Quantitative Analysis of SPECT-CT Data in Metastatic Breast Cancer Patients—The Clinical Significance
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
- ○
- breast carcinoma confirmed through biopsy in different clinical scenarios: initial staging in symptomatic patients or initial staging for patients with clinical stage III and IV, restaging for patients with new bone pain or increase in alkaline phosphatase level, and restaging for nonosseous recurrence [26]
- ○
- availability of the data regarding the time of injection, the injected activity, residual activity measurement, and time of the acquisition
- ○
- access to the patient’s medical history
- ○
- at least one metastatic and degenerative lesion in the SPECT-CT field of view (FOV)
2.2. Image Acquisition and Reconstruction
2.3. Image Interpretation and Quantitative Assessment
2.4. SUV Calculation
- SUVlbm = (SPECT image Pixels uptake (Bqml)) × units g/mL
- for males: LBM in kg = 1.10 × (weight in kg) − 120 × [
- for females: LBM in kg = 1.07 × (weight in kg) − 148 × [
- actual activity = decay scan × decay1 × (measure activity − (decay2 × post-injection activity))
- λ= 0.693 ÷ half lifetime
- decay1 = exp (λ × (measured time − administered time))
- decay2 = exp (λ × (post-injection time − measured time))
- decay scan (injection-scan time) = exp (λ × (administered time-scan time))
- LBM in kg = calculated using the dedicated formula for each gender
- measure activity = pre-injection activity
- measured time = pre-injection time [30]
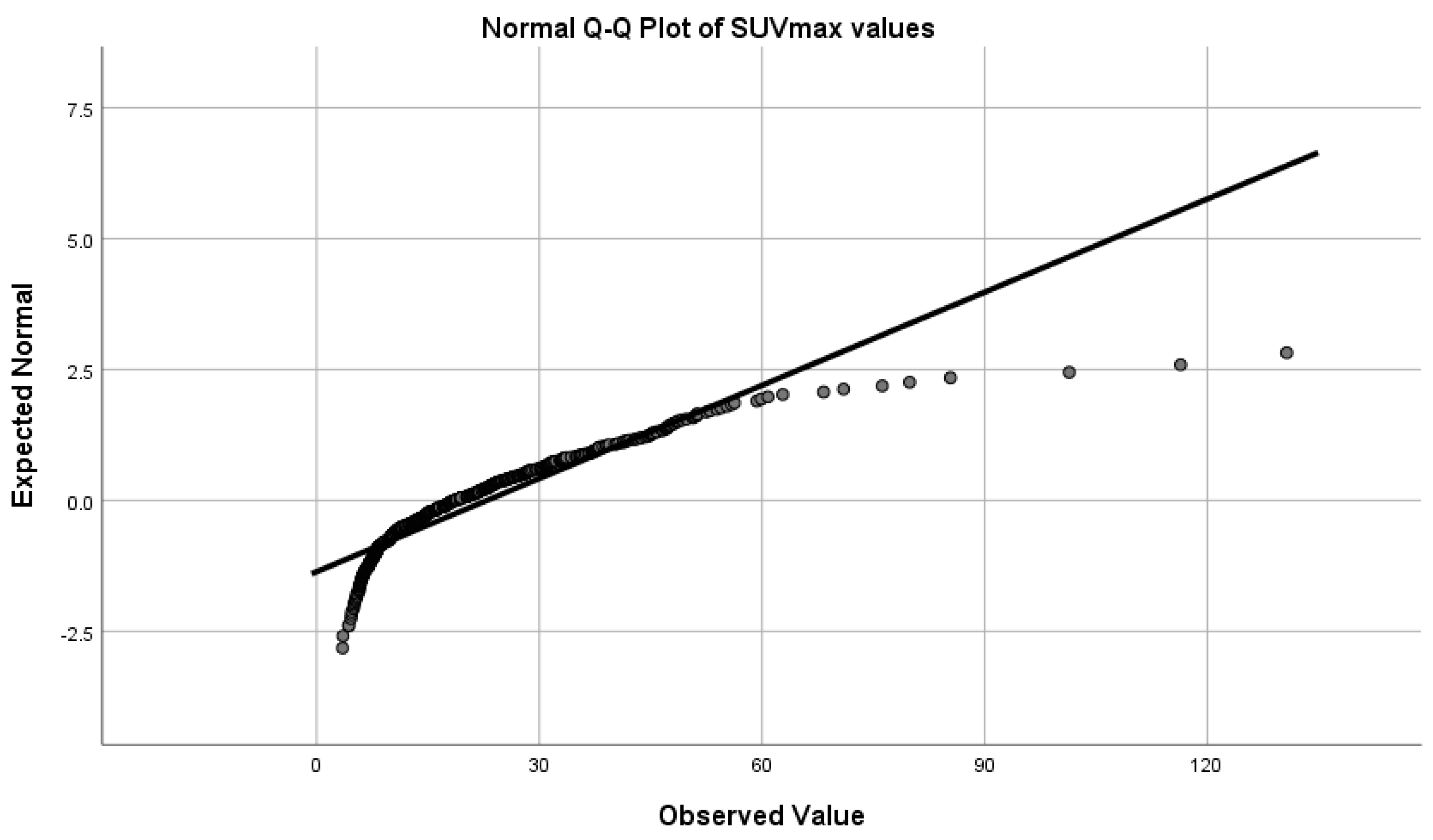
2.5. Statistical Analysis of the Data
3. Results
3.1. Lesions Distribution
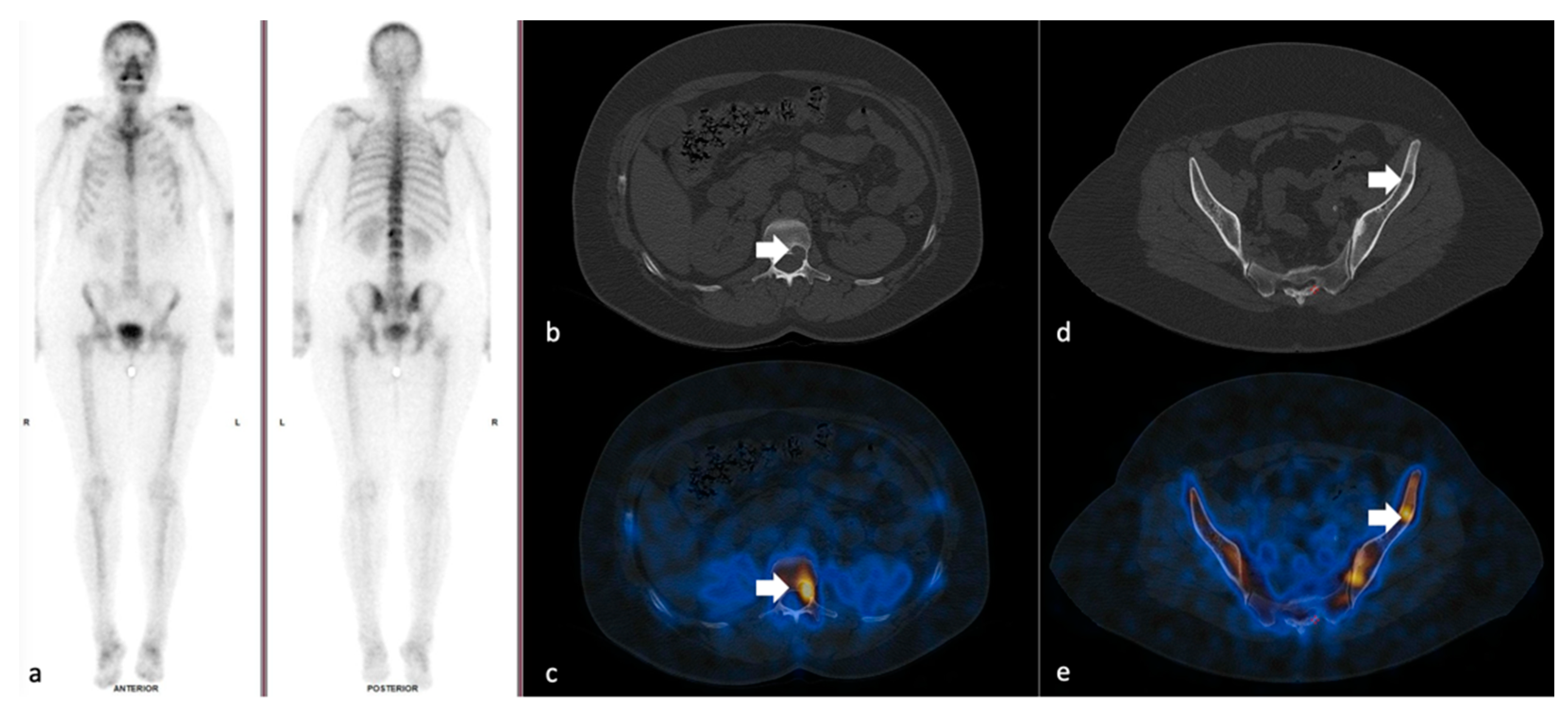
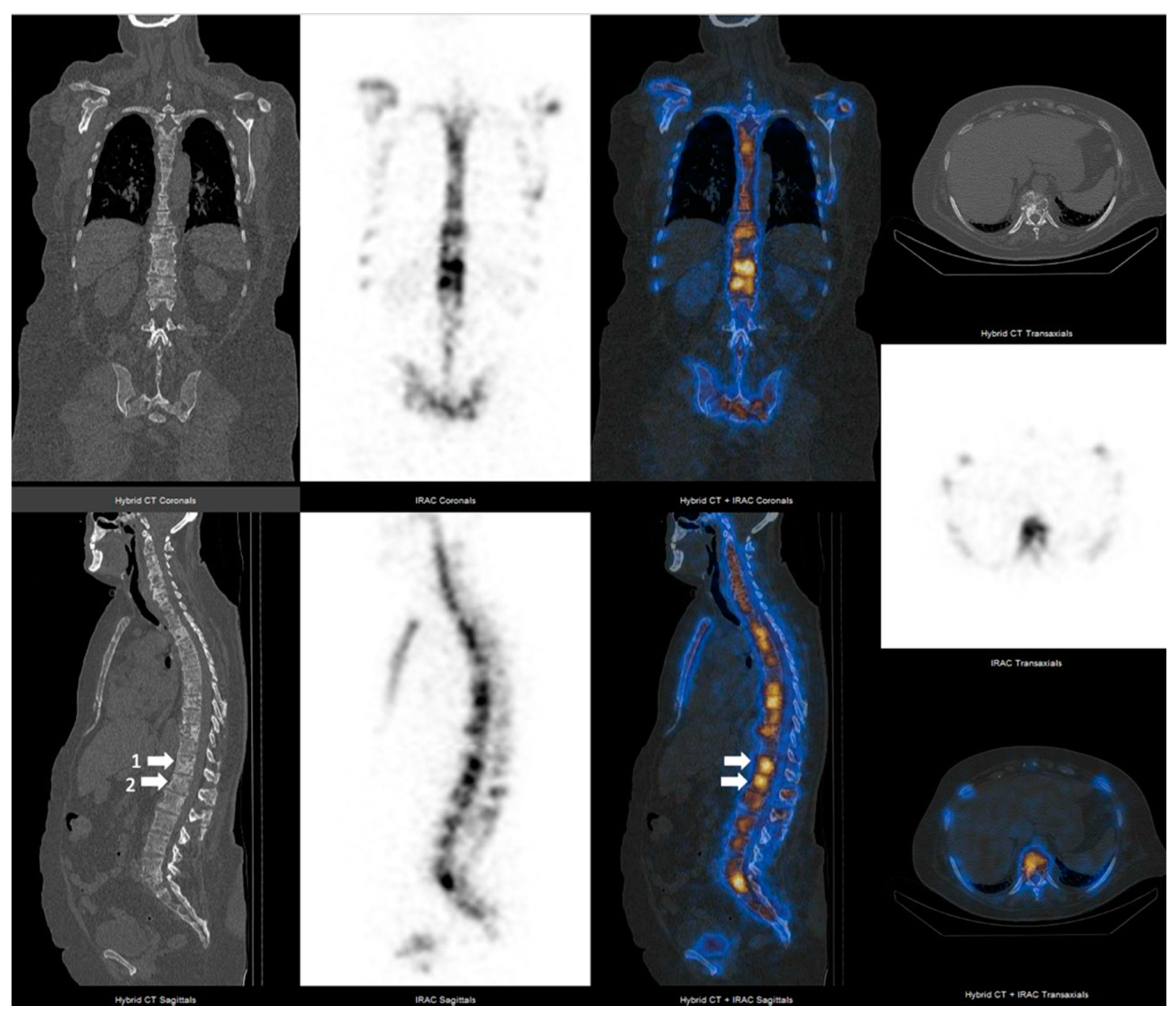
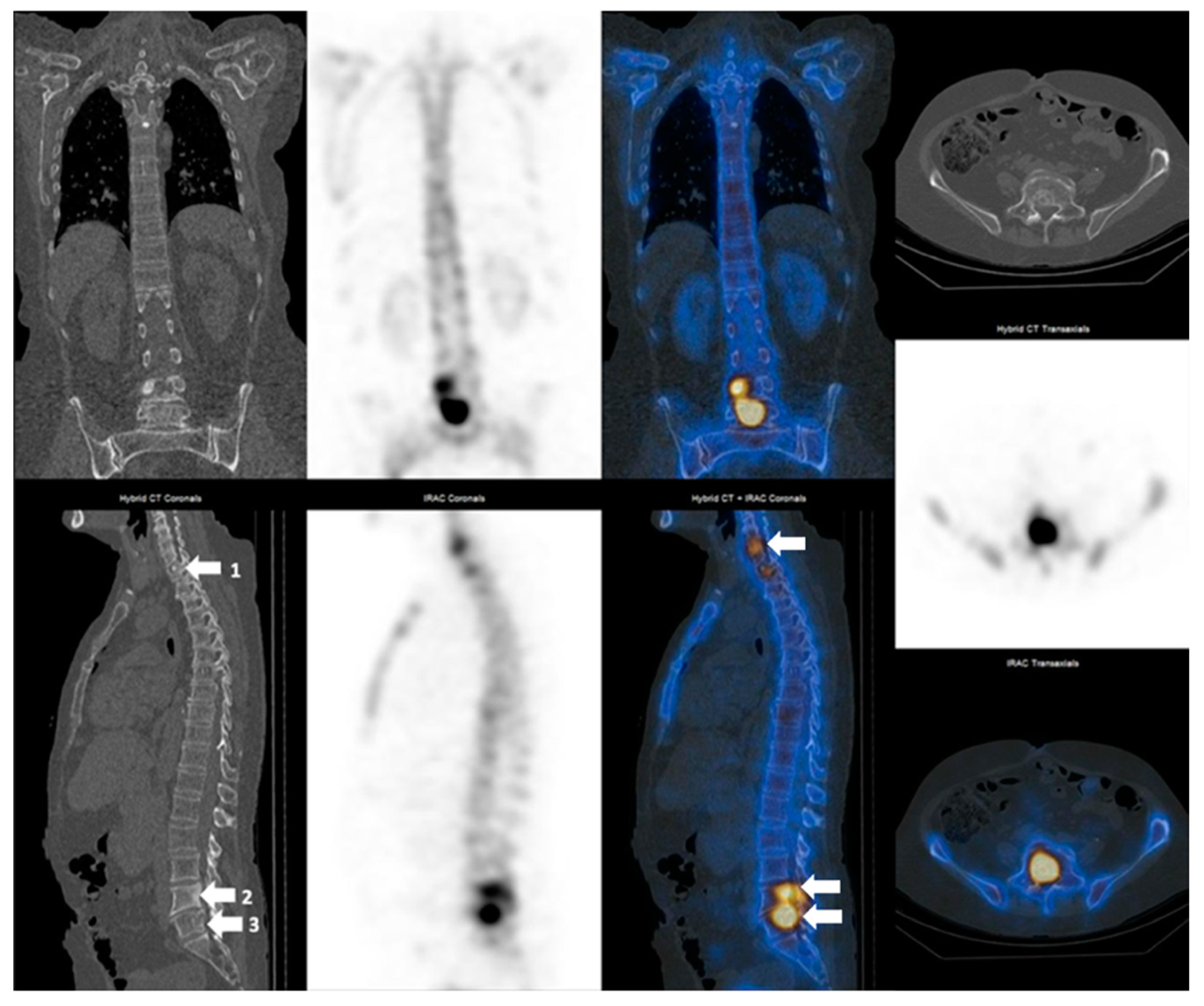
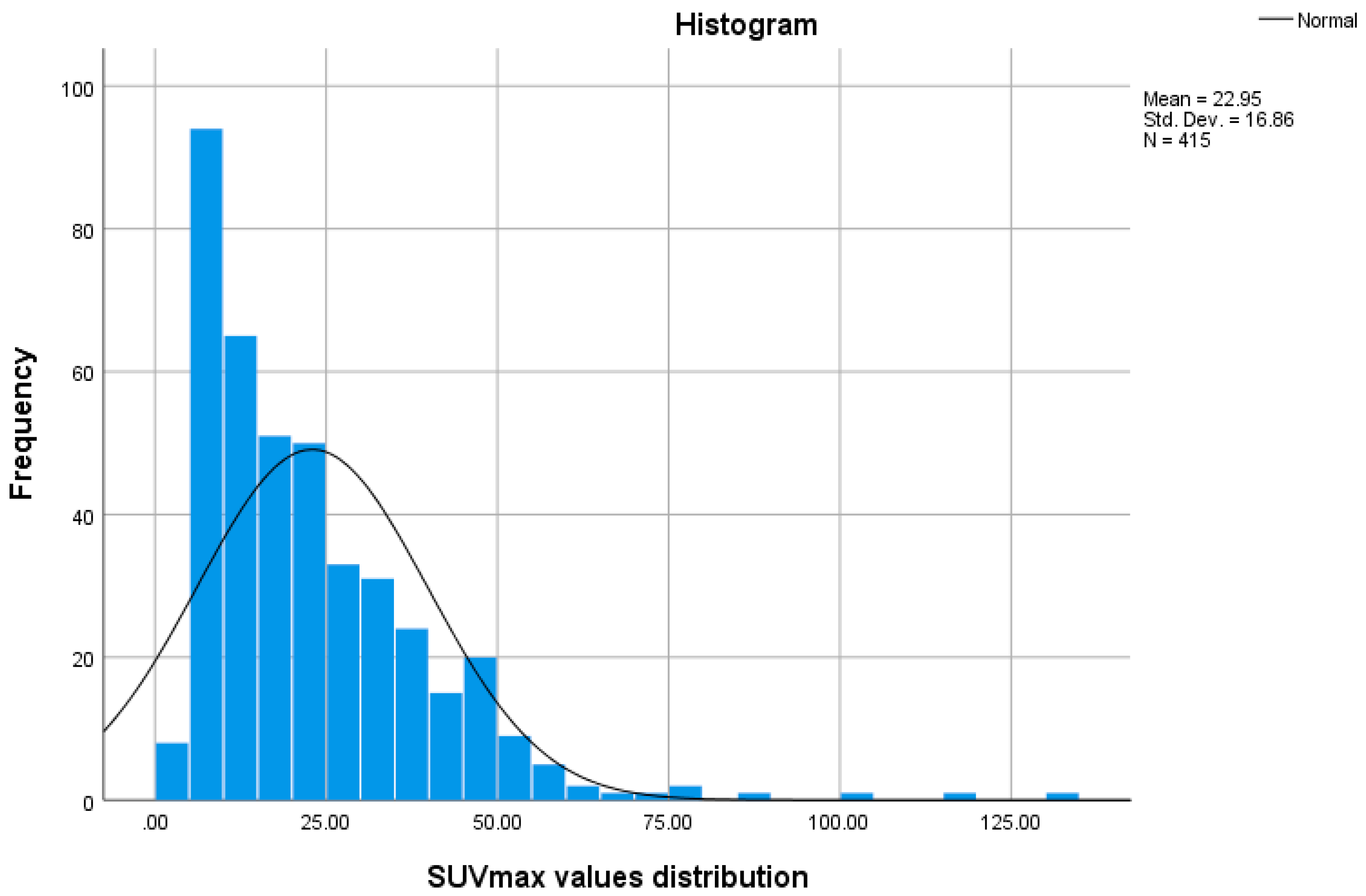
3.2. SPECT-CT SUVmax in Metastatic Lesions and Degenerative Bone Disease
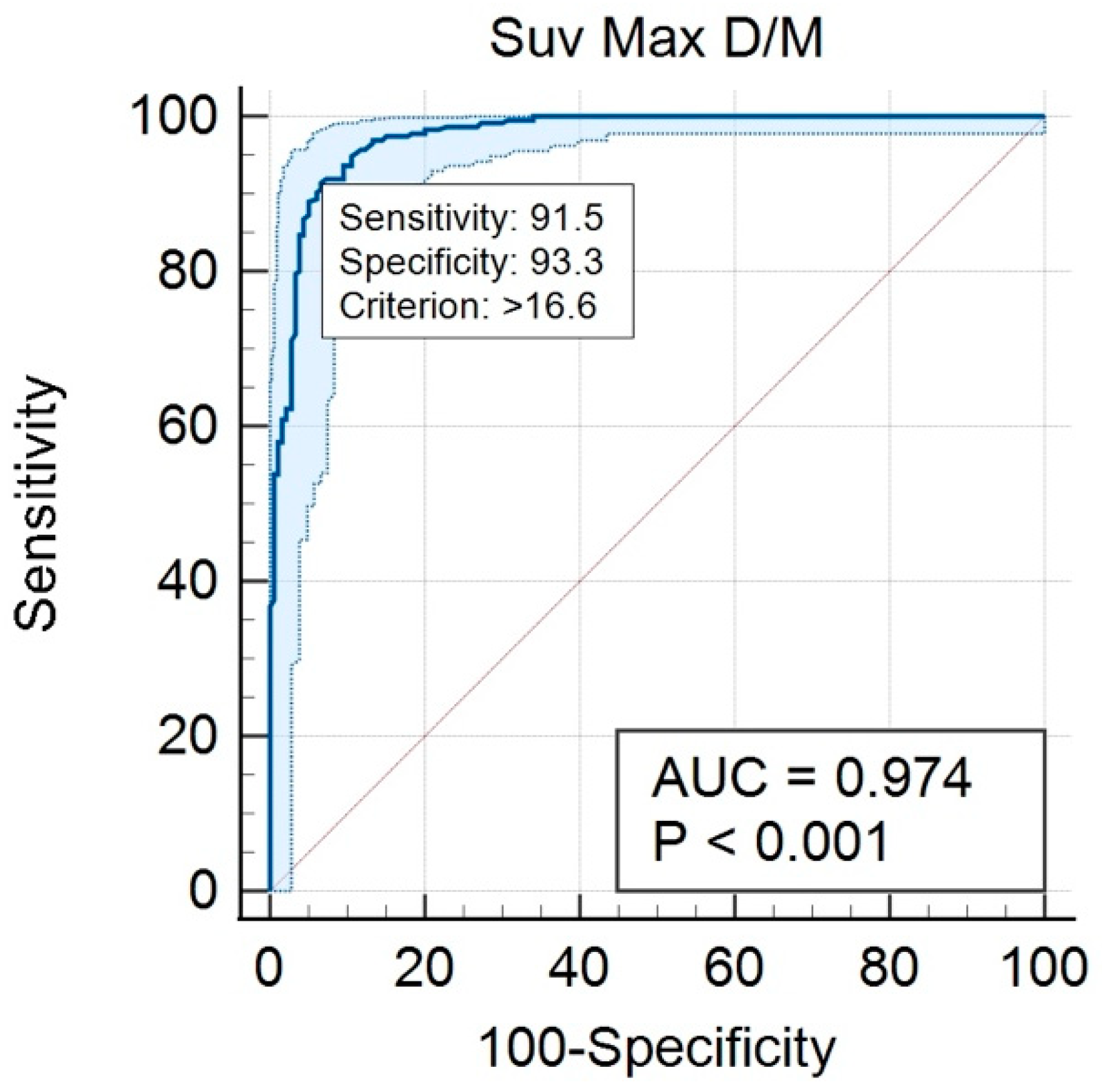
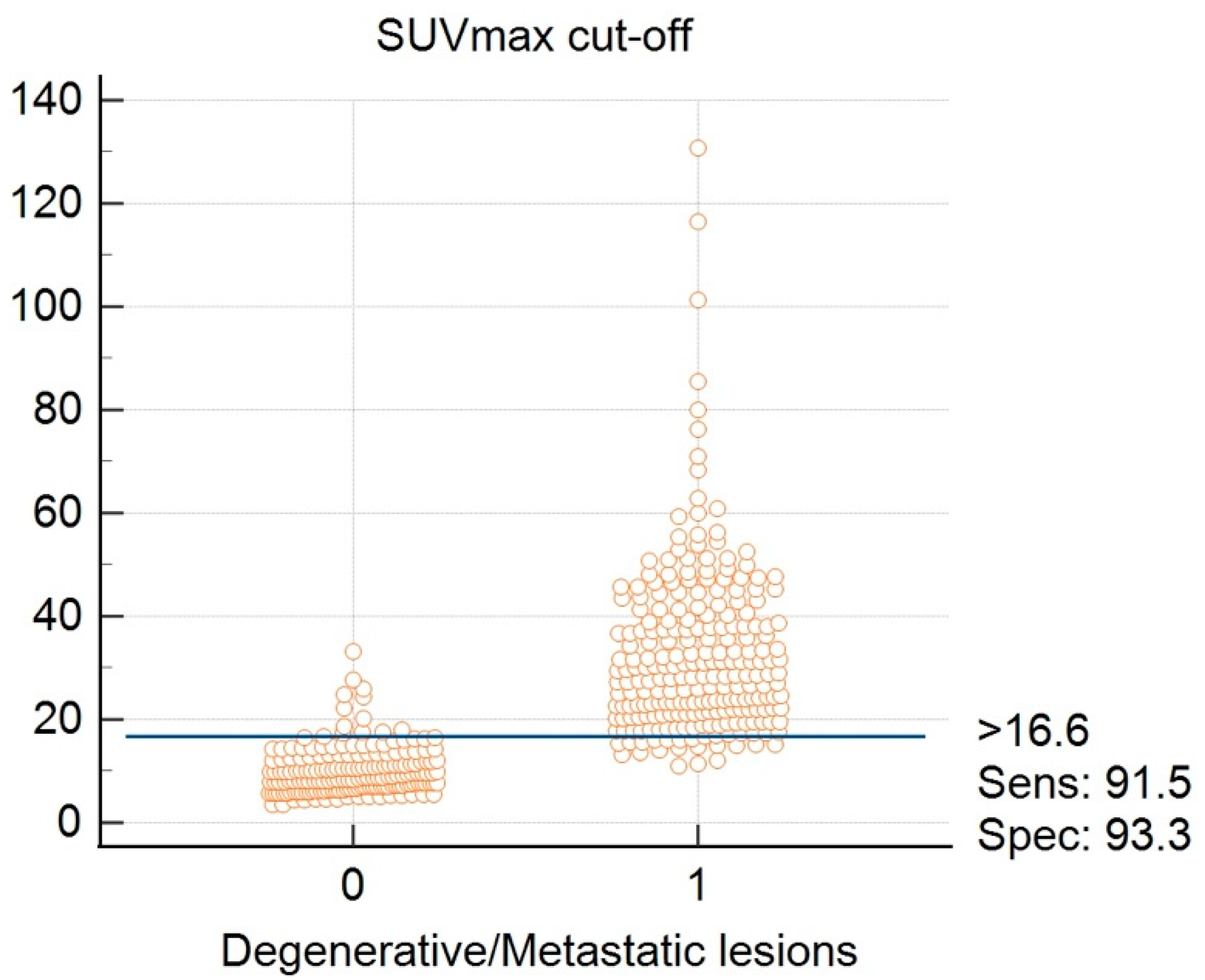
3.3. SUVmax Cutt-off Value in Differentiating between Degenerative and Metastatic Lesions
3.4. SUVmax Overlapping
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GLOBOCAN 2020 Cancer Data. Available online: https://gco.iarc.fr/today/data/factsheets/populations/900-world-fact-sheets.pdf (accessed on 11 December 2021).
- Huang, J.-F.; Shen, J.; Li, X.; Rengan, R.; Silvestris, N.; Wang, M.; DeRosa, L.; Zheng, X.; Belli, A.; Zhang, X.-L.; et al. Incidence of patients with bone metastases at diagnosis of solid tumors in adults: A large population-based study. Ann. Transl. Med. 2020, 8, 482. [Google Scholar] [CrossRef]
- Kuchuk, I.; Hutton, B.; Moretto, P.; Ng, T.; Addison, C.; Clemons, M. Incidence, consequences and treatment of bone metastases in breast cancer patients—Experience from a single cancer centre. J. Bone Oncol. 2013, 2, 137–144. [Google Scholar] [CrossRef] [Green Version]
- Coleman, R.E. THE NATURE OF BONE METASTASES Metastatic bone disease: Clinical features, pathophysiology and treatment strategies. Reviews 2001, 27, 165–176. [Google Scholar] [CrossRef]
- Voinea, S.; Sandru, A.; Gherghe, M.; Blidaru, A. Peculiarities of lymphatic drainage in cutaneous malignant melanoma: Clinical experience in 75 cases. Chirurgia 2014, 109, 26–33. [Google Scholar] [PubMed]
- Gherghe, M.; Bordea, C.; Blidaru, A. Clinical significance of the lymphoscintigraphy in the evaluation of non-axillary sentinel lymph node localization in breast cancer. Chirurgia 2015, 110, 26–32. [Google Scholar]
- Fang, J.; Xu, Q. Differences of osteoblastic bone metastases and osteolytic bone metastases in clinical features and molecular characteristics. Clin. Transl. Oncol. 2014, 17, 173–179. [Google Scholar] [CrossRef]
- Zaidi, H. Quantum Analysis in Nuclear Medicine Imaging; Springer: Berlin/Heidelberg, Germany, 2005. [Google Scholar]
- Bailey, D.L.; Willowson, K.P. An Evidence-Based Review of Quantitative SPECT Imaging and Potential Clinical Applications. J. Nucl. Med. 2013, 54, 83–89. [Google Scholar] [CrossRef] [Green Version]
- Cachovan, M.; Vija, A.H.; Hornegger, J.; Kuwert, T. Quantification of 99mTc-DPD concentration in the lumbar spine with SPECT/CT. EJNMMI Res. 2013, 3, 45. [Google Scholar] [CrossRef] [Green Version]
- Patton, J.A.; Turkington, T.G. SPECT/CT Physical Principles and Attenuation Correction. J. Nucl. Med. Technol. 2008, 36, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Voinea, S.; Sandru, A.; Gherghe, M. Pitfalls in Cutaneous Melanoma Lymphatic Drainage. Chirurgia 2016, 111, 87–89. [Google Scholar] [PubMed]
- Seo, Y.; Mari, C.; Hasegawa, B.H. Technological Development and Advances in Single-Photon Emission Computed Tomography/Computed Tomography. Semin. Nucl. Med. 2008, 38, 177–198. [Google Scholar] [CrossRef] [Green Version]
- Hicks, R.J.; Hofman, M. Is there still a role for SPECT–CT in oncology in the PET–CT era? Nat. Rev. Clin. Oncol. 2012, 9, 712–720. [Google Scholar] [CrossRef]
- Bailey, D.L.; Willowson, K.P. Quantitative SPECT/CT: SPECT joins PET as a quantitative imaging modality. Eur. J. Nucl. Med. Mol. Imaging 2013, 41 (Suppl. S1), 17–25. [Google Scholar] [CrossRef]
- Ritt, P.; Vija, H.; Hornegger, J.; Kuwert, T. Absolute quantification in SPECT. Eur. J. Pediatr. 2011, 38, 69–77. [Google Scholar] [CrossRef]
- Heindel, W.; Gübitz, R.; Vieth, V.; Weckesser, M.; Schober, O.; Schäfers, M. The Diagnostic Imaging of Bone Metastases. Dtsch. Aerzteblatt Int. 2014, 111, 741–747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arvola, S.; Jambor, I.; Kuisma, A.; Kemppainen, J.; Kajander, S.; Seppänen, M.; Noponen, T. Comparison of standardized uptake values between 99mTc-HDP SPECT/CT and 18F-NaF PET/CT in bone metastases of breast and prostate cancer. EJNMMI Res. 2019, 9, 6. [Google Scholar] [CrossRef] [Green Version]
- Suh, M.S.; Lee, W.W.; Kim, Y.-K.; Yun, P.-Y.; Kim, S.E. Maximum Standardized Uptake Value of99mTc Hydroxymethylene Diphosphonate SPECT/CT for the Evaluation of Temporomandibular Joint Disorder. Radiology 2016, 280, 890–896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaneta, T.; Ogawa, M.; Daisaki, H.; Nawata, S.; Yoshida, K.; Inoue, T. SUV measurement of normal vertebrae using SPECT/CT with Tc-99m methylene diphosphonate. Am. J. Nucl. Med. Mol. Imaging 2016, 6, 262–268. [Google Scholar]
- Kuji, I.; Yamane, T.; Seto, A.; Yasumizu, Y.; Shirotake, S.; Oyama, M. Skeletal standardized uptake values obtained by quantitative SPECT/CT as an osteoblastic biomarker for the discrimination of active bone metastasis in prostate cancer. Eur. J. Hybrid Imaging 2017, 1, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beck, M.; Sanders, J.C.; Ritt, P.; Reinfelder, J.; Kuwert, T. Longitudinal analysis of bone metabolism using SPECT/CT and (99m)Tc-diphosphono-propanedicarboxylic acid: Comparison of visual and quantitative analysis. EJNMMI Res. 2016, 6, 60. [Google Scholar] [CrossRef] [Green Version]
- Ahmadzadehfar, H.; Marx, C.; Ebert, A.; Kreft, B.; Menschik, T.; Ko, Y.; Vorreuther, R.; Ezziddin, S.; Biersack, H.J.; Palmedo, H. Diagnostic accuracy of SPECT-CT in comparison to whole body scintigraphy and SPECT in patients with suspected osseous metastases: Results of a two center study. J. Nucl. Med. 2012, 53 (Suppl. 1), 336. [Google Scholar]
- Han, S.; Colville, D.; Ainslie-McLaren, G.; Lang, J.; Watt, S. Clinical impact of SPECT/CT bone scan in the assessment of bone metastases in breast cancer. J. Nucl. Med. 2010, 51 (Suppl. 2), 541. [Google Scholar]
- Pesapane, F.; Downey, K.; Rotili, A.; Cassano, E.; Koh, D.-M. Imaging diagnosis of metastatic breast cancer. Insights Into Imaging 2020, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Donohoe, K.J.; Cohen, E.J.; Giammarile, F.; Grady, E.; Greenspan, B.S.; E Henkin, R.; Millstine, J.; Smith, G.T.; Srinivas, S.; Kauffman, J.; et al. Appropriate Use Criteria for Bone Scintigraphy in Prostate and Breast Cancer: Summary and Excerpts. J. Nucl. Med. 2017, 58, 14N–17N. [Google Scholar]
- Even-Sapir, E.; Martin, R.H.; Barnes, D.C.; Pringle, C.R.; E Iles, S.; Mitchell, M.J. Role of SPECT in differentiating malignant from benign lesions in the lower thoracic and lumbar vertebrae. Radiology 1993, 187, 193–198. [Google Scholar] [CrossRef]
- Hetzel, M.; Arslandemir, C.; König, H.-H.; Buck, A.; Nüssle, K.; Glatting, G.; Gabelmann, A.; Hetzel, J.; Hombach, V.; Schirrmeister, H. F-18 NaF PET for Detection of Bone Metastases in Lung Cancer: Accuracy, Cost-Effectiveness, and Impact on Patient Management. J. Bone Miner. Res. 2003, 18, 2206–2214. [Google Scholar] [CrossRef]
- Schirrmeister, H.; Glatting, G.; Hetzel, J.; Nüssle, K.; Arslandemir, C.; Buck, A.; Dziuk, K.; Gabelmann, A.; Reske, S.N.; Hetzel, M. Prospective evaluation of the clinical value of planar bone scans, SPECT, and (18)F-labeled NaF PET in newly diagnosed lung cancer. J. Nucl. Med. 2001, 42, 1800–1804. [Google Scholar]
- Healthcare, G.E.; Metrix, Q. Quantitative SPECT SUV Results with Multi-Dimensional Organ and Lesion Characterization. 2014. Available online: www.gehealthcare.com (accessed on 22 February 2021).
- Tahara, R.K.; Brewer, T.M.; Theriault, R.L.; Ueno, N.T. Bone Metastasis of Breast Cancer. Free Radic. Diagn. Med. 2019, 1152, 105–129. [Google Scholar] [CrossRef]
- Rohani, M.F.M.; Nawi, N.M.; Shamim, S.E.; Sohaimi, W.F.W.; Zainon, W.M.N.W.; Musarudin, M.; Said, M.A.; Hashim, H. Maximum standardized uptake value from quantitative bone single-photon emission computed tomography/computed tomography in differentiating metastatic and degenerative joint disease of the spine in prostate cancer patients. Ann. Nucl. Med. 2019, 34, 39–48. [Google Scholar] [CrossRef]
- Davila, D.; Antoniou, A.; Chaudhry, M.A. Evaluation of Osseous Metastasis in Bone Scintigraphy. Semin. Nucl. Med. 2015, 45, 3–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarikaya, I.; Albatineh, A.N.; Sarikaya, A. Revisiting Weight-Normalized SUV and Lean-Body-Mass–Normalized SUV in PET Studies. J. Nucl. Med. Technol. 2019, 48, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, S.; Matsutake, Y.; Hashimoto, T.; Ikematsu, R.; Kawaji, Y.; Ideguchi, T.; Fukushima, S.; Hayabuchi, N. Study on the Use Order of Subsets in OSEM Method. March 2012. Available online: https://junshin.repo.nii.ac.jp/?action=repository_action_common_download&item_id=63&item_no=1&attribute_id=22&file_no=1 (accessed on 5 December 2021).
- Brook, N.; Brook, E.; Dharmarajan, A.; Dass, C.R.; Chan, A. Breast cancer bone metastases: Pathogenesis and therapeutic targets. Int. J. Biochem. Cell Biol. 2018, 96, 63–78. [Google Scholar] [CrossRef] [PubMed]



| Region | No. of Lesions | No. of Metastatic Lesions | No. of Degenerative Lesions |
|---|---|---|---|
| Lumbar vertebrae (L) | 124 | 50 | 74 |
| Thoracic vertebrae (T) | 104 | 50 | 54 |
| Pelvic bones (P) | 77 | 61 | 16 |
| Other bone sites (O) | 110 | 75 | 35 |
| SUVMax Value | No. | Min. | Max. | Mean | Std.dev. |
|---|---|---|---|---|---|
| Metastatic lesions | 236 | 10.90 | 130.70 | 32.56 | 16.39 |
| Degenerative lesions | 179 | 3.50 | 27.00 | 10.26 | 4.67 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gherghe, M.; Mutuleanu, M.-D.; Stanciu, A.E.; Irimescu, I.; Lazar, A.; Bacinschi, X.; Anghel, R.M. Quantitative Analysis of SPECT-CT Data in Metastatic Breast Cancer Patients—The Clinical Significance. Cancers 2022, 14, 273. https://doi.org/10.3390/cancers14020273
Gherghe M, Mutuleanu M-D, Stanciu AE, Irimescu I, Lazar A, Bacinschi X, Anghel RM. Quantitative Analysis of SPECT-CT Data in Metastatic Breast Cancer Patients—The Clinical Significance. Cancers. 2022; 14(2):273. https://doi.org/10.3390/cancers14020273
Chicago/Turabian StyleGherghe, Mirela, Mario-Demian Mutuleanu, Adina Elena Stanciu, Ionela Irimescu, Alexandra Lazar, Xenia Bacinschi, and Rodica Maricela Anghel. 2022. "Quantitative Analysis of SPECT-CT Data in Metastatic Breast Cancer Patients—The Clinical Significance" Cancers 14, no. 2: 273. https://doi.org/10.3390/cancers14020273
APA StyleGherghe, M., Mutuleanu, M.-D., Stanciu, A. E., Irimescu, I., Lazar, A., Bacinschi, X., & Anghel, R. M. (2022). Quantitative Analysis of SPECT-CT Data in Metastatic Breast Cancer Patients—The Clinical Significance. Cancers, 14(2), 273. https://doi.org/10.3390/cancers14020273






