Diagnosis and Management of Porocarcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Epidemiology
3. Pathogenesis
4. Diagnosis
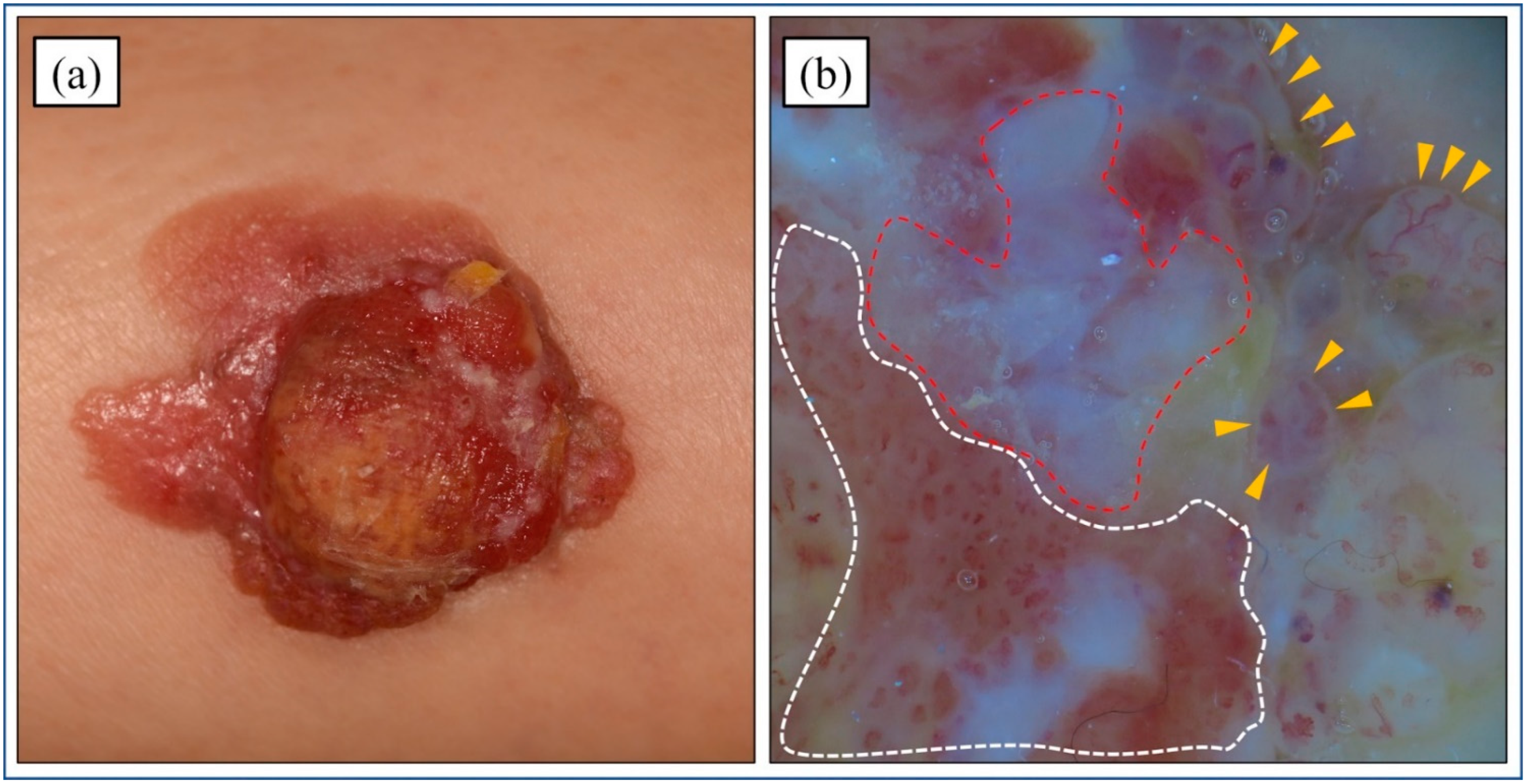
4.1. Clinical Features
4.2. Dermoscopic Features
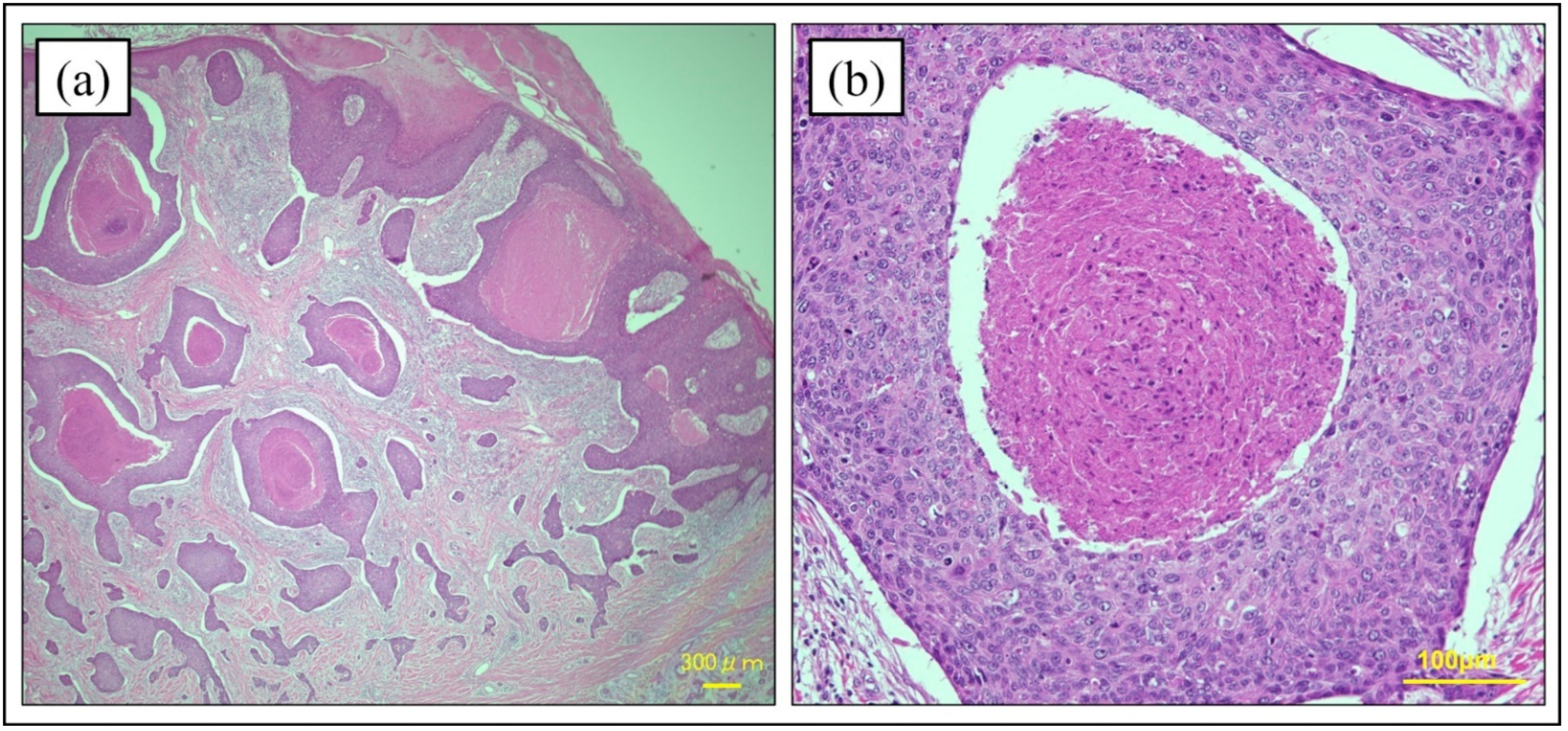
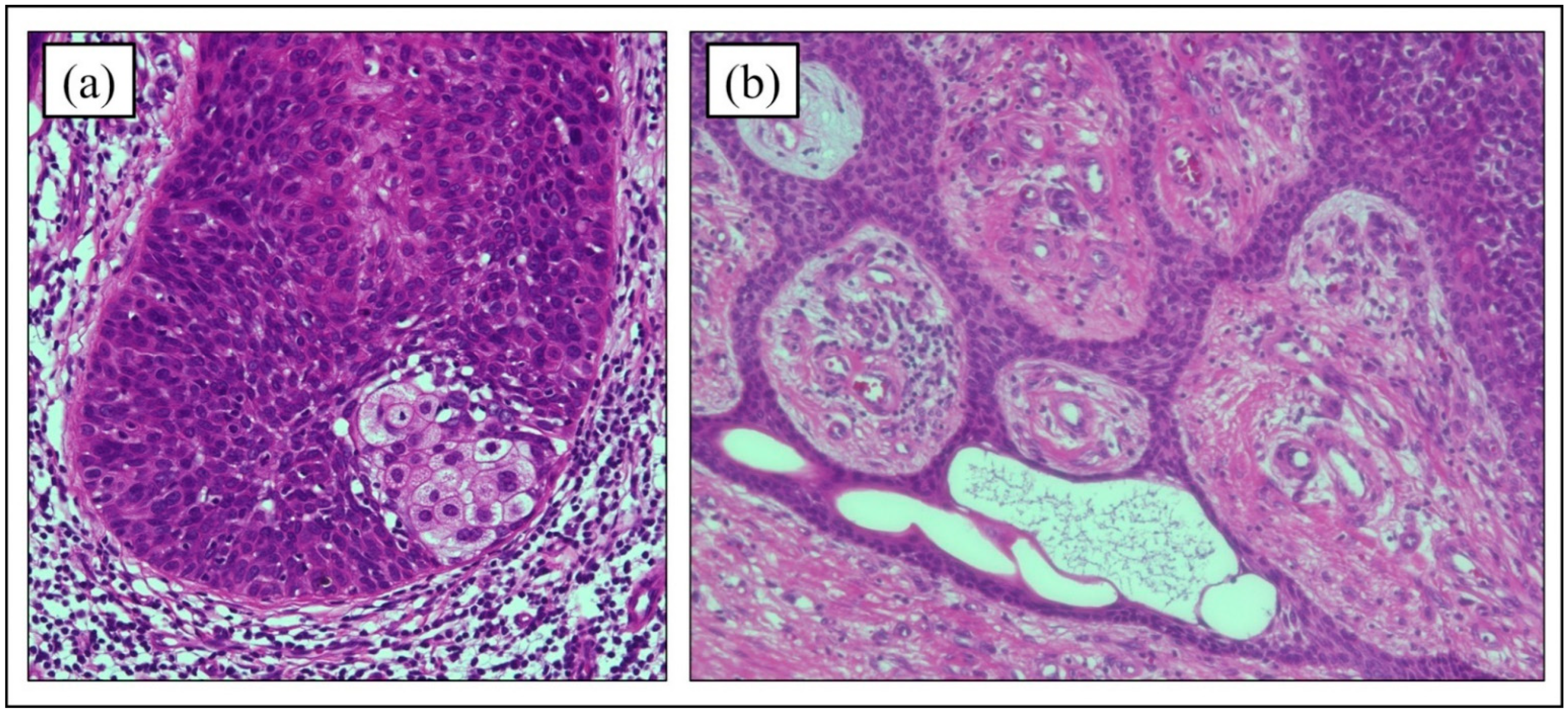
4.3. Histopathology of Hematoxylin and Eosin Staining
4.4. Immunohistochemistry
5. Prognosis and Risk Factors for Metastasis/Recurrence/Disease-Specific Survival
6. Treatments
6.1. Surgical Treatments
6.2. Radiotherapy
6.3. Chemotherapy
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AIDS | acquired immune deficiency syndrome |
| HE | hematoxylin and eosin |
| MMS | Mohs micrographic surgery |
| PC | porocarcinoma |
| SCC | squamous cell carcinoma |
| USA | United States of America |
| WLE | wide local excision |
| WHO | World Health Organization |
| XP | xeroderma pigmentosum |
References
- Kaseb, H.; Babiker, H.M. Eccrine Carcinoma; StatPearls Publishing: Treasure Island, FL, USA, 2022.
- Pinkus, H.; Mehregan, A.H. Epidermoptropic eccrine carcinoma: A case combining features of eccrine poroma and Paget’s disease. Arch. Dermatol. 1963, 88, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Mishima, Y.; Morioka, S. Oncogenic differentiation of the intraepidermal eccrine sweat duct: Eccrine poroma, poroepithelioma and porocarcinoma. Dermatology 1969, 138, 238–250. [Google Scholar] [CrossRef] [PubMed]
- Elder, D.E.M.D.; Scolyer, R.A.; Willemze, R. Appendageal tumours. In WHO Classification of Skin Tumours, 4th ed.; International Agency for Research on Cancer: Lyon, France, 2018; Volume 11, p. 159. ISBN 9789283224402/928322440X. [Google Scholar]
- Robson, A.; Greene, J.; Ansari, N.; Kim, B.; Seed, P.T.; McKee, P.H.; Calonje, E. Eccrine porocarcinoma (malignant eccrine poroma): A clinicopathologic study of 69 cases. Am. J. Surg. Pathol. 2001, 25, 710–720. [Google Scholar] [CrossRef] [PubMed]
- Blake, P.W.; Bradford, P.T.; Devesa, S.S.; Toro, J.R. Cutaneous appendageal carcinoma incidence and survival patterns in the United States: A population-based study. Arch. Dermatol. 2010, 146, 625–632. [Google Scholar] [CrossRef]
- Merilainen, A.S.; Pukkala, E.; Bohling, T.; Koljonen, V. Malignant eccrine porocarcinoma in Finland during 2007 to 2017. Acta Derm.-Venereol. 2021, 101, adv00363. [Google Scholar] [CrossRef]
- Gibbs, D.C.; Yeung, H.; Blalock, T.W. Incidence and trends of cutaneous adnexal tumors in the United States in 2000-2018: A population-based study. J. Am. Acad. Dermatol. 2022. [Google Scholar] [CrossRef]
- Tolkachjov, S.N.; Schmitt, A.R.; Muzic, J.G.; Weaver, A.L.; Baum, C.L. Incidence and clinical features of rare cutaneous malignancies in Olmsted County Minnesota, 2000 to 2010. Dermatol. Surg. 2017, 43, 116–124. [Google Scholar] [CrossRef]
- Goon, P.K.C.; Gurung, P.; Levell, N.J.; Subramanian, P.; Yong, A.S.W.; Lee, K.Y.C.; Igali, L.; Greenberg, D.; Shah, S.N.; Tan, E.K.H. Eccrine porocarcinoma of the skin is rising in incidence in the East of England. Acta Derm.-Venereol. 2018, 98, 991–992. [Google Scholar] [CrossRef]
- Salih, A.M.; Kakamad, F.H.; Baba, H.O.; Salih, R.Q.; Hawbash, M.R.; Mohammed, S.H.; Othman, S.; Saeed, Y.A.; Habibullah, I.J.; Muhialdeen, A.S.; et al. Porocarcinoma; presentation and management, a meta-analysis of 453 cases. Ann. Med. Surg. 2017, 20, 74–79. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, A.; Moon, K.C.; Seo, S.H.; Kim, I.H.; Kim, A.; Baek, Y.S. Eccrine Porocarcinoma: A Multicenter Retrospective Study with Review of the Literatures Reported in Korea. Ann. Dermatol. 2020, 32, 223–229. [Google Scholar] [CrossRef]
- Valverde, K.; Senger, C.; Ngan, B.Y.; Chan, H.S. Eccrine porocarcinoma in a child that evolved rapidly from an eccrine poroma. Med. Pediatr. Oncol. 2001, 37, 412–414. [Google Scholar] [CrossRef] [PubMed]
- Poiares Baptista, A.; Tellechea, O.; Reis, J.P.; Cunha, M.F.; Fiqueiredo, P. Eccrine porocarcinoma. A review of 24 cases. Ann. Dermatol. Venereol. 1993, 120, 107–115. [Google Scholar] [PubMed]
- Scampa, M.; Merat, R.; Kalbermatten, D.F.; Oranges, C.M. Head and Neck Porocarcinoma: SEER Analysis of Epidemiology and Survival. J. Clin. Med. 2022, 11, 2185. [Google Scholar] [CrossRef] [PubMed]
- El-Domeiri, A.A.; Brasfield, R.D.; Huvos, A.G.; Strong, E.W. Sweat gland carcinoma: A clinico-pathologic study of 83 patients. Ann. Surg. 1971, 173, 270–274. [Google Scholar] [CrossRef]
- De Giorgi, V.; Silvestri, F.; Savarese, I.; Venturi, F.; Scarfì, F.; Trane, L.; Bellerba, F.; Zuccaro, B.; Maio, V.; Massi, D.; et al. Porocarcinoma: An epidemiological, clinical, and dermoscopic 20-year study. Int. J. Dermatol. 2022, 61, 1098–1105. [Google Scholar] [CrossRef]
- Pylyser, K.; Wolf-Peters, C.; Marien, K. Histology of eccrine poromas: A study of 14 cases. Dermatology 1983, 167, 243–249. [Google Scholar] [CrossRef]
- Shaw, M.; McKee, P.H.; Lowe, D.; Black, M.M. Malignant eccrine poroma: A study of twenty-seven cases. Br. J. Dermatol. 1982, 107, 675–680. [Google Scholar] [CrossRef]
- Olmos Nieva, C.C.; Samaniego González, E.; González Morán, M.A.; Rodríguez Prieto, M.A. Eccrine Porocarcinoma: A Clinical and Histologic Description of a Series of 11 Cases Treated at the University Hospital Complex in Leon, Spain. Actas Dermo-Sifiliogr. 2021, 112, 478–481. [Google Scholar] [CrossRef]
- Puttick, L.; Ince, P.; Comaish, J.S. Three cases of eccrine porocarcinoma. Br. J. Dermatol. 1986, 115, 111–116. [Google Scholar] [CrossRef]
- Puttonen, M.; Isola, J.; Ylinen, O.; Böhling, T.; Koljonen, V.; Sihto, H. UV-induced local immunosuppression in the tumour microenvironment of eccrine porocarcinoma and poroma. Sci. Rep. 2022, 12, 5529. [Google Scholar] [CrossRef]
- Wong, S.Q.; Waldeck, K.; Vergara, I.A.; Schröder, J.; Madore, J.; Wilmott, J.S.; Colebatch, A.J.; De Paoli-Iseppi, R.; Li, J.; Lupat, R.; et al. UV-associated mutations underlie the etiology of MCV-negative Merkel cell carcinomas. Cancer Res. 2015, 75, 5228–5234. [Google Scholar] [CrossRef] [PubMed]
- Mahomed, F.; Blok, J.; Grayson, W. The squamous variant of eccrine porocarcinoma: A clinicopathological study of 21 cases. J. Clin. Pathol. 2008, 61, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, S.; Antoniou, A.; Patsatsi, A.; Kostogloudis, N.; Demiri, E.; Foroglou, P. Eccrine porocarcinoma of the thumb in a patient with chronic exposure to benzene glue. J. Hand Microsurg. 2015, 7, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Helmke, B.; Starz, H.; Bachter, D.; Balda, B.R. Metastasising porocarcinoma following exposure to poison gas. Lancet 2002, 359, 1685. [Google Scholar] [CrossRef]
- Thibodeau, M.L.; Bonakdar, M.; Zhao, E.; Mungall, K.L.; Reisle, C.; Zhang, W.; Bye, M.H.; Thiessen, N.; Bleile, D.; Mungall, A.J.; et al. Whole genome and whole transcriptome genomic profiling of a metastatic eccrine porocarcinoma. NPJ Precis. Oncol. 2018, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Bosic, M.; Kirchner, M.; Brasanac, D.; Leichsenring, J.; Lier, A.; Volckmar, A.L.; Oliveira, C.; Buchhalter, I.; Stögbauer, F.; Zivkovic-Perisic, S.; et al. Targeted molecular profiling reveals genetic heterogeneity of poromas and porocarcinomas. Pathology 2018, 50, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Harms, P.W.; Hovelson, D.H.; Cani, A.K.; Omata, K.; Haller, M.J.; Wang, M.L.; Arps, D.; Patel, R.M.; Fullen, D.R.; Wang, M.; et al. Porocarcinomas harbor recurrent HRAS-activating mutations and tumor suppressor inactivating mutations. Hum. Pathol. 2016, 51, 25–31. [Google Scholar] [CrossRef]
- Takata, M.; Hashimoto, K.; Mehregan, P.; Lee, M.W.; Yamamoto, A.; Mohri, S.; Ohara, K.; Takehara, K. Genetic changes in sweat gland carcinomas. J. Cutan. Pathol. 2000, 51, 30–35. [Google Scholar] [CrossRef]
- Westphal, D.; Garzarolli, M.; Sergon, M.; Horak, P.; Hutter, B.; Becker, J.C.; Wiegel, M.; Maczey, E.; Blum, S.; Grosche-Schlee, S.; et al. High tumour mutational burden and EGFR/MAPK pathway activation are therapeutic targets in metastatic porocarcinoma. Br. J. Dermatol. 2021, 185, 1186–1199. [Google Scholar] [CrossRef]
- Denisova, E.; Westphal, D.; Surowy, H.M.; Meier, F.; Hutter, B.; Reifenberger, J.; Rütten, A.; Schulz, A.; Sergon, M.; Ziemer, M.; et al. Whole-exome sequencing in eccrine porocarcinoma indicates promising therapeutic strategies. Cancer Gene Ther. 2022, 29, 697–708. [Google Scholar] [CrossRef]
- Cheok, C.F.; Verma, C.S.; Baselga, J.; Lane, D.P. Translating p53 into the clinic. Nat. Rev. Clin. Oncol. 2011, 8, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Granada, C.; Morlote, D.; Pavlidakey, P.; Rodriguez-Waitkus, P.; Ramirez, C.; Florento, E.; Swensen, J.; Gatalica, Z.; Stevens, T.M. Poroid adnexal skin tumors with YAP1 fusions exhibit similar histopathologic features: A series of six YAP1 rearranged adnexal skin tumors. J. Cutan. Pathol. 2021, 48, 1139–1149. [Google Scholar] [CrossRef] [PubMed]
- Snow, J.T.; Georgantzoglou, N.; Green, D.C.; Parra, O.; LeBlanc, R.E.; Yan, S.; Sriharan, A.; Momtahen, S.; Winnick, K.N.; Dimonitsas, E.; et al. Molecular analysis of NUT-positive poromas and porocarcinomas identifies novel break points of YAP1:NUTM1 fusions. J. Cutan. Pathol. 2022, 49, 850–858. [Google Scholar] [CrossRef] [PubMed]
- Sekine, S.; Kiyono, T.; Ryo, E.; Ogawa, R.; Wakai, S.; Ichikawa, H.; Suzuki, K.; Arai, S.; Tsuta, K.; Ishida, M.; et al. Recurrent YAP1-MAML2 and YAP1-NUTM1 fusions in poroma and porocarcinoma. J. Clin. Investig. 2019, 130, 3827–3832. [Google Scholar] [CrossRef]
- Taha, Z.; Janse van Rensburg, H.J.; Yang, X. The hippo pathway: Immunity and cancer. Cancers 2018, 10, 94. [Google Scholar] [CrossRef]
- Belin, E.; Ezzedine, K.; Stanislas, S.; Lalanne, N.; Beylot-Barry, M.; Taieb, A.; Vergier, B.; Jouary, T. Factors in the surgical management of primary eccrine porocarcinoma: Prognostic histological factors can guide the surgical procedure. Br. J. Dermatol. 2011, 165, 985–989. [Google Scholar] [CrossRef]
- Sawaya, J.L.; Khachemoune, A. Poroma: A review of eccrine, apocrine, and malignant forms. Int. J. Dermatol. 2014, 53, 1053–1061. [Google Scholar] [CrossRef]
- Suzaki, R.; Shioda, T.; Konohana, I.; Ishizaki, S.; Sawada, M.; Tanaka, M. Dermoscopic features of eccrine porocarcinoma arising from hidroacanthoma simplex. Dermatol. Res. Pract. 2010, 2010, 192371. [Google Scholar] [CrossRef]
- Nazemi, A.; Higgins, S.; Swift, R.; In, G.; Miller, K.; Wysong, A. Eccrine Porocarcinoma: New Insights and a Systematic Review of the Literature. Dermatol. Surg. 2018, 44, 1247–1261. [Google Scholar] [CrossRef]
- Riera-Leal, L.; Guevara-Gutiérrez, E.; Barrientos-García, J.G.; Madrigal-Kasem, R.; Briseño-Rodríguez, G.; Tlacuilo-Parra, A. Eccrine porocarcinoma: Epidemiologic and histopathologic characteristics. Int. J. Dermatol. 2015, 54, 580–586. [Google Scholar] [CrossRef]
- Perna, C.; Cuevas, J.; Jimenez-Heffernan, J.A.; Hardisson, D.; Contreras, F. Eccrine porocarcinoma (malignant eccrine poroma). Am. J. Surg. Pathol. 2002, 26, 272–274. [Google Scholar] [CrossRef] [PubMed]
- Shiohara, J.; Koga, H.; Uhara, H.; Takata, M.; Saida, T. Eccrine porocarcinoma: Clinical and pathological studies of 12 cases. J. Dermatol. 2007, 34, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Beer, T.W.; Shepherd, P.; Theaker, J.M. BerEP4 and epithelial membrane antigen aid distinction of basal cell, squamous cell and basosquamous carcinomas of the skin. Histopathology 2000, 37, 218. [Google Scholar] [CrossRef]
- Goto, K.; Takai, T.; Fukumoto, T.; Anan, T.; Kimura, T.; Ansai, S.; Oshitani, Y.; Murata, Y.; Sakuma, T.; Hirose, T. CD117 (KIT) is a useful immunohistochemical marker for differentiating porocarcinoma from squamous cell carcinoma. J. Cutan. Pathol. 2016, 43, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Ishikawa, M.; Hamada, K.; Muramatsu, K.; Naka, M.; Honma, K.; Sugino, T. Comparison of Immunohistochemical Expression of Cytokeratin 19, c-KIT, BerEP4, GATA3, and NUTM1 Between Porocarcinoma and Squamous Cell Carcinoma. Am. J. Dermatopathol. 2021, 43, 781–787. [Google Scholar] [CrossRef]
- Zahn, J.; Chan, M.P.; Wang, G.; Patel, R.M.; Andea, A.A.; Bresler, S.C.; Harms, P.W. Altered Rb, p16, and p53 expression is specific for porocarcinoma relative to poroma. J. Cutan. Pathol. 2019, 46, 659–664. [Google Scholar] [CrossRef] [PubMed]
- Macagno, N.; Kervarrec, T.; Sohier, P.; Poirot, B.; Haffner, A.; Carlotti, A.; Balme, B.; Castillo, C.; Jullie, M.L.; Osio, A.; et al. NUT Is a Specific Immunohistochemical Marker for the Diagnosis of YAP1-NUTM1-rearranged Cutaneous Poroid Neoplasms. Am. J. Surg. Pathol. 2021, 45, 1221–1227. [Google Scholar] [CrossRef]
- Storino, A.; Drews, R.E.; Tawa, N.E., Jr. Malignant Cutaneous Adnexal Tumors and Role of SLNB. J. Am. Coll. Surg. 2021, 232, 889–898. [Google Scholar] [CrossRef]
- Song, S.S.; Wu Lee, W.; Hamman, M.S.; Jiang, S.I. Mohs micrographic surgery for eccrine porocarcinoma: An update and review of the literature. Dermatol. Surg. 2015, 41, 301–306. [Google Scholar] [CrossRef]
- Koh, M.; Telang, G.; Fonseca, A.; Ghanian, S.; Walker, J. Clear Cell Differentiation in Eccrine Porocarcinoma as a High-Risk Feature: Epidemiologic and Pathologic Features of Eccrine Porocarcinoma in a Single-Center Case Series. Am. J. Dermatopathol. 2021, 43, 647–652. [Google Scholar] [CrossRef]
- Hillen, U.; Leiter, U.; Haase, S.; Kaufmann, R.; Becker, J.; Gutzmer, R.; Terheyden, P.; Krause-Bergmann, A.; Schulze, H.J.; Hassel, J.; et al. Advanced cutaneous squamous cell carcinoma: A retrospective analysis of patient profiles and treatment patterns-Results of a non-interventional study of the DeCOG. Eur. J. Cancer 2018, 96, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Le, N.S.; Janik, S.; Liu, D.T.; Grasl, S.; Faisal, M.; Pammer, J.; Schickinger-Fischer, B.; Hamzavi, J.S.; Seemann, R.; Erovic, B.M. Eccrine porocarcinoma of the head and neck: Meta-analysis of 120 cases. Head Neck 2020, 42, 2644–2659. [Google Scholar] [CrossRef] [PubMed]
- Fionda, B.; Di Stefani, A.; Lancellotta, V.; Gentileschi, S.; Caretto, A.A.; Casà, C.; Federico, F.; Rembielak, A.; Rossi, E.; Morganti, A.G.; et al. The role of postoperative radiotherapy in eccrine porocarcinoma: A multidisciplinary systematic review. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 1695–1700. [Google Scholar] [PubMed]
- Wang, L.S.; Handorf, E.A.; Wu, H.; Liu, J.C.; Perlis, C.S.; Galloway, T.J. Surgery and Adjuvant Radiation for High-risk Skin Adnexal Carcinoma of the Head and Neck. Am. J. Clin. Oncol. 2017, 40, 429–432. [Google Scholar] [CrossRef]
- Marone, U.; Caracò, C.; Anniciello, A.M.; Di Monta, G.; Chiofalo, M.G.; Di Cecilia, M.L.; Mozzillo, N. Metastatic eccrine porocarcinoma: Report of a case and review of the literature. World J. Surg. Oncol. 2011, 9, 32. [Google Scholar] [CrossRef]
- Lee, K.A.; Cioni, M.; Robson, A.; Bataille, V. Metastatic porocarcinoma achieving complete radiological and clinical response with pembrolizumab. BMJ Case Rep. 2019, 12, e228917. [Google Scholar] [CrossRef]
- Fukuda, K.; Funakoshi, T.; Fukuyama, M.; Kakuta, R.; Sato, M.; Nakamura, Y.; Tanese, K.; Masugi, Y.; Amagai, M. Metastatic eccrine porocarcinoma successfully treated with carboplatin and epirubicin chemotherapy. J. Dermatol. 2015, 42, 928–930. [Google Scholar] [CrossRef]
- McGuire, C.; Fadel, Z.; Samargandi, O.; Williams, J. Primary eccrine porocarcinoma of the thumb with multiple metastases: A case report and review of the literature. Case Rep. Plast. Surg. Hand Surg. 2019, 6, 88–91. [Google Scholar] [CrossRef]
- Yamashita, H.; Kadono, T.; Tamaki, K.; Nakagawa, K. Interesting response to concurrent chemoradiation in metastatic eccrine porocarcinoma. J. Dermatol. 2008, 35, 606–607. [Google Scholar] [CrossRef]
- Imafuku, K.; Hata, H.; Kitamura, S.; Iwata, H.; Shimizu, H. In-transit metastasis of advanced eccrine porocarcinoma. Int. J. Dermatol. 2015, 54, e503–e505. [Google Scholar] [CrossRef]
- Aaribi, I.; Mohtaram, A.; Ben Ameur El Youbi, M.; Kharmoum, J.; El Kabous, M.; Mrabti, H.; El Khannoussi, B.; Errihani, H. Successful management of metastatic eccrine porocarcinoma. Case Rep. Oncol. Med. 2013, 2013, 282536. [Google Scholar] [CrossRef] [PubMed]
- Chow, K.L.; Peters, X.; Mashbari, H.; Shokouh-Amiri, M.; Benjamin, M.; Warso, M. A Case Report of Malignant Eccrine Porocarcinoma Involving the Palm Requiring Surgical Excision and Free Flap Reconstruction. Am. J. Case Rep. 2020, 21, e925231. [Google Scholar] [CrossRef] [PubMed]
- Godillot, C.; Boulinguez, S.; Riffaud, L.; Sibaud, V.; Chira, C.; Tournier, E.; Paul, C.; Meyer, N. Complete response of a metastatic porocarcinoma treated with paclitaxel, cetuximab and radiotherapy. Eur. J. Cancer 2018, 90, 142–145. [Google Scholar] [CrossRef]
- González-López, M.A.; Vázquez-López, F.; Soler, T.; Gómez-Diéz, S.; Garcia, Y.H.; Manjón, J.A.; López-Escobar, M.; Pérez-Oliva, N. Metastatic eccrine porocarcinoma: A 5.6-year follow-up study of a patient treated with a combined therapeutic protocol. Dermatol. Surg. 2003, 29, 1227–1232. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Nguyen, L.; Everest, S.; Vinogradov, M. Metastatic Porocarcinoma Effectively Managed by Pembrolizumab. Cureus 2021, 13, e20004. [Google Scholar] [CrossRef] [PubMed]
- Gutermuth, J.; Audring, H.; Voit, C.; Trefzer, U.; Haas, N. Antitumour activity of paclitaxel and interferon-alpha in a case of metastatic eccrine porocarcinoma. J. Eur. Acad. Dermatol. Venereol. 2004, 18, 477–479. [Google Scholar] [CrossRef] [PubMed]
- Ishida, M.; Hotta, M.; Kushima, R.; Okabe, H. A case of porocarcinoma arising in pigmented hidroacanthoma simplex with multiple lymph node, liver and bone metastases. J. Cutan. Pathol. 2011, 38, 227–231. [Google Scholar] [CrossRef]
- Khaja, M.; Ashraf, U.; Mehershahi, S.; Ayyadurai, P.; Malik, S. Recurrent Metastatic Eccrine Porocarcinoma: A Case Report and Review of the Literature. Am. J. Case Rep. 2019, 20, 179–183. [Google Scholar] [CrossRef]
- Fujimine-Sato, A.; Toyoshima, M.; Shigeta, S.; Toki, A.; Kuno, T.; Sato, I.; Watanabe, M.; Niikura, H.; Yaegashi, N. Eccrine porocarcinoma of the vulva: A case report and review of the literature. J. Med. Case Rep. 2016, 10, 319. [Google Scholar] [CrossRef]
- Choi, C.M.; Cho, H.R.; Lew, B.L.; Sim, W.Y. Eccrine porocarcinoma presenting with unusual clinical manifestations: A case report and review of the literature. Ann. Dermatol. 2011, 23, s79–s83. [Google Scholar] [CrossRef]
- Kurt, M.; Kilickap, S.; Ozkaya, O.; Aksoy, S.; Erman, M. Malignant eccrine poroma presenting with pulmonary and liver metastases. Int. J. Dermatol. 2006, 45, 1263–1265. [Google Scholar] [CrossRef] [PubMed]
- Kurashige, Y.; Minemura, T.; Nagatani, T. Eccrine porocarcinoma: Clinical and pathological report of eight cases. Case Rep. Dermatol. 2013, 5, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Comito, F.; Nigro, M.C.; Sperandi, F.; Melotti, B.; Ardizzoni, A. Immunotherapy- refractory, EGFR overexpressing metastatic porocarcinoma responding to cetuximab. Eur. J. Cancer 2021, 146, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Dewan, P.; Moir, G.; Cerio, R.; Harwood, C. Aggressive eccrine porocarcinoma associated with haematological disorders: Report of two cases. Clin. Exp. Dermatol. 2010, 35, e207–e209. [Google Scholar] [CrossRef]
- Anitei, G.M.; Ioanid, N.Ş.; Bandol, G.; Gafton, E.R.; Patraşcu, A.M.; Ferariu, D.; Slătineanu, A.; Bugean, G.; Scripcariu, V. Porocarcinoma: A rare cause of lateral cervical tumor. Arch. Clin. Cases 2021, 6, 53–58. [Google Scholar] [CrossRef][Green Version]
- Lehmann, C.; Rodriguez Ossa, P.; Vargas Manrique, M.; Acosta, A.E.; Quintero Pérez, Y. Eccrine Porocarcinoma with Zosteriform Metastasis. Cureus 2020, 12, e6873. [Google Scholar] [CrossRef]
- Fernández-Ferreira, R.; Alvarado-Luna, G.; Motola-Kuba, D.; Mackinney-Novelo, I.; Cervera-Ceballos, E.E.; Segura-Rivera, R. Intergluteal Cleft Eccrine Porocarcinoma with Metastasis to Inguinal Region and Lung: Case Report and Review of the Literature. Case Rep. Oncol. 2020, 13, 1463–1473. [Google Scholar] [CrossRef]
- Ulrich, A.; Weiler, S.; Weller, M.; Rordorf, T.; Tarnutzer, A.A. Cetuximab induced aseptic meningitis. J. Clin. Neurosci. 2015, 22, 1061–1063. [Google Scholar] [CrossRef]
| Case | Clinical Findings | Treatment | Clinical Course | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Sex | Site | Size (mm) | Lymph Node Metastasis | Distant Metastasis | Surgical Resection | Chemotherapy | Radiation Therapy | RECIST | Postoperative Metastasis | Reference | |
| 1 | 42 | M | axillary | n.d. | + | - | + | bleomycin + electric pulse | - | CR | - | [57] |
| 2 | 67 | F | lower limb | n.d. | - | - | + | CBDCA + CAPE, Pembrolizumab | + | CR | + | [58] |
| 3 | 77 | M | foot | n.d. | + | - | + | CBDCA + MMC | - | CR | - | [59] |
| 4 | 56 | M | thumb | 18 × 13 | + | - | + | CBDCA + PTX + IL-2 | - | CR | + | [60] |
| 5 | 61 | M | leg | 30 | + | - | + | CDDP + 5-FU | +(50.4 Gy/28 Fr) | CR | + | [61] |
| 6 | 67 | M | foot | n.d. | + | - | + | CDDP + 5-FU | +(50 Gy/25 Fr) | CR | + | [62] |
| 7 | 54 | M | breast | n.d. | - | - | + | CDDP + 5-FU, DTX | - | CR | + | [63] |
| 8 | 63 | M | palm | 50 × 60 | - | - | + | CDDP + DTX | +(50 Gy/25 Fr) | CR | + | [64] |
| 9 | 64 | F | neck | 50 | + | - | + | PTX + cetuximab | +(57.5 Gy) | CR | + | [65] |
| 10 | 71 | M | thigh | 40 × 35 | - | - | + | VCR | +(45 Gy) | CR | + | [66] |
| 11 | 79 | M | scalp | n.d. | + | - | + | pembrolizmab | + | PR | - | [67] |
| 12 | 67 | M | neck | 30 × 25 | - | - | + | PTX + IFN-α | - | PR | + | [68] |
| 13 | 75 | M | leg | 91 | + | - | + | UFT | - | SD | - | [44] |
| 14 | 72 | M | thigh | 17 × 12 | - | - | + | CBDCA + farmourubicin | - | PD | + | [69] |
| 15 | 67 | M | scalp | 30 × 20 | - | - | + | CBDCA + DTX | + | PD | + | [70] |
| 16 | 81 | F | buttock | 25 | - | - | + | CDDP+ 5-FU | - | PD | + | [44] |
| 17 | 62 | F | head | 98 | + | - | + | CDDP + ADM + VDS, PEP + 5-FU, CPA + pirabubicin, ACNU + UFT | +(50 Gy) | PD | + | [44] |
| 18 | 54 | F | vulva | 10 × 6 | - | - | + | CDDP, PTX + CBDCA | +(50.4 Gy/28 Fr) | PD | + | [71] |
| 19 | 44 | M | scrotum | 60 × 70 | + | + | - | CDDP + 5-FU | - | PD | N/A | [72] |
| 20 | 62 | M | scalp | 5 × 6 | + | + | - | CDDP + 5-FU | - | PD | N/A | [73] |
| 21 | 50 | M | arm | 80 | + | + | + | CDDP + DTX | +(21 Gy) | PD | + | [74] |
| 22 | 70 | M | scalp | n.d. | + | - | + | DTX, pembrolizumab, cetuximab + CAPE | - | PD | + | [75] |
| 23 | 79 | F | leg | n.d. | - | - | + | IFN | - | PD | + | [76] |
| 24 | 64 | M | leg | 16 | - | - | - | MMC + VCR + EPI-ADM + CDDP + 5-FU + PEP, CDDP + 5-FU | +(50 Gy) | PD | N/A | [44] |
| 25 | 67 | F | neck | n.d. | + | - | + | platinum derivatives + taxanes | +(50 Gy/25 Fr) | PD | + | [77] |
| 26 | 77 | F | leg | n.d. | - | - | + | PTX + CAPE + IFN-α | - | PD | + | [76] |
| 27 | 64 | M | lateral wall | n.d. | + | + | - | CBDCA + taxanes | +(53 Gy) | n.d. | N/A | [78] |
| 28 | 67 | M | hip | 25 × 25 | + | - | + | etoposide, VDS, CBDCA | - | n.d. | - | [79] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyamoto, K.; Yanagi, T.; Maeda, T.; Ujiie, H. Diagnosis and Management of Porocarcinoma. Cancers 2022, 14, 5232. https://doi.org/10.3390/cancers14215232
Miyamoto K, Yanagi T, Maeda T, Ujiie H. Diagnosis and Management of Porocarcinoma. Cancers. 2022; 14(21):5232. https://doi.org/10.3390/cancers14215232
Chicago/Turabian StyleMiyamoto, Kodai, Teruki Yanagi, Takuya Maeda, and Hideyuki Ujiie. 2022. "Diagnosis and Management of Porocarcinoma" Cancers 14, no. 21: 5232. https://doi.org/10.3390/cancers14215232
APA StyleMiyamoto, K., Yanagi, T., Maeda, T., & Ujiie, H. (2022). Diagnosis and Management of Porocarcinoma. Cancers, 14(21), 5232. https://doi.org/10.3390/cancers14215232






