Establishment and Characterization of a New Human Intrahepatic Cholangiocarcinoma Cell Line LIV27
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Information
2.2. NOD/SCID/Il2rg Null (NSG) Mouse Implantation and Cell Line Establishment
2.3. Morphologic Examination and Growth Kinetics
2.4. Tumorigenicity in Nude Mice
2.5. Immunofluorescence
2.6. Western Blot
2.7. Karyotyping and STR Profiling
2.8. Mycoplasma Detection
3. Results
3.1. Establishment of the LIV27 Cell Line
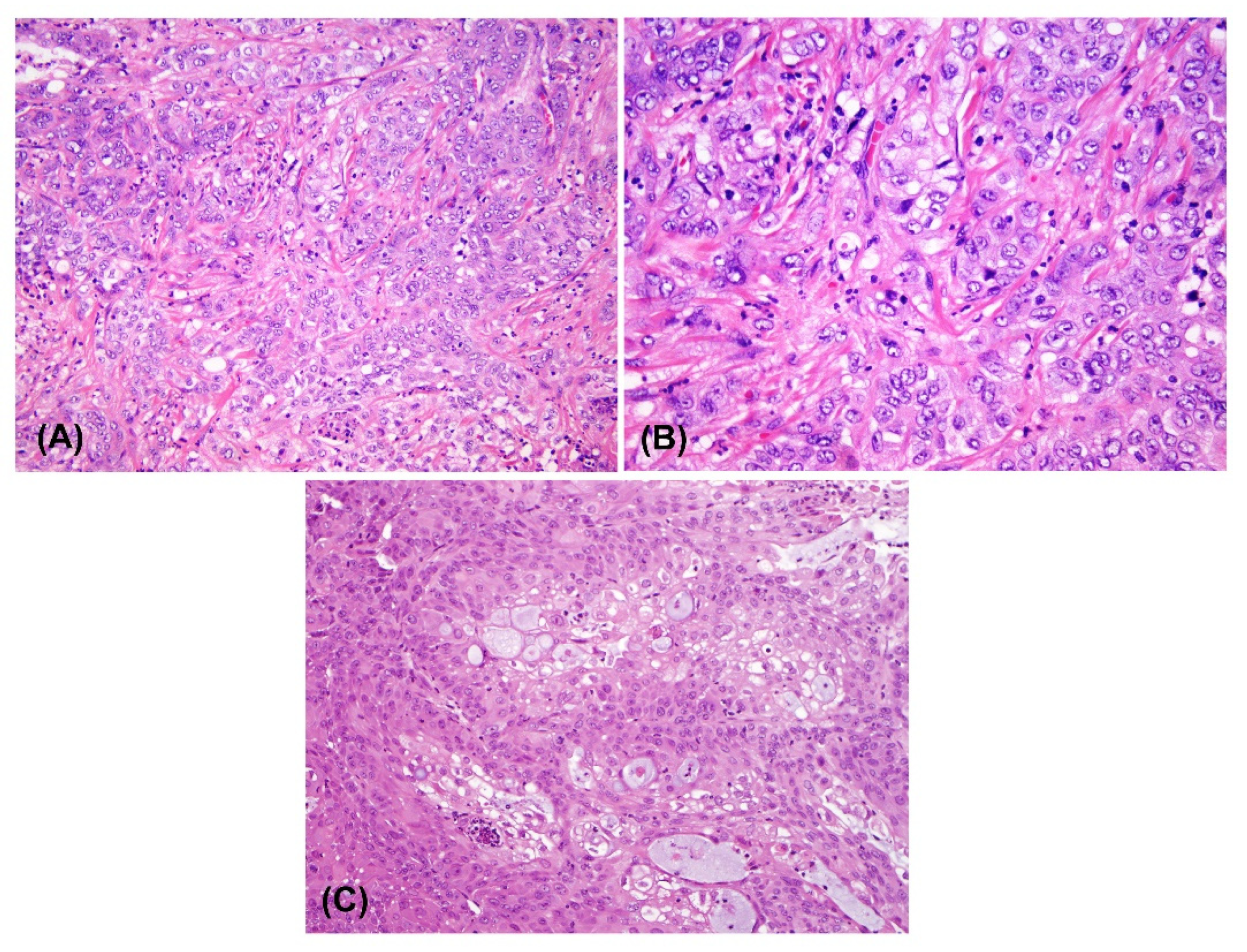
3.2. Morphological Analysis and Population Doubling Time
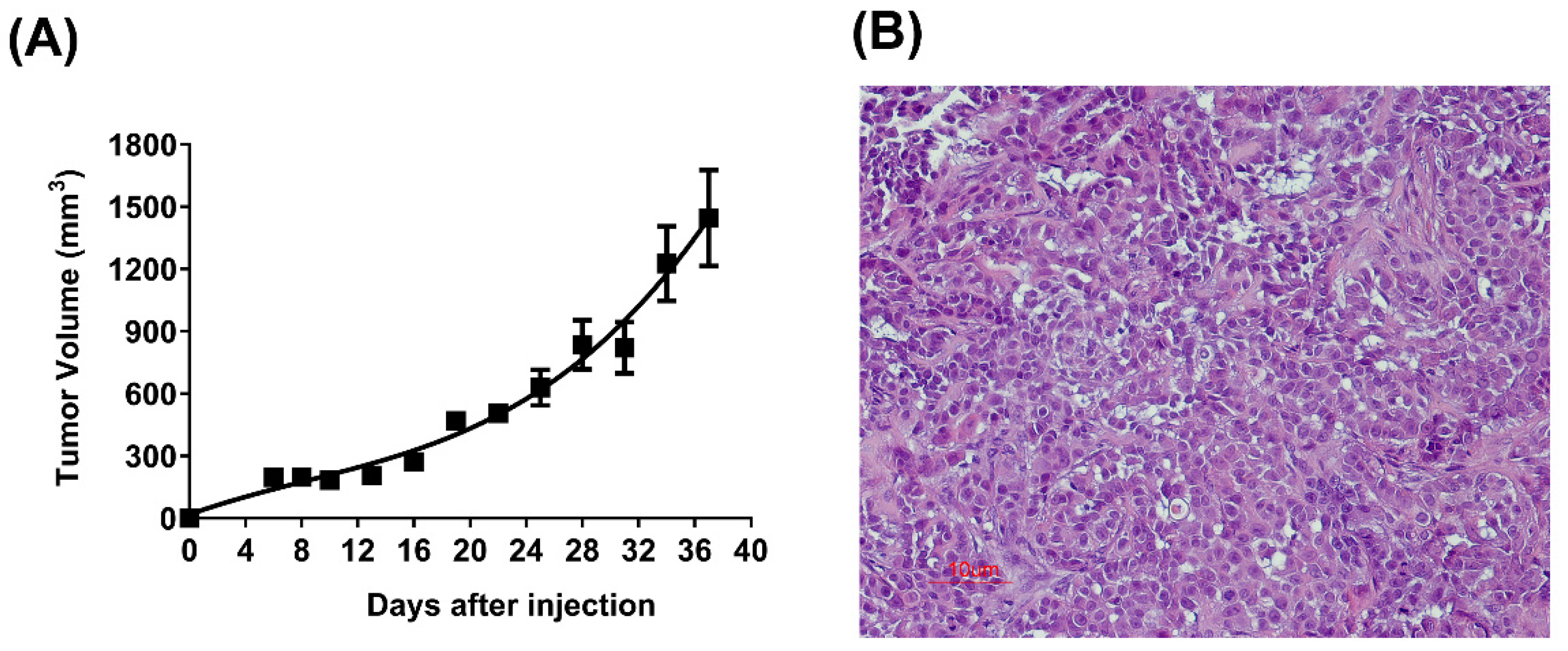
3.3. Tumorigenicity in Nude Mice
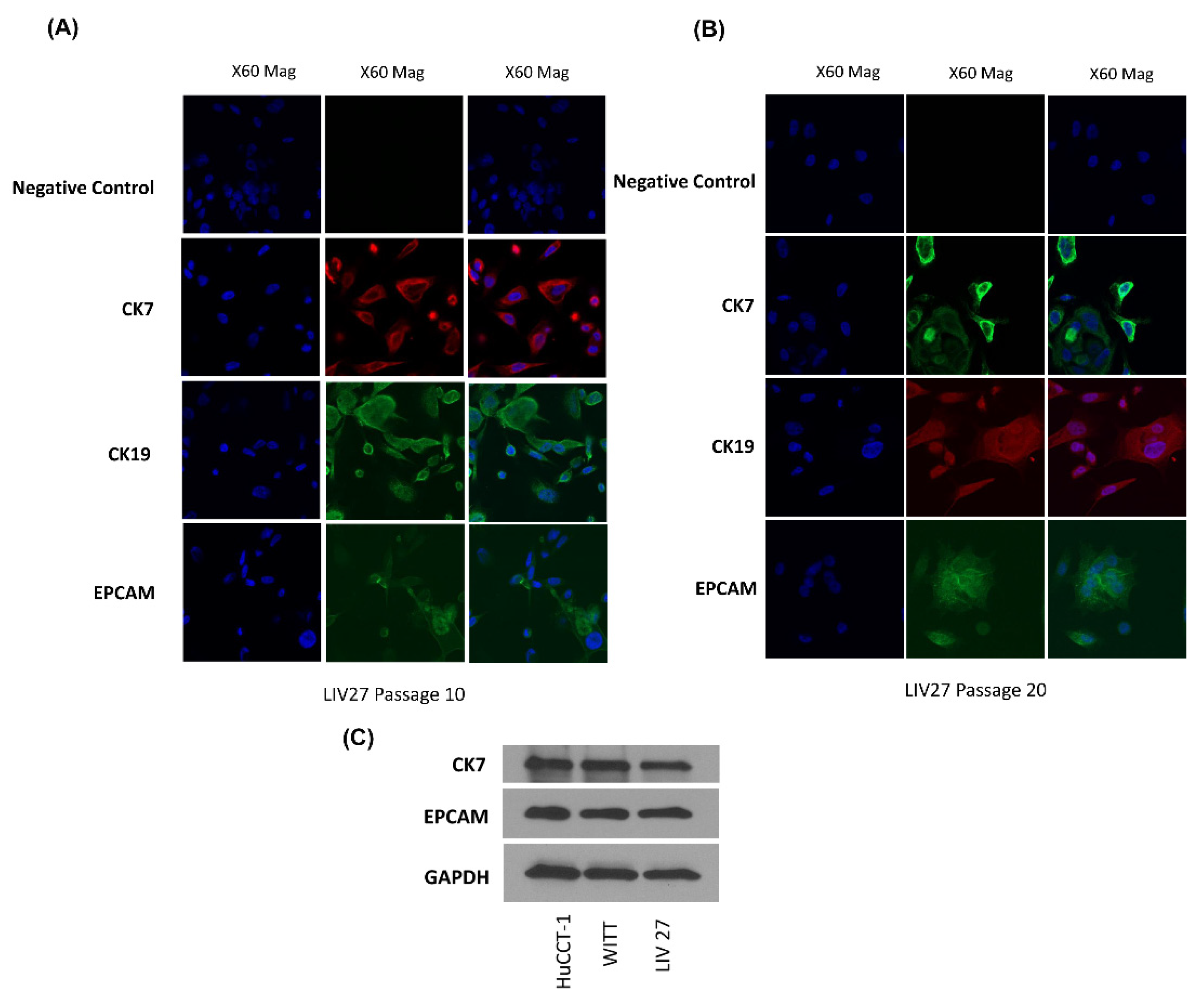
3.4. Expression of Biliary Marker
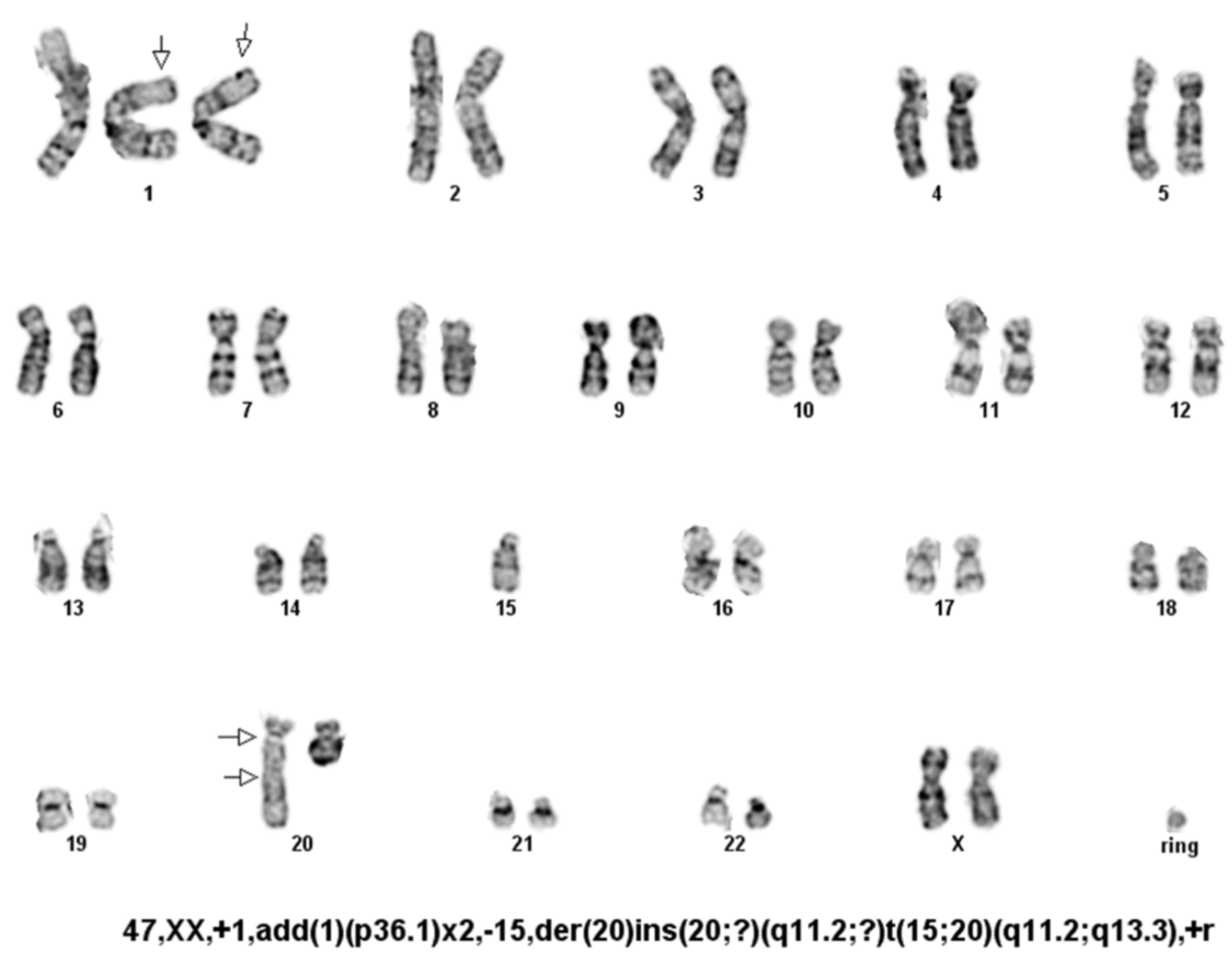
3.5. Karyotype Analysis
3.6. STR Analysis
3.7. Mycoplasma Detection
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Razumilava, N.; Gores, G.J. Cholangiocarcinoma. Lancet 2014, 383, 2168–2179. [Google Scholar] [CrossRef]
- Prueksapanich, P.; Piyachaturawat, P.; Aumpansub, P.; Ridtitid, W.; Chaiteerakij, R.; Rerknimitr, R. Liver Fluke-Associated Biliary Tract Cancer. Gut Liver 2018, 12, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Banales, J.M.; Marin, J.J.G.; Lamarca, A.; Rodriguez, P.M.; Khan, S.A.; Roberts, L.R.; Cardinale, V.; Carpino, G.; Andersen, J.B.; Braconi, C.; et al. Cholangiocarcinoma 2020: The next horizon in mechanisms and management. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 557–588. [Google Scholar] [CrossRef]
- Buranarom, A.; Navasumrit, P.; Ngaotepprutaram, T.; Ruchirawat, M. Dichloromethane increases mutagenic DNA damage and transformation ability in cholangiocytes and enhances metastatic potential in cholangiocarcinoma cell lines. Chem. Biol. Interact 2021, 346, 109580. [Google Scholar] [CrossRef] [PubMed]
- von Hahn, T.; Ciesek, S.; Wegener, G.; Plentz, R.R.; Weismuller, T.J.; Wedemeyer, H.; Manns, M.P.; Greten, T.F.; Malek, N.P. Epidemiological trends in incidence and mortality of hepatobiliary cancers in Germany. Scand. J. Gastroenterol. 2011, 46, 1092–1098. [Google Scholar] [CrossRef]
- Yang, J.D.; Kim, B.; Sanderson, S.O.; Sauver, J.S.; Yawn, B.P.; Larson, J.J.; Therneau, T.M.; Roberts, L.R.; Gores, G.J.; Kim, W.R. Biliary tract cancers in Olmsted County, Minnesota, 1976–2008. Am. J. Gastroenterol. 2012, 107, 1256–1262. [Google Scholar] [CrossRef]
- Pinter, M.; Hucke, F.; Zielonke, N.; Waldhor, T.; Trauner, M.; Peck-Radosavljevic, M.; Sieghart, W. Incidence and mortality trends for biliary tract cancers in Austria. Liver Int. 2014, 34, 1102–1108. [Google Scholar] [CrossRef]
- Saha, S.K.; Zhu, A.X.; Fuchs, C.S.; Brooks, G.A. Forty-Year Trends in Cholangiocarcinoma Incidence in the U.S.: Intrahepatic Disease on the Rise. Oncologist 2016, 21, 594–599. [Google Scholar] [CrossRef]
- Brindley, P.J.; Bachini, M.; Ilyas, S.I.; Khan, S.A.; Loukas, A.; Sirica, A.E.; Teh, B.T.; Wongkham, S.; Gores, G.J. Cholangiocarcinoma. Nat. Rev. Dis. Primers 2021, 9, 65. [Google Scholar] [CrossRef] [PubMed]
- Borad, M.J.; Champion, M.D.; Egan, J.B.; Liang, W.S.; Fonseca, R.; Bryce, A.H.; McCullough, A.E.; Barrett, M.T.; Hunt, K.; Patel, M.D.; et al. Integrated genomic characterization reveals novel, therapeutically relevant drug targets in FGFR and EGFR pathways in sporadic intrahepatic cholangiocarcinoma. PLoS Genet. 2014, 10, e1004135. [Google Scholar] [CrossRef] [PubMed]
- Jusakul, A.; Cutcutache, I.; Yong, C.H.; Lim, J.Q.; Huang, M.N.; Padmanabhan, N.; Nellore, V.; Kongpetch, S.; Ng, A.; Ng, L.M.; et al. Whole-Genome and Epigenomic Landscapes of Etiologically Distinct Subtypes of Cholangiocarcinoma. Cancer Discov. 2017, 7, 1116–1135. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, S.; Khan, S.A.; Hallemeier, C.L.; Kelley, R.K.; Gores, G.J. Cholangiocarcinoma—Evolving concepts and therapeutic strategies. Nat. Rev. Clin. Oncol. 2017, 15, 95–111. [Google Scholar] [CrossRef] [PubMed]
- Javle, M.; Roychowdhury, S.; Kelley, R.K.; Sadeghi, S.; Macarulla, T.; Weiss, K.H.; Waldschmidt, D.T.; Goyal, L.; Borbath, I.; El-Khoueiry, A.; et al. Infigratinib (BGJ398) in previously treated patients with advanced or metastatic cholangiocarcinoma with FGFR2 fusions or rearrangements: Mature results from a multicentre, open-label, single-arm, phase 2 study. Lancet Gastroenterol. Hepatol. 2021, 6, 803–815. [Google Scholar] [CrossRef]
- Javle, M.; Lowery, M.; Shroff, R.T.; Weiss, K.H.; Springfeld, C.; Borad, M.J.; Ramanathan, R.K.; Goyal, L.; Sadeghi, S.; Macarulla, T.; et al. Phase II Study of BGJ398 in Patients with FGFR-Altered Advanced Cholangiocarcinoma. J. Clin. Oncol. 2018, 36, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Makawita, S.K.; Abou-Alfa, G.; Roychowdhury, S.; Sadeghi, S.; Borbath, I.; Goyal, L.; Cohn, A.; Lamarca, A.; Oh, D.Y.; Macarulla, T.T.; et al. Infigratinib in patients with advanced cholangiocarcinoma with FGFR2 gene fusions/translocations: The PROOF 301 trial. Future Oncol. 2020, 16, 2375–2384. [Google Scholar] [CrossRef] [PubMed]
- Golub, D.; Iyengar, N.; Dogra, S.; Wong, T.; Bready, D.; Tang, K.; Modrek, A.S.; Placantonakis, D.G. Mutant Isocitrate Dehydrogenase Inhibitors as Targeted Cancer Therapeutics. Front. Oncol. 2019, 9, 417. [Google Scholar] [CrossRef]
- Mertens, J.C.; Rizvi, S.; Gores, G.J. Targeting cholangiocarcinoma. Biochim. Biophys. Acta Mol. Basis Dis. 2018, 1864 (4 Pt B), 1454–1460. [Google Scholar] [CrossRef]
- Kelley, R.K.; Bridgewater, J.; Gores, G.J.; Zhu, A.X. Systemic therapies for intrahepatic cholangiocarcinoma. J. Hepatol. 2020, 72, 353–363. [Google Scholar] [CrossRef]
- Gossard, A.A.; Gores, G.J. Primary Sclerosing Cholangitis: What the Gastroenterologist and Hepatologist Needs to Know. Clin. Liver Dis. 2017, 21, 725–737. [Google Scholar] [CrossRef]
- Horsley-Silva, J.L.; Rodriguez, E.A.; Franco, D.L.; Lindor, K.D. An update on cancer risk and surveillance in primary sclerosing cholangitis. Liver Int. 2017, 37, 1103–1109. [Google Scholar] [CrossRef]
- Rizvi, S.; Eaton, J.E.; Gores, G.J. Primary Sclerosing Cholangitis as a Premalignant Biliary Tract Disease: Surveillance and Management. Clin. Gastroenterol. Hepatol. 2015, 13, 2152–2165. [Google Scholar] [CrossRef]
- Ma, S.; Hu, L.; Huang, X.H.; Cao, L.Q.; Chan, K.W.; Wang, Q.; Guan, X.Y. Establishment and characterization of a human cholangiocarcinoma cell line. Oncol. Rep. 2007, 18, 1195–1200. [Google Scholar]
- Ku, J.L.; Yoon, K.A.; Kim, I.J.; Kim, W.H.; Jang, J.Y.; Suh, K.S.; Kim, S.W.; Park, Y.H.; Hwang, J.H.; Yoon, Y.B.; et al. Establishment and characterisation of six human biliary tract cancer cell lines. Br. J. Cancer 2002, 87, 187–193. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saijyo, S.; Kudo, T.; Suzuki, M.; Katayose, Y.; Shinoda, M.; Muto, T.; Fukuhara, K.; Suzuki, T.; Matsuno, S. Establishment of a new extrahepatic bile duct carcinoma cell line, TFK-1. Tohoku J. Exp. Med 1995, 177, 61–71. [Google Scholar] [CrossRef]
- Knuth, A.; Gabbert, H.; Dippold, W.; Klein, O.; Sachsse, W.; Bitter-Suermann, D.; Prellwitz, W.; Meyer zum Büschenfelde, K.H. Biliary adenocarcinoma. Characterisation of three new human tumor cell lines. J. Hepatol. 1985, 1, 579–596. [Google Scholar] [CrossRef]
- Yano, H.; Maruiwa, M.; Iemura, A.; Mizoguchi, A.; Kojiro, M. Establishment and characterization of a new human extrahepatic bile duct carcinoma cell line (KMBC). Cancer 1992, 69, 1664–1673. [Google Scholar] [CrossRef]
- Miyagiwa, M.; Ichida, T.; Tokiwa, T.; Sato, J.; Sasaki, H. A new human cholangiocellular carcinoma cell line (HuCC-T1) producing carbohydrate antigen 19/9 in serum-free medium. In Vitro Cell Dev. Biol. 1989, 25, 503–510. [Google Scholar] [CrossRef]
- Zhang, Y.; Luo, J.; Dong, X.; Yang, F.; Zhang, M.; Zhao, J.; Wang, Q.; Zhou, F.; Sun, J.; Yang, X. Establishment and Characterization of Two Novel Cholangiocarcinoma Cell Lines. Ann. Surg. Oncol. 2019, 26, 4134–4147. [Google Scholar] [CrossRef]
- Shimizu, Y.; Demetris, A.J.; Gollin, S.M.; Storto, P.D.; Bedford, H.M.; Altarac, S.; Iwatsuki, S.; Herberman, R.B.; Whiteside, T.L. Two new human cholangiocarcinoma cell lines and their cytogenetics and responses to growth factors, hormones, cytokines or immunologic effector cells. Int. J. Cancer 1992, 52, 252–260. [Google Scholar] [CrossRef]
- Jiao, W.; Yakushiji, H.; Kitajima, Y.; Ogawa, A.; Miyazaki, K. Establishment and characterization of human hilar bile duct carcinoma cell line and cell strain. J. Hepato-Biliary-Pancreat Surg. 2000, 7, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, N.; Morioka, H.; Ohkura, H.; Hirohashi, S.; Kawai, K. Establishment and characterization of the human cholangiocarcinoma cell line HChol-Y1 in a serum-free, chemically defined medium. J. Natl. Cancer Inst. 1985, 75, 29–35. [Google Scholar]
- Kusaka, Y.; Tokiwa, T.; Sato, J. Establishment and characterization of a cell line from a human cholangiocellular carcinoma. Res. Exp. Med. 1988, 188, 367–375. [Google Scholar] [CrossRef]
- Sripa, B.; Leungwattanawanit, S.; Nitta, T.; Wongkham, C.; Bhudhisawasdi, V.; Puapairoj, A.; Sripa, C.; Miwa, M. Establishment and characterization of an opisthorchiasis-associated cholangiocarcinoma cell line (KKU-100). World J. Gastroenterol. 2005, 11, 3392–3397. [Google Scholar] [CrossRef]
- Huang, Y.; Liu, Y.; Zheng, C.; Shen, C. Investigation of Cross-Contamination and Misidentification of 278 Widely Used Tumor Cell Lines. PLoS ONE 2017, 12, e0170384. [Google Scholar] [CrossRef]
- Masters, J.R.; Thomson, J.A.; Daly-Burns, B.; Reid, Y.A.; Dirks, W.G.; Packer, P.; Toji, L.H.; Ohno, T.; Tanabe, H.; Arlett, C.F.; et al. Short tandem repeat profiling provides an international reference standard for human cell lines. Proc. Natl. Acad. Sci. USA 2001, 98, 8012–8017. [Google Scholar] [CrossRef]
- Zakharia, K.; Miyabe, K.; Wang, Y.; Wu, D.; Moser, C.D.; Borad, M.J.; Roberts, L.R. Preclinical In Vitro and In Vivo Evidence of an Antitumor Effect of CX-4945, a Casein Kinase II Inhibitor, in Cholangiocarcinoma. Transl. Oncol. 2019, 12, 143–153. [Google Scholar] [CrossRef]
- Ding, X.; Chaiteerakij, R.; Moser, C.D.; Shaleh, H.; Boakye, J.; Chen, G.; Ndzengue, A.; Li, Y.; Zhou, Y.; Huang, S.; et al. Antitumor effect of the novel sphingosine kinase 2 inhibitor ABC294640 is enhanced by inhibition of autophagy and by sorafenib in human cholangiocarcinoma cells. Oncotarget 2016, 7, 20080–20092. [Google Scholar] [CrossRef] [PubMed]

| STR Locus | LIV27 Cell Line |
|---|---|
| TH01 | 9; 9.3 |
| D21S11 | 29 |
| D5S818 | 13 |
| D13S317 | 11; 13 |
| D7S820 | 8; 14 |
| D16S539 | 8; 12 |
| CSF1PO | 10; 12 |
| AMEL | X |
| vWA | 14; 19 |
| TPOX | 8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ding, X.; Zakharia, K.; Moser, C.D.; Campbell, N.A.; Hu, C.; Razumilava, N.; Chaiteerakij, R.; Shaleh, H.M.; Greipp, P.T.; Graham, R.P.; et al. Establishment and Characterization of a New Human Intrahepatic Cholangiocarcinoma Cell Line LIV27. Cancers 2022, 14, 5080. https://doi.org/10.3390/cancers14205080
Ding X, Zakharia K, Moser CD, Campbell NA, Hu C, Razumilava N, Chaiteerakij R, Shaleh HM, Greipp PT, Graham RP, et al. Establishment and Characterization of a New Human Intrahepatic Cholangiocarcinoma Cell Line LIV27. Cancers. 2022; 14(20):5080. https://doi.org/10.3390/cancers14205080
Chicago/Turabian StyleDing, Xiwei, Kais Zakharia, Catherine D. Moser, Nellie A. Campbell, Chunling Hu, Nataliya Razumilava, Roongruedee Chaiteerakij, Hassan M. Shaleh, Patricia T. Greipp, Rondell P. Graham, and et al. 2022. "Establishment and Characterization of a New Human Intrahepatic Cholangiocarcinoma Cell Line LIV27" Cancers 14, no. 20: 5080. https://doi.org/10.3390/cancers14205080
APA StyleDing, X., Zakharia, K., Moser, C. D., Campbell, N. A., Hu, C., Razumilava, N., Chaiteerakij, R., Shaleh, H. M., Greipp, P. T., Graham, R. P., Zou, X., Chandan, V. S., & Roberts, L. R. (2022). Establishment and Characterization of a New Human Intrahepatic Cholangiocarcinoma Cell Line LIV27. Cancers, 14(20), 5080. https://doi.org/10.3390/cancers14205080









