Clinical Effectiveness of Faecal Immunochemical Test in the Early Detection of Colorectal Cancer—An Umbrella Review
Abstract
:Simple Summary
Abstract
1. Introduction
- Colon—600,896 in men (13.1), 547,619 in women (10.0);
- Rectum—443,358 in men (9.8), 288,852 in women (5.6) [1].
- OC-Sensor—quantitative (test principle: latex agglutination, measured as optical change);
- OC-Light—qualitative (immunochromatographic);
- OC-Hemodia—quantitative (latex agglutination, measured as optical change) or qualitative (visual particle agglutination) [4].
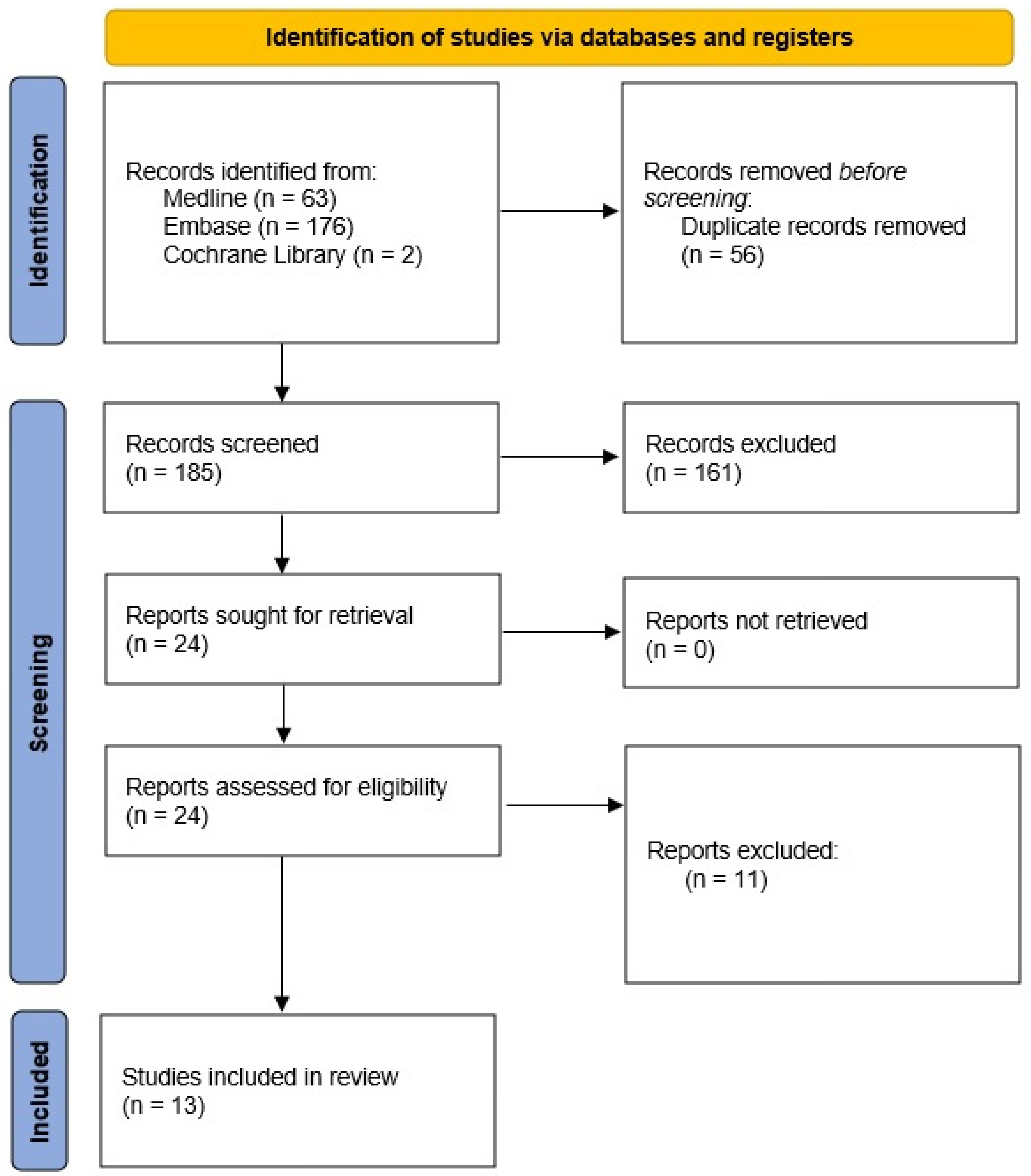
2. Material and Method
- defining the criteria for including studies for reviews;
- development/verification of a research report search strategy;
- searching for sources of medical information/updating of searching for sources of medical information;
- finding full texts of scientific reports that are potentially useful in clinical analysis;
- selection of studies based on inclusion criteria for the review;
- research results development;
- qualitative synthesis consisting of the analysis of the statistical and clinical relevance of the results of studies included in the analysis.
- population: general adult population;
- interventions: FIT;
- alternative technologies (comparators): unlimited;
- methodologies: meta-analyzes of randomised and/or observational trials; systematic reviews of randomised and/or observational studies;
- endpoints: to assess the sensitivity, specificity, and clinical efficacy of FIT.
3. Results
- Forbes 2021—a systematic review based on 8 observational studies, which analysed the impact of specific time intervals from a positive FIT result to colonoscopy on the presence of CRC, the presence of advanced CRC at diagnosis, overall mortality, and CRC mortality [7];
- Lin 2021—a meta-analysis of 223 publications (RCT and observational studies), which analysed the effectiveness and diagnostic precision of tests, and harms related to CRC screening as part of the USPSTF recommendation [8];
- Mutneja 2021a—5 RCT meta-analyses comparing the effectiveness of FIT with sigmoidoscopy in screening for CRC [9];
- Mutneja 2021b—a meta-analysis of 6 observational studies, evaluating the influence of the time after a positive colonoscopy following faecal occult blood test on CRC detection [10];
- Gini 2020—a systematic review of 18 RCTs and observational studies comparing the impact of CRC screening on mortality in European regions [11];
- Meklin 2020—a meta-analysis of 31 single-arm clinical trials assessing the diagnostic precision of FIT and gFOBT in screening tests [12];
- Niedermaier 2020—a meta-analysis of 44 observational studies, determining the diagnostic precision of FIT depending on the stage of CRC stage [13];
- Zhong 2020—6 RCT meta-analyses comparing the effectiveness of FIT and colonoscopy in detecting CRC in the intermediate-risk population [14];
- Imperiale 2019—a meta-analysis of 31 observational studies, defining the diagnostic precision of FIT in the detection of CRC and advanced colorectal adenomas in people from the intermediate risk group undergoing screening colonoscopy [15];
- Selby 2019—a meta-analysis of 46 observational studies, defining the diagnostic precision of FIT in the detection of CRC and advanced colorectal adenoma at different diagnostic thresholds in regards to gender and age [16];
- Stonestreet 2019—a meta-analysis of 17 observational studies, assessing the diagnostic precision of FIT in the detection of CRC in symptomatic and asymptomatic people [17];
- Katsoula 2017—a meta-analysis of 1 RCT and 11 observational studies, determining the diagnostic precision of FIT in the detection of CRC or advanced neoplasia of the large intestine in asymptomatic people at high risk [18];
- Zhang 2017—a meta-analysis of 44 RCTs and observational studies, evaluating the effectiveness of screening methods in preventing CRC disease and death [19];
3.1. Sensitivity and Specificity of FIT in the Detection of CRC
3.2. Reporting for Screening and CRC-Related Detection, Occurrence, and Deaths
3.3. Time of Colonoscopy Measured from Positive FIT Result
4. Discussion
5. Review Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation. GBD Results Tool: Colon and Rectum Cancer. Available online: https://ghdx.healthdata.org/gbd-results-tool (accessed on 27 March 2022).
- Kanth, P.; Inadomi, J.M. Screening and prevention of colorectal cancer. BMJ 2021, 374, n1855. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.S.; Piper, M.A.; Perdue, L.A.; Rutter, C.M.; Webber, E.M.; O’Connor, E.; Smith, N.; Whitlock, E.P. Screening for Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2016, 315, 2576–2594. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions; Version 6.2; The Cochrane Collaboration in London: London, UK, 2021. [Google Scholar]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include andomized or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Forbes, N.; Hilsden, R.J.; Martel, M.; Ruan, Y.; Dube, C.; Rostom, A.; Shorr, R.; Menard, C.; Brenner, D.R.; Barkun, A.N.; et al. Association Between Time to Colonoscopy After Positive Fecal Testing and Colorectal Cancer Outcomes: A Systematic Review. Clin. Gastroenterol. Hepatol. 2021, 19, 1344–1354.e8. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.S.; Perdue, L.A.; Henrikson, N.B.; Bean, S.I.; Blasi, P.R. Screening for Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2021, 325, 1978–1998. [Google Scholar] [CrossRef]
- Mutneja, H.; Agrawal, R.; Bhurwal, A.; Arora, S.; Go, A.; Attar, B. Comparative Effectiveness of Fecal Immunochemical Tests versus Flexible Sigmoidoscopy for Colorectal Cancer Screening: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J. Gastrointest. Liver Dis. 2021, 30, 267–273. [Google Scholar] [CrossRef]
- Mutneja, H.R.; Bhurwal, A.; Arora, S.; Vohra, I.; Attar, B.M. A delay in colonoscopy after positive fecal tests leads to higher incidence of colorectal cancer: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2021, 36, 1479–1486. [Google Scholar] [CrossRef]
- Gini, A.; Jansen, E.E.L.; Zielonke, N.; Meester, R.G.S.; Senore, C.; Anttila, A.; Segnan, N.; Mlakar, D.N.; de Koning, H.J.; Lansdorp-Vogelaar, I.; et al. Impact of colorectal cancer screening on cancer-specific mortality in Europe: A systematic review. Eur. J. Cancer 2020, 127, 224–235. [Google Scholar] [CrossRef]
- Meklin, J.; Syrjänen, K.; Eskelinen, M. Fecal Occult Blood Tests in Colorectal Cancer Screening: Systematic Review and Meta-analysis of Traditional and New-generation Fecal Immunochemical Tests. Anticancer Res. 2020, 40, 3591–3604. [Google Scholar] [CrossRef]
- Niedermaier, T.; Balavarca, Y.; Brenner, H. Stage-Specific Sensitivity of Fecal Immunochemical Tests for Detecting Colorectal Cancer: Systematic Review and Meta-Analysis. Am. J. Gastroenterol. 2020, 115, 56–69. [Google Scholar] [CrossRef] [PubMed]
- Zhong, G.-C.; Sun, W.-P.; Wan, L.; Hu, J.-J.; Hao, F.-B. Efficacy and cost-effectiveness of fecal immunochemical test versus colonoscopy in colorectal cancer screening: A systematic review and meta-analysis. Gastrointest. Endosc. 2020, 91, 684–697.e15. [Google Scholar] [CrossRef] [PubMed]
- Imperiale, T.F.; Gruber, R.N.; Stump, T.E.; Emmett, T.W.; Monahan, P.O. Performance Characteristics of Fecal Immunochemical Tests for Colorectal Cancer and Advanced Adenomatous Polyps: A Systematic Review and Meta-analysis. Ann. Intern. Med. 2019, 170, 319–329. [Google Scholar] [CrossRef]
- Selby, K.; Levine, E.H.; Doan, C.; Gies, A.; Brenner, H.; Quesenberry, C.; Lee, J.K.; Corley, D.A. Effect of Sex, Age, and Positivity Threshold on Fecal Immunochemical Test Accuracy: A Systematic Review and Meta-analysis. Gastroenterology 2019, 157, 1494–1505. [Google Scholar] [CrossRef]
- Stonestreet, J.; Chandrapalan, S.; Woolley, D.; Uthman, U.; Arasaradnam, R.P. Systematic review and meta-analysis: Diagnostic accuracy of faecal immunochemical testing for haemoglobin (FIT) in detecting colorectal cancer for both symptomatic and screening population. Acta Gastro-Enterol. Belg. 2019, 82, 291–299. [Google Scholar]
- Katsoula, A.; Paschos, P.; Haidich, A.B.; Tsapas, A.; Giouleme, O. Diagnostic Accuracy of Fecal Immunochemical Test in Patients at Increased Risk for Colorectal Cancer: A Meta-analysis. JAMA Intern. Med. 2017, 177, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Cheng, Z.; Ma, Y.; He, C.; Lu, Y.; Zhao, Y.; Chang, X.; Zhang, Y.; Bai, Y.; Cheng, N. Effectiveness of Screening Modalities in Colorectal Cancer: A Network Meta-Analysis. Clin. Colorectal Cancer 2017, 16, 252–263. [Google Scholar] [CrossRef]
- Lopes, G.; Stern, M.C.; Temin, S.; Sharara, A.I.; Cervantes, A.; Costas-Chavarri, A.; Engineer, R.; Hamashima, C.; Ho, G.F.; Huitzil, F.D.; et al. Early Detection for Colorectal Cancer: ASCO Resource-Stratified Guideline. J. Glob. Oncol. 2019, 5, 1–22. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Population Screening: Evidence Summary and Recommendations (PSC1a-d). Available online: https://wiki.cancer.org.au/australia/Guidelines:Colorectal_cancer/Population_screening_recommendations (accessed on 10 January 2022).
- American Academy of Family Physicians. Colorectal Cancer Screening, Adults. Available online: https://www.aafp.org/family-physician/patient-care/clinical-recommendations/all-clinical-recommendations/colorectal-cancer-adults.html (accessed on 5 January 2022).
- Shaukat, A.; Kahi, C.J.; Burke, C.A.; Rabeneck, L.; Sauer, B.G.; Rex, D.K. ACG Clinical Guidelines: Colorectal Cancer Screening 2021. Am. J. Gastroenterol. 2021, 116, 458–479. [Google Scholar] [CrossRef]
- American Cancer Society. Guideline for Colorectal Cancer Screening. Available online: https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html (accessed on 5 January 2022).
- US Preventive Services Task Force. Colorectal Cancer: Screening. Available online: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening (accessed on 4 January 2022).
- Qaseem, A.; Crandall, C.J.; Lin, J.S.; Mustafa, R.A.; Clinical Guidelines Committee of the American College of Physicians; Forciea, M.A.; Fitterman, N.; Horwitch, C.A.; Kansagara, D.; Maroto, M.; et al. Screening for Colorectal Cancer in Asymptomatic Average-Risk Adults: A Guidance Statement from the American College of Physicians. Ann. Intern. Med. 2019, 171, 643–654. [Google Scholar] [CrossRef]
- American Society for Gastrointestinal Endoscopy. Colorectal Cancer Screening. Available online: https://www.asge.org/home/about-asge/newsroom/media-backgrounders-detail/colorectal-cancer-screening (accessed on 4 January 2022).
- Rex, D.K.; Boland, C.R.; Dominitz, J.A.; Giardiello, F.M.; Johnson, D.A.; Kaltenbach, T.; Levin, T.R.; Lieberman, D.; Robertson, D.J. Colorectal Cancer Screening: Recommendations for Physicians and Patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Am. J. Gastroenterol. 2017, 112, 1016–1030. [Google Scholar] [CrossRef]
- Canadian Task Force on Preventive Health Care. Screening for Colorectal Cancer (CRC). 2016. Available online: https://canadiantaskforce.ca/tools-resources/colorectal-cancer-clinician-recommendation-table/ (accessed on 10 January 2022).
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Colorectal Cancer Screening. 2021. Available online: https://www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf (accessed on 4 January 2022).
- Cunningham, C.; Leong, K.; Clark, S.; Plumb, A.; Taylor, S.; Geh, I.; Karandikar, S.; Moran, B. Association of Coloproctology of Great Britain & Ireland (ACPGBI): Guidelines for the Management of Cancer of the Colon, Rectum and Anus (2017)—Diagnosis, Investigations and Screening. Colorectal Dis. 2017, 19 (Suppl. S1), 9–17. [Google Scholar]
- Jenkins, M.A.; Ouakrim, D.A.; Boussioutas, A.; Hopper, J.L.; Ee, H.C.; Emery, J.D.; Macrae, F.A.; Chetcuti, A.; Wuellner, L.; St John, D.J.B. Revised Australian National Guidelines for Colorectal Cancer Screening: Family History. Available online: https://www.mja.com.au/system/files/issues/209_10/10.5694mja18.00142.pdf (accessed on 4 January 2022).
- Cancer Council Australia. Clinical Practice Guidelines for the Prevention, Early Detection Management of Colorectal Cancer. Available online: https://wiki.cancer.org.au/australiawiki/images/e/ed/Colorectal_cancer_guidelines_short_form.pdf (accessed on 5 January 2022).
- The Royal Australian College of General Practitioners. Guidelines for Preventive Activities in General Practice. Colorectal Cancer. Available online: https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/guidelines-for-preventive-activities-in-general-pr/early-detection-of-cancers/colorectal-cancer (accessed on 5 January 2022).
- United Kingdom National Screening Committee. Adult Screening Program. Bowel Cancer. 2018. Available online: https://view-health-screening-recommendations.service.gov.uk/bowel-cancer/ (accessed on 10 January 2022).
- Robertson, D.J.; Lee, J.K.; Boland, C.R.; Dominitz, J.A.; Giardiello, F.M.; Johnson, D.A.; Kaltenbach, T.; Lieberman, D.; Levin, T.; Rex, D. Recommendations on Fecal Immunochemical Testing to Screen for Colorectal Neoplasia: A Consensus Statement by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2017, 152, 1217–1237.e3. [Google Scholar] [CrossRef] [PubMed]
- British Columbia Guidelines. Colorectal Screening for Cancer Prevention in Asymptomatic Patients. Available online: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/colorectal-cancer-screening (accessed on 10 January 2022).
- Cardoso, R.; Guo, F.; Heisser, T.; Hoffmeister, M.; Brenner, H. Utilisation of Colorectal Cancer Screening Tests in European Countries by Type of Screening Offer: Results from the European Health Interview Survey. Cancers 2020, 12, 1409. [Google Scholar] [CrossRef] [PubMed]
- Navarro, M.; Nicolas, A.; Ferrandez, A.; Lanas, A. Colorectal cancer population screening programs worldwide in 2016: An update. World J. Gastroenterol. 2017, 23, 3632–3642. [Google Scholar] [CrossRef] [PubMed]
- International Agency for Research on Cancer. Cancer Screening and the European Union. 2017. Available online: https://screening.iarc.fr/Eureport.php (accessed on 10 January 2022).
- Quintero, E.; Castells, A.; Bujanda, L.; Cubiella, J.; Salas, D.; Lanas, Á.; Andreu, M.; Carballo, F.; Morillas, J.D.; Hernández, C.; et al. Colonoscopy versus Fecal Immunochemical Testing in Colorectal-Cancer Screening. N. Engl. J. Med. 2012, 366, 697–706. [Google Scholar] [CrossRef]
- Kaminski, M.F.; Bretthauer, M.; Zauber, A.G.; Kuipers, E.J.; Adami, H.-O.; van Ballegooijen, M.; Regula, J.; van Leerdam, M.; Stefansson, T.; Påhlman, L.; et al. The NordICC Study: Rationale and design of a randomized trial on colonoscopy screening for colorectal cancer. Laryngo-Rhino-Otologie 2012, 44, 695–702. [Google Scholar] [CrossRef]
- Ding, H.; Lin, J.; Xu, Z.; Chen, X.; Wang, H.H.X.; Huang, L.; Huang, J.; Zheng, Z.; Wong, M.C.S. A Global Evaluation of the Performance Indicators of Colorectal Cancer Screening with Fecal Immunochemical Tests and Colonoscopy: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 1073. [Google Scholar] [CrossRef]
- Program Badań Przesiewowych Raka Jelita Grubego. Available online: http://pbp.org.pl/program/statkieta/ (accessed on 10 January 2022).
- Khalili, F.; Najafi, B.; Mansour-Ghanaei, F.; Yousefi, M.; Abdollahzad, H.; Motlagh, A. Cost-Effectiveness Analysis of Colorectal Cancer Screening: A Systematic Review. Risk Manag. Healthc. Policy 2020, 13, 1499–1512. [Google Scholar] [CrossRef]
- Areia, M.; Fuccio, L.; Hassan, C.; Dekker, E.; Dias-Pereira, A.; Dinis-Ribeiro, M. Cost-utility analysis of colonoscopy or faecal immunochemical test for population-based andomize colorectal cancer screening. United Eur. Gastroenterol. J. 2019, 7, 105–113. [Google Scholar] [CrossRef]
- Babela, R.; Orsagh, A.; Ricova, J.; Lansdorp-Vogelaar, I.; Csanadi, M.; De Koning, H.; Reckova, M. Cost-Effectiveness of Colorectal Cancer Screening in Slovakia. 2021. Available online: https://journals.lww.com/eurjcancerprev/Abstract/9000/Cost_effectiveness_of_colorectal_cancer_screening.99003.aspx (accessed on 25 January 2022).
- Brenner, H.; Tao, S. Superior diagnostic performance of faecal immunochemical tests for haemoglobin in a head-to-head comparison with guaiac based faecal occult blood test among 2235 participants of screening colonoscopy. Eur. J. Cancer 2013, 49, 3049–3054. [Google Scholar] [CrossRef] [PubMed]
- Hassan, C.; Rossi, P.G.; Camilloni, L.; Rex, D.K.; Jimenez-Cendales, B.; Ferroni, E.; Borgia, P.; Zullo, A.; Guasticchi, G.; HTA Group. Meta-analysis: Adherence to colorectal cancer screening and the detection rate for advanced neoplasia, according to the type of screening test. Aliment. Pharmacol. Ther. 2012, 36, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Hol, L.; van Leerdam, M.E.; van Ballegooijen, M.; van Vuuren, A.J.; van Dekken, H.; Reijerink, J.C.I.Y.; van der Togt, A.C.M.; Habbema, J.D.F.; Kuipers, E.J. Screening for colorectal cancer: Andomized trial comparing guaiac-based and immunochemical faecal occult blood testing and flexible sigmoidoscopy. Gut 2010, 59, 62–68. [Google Scholar] [CrossRef]
- Dancourt, V.; Lejeune, C.; Lepage, C.; Gailliard, M.C.; Meny, B.; Faivre, J. Immunochemical faecal occult blood tests are superior to guaiac-based tests for the detection of colorectal neoplasms. Eur. J. Cancer 2008, 44, 2254–2258. [Google Scholar] [CrossRef]
- Von Karsa, L.; Patnick, J.; Segnan, N.; Atkin, W.; Halloran, S.; Lansdorp-Vogelaar, I.; Malila, N.; Minozzi, S.; Moss, S.; Quirke, P.; et al. European guidelines for quality assurance in colorectal cancer screening and diagnosis: Overview and introduction to the full supplement publication. Endoscopy 2013, 45, 51–59. [Google Scholar] [PubMed]
- Tran, T.N.; Peeters, M.; Hoeck, S.; Van Hal, G.; Janssens, S.; De Schutter, H. Optimizing the colorectal cancer screening programme using faecal immunochemical test (FIT) in Flanders, Belgium from the “interval cancer” perspective. Br. J. Cancer 2022, 126, 1091–1099. [Google Scholar] [CrossRef]
- Zorzi, M.; Hassan, C.; Senore, C.; Capodaglio, G.; Turrin, A.; Narne, E.; Mussato, A.; Rizzato, S.; Chinellato, E.; Zamberlan, S.; et al. Interval colorectal cancers after negative faecal immunochemical test in a 13-year screening programme. J. Med Screen. 2021, 28, 131–139. [Google Scholar] [CrossRef]
- Toes-Zoutendijk, E.; Kooyker, A.I.; Dekker, E.; Spaander, M.C.; Winden, A.W.O.-V.; Ramakers, C.; Buskermolen, M.; van Vuuren, A.J.; Kuipers, E.J.; van Kemenade, F.J.; et al. Incidence of Interval Colorectal Cancer After Negative Results from First-Round Fecal Immunochemical Screening Tests, by Cutoff Value and Participant Sex and Age. Clin. Gastroenterol. Hepatol. 2020, 18, 1493–1500. [Google Scholar] [CrossRef]
- Portillo, I.; Arana-Arri, E.; Idigoras, I.; Bilbao, I.; Martinez, L.; Bujanda, L.; Gutierrez-Ibarluzea, I. Colorectal and interval cancers of the Colorectal Cancer Screening Program in the Basque Country (Spain). World J. Gastroenterol. 2017, 23, 2731–2742. [Google Scholar] [CrossRef]
- Zorzi, M.; Fedato, C.; Grazzini, G.; Stocco, F.C.; Banovich, F.; Bortoli, A.; Cazzola, L.; Montaguti, A.; Moretto, T.; Zappa, M.; et al. High sensitivity of five colorectal screening programmes with faecal immunochemical test in the Veneto Region, Italy. Gut 2011, 60, 944–949. [Google Scholar] [CrossRef]
- Mlakar, D.N.; Bric, T.K.; Škrjanec, A.L.; Krajc, M. Interval cancers after negative immunochemical test compared to screen and non-responders’ detected cancers in Slovenian colorectal cancer screening programme. Radiol. Oncol. 2018, 52, 413–421. [Google Scholar] [CrossRef] [PubMed]
- van der Vlugt, M.; Grobbee, E.J.; Bossuyt, P.M.; Bos, A.; Bongers, E.; Spijker, W.; Kuipers, E.J.; Lansdorp-Vogelaar, I.; Spaander, M.C.; Dekker, E. Interval Colorectal Cancer Incidence Among Subjects Undergoing Multiple Rounds of Fecal Immunochemical Testing. Gastroenterology 2017, 153, 439–447.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ibáñez-Sanz, G.; Milà, N.; Vidal, C.; Rocamora, J.; Moreno, V.; Sanz-Pamplona, R.; Garcia, M. Positive impact of a faecal-based screening programme on colorectal cancer mortality risk. PLoS ONE 2021, 16, e0253369. [Google Scholar] [CrossRef] [PubMed]
- Zorzi, M.; Gennaro, N.; Capodaglio, G.; Urso, E.D.L.; Pucciarelli, S.; Memo, L.; Carpin, E.; Corti, M.; Rugge, M.; Fedeli, U. Colorectal cancer screening: The surgery rates they are a-changing. A nationwide study on surgical resections in Italy. Dig. Liver Dis. 2019, 51, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Zorzi, M.; Urso, E.D.L. Impact of colorectal cancer screening on incidence, mortality and surgery rates: Evidences from programs based on the fecal immunochemical test in Italy. Dig. Liver Dis. 2022. [Google Scholar] [CrossRef] [PubMed]
- Fedeli, U.; Zorzi, M.; Urso, E.D.; Gennaro, N.; Tos, A.P.D.; Saugo, M. Impact of fecal immunochemical test-based screening programs on proximal and distal colorectal cancer surgery rates: A natural multiple-baseline experiment. Cancer 2015, 121, 3982–3989. [Google Scholar] [CrossRef] [PubMed]
- Cubiella, J.; González, A.; Almazán, R.; Rodríguez-Camacho, E.; Zubizarreta, R.; Peña-Rey Lorenzo, I. Overtreatment in nonmalignant lesions detected in a colorectal cancer screening program: A retrospective cohort study. BMC Cancer 2021, 21, 869. [Google Scholar] [CrossRef]
| Author/Year | Number and Type of Studies | Population | FIT Cut-Off (µg/g) | FIT-Brand | Result | |||
|---|---|---|---|---|---|---|---|---|
| Description | Population Size | Sensitivity% (95% CI) | Specificity% (95% CI) | |||||
| Lin 2021 [8] (MA) | 13 observational studies | Asymptomatic people aged ≥ 40 years have a general risk of developing CRC | 44,887 | - | OC-Sensor | 74 (64–83) | 94 (93–96) | |
| 4 observational studies | 32,424 | OC-Light | 81 (70–91) | 93 (91–96) | ||||
| Meklin 2020 [12] (MA) | 24 observational studies | General | 87,073 | - | - | 86 (78–93) | 85 (81–88) | |
| Niedermaier 2020 [13] (MA) | 10 cohort studies | People at moderate risk of CRC (population screening) who underwent colonoscopy | 203 | - | - | I/A: 75 (56–88) | 87 (75–94) | |
| II/B: 77 (63–87) | ||||||||
| III/C: 85 (65–94) | ||||||||
| IV/D: 79 (42–95) | ||||||||
| 17 cohort studies | Symptomatic patients who underwent colonoscopy | 799 | - | - | I/A: 79 (68–86) | 87 (83–90) | ||
| II/B: 88 (80–93) | ||||||||
| III/C: 85 (75–91) | ||||||||
| IV/D: 87 (76–93) | ||||||||
| 11 case-control studies | Patients diagnosed with CRC who underwent colonoscopy | 1228 | - | - | I/A: 64 (50–76) | 89 (85–92) | ||
| II/B: 80 (74–84) | ||||||||
| III/C: 82 (77–87) | ||||||||
| IV/D: 79 (70–86) | ||||||||
| 27 cohort studies, 11 case-control studies | All of the above patients (Total) | 2230 | - | - | I/A: 73 (65–79) | 89 (85–92) | ||
| II/B: 80 (74–84) | ||||||||
| III/C: 82 (77–87) | ||||||||
| IV/D: 79 (70–86) | ||||||||
| Imperiale 2019 [15] (MA) | 10 observational studies | Asymptomatic people at moderate risk of CRC, at the age of screening (usually between 50 and 75 years of age) who have participated in colonoscopy screening | 8364 | <10 | - | 78 (63–88) | 90 (81–95) | |
| 16 observational studies | 50,892 | 10 | - | 91 (84–95) | 90 (86–93) | |||
| 7 observational studies | 12,727 | >10–<20 | - | 82 (63–92) | 93 (91–95) | |||
| 14 observational studies | 56,638 | 20 | - | 75 (61–86) | 95 (92–96) | |||
| 12 observational studies | 17,341 | >20 | - | 71 (56–83) | 95 (94–96) | |||
| 7 observational studies | 6715 | ≤10 | OC-Sensor | 86 (75–93) | 90 (86–93) | |||
| 4 observational studies | 3890 | >10–<20 | 81 (55–94) | 93 (91–93) | ||||
| 11 observational studies | 27,827 | 20 | 77 (66–85) | 94 (91–96) | ||||
| 7 observational studies | 4347 | >20 | 73 (48–89) | 95 (94–96) | ||||
| 5 observational studies | 3428 | 10 | OC-Light | 90 (72–97) | 91 (83–95) | |||
| 1 observational study | 4260 | ≤10 | OC-Hemodia | 89 (72–96) | 94 (93–95) | |||
| 1 observational study | 3090 | >10–<20 | 53 (32–73) | 87 (86–89) | ||||
| 1 observational study | 3794 | 20 | 25 (6–57) | 96 (96–97) | ||||
| 2 observational studies | 4260 | >20 | 70 (47–86) | 97 (96–97) | ||||
| Selby 2019 [16] (MA) | 18 observational studies | Asymptomatic adults screened for CRC | 447 * | ≤10 | - | 80 (76–83) | 91 (89–93) | |
| 26 observational studies | 432 * | >10–≤20 | - | 69 (63–75) | 94 (93–96) | |||
| 12 observational studies | 188 * | >10–≤30 | - | 73 (62–81) | 96 (95–97) | |||
| 8 observational studies | 188 * | >30 | - | 66 (55–75) | 96 (94–97) | |||
| 8 observational studies | 14,407 | ≤10 | OC-Sensor /OC-Micro | 31 (25–38) | 92 (88–95) | |||
| 13 observational studies | 49,510 | >10–≤20 | 71 (64–78) | 94 (92–96) | ||||
| 3 observational studies | 5029 | >20 | 64 (26–90) | 96 (95–97) | ||||
| 3 observational studies | 4267 | - | FOB Gold | 95 (60–100) | 90 (85–94) | |||
| 3 observational studies | 30,301 | - | Magstream | 91 (31–100) | 94 (92–95) | |||
| 6 observational studies | 67,894 | - | OC-Hemodia | 68 (47–83) | 96 (93–98) | |||
| 3 observational studies | Asymptomatic adults screened for CRC | Women | 1,459,185 | - | - | 81 (60–100) | 94 (91–97) | |
| Men | 1,459,185 | - | - | 77 (75–79) | 92 (89–95) | |||
| 3 observational studies | At the age of 50–59 | 1,393,499 | - | - | 85 (71–99) | 94 (92–97) | ||
| At the age of 60–69 | 1,393,499 | - | - | 73 (71–75) | 93 (90–96) | |||
| 46 observational studies | All of the above patients screened for CRC (Total) | 2,412,518 | - | - | 76 (72–80) | 94 (92–95) | ||
| Stonestreet 2019 [17] (MA) | 8 observational studies | Adults with symptoms of gastrointestinal disease and asymptomatic adults over 50 years of age | 34,186 | - | - | 69 (54–81) | 94 (94–95) | |
| Katsoula 2017 [18] (MA) | 1 RCT, 11 observational studies | Asymptomatic patients with a family history of CRC or a history of polypectomy | 4872 | - | - | 93 (53–99) | 91 (59–99) | |
| Author/Year | N Studies | Population | Screening Method | End Point | OR/RR Score (95% CI) ** | ||
|---|---|---|---|---|---|---|---|
| Description | Size (n/N) * | Intervention | Comparator | ||||
| Mutneja 2021a [9] (MA) | 5 RCT | Patients > 50 years of age | 65,368/122,264 (I); 47,025/114,498 (C) | FIT | FS | Reportability for screening | OR = 2.11 (1.29–3.44) |
| 266/65,368 (I); 255/47,025 (C) per protocol | CRC detection indicator | OR = 0.76 (0.61–0.96) | |||||
| 266/122,264 (I); 254/114,498 (C) intention-to-treat | OR = 1.15 (0.65–2.02) | ||||||
| Zhong 2020 [14] (MA) | 6 RCT | People at medium risk of CRC (aged 59–69) | 19,233/46,189 (I); 8081/36,853 (C) | FIT | Colonoscopy | Reportability for screening | RR = 1.73 (1.29–2.34) |
| 57/19,169 (I); 52/8043 (C) per protocol | CRC detection indicator | RR = 0.53 (0.33–0.83) | |||||
| 54/45,955 (I); 55/36,639 (C) intention-to-treat | RR = 0.73 (0.37–1.42) | ||||||
| Author/Year | Number of Studies | Population | Screening Method | End Point | RR Score (95% CI) * | |
|---|---|---|---|---|---|---|
| Characteristics of the Population | Population Size | |||||
| Lin 2021 [8] (MA) | cohort study | Asymptomatic people aged ≥40 years have a general risk of developing CRC | 5,417,699 | FIT | Death due to CRC | RR = 0.90 (0.84–0.95) |
| Gini 2020 [11] (SR) | 1 RCT | People invited to or participating in CRC screening | 10,283 | FS + FIT | RR = 0.75 (0.57–0.99) | |
| Zhang 2017 [19] (MA) | 1 case-control study, 2 cohort studies | General population with an average risk of developing CRC | 5,460,619 | FIT | RR = 0.41 (0.29–0.59) | |
| 2 cohort studies | 75,396 | FIT | Incidence of CRC | RR = 0.79 (0.69–0.92) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Świtalski, J.; Tatara, T.; Wnuk, K.; Miazga, W.; Karauda, D.; Matera, A.; Jabłońska, M.; Jopek, S.; Religioni, U.; Gujski, M. Clinical Effectiveness of Faecal Immunochemical Test in the Early Detection of Colorectal Cancer—An Umbrella Review. Cancers 2022, 14, 4391. https://doi.org/10.3390/cancers14184391
Świtalski J, Tatara T, Wnuk K, Miazga W, Karauda D, Matera A, Jabłońska M, Jopek S, Religioni U, Gujski M. Clinical Effectiveness of Faecal Immunochemical Test in the Early Detection of Colorectal Cancer—An Umbrella Review. Cancers. 2022; 14(18):4391. https://doi.org/10.3390/cancers14184391
Chicago/Turabian StyleŚwitalski, Jakub, Tomasz Tatara, Katarzyna Wnuk, Wojciech Miazga, Dagmara Karauda, Adrian Matera, Magdalena Jabłońska, Sylwia Jopek, Urszula Religioni, and Mariusz Gujski. 2022. "Clinical Effectiveness of Faecal Immunochemical Test in the Early Detection of Colorectal Cancer—An Umbrella Review" Cancers 14, no. 18: 4391. https://doi.org/10.3390/cancers14184391
APA StyleŚwitalski, J., Tatara, T., Wnuk, K., Miazga, W., Karauda, D., Matera, A., Jabłońska, M., Jopek, S., Religioni, U., & Gujski, M. (2022). Clinical Effectiveness of Faecal Immunochemical Test in the Early Detection of Colorectal Cancer—An Umbrella Review. Cancers, 14(18), 4391. https://doi.org/10.3390/cancers14184391







