida, M.; Naitoh, T.; Katayose, Y.; Egawa, S.; Unno, M. Effect of hospital volume on surgical outcomes after pancreaticoduodenectomy: A systematic review and meta-analysis. Ann. Surg. 2016, 263, 664–672. [Google Scholar] [CrossRef]
- Ahola, R.; Sand, J.; Laukkarinen, J. Centralization of pancreatic surgery improves results: Review. Scand. J. Surg. 2020, 109, 4–10. [Google Scholar] [CrossRef]
- Ahmad, A.; van Roest, M.H.G.; van der Aa, M.A.; van der Geest, L.G.M.; de Jong, K.P. The impact of socioeconomic status, surgical resection and type of hospital on survival in patients with pancreatic cancer. A population-based study in the netherlands. PLoS ONE 2016, 11, e0166449. [Google Scholar]
| Patients’ Characteristics | All | |
|---|---|---|
| n = 538 | ||
| Clinical and biological characteristics | ||
| Sex | ||
| Male | 288 | (53.5%) |
| Female | 250 | (46.5%) |
| Age * | 71.60 [63.80–78.30] | |
| ≤70 | 238 | (44.2%) |
| >70 | 300 | (55.8%) |
| BMI | ||
| <20 | 58 | (10.8%) |
| [20–24] | 243 | (45.2%) |
| [25–29] | 161 | (29.9%) |
| ≥30 | 76 | (14.1%) |
| Past medical history | ||
| Diabetes | 156 | (29.0%) |
| Tobacco | 173 | (32.2%) |
| Previous cancer | 79 | (14.7%) |
| Circumstances of cancer diagnosis | ||
| Incidental | 57 | (10.6%) |
| Presence of symptoms | 481 | (89.4%) |
| Abdominal pain | 295 | (54.8%) |
| Jaundice | 135 | (25.1%) |
| Loss of weight | 121 | (22.5%) |
| Other symptoms | 173 | (32.2%) |
| Stage at the diagnosis | ||
| Missing data | 6 | |
| Resectable | 116 | (21.8%) |
| Borderline | 64 | (12.0%) |
| Locally advanced | 147 | (27.6%) |
| Metastatic | 205 | (38.5%) |
| Histological differenciation grade | ||
| Missing data | 233 | |
| Well differentiated | 77 | (25.2%) |
| Moderately differentiated | 178 | (58.4%) |
| Poorly differentiated | 50 | (16.4%) |
| Socio-spatial determinants | ||
| French deprivation index (Fdep) * | −0.11 [−1.05–0.80] | |
| ≤−1.3 | 105 | (21.4%) |
| [−1.2; −0.5] | 115 | (20.8%) |
| [−0.4; 0.3] | 112 | (18.2%) |
| [0.4; 1] | 98 | (20.1%) |
| >1 | 108 | (19.5%) |
| Accessibility of General Practitioners (Localized Potential Accessibility index) * | 70.43 [52.74–82.61] | |
| ≤46.7 | 108 | (19.7%) |
| [46.8; 63.8] | 106 | (21.9%) |
| [63.9; 74.3] | 118 | (18.4%) |
| [74.4; 86.4] | 99 | (19.9%) |
| >86.4 | 107 | (20.1%) |
| Population density * (inhabitants/km2) | 446.55 [107.62–2132.50] | |
| ≤83.7 | 107 | (19.9%) |
| [83.8; 254.7] | 109 | (20.3%) |
| [254.8; 798.1] | 108 | (20.1%) |
| [798.2; 2159.9] | 106 | (19.7%) |
| >2159.9 | 108 | (20.1%) |
| Travel time to the nearest specialized center (in minutes) | 48.0 [18.0–71.0] | |
| ≤13 | 115 | (21.4%) |
| [14; 36] | 101 | (18.8%) |
| [37; 58] | 109 | (20.3%) |
| [59; 79] | 107 | (19.9%) |
| >79 | 106 | (19.7%) |
| GeoClasH Classification | ||
| Wealthy Metropolitan Areas | 139 | (25.8%) |
| Precarious Population Districts | 249 | (46.3%) |
| Residential Outskirts | 80 | (14.9%) |
| Agricultural and Industrial Plains | 17 | (3.2%) |
| Rural Margins | 53 | (9.9%) |
| Therapeutic strategies | ||
| Curative intent | ||
| Surgical resection alone | 26 | (4.8%) |
| Surgical resection with chemotherapy | 108 | (20.1%) |
| Surgical resection with chemotherapy and radiation therapy | 13 | (2.4%) |
| Palliative intent | ||
| Chemotherapy alone | 230 | (42.8%) |
| Chemotherapy with radiation therapy | 24 | (4.5%) |
| Radiation therapy alone | 3 | (0.6%) |
| Other types of surgery alone | 8 | (1.5%) |
| Other types of surgery with chemotherapy | 22 | (4.1%) |
| Other types of surgery with chemotherapy and radiation therapy | 4 | (0.7%) |
| Exclusive best supportive care | 100 | (18.6%) |
| Variables | Value | HR | IC95 | p-Value |
|---|---|---|---|---|
| Clinical characteristics | ||||
| Sex | Female | NS(1) | ||
| Male | ||||
| Age (years) | ≤70 | <0.0001 | ||
| >70 | 1.462 | [1.22–1.75] | ||
| BMI | <20 | NS(4) | ||
| [20–24] | ||||
| [25–29] | ||||
| ≥30 | ||||
| Presence of diabetes | No | NS(7) | ||
| Yes | ||||
| Circumstances of cancer diagnosis | Incidental diagnosis | 0.0042 | ||
| Presence of symptoms | 1.564 | [1.15–2.13] | ||
| Stage at the diagnosis | Resectable | <0.0001 | ||
| Borderline/locally advanced | 1.768 | [1.38–2.26] | ||
| Metastatic | 6.11 | [4.68–7.98] | ||
| Socio-spatial determinants | ||||
| French deprivation index | ≤−1.3 | NS(8) | ||
| [−1.2; −0.5] | ||||
| [−0.4; 0.3] | ||||
| [0.4; 1] | ||||
| >1 | ||||
| Accessibility of General Practitioners (Localized Potential Accessibility index) | ≤46.7 | NS(10) | ||
| [46.8; 63.8] | ||||
| [63.9; 74.3] | ||||
| [74.4; 86.4] | ||||
| >86.4 | ||||
| Population density (inhabitants/km2) | ≤83.7 | NS(3) | ||
| [83.8; 254.7] | ||||
| [254.8; 798.1] | ||||
| [798.2; 2159.9] | ||||
| >2159.9 | ||||
| GeoClasH Classification | Wealthy Metropolitan Areas areas | NS(6) | ||
| Precarious Population Districts areas | ||||
| Residential Outskirts | ||||
| Agricultural and Industrial Plains | ||||
| Rural Margins | ||||
| Travel time to the nearest specialized center (in minutes) | ≤13 | NS(5) | ||
| [14; 36] | ||||
| [37; 58] | ||||
| [59; 79] | ||||
| >79 |
| Variables | HR | IC95 | p-Value | |
|---|---|---|---|---|
| Clinical characteristics | ||||
| Sex | Female | NS(5) | ||
| Male | ||||
| Age class | ≤70 | NS(6) | ||
| >70 | ||||
| BMI | <20 | NS(10) | ||
| [20–24] | ||||
| [25–29] | ||||
| ≥30 | ||||
| Presence of diabetes | No | NS(9) | ||
| Yes | ||||
| Circumstances of cancer diagnosis | Incidental diagnosis | NS(11) | ||
| Presence of symptoms | ||||
| Stage at the diagnosis | Resectable | NS(4) | ||
| Borderline/locally advanced | ||||
| Metastatic | ||||
| Surgical features | ||||
| Resection margin status | R0 | NS(8) | ||
| R1 | ||||
| Surgery-related adverse events | No | NS(7) | ||
| Yes | ||||
| Number of pancreatic surgeries per center per year | <5 | 2.236 | [1.34–3.72] | 0.0081 |
| 5–20 | 1.215 | [0.86–1.72] | ||
| >20 | ||||
| Socio-spatial determinants | ||||
| French deprivation index | ≤−1.3 | 1.336 | [0.80–2.24] | 0.0199 |
| [−1.2; −0.5] | 0.575 | [0.34–0.98] | ||
| [−0.4; 0.3] | ||||
| [0.4; 1] | 1.136 | [0.67–1.92] | ||
| >1 | 0.888 | [0.52–1.50] | ||
| Accessibility of General Practitioners (Localized Potential Accessibility index) | ≤46.7 | NS(12) | ||
| [46.8; 63.8] | ||||
| [63.9; 74.3] | ||||
| [74.4; 86.4] | ||||
| >86.4 | ||||
| Population density (inhabitants/km2) | ≤83.7 | NS(3) | ||
| [83.8; 254.7] | ||||
| [254.8; 798.1] | ||||
| [798.2; 2159.9] | ||||
| >2159.9 | ||||
| GeoClasH Classification | Wealthy Metropolitan Areas | NS(2) | ||
| Precarious Population Districts | ||||
| Residential Outskirts | ||||
| Agricultural and Industrial Plains | ||||
| Rural Margins | ||||
| Travel time to the nearest specialized center (in minutes) | ≤13 | NS(1) | ||
| [14; 36] | ||||
| [37; 58] | ||||
| [59; 79] | ||||
| >79 | ||||
| Variables | OR | IC 95 | p-Value | |
|---|---|---|---|---|
| Accessibility of GeneralPractitioners | <74.3 | 0.0153 | ||
| ≥74.3 | 1.673 | [1.10–2.54] | ||
| Population density (inhabitants/km2) | <795.1 | 1.881 | [1.20–2.94] | 0.0057 |
| ≥795.1 | ||||
| Travel time to the nearest specialized center (in minutes) | <58 | 0.2162 | ||
| ≥58 | 1.300 | [0.86–1.97] | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roth, G.S.; Fayet, Y.; Benmameche-Medjahed, S.; Ducimetière, F.; Charreton, A.; Cropet, C.; Chabaud, S.; Marion-Audibert, A.-M.; Berthelet, O.; Walter, T.; et al. Structural and Socio-Spatial Determinants Influencing Care and Survival of Patients with a Pancreatic Adenocarcinoma: Results of the PANDAURA Cohort. Cancers 2022, 14, 5413. https://doi.org/10.3390/cancers14215413
Roth GS, Fayet Y, Benmameche-Medjahed S, Ducimetière F, Charreton A, Cropet C, Chabaud S, Marion-Audibert A-M, Berthelet O, Walter T, et al. Structural and Socio-Spatial Determinants Influencing Care and Survival of Patients with a Pancreatic Adenocarcinoma: Results of the PANDAURA Cohort. Cancers. 2022; 14(21):5413. https://doi.org/10.3390/cancers14215413
Chicago/Turabian StyleRoth, Gaël S., Yohan Fayet, Sakina Benmameche-Medjahed, Françoise Ducimetière, Amandine Charreton, Claire Cropet, Sylvie Chabaud, Anne-Marie Marion-Audibert, Olivier Berthelet, Thomas Walter, and et al. 2022. "Structural and Socio-Spatial Determinants Influencing Care and Survival of Patients with a Pancreatic Adenocarcinoma: Results of the PANDAURA Cohort" Cancers 14, no. 21: 5413. https://doi.org/10.3390/cancers14215413
APA StyleRoth, G. S., Fayet, Y., Benmameche-Medjahed, S., Ducimetière, F., Charreton, A., Cropet, C., Chabaud, S., Marion-Audibert, A.-M., Berthelet, O., Walter, T., Adham, M., Baconnier, M., Tavan, D., Williet, N., Artru, P., Huet-Penz, F., Ray-Coquard, I., Farsi, F., Labrosse, H., & de la Fouchardière, C. (2022). Structural and Socio-Spatial Determinants Influencing Care and Survival of Patients with a Pancreatic Adenocarcinoma: Results of the PANDAURA Cohort. Cancers, 14(21), 5413. https://doi.org/10.3390/cancers14215413







