Symptom Management and Quality of Life of Breast Cancer Patients Using Acupuncture-Related Therapies and Herbal Medicine: A Scoping Review
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Identifying the Research Questions
- What kind of research has been conducted?
- Which acupuncture-related therapies and herbal medicine types are mainly used?
- What were the main outcomes related to pain and quality of life?
- What were the results of the treatments?
- What is the level of evidence regarding the effectiveness of acupuncture-related therapies and herbal medicines?
2.2. Identifying the Relevant Studies
2.3. Study Selection
Inclusion/Exclusion Criteria
2.4. Screening and Agreement
2.5. Charting the Data
2.6. Collecting, Summarising, and Reporting the Results
3. Results
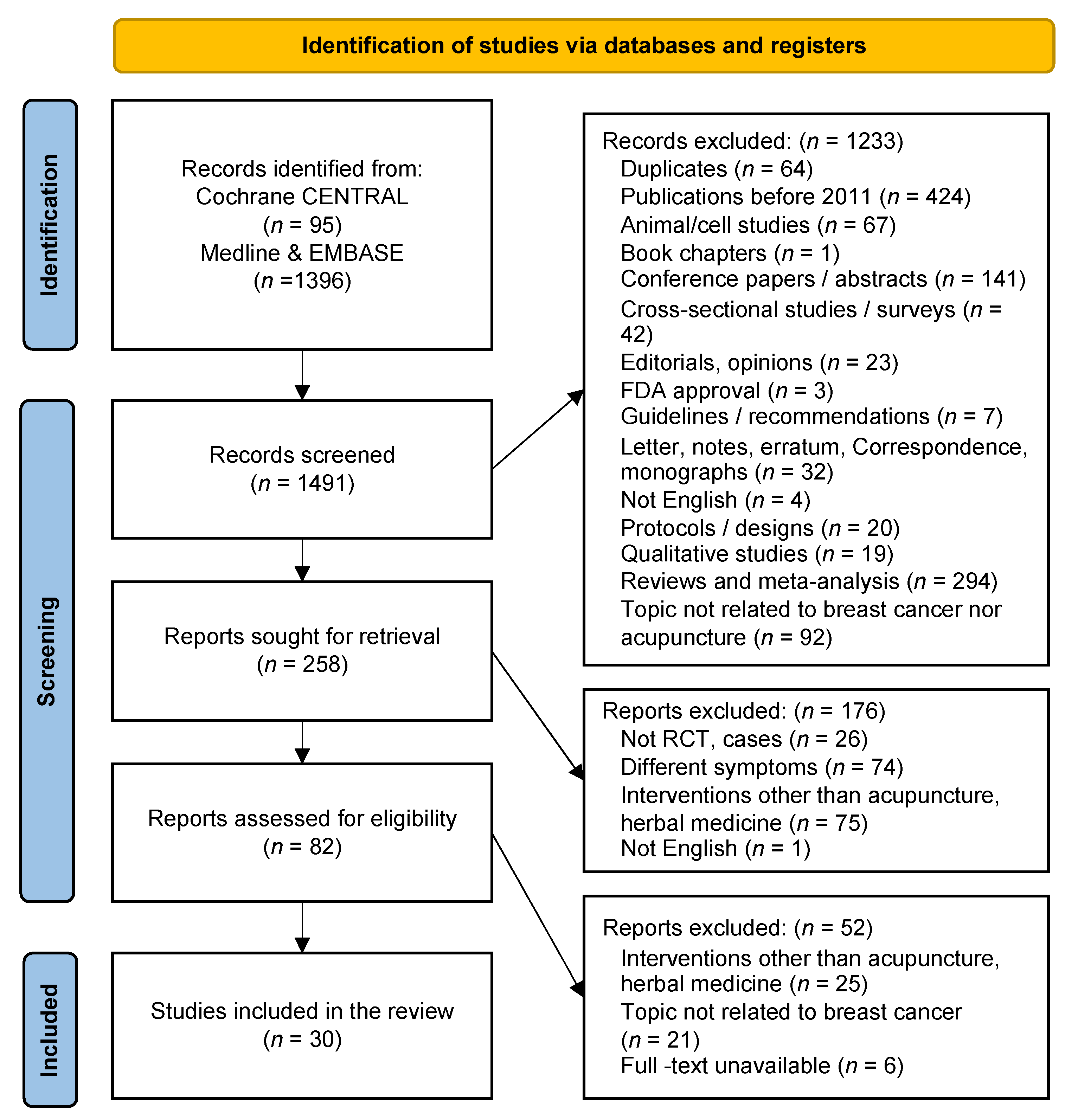
3.1. Literature Search and Selection Process
3.2. General Characteristics of the Identified Literature
3.2.1. Publication Year
3.2.2. Study Design Types
3.2.3. Research Regions
3.3. Characteristics of Study Participants
3.3.1. Participants
3.3.2. Type of Anti-Cancer Treatments Received by the Patients
3.3.3. Main Symptoms of Patients
3.4. Treatment Details
3.4.1. Acupuncture-Related Treatments
3.4.2. Herbal Medicine
3.5. Control
3.6. Evaluation Tools
3.7. Treatment Effects
- Acupuncture-related therapies
- 2.
- Herbal medicine
- 3.
- Acupuncture combined with herbal medicine
- 4.
- Safety
4. Discussion
4.1. Main Findings
4.2. Limitations of This Analysis
5. Conclusions
5.1. Implications for Research
5.2. Implications for Practice
Author Contributions
Funding
Conflicts of Interest
References
- Azamjah, N.; Soltan-Zadeh, Y.; Zayeri, F. Global Trend of Breast Cancer Mortality Rate: A 25-Year Study. Asian Pac. J. Cancer Prev. 2019, 20, 2015–2020. [Google Scholar] [CrossRef] [PubMed]
- Korea Central Cancer Registry, N.C.C. Annual Report of Cancer Statistics in Korea in 2018; Ministry of Health and Welfare: Seoul, Korea, 2020.
- Hyang-Ha, C.; Hwa-Jeong, S. The Risk of Breast Cancer in Women in Their 40s by Economic Activity. J. Radiol. Sci. Technol. 2020, 43, 23–27. [Google Scholar]
- Kang, S.Y.; Kim, Y.S.; Kim, Z.; Kim, H.Y.; Kim, H.J.; Park, S.; Bae, S.Y.; Yoon, K.H.; Lee, S.B.; Lee, S.K.; et al. Breast Cancer Statistics in Korea in 2017: Data from a Breast Cancer Registry. J. Breast Cancer 2020, 23, 115–128. [Google Scholar] [CrossRef]
- Campagna, M.; Loscerbo, R.; Pilia, I.; Meloni, F. Return to Work of Breast Cancer Survivors: Perspectives and Challenges for Occupational Physicians. Cancers 2020, 12, 355. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, S.M.; Stanton, A.L.; Petrie, K.J.; Partridge, A.H. Symptoms and Symptom Attribution Among Women on Endocrine Therapy for Breast Cancer. Oncologist 2015, 20, 598–604. [Google Scholar] [CrossRef]
- Kwekkeboom, K.L. Cancer Symptom Cluster Management. Semin. Oncol. Nurs. 2016, 32, 373–382. [Google Scholar] [CrossRef]
- Cameron, D.; Piccart-Gebhart, M.J.; Gelber, R.D.; Procter, M.; Goldhirsch, A.; de Azambuja, E.; Castro, G., Jr.; Untch, M.; Smith, I.; Gianni, L.; et al. 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: Final analysis of the HERceptin Adjuvant (HERA) trial. Lancet 2017, 389, 1195–1205. [Google Scholar] [CrossRef]
- Zhang, X.; Oliveri, J.M.; Paskett, E.D. Features, Predictors, and Treatment of Breast Cancer-related Lymphedema. Curr. Breast Cancer Rep. 2020, 12, 244–254. [Google Scholar] [CrossRef]
- Chappell, A.G.; Bai, J.; Yuksel, S.; Ellis, M.F. Post-Mastectomy Pain Syndrome: Defining Perioperative Etiologies to Guide New Methods of Prevention for Plastic Surgeons. World J. Plast. Surg. 2020, 9, 247–253. [Google Scholar] [CrossRef]
- Santen, R.J.; Stuenkel, C.A.; Davis, S.R.; Pinkerton, J.V.; Gompel, A.; Lumsden, M.A. Managing Menopausal Symptoms and Associated Clinical Issues in Breast Cancer Survivors. J. Clin. Endocrinol. Metab. 2017, 102, 3647–3661. [Google Scholar] [CrossRef]
- Ho, P.J.; Gernaat, S.A.M.; Hartman, M.; Verkooijen, H.M. Health-related quality of life in Asian patients with breast cancer: A systematic review. BMJ Open 2018, 8, e020512. [Google Scholar] [CrossRef] [PubMed]
- Buckner, C.A.; Lafrenie, R.M.; Denommee, J.A.; Caswell, J.M.; Want, D.A. Complementary and alternative medicine use in patients before and after a cancer diagnosis. Curr. Oncol. 2018, 25, e275–e281. [Google Scholar] [CrossRef] [PubMed]
- Molassiotis, A.; Scott, J.A.; Kearney, N.; Pud, D.; Magri, M.; Selvekerova, S.; Bruyns, I.; Fernadez-Ortega, P.; Panteli, V.; Margulies, A.; et al. Complementary and alternative medicine use in breast cancer patients in Europe. Support Care Cancer 2006, 14, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Collins, K.B.; Thomas, D.J. Acupuncture and acupressure for the management of chemotherapy-induced nausea and vomiting. J. Am. Acad. Nurse Pract. 2004, 16, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Zhang, Y.; Jing, N.C.; Lu, Y.; Xiao, H.Y.; Xu, G.L.; Wang, X.G.; Wang, L.M.; Zhang, Y.M.; Zhang, D.J.; et al. Electroacupuncture at Zusanli (ST 36) for treatment of nausea and vomiting caused by the chemotherapy of the malignant tumor: A multicentral randomized controlled trial. Zhongguo Zhen Jiu 2009, 29, 955–958. [Google Scholar]
- Deng, G.; Vickers, A.; Yeung, S.; D’Andrea, G.M.; Xiao, H.; Heerdt, A.S.; Sugarman, S.; Troso-Sandoval, T.; Seidman, A.D.; Hudis, C.A.; et al. Randomized, controlled trial of acupuncture for the treatment of hot flashes in breast cancer patients. J. Clin. Oncol. 2007, 25, 5584–5590. [Google Scholar] [CrossRef]
- Frisk, J.; Carlhall, S.; Kallstrom, A.C.; Lindh-Astrand, L.; Malmstrom, A.; Hammar, M. Long-term follow-up of acupuncture and hormone therapy on hot flushes in women with breast cancer: A prospective, randomized, controlled multicenter trial. Climacteric 2008, 11, 166–174. [Google Scholar] [CrossRef]
- Hervik, J.; Mjaland, O. Acupuncture for the treatment of hot flashes in breast cancer patients, a randomized, controlled trial. Breast Cancer Res. Treat. 2009, 116, 311–316. [Google Scholar] [CrossRef]
- Deng, G.; Chan, Y.; Sjoberg, D.; Vickers, A.; Yeung, K.S.; Kris, M.; Straus, D.; Cassileth, B. Acupuncture for the treatment of post-chemotherapy chronic fatigue: A randomized, blinded, sham-controlled trial. Support Care Cancer 2013, 21, 1735–1741. [Google Scholar] [CrossRef]
- Molassiotis, A.; Bardy, J.; Finnegan-John, J.; Mackereth, P.; Ryder, D.W.; Filshie, J.; Ream, E.; Richardson, A. Acupuncture for cancer-related fatigue in patients with breast cancer: A pragmatic randomized controlled trial. J. Clin. Oncol. 2012, 30, 4470–4476. [Google Scholar] [CrossRef]
- Molassiotis, A.; Bardy, J.; Finnegan-John, J.; Mackereth, P.; Ryder, W.D.; Filshie, J.; Ream, E.; Eaton, D.; Richardson, A. A randomized, controlled trial of acupuncture self-needling as maintenance therapy for cancer-related fatigue after therapist-delivered acupuncture. Ann. Oncol. 2013, 24, 1645–1652. [Google Scholar] [CrossRef] [PubMed]
- Kiecolt-Glaser, J.K.; Bennett, J.M.; Andridge, R.; Peng, J.; Shapiro, C.L.; Malarkey, W.B.; Emery, C.F.; Layman, R.; Mrozek, E.E.; Glaser, R. Yoga’s impact on inflammation, mood, and fatigue in breast cancer survivors: A randomized controlled trial. J. Clin. Oncol. 2014, 32, 1040–1049. [Google Scholar] [CrossRef] [PubMed]
- Taso, C.J.; Lin, H.S.; Lin, W.L.; Chen, S.M.; Huang, W.T.; Chen, S.W. The effect of yoga exercise on improving depression, anxiety, and fatigue in women with breast cancer: A randomized controlled trial. J. Nurs. Res. 2014, 22, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Greenlee, H.; DuPont-Reyes, M.J.; Balneaves, L.G.; Carlson, L.E.; Cohen, M.R.; Deng, G.; Johnson, J.A.; Mumber, M.; Seely, D.; Zick, S.M.; et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA Cancer J. Clin. 2017, 67, 194–232. [Google Scholar] [CrossRef] [PubMed]
- Northern Cancer Alliance, National Health Service. Breast Cancer Clinical Guidelines; Northern Cancer Alliance, National Health Service: Newcastle Upon Tyne, UK, 2020. [Google Scholar]
- Abbasi, B.; Mirzakhany, N.; Angooti Oshnari, L.; Irani, A.; Hosseinzadeh, S.; Tabatabaei, S.M.; Haghighat, S. The effect of relaxation techniques on edema, anxiety and depression in post-mastectomy lymphedema patients undergoing comprehensive decongestive therapy: A clinical trial. PLoS ONE 2018, 13, e0190231. [Google Scholar] [CrossRef]
- De Groef, A.; Van Kampen, M.; Vervloesem, N.; De Geyter, S.; Christiaens, M.R.; Neven, P.; Vos, L.; De Vrieze, T.; Geraerts, I.; Devoogdt, N. Myofascial techniques have no additional beneficial effects to a standard physical therapy programme for upper limb pain after breast cancer surgery: A randomized controlled trial. Clin. Rehabil. 2017, 31, 1625–1635. [Google Scholar] [CrossRef]
- Lu, W.; Giobbie-Hurder, A.; Freedman, R.A.; Shin, I.H.; Lin, N.U.; Partridge, A.H.; Rosenthal, D.S.; Ligibel, J.A. Acupuncture for Chemotherapy-Induced Peripheral Neuropathy in Breast Cancer Survivors: A Randomized Controlled Pilot Trial. Oncologist 2020, 25, 310–318. [Google Scholar] [CrossRef]
- Liu, X.; Lu, J.; Wang, G.; Chen, X.; Xv, H.; Huang, J.; Xue, M.; Tang, J. Acupuncture for Arthralgia Induced by Aromatase Inhibitors in Patients with Breast Cancer: A Systematic Review and Meta-analysis. Integr. Cancer Ther. 2021, 20, 1534735420980811. [Google Scholar] [CrossRef]
- Colquhoun, H.L.; Levac, D.; O’Brien, K.K.; Straus, S.; Tricco, A.C.; Perrier, L.; Kastner, M.; Moher, D. Scoping reviews: Time for clarity in definition, methods, and reporting. J. Clin. Epidemiol. 2014, 67, 1291–1294. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Chino, A.; Okamoto, H.; Hirasaki, Y.; Ueda, K.; Ogawa, K.; Namiki, T. A case of aromatase inhibitor (anastrozole)-induced side-effects successfully treated with Kampo medicines. J. Altern. Complement. Med. 2011, 17, 1075–1077. [Google Scholar] [CrossRef] [PubMed]
- Beuth, J.; van Leendert, R.; Schneider, B.; Uhlenbruck, G. Complementary medicine on side-effects of adjuvant hormone therapy in patients with breast cancer. In Vivo 2013, 27, 781–869. [Google Scholar] [PubMed]
- Oh, B.; Kimble, B.; Costa, D.S.J.; Davis, E.; McLean, A.; Orme, K.; Beith, J. Acupuncture for treatment of arthralgia secondary to aromatase inhibitor therapy in women with early breast cancer: Pilot study. Acupunct. Med. 2013, 31, 264–271. [Google Scholar] [CrossRef]
- Mao, J.J.; Farrar, J.T.; Bruner, D.; Zee, J.; Bowman, M.; Seluzicki, C.; DeMichele, A.; Xie, S.X. Electroacupuncture for fatigue, sleep, and psychological distress in breast cancer patients with aromatase inhibitor-related arthralgia: A randomized trial. Cancer 2014, 120, 3744–3751. [Google Scholar] [CrossRef]
- Mao, J.J.; Xie, S.X.; Farrar, J.T.; Stricker, C.T.; Bowman, M.A.; Bruner, D.; DeMichele, A. A randomised trial of electro-acupuncture for arthralgia related to aromatase inhibitor use. Eur. J. Cancer. 2014, 50, 267–276. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, Z.; Cui, F.; Liu, J.; Wang, Y.; Jiang, J.; Ma, W.; Lu, W. Traditional Chinese medicine bionic tiger bone powder for the treatment of ai-Associated musculoskeletal symptoms. Evid. Based Complement. Alternat. Med. 2017, 2017, 2478565. [Google Scholar] [CrossRef]
- Peng, N.; Yu, M.; Yang, G.; Fu, Q.; Xu, Y.; Yu, J.; Liu, Q.; Li, C.; Xu, W.; Zhang, Y.; et al. Effects of the Chinese medicine Yi Shen Jian Gu granules on aromatase inhibitor-associated musculoskeletal symptoms: A randomized, controlled clinical trial. Breast 2018, 37, 18–27. [Google Scholar] [CrossRef]
- Zhang, X.; Peng, N.; Yu, M.-W.; Zhang, G.-L.; Sun, X.; Yang, G.-W.; Li, C.; Yang, L.; Wang, X.-M. Chinese Medicine Yishen Jiangu Granules () on Aromatase Inhibitor-Associated Musculoskeletal Symptoms. Chin. J. Integr. Med. 2018, 24, 867–872. [Google Scholar] [CrossRef]
- Kim, T.H.; Kang, J.W. Acupuncture for symptoms management in Korean breast cancer survivors: A prospective pilot study. Acupunct. Med. 2019, 37, 164–174. [Google Scholar] [CrossRef]
- Ms, B.R.C.; Van Zee, K.; Yeung, K.; Ma, M.I.C.; Cohen, S.; Chan, Y.H.; Vickers, A.; Ma, D.D.S.; Hudis, C.A. Acupuncture in the treatment of upper-limb lymphedema: Results of a pilot study. Cancer 2013, 119, 2455–24561. [Google Scholar] [CrossRef]
- Jeong, Y.J.; Kwon, H.J.; Park, Y.S.; Kwon, O.C.; Shin, I.H.; Park, S.H. Treatment of Lymphedema with Saam Acupuncture in Patients with Breast Cancer: A Pilot Study. Med. Acupunct. 2015, 27, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Bao, T.; Zhi, W.I.; Vertosick, E.A.; Li, Q.S.; DeRito, J.; Vickers, A.; Cassileth, B.R.; Mao, J.J.; Van Zee, K.J. Acupuncture for breast cancer-related lymphedema: A randomized controlled trial. Breast Cancer Res. Treat. 2018, 170, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhang, Y.; Yang, M.; Liu, Y.; Zhu, Y.; Fan, Y.; Li, Q.; Pei, X. Bloodletting puncture and cupping as an adjuvant therapy for breast cancer-related lymphedema in female adults: A non-randomized controlled pragmatic trial. J. Tradit. Chin. Med. Sci. 2018, 5, 255–263. [Google Scholar] [CrossRef]
- Wang, C.; Yang, M.; Fan, Y.; Pei, X. Moxibustion as a Therapy for Breast Cancer-Related Lymphedema in Female Adults: A Preliminary Randomized Controlled Trial. Integr. Cancer Ther. 2019, 18, 1534735419866919. [Google Scholar] [CrossRef]
- Han, K.; Kwon, O.; Park, H.-J.; Kim, A.-R.; Lee, B.; Kim, M.; Kim, J.-H.; Yang, C.-S.; Yoo, H.-S. Electronic Moxibustion for Breast Cancer-Related Lymphedema: A Pilot Clinical Trial. Integr. Cancer Ther. 2020, 19, 1534735420962854. [Google Scholar] [CrossRef]
- Bauml, J.; Basal, C.; Mao, J.J. Treatment of post-mastectomy pain syndrome with acupuncture: A case report. Acupunct. Med. 2014, 32, 183–185. [Google Scholar] [CrossRef]
- Mallory, M.J.; Croghan, K.A.; Sandhu, N.P.; Lemaine, V.; Degnim, A.C.; Bauer, B.A.; Cha, S.S.; Croghan, I.T. Acupuncture in the postoperative setting for breast cancer patients: A feasibility study. Am. J. Chin. Med. 2015, 43, 45–56. [Google Scholar] [CrossRef]
- Giron, P.S.; Haddad, C.A.S.; Rizzi, S.K.; Nazário, A.C.P.; Facina, G. Effectiveness of acupuncture in rehabilitation of physical and functional disorders of women undergoing breast cancer surgery. Support Care Cancer 2016, 24, 2491–2496. [Google Scholar] [CrossRef]
- Quinlan-Woodward, J.; Gode, A.; Dusek, J.; Reinstein, A.; Johnson, J.; Sendelbach, S. Assessing the Impact of Acupuncture on Pain, Nausea, Anxiety, and Coping in Women Undergoing a Mastectomy. Oncol. Nurs. Forum. 2016, 43, 725–732. [Google Scholar] [CrossRef]
- Ao, L.; Shi, J.; Bai, Y.; Zhang, S.; Gan, J. Effects of transcutaneous electrical acupoint stimulation on perioperative immune function and postoperative analgesia in patients undergoing radical mastectomy: A randomized controlled trial. Exp. Ther. Med. 2021, 21, 184. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, K.; Ogawa, M.; Nishijima, K.; Tsuda, M.; Nishimura, G. Efficacy of contact needle therapy for chemotherapy-induced peripheral neuropathy. Evid. Based Complement. Alternat. Med. 2013, 2013, 928129. [Google Scholar] [CrossRef] [PubMed]
- Greenlee, H.; Crew, K.D.; Capodice, J.; Awad, D.; Buono, D.; Shi, Z.; Jeffres, A.; Wyse, S.; Whitman, W.; Trivedi, M.S.; et al. Randomized sham-controlled pilot trial of weekly electro-acupuncture for the prevention of taxane-induced peripheral neuropathy in women with early stage breast cancer. Breast Cancer Res. Treat. 2016, 156, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Bao, T.; Seidman, A.D.; Piulson, L.; Vertosick, E.; Chen, X.; Vickers, A.J.; Blinder, V.S.; Zhi, W.I.; Li, Q.; Vahdat, L.T.; et al. A phase IIA trial of acupuncture to reduce chemotherapy-induced peripheral neuropathy severity during neoadjuvant or adjuvant weekly paclitaxel chemotherapy in breast cancer patients. Eur. J. Cancer 2018, 101, 12–19. [Google Scholar] [CrossRef]
- Jeong, Y.J.; Kwak, M.A.; Seo, J.C.; Park, S.H.; Bong, J.G.; Shin, I.H.; Park, S.H. Acupuncture for the treatment of taxane-induced peripheral neuropathy in breast cancer patients: A pilot trial. Evid. Based Complement. Alternat. Med. 2018, 2018, 5367014. [Google Scholar] [CrossRef]
- Rostock, M.; Fischer, J.; Mumm, A.; Stammwitz, U.; Saller, R.; Bartsch, H.H. Black cohosh (Cimicifuga racemosa) in tamoxifen-treated breast cancer patients with climacteric complaints a prospective observational study. Gynecol. Endocrinol. 2011, 27, 844–848. [Google Scholar] [CrossRef]
- Ben-Arye, E.; Israely, P.; Baruch, E.; Dagash, J. Integrating family medicine and complementary medicine in cancer care: A cross-cultural perspective. Patient Educ. Couns. 2014, 97, 135–139. [Google Scholar] [CrossRef]
- Zhu, L.M. One case report of postoperative bone metastases after treatment of Yiqi Yangyin Jiedu Decoction to breast cancer. J. Shanghai Jiao Tong Univ. 2014, 34, 126–128. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Shiu, J.-H.; Chen, F.-P.; Chiu, J.-H. Building an Integrative Outpatient Care Program for Breast Cancer Patients in Taiwan. Integr Cancer Ther. 2016, 15, 343–348. [Google Scholar] [CrossRef]
- Saghatelyan, T.; Tananyan, A.; Janoyan, N.; Tadevosyan, A.; Petrosyan, H.; Hovhannisyan, A.; Hayrapetyan, L.; Arustamyan, M.; Arnhold, J.; Rotmann, A.-R.; et al. Efficacy and safety of curcumin in combination with paclitaxel in patients with advanced, metastatic breast cancer: A comparative, randomized, double-blind, placebo-controlled clinical trial. Phytomedicine 2020, 70, 153218. [Google Scholar] [CrossRef]
| No. | Search Terms |
|---|---|
| #1 | breast neoplasm [MeSH Terms] OR “breast carcinoma” OR “Neoplasm, Breast” OR “Breast Tumors” OR “Breast Tumor” OR “Tumor, Breast” OR “Tumors, Breast” OR “Neoplasms, Breast” OR “Breast Cancer” OR “Cancer, Breast” OR “Mammary Cancer” OR “Cancer, Mammary” OR “Cancers, Mammary” OR “Mammary Cancers” OR “Malignant Neoplasm of Breast” OR “Breast Malignant Neoplasm” OR “Breast Malignant Neoplasms” OR “Malignant Tumor of Breast” OR “Breast Malignant Tumor” OR “Breast Malignant Tumors” OR “Cancer of Breast” OR “Cancer of the Breast” OR “Mammary Carcinoma, Human” OR “Human Mammary Carcinomas” OR “Human Mammary Carcinoma” OR “Human Mammary Neoplasms” |
| #2 | pain OR “pain management” OR arthralgia OR “aromatase-inhibitor induced arthralgia” OR “aromatase-inhibitor associated arthralgia” OR “post-mastectomy pain syndrome” |
| #3 | Breast Cancer Lymphedema [MH] OR “Lymphedema, Breast Cancer” OR “Breast Cancer Treatment-Related Lymphedema” OR “Breast Cancer Treatment Related Lymphedema” OR “Breast Cancer-Related Arm Lymphedema” OR “Breast Cancer Related Arm Lymphedema” OR “Breast Cancer Related Lymphedema” OR “Postmastectomy Lymphedema” OR “Lymphedema, Postmastectomy” OR “Post-mastectomy Lymphedema” OR “Lymphedema, Post-mastectomy” OR “Post mastectomy Lymphedema” |
| #4 | complementary therapy [MH] |
| #5 | herbal medicine [MH] OR Drugs, Chinese Herbal [MH] OR “herbal medicine” OR herb OR herbs OR herbal OR Medicine, Chinese Traditional [MH] OR “Traditional Chinese Medicine” OR “Traditional Medicine, Chinese” OR “Chinese Traditional Medicine” OR “Chinese Medicine, Traditional” OR Medicine, Korean Traditional [MH] OR “Traditional Medicine, Korean” OR “Korean Traditional Medicine” OR “kampo” OR tang OR decoction OR granule |
| #6 | Acupuncture [MH] OR Acupuncture therapy [MH] OR Acupuncture OR “Acupuncture therapy” OR “Acupuncture Treatment” OR “Acupuncture Treatments” OR “Treatment, Acupuncture” OR “Therapy, Acupuncture” OR “Pharmacoacupuncture Treatment” OR “Treatment, Pharmacoacupuncture” OR “Pharmacoacupuncture Therapy” OR “Therapy, Pharmacoacupuncture” OR Acupotomy OR Acupotomies OR Needling OR Needle OR Electroacupuncture [MH] OR Electroacupuncture OR Acupoint OR Meridian [MH] OR Meridian OR Acupuncture point [MH] OR “Acupuncture point” OR “Body acupuncture” OR “Auricular acupuncture” OR “Ear acupuncture” OR “acupuncture, Ear” [MH] OR “Scalp acupuncture” OR “Intradermal needle” OR “Fire needle” OR “Elongated needle” OR “Warm needle” OR Dry needling [MH] OR “Dry needle” OR “Skin acupuncture” |
| #7 | Moxibustion [MH] |
| #8 | cupping therapy [MH] |
| #9 | ((#1 AND #2) OR #3) AND (#4 OR #5 OR #6 OR #7 OR #8) |
| Criteria | Details |
|---|---|
| Study type | Human studies including randomized controlled trials, controlled clinical trials, case series, case reports, pilot clinical studies, and retrospective observational studies (In vivo and in vitro experiments, reviews, duplicate articles, ongoing studies, and studies that failed to provide detailed results or with incomplete data were also excluded) |
| Patients | Breast cancer patients (1) over 18 years of age, (2) who were, or had been, going through anti-cancer therapy, such as breast cancer surgery (either mastectomy or lumpectomy), chemotherapy, immunotherapy, and/or endocrine therapy, and (3) who were experiencing post-surgery pain, neuropathic pain, joint pain, or lymphedema due to anti-cancer therapy |
| Intervention | adjuvant acupuncture-related therapies (as acupuncture, acupressure, electro-acupuncture, laser acupuncture, massage, moxibustion, and cupping therapy) or herbal medicine (vitamin supplements; mindfulness therapies, such as meditation; and yoga were excluded) |
| Language | English |
| Publication Year | Published in the last 10 years |
| Miscellaneous | No restriction was applied on sex, ethnicity, symptom severity, cancer stage, disease duration, clinical setting, and country of study. |
| Variables | Categories | N (%) |
|---|---|---|
| Publication year | 2011 | 2 |
| 2012 | 0 | |
| 2013 | 4 | |
| 2014 | 5 | |
| 2015 | 1 | |
| 2016 | 4 | |
| 2017 | 1 | |
| 2018 | 7 | |
| 2019 | 2 | |
| 2020 | 3 | |
| 2021 | 1 | |
| Location | Korea | 4 |
| USA | 13 | |
| China | 7 | |
| Japan | 1 | |
| Taiwan | 1 | |
| Switzerland | 1 | |
| Israel | 1 | |
| Brazil | 1 | |
| Armenia | 1 | |
| Study type | Case report | 3 |
| Case series | 1 | |
| Randomized controlled trial | 13 | |
| Before-and-after study (Single arm study) | 12 | |
| Non-randomized controlled trial | 1 |
| Study | Location | Design | Intervention | Comparator | Outcomes | Significant Findings | Adverse Event |
|---|---|---|---|---|---|---|---|
| Chino et al. [34] | Japan | A case study | 1. Juzentaihoto 2. aconitine root | none | 1. Genital bleeding 2. arthralgia | 1. the atypical genital bleeding disappeared 2. the arthralgia almost completely disappeared | There have been no signs of side-effects for 2 years |
| Beuth et al. [35] | Germany | A single-arm study | Lens culinaris lectin (oral medication containing sodium selenite (300 μg/day), proteolytic enzymes (bromelaine 400 mg/day and papain 400 mg/day) and Lens culinaris lectin (20 mg/day). | none | 1. Mean scores of symptoms (arthralgia, mucosal dryness) 2. The severity of side-effects of hormone therapy using scoring system | The severity of side effects of hormone therapy was reduced by complementary treatment. Mean scores of symptoms declined from 4.92 before treatment to 3.16 after four weeks of treatment for arthralgia and from 4.83 before treatment to 3.21 after four weeks of treatment for mucosal dryness, and these were the primary aims of this investigation. | Adverse reactions (e.g., nausea, bloating 12% of patients; 3% stopped the medication) were documented. |
| Oh et al. [36] | Australia | A pilot randomized controlled trial | Electro-acupuncture (EA) | sham electro-acupuncture | 1. Joint pain, stiffness, and physical function were measured with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) 2. Pain severity and interference: Brief Pain Inventory Short Form (BPI-SF) 3. Quality of life (QOL): Functional Assessment of Cancer Therapy-General (FACT-G) 3. Hand strength: grip test 4. a serum marker of inflammation (C reactive protein (CRP)) | There were no significant differences in outcome measures. However, positive trends were observed in stiffness and physical function at week 12 in favor of real EA | No serious adverse events were reported during or after acupuncture treatments. |
| Mao et al. [37] | USA | Randomized controlled trial | Electro-acupuncture (EA) | 1. Waitlist 2. Sham electro-acupuncture (SA) | 1. Fatigue: Brief Fatigue Inventory (BFI) 2. sleep disturbance: Pittsburgh Sleep Quality Index (PSQI) 3. anxiety, and depression: Hospital Anxiety and Depression Scale (HADS) | Compared to usual care, EA produced significant improvement in fatigue, anxiety, and depression, whereas SA improved only depression in women experiencing AI-related arthralgia. | No mention |
| Mao et al. [38] | USA | Randomized controlled trial | Electro-acupuncture (EA) | 1. Waitlist 2. Sham electro-acupuncture (SA) | 1. Pain severity: Brief Pain Inventory (BPI) | Compared to usual care, EA produced clinically important and durable improvement in arthralgia related to AIs in breast cancer patients, and SA had a similar effect. Both EA and SA were safe. | Despite needle placement in the same arm as breast cancer surgery, no case of infection, no reports of development or worsening of lymphedema occurred in either EA or SA groups. Eighteen related adverse events (AEs) were reported by eight subjects in the EA or SA groups during 398 intervention episodes. These AEs were mild in severity and spontaneously resolved without additional medical interventions. The EA group had more adverse events reported than the SA group (16 vs. 4). A major category of AEs reported in the EA group was related to the “De Qi” sensation (N = 6, such as tingling, numbness during the acupuncture process). Both EA and SA groups had similar rates of pain at the needling site (5 and 4 respectively) |
| Li et al. [39] | China | Randomized controlled trial | Tiger bone powder (Chinese traditional herb) | Placebo | 1. Modified Brief Pain Inventory (M-BPI) 2. Visual Analog Scale (VAS) for pain 3. Functional Assessment of Cancer Therapy-Breast (FACT-B). 4. Serum estradiol (E2), follicle-stimulating hormone (FSH) level | 1. Reduced pain (M-BPI) -Treatment group : 4.6 → 2.0 -Control group : 4.9 → 5.6 (p < 0.001) 2. Reduced pain (VAS) -Treatment group : 6.3 → 3.0 -Control group : 6.4 → 6.6 (p < 0.001) 3. Improved QoL -Treatment vs. Control : 22.23 vs. 19.93 (p < 0.05) 4. No significant differences were found for the E2 and FSH | Of all 72 enrolled participants, 6 of them (2 in TB and 4 in placebo) reported stomach discomfort, but tolerable. Thus, we suggested to them taking pills half an hour after meals, and no other adverse events were reported. Two participants failed to continue the intervention. One in TB group lost her mother at 3 weeks; thus, she had difficulties in scheduling. Another participant in placebo group, her husband had a job change, and the whole family had moved to Japan on week 8. Other 70 participants had finished the intervention, and there were no lost cases. |
| Peng et al. [40] | China | Randomized controlled trial | Yi Shen Jian Gu granules (YSJG) | Placebo | 1. Brief Pain Inventory Short Form (BPI-SF) 2. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) 3. Modified Score for the Assessment and Quantification of Chronic Rheumatoid Affections of the Hands (M-SACRAH) 4. Functional Assessment of Cancer Therapy-Breast (FACT-B) 5. Bone mineral density (BMD) | 1. Reduced pain (BPI-SF) -Treatment group : 6.18 → 3.08 -Control group : 6.05 → 4.42 (p = 0.001) 2. Improved joint symptoms measured by WOMAC and M-SACRAH 3. Improved QoL 4. BMD showed no apparent change after 12 weeks for both groups | There was a total of 14 participants reporting adverse events among those receiving YSJG granules (33%) and 16 participants among those receiving Placebo granules (39%). |
| Zhang et al. [41] | China | A single-arm study | Yishen Jiangu Granules (YSJGG) | None | 1. Brief Pain Inventory Short Form (BPI-SF) 2. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) 3. Modified Score for the Assessment of Chronic Rheumatoid Affections of the Hands (M-SACRAH) 4. Functional Assessment of Cancer Therapy-Breast (FACT-B) 5. Bone mineral density (BMD) 6. Blood indices, such as calcium (Ca), phosphate (P), and alkaline phosphatase (ALP) | 1. Reduced pain (BPI-SF) : 5.75 ± 1.87→3.58 ± 2.15 (p = 0.002) 2. Improved joint symptoms measured by WOMAC and M-SACRAH 3. Improved QoL (only in physical and functional well-being) 4. Level of BMD, Ca, and P showed no apparent change after 12 weeks for both groups | In the period of this study, 6 out of 30 participants reported adverse events. Three patients reported mild epigastric discomfort, heartburn, and hiccup. Two patients experienced mild diarrhea, and one moderate. All symptoms were alleviated after discontinuing therapy, and symptoms did not appear when patients restarted therapy. There was no dropout because of AEs. |
| Kim et al. [42] | Korea | A prospective pilot single-arm study | Acupuncture | None | 1. Feasibility of the recruitment strategy and enrolment procedure, compliance with the acupuncture sessions and outcome assessments, acupuncture-related adverse events (AEs), and patients’ expectations and experience of acupuncture during the study using Was It Worth It (WIWI) questionnaire 2. Numerical rating scale (NRS) for symptoms for overall symptom severity 3. European Organization for Research and Treatment of Cancer Breast Cancer-Specific Quality of Life Questionnaire (EORCT QLQ-BR23) 4. Measure Yourself Medical Outcome Profile–Version 2 (MYMOP2) 5. Functional Assessment of Chronic Illness Therapy–Fatigue (FACIT-Fatigue) scales 6. Aromatase inhibitor–related knee pain: the Brief Pain Inventory–Short Form (BPI-SF), Western Ontario and McMaster Universities Arthritis Index (WOMAC) 7. Vasomotor symptoms: a hot flush symptom diary (severity and frequency), Menopausal Rating Scale (MRS) 8. Insomnia: Pittsburgh Sleep Quality Index (PSQI-K), Women’s Health Initiative Insomnia Rating Scale (WHI-IRS) 9. Sexual dysfunction: Female Sexual Functioning Index (FSFI), Female Sexual Distress Scale (FSDS) and Arizona Sexual Experience Scale (ASES) 10. Post-mastectomy chest wall or shoulder pain: BPI-SF, Shoulder Range of Motion (ROM) tool | Improved pain (BPI-SF) : 5.0→ 4.3 | Six minor self-limiting adverse events were recorded during a total of 78 acupuncture sessions, giving an incidence rate of 8%. These minor AEs consisted of subcutaneous bleeding (n = 4) and needle pain (n = 2), which were considered to have a causal relationship with acupuncture. There were also other miscellaneous events, including flu-like symptoms (n = 6), headache (n = 3), facial pain (n = 2), fatigue (n = 1), dizziness (n = 1), diarrhea (n = 1), indigestion (n = 1), a fall-related injury (n = 1), and tingling sensation in the breast (n = 1). |
| Cassileth et al. [43] | USA | A pilot single-arm study | Acupuncture | None | Arm circumference | Arm circumference 4.6 ± 2.2 → 3.7 ± 2.3 (p < 0.0005) | During the treatment period, 12 of the 33 patients reported mild bruising or minor pain/tingling in the arm, shoulder, or acupuncture site at least once. One patient experienced a transient (4-day) increase in lymphedema in the axilla of the lymphedematous arm. There were no serious adverse events—no infections or severe exacerbations—after 255 treatment sessions. Similarly there were no treatment-related infections, severe exacerbations, or other serious adverse events during 6 months of follow-up interviews |
| Jeong et al. [44] | USA | A pilot single-arm study | Acupuncture | None | Arm circumference | There was a significant reduction in the average circumference of the upper arms, the elbow, and the forearms for both the affected and the unaffected limb at the end of treatment (p < 0.001, p < 0.001, p < 0.001 for the affected limb; p = 0.027, p < 0.001, and p < 0.001 for the unaffected limb, respectively). | There were no serious adverse events and no infections or severe exacerbations after 255 treatment sessions and 6 months of follow-up interviews |
| Bao et al. [45] | USA | Randomized controlled trial | Acupuncture | Waitlist | Circumference and bioimpedance | Arm circumference -Acupuncture group (AC) : 4.74 (2.23) → 4.29 (2.67) -Waitlist group (WL) : 4.82 (2.32) → 4.76 (2.68) Difference between AC and WL : − 0.38 (p = 0.14) | No adverse events were reported in the waitlist group at week 6 and no severe adverse events were reported in either arm throughout the course of study. Adverse events were well balanced between the acupuncture group and the waitlist group that crossed over to acupuncture for weeks 6–12. Grade 1 treatment-related AEs, such as bruising (58%), hematoma (2%), and pain (2%), were reported in patients who received acupuncture. Among the 837 acupuncture treatments provided, one possibly related grade 2 skin infection was reported. |
| Wang et al. [46] | China | A non-randomized controlled trial | Bloodletting puncture and cupping with exercise | Exercise | 1. Arm circumference (at the wrist crease, 10 cm distal to the wrist crease, the elbow crease, and 10 cm distal to the elbow crease) 2. Visual analogue scale (VAS) score for pain | 1. Bloodletting puncture and cupping significantly reduced the circumference of the affected arm. Arm circumference reduction mainly occurred in the region from the wrist crease to 10 cm distal to the wrist crease -effective rate 95.8% (treatment group) vs. 58.3% (control group) (p < 0.001) 2. VAS scores of the two groups were significantly improved after treatment compared with before treatment -Treatment group: 1.30 (1.93) →0.88 (1.20) (p = 0.00) -Control group: 0.92 (1.22) → 0.92 (1.35) (p = 0.02) | No patient in either group experienced any adverse effects. |
| Wang et al. [47] | China | A Preliminary Randomized Controlled Trial | Moxibustion | Compression garment | 1. Arm circumference (affected arm) 2. Subjective sensation of swelling: visual analogue scale (VAS) 3. Fatigue: Revised Piper Fatigue Scale (RPFS) scores | 1. Decreased arm circumference (the difference value in the treatment group was superior to that in the control group) -Moxibustion group: 25.61 ± 2.11→ 24.48 ± 2.02 (p = 0.000) -Control group: 26.70 ± 1.93 → 26.09 ± 1.81 (p = 0.003) 2. Improved swelling -Moxibustion group: 7.57 ± 1.16 → 4.87 ± 0.87 (p = 0.000) -Control group: 7.32 ± 0.89 → 5.41 ± 0.80 (p = 0.000) 3. Improved fatigue -Moxibustion group: 4.85 ± 0.79 → 4.43 ± 0.63 (p = 0.000) -Control group: 4.87 ± 0.98 → 4.69 ± 0.77 (p = 0.000) | No adverse events, such as local burns, bleeding, ecchymosis, or inflammatory reactions, occurred during treatment. |
| Han et al. [48] | Korea | A single-arm pilot clinical trial | Electronic Moxibustion (EM) | None | 1. Differences in Circumferences between Affected Arm and Unaffected Arm 2. Differences in Range of Motion between Affected Arm and Unaffected Arm 3. Changes in Quality of Life Scores using European Organization for Research and Treatment of Cancer QLQ-BR23 (EORTC QLQ-BR23) | 1. After 8 weeks of EM treatment, the mean differences in arm circumferences between affected and unaffected upper limbs decreased. 37.10 mm→29.30 mm (p = 0.0078) 2. The differences in ROM between affected and unaffected upper extremities improved an average of 8.3° for flexion (p = 0.0488) and 3.2° for internal rotation (p = 0.0371) 3. Improvement of arm symptoms was significant only at week 5 (p = 0.0469). | After 8 weeks of intervention, there were no significant changes in blood analysis and vital signs. One serious adverse event (SAE) and 6 adverse events were reported during the trial, but most were irrelevant to the intervention. |
| Bauml et al. [49] | USA | A case report | Acupuncture | None | Visual analogue scale (VAS) for post-mastectomy pain syndrome | Resolution of pain VAS: 5 → 0 | No mention |
| Mallory et al. [50] | USA | A single arm study | Acupuncture | None | 1. Was-it-Worth-it (WIWI) questionnaire 2. Pain, relaxation, anxiety, tension/muscular discomfort: Visual analogue scale (VAS) | Improved anxiety, tension/muscular discomfort, and pain. | No mention |
| Giron et al. [51] | Brazil | A randomized controlled trial | Acupuncture with kinesiotherapy | Kinesiotherapy | 1. Shoulder range of motion, arm circumference, pain, upper limb function: Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire 2. Depression: Beck Depression Inventory (BDI) | Both groups showed statistically significant improvement of the items assessed: pain, depression, upper limb function, and ADM, and there was no difference between groups | No mention |
| Quinlan-Wood-ward et al. [52] | USA | A pilot study | Acupuncture | Usual care | 1. Pain, nausea, anxiety, ability to cope: Numeric rating scales (NRS) | Acupuncture delivered postoperatively in the hospital after mastectomy can reduce the severity of symptoms experienced, as well as increase the patient’s ability to cope with her symptoms. | No mention |
| Ao et al. [53] | China | A randomized controlled trial | Transcutaneous electrical acupoint stimulation (TEAS) | Sham transcutaneous electrical acupoint stimulation | 1. Pain: Visual analogue scale (VAS) 2. Blood sample collection: Cytokine assays (IL-2, IL-4, IFN-γ) | 1. The postoperative VAS scores at T2 and T3 in the TEAS group were significantly lower compared with the sham TEAS group 2. Compared with baseline levels at T0, serum levels of IL-2, IFN-γ and the ratio of IL-2/IL-4 were significantly decreased at T1-T4 in the sham TEAS group | No mention |
| Ogawa et al. [54] | Japan | A single arm pilot study | Contact needle therapy (CNT) | None | 1. Chemotherapy-Induced Peripheral Neuropathy (CIPN): Common Terminology Criteria for Adverse Events (CTCAE), Functional Assessment of Cancer Therapy/Gynecologic Oncology Group -Neurotoxicity (FACT/GOG-NTX) 2. Breakthrough pain: Numerical Rating Scale (0–4) 3. Patients’ objective evaluation | CNT may improve the symptoms of CIPN and associated side effects during the course of chemotherapy and even after a long interval since the last chemotherapy. CNT might be considered one of the safe and effective alternative methods for CIPN. | No mention |
| Greenlee et al. [55] | USA | A randomized controlled trial | Electro-acupuncture (EA) | Sham electro-acupuncture | 1. Pain: Brief Pain Inventory-Short Form (BPI-SF) 2. Quality of life: Functional Assessment of Cancer Therapy- Taxane (FACT-TAX) 3. Neurotoxicity: Functional Assessment of Cancer Therapy-neurotoxicity (FACT-NTX) 4. Peripheral neuropathic pain: Neuropathic Pain Scale (NPS) 5. Sensory neuropathy: biothesiometer 6. Motor neurologic dysfunction: grooved pegboard test | In this randomized, sham-controlled trial of EA to prevent CIPN in women receiving taxane-based chemotherapy for early stage breast cancer treatment, we did not observe differences in pain or neuropathy symptoms between treatment arms at 12 weeks. Unexpectedly, compared to SEA subjects, women on EA experienced greater increases in pain at 4 weeks after taxane completion. No differences were observed between groups with regard to taxane adherence | One adverse event was reported, which was a grade 1 acupuncture needle site reaction with discomfort, minor swelling, and bruising after acupuncture needle withdrawal. |
| Bao et al. [56] | USA | A single-arm clinical trial | Acupuncture | None | 1. Chemotherapy-Induced Peripheral Neuropathy (CIPN): NCI-CTCAE CIPN grade, Functional Assessment of Cancer Therapy/Gynecologic Oncology Group-Neurotoxicity (FACT/GOG-Ntx), Neuropathic Pain Scale (NPS) 2. Vibration sensation test 3. brain-derived neurotrophic factors (BDNF) | Acupuncture was safe and showed preliminary evidence of effectiveness in reducing the incidence of high grade CIPN during chemotherapy | Acupuncture was safe, and tolerable; the only toxicity noted was that four of 27 (15%) patients reported mild bruising. |
| Jeong et al. [57] | Korea | A prospective single-arm observational study | Acupuncture | None | 1. Chemotherapy-Induced Peripheral Neuropathy (CIPN): Neuropathic Pain Symptom Inventory (NPSI), Nerve Conduction Study (NCS) 2. Quality of life: 36-Item Short From Health Survey (SF-36) | Acupuncture improved symptoms of CIPN and QoL in Korean women suffering from peripheral neuropathy after chemotherapy for breast cancer. | All participants were well adapted to acupuncture treatment during the entire treatment period. No serious adverse events were reported |
| Lu et al. [29] | USA | Randomized controlled trial | Acupuncture | Waitlist | 1. Chemotherapy-Induced Peripheral Neuropathy (CIPN): Patient Neurotoxicity Questionnaire (PNQ) 2. CIPN-specific quality of life (QOL): Functional Assessment of Cancer Therapy-Neurotoxicity (FACT-NTX) 3. Neuropathic pain: Brief Pain Inventory-short form (BPI-SF) | 8-week acupuncture intervention, versus usual care, led to clinically meaningful and statistically significant improvements in neuropathic sensory symptoms in breast cancer survivors with mild and moderate CIPN after the completion of chemotherapy. | There were no serious adverse events reported in response to the acupuncture intervention in either the immediate acupuncture group or in the waitlist control group. Two participants (one in each group) reported mild reactions that were possibly related to the acupuncture: one developed grade 1 pruritis in the feet, and one developed grade 2 joint pain. |
| Rostocket al. [58] | Switzerland | A Prospective observational study | Isopropanolic extract of black cohosh (1–4 tablets, 2.5 mg) | None | Menopause rating scale (MRS II) | The reduction of the total MRS II score under black cohosh treatment from 17.6 to 13.6 was statistically significant. | Only one adverse event (nausea) was possibly related to the study medication. |
| Ben-Arye et al. [59] | Isarael | case report | Cimicifuga racemosa herbal capsules & Acupuncture | None | 1. Quality of life: Edmonton Symptom Assessment Scale (ESAS) 2. Headache, hot flashes, well-being: Measure Yourself Concerns and Wellbeing questionnaire (MYCAW) | Improved fatigue, nausea, anxiety, drowsiness, dyspnea, appetite, sleep, well-being on ESAS scores and headache, hot flashes and well-being on MYCAW scores | No mention |
| Lin et al. [60] | Taiwan | single arm prospective test | Acupuncture | None | 1. Quality of life: Medical Outcomes Study 12-Item Short-Form Health Survey (SF-12) 2. Patient satisfaction questionnaire | Most patients were satisfied with the program. SF-12 showed improvement significantly at the end of study. | No serious adverse effect was reported. |
| Zhu [61] | China | Case report | Yiqi Yangyin Jiedu Decoction | None | Symptoms of debilitation, waist pain, restlessness at night, loss of appetite, constipation, dry mouth, and bitter mouth | The patient has no bone pain with good appetite and spirit, and gained 11 kg in weight. The treatment has a good clinical effect for eight years | No mention |
| Saghatel-yan et al. [62] | Armenia4. BMD showed no apparent change after 12 weeks for both groups | Randomized controlled trial | Curcumin (CUC-1®, 300 mg solution, once per week) | Placebo | 1. Objective response rate (ORR) by Response Evaluation Criteria in Solid Tumors (RECIST) 2. Physical condition (PC): ECOG performance status 3. Patient-reported quality of life (QOL): European Organization for Research and Treatment of Cancer (EORTC) quality of life questionnaire (QLQ), patient’s self-assessment questionnaire (QLQ-C30 version 1.0) 4. Carcinoembryonic antigen (CEA) and cancer antigen 15-3 (Ca 15-3) | Curcumin in combination with paclitaxel is efficacious in the treatment of advanced and metastatic breast cancer. | No mention |
| Study | Sample Size (Male/ Female) (If RCT, Randomized) | Age (Treatment /Control) | Disease Duration | Main Symptoms | Type of Anticancer Treatment | Target Disease | ||
|---|---|---|---|---|---|---|---|---|
| AI side effects | ||||||||
| Chino et al. [34] | 1(0/1) | 55 | 9 years | atypical genital bleeding from vaginal mucosa and joint pain of bilateral hands and knees | total mastectomy Chemotherapy anastrozole | AI side effects | ||
| Beuth et al. [35] | 680 (0/680) | 58.3 | Unknown | mucosal dryness and arthralgia | adjuvant hormone therapy | AI side effects | ||
| Oh et al. [36] | 32(0/32) | <45 12 (86)/14 (93) ≥ 45 2 (14)/1(7) | ≤5 years 11 (79)/13 (87) >5 years 3(21)/2(13) | pain and/or stiffness in one or more joints | Aromatase inhibitors | AI side effects | ||
| Mao et al. [37] | 76(0/76) | 59.7 | Unknown | fatigue, sleep, and psychological distress | Aromatase inhibitor | AI side effects | ||
| Mao et al. [38] | 67(0/67) | 57.5 ± 10.1/60.9 ± 6.5/60.6 ± 8.2 | Unknown | Arthralgia | Aromatase inhibitors | AI side effects | ||
| Li et al. [39] | 72(0/72) | 55(27–73)/ 52(31–72) | Unknown | Pain, quality of life | Adjuvant chemotherapy Adjuvant taxane Aromatase inhibitors (Anastrozole Letrozole Exemestane) | AI side effects | ||
| Peng et al. [40] | 84(0/84) | 57.3(46–74) /59.3(43–76) | Unknown | musculoskeletal symptoms (arthralgia and/or stiffness and/or swelling in one or more joints, bone pain, myalgia, carpal tunnel syndrome, trigger finger) | Aromatase inhibitors Prior tamoxifen Anastrozole Letrozole Exemestane | AI side effects | ||
| Zhang et al. [41] | 30(0/30) | 59.3 ± 8.4 | Unknown | Arthralgia Bone pain Myalgia Morning stiffness Carpal tunnel syndrome Trigger finger | Aromatase inhibitor Anastrozole Letrozole Exemestane | AI side effects | ||
| Kim et al. [42] | 8(0/8) | 40–49: 2 50–59: 5 60–69: 1 | Unknown | AI-related arthralgia (particularly knee pain), Vasomotor symptoms, including hot flushes and sweating after anti-estrogen therapy, Insomnia, Sexual dysfunction (vaginal dryness, dyspareunia), Post-mastectomy pain of the chest wall or shoulder | aromatase inhibitors, five were taking anti-estrogen agents, two were receiving sedatives and two were taking analgesics | AI side effects, General pain | ||
| Rostock et al. [58] | 50(0/50) | 56 (43–77) | 8.6 (+ 6.2) month | climacteric complaints | Tamoxifen | AI side effects | ||
| Lin et al. [60] | 45(0/45) | 53.3 ± 8.3 | Unknown | Fatigue, arthralgia, nausea, and insomnia | hormonal therapy (Tamoxifen, Anastrozole) | AI induced symptoms | ||
| Lymphedema | ||||||||
| Cassileth et al. [43] | 37(0/37) | 55(55/65) | Unknown | Upper-limb lymphedema | breast-cancer surgery | Lymphedema | ||
| Jeong et al. [44] | 9(0/9) | 58.44 ± 7.21 | Duration of lymph-edema (month) 67.44 38.12 | lymphedema | breast-cancer surgery | Lymphedema | ||
| Bao et al. [45] | 82(0/82) | 65(54–71)/ 58(49–70) | Duration of lymph-edema 2.5/2.2 | lymphedema | breast-cancer surgery | Lymphedema | ||
| Type of breast cancer surgery | ||||||||
| Lumpectomy | 10 (25%) | 11 (26%) | ||||||
| Mastectomy | 30 (75%) | 31 (74%) | ||||||
| Type of axillary surgery | ||||||||
| Sentinel lymph node biopsy | 2 (5%) | 0 (0%) | ||||||
| Axillary lymph node dissection | 37 (93%) | 42 (100%) | ||||||
| Unknown | 1 (2%) | 0 (0%) | ||||||
| Wang et al. [46] | 75(0/75) | 59.90 ± 7.02/ 56.96 ± 5.33 | Unknown | lymphedema | breast-cancer surgery Breast conserving surgery (right) Breast cancer modified radical mastectomy (right) Radical mastectomy (right) Total mastectomy (right) Breast conserving surgery (left) Breast cancer modified radical mastectomy (left) Total mastectomy | Lymphedema | ||
| Wang et al. [47] | 48(0/48) | 59.42 ± 7.02/58.25 ± 6.19 | Unknown | Lymphedema, Fatigue | breast-cancer surgery Breast conserving surgery (right) Breast cancer modified radical mastectomy (right) Total mastectomy (right) Breast cancer modified radical mastectomy (left) Total mastectomy (left) | Lymphedema | ||
| Han et al. [48] | 10(0/10) | 53.0 (45.0–60.0) /- | Unknown | Lymphedema (arm circumference, shoulder range of motion), Quality of life | breast-cancer surgery | Lymphedema | ||
| Post-mastectomy symptoms | ||||||||
| Bauml et al. [49] | 1(0/1) | 47 | 4 years | postmastectomy pain syndrome, fatigue, depressed mood | breast-cancer surgery | Post-mastectomy pain | ||
| Mallory et al. [50] | 20(0/20) | Unknown | Unknown | anxiety, tension/muscular discomfort and pain | mastectomy and/or breast reconstruction | Post-mastectomy pain | ||
| Giron et al. [51] | 48(0/48) | 53.7 ± 11.1 (total) | Unknown | Lymphedema, (Pain, arm circumference, shoulder range of motion) depression | breast-cancer surgery Quadrantectomy Mastectomy Immediate reconstruction | Post-mastectomy pain | ||
| Quinlan-Wood-ward et al. [52] | 30(0/30) | 53.7± 9.4/62.5± 11.5 | Unknown | Pain, Nausea, Anxiety, and Coping | mastectomy | Post-mastectomy pain | ||
| Ao et al. [53] | 70(0/70) | 45.6 ± 9.8/46.9 ± 8.6 | Unknown | Pain, postoperative nausea and vomiting, pruritus, dizziness and headache | mastectomy | Post-mastectomy pain | ||
| Zhu [61] | 1 | 51 | 11 years | Debilitation, waist pain, restlessness at night, loss of appetite, constipation, dry mouth, and bitter mouth | Breast surgery | General symptoms | ||
| Chemotherapy-Induced Peripheral Neuropathy (CIPN) | ||||||||
| Ogawa et al. [54] | 6(0/6) | 64.3 | Unknown | Pain, quality of life | Chemotherapy (taxanes and oxaliplatin) | Chemotherapy-Induced Peripheral Neuropathy | ||
| Greenlee et al. [55] | 63(0/63) | 51.8 ± 10.7 /48.3 ± 12.0 | Unknown | Pain, quality of life | Taxane | Chemotherapy-Induced Peripheral Neuropathy | ||
| Bao et al. [56] | 109 (0/109) | 47(39–53) | Unknown | Pain, quality of life | paclitaxel | Chemotherapy-Induced Peripheral Neuropathy | ||
| Jeong et al. [57] | 10(0/10) | 58.7 ± 7.5 | Unknown | Pain, quality of life | Taxane | Chemotherapy-Induced Peripheral Neuropathy | ||
| Lu et al. [29] | 40(0/40) | 54.0(32.0–68.0) /53.5(36.0–71.0) | 17.3 (1.4–92.0) month/13.3 (5.3–92.4) month | Pain, quality of life | Taxane | Chemotherapy-induced Peripheral Neuropathy | ||
| Chemotherapy induced symptoms | ||||||||
| Ben-Arye et al. [59] | 1(0/1) | 27 | Unknown | hot flashes, insomnia, quality of life | palliative chemotherapy with docetaxel | Chemo-therapy induced symptoms | ||
| Saghatel-yan et al. [62] | 150 (0/150) | 57.59/54.17 | Unknown | Quality of life | adjuvant or neoadjuvant chemotherapy | Chemo-therapy induced symptoms | ||
| Study | Intervention | Acupoint | Frequency | Treatment Period |
|---|---|---|---|---|
| Oh et al. [36] | Electro-acupuncture | Day 1: LI4, LI11, GB34, ST40, LR3, GV20, Shishencong, Baxie Day 2: GB21, TE5, ST36, SP6, LR3, GV20, Shishencong, Baxie pain and stiffness of the arms and hands: LI11, LI4, GB21, TE5, the Baxie extra point pain and stiffness of the legs and feet: GB34, ST36, ST40, SP6, LR3 stress levels and cognitive function: GV20, Shishencong. LR3 immune function: ST36, LI4 | 1.20 min, 2.alternating frequencies of 2–10 Hz | 1. twice weekly for 6 weeks 2. total, 12 sessions |
| Mao et al. [37] | Electro-acupuncture | A Shi point and at least four distant points (the acupuncturist chose at least four local points around the joint with the most pain. Additionally, at least four distant points were used to address non-pain symptoms, such as depression/anxiety and fatigue, that are commonly seen in conjunction with pain) | 1. 30 min 2. 2 Hz | 1. twice a week for two weeks, then weekly for six more weeks, for a total of ten treatments over eight weeks 2. total, 10 sessions. |
| Kim et al. [42] | Manual acupuncture & Electro-acupuncture & Auricular acupuncture | 1. AI-related arthralgia (particularly knee pain MA: LI4, LR3, GB39, SP6 EA: SP10-SP9, ST34-ST36, GB33-GB34 2. Vasomotor symptoms, including hot flushes and sweating after anti-oestrogen therapy MA: GB20, HT7, LR3, PC6, SP6, SP9, ST36 EA: BL23-BL32 AA: Shenmen, Internal secretion 3. Insomnia MA: Sishencong, GV20, HT7, PC6, SP6, BL62, KI6 AA: Shenmen 4. Sexual dysfunction (vaginal dryness, dyspareunia) MA: PC6, ST30, ST36, SP6, LI4, LR3, CV2, CV4 EA: BL32-BL33 AA: Shenmen 5. Post-mastectomy pain of the chest wall or shoulder MA: LI4, LI11, PC6, ST36, HT7 plus Ah shi points EA: Jiaji (point selection based on dermatomes affected by the lesion) AA: Shenmen, Internal secretion | 1. 20 min 2. Low-frequency (2 Hz) and high-intensity (nearly 80% of the patient’s pain threshold) stimulation was used for EA | 1. giving a total of 8–12 sessions during the 4-week study period |
| Cassileth et al. [43] | Manual acupuncture | TE14, LI15, LU5, CV12, CV3, LI4, ST36, SP6 | 1. 30 min 2. rotation of the needles with lift and thrust | 1. twice weekly for 30 min over 4 consecutive weeks 2. total, 8 sessions |
| Jeong et al. [44] | Manual acupuncture | KI10, LR8, LU8, LR4, HT8, LR2, KI2, LU5, LR8, LR1, SP3, SP2, HT9, HT3, HT7, LU10, SP1, SP5, SP9, LU9, KI7, KI3, KI1, PC9, PC3, PC7, PC8, BL66, LI1, SI5, BL60, LI2, GB43, GB44, GB38, GB41, ST36, ST41, SI3, SI2, SI8, LI11, ST44, BL67 BL40, BL65, TE3, TE2, TE10, TE6 (identifying a pattern of each patient’s symptoms and signs, target meridian and acupuncture points were selected for each patient. Basic combination formulas of Saam acupuncture were determined according to the pattern, which is relevant to one of four syndromes) | 1. 30—5 min at each session. 2. manipulated manually to obtain De Qi | 1. 6 weeks of the treatment with 3 acupuncture sessions per week 2. total, 18 sessions |
| Bao et al. [45] | Manual acupuncture | CV12, CV3, TE14, LI15, LU5, LI4, ST36, SP6 | 1. lasted 30 min 2. De-qi sensation was achieved at certain acupoints, such as LI4 and ST36 | 1. twice a week for six consecutive weeks. 2. total, 12 sessions |
| Wang et al. [46] | Bloodletting puncture and cupping | LI14, LI13, LU6, HT2, TE5, SI9, PC3, or ashi points (the most swollen areas or subcutaneous nodules) on the affected arm | 1. 15 min, | 1. every 5 days for 15 min/session |
| Wang et al. [47] | Moxibustion | LI14,LI13, TE5, SI9, BL23, and any Ashi points | 1. 30 min | 1. 4 consecutive weeks. 2. 30 min every 2 days |
| Han et al. [48] | Electronic Moxibustion | LI14, LI11, TE5 | 1. 30 min | 1.8 consecutive weeks 2. twice per week for 8 weeks |
| Bauml et al. [49] | Manual acupuncture | distal points: GV20, LI4, SP6, BL60 | 1. 20 min~30 min 2. needling manipulation until de qi sensation was achieved. | 1. weekly for eight treatment sessions. |
| Mallory et al. [50] | Manual acupuncture | GV20, EX-HN3, LI4, LI11, PC6, SP10, SP6, ST36, LR3, GB40 | De-qi sensation | No mention |
| Giron et al. [51] | Manual acupuncture | CV3, SP9, ST36, KI7, LR3, GB21, LI15, HT14, LU5, LI 4, ST 38, BL 60 | 30 min | 1. once a week for 10 weeks 2. 10 sessions |
| Quinlan-Woodward et al. [52] | Manual acupuncture | No mention | 36 min | No mention |
| Ao et al. [53] | Transcutaneous electrical acupoint stimulation (TEAS) | LI4, PC6, ST36 | 1.30 min 2. dense-and-disperse frequency of 2/100 Hz | 1. TEAS was performed for 30 min prior to the induction of anesthesia. 2. Postoperative TEAS was performed for 30 min each time at 4 and 12 h post-surgery on the day of surgery, and administered three times (8 a.m., 2 p.m. and 8 p.m.) daily at postoperative days 1 and 2. |
| Ogawa et al. [54] | Contact needle therapy | 1. Points for all patients: CV12, CV4, ST25, KI2 2. Selected points: LR8, LR14, SP3, LR13, LU9, LU1, KI7, GB25, PC7, CV17, CV6, CV4, ST36, LU1, BL20, BL13, BL18, BL23 | 30–60 s | 4–6 sessions |
| Greenlee et al. [55] | Electroacupuncture | GB34, ST36, LI4, LI10, L3, L5, Ba Feng, C5, C7, Ba Xie | 1. 30 min 2. 2 Hz of mixed pulsatile intervals 3. De qi sensation | 1. 16 sessions 2. once a week for 16 weeks |
| Bao et al. [56] | Manual acupuncture & Auricular acupuncture | MA: LI4, TE5, LI11, ST40, Ba Feng AA: shen men, point zero, and two additional auricular acupuncture points where electrodermal signal was detected | 30 min De qi sensation | No mention |
| Jeong et al. [57] | Manual acupuncture | LI 4, LI 11, ST 36, LR3, M-UE-9 (Ba Xie), M-LE8 (Ba Feng) | 1. 25 ± 5 min at each session. 2. gently manipulated manually to obtain De Qi, | 1. 8 weeks 2. 4 weeks of acupuncture treatment and 4 weeks of follow-up after the last treatment. 3. 3 times a week during the first 4 consecutive weeks. |
| Lu et al. [29] | Manual acupuncture (MA) & Electroacupuncture (EA) | MA: Yin Tang, LI11, SP9, ST36, K3, Qiduan EA: TE5, Baxie, SP6, LR3 | 1. De Qi sensation 2. alternating 2–10 Hz 3. 30 min each session | 1. 18 sessions of acupuncture over 8 weeks, |
| Ben-Arye et al. [59] | Acupuncture & Herbal medicine | No mention | 15 min | No mention |
| Zhu et al. [60] | auricle acupuncture & manual acupuncture & Electro-acupuncture & transcutaneous nerve stimulation (TENS) & Silver Spike Point (SSP) | face: S7 shoulder: GB21, LI15, SI11 upper extremities: LI11, LI10, TE5, LI4 lower extremities: SP10, ST36, SP9, KI7 | 1. 2 and 100 Hz, alternatively | 1. 6 sessions 2. 2 to 3 times per week |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, G.; Lee, Y.-S.; Jang, H.J.; Kim, S.-Y.; Lee, Y.J.; Ha, I.-H. Symptom Management and Quality of Life of Breast Cancer Patients Using Acupuncture-Related Therapies and Herbal Medicine: A Scoping Review. Cancers 2022, 14, 4683. https://doi.org/10.3390/cancers14194683
Han G, Lee Y-S, Jang HJ, Kim S-Y, Lee YJ, Ha I-H. Symptom Management and Quality of Life of Breast Cancer Patients Using Acupuncture-Related Therapies and Herbal Medicine: A Scoping Review. Cancers. 2022; 14(19):4683. https://doi.org/10.3390/cancers14194683
Chicago/Turabian StyleHan, Gajin, Ye-Seul Lee, Hee Jae Jang, Song-Yi Kim, Yoon Jae Lee, and In-Hyuk Ha. 2022. "Symptom Management and Quality of Life of Breast Cancer Patients Using Acupuncture-Related Therapies and Herbal Medicine: A Scoping Review" Cancers 14, no. 19: 4683. https://doi.org/10.3390/cancers14194683
APA StyleHan, G., Lee, Y.-S., Jang, H. J., Kim, S.-Y., Lee, Y. J., & Ha, I.-H. (2022). Symptom Management and Quality of Life of Breast Cancer Patients Using Acupuncture-Related Therapies and Herbal Medicine: A Scoping Review. Cancers, 14(19), 4683. https://doi.org/10.3390/cancers14194683





