Identification of a Biomarker Combination for Survival Stratification in pStage II/III Gastric Cancer after Curative Resection
Abstract
Simple Summary
Abstract
1. Introduction
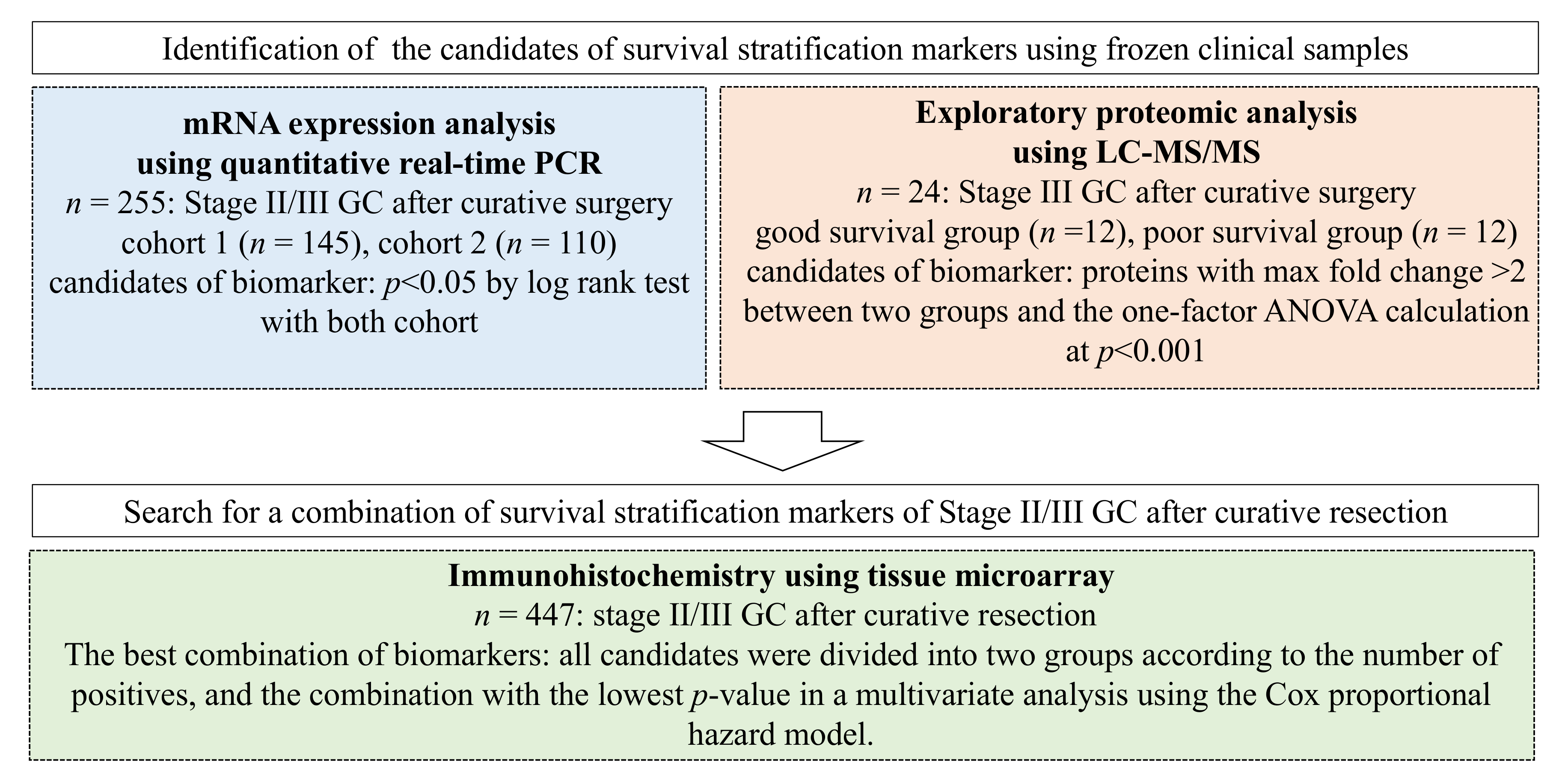
2. Materials and Methods
2.1. Search for Candidate Biomarkers for Risk Stratification by Quantitative Real-Time PCR (qPCR) in Patients Who Underwent Curative Resection of GC
2.1.1. Patients and Samples
2.1.2. RNA Extraction and Complementary DNA (cDNA) Synthesis
2.1.3. Quantitative Real-Time PCR (qPCR)
2.1.4. Gene Selection
2.1.5. Statistical Analysis
2.2. Identification of Candidate Markers for Risk Stratification after Radical Resection of GC by Exploratory Proteome Analysis Using Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS)
2.2.1. Patients and Samples
2.2.2. Sample Preparation for MS-Based Proteomics
2.2.3. LC-MS/MS Analysis
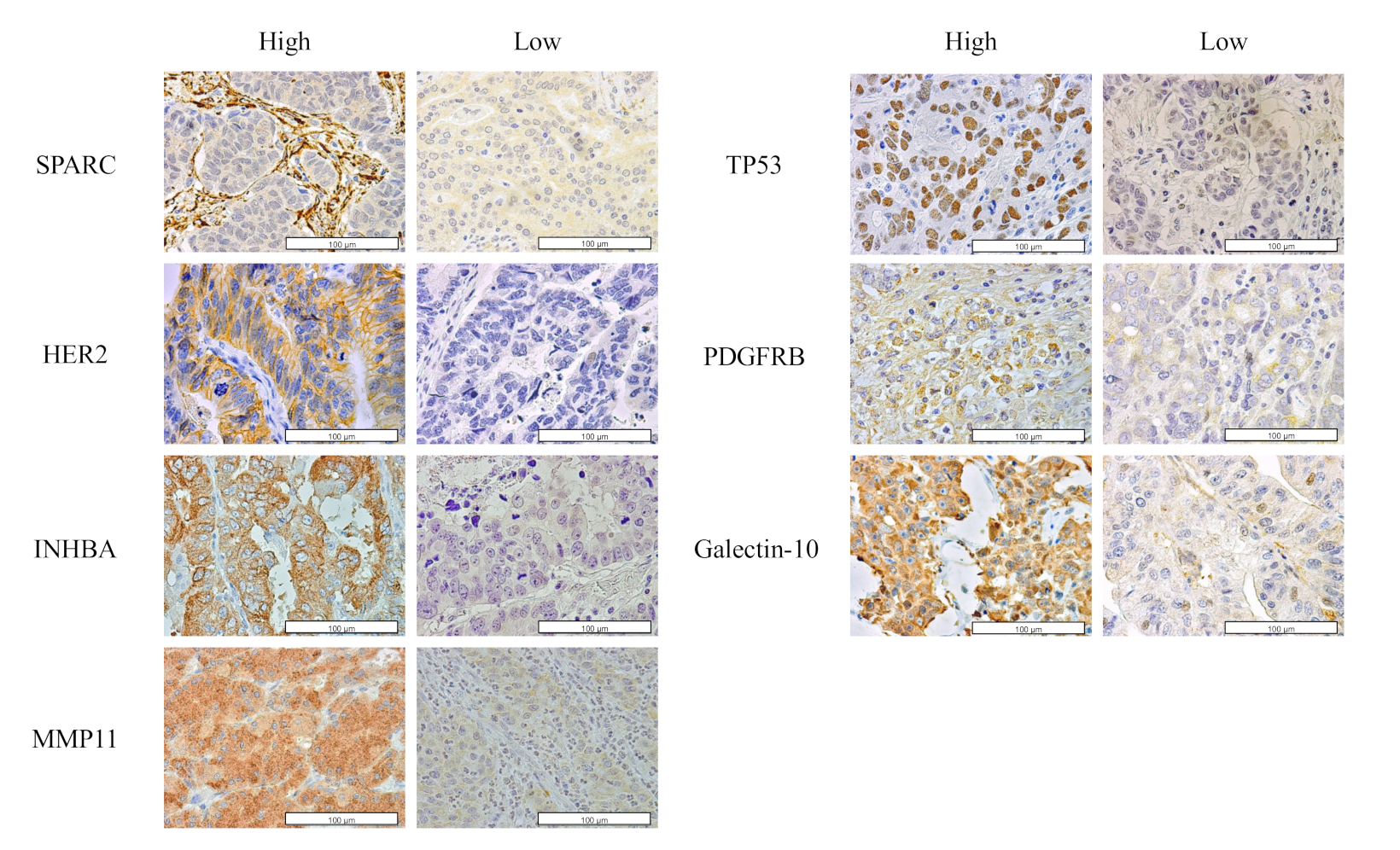
2.3. Tissue Microarray Analysis (TMA)
2.3.1. Patients and Samples
2.3.2. IHC Analysis Using TMA
2.3.3. Statistical Analysis
3. Results
3.1. Identification of Candidate Markers for Risk Stratification
3.2. Proteomic Analysis of Candidate Survival Stratification Biomarkers
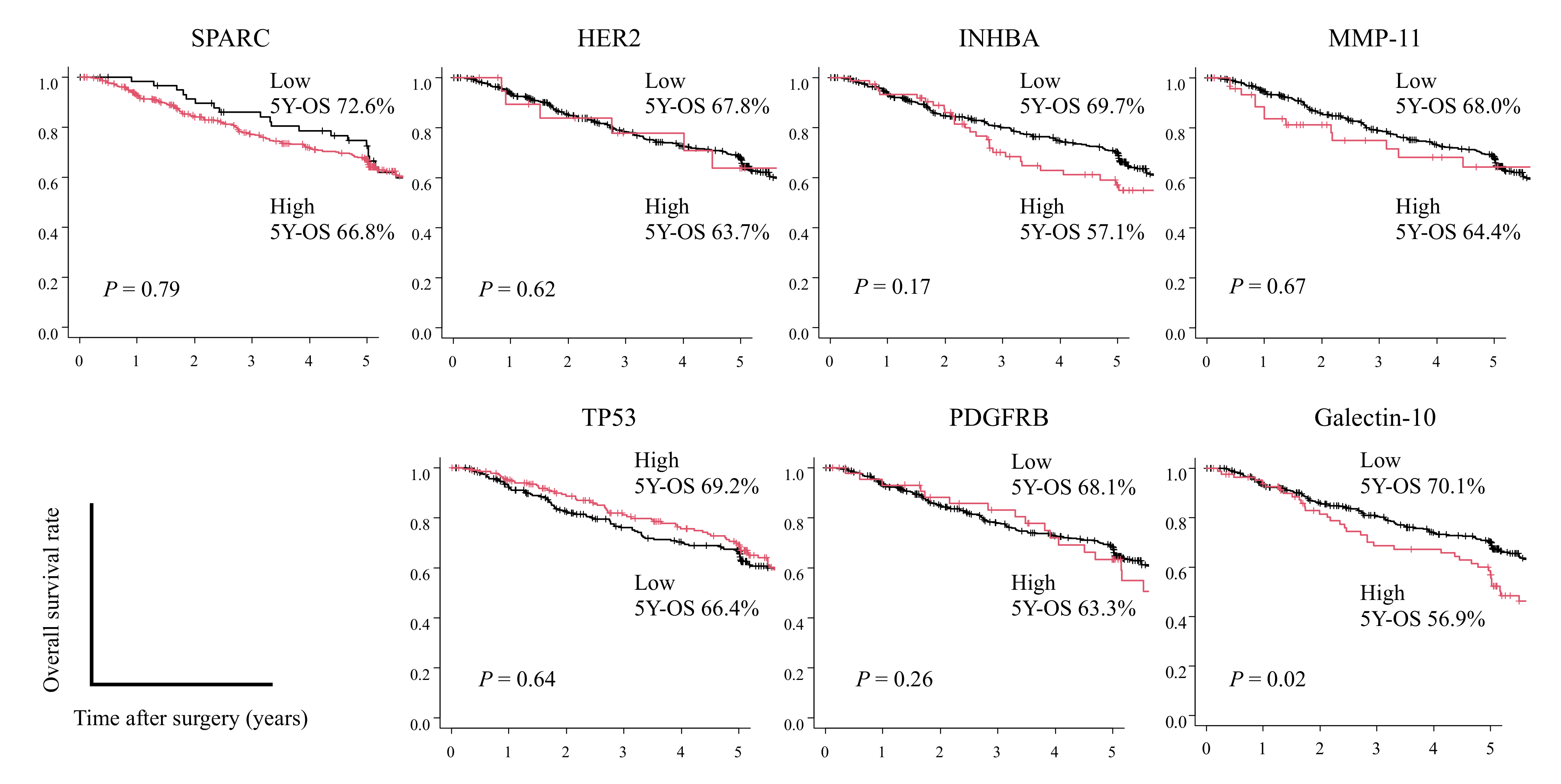
3.3. Identification of the Best Combination of Candidate Survival Stratification Markers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France, 2020; Available online: https://gco.iarc.fr/today (accessed on 17 February 2021).
- Sakuramoto, S.; Sasako, M.; Yamaguchi, T.; Kinoshita, T.; Fujii, M.; Nashimoto, A.; Furukawa, H.; Nakajima, T.; Ohashi, Y.; Imamura, H.; et al. Adjuvant Chemotherapy for Gastric Cancer with S-1, an Oral Fluoropyrimidine. N. Engl. J. Med. 2007, 357, 1810–1820. [Google Scholar] [CrossRef] [PubMed]
- Sasako, M.; Sakuramoto, S.; Katai, H.; Kinoshita, T.; Furukawa, H.; Yamaguchi, T.; Nashimoto, A.; Fujii, M.; Nakajima, T.; Ohashi, Y. Five-Year Outcomes of a Randomized Phase III Trial Comparing Adjuvant Chemotherapy With S-1 Versus Surgery Alone in Stage II or III Gastric Cancer. J. Clin. Oncol. 2011, 29, 4387–4393. [Google Scholar] [CrossRef] [PubMed]
- Bang, Y.-J.; Kim, Y.-W.; Yang, H.-K.; Chung, H.; Park, Y.-K.; Lee, K.H.; Lee, K.-W.; Kim, Y.H.; Noh, S.-I.; Cho, J.Y.; et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): A phase 3 open-label, randomised controlled trial. Lancet 2012, 379, 315–321. [Google Scholar] [CrossRef]
- Noh, S.H.; Park, S.R.; Yang, H.-K.; Chung, H.C.; Chung, I.-J.; Kim, S.-W.; Kim, H.-H.; Choi, J.-H.; Kim, H.-K.; Yu, W.; et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014, 15, 1389–1396. [Google Scholar] [CrossRef]
- Yoshida, K.; Kodera, Y.; Kochi, M.; Ichikawa, W.; Kakeji, Y.; Sano, T.; Nagao, N.; Takahashi, M.; Takagane, A.; Watanabe, T.; et al. Addition of Docetaxel to Oral Fluoropyrimidine Improves Efficacy in Patients With Stage III Gastric Cancer: Interim Analysis of JACCRO GC-07, a Randomized Controlled Trial. J. Clin. Oncol. 2019, 37, 1296–1304. [Google Scholar] [CrossRef] [PubMed]
- Ichikawa, W.; Terashima, M.; Ochiai, A.; Kitada, K.; Kurahashi, I.; Sakuramoto, S.; Katai, H.; Sano, T.; Imamura, H.; Sasako, M. Impact of insulin-like growth factor-1 receptor and amphiregulin expression on survival in patients with stage II/III gastric cancer enrolled in the Adjuvant Chemotherapy Trial of S-1 for Gastric Cancer. Gastric Cancer 2017, 20, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Terashima, M.; Kitada, K.; Ochiai, A.; Ichikawa, W.; Kurahashi, I.; Sakuramoto, S.; Katai, H.; Sano, T.; Imamura, H.; Sasako, M.; et al. Impact of Expression of Human Epidermal Growth Factor Receptors EGFR and ERBB2 on Survival in Stage II/III Gastric Cancer. Clin. Cancer Res. 2012, 18, 5992–6000. [Google Scholar] [CrossRef]
- Sasako, M.; Terashima, M.; Ichikawa, W.; Ochiai, A.; Kitada, K.; Kurahashi, I.; Sakuramoto, S.; Katai, H.; Sano, T.; Imamura, H. Impact of the expression of thymidylate synthase and dihydropyrimidine dehydrogenase genes on survival in stage II/III gastric cancer. Gastric Cancer 2015, 18, 538–548. [Google Scholar] [CrossRef][Green Version]
- Cheong, J.-H.; Yang, H.-K.; Kim, H.; Kim, W.H.; Kim, Y.-W.; Kook, M.-C.; Park, Y.-K.; Kim, H.-H.; Lee, H.S.; Lee, K.H.; et al. Predictive test for chemotherapy response in resectable gastric cancer: A multi-cohort, retrospective analysis. Lancet Oncol. 2018, 19, 629–638. [Google Scholar] [CrossRef]
- Sundar, R.; Kumarakulasinghe, N.B.; Chan, Y.H.; Yoshida, K.; Yoshikawa, T.; Miyagi, Y.; Rino, Y.; Masuda, M.; Guan, J.; Sakamoto, J.; et al. Machine-learning model derived gene signature predictive of paclitaxel survival benefit in gastric cancer: Results from the randomised phase III SAMIT trial. Gut 2022, 71, 676–685. [Google Scholar] [CrossRef]
- Oshima, T.; Tsuburaya, A.; Yoshida, K.; Yoshikawa, T.; Miyagi, Y.; Rino, Y.; Masuda, M.; Guan, J.; Tan, P.; Grabsch, H.I.; et al. Gastric cancer biomarker analysis in patients treated with different adjuvant chemotherapy regimens within SAMIT, a phase III randomized controlled trial. Sci. Rep. 2022, 12, 8509. [Google Scholar] [CrossRef] [PubMed]
- Tan, I.B.; Ivanova, T.; Lim, K.H.; Ong, C.W.; Deng, N.; Lee, J.; Tan, S.H.; Wu, J.; Lee, M.H.; Ooi, C.H.; et al. Intrinsic Subtypes of Gastric Cancer, Based on Gene Expression Pattern, Predict Survival and Respond Differently to Chemotherapy. Gastroenterology 2011, 141, 476–485.e1–11. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Fang, W.-L.; Huang, K.-H.; Chen, M.-H.; Liu, C.-A.; Hung, Y.-P.; Chao, Y.; Tai, L.-C.; Lo, S.-S.; Li, A.F.-Y.; Wu, C.-W.; et al. Comparative study of the 7th and 8th AJCC editions for gastric cancer patients after curative surgery. PLoS ONE 2017, 12, e0187626. [Google Scholar] [CrossRef]
- Masuda, T.; Tomita, M.; Ishihama, Y. Phase Transfer Surfactant-Aided Trypsin Digestion for Membrane Proteome Analysis. J. Proteome Res. 2008, 7, 731–740. [Google Scholar] [CrossRef]
- Rappsilber, J.; Ishihama, Y.; Mann, M. Stop and Go Extraction Tips for Matrix-Assisted Laser Desorption/Ionization, Nanoelectrospray, and LC/MS Sample Pretreatment in Proteomics. Anal. Chem. 2003, 75, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Ueki, S.; Tokunaga, T.; Melo, R.C.N.; Saito, H.; Honda, K.; Fukuchi, M.; Konno, Y.; Takeda, M.; Yamamoto, Y.; Hirokawa, M.; et al. Charcot-Leyden crystal formation is closely associated with eosinophil extracellular trap cell death. Blood 2018, 132, 2183–2187. [Google Scholar] [CrossRef] [PubMed]
- Kubach, J.; Lutter, P.; Bopp, T.; Stoll, S.; Becker, C.; Huter, E.; Richter, C.; Weingarten, P.; Warger, T.; Knop, J.; et al. Human CD4+CD25+ regulatory T cells: Proteome analysis identifies galectin-10 as a novel marker essential for their anergy and suppressive function. Blood 2007, 110, 1550–1558. [Google Scholar] [CrossRef]
- Gaddy-Kurten, D.; Tsuchida, K.; Vale, W. Activins and the Receptor Serine Kinase Superfamily. Recent Prog. Horm. Res. 1995, 50, 109–129. [Google Scholar] [CrossRef]
- Vale, W.; Rivier, C.; Hsueh, A.; Campen, C.; Meunier, H.; Bicsak, T.; Vaughan, J.; Corrigan, A.; Bardin, W.; Sawchenko, P.; et al. Chemical and Biological Characterization of the Inhibin Family of Protein Hormones. In Recent Progress in Hormone Research; Academic Press: Cambridge, MA, USA, 1988; Volume 44, pp. 1–34. [Google Scholar] [CrossRef]
- Ying, S.-Y. Inhibins, Activins, and Follistatins: Gonadal Proteins Modulating the Secretion of Follicle-Stimulating Hormone. Endocr. Rev. 1988, 9, 267–293. [Google Scholar] [CrossRef]
- Seachrist, D.D.; Keri, R.A. The Activin Social Network: Activin, Inhibin, and Follistatin in Breast Development and Cancer. Endocrinology 2019, 160, 1097–1110. [Google Scholar] [CrossRef] [PubMed]
- Seder, C.W.; Hartojo, W.; Lin, L.; Silvers, A.L.; Wang, Z.; Thomas, D.G.; Giordano, T.J.; Chen, G.; Chang, A.C.; Orringer, M.B.; et al. INHBA Overexpression Promotes Cell Proliferation and May Be Epigenetically Regulated in Esophageal Adenocarcinoma. J. Thorac. Oncol. 2009, 4, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Wen, Y.-G.; Li, D.-P.; Xia, J.; Zhou, C.-Z.; Yan, D.-W.; Tang, H.-M.; Peng, Z.-H. Upregulated INHBA expression is associated with poor survival in gastric cancer. Med. Oncol. 2012, 29, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Oshima, T.; Yoshihara, K.; Aoyama, T.; Hasegawa, S.; Sato, T.; Yamamoto, N.; Akito, N.; Shiozawa, M.; Yoshikawa, T.; Numata, K.; et al. Relation of INHBA gene expression to outcomes in gastric cancer after curative surgery. Anticancer Res. 2014, 34, 2303–2309. [Google Scholar] [PubMed]
- Katayama, Y.; Oshima, T.; Sakamaki, K.; Aoyama, T.; Sato, T.; Masudo, K.; Shiozawa, M.; Yoshikawa, T.; Rino, Y.; Imada, T.; et al. Clinical Significance of INHBA Gene Expression in Patients with Gastric Cancer who Receive Curative Resection Followed by Adjuvant S-1 Chemotherapy. In Vivo 2017, 31, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Rio, M.-C. Stromelysin-3, a particular member of the matrix metalloproteinase family. In Proteases and Their Inhibitors in Cancer Metastasis. Cancer Metastasis—Biology and Treatment; Foidart, J.-M., Muschel, R.J., Eds.; Springer Netherlands: Dordrecht, The Netherlands, 2002; pp. 81–107. [Google Scholar]
- Deng, H.; Guo, R.-F.; Li, W.-M.; Zhao, M.; Lu, Y.-Y. Matrix metalloproteinase 11 depletion inhibits cell proliferation in gastric cancer cells. Biochem. Biophys. Res. Commun. 2005, 326, 274–281. [Google Scholar] [CrossRef]
- Motrescu, E.R.; Blaise, S.; Etique, N.; Messaddeq, N.; Chenard, M.-P.; Stoll, I.; Tomasetto, C.; Rio, M.-C. Matrix metalloproteinase-11/stromelysin-3 exhibits collagenolytic function against collagen VI under normal and malignant conditions. Oncogene 2008, 27, 6347–6355. [Google Scholar] [CrossRef]
- Andarawewa, K.L.; Motrescu, E.R.; Chenard, M.-P.; Gansmuller, A.; Stoll, I.; Tomasetto, C.; Rio, M.-C. Stromelysin-3 Is a Potent Negative Regulator of Adipogenesis Participating to Cancer Cell-Adipocyte Interaction/Crosstalk at the Tumor Invasive Front. Cancer Res. 2005, 65, 10862–10871. [Google Scholar] [CrossRef]
- Yang, Y.-H.; Deng, H.; Li, W.-M.; Zhang, Q.-Y.; Hu, X.-T.; Xiao, B.; Zhu, H.-H.; Geng, P.-L.; Lu, Y.-Y. Identification of Matrix Metalloproteinase 11 as a Predictive Tumor Marker in Serum Based on Gene Expression Profiling. Clin. Cancer Res. 2008, 14, 74–81. [Google Scholar] [CrossRef]
- Yan, D.; Dai, H.; Liu, J.-W. Serum levels of MMP-11 correlate with clinical outcome in Chinese patients with advanced gastric adenocarcinoma. BMC Cancer 2011, 11, 151. [Google Scholar] [CrossRef]
- Yan, Q.; Sage, E.H. SPARC, a Matricellular Glycoprotein with Important Biological Functions. J. Histochem. Cytochem. 1999, 47, 1495–1505. [Google Scholar] [CrossRef] [PubMed]
- Lane, T.F.; Sage, E.H. The biology of SPARC, a protein that modulates cell-matrix interactions. FASEB J. 1994, 8, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-S.; Lin, K.-H.; Chen, S.-L.; Chan, Y.-F.; Hsueh, S. Overexpression of SPARC gene in human gastric carcinoma and its clinic–pathologic significance. Br. J. Cancer 2004, 91, 1924–1930. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Oshima, T.; Yamamoto, N.; Yamada, T.; Hasegawa, S.; Yukawa, N.; Numata, K.; Kunisaki, C.; Tanaka, K.; Shiozawa, M.; et al. Clinical significance of SPARC gene expression in patients with gastric cancer. J. Surg. Oncol. 2013, 108, 364–368. [Google Scholar] [CrossRef]
- Östman, A. PDGF receptors-mediators of autocrine tumor growth and regulators of tumor vasculature and stroma. Cytokine Growth Factor Rev. 2004, 15, 275–286. [Google Scholar] [CrossRef]
- Raja, U.M.; Gopal, G.; Shirley, S.; Ramakrishnan, A.S.; Rajkumar, T. Immunohistochemical expression and localization of cytokines/chemokines/growth factors in gastric cancer. Cytokine 2017, 89, 82–90. [Google Scholar] [CrossRef]
- Wang, J.X.; Zhou, J.F.; Huang, F.K.; Zhang, L.; He, Q.L.; Qian, H.Y.; Lai, H.L. GLI2 induces PDGFRB expression and mod-ulates cancer stem cell properties of gastric cancer. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 3857–3865. [Google Scholar]
- Higuchi, A.; Oshima, T.; Yoshihara, K.; Sakamaki, K.; Aoyama, T.; Suganuma, N.; Yamamoto, N.; Sato, T.; Cho, H.; Shiozawa, M.; et al. Clinical significance of platelet-derived growth factor receptor-β gene expression in stage II/III gastric cancer with S-1 adjuvant chemotherapy. Oncol. Lett. 2017, 13, 905–911. [Google Scholar] [CrossRef]

| Variables/Categories | Population 1 (n = 145) | Population 2 (n = 110) | p-Value | |
|---|---|---|---|---|
| Age | <70 y | 77 | 57 | 0.8387 |
| ≧70 y | 68 | 53 | ||
| Sex | male | 95 | 76 | 0.5476 |
| female | 50 | 34 | ||
| Histological type | well/moderately/ | 65 | 48 | 0.8496 |
| poorly | 80 | 62 | ||
| Tumor size | <65 mm | 76 | 61 | 0.6296 |
| ≧65 mm | 69 | 49 | ||
| Depth of invasion | pT1 | 4 | 4 | 0.0752 |
| pT2 | 19 | 16 | ||
| pT3 | 54 | 25 | ||
| pT4 | 68 | 65 | ||
| Lymph node metastasis | pN0, pN1 | 98 | 76 | 0.7982 |
| pN2, pN3 | 47 | 34 | ||
| venous invasion | (−) | 53 | 20 | 0.4895 |
| (+) | 92 | 68 | ||
| lymphatic invasion | (−) | 46 | 33 | 0.3666 |
| (+) | 99 | 55 | ||
| pStage | II | 63 | 31 | 0.2149 |
| III | 82 | 57 | ||
| Adjuvant chemotherapy | (−) | 65 | 33 | 0.272 |
| (+) | 80 | 55 | ||
| T4a Nx M0, StageIII, Curative Resection and Adjuvant Chemotherapy with S-1 for 1 Year | ||||
|---|---|---|---|---|
| Variables/Categories | Recurrence and Death < 3 Years (n = 12) | Relapse-Free Survival > 5 Years (n = 12) | p-Value | |
| Age | (mean SD) | 66.25 (8.04) | 64.58 (8.11) | 0.618 |
| Sex | male | 3 (25.0) | 4 (33.3) | 1.000 |
| female | 9 (75.0) | 8 (66.7) | ||
| Histological type | diffuse | 8 (66.7) | 10 (83.3) | 0.640 |
| intestinal | 4 (33.3) | 2 (16.7) | ||
| pStage | IIIA | 4 (33.3) | 2 (16.7) | 0.413 |
| IIIB | 1 (8.3) | 4 (33.3) | ||
| IIIC | 7 (58.3) | 6 (50.0) | ||
| Survival time (days) | (mean SD) | 675.42 (249.95) | 1931.17 (76.48) | <0.001 |
| Gene | Population 1 | Population 2 | ||
|---|---|---|---|---|
| Hazard Ratio | p-Value | Hazard Ratio | p-Value | |
| SPARC | 2.651 | 0.0022 | 2.876 | 0.0121 |
| ERBB2 | 2.632 | 0.0073 | 2.245 | 0.0281 |
| INHBA | 5.93 | 0.0031 | 2.274 | 0.0241 |
| MMP11 | 4.02 | <0.0001 | 2.217 | 0.0578 |
| TP53 | 2.386 | 0.0146 | 1.704 | 0.1708 |
| PDGFRB | 2.687 | 0.0261 | 1.611 | 0.1954 |
| Accession | Description | Gene Name | Peptide Number | Anova (p) | Max Fold Change |
|---|---|---|---|---|---|
| P09486 | SPARC | SPARC | 1 | 0.00059 | 2.32 |
| Q05315 | Galectin-10 | CLC | 1 | 0.00038 | 2.61 |
| Factors | Number of Patients | Univariate | p-Value | Multivariate | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| HR | 95%CI | HR | 95%CI | |||||
| Age | ≦65 | 217 | 1 | 1 | ||||
| >65 | 230 | 1.42 | 1.08–1.88 | 0.014 | 1.38 | 1.04–1.83 | 0.025 | |
| Sex | female | 134 | 1 | |||||
| male | 313 | 1.12 | 0.82–1.51 | 0.482 | ||||
| Histological type | well/moderately/ | 193 | 1 | |||||
| poorly | 254 | 1.07 | 0.81–1.41 | 0.643 | ||||
| Lymphatic invasion | (−) | 132 | 1 | |||||
| (+) | 315 | 0.96 | 0.71–1.29 | 0.780 | ||||
| Venous invasion | (−) | 128 | 1 | |||||
| (+) | 319 | 1.26 | 0.93–1.71 | 0.138 | ||||
| Stage | II | 170 | 1 | 1 | ||||
| III | 277 | 1.46 | 1.10–1.94 | 0.009 | 1.47 | 1.11–1.96 | 0.008 | |
| Combination of survival stratification markers * | 0–1 | 394 | 1 | 1 | ||||
| 2–4 | 53 | 1.82 | 1.21–2.72 | 0.004 | 1.71 | 1.14–2.56 | 0.010 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hashimoto, I.; Kimura, Y.; Oue, N.; Hiroshima, Y.; Aoyama, T.; Rino, Y.; Yokose, T.; Yasui, W.; Miyagi, Y.; Oshima, T. Identification of a Biomarker Combination for Survival Stratification in pStage II/III Gastric Cancer after Curative Resection. Cancers 2022, 14, 4427. https://doi.org/10.3390/cancers14184427
Hashimoto I, Kimura Y, Oue N, Hiroshima Y, Aoyama T, Rino Y, Yokose T, Yasui W, Miyagi Y, Oshima T. Identification of a Biomarker Combination for Survival Stratification in pStage II/III Gastric Cancer after Curative Resection. Cancers. 2022; 14(18):4427. https://doi.org/10.3390/cancers14184427
Chicago/Turabian StyleHashimoto, Itaru, Yayoi Kimura, Naohide Oue, Yukihiko Hiroshima, Toru Aoyama, Yasushi Rino, Tomoyuki Yokose, Wataru Yasui, Yohei Miyagi, and Takashi Oshima. 2022. "Identification of a Biomarker Combination for Survival Stratification in pStage II/III Gastric Cancer after Curative Resection" Cancers 14, no. 18: 4427. https://doi.org/10.3390/cancers14184427
APA StyleHashimoto, I., Kimura, Y., Oue, N., Hiroshima, Y., Aoyama, T., Rino, Y., Yokose, T., Yasui, W., Miyagi, Y., & Oshima, T. (2022). Identification of a Biomarker Combination for Survival Stratification in pStage II/III Gastric Cancer after Curative Resection. Cancers, 14(18), 4427. https://doi.org/10.3390/cancers14184427





