Treatment Outcomes of Computer Tomography-Guided Brachytherapy in Cervical Cancer in Hong Kong: A Retrospective Review
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
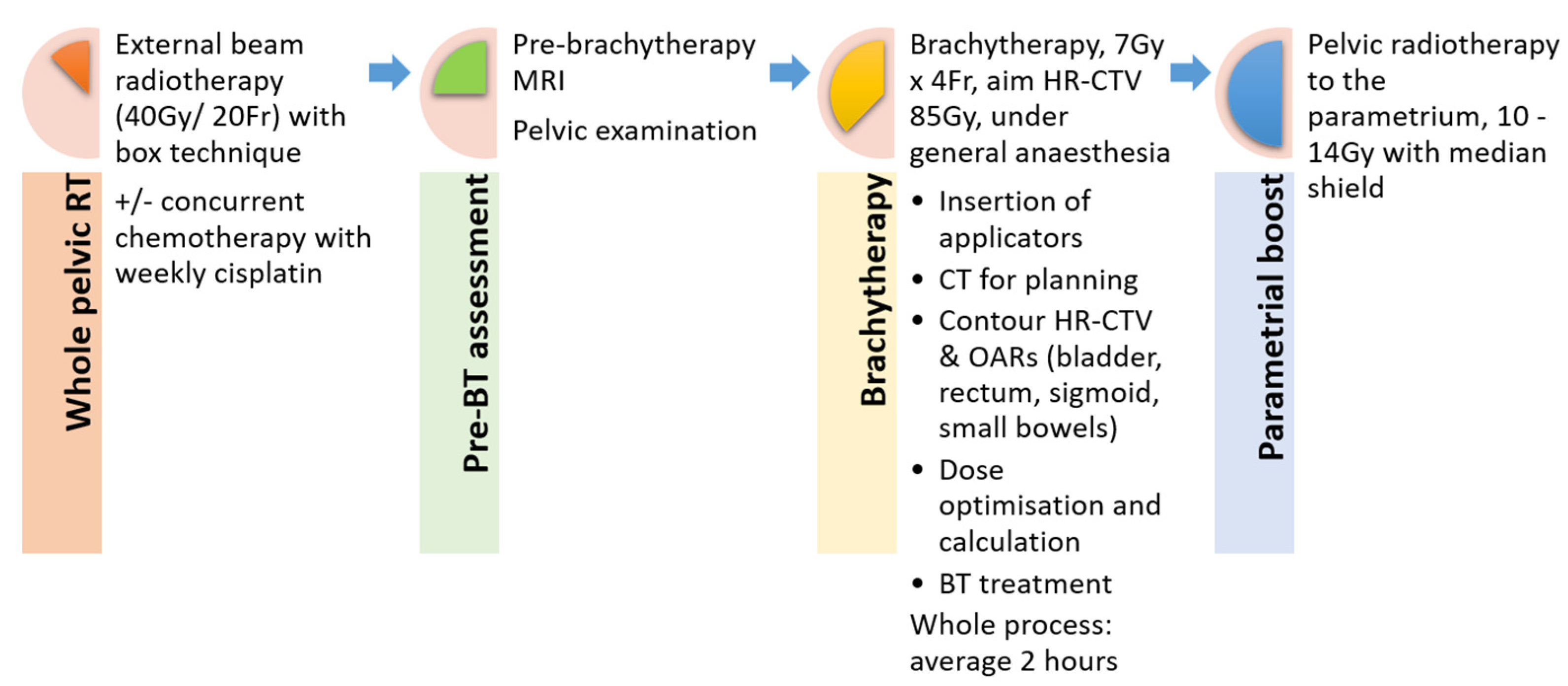
2.2. Treatment Delivery
2.2.1. Pelvic Radiotherapy
2.2.2. Brachytherapy
2.3. Follow Up
2.4. Endpoint and Statistical Analysis
3. Results
3.1. Treatment
3.2. Clinical Outcomes
3.3. Prognostic Factors for Local Control, Pelvic Control, Distant Metastasis-Free Survival and Overall Survival Rates
3.4. Late Toxicities
3.5. Time to Complete Brachytherapy Procedure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer 2021—GLOBOCAN 2020. Available online: https://gco.iarc.fr/tomorrow (accessed on 23 May 2022).
- Authority, H. Hong Kong Cancer Registry 2019. Available online: www3.ha.org.hk/cancereg (accessed on 1 February 2022).
- Haie-Meder, C.; Pötter, R.; Van Limbergen, E.; Briot, E.; De Brabandere, M.; Dimopoulos, J.; Dumas, I.; Hellebust, T.P.; Kirisits, C.; Lang, S.; et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): Concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother. Oncol. 2005, 74, 235–245. [Google Scholar] [CrossRef]
- Hellebust, T.P.; Kirisits, C.; Berger, D.; Pérez-Calatayud, J.; De Brabandere, M.; De Leeuw, A.; Dumas, I.; Hudej, R.; Lowe, G.; Wills, R.; et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group: Considerations and pitfalls in commissioning and applicator reconstruction in 3D image-based treatment planning of cervix cancer brachytherapy. Radiother. Oncol. 2010, 96, 153–160. [Google Scholar] [CrossRef]
- The Royal College of Radiologists. Implementing Image Guided Brachytherapy for Cervix Cancer in the UK; The Royal College of Radiologists: London, UK, 2009. [Google Scholar]
- Nag, S.; Erickson, B.; Thomadsen, B.; Orton, C.; Demanes, J.D.; Petereit, D. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. Int. J. Radiat. Oncol. Biol. Phys. 2000, 48, 201–211. [Google Scholar] [CrossRef]
- Pötter, R.; Tanderup, K.; Schmid, M.P.; Jürgenliemk-Schulz, I.; Haie-Meder, C.; Fokdal, L.U.; Sturdza, A.E.; Hoskin, P.; Mahantshetty, U.; Segedin, B.; et al. MRI-guided adaptive brachytherapy in locally advanced cervical cancer (EMBRACE-I): A multicentre prospective cohort study. Lancet Oncol. 2021, 22, 538–547. [Google Scholar] [CrossRef]
- Sturdza, A.; Pötter, R.; Fokdal, L.U.; Haie-Meder, C.; Tan, L.T.; Mazeron, R.; Petric, P.; Šegedin, B.; Jurgenliemk-Schulz, I.M.; Nomden, C.; et al. Image guided brachytherapy in locally advanced cervical cancer: Improved pelvic control and survival in RetroEMBRACE, a multicenter cohort study. Radiother. Oncol. 2016, 120, 428–433. [Google Scholar] [CrossRef]
- Horeweg, N.; Creutzberg, C.L.; Rijkmans, E.C.; Laman, M.S.; Velema, L.A.; Coen, V.L.M.; Stam, T.C.; Kerkhof, E.M.; Kroep, J.R.; De Kroon, C.D.; et al. Efficacy and toxicity of chemoradiation with image-guided adaptive brachytherapy for locally advanced cervical cancer. Int. J. Gynecol. Cancer 2019, 29, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Pötter, R.; Georg, P.; Dimopoulos, J.C.; Grimm, M.; Berger, D.; Nesvacil, N.; Georg, D.; Schmid, M.P.; Reinthaller, A.; Sturdza, A.; et al. Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother. Oncol. 2011, 100, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Charra-Brunaud, C.; Harter, V.; Delannes, M.; Haie-Meder, C.; Quetin, P.; Kerr, C.; Castelain, B.; Thomas, L.; Peiffert, D. Impact of 3D image-based PDR brachytherapy on outcome of patients treated for cervix carcinoma in France: Results of the French STIC prospective study. Radiother. Oncol. 2012, 103, 305–313. [Google Scholar] [CrossRef]
- Okonogi, N.; Wakatsuki, M.; Mizuno, H.; Fukuda, S.; Cao, J.; Kodrat, H.; Lau, F.N.; Calaguas, M.J.; Reyes, R.H.D.L.; Chansilpa, Y.; et al. Preliminary survey of 3D image-guided brachytherapy for cervical cancer at representative hospitals in Asian countries. J. Radiat. Res. 2020, 61, 608–615. [Google Scholar] [CrossRef]
- Lim, K.; Van Dyk, S.; Khaw, P.; Veera, J.; Mileshkin, L.; Ohanessian, L.; Harrison, M.; Vinod, S.K. Patterns of practice survey for brachytherapy for cervix cancer in Australia and New Zealand. J. Med. Imaging Radiat. Oncol. 2017, 61, 674–681. [Google Scholar] [CrossRef] [PubMed]
- Phan, T.; Mula-Hussain, L.; Pavamani, S.; Pearce, A.; D’Souza, D.; Patil, N.; Traptow, L.; Doll, C. The Changing Landscape of Brachytherapy for Cervical Cancer: A Canadian Practice Survey. Curr. Oncol. 2015, 22, 356–360. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shahid, N.; Craig, T.; Westerland, M.; Ashworth, A.; Ang, M.; D’Souza, D.; Sankreacha, R.; Fyles, A.; Milosevic, M.; Kong, I. Moving toward uniform and evidence-based practice of radiotherapy for management of cervical cancer in Ontario, Canada. Brachytherapy 2018, 17, 660–666. [Google Scholar] [CrossRef] [PubMed]
- Benedet, J.L.; Bender, H.; Jones, H., 3rd; Ngan, H.Y.; Pecorelli, S. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. Int. J. Gynaecol. Obstet. 2000, 70, 209–262. [Google Scholar] [PubMed]
- Viswanathan, A.N.; Erickson, B.; Gaffney, D.K.; Beriwal, S.; Bhatia, S.K.; Burnett, O.L.; D’Souza, D.P.; Patil, N.; Haddock, M.G.; Jhingran, A.; et al. Comparison and Consensus Guidelines for Delineation of Clinical Target Volume for CT- and MR-Based Brachytherapy in Locally Advanced Cervical Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2014, 90, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Horne, Z.D.; Karukonda, P.; Kalash, R.; Edwards, R.P.; Kelley, J.L.; Comerci, J.T.; Olawaiye, A.B.; Courtney-Brooks, M.; Bochmeier, M.M.; Berger, J.L.; et al. Single-Institution Experience in 3D MRI-Based Brachytherapy for Cervical Cancer for 239 Women: Can Dose Overcome Poor Response? Int. J. Radiat. Oncol Biol. Phys. 2019, 104, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Gill, B.S.; Kim, H.; Houser, C.; Olsen, A.; Kelley, J.; Edwards, R.P.; Comerci, J.; Sukumvanich, P.; Olawaiye, A.B.; Huang, M.; et al. Image-based three-dimensional conformal brachytherapy for medically inoperable endometrial carcinoma. Brachytherapy 2014, 13, 542–547. [Google Scholar] [CrossRef]
- Tomizawa, K.; Kaminuma, T.; Murata, K.; Noda, S.-E.; Irie, D.; Kumazawa, T.; Oike, T.; Ohno, T. FIGO 2018 Staging for Cervical Cancer: Influence on Stage Distribution and Outcomes in the 3D-Image-Guided Brachytherapy Era. Cancers 2020, 12, 1770. [Google Scholar] [CrossRef]
- Zolciak-Siwinska, A.; Gruszczynska, E.; Bijok, M.; Jonska-Gmyrek, J.; Dabkowski, M.; Staniaszek, J.; Michalski, W.; Kowalczyk, A.; Milanowska, K. Computed Tomography–Planned High-Dose-Rate Brachytherapy for Treating Uterine Cervical Cancer. Int. J. Radiat. Oncol. 2016, 96, 87–92. [Google Scholar] [CrossRef]
- Ohno, T.; Noda, S.-E.; Okonogi, N.; Murata, K.; Shibuya, K.; Kiyohara, H.; Tamaki, T.; Ando, K.; Oike, T.; Ohkubo, Y.; et al. In-room computed tomography–based brachytherapy for uterine cervical cancer: Results of a 5-year retrospective study. J. Radiat. Res. 2016, 58, 543–551. [Google Scholar] [CrossRef]
- Singhal, S.; Veeratterapillay, J.; Locks, S.; Morgan, D.; Patil, R.; Chamberlain, H. Magnetic Resonance Imaging-Guided Adaptive Brachytherapy for the Treatment of Cervical Cancer and its Impact on Clinical Outcome. Clin. Oncol. 2022, 34, 442–451. [Google Scholar] [CrossRef] [PubMed]
- Mahantshetty, U.; Poetter, R.; Beriwal, S.; Grover, S.; Lavanya, G.; Rai, B.; Petric, P.; Tanderup, K.; Carvalho, H.; Hegazy, N.; et al. IBS-GEC ESTRO-ABS recommendations for CT based contouring in image guided adaptive brachytherapy for cervical cancer. Radiother. Oncol. 2021, 160, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, M.C.; Beriwal, S.; Dyer, B.A.; Klopp, A.H.; Lee, S.I.; McGinnis, G.J.; Robbins, J.B.; Rauch, G.M.; Sadowski, E.A.; Simiele, S.J.; et al. Contemporary image-guided cervical cancer brachytherapy: Consensus imaging recommendations from the Society of Abdominal Radiology and the American Brachytherapy Society. Brachytherapy 2022, 21, 369–388. [Google Scholar] [CrossRef]
- Pötter, R.; Haie-Meder, C.; Van Limbergen, E.; Barillot, I.; De Brabandere, M.; Dimopoulos, J.; Dumas, I.; Erickson, B.; Lang, S.; Nulens, A.; et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): Concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy—3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother. Oncol. 2006, 78, 67–77. [Google Scholar] [CrossRef]
- Dimopoulos, J.C.; Petrow, P.; Tanderup, K.; Petric, P.; Berger, D.; Kirisits, C.; Pedersen, E.M.; Van Limbergen, E.; Haie-Meder, C.; Pötter, R. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (IV): Basic principles and parameters for MR imaging within the frame of image based adaptive cervix cancer brachytherapy. Radiother. Oncol. 2012, 103, 113–122. [Google Scholar] [CrossRef]
- Lee, L.J.; Das, I.J.; Higgins, S.A.; Jhingran, A.; Small, W.; Thomadsen, B.; Viswanathan, A.N.; Wolfson, A.; Eifel, P. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part III: Low-dose-rate and pulsed-dose-rate brachytherapy. Brachytherapy 2012, 11, 53–57. [Google Scholar] [CrossRef]
- Yao, G.; Qiu, J.; Zhu, F.; Wang, X. Survival of Patients With Cervical Cancer Treated With Definitive Radiotherapy or Concurrent Chemoradiotherapy According to Histological Subtype: A Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 843262. [Google Scholar] [CrossRef]
- Li, D.; Huang, S.; Liu, K.; Qin, Y.; Zhang, Y.; Yang, Y. Clinicopathological characteristics and survival outcomes in human papillomavirus independent cervical cancer: A propensity score matched analysis. Int. J. Gynecol. Cancer 2022, 32, 599–605. [Google Scholar] [CrossRef]
- Miyahara, S.; Tsuji, K.; Shimada, M.; Shibuya, Y.; Shigeta, S.; Nagai, T.; Umezawa, R.; Tokunaga, H.; Jingu, K.; Yaegashi, N. The Impact of Histological Subtype on Survival Outcome of Patients with Stage IIB-IVA Cervical Cancer Who Received Definitive Radiotherapy. Tohoku J. Exp. Med. 2021, 255, 303–313. [Google Scholar] [CrossRef]
- Hu, K.; Wang, W.; Liu, X.; Meng, Q.; Zhang, F. Comparison of treatment outcomes between squamous cell carcinoma and adenocarcinoma of cervix after definitive radiotherapy or concurrent chemoradiotherapy. Radiat. Oncol. 2018, 13, 249. [Google Scholar] [CrossRef]
- Katanyoo, K.; Sanguanrungsirikul, S.; Manusirivithaya, S. Comparison of treatment outcomes between squamous cell carcinoma and adenocarcinoma in locally advanced cervical cancer. Gynecol. Oncol. 2012, 125, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.J.; Byun, J.M.; Kim, Y.N.; Lee, K.B.; Sung, M.S.; Kim, K.T.; Jeong, D.H. Cervical Adenocarcinoma Has a Poorer Prognosis and a Higher Propensity for Distant Recurrence Than Squamous Cell Carcinoma. Int. J. Gynecol. Cancer 2017, 27, 1228–1236. [Google Scholar] [CrossRef] [PubMed]
- Eifel, P.; Burke, T.; Morris, M.; Smith, T. Adenocarcinoma as an Independent Risk Factor for Disease Recurrence in Patients with Stage IB Cervical Carcinoma. Gynecol. Oncol. Biol. Phys. 1995, 59, 38–44. [Google Scholar] [CrossRef]
- Huang, Y.-T.; Wang, C.-C.; Tsai, C.-S.; Lai, C.-H.; Chang, T.-C.; Chou, H.-H.; Hsueh, S.; Chen, C.-K.; Lee, S.P.; Hong, J.-H. Long-Term Outcome and Prognostic Factors for Adenocarcinoma/Adenosquamous Carcinoma of Cervix After Definitive Radiotherapy. Int. J. Radiat. Oncol. 2011, 80, 429–436. [Google Scholar] [CrossRef]
- Liu, P.; Ji, M.; Kong, Y.; Huo, Z.; Lv, Q.; Xie, Q.; Wang, D.; Chen, B.; Wang, H.; Cui, Z.; et al. Comparison of survival outcomes between squamous cell carcinoma and adenocarcinoma/adenosquamous carcinoma of the cervix after radical radiotherapy and chemotherapy. BMC Cancer 2022, 22, 326. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network Clinical Practice Guideline in Oncology. Cervical Cancer. Available online: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf (accessed on 19 December 2018).
- Cibula, D.; Pötter, R.; Planchamp, F.; Avall-Lundqvist, E.; Fischerova, D.; Haie-Meder, C.; Köhler, C.; Landoni, F.; Lax, S.; Lindegaard, J.C.; et al. The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology Guidelines for the Management of Patients with Cervical Cancer. Virchows Arch. 2018, 472, 919–936. [Google Scholar] [CrossRef]
- Arakaki, Y.; Ariga, T.; Heianna, J.; Shimoji, Y.; Nakasone, T.; Taira, Y.; Nakamoto, T.; Ooyama, T.; Kudaka, W.; Kaneshima, I.; et al. Long-term Outcomes of Cervical Adenocarcinoma Treated With Concurrent Chemoradiotherapy Using Paclitaxel and Cisplatin. In Vivo 2020, 34, 2739–2743. [Google Scholar] [CrossRef]
- Green, H.; Counsell, N.; Ward, A.; McCormack, M. Neoadjuvant Chemotherapy in Locally Advanced Cervical Carcinoma—A Role in Patients with Para-aortic Lymph Node Involvement? A 10-year Institutional Experience. Clin. Oncol. 2022, 34, e281–e290. [Google Scholar] [CrossRef]
- Li, J.; Liu, H.; Li, Y.; Li, J.; Shen, L.; Long, W.; Yang, C.; Xu, H.; Xi, W.; Cai, R.; et al. Comparison of outcomes and side effects for neoadjuvant chemotherapy with weekly cisplatin and paclitaxel followed by chemoradiation vs. chemoradiation alone in stage IIB–IVA cervical cancer: Study protocol for a randomized controlled trial. Trials 2022, 23, 29. [Google Scholar] [CrossRef]
- Horeweg, N.; Mittal, P.; Gradowska, P.L.; Boere, I.; Nout, R.A.; Chopra, S. A systematic review and meta-analysis of adjuvant chemotherapy after chemoradiation for locally advanced cervical cancer. Crit. Rev. Oncol. 2022, 172, 103638. [Google Scholar] [CrossRef]
- Mileshkin, L.R.; Moore, K.N.; Barnes, E.; Gebski, V.; Narayan, K.; Bradshaw, N.; Lee, Y.C.; Diamante, K.; Fyles, A.W.; Small, W.; et al. Adjuvant chemotherapy following chemoradiation as primary treatment for locally advanced cervical cancer compared to chemoradiation alone: The randomized phase III OUTBACK Trial (ANZGOG 0902, RTOG 1174, NRG 0274). J. Clin. Oncol. 2021, 39 (Suppl. S18), LBA3. [Google Scholar] [CrossRef]
- Tovanabutra, C.; Asakij, T.; Rongsriyam, K.; Tangjitgamol, S.; Tharavichitkul, E.; Sukhaboon, J.; Kridakara, L.C.A.; Paengchit, K.; Khunnarong, J.; Atjimakul, T.; et al. Long-Term Outcomes and Sites of Failure in Locally Advanced, Cervical Cancer Patients Treated by Concurrent Chemoradiation with or without Adjuvant Chemotherapy: ACTLACC Trial. Asian Pac. J. Cancer Prev. 2021, 22, 2977–2985. [Google Scholar] [CrossRef] [PubMed]
- Wakatsuki, M.; Kato, S.; Ohno, T.; Karasawa, K.; Kiyohara, H.; Tamaki, T.; Ando, K.; Tsujii, H.; Nakano, T.; Kamada, T.; et al. Clinical outcomes of carbon ion radiotherapy for locally advanced adenocarcinoma of the uterine cervix in phase 1/2 clinical trial (protocol 9704). Cancer 2014, 120, 1663–1669. [Google Scholar] [CrossRef]
- Wakatsuki, M.; Kato, S.; Ohno, T.; Kiyohara, H.; Karasawa, K.; Tamaki, T.; Ando, K.; Irie, D.; Shiba, S.; Tsujii, H.; et al. Difference in distant failure site between locally advanced squamous cell carcinoma and adenocarcinoma of the uterine cervix after C-ion RT. J. Radiat. Res. 2015, 56, 523–528. [Google Scholar] [CrossRef]
| Total | 135 Patients | |
|---|---|---|
| Median | Range | |
| Age | 56 years old | 27–83 years old |
| Follow-up period | 53.6 months | 3.0–99.6 months |
| Tumor characteristics | ||
| Tumor width at diagnosis | 4.8 cm | 2–9.3 cm |
| Tumor depth at diagnosis | 3.2 cm | 0.8–4.6 cm |
| HPV-related | ||
| Yes | 29 | 21.5% |
| No | 7 | 5.2% |
| Unknown | 99 | 73.3% |
| Number | Percentage | |
| Stage | ||
| IB | 23 | 17.0% |
| IIA | 20 | 14.8% |
| IIB | 62 | 45.9% |
| IIIA | 5 | 3.7% |
| IIIB | 25 | 18.5% |
| Pelvic lymph node involvement | 78 | 57.8% |
| Para-aortic lymph node involvement | 3 | 2.2% |
| Type of carcinoma | ||
| Squamous cell carcinoma | 107 | 79.3% |
| Adenocarcinoma/adenosquamous cell carcinoma | 28 | 20.7% |
| Number | Percentage | ||
|---|---|---|---|
| Completed external beam radiotherapy | 135 | 100% | |
| Concurrent chemotherapy | 110 | 81.5% | |
| Brachytherapy | |||
| 100 | 74.1% | |
| 35 | 25.9% | |
| Mean ± SD | Range | ||
| Time to complete brachytherapy | 142 ± 17 min | 116–189 min | |
| HR-CTV volume | 42 ± 8.9 cm3 | 20.5–65.6 cm3 | |
| HR-CTV D90 | 84 ± 7.54 Gy | 67–104 Gy | |
| D2cc for | Bladder | 82 ± 9.37 Gy | 55–105 Gy |
| Rectum | 66 ± 6.61 Gy | 51–83 Gy | |
| Sigmoid | 65 ± 8.35 Gy | 47–80 Gy | |
| Bowel | 61 ± 8.94 Gy | 44–80 Gy | |
| Event Outcome | Squamous Cell Carcinoma | % | Adeno-Carcinoma | % | Total | % | p * |
|---|---|---|---|---|---|---|---|
| (n = 107) | (n = 28) | (n = 135) | |||||
| Local failure | 5 | 4.70% | 7 | 25.00% | 12 | 8.90% | 0.003 |
| - Persistent disease | 2 | 1.90% | 5 | 17.90% | 7 | 5.20% | |
| 1 | 0.90% | 3 | 10.70% | 4 | 3.00% | |
| - Local recurrence after remission | 3 | 2.80% | 2 | 7.10% | 5 | 3.70% | |
| Pelvic failure | 10 | 9.30% | 10 | 35.70% | 20 | 14.80% | 0.001 |
| - Pelvic lymph node recurrence | 5 | 4.70% | 3 | 10.70% | 8 | 5.90% | |
| Distant failure | 15 | 14.00% | 9 | 32.10% | 24 | 17.80% | 0.048 |
| - Subsequent systemic treatment | 14 | 13.10% | 7 | 25.00% | 21 | 15.60% | |
| Death | 6 | 5.60% | 8 | 28.60% | 14 | 10.40% | 0.002 |
| Study | IGABT Technique | No. of Patients | Medan HR-CTV Volume (cm3) | Local Control | Overall Survival |
| Present study | CT | 135 | 42 | 90.7% (5-year) | 87.2% (5-year) |
| Potter et al. [8] | MRI | 1416 | 28 | 92% (5-year) | 74% (5-year) |
| Potter et al. [11] | MRI | 156 | Mean tumor size > 5 cm | 95% (3-year) | 68% (3-year) |
| Charra-Brunaud et al. [12] | MRI | 117 | 35.2 | 78.5% (2-year) | 74% (2-year) |
| Sturdza et al. [9] | CT/MRI | 731 | 37 | 89% (5-year) | 65% (5-year) |
| Horne et al. [19] | MRI | 239 | 31 | 90.8% (5-year) | 72.7% (5-year) |
| Gill et al. [20] | CT/MRI | 128 | 31 | 92% (2-year) | 85% (2-year) |
| Horeweg et al. [10] | CT/MRI | 155 | Mean tumor size 4.6 cm | 90.4% (5-year) | 65.9% (5-year) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, W.-L.; Cheng, M.H.-F.; Wu, J.T.-K.; Choi, C.-W.; Tse, R.P.-Y.; Ho, P.P.-Y.; Cheung, E.E.; Cheung, A.; Test, K.-Y.; Chan, K.K.-L.; et al. Treatment Outcomes of Computer Tomography-Guided Brachytherapy in Cervical Cancer in Hong Kong: A Retrospective Review. Cancers 2022, 14, 3934. https://doi.org/10.3390/cancers14163934
Chan W-L, Cheng MH-F, Wu JT-K, Choi C-W, Tse RP-Y, Ho PP-Y, Cheung EE, Cheung A, Test K-Y, Chan KK-L, et al. Treatment Outcomes of Computer Tomography-Guided Brachytherapy in Cervical Cancer in Hong Kong: A Retrospective Review. Cancers. 2022; 14(16):3934. https://doi.org/10.3390/cancers14163934
Chicago/Turabian StyleChan, Wing-Lok, Matthew Ho-Fai Cheng, Jacky Tsun-Kit Wu, Cheuk-Wai Choi, Rosa Piu-Ying Tse, Patty Piu-Ying Ho, Emina Edith Cheung, Andy Cheung, Ka-Yu Test, Karen Kar-Loen Chan, and et al. 2022. "Treatment Outcomes of Computer Tomography-Guided Brachytherapy in Cervical Cancer in Hong Kong: A Retrospective Review" Cancers 14, no. 16: 3934. https://doi.org/10.3390/cancers14163934
APA StyleChan, W.-L., Cheng, M. H.-F., Wu, J. T.-K., Choi, C.-W., Tse, R. P.-Y., Ho, P. P.-Y., Cheung, E. E., Cheung, A., Test, K.-Y., Chan, K. K.-L., Ngan, H. Y.-S., Siu, S. W.-K., Ngan, R. K.-C., & Lee, A. W.-M. (2022). Treatment Outcomes of Computer Tomography-Guided Brachytherapy in Cervical Cancer in Hong Kong: A Retrospective Review. Cancers, 14(16), 3934. https://doi.org/10.3390/cancers14163934






