The Role of Conization before Radical Hysterectomy in Cervical Cancer including High Risk Factors of Recurrence: Propensity Score Matching
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Clinical Characteristics of the Entire Cohort
3.2. Analysis after Propensity Score Matching
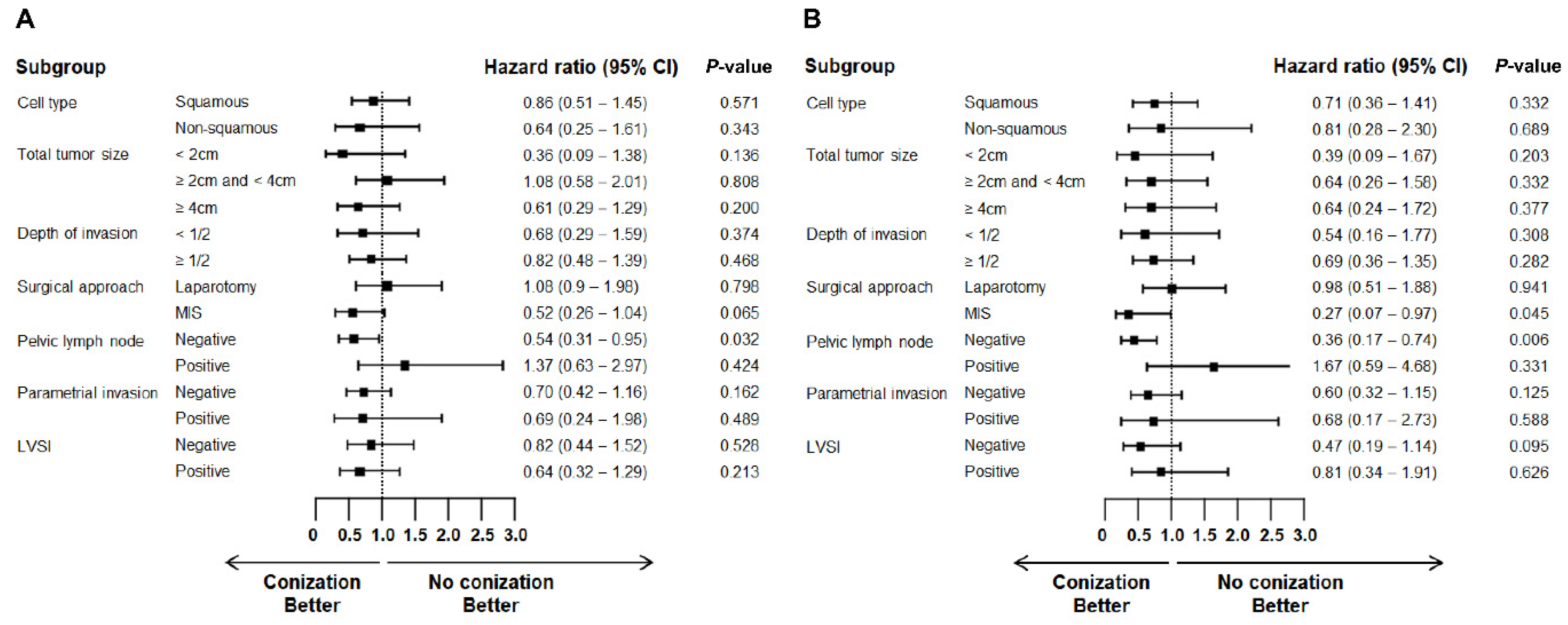
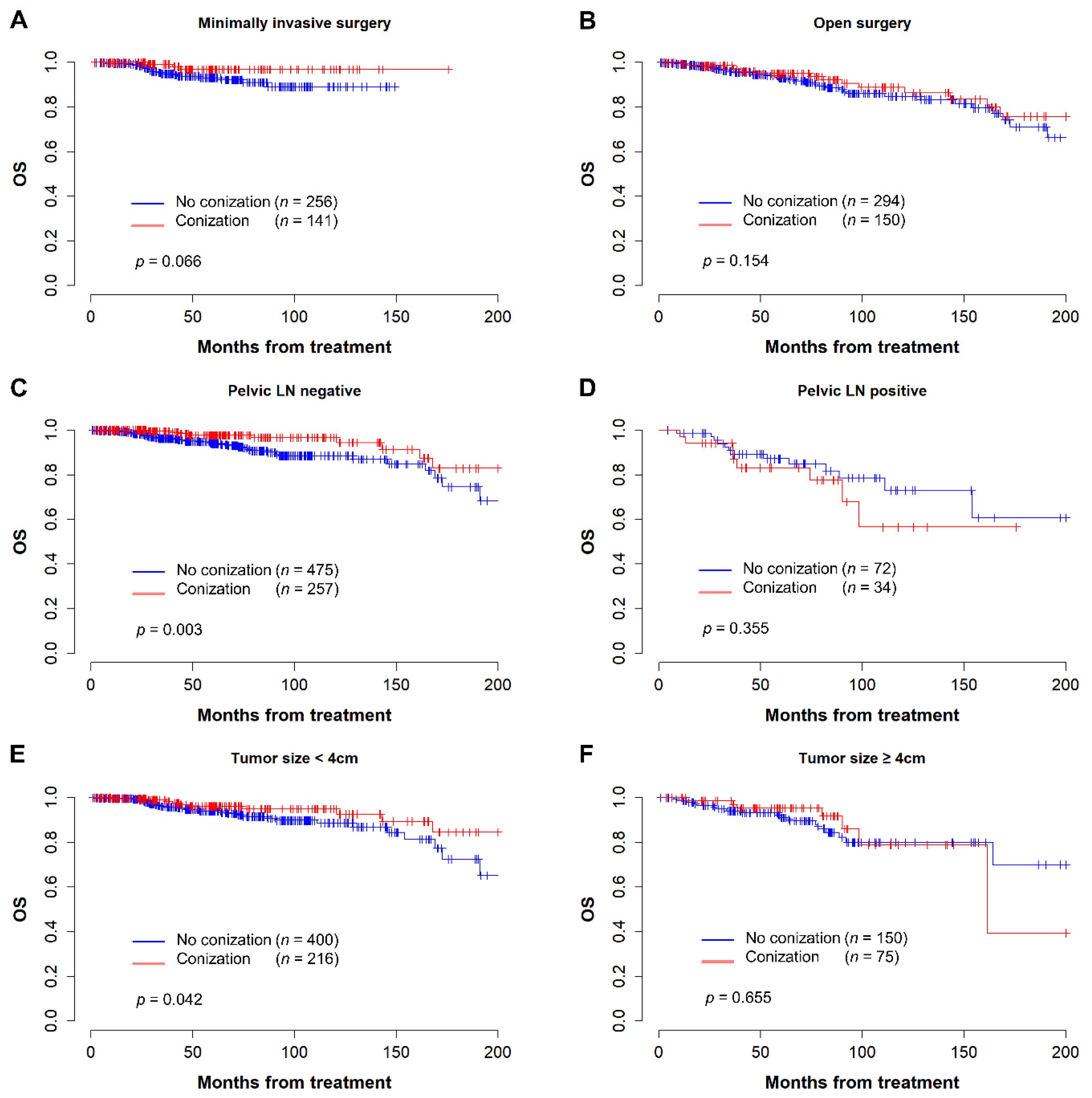
3.3. Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar]
- Abdalla, E.; Troy, R.; Fall, S.; Elhussin, I.; Egiebor-Aiwan, O.; Nganwa, D. Racial differences in 5-year relative survival rates of cervical cancer by stage at diagnosis, between African American (black) and white women, living in the state of Alabama, USA. BMC Cancer 2020, 20, 830. [Google Scholar]
- Perkins, R.B.; Guido, R.S.; Castle, P.E.; Chelmow, D.; Einstein, M.H.; Garcia, F.; Huh, W.K.; Kim, J.J.; Moscicki, A.B.; Nayar, R.; et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J. Low. Genit. Tract. Dis. 2020, 24, 102–131. [Google Scholar]
- NCCN Clinical Practice Guidelines in Oncology: Cervical Cancer. Version 1.2022. Available online: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf (accessed on 23 July 2022).
- Ramirez, P.T.; Frumovitz, M.; Pareja, R.; Lopez, A.; Vieira, M.; Ribeiro, R.; Buda, A.; Yan, X.; Shuzhong, Y.; Chetty, N.; et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N. Engl. J. Med. 2018, 379, 1895–1904. [Google Scholar]
- Tewari, K.S. Minimally Invasive Surgery for Early-Stage Cervical Carcinoma: Interpreting the Laparoscopic Approach to Cervical Cancer Trial Results. J. Clin. Oncol. 2019, 37, 3075–3080. [Google Scholar]
- Kohler, C.; Hertel, H.; Herrmann, J.; Marnitz, S.; Mallmann, P.; Favero, G.; Plaikner, A.; Martus, P.; Gajda, M.; Schneider, A. Laparoscopic radical hysterectomy with transvaginal closure of vaginal cuff—A multicenter analysis. Int. J. Gynecol. Cancer 2019, 29, 845–850. [Google Scholar]
- Chiva, L.; Zanagnolo, V.; Querleu, D.; Martin-Calvo, N.; Arevalo-Serrano, J.; Capilna, M.E.; Fagotti, A.; Kucukmetin, A.; Mom, C.; Chakalova, G.; et al. SUCCOR study: An international European cohort observational study comparing minimally invasive surgery versus open abdominal radical hysterectomy in patients with stage IB1 cervical cancer. Int. J. Gynecol. Cancer 2020, 30, 1269–1277. [Google Scholar]
- Uppal, S.; Gehrig, P.A.; Peng, K.; Bixel, K.L.; Matsuo, K.; Vetter, M.H.; Davidson, B.A.; Cisa, M.P.; Lees, B.F.; Brunette, L.L.; et al. Recurrence Rates in Patients With Cervical Cancer Treated With Abdominal Versus Minimally Invasive Radical Hysterectomy: A Multi-Institutional Retrospective Review Study. J. Clin. Oncol. 2020, 38, 1030–1040. [Google Scholar]
- Kanao, H.; Matsuo, K.; Aoki, Y.; Tanigawa, T.; Nomura, H.; Okamoto, S.; Takeshima, N. Feasibility and outcome of total laparoscopic radical hysterectomy with no-look no-touch technique for FIGO IB1 cervical cancer. J. Gynecol. Oncol. 2019, 30, e71. [Google Scholar]
- Mun, J.; Park, S.J.; Yim, G.W.; Chang, S.J.; Kim, H.; Trial Monitoring Committee of SOLUTION Trial. Solution to prevent tumor spillage in minimally invasive radical hysterectomy using the endoscopic stapler for treating early-stage cervical cancer: Surgical technique with video. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102211. [Google Scholar]
- Casarin, J.; Bogani, G.; Papadia, A.; Ditto, A.; Pinelli, C.; Garzon, S.; Donadello, N.; Lagana, A.S.; Cromi, A.; Mueller, M.; et al. Preoperative Conization and Risk of Recurrence in Patients Undergoing Laparoscopic Radical Hysterectomy for Early Stage Cervical Cancer: A Multicenter Study. J. Minim. Invasive Gynecol. 2021, 28, 117–123. [Google Scholar]
- Benoit, L.; Koual, M.; Nguyen-Xuan, H.T.; Balaya, V.; Nos, C.; Montero-Macias, R.; Bats, A.S. Does a pre-operative conization improve disease-free survival in early-stage cervical cancer? Arch. Gynecol. Obstet. 2021, 303, 231–239. [Google Scholar]
- Bizzarri, N.; Pedone Anchora, L.; Kucukmetin, A.; Ratnavelu, N.; Korompelis, P.; Carbone, V.; Fedele, C.; Bruno, M.; Vizzielli, G.; Gallotta, V.; et al. Protective Role of Conization Before Radical Hysterectomy in Early-Stage Cervical Cancer: A Propensity-Score Matching Study. Ann. Surg. Oncol. 2021, 28, 3585–3594. [Google Scholar]
- Kim, S.I.; Choi, B.R.; Kim, H.S.; Chung, H.H.; Kim, J.W.; Park, N.H.; Song, Y.S.; Choi, C.H.; Lee, M. Cervical conization before primary radical hysterectomy has a protective effect on disease recurrence in early cervical cancer: A two-center matched cohort study according to surgical approach. Gynecol. Oncol. 2022, 164, 535–542. [Google Scholar]
- Chacon, E.; Manzour, N.; Zanagnolo, V.; Querleu, D.; Nunez-Cordoba, J.M.; Martin-Calvo, N.; Capilna, M.E.; Fagotti, A.; Kucukmetin, A.; Mom, C.; et al. SUCCOR cone study: Conization before radical hysterectomy. Int. J. Gynecol. Cancer 2022, 32, 117–124. [Google Scholar]
- Peters, W.A., 3rd; Liu, P.Y.; Barrett, R.J., 2nd; Stock, R.J.; Monk, B.J.; Berek, J.S.; Souhami, L.; Grigsby, P.; Gordon, W., Jr.; Alberts, D.S. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J. Clin. Oncol. 2000, 18, 1606–1613. [Google Scholar]
- Sedlis, A.; Bundy, B.N.; Rotman, M.Z.; Lentz, S.S.; Muderspach, L.I.; Zaino, R.J. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol. Oncol. 1999, 73, 177–183. [Google Scholar]
- Obermair, A.; Asher, R.; Pareja, R.; Frumovitz, M.; Lopez, A.; Moretti-Marques, R.; Rendon, G.; Ribeiro, R.; Tsunoda, A.; Behan, V.; et al. Incidence of adverse events in minimally invasive vs open radical hysterectomy in early cervical cancer: Results of a randomized controlled trial. Am. J. Obstet. Gynecol. 2020, 222, 249.e241–249.e210. [Google Scholar]
- Frumovitz, M.; Obermair, A.; Coleman, R.L.; Pareja, R.; Lopez, A.; Ribero, R.; Isla, D.; Rendon, G.; Bernardini, M.Q.; Buda, A.; et al. Quality of life in patients with cervical cancer after open versus minimally invasive radical hysterectomy (LACC): A secondary outcome of a multicentre, randomised, open-label, phase 3, non-inferiority trial. Lancet Oncol. 2020, 21, 851–860. [Google Scholar]
- Boria, F.; Chiva, L.; Zanagnolo, V.; Querleu, D.; Martin-Calvo, N.; Capilna, M.E.; Fagotti, A.; Kucukmetin, A.; Mom, C.; Chakalova, G.; et al. Radical hysterectomy in early cervical cancer in Europe: Characteristics, outcomes and evaluation of ESGO quality indicators. Int. J. Gynecol. Cancer 2021, 31, 1212–1219. [Google Scholar]
- Bogani, G.; Di Donato, V.; Muzii, L.; Casarin, J.; Ghezzi, F.; Malzoni, M.; Greggi, S.; Landoni, F.; Bazzurini, L.; Zanagnolo, V.; et al. Assessing the role of minimally invasive radical hysterectomy for early-stage cervical cancer. Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 275, 64–69. [Google Scholar]
- Bogani, G.; Ghezzi, F.; Chiva, L.; Gisone, B.; Pinelli, C.; Dell’Acqua, A.; Casarin, J.; Ditto, A.; Raspagliesi, F. Patterns of recurrence after laparoscopic versus open abdominal radical hysterectomy in patients with cervical cancer: A propensity-matched analysis. Int. J. Gynecol. Cancer 2020, 30, 987–992. [Google Scholar]
- Manzour, N.; Chiva, L.; Chacon, E.; Martin-Calvo, N.; Boria, F.; Minguez, J.A.; Alcazar, J.L.; Group, S.S. SUCCOR Risk: Design and Validation of a Recurrence Prediction Index for Early-Stage Cervical Cancer. Ann. Surg. Oncol. 2022, 29, 4819–4829. [Google Scholar]
- Bogani, G.; Ditto, A.; Chiappa, V.; Pinelli, C.; Sonetto, C.; Raspagliesi, F. Primary conization overcomes the risk of developing local recurrence following laparoscopic radical hysterectomy in early stage cervical cancer. Int. J. Gynaecol. Obstet. 2020, 151, 43–48. [Google Scholar]
- Yin, X.; Zhu, L.; Tan, W.; Zhu, X.; Liu, S.; Xu, W. Time Intervals Between Prior Cervical Conization and Posterior Hysterectomy Influence Postoperative Infection in Patients with Cervical Intraepithelial Neoplasia or Cancer. Med. Sci. Monit. 2018, 24, 9063–9072. [Google Scholar]
- Li, H.; Jang, J.Y.; Li, H.; Chen, K.; Shao, X.G. The influence of interval between conization and laparoscopic radical hysterectomy on the morbidity of patients with cervical cancer. Eur. J. Gynaecol. Oncol. 2012, 33, 601–604. [Google Scholar]
- Samlal, R.A.; van der Velden, J.; Schilthuis, M.S.; Ten Kate, F.J.; Hart, A.A.; Lammes, F.B. Influence of diagnostic conization on surgical morbidity and survival in patients undergoing radical hysterectomy for stage IB and IIA cervical carcinoma. Eur. J. Gynaecol. Oncol. 1997, 18, 478–481. [Google Scholar]
- Kim, Y.T.; Yoon, B.S.; Kim, S.H.; Kim, J.H.; Kim, J.W.; Park, Y.W. The influence of time intervals between loop electrosurgical excision and subsequent hysterectomy on the morbidity of patients with cervical neoplasia. Gynecol. Oncol. 2005, 96, 500–503. [Google Scholar]
- Nanthamongkolkul, K.; Hanprasertpong, J. Longer waiting times for early stage cervical cancer patients undergoing radical hysterectomy are associated with diminished long-term overall survival. J. Gynecol. Oncol. 2015, 26, 262–269. [Google Scholar]
- Umezu, T.; Shibata, K.; Kajiyama, H.; Yamamoto, E.; Mizuno, M.; Kikkawa, F. Prognostic factors in stage IA-IIA cervical cancer patients treated surgically: Does the waiting time to the operation affect survival? Arch. Gynecol. Obstet. 2012, 285, 493–497. [Google Scholar]
- Benard, V.B.; Howe, W.; Royalty, J.; Helsel, W.; Kammerer, W.; Richardson, L.C. Timeliness of cervical cancer diagnosis and initiation of treatment in the National Breast and Cervical Cancer Early Detection Program. J. Womens Health 2012, 21, 776–782. [Google Scholar]
- Noh, K.W.; Kim, B.; Choi, C.H.; Kim, T.J.; Lee, J.W.; Kim, B.G.; Bae, D.S.; Cho, W.K.; Park, W.; Lee, Y.Y. Effect of Waiting Time from Pathological Diagnosis to Definitive Concurrent Chemoradiation for Cervical Cancer on Overall Survival. Cancer Res. Treat. 2022, 54, 245–252. [Google Scholar]
- Perri, T.; Issakov, G.; Ben-Baruch, G.; Felder, S.; Beiner, M.E.; Helpman, L.; Hogen, L.; Jakobson-Setton, A.; Korach, J. Effect of treatment delay on survival in patients with cervical cancer: A historical cohort study. Int. J. Gynecol. Cancer 2014, 24, 1326–1332. [Google Scholar]
- Petereit, D.G.; Sarkaria, J.N.; Chappell, R.; Fowler, J.F.; Hartmann, T.J.; Kinsella, T.J.; Stitt, J.A.; Thomadsen, B.R.; Buchler, D.A. The adverse effect of treatment prolongation in cervical carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 1995, 32, 1301–1307. [Google Scholar]
- Vitzthum, L.; Yuan, J.; Jones, D.; Boldt, A.; Dusenbery, K. Reducing prolonged chemoradiation treatment times for cervical cancer. BMJ Open Qual. 2019, 8, e000516. [Google Scholar]


| Unmatched | Matched | |||||
|---|---|---|---|---|---|---|
| without Conization (n = 1508) | with Conization (n = 291) | p-Value | without Conization (n = 550) | with Conization (n = 291) | p-Value | |
| Age | 48 [16–83] | 46 [23–87] | 0.001 | 46 [16–83] | 46 [23–87] | 0.282 |
| Year of diagnosis | 0.009 | 0.736 | ||||
| ~2000 | 219 (14.52%) | 27 (9.28%) | 49 (8.91%) | 27 (9.28%) | ||
| 2000~2010 | 614 (40.72%) | 109 (37.46%) | 221 (40.18%) | 109 (37.46%) | ||
| 2010~ | 675 (44.76%) | 155 (53.26%) | 280 (50.91%) | 155 (53.26%) | ||
| Stage | <0.001 | 0.063 | ||||
| IB1 + IB2 | 1197 (79.38%) | 274 (94.16%) | 505 (91.82%) | 274 (94.16%) | ||
| IIA1 + IIA2 + IIB | 311 (20.62%) | 17 (5.84%) | 45 (8.18%) | 17 (5.84%) | ||
| Cell type | 0.011 | 0.962 | ||||
| Squamous | 1055 (69.96%) | 225 (77.32%) | 426 (77.45%) | 225 (77.32%) | ||
| Non-squamous | 453 (30.04%) | 66 (22.68%) | 124 (22.55%) | 66 (22.68%) | ||
| Hysterectomy type | 0.481 | 0.788 | ||||
| Type 1,2 | 27 (1.79%) | 7 (2.41%) | 15 (2.73%) | 7 (2.41%) | ||
| Type 3 | 1481 (98.21%) | 284 (97.59%) | 535 (97.27%) | 284 (97.59%) | ||
| Surgical approach | <0.001 | 0.509 | ||||
| Laparotomy | 1062 (70.42%) | 150 (51.55%) | 294 (53.45%) | 150 (51.55%) | ||
| MIS | 446 (29.58%) | 141 (48.45%) | 256 (46.55%) | 141 (48.45%) | ||
| Total tumor size (cm) | 3.2 [0.5–11] | 2.5 [0.5–12] | <0.001 | 3 [0.5–10.5] | 2.5 [0.5–12] | 0.328 |
| Depth of invasion | <0.001 | 0.494 | ||||
| <1/2 | 457 (30.31%) | 122 (41.92%) | 218 (39.64%) | 122 (41.92%) | ||
| >1/2 | 1051 (69.69%) | 169 (58.08%) | 332 (60.36%) | 169 (58.08%) | ||
| LVSI | <0.001 | 0.662 | ||||
| Negative | 706 (46.82%) | 189 (64.95%) | 345 (62.73%) | 189 (64.95%) | ||
| Positive | 579 (38.4%) | 74 (25.43%) | 144 (26.18%) | 74 (25.43%) | ||
| Unknown | 223 (14.79%) | 28 (9.62%) | 61 (11.09%) | 28 (9.62%) | ||
| Parametrial invasion | <0.001 | 0.509 | ||||
| Negative | 1223 (81.1%) | 262 (90.03%) | 487 (88.55%) | 262 (90.03%) | ||
| Positive | 285 (18.9%) | 29 (9.97%) | 63 (11.45%) | 29 (9.97%) | ||
| Resection margin | 0.523 | 0.778 | ||||
| Negative | 1473 (97.68%) | 286 (98.28%) | 539 (98%) | 286 (98.28%) | ||
| Positive | 35 (2.32%) | 5 (1.72%) | 11 (2%) | 5 (1.72%) | ||
| Pelvic lymph node | <0.001 | 0.526 | ||||
| Negative | 1149 (76.55%) | 257 (88.32%) | 475 (86.84%) | 257 (88.32%) | ||
| Positive | 352 (23.45%) | 34 (11.68%) | 72 (13.16%) | 34 (11.68%) | ||
| Paraaortic lymph node | 0.042 | 0.744 | ||||
| Negative | 1468 (97.35%) | 289 (99.31%) | 547 (99.45%) | 289 (99.31%) | ||
| Positive | 40 (2.65%) | 2 (0.69%) | 3 (0.55%) | 2 (0.69%) | ||
| Initial treatment | <0.001 | <0.001 | ||||
| Surgery | 644 (42.71%) | 200 (68.73%) | 286 (52%) | 200 (68.73%) | ||
| Surgery + RT | 409 (27.12%) | 40 (13.75%) | 141 (25.64%) | 40 (13.75%) | ||
| Surgery + CCRT | 455 (30.17%) | 51 (17.53%) | 123 (22.36%) | 51 (17.53%) | ||
| PFS | OS | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Conization | ||||
| Not done | 1 | 1 | ||
| Done | 0.65 (0.41–1.01) | 0.056 | 0.59 (0.34–1.02) | 0.059 |
| Age | 0.98 (0.96–1.00) | 0.068 | 1.03 (1.01–1.05) | 0.011 |
| Cell type | ||||
| Squamous | 1 | 1 | ||
| Non-squamous | 1.92 (1.26–2.94) | 0.002 | 2.10 (1.27–3.48) | 0.004 |
| Total tumor size (cm) | 1.09 (0.97–1.21) | 0.139 | ||
| Depth of invasion | ||||
| <1/2 | 1 | |||
| >1/2 | 1.54 (0.95–2.48) | 0.080 | ||
| LVSI | ||||
| Negative | 1 | |||
| Positive | 1.98 (1.24–3.17) | 0.004 | ||
| Parametrial invasion | ||||
| Negative | 1 | 1 | ||
| Positive | 1.77 (0.95–3.29) | 0.072 | 2.10 (1.10–4.01) | 0.025 |
| Resection margin | ||||
| Negative | 1 | |||
| Positive | 2.71 (0.92–7.99) | 0.071 | ||
| Pelvic lymph node | ||||
| Negative | 1 | 1 | ||
| Positive | 1.91 (0.98–3.72) | 0.057 | 1.99 (1.08–3.67) | 0.027 |
| Paraaortic lymph node | ||||
| Negative | 1 | 1 | ||
| Positive | 10.86 (3.92–30.12) | <0.001 | 10.42 (3.43–31.64) | <0.001 |
| Initial treatment | ||||
| Surgery | 1 | |||
| Surgery + RT | 0.47 (0.25–0.89) | 0.020 | ||
| Surgery + CCRT | 0.45 (0.22–0.95) | 0.037 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, C.-S.; Min, J.S.; Song, K.H.; Choi, C.H.; Kim, T.-J.; Lee, J.-W.; Kim, B.-G.; Lee, Y.-Y. The Role of Conization before Radical Hysterectomy in Cervical Cancer including High Risk Factors of Recurrence: Propensity Score Matching. Cancers 2022, 14, 3863. https://doi.org/10.3390/cancers14163863
Chang C-S, Min JS, Song KH, Choi CH, Kim T-J, Lee J-W, Kim B-G, Lee Y-Y. The Role of Conization before Radical Hysterectomy in Cervical Cancer including High Risk Factors of Recurrence: Propensity Score Matching. Cancers. 2022; 14(16):3863. https://doi.org/10.3390/cancers14163863
Chicago/Turabian StyleChang, Chi-Son, Ji Song Min, Ki Hyeon Song, Chel Hun Choi, Tae-Joong Kim, Jeong-Won Lee, Byoung-Gie Kim, and Yoo-Young Lee. 2022. "The Role of Conization before Radical Hysterectomy in Cervical Cancer including High Risk Factors of Recurrence: Propensity Score Matching" Cancers 14, no. 16: 3863. https://doi.org/10.3390/cancers14163863
APA StyleChang, C.-S., Min, J. S., Song, K. H., Choi, C. H., Kim, T.-J., Lee, J.-W., Kim, B.-G., & Lee, Y.-Y. (2022). The Role of Conization before Radical Hysterectomy in Cervical Cancer including High Risk Factors of Recurrence: Propensity Score Matching. Cancers, 14(16), 3863. https://doi.org/10.3390/cancers14163863







