Simple Summary
This review summarizes reports from the latest clinical trials assessing the safety and clinical effectiveness of new biological drugs stimulating the immune system to fight cancer. The aim of this study is to show the enormous therapeutic potential of monoclonal antibodies in the treatment of cancer, in particular triple negative breast cancer (TNBC). Introduction of these innovative drugs to the standard clinical cancer therapies, including TNBC, allows for an increase in the response rate to the applied treatment, and consequently extending the lives of patients suffering from cancer. We hope to draw attention to the extremely difficult-to-treat TNBC, as well as the importance of the development of clinical trials evaluating drugs modulating the immune system in TNBC therapy.
Abstract
Triple-Negative Breast Cancer is a subtype of breast cancer characterized by the lack of expression of estrogen receptors, progesterone receptors, as well as human epidermal growth factor receptor 2. This cancer accounts for 15–20% of all breast cancers and is especially common in patients under 40 years of age, as well as with the occurring BRCA1 mutation. Its poor prognosis is reflected in the statistical life expectancy of 8–15 months after diagnosis of metastatic TNBC. So far, the lack of targeted therapy has narrowed therapeutic possibilities to classic chemotherapy. The idea behind the use of humanized monoclonal antibodies, as inhibitors of immunosuppressive checkpoints used by the tumor to escape from immune system control, is to reduce immunotolerance and direct an intensified anti-tumor immune response. An abundance of recent studies has provided numerous pieces of evidence about the safety and clinical benefits of immunotherapy using humanized monoclonal antibodies in the fight against many types of cancer, including TNBC. In particular, phase three clinical trials, such as the IMpassion 130, the KEYNOTE-355 and the KEYNOTE-522 resulted in the approval of immunotherapeutic agents, such as atezolizumab and pembrolizumab by the US Food and Drug Administration in TNBC therapy. This review aims to present the huge potential of immunotherapy using monoclonal antibodies directed against immunosuppressive checkpoints—such as atezolizumab, avelumab, durvalumab, pembrolizumab, nivolumab, cemiplimab, tremelimumab, ipilimumab—in the fight against difficult to treat TNBCs as monotherapy as well as in more advanced combination strategies.
1. Introduction
It is estimated that in 2020 there were approximately 2.3 million patients diagnosed with breast cancer (BC) worldwide and 685,000 died of BC [1]. It is supposed that triple negative breast cancer (TNBC) may account for 10–15% of diagnosed breast cancer [2]. This subtype of tumor is often found in patients under 40 years of age and/or with an occurring BRCA1 mutation [3]. Extensive research was conducted to better recognize the molecular phenotypes of breast cancer, which helps adjust treatment and develop new therapeutic opportunities. The clinical classification of BC includes hormone receptor-positive (HR+) tumors with the expression of estrogen (ER) and/or progesterone (PR) receptors, human epidermal receptor 2 (HER2) -enriched tumors with overexpression of HER2 in the absence of HR expression as well as triple-negative tumors without the expression of these three receptors [4]. Furthermore, BC can be categorized into molecular subtypes based on the immunohistochemical markers and complementary DNA (cDNA) microarrays:
- Luminal A (ER and PR positive and HER2 negative);
- Luminal B (ER and PR positive and HER2 positive or negative);
- Basal-like (ER and PR negative, HER2 positive or negative);
- HER2 overexpressing (ER and PR negative and HER2 positive) [5].
As TNBC do not express ER, PR, and HER2, TNBC is more diverse than other types in terms of worse outcomes, narrow therapeutic possibilities, and malignant characteristics such as rapid growth and formation of metastases [6]. Its aggressive characteristics reflect the dismal prognosis: the median overall survival of metastatic TNBC is 8–15 months [7]. Because of the actionable molecular targets, chemotherapy remains the main option in TNBC treatment. However, systemic chemotherapy provokes adverse effects and most patients quickly develop resistance. Furthermore, TNBC tends to relapse frequently, which creates the necessity to develop new therapeutic strategies [8].
2. Role of the Immune System
The immune system is a very important factor in the fight against cancer. Its role is to prevent the growth of neoplasm by destroying cancer cells as well as decreasing the possibility to metastasize. However, it can promote tumor progression [9]. The immune system is under self-control by immune checkpoints to protect the body’s natural, healthy cells from immune-mediated death, a process called peripheral tolerance [10]. The basis of this process is the recognition and binding of a T-cell receptor (TCR) to an antigen presented in the major histocompatibility complex (MHC) on the surface of an antigen-presented cell (APC). The cytotoxic T-lymphocyte-associated antigen-4 (CTLA-4), programmed cell death-1 (PD-1), and its ligands (PD-L1) are involved in the suppression of the T-cell immune response. It is supposed that the CTLA-4 and PD-1 pathways play roles at different stages of immune system activity. CTLA-4 is responsible for inhibiting a potentially autoaggressive T-cell at the early stages, especially in the lymph nodes. While the PD-1 pathway provides self-tolerance by regulating already activated T-cells at the later stages of an immune response—mostly in peripheral tissue [11].
Immunotherapy has shown high efficacy in the treatment of some types of tumors—such as melanoma, kidney and non-small cell lung cancer (NSCLC)—including immune checkpoint inhibitors (ICIs) as indications for treatment [12,13,14]. In TNBC with a lack of ER, PR and HER2, the use of monoclonal antibodies alone or with other therapeutic options such as chemotherapy, radiotherapy as well as select targeted therapies seems hopeful in early or advanced stages of TNBC. In this review, we aim to shed a light on immunotherapeutic opportunities using monoclonal antibodies approved by the U.S. Food and Drug Administration (FDA) in the treatment of TNBCs, such as atezolizumab and pembrolizumab, We also discuss additional immune checkpoint inhibitors (ICIs), such as nivolumab, avelumab, durvalumab, cemiplimab, tremelimumab and ipilimumab—currently undergoing clinical trials for evaluation of their safety and efficacy in patients with TNBC.
3. CTLA-4 Pathway
CTLA-4 is an immune checkpoint receptor expressed on the surface of activated T-cells. It is a CD28 homolog, however, it binds significantly stronger to B7-1 (CD80) or B7-2 (CD86) molecules presented on the APC [15]. Activation of the T-cells is possible due to the interaction of CD28 with B7-1/2. This leads to the proliferation of T-cells, increased T-cell survival and differentiation due to interleukin-2 production (as a growth factor), as well as increased energy metabolism and upregulation of cell survival genes. Nevertheless, the effect of interaction between CTLA-4 and B7 does not provide stimulation and it is suggested, that suppressive signals may be the result of this process [16]. This is particularly important when the immune system is overactive. Thus, the binding ratio of CD28 and B7 to CTLA-4 and B7 determines whether the T-cells will be activated or inhibited [17]. Furthermore, CTLA-4 may contribute to immune system control through other mechanisms. The expression of CTLA-4 on the surface of regulatory T-cells (Tregs) is constant. Tregs are responsible for regulating the activity of the effector T-cells by downregulating B7 ligands on APCs, leading to limited CD28 costimulation [18]. As a result, of the impairment of CD28:B7-mediated costimulation, there is a limitation of T-cell proliferation and their effector functions [19].
4. PD-1/PD-L1 Pathway
Programmed cell death protein 1 (PD-1) is a transmembrane protein from the B7-CD28 family and is referred to as an inhibitory immune checkpoint that affects T-cell regulation. The basis of this process is the interaction of PD-1 with its ligand—PD-L1 or PD-L2. It is thought that the PD-1 pathway contributes to the inhibition of T-cells proliferation, decreased production of interferon-γ (IFN-γ), tumor necrosis factor-α (TNF-α) and interleukine-2 (IL-2), as well as reduced T-cell survival [20].
PD-1 expression is noticed during T-cell activation and is present on the surface of all subsets of T-cells as well as other immune-related cells—such as B cells, natural killer (NK) cells, and myeloid cells [21]. Interestingly, PD-1 is expressed significantly higher on tumor-infiltrating T-cells [22]. It has been shown that higher expression of PD-1 is related to exhausted T-cells leading to an impaired antitumor response [23].
Binding T-cells by their TCR to an antigen expressed on the cell surface, leads to T-cell activation, proliferation, PD-1 upregulation, and inflammatory cytokine production. Their secretion may contribute to PD-L1 expression on the cancer cell surface, and subsequently after PD-1 and PD-L1 binding, results in suppression of TCR-mediated immune response [24]. Sustained expression of PD-1 and its ligands is usually noticeable during certain conditions—such as chronic infections or cancer. Thus, improvement of T-cell functions and reduction of tumor burden may be achieved by blocking the PD-1 pathway [25,26].
Moreover, it is thought that vascular endothelial growth factor A (VEGF-A)—a proangiogenic molecule produced from cancer cells—is a meaningful factor in the development of an immunosuppressive microenvironment. The basis of this process is the accumulation of myeloid-derived suppressor cells, the inhibition of dendritic cell maturation as well as the induction of regulatory T-cells. A recent study demonstrated that VEGF-A produced in the tumor microenvironment increased the expression of PD-1 and other inhibitory checkpoints involved in CD8+ T-cell exhaustion, which could be counteracted by antiangiogenic agents targeting VEGF-A-VEGFR [27].
5. Immunotherapy Using PD-1/PD-L1 Checkpoint Inhibitors
Cancer cells very often acquire the features that enable them to evade the immune system’s responses through immune checkpoint pathways or by forming an immunosuppressive microenvironment that causes tumor recognition impairment and disease development [28].
The immune checkpoints pathway is essential to protect normal tissue from immune system hyperactivity. The expression of PD-L1 in TNBC is about 20%, which is correlated with the development of resistance to specific CD8+ T-cells and higher tumorigenesis [29]. T-cells, B cells, natural killer (NK) T-cells express PD-1 receptor on their surface and it is correlated with the silencing of the immune system by the tumor. The purpose of using ICIs is to elicit an immune response by suppressing the inhibitory pathways (Figure 1) [30]. Thus, these features suggest a promising therapeutic target for this disease.
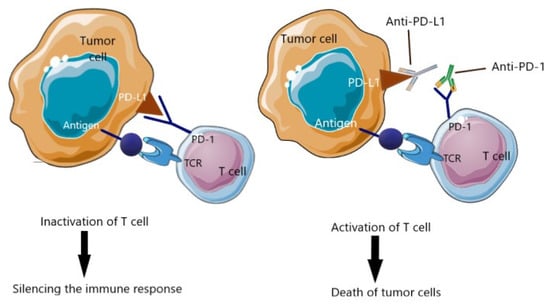
Figure 1.
Immune checkpoint inhibitors. The expression of PD-L1 allows tumor cells to switch T-cells off and keep the cancer cells from being killed. The use of immune checkpoint inhibitors permits boosting the immune response to kill the cancer cells. TCR, T-cell receptor; PD-1, programmed death protein 1; PD-L1, programmed death-ligand 1 [Own illustration designed on the basis of [4]].
Drugs including immunotherapeutic agents that are approved for TNBC therapy such as atezolizumab and pembrolizumab as well as other drugs such as AKT inhibitors, monoclonal antibodies, Poly ADP-Ribose Polymerase (PARP) inhibitors and antibody-drug conjugate currently being investigated in TNBC treatment are shown in Figure 2.
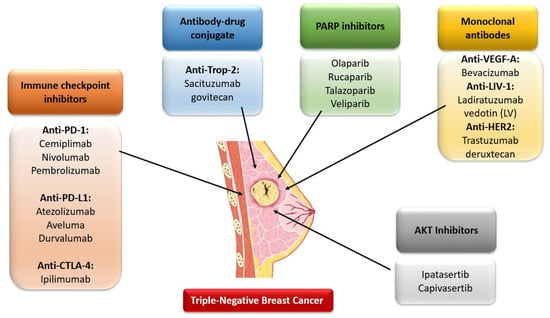
Figure 2.
Drugs including immunotherapeutic agents that are currently being investigated in TNBC treatment [Own illustration designed on the basis of [8]].
5.1. Atezolizumab
Atezolizumab is an Fc-engineered, humanized, monoclonal IgG1 antibody that selectively binds to programmed death-ligand 1 (PD-L1) and inhibits its interactions with PD-1 and B7.1 receptors causing T-cells more sensitive to the tumor. In a phase one of the clinical trial, atezolizumab as a single agent was evaluated in terms of safety and antitumor activity and showed good clinical outcomes and potential benefits in patients with metastatic TNBC especially in earlier lines of treatment or those with higher levels of tumor-infiltrating immune cells (ICs) and PD-L1 positive ICs [31].
The IMpassion130 was carried out to investigate the antitumor effects and clinical benefits of combining atezolizumab with taxane chemotherapeutic agent—paclitaxel in the form of nanoparticle albumin-bound (nab-paclitaxel)—in patients with unresectable, locally advanced or metastatic TNBC. In the first interim analysis, this combined therapy increased progression-free survival (PFS) compared with placebo plus nab-paclitaxel—(7.2 months compared to 5.5 months, respectively). Furthermore, higher differences were noticed among patients with PD-L1-positive tumors. The median PFS was 7.5 months in the atezolizumab group and 5.0 months in the placebo groups. Interestingly, therapy with atezolizumab prolonged overall survival (OS), particularly in groups with PD-L1 expression. There were 3.7 months of difference between the atezolizumab and control groups (21.3 vs. 17.6 months). In addition, there was a ten-month difference in median overall survival between the PD-L1 groups receiving atezolizumab and placebo (25.0 vs. 15.5 months properly). There were no significant differences between races. The most meaningful benefits occurred in the oldest patient TNBC group (≥65 years of age) [32].
The next interim overall survival analysis of IMpassion130 confirmed the previous results of improvement in PFS and OS. Thus, these findings clearly indicate antitumor activity as well as clinical benefits of combination therapy with atezolizumab and nab-paclitaxel, particularly for patients with PD-L1 immune cell-positive metastatic TNBC [33]. Based on the findings from the IMpassion130 clinical trial, the U.S. Food and Drug Administration and the European Commission have approved atezolizumab plus nab-paclitaxel for the treatment of adult patients with unresectable locally advanced or metastatic TNBC whose tumors have PD-L1 expression ≥1% and who have not received prior chemotherapy for metastatic disease [34].
The safety and efficacy of therapy with atezolizumab and nab-paclitaxel were also evaluated in a Japanese subgroup. The outcomes were consistent with those received from IMpassion130. This therapy prolonged PFS and showed a high objective response rate (ORR) even higher than the ORR announced in the IMpassion130 trial. Objectively, atezolizumab had a demonstrated safety profile and was well-tolerated in the Japanese population however, there were adverse events such as alopecia, peripheral sensory neuropathy, decreased neutrophil count, nasopharyngitis and decreased white blood cell count occurring more frequently than in the overall Impasssion130 population. These findings were limited by the small study population but can be contributed to the adjustment of combined therapy with the use of atezolizumab and nab-paclitaxel to the standards of treatment available in Japan [35].
5.2. Pembrolizumab
Pembrolizumab is a humanized, monoclonal IgG4 antibody that selectively binds to programmed death-1 (PD-1) receptor and inhibits interaction with its ligands—PD-L1 and PD-L2. The KEYNOTE-012 was the first study evaluating the safety and anti-cancer efficacy of pembrolizumab as a monotherapy in 32 enrolled, previously treated with chemotherapy patients with PD-L1-positive, advanced TNBC. In this 1b cohort study, this single agent showed an encouraging overall response rate (ORR) of 18.5% and with a demonstrated safety profile consistent with previous findings [36]. However, in the phase two of the KEYNOTE-086 study (cohort A) pembrolizumab did not provide significant outcomes in patients with mTNBC. ORR was 5.3% in a total group of 170 previously treated PD-L1-unselected patients [37]. Interestingly, in cohort B of the same investigation, ORR was 21.4% in patients with untreated PD-L1-positive tumors. Moreover, pembrolizumab demonstrated a clinically relevant median duration of response of 10.4 months and was well-tolerated. Thus, these results indicate that pembrolizumab has greater efficacy in the treatment of earlier metastatic stages [38].
In addition, some results point to the immunomodulatory potential of chemotherapy to improve anticancer response to ICIs [39]. A clinically significant antitumor effect of pembrolizumab combined with chemotherapy was demonstrated in the KEYNOTE-355 phase three clinical trial. In this randomized clinical trial—with 1372 patients enrolled—the combined therapy with this monoclonal antibody prolonged PFS as much as 4.1 months compared with placebo plus chemotherapy (9.7 months in the pembrolizumab plus chemotherapy group and 5.6 months in the chemotherapy alone group) among mTNBC patients with PD-L1 expression in whom a combined positive score (CPS) was ≥10. Furthermore, this trial included not only one chemotherapeutic option, such as presented in the IMPASSION-130 clinical trial (atezolizumab and nab-paclitaxel), but investigated several therapeutic standards—such as nab-paclitaxel, paclitaxel, or gemcitabine plus carboplatin—expanding the spectrum of possibilities. There were no new safety concerns. Adverse effects were noticed in 68% of the pembrolizumab group and 67% of the placebo group [40].
Pembrolizumab and Radiotherapy
Consistent with the previously noted findings concerning the immunomodulatory effects of radiotherapy (RT) in combination with ICIs, based on increasing cytotoxic T-cell levels and activation of apoptosis pathways, a phase two clinical trial demonstrated promising clinical benefits from the combination of RT and pembrolizumab. This study included a small group of 17 TNBC patients showing poor prognosis. The women were not divided into groups in terms of PD-L1 expression. The median ORR was 17.6%, similar to the findings with pembrolizumab as a single agent in pretreated patients with PD-L1-positive mTNBC. Furthermore, this combined therapy seemed to be safe with-low grade adverse effects. This study was limited to a small single-arm group and more future clinical trials are needed to confirm the clinical effectiveness [41].
5.3. Immunotherapy Combined with Antiangiogenic Factor
The impaired function of the tumor blood vessels may contribute to the decreasing levels of cytotoxic T-cells (involved in the fight against cancer) and increasing levels of myeloid-derived suppressor cells (MDSC) and regulatory T-cells (involved in inhibiting of the immune response). In addition, some research indicates that antiangiogenic therapy leads to the augmentation of PD-L1 expression as well as CD8+ T-cell infiltration in the tumor microenvironment. Thus, a reduction of the immunosuppression, as well as sensitizing the tumor to the immune response could be achieved by restoring proper perfusion [42].
Consistent with these promising findings, camrelizumab (PD-1 inhibitor) in combination with apatinib (tyrosine kinase inhibitor, which selectively inhibits vascular endothelial growth factor receptor 2 (VEGFR2)) was was investigated in patients with advanced TNBC. In this two phase clinical trial, this therapy showed a significant ORR of 43.3% and was well-tolerated, irrespective of PD-L1 expression. However, this open-label study had several limitations and large clinical trials with randomization are needed to confirm these results as to compare ICIs in combination with VEGFR2 inhibitors with ICIs plus placebo [7].
5.4. Durvalumab with Neoadjuvant Therapy
As previously mentioned, ICIs showed promising therapeutic benefits, especially in combination with chemotherapy. In the GeparNuevo phase two clinical trial, the combination of durvalumab (PD-1 inhibitor) with standard neoadjuvant chemotherapy was evaluated in early TNBC. In this study, the patients were randomized in terms of stromal tumor-infiltrating lymphocytes. Two weeks before starting treatment with chemotherapy, the patients received durvalumab or a placebo in monotherapy. Subsequently, the patients were treated with durvalumab or placebo (every four weeks) and nab-paclitaxel (weekly) for 12 weeks, followed by durvalumab or placebo and epirubicin/cyclo- phosphamide (EC) (four cycles). The use of durvalumab in combined therapy with nab-paclitaxel and EC demonstrated a higher pCR rate than the placebo group (53.4% vs. 44.2% respectively), however without statistical significance (p = 0.287). Nevertheless, the patients who had received durvalumab as a monotherapy two weeks before the main treatment showed a higher pCR rate than the placebo group (61.0% vs. 41.4%, p = 0.035). Thus, these findings suggest the potential benefits derived from using durvalumab with anthracycline/taxane-based therapy, particularly in patients pretreated with durvalumab as a single agent before the main therapy [43].
5.5. Nivolumab
Nivolumab is a human monoclonal antibody directed against the PD-1 immunoregulatory receptor located on the surface of T-cells. Despite the numerous indications for solid tumor treatment (melanoma, non-small cell lung cancer, malignant pleural mesothelioma, renal cell carcinoma, squamous cell cancer of the head and neck, urothelial cancer, colorectal cancer, oesophageal squamous cell carcinoma), research concerning the use of nivolumab in TNBC therapy is limited.
Recently, in the first stage of phase two TONIC clinical trial, nivolumab had shown high clinical efficacy among patients with metastatic TNBC. In this trial, 67 patients were divided into five cohorts, the first one was a control group with a two-week waiting period, and the other four included patients who received the induction treatment consisting of irradiation, low-dose cyclophosphamide, cisplatin, or doxorubicin for two weeks. After this short-term treatment, the therapy was continued for eight weeks with three cycles of nivolumab. In all cohorts, the objective response rate was 20% after full treatment. Additionally, the median progression-free survival was 1.9 months. The best results were noticed in the cisplatin and doxorubicin cohorts, where the ORR was 23% and 35%, respectively. Furthermore, treatment with cisplatin and doxorubicin was associated with the upregulation of immune-related genes involved in the PD-1/PD-L1 and T-cell cytotoxicity pathways. Thus, consistent with these findings pretreatment with the use of immunomodulating chemotherapeutic agents—such as cisplatin and doxorubicin—promotes a more favorable tumor microenvironment and provides a high and durable response to nivolumab, as well as the clinical benefits derived from this induction strategies therapy [44].
5.6. Avelumab
Avelumab is another immune checkpoint inhibitor. This human IgG1 monoclonal antibody directed against PD-L1 blocks the PD-1/PD-L1 pathway but does not affect PD-1/PD-L2 interaction [45]. The specific feature that distinguishes this agent is its second mechanism of action. In the preclinical studies, avelumab showed an additional advantage consisting of the ability to destroy human cancer cells by inducing antibody-dependent cell-mediated cytotoxicity (ADCC) [46]. Furthermore, an in vitro study was carried out to evaluate the avelumab-mediated ADCC on TNBC line cells, whose PD-L1 expression was changed with the use of peripheral blood mononuclear cells (PBMC) or purified NK cells from healthy donors. In this research, avelumab showed antitumor activity against TNBC cells independent of the PD-1/PD-L1 pathway. Avelumab increased TNBC cell death through an NK-mediated cytotoxicity mechanism. Additionally, higher expression of PD-L1 on tumor cells was related to increasing sensitivity to avelumab-mediated ADCC. Interestingly, the addition of IL-2 and IL-15 to the tumor cells contributed to the enhancement of the lysis of tumor cells through increased NK cell activity [47]. However, in clinical conditions in patients with metastatic breast cancer, avelumab in monotherapy did not show significant results. The phase one clinical trial JAVELIN enrolled 168 patients with various subtypes of breast cancer. This population included 58 patients with TNBC. The pretreatment of all patients had been a median of three prior therapies for metastatic disease. Among patients with TNBC, 50% of them had been previously treated with ≥2 prior lines of therapy for metastatic disease. The overall objective response rate was 3.0%, and 5.2% in the subgroup with TNBC. Furthermore, the percentage of patients in the overall population with PD-L1-positive tumors achieved a much higher ORR relative to the patients without PD-L1 expression (16.7% vs. 1.6% respectively and 22.2% vs. 2.6% respectively, in the TNBC subgroup). Additionally, avelumab as a single agent was well-tolerated and showed a safety profile consistent with previous findings [48].
5.7. Cemiplimab
Cemiplimab is an IgG4 monoclonal antibody blocking the PD-1 pathway. In a clinical trial among patients with metastatic cutaneous squamous cell carcinoma (CSCC), Cemiplimab showed a safety profile and high efficacy. Consistent with these findings, this agent was approved by the U.S. FDA for patients with metastatic CSCC or locally advanced CSCC [49]. However, to date, studies evaluating the safety and efficacy of TNBC therapy are ongoing and results are not yet available.
5.8. Tremelimumab
Tremelimumab is one of the first CTLA-4-pathway immune checkpoint inhibitors. This IgG2 monoclonal antibody has antitumor activity potential by inhibiting the CTLA-4 receptor expressed on activated T-cells, preventing the interaction between the antigen-presenting cell ligands B7-1 (CD80), B7-2 (CD86), and CTLA4. Disabling the CTLA-4-mediated inhibition pathway leads to binding the CD28 protein presented on T-cells with its B7-1/2 ligand on APCs. Thus, the use of this agent allows for increasing the activation of T-cells, as well as their effector functions to kill the cancer cells [50,51]. Currently, its safety and antitumor activity have been evaluated in many types of cancer. To date, tremelimumab has no indications for the treatment of any type of breast cancer. Its safety and activity were assessed in patients with HR-positive metastatic BC in combination with a steroidal aromatase inhibitor—exemestane. In this clinical trial, tremelimumab in combined therapy was well-tolerated with stable responses for ≥12 weeks in 42% of patients. Additionally, the immunomodulatory activity of tremelimumab was observed and associated with the augmented expression of inducible costimulator (ICOS) on CD4+ and CD8+ T-cells as well as a decreased number of FoxP3+ Treg cells [51,52]. Furthermore, a phase one clinical trial was conducted to investigate the safety and efficacy of tremelimumab with radiotherapy in patients with metastatic breast cancer. This study enrolled six patients—five with HR+ metastatic BC and one with TNBC. Tremelimumab in this strategy was safe and well-tolerated with the frequent adverse events such as lymphopenia, fatigue and rash. Objective responses were not observed. The most meaningful response was stable disease. Progression-free survival was 1.5 months, and overall survival was 50.8 months [52,53].
5.9. Ipilimumab
Ipilimumab is the second CTLA-4-pathway antagonist. It is a human IgG1 monoclonal antibody selectively binding with CTLA-4 receptor presented on the activated T-lymphocytes. To date, ipilimumab is approved by the U.S. Food and Drug Administration for the treatment of melanoma, renal cell carcinoma, colorectal cancer, hepatocellular carcinoma, non-small cell lung cancer and malignant pleural mesothelioma [53,54]. Despite many clinical trials in the treatment of solid tumors, studies focused on the efficacy and toxicity of ipilimumab in the treatment of breast cancer, especially in TNBC, are less abundant. An in vitro study showed that the inhibition of CTLA-4 receptors by ipilimumab has an impact on the release of IL-2 by tumor cells simultaneously regulating the tumor microenvironment and increasing the immune response [55]. In a clinical study in a group of 29 patients with relapsed malignancy, after a single infusion of ipilimumab, enhanced intracellular CTLA-4 expression (probably due to T-cell activation) as well as increased levels of activated T lymphocytes were observed without significant changes in the regulatory T-cell population [56]. In addition, ipilimumab was evaluated in a pilot study in patients with breast cancer. Nineteen patients were enrolled in this clinical trial, 12 of them received ipilimumab—six patients received ipilimumab in monotherapy and six patients received ipilimumab with cryoablation. After the use of combination immunotherapy, an increase in T helper type 1 cytokines, ICOS+Ki67+CD4+, and ICOS+Ki67+CD8+ T-cells was observed as well as an increased CD8+ Tcell/FoxP3+ Treg ratio within the tumor. Thus, consistent with these findings, the combination of Ipilimumab with cryoablation may contribute to the anti-tumor benefits derived from this strategy [57,58].
6. Biomarkers
Because not all patients respond to the administered immunotherapy, there is a strong need to identify prognostic and predictive biomarkers of response to the applied treatment, which would allow the selection of patients only to the group that would respond to the applied treatment. As it turns out, the implementation of ICIs for mTNBC therapy in patients with high tumor-infiltrating lymphocytes (TILs) shows encouraging results, which indicates the potential benefits of the applied immunotherapy for these patients [59]. Some authors, for instance, Xiao, Y., et al., in their studies, suggest the use of TILs and immune checkpoint molecules as biomarkers providing information about the effectiveness of treatment using ICIs in patients with TNBC [60]. Interestingly, the selection based on PD-L1 is quite controversial due to the lack of a consistent assessment standard. Additionally, new biomarkers like immune gene signatures liquid biopsy, and gut microbiome are still under research and cannot yet be used in clinical practice. Therefore, it is necessary to develop complex methods and further research into new and already known potential biomarkers of the response to immunotherapy in patients with TNBC [59].
7. Immune-Related Adverse Events (IRAEs)
The activation of the immune system using ICIs is also associated with the occurrence of characteristic side effects that differ from chemotherapy due to the mechanism of immune-related toxicity, a delayed onset and prolonged duration. IRAEs usually develop within weeks to months of starting immunotherapy. Nevertheless, they can appear at any time, even after the use of ICIs has been discontinued. The most common IRAEs include dermatologic toxicities, endocrine toxicities, gastrointestinal toxicities and hepatitis. Rarely developing IRAEs involve the cardiovascular, pulmonary, musculoskeletal, ocular, and central nervous systems. Nevertheless, these toxicities can develop in almost any organ. Reducing IRAEs very often requires a comprehensive approach and the involvement of a multidisciplinary medical team. Corticosteroids are most commonly used to mitigate the effects of ICIs, but other measures may also be required, such as additional immunosuppression, delay, or discontinuation of treatment. Therefore, it is also extremely important to educate both healthcare professionals and patients to identify IRAEs early and manage treatment appropriately [61].
8. Conclusions
Immunotherapy is without a doubt a groundbreaking achievement having a big impact on the improvement of clinical conditions and could be a life-changing opportunity for patients struggling with a highly aggressive type of breast cancer. Immune checkpoints are the most often used by cancer to switch T-cells off and keep the cancer cells from being killed. The use of immune checkpoint inhibitors permits boosting the immune response to kill the cancer cells. Current studies clearly indicate the necessity to combine the ICIs in various therapeutic regimens in order to increase their effectiveness and clinical benefits (Table 1, Table 2, Table 3, Table 4, Table 5, Table 6, Table 7 and Table 8). Furthermore, there is a strong need to implement immunotherapy in the early-stage setting of metastatic treatment to increase the overall response rate [58].

Table 1.
Atezolizumab.

Table 2.
Pembrolizumab.

Table 3.
Nivolumab.

Table 4.
Avelumab.

Table 5.
Cemiplimab.

Table 6.
Durvalumab.

Table 7.
Ipilimumab.

Table 8.
Tremelimumab.
Author Contributions
Conceptualization, J.W. and A.T.-K.; writing—original draft preparation, J.W. and A.T.-K.; writing—review and editing, J.W., A.T.-K. and D.P.; figures preparation, J.W.; supervision, D.P.; funding acquisition, A.T.-K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the Medical University of Bialystok, Poland (grant number SUB/2/DN/22/001/2228).
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/breast-cancer (accessed on 15 October 2021).
- Keenan, T.E.; Tolaney, S.M. Role of Immunotherapy in Triple-Negative Breast Cancer. J. Natl. Compr. Cancer. Netw. 2020, 18, 479–489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Irvin, W.J.J.; Carey, L.A. What is triple-negative breast cancer? Eur. J. Cancer 2008, 44, 2799–2805. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.; Al-Khadairi, G.; Decock, J. Immune Checkpoint Inhibitors in Triple Negative Breast Cancer Treatment: Promising Future Prospects. Front. Oncol. 2021, 10, 600573. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Aggarwal, R. An overview of triple-negative breast cancer. Arch. Gynecol. Obs. 2016, 293, 247–269. [Google Scholar] [CrossRef]
- American Cancer Society: Triple-Negative Breast Cancer. Available online: https://www.cancer.org/cancer/breast-cancer/about/types-of-breast-cancer/triple-negative.html (accessed on 15 October 2021).
- Liu, J.; Liu, Q.; Li, Y.; Li, Q.; Su, F.; Yao, H.; Su, S.; Wang, Q.; Jin, L.; Wang, Y.; et al. Efficacy and safety of camrelizumab combined with apatinib in advanced triple-negative breast cancer: An open-label phase II trial. J. Immunother. Cancer 2020, 8, e000696. [Google Scholar] [CrossRef]
- American Cancer Society: Treatment of Triple-Negative Breast Cancer. Available online: https://www.cancer.org/cancer/breast-cancer/treatment/treatment-of-triple-negative.html (accessed on 15 October 2021).
- Disis, M.L. Immune regulation of cancer. J. Clin. Oncol. 2010, 28, 4531–4538. [Google Scholar] [CrossRef]
- ElTanbouly, M.A.; Noelle, R.J. Rethinking peripheral T-cell tolerance: Checkpoints across a T-cell’s journey. Nat. Rev. Immunol. 2021, 21, 257–267. [Google Scholar] [CrossRef]
- Fife, B.T.; Bluestone, J.A. Control of peripheral T-cell tolerance and autoimmunity via the CTLA-4 and PD-1 pathways. Immunol. Rev. 2008, 224, 166–182. [Google Scholar] [CrossRef]
- Gettinger, S.; Horn, L.; Jackman, D.; Spigel, D.; Antonia, S.; Hellmann, M.; Powderly, J.; Heist, R.; Sequist, L.V.; Smith, D.C.; et al. Five-Year Follow-Up of Nivolumab in Previously Treated Advanced Non-Small-Cell Lung Cancer: Results From the CA209-003 Study. J. Clin. Oncol. 2018, 36, 1675–1684. [Google Scholar] [CrossRef]
- Wolchok, J.D.; Chiarion-Sileni, V.; Gonzalez, R.; Rutkowski, P.; Grob, J.J.; Cowey, C.L.; Lao, C.D.; Wagstaff, J.; Schadendorf, D.; Ferrucci, P.F.; et al. Overall Survival with Combined Nivolumab and Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2017, 377, 1345–1356. [Google Scholar] [CrossRef]
- Motzer, R.J.; Escudier, B.; McDermott, D.F.; George, S.; Hammers, H.J.; Srinivas, S.; Tykodi, S.S.; Sosman, J.A.; Procopio, G.; Plimack, E.R.; et al. CheckMate 025 Investigators. Nivolumab versus Everolimus in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2015, 373, 1803–1813. [Google Scholar] [CrossRef] [Green Version]
- Collins, A.V.; Brodie, D.W.; Gilbert, R.J.; Iaboni, A.; Manso-Sancho, R.; Walse, B.; Stuart, D.I.; van der Merwe, P.A.; Davis, S.J. The interaction properties of costimulatory molecules revisited. Immunity 2002, 17, 201–210. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.; Flies, D.B. Molecular mechanisms of T-cell co-stimulation and co-inhibition. Nat. Rev. Immunol. 2013, 13, 227–242. [Google Scholar] [CrossRef]
- Krummel, M.F.; Allison, J.P. CD28 and CTLA-4 have opposing effects on the response of T-cells to stimulation. J. Exp. Med. 1995, 182, 459–465. [Google Scholar] [CrossRef] [Green Version]
- Qureshi, O.S.; Zheng, Y.; Nakamura, K.; Attridge, K.; Manzotti, C.; Schmidt, E.M.; Baker, J.; Jeffery, L.E.; Kaur, S.; Briggs, Z.; et al. Trans-endocytosis of CD80 and CD86: A molecular basis for the cell-extrinsic function of CTLA-4. Science 2011, 332, 600–603. [Google Scholar] [CrossRef] [Green Version]
- Wing, K.; Onishi, Y.; Prieto-Martin, P.; Yamaguchi, T.; Miyara, M.; Fehervari, Z.; Nomura, T.; Sakaguchi, S. CTLA-4 control over Foxp3+ regulatory T-cell function. Science 2008, 322, 271–275. [Google Scholar] [CrossRef]
- Keir, M.E.; Butte, M.J.; Freeman, G.J.; Sharpe, A.H. PD-1 and its ligands in tolerance and immunity. Annu. Rev. Immunol. 2008, 26, 677–704. [Google Scholar] [CrossRef] [Green Version]
- Sharpe, A.H.; Pauken, K.E. The diverse functions of the PD1 inhibitory pathway. Nat. Rev. Immunol. 2018, 18, 153–167. [Google Scholar] [CrossRef]
- Han, Y.; Liu, D.; Li, L. PD-1/PD-L1 pathway: Current researches in cancer. Am. J. Cancer Res. 2020, 10, 727–742. [Google Scholar]
- Ahmadzadeh, M.; Johnson, L.A.; Heemskerk, B.; Wunderlich, J.R.; Dudley, M.E.; White, D.E.; Rosenberg, S.A. Tumor antigen-specific CD8 T-cells infiltrating the tumor express high levels of PD-1 and are functionally impaired. Blood 2009, 114, 1537–1544. [Google Scholar] [CrossRef]
- Buchbinder, E.I.; Desai, A. CTLA-4 and PD-1 Pathways: Similarities, Differences, and Implications of Their Inhibition. Am. J. Clin. Oncol. 2016, 39, 98–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barber, D.L.; Wherry, E.J.; Masopust, D.; Zhu, B.; Allison, J.P.; Sharpe, A.H.; Freeman, G.J.; Ahmed, R. Restoring function in exhausted CD8 T-cells during chronic viral infection. Nature 2006, 439, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Pauken, K.E.; Wherry, E.J. Overcoming T-cell exhaustion in infection and cancer. Trends Immunol. 2015, 36, 265–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voron, T.; Colussi, O.; Marcheteau, E.; Pernot, S.; Nizard, M.; Pointet, A.L.; Latreche, S.; Bergaya, S.; Benhamouda, N.; Tanchot, C.; et al. VEGF-A modulates expression of inhibitory checkpoints on CD8+ T-cells in tumors. J. Exp. Med. 2015, 212, 139–148. [Google Scholar] [CrossRef]
- Schreiber, R.D.; Old, L.J.; Smyth, M.J. Cancer immunoediting: Integrating immunity’s roles in cancer suppression and promotion. Science 2011, 331, 1565–1570. [Google Scholar] [CrossRef] [Green Version]
- Mittendorf, E.A.; Philips, A.V.; Meric-Bernstam, F.; Qiao, N.; Wu, Y.; Harrington, S.; Su, X.; Wang, Y.; Gonzalez-Angulo, A.M.; Akcakanat, A.; et al. PD-L1 expression in triple-negative breast cancer. Cancer Immunol. Res. 2014, 2, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Bayraktar, S.; Batoo, S.; Okuno, S.; Glück, S. Immunotherapy in breast cancer. J. Carcinog. 2019, 18, 2. [Google Scholar] [CrossRef]
- Emens, L.A.; Cruz, C.; Eder, J.P.; Braiteh, F.; Chung, C.; Tolaney, S.M.; Kuter, I.; Nanda, R.; Cassier, P.A.; Delord, J.P.; et al. Long-term Clinical Outcomes and Biomarker Analyses of Atezolizumab Therapy for Patients With Metastatic Triple-Negative Breast Cancer: A Phase 1 Study. JAMA Oncol. 2019, 5, 74–82. [Google Scholar] [CrossRef]
- Schmid, P.; Adams, S.; Rugo, H.S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Hegg, R.; Im, S.A.; Shaw Wright, G.; et al. IMpassion130 Trial Investigators. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2018, 379, 2108–2121. [Google Scholar] [CrossRef]
- Schmid, P.; Rugo, H.S.; Adams, S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Henschel, V.; Molinero, L.; Chui, S.Y.; et al. Atezolizumab plus nab-paclitaxel as first-line treatment for unresectable, locally advanced or metastatic triple-negative breast cancer (IMpassion130): Updated efficacy results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2020, 21, 44–59. [Google Scholar] [CrossRef]
- Narayan, P.; Wahby, S.; Gao, J.J.; Amiri-Kordestani, L.; Ibrahim, A.; Bloomquist, E.; Tang, S.; Xu, Y.; Liu, J.; Fu, W.; et al. FDA Approval Summary: Atezolizumab Plus Paclitaxel Protein-bound for the Treatment of Patients with Advanced or Metastatic TNBC Whose Tumors Express PD-L1. Clin. Cancer Res. 2020, 26, 2284–2289. [Google Scholar] [CrossRef] [Green Version]
- Iwata, H.; Inoue, K.; Kaneko, K.; Ito, Y.; Tsugawa, K.; Hasegawa, A.; Nakagawa, S.; Kuratomi, H.; Tamura, K. Subgroup analysis of Japanese patients in a Phase 3 study of atezolizumab in advanced triple-negative breast cancer (IMpassion130). Jpn. J. Clin. Oncol. 2019, 49, 1083–1091. [Google Scholar] [CrossRef] [Green Version]
- Nanda, R.; Chow, L.Q.; Dees, E.C.; Berger, R.; Gupta, S.; Geva, R.; Pusztai, L.; Pathiraja, K.; Aktan, G.; Cheng, J.D.; et al. Pembrolizumab in Patients With Advanced Triple-Negative Breast Cancer: Phase Ib KEYNOTE-012 Study. J. Clin. Oncol. 2016, 34, 2460–2467. [Google Scholar] [CrossRef]
- Adams, S.; Schmid, P.; Rugo, H.S.; Winer, E.P.; Loirat, D.; Awada, A.; Cescon, D.W.; Iwata, H.; Campone, M.; Nanda, R.; et al. Pembrolizumab monotherapy for previously treated metastatic triple-negative breast cancer: Cohort A of the phase II KEYNOTE-086 study. Ann. Oncol. 2019, 30, 397–404. [Google Scholar] [CrossRef] [Green Version]
- Adams, S.; Loi, S.; Toppmeyer, D.; Cescon, D.W.; De Laurentiis, M.; Nanda, R.; Winer, E.P.; Mukai, H.; Tamura, K.; Armstrong, A.; et al. Pembrolizumab monotherapy for previously untreated, PD-L1-positive, metastatic triple-negative breast cancer: Cohort B of the phase II KEYNOTE-086 study. Ann. Oncol. 2019, 30, 405–411. [Google Scholar] [CrossRef] [Green Version]
- Ramakrishnan, R.; Gabrilovich, D.I. Mechanism of synergistic effect of chemotherapy and immunotherapy of cancer. Cancer Immunol. Immunother. 2011, 60, 419–423. [Google Scholar] [CrossRef]
- Cortes, J.; Cescon, D.W.; Rugo, H.S.; Nowecki, Z.; Im, S.A.; Yusof, M.M.; Gallardo, C.; Lipatov, O.; Barrios, C.H.; Holgado, E.; et al. KEYNOTE-355 Investigators. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): A randomised, placebo-controlled, double-blind, phase 3 clinical trial. Lancet 2020, 396, 1817–1828. [Google Scholar] [CrossRef]
- Ho, A.Y.; Barker, C.A.; Arnold, B.B.; Powell, S.N.; Hu, Z.I.; Gucalp, A.; Lebron-Zapata, L.; Wen, H.Y.; Kallman, C.; D’Agnolo, A.; et al. A phase 2 clinical trial assessing the efficacy and safety of pembrolizumab and radiotherapy in patients with metastatic triple-negative breast cancer. Cancer 2020, 126, 850–860. [Google Scholar] [CrossRef]
- Li, Q.; Wang, Y.; Jia, W.; Deng, H.; Li, G.; Deng, W.; Chen, J.; Kim, B.Y.S.; Jiang, W.; Liu, Q.; et al. Low-Dose Anti-Angiogenic Therapy Sensitizes Breast Cancer to PD-1 Blockade. Clin. Cancer Res. 2020, 26, 1712–1724. [Google Scholar] [CrossRef] [Green Version]
- Loibl, S.; Untch, M.; Burchardi, N.; Huober, J.; Sinn, B.V.; Blohmer, J.U.; Grischke, E.M.; Furlanetto, J.; Tesch, H.; Hanusch, C.; et al. A randomised phase II study investigating durvalumab in addition to an anthracycline taxane-based neoadjuvant therapy in early triple-negative breast cancer: Clinical results and biomarker analysis of GeparNuevo study. Ann. Oncol. 2019, 30, 1279–1288. [Google Scholar] [CrossRef] [Green Version]
- Voorwerk, L.; Slagter, M.; Horlings, H.M.; Sikorska, K.; van de Vijver, K.K.; de Maaker, M.; Nederlof, I.; Kluin, R.J.C.; Warren, S.; Ong, S.; et al. Immune induction strategies in metastatic triple-negative breast cancer to enhance the sensitivity to PD-1 blockade: The TONIC trial. Nat. Med. 2019, 25, 920–928. [Google Scholar] [CrossRef]
- Heery, C.R.; O’Sullivan-Coyne, G.; Madan, R.A.; Cordes, L.; Rajan, A.; Rauckhorst, M.; Lamping, E.; Oyelakin, I.; Marté, J.L.; Lepone, L.M.; et al. Avelumab for metastatic or locally advanced previously treated solid tumours (JAVELIN Solid Tumor): A phase 1a, multicohort, dose-escalation trial. Lancet Oncol 2017, 18, 587–598. [Google Scholar] [CrossRef]
- Boyerinas, B.; Jochems, C.; Fantini, M.; Heery, C.R.; Gulley, J.L.; Tsang, K.Y.; Schlom, J. Antibody-Dependent Cellular Cytotoxicity Activity of a Novel Anti-PD-L1 Antibody Avelumab (MSB0010718C) on Human Tumor Cells. Cancer Immunol. Res. 2015, 3, 1148–1157. [Google Scholar] [CrossRef] [Green Version]
- Juliá, E.P.; Amante, A.; Pampena, M.B.; Mordoh, J.; Levy, E.M. Avelumab, an IgG1 anti-PD-L1 Immune Checkpoint Inhibitor, Triggers NK Cell-Mediated Cytotoxicity and Cytokine Production Against Triple Negative Breast Cancer Cells. Front. Immunol. 2018, 9, 2140. [Google Scholar] [CrossRef]
- Dirix, L.Y.; Takacs, I.; Jerusalem, G.; Nikolinakos, P.; Arkenau, H.T.; Forero-Torres, A.; Boccia, R.; Lippman, M.E.; Somer, R.; Smakal, M.; et al. Avelumab, an anti-PD-L1 antibody, in patients with locally advanced or metastatic breast cancer: A phase 1b JAVELIN Solid Tumor study. Breast Cancer Res. Treat. 2018, 167, 671–686. [Google Scholar] [CrossRef] [Green Version]
- Migden, M.R.; Chandra, S.; Rabinowits, G.; Chen, C.I.; Desai, J.; Seluzhytsky, A.; Sasane, M.; Campanelli, B.; Chen, Z.; Freeman, M.L.; et al. CASE (CemiplimAb-rwlc Survivorship and Epidemiology) study in advanced cutaneous squamous cell carcinoma. Future Oncol. 2020, 16, 11–19. [Google Scholar] [CrossRef] [Green Version]
- National Cancer Institute. Available online: https://www.cancer.gov/publications/dictionaries/cancer-drug/def/tremelimumab (accessed on 10 December 2021).
- Vonderheide, R.H.; LoRusso, P.M.; Khalil, M.; Gartner, E.M.; Khaira, D.; Soulieres, D.; Dorazio, P.; Trosko, J.A.; Rüter, J.; Mariani, G.L.; et al. Tremelimumab in combination with exemestane in patients with advanced breast cancer and treatment-associated modulation of inducible costimulator expression on patient T-cells. Clin. Cancer Res. 2010, 16, 3485–3494. [Google Scholar] [CrossRef] [Green Version]
- Jiang, D.M.; Fyles, A.; Nguyen, L.T.; Neel, B.G.; Sacher, A.; Rottapel, R.; Wang, B.X.; Ohashi, P.S.; Sridhar, S.S. Phase I study of local radiation and tremelimumab in patients with inoperable locally recurrent or metastatic breast cancer. Oncotarget 2019, 10, 2947–2958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaddepally, R.K.; Kharel, P.; Pandey, R.; Garje, R.; Chandra, A.B. Review of Indications of FDA-Approved Immune Checkpoint Inhibitors per NCCN Guidelines with the Level of Evidence. Cancers 2020, 12, 738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yervoy FDA Approval History. Available online: https://www.drugs.com/history/yervoy.html (accessed on 10 December 2021).
- Navarrete-Bernal, M.G.C.; Cervantes-Badillo, M.G.; Martínez-Herrera, J.F.; Lara-Torres, C.O.; Gerson-Cwilich, R.; Zentella-Dehesa, A.; Ibarra-Sánchez, M.J.; Esparza-López, J.; Montesinos, J.J.; Cortés-Morales, V.A.; et al. Biological Landscape of Triple Negative Breast Cancers Expressing CTLA-4. Front. Oncol. 2020, 10, 1206. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Bashey, A.; Zhong, R.; Corringham, S.; Messer, K.; Pu, M.; Ma, W.; Chut, T.; Soiffer, R.; Mitrovich, R.C.; et al. CTLA-4 blockade following relapse of malignancy after allogeneic stem cell transplantation is associated with T-cell activation but not with increased levels of T regulatory cells. Biol. Blood Marrow Transplant. 2011, 17, 682–692. [Google Scholar] [CrossRef] [Green Version]
- McArthur, H.L.; Diab, A.; Page, D.B.; Yuan, J.; Solomon, S.B.; Sacchini, V.; Comstock, C.; Durack, J.C.; Maybody, M.; Sung, J.; et al. A Pilot Study of Preoperative Single-Dose Ipilimumab and/or Cryoablation in Women with Early-Stage Breast Cancer with Comprehensive Immune Profiling. Clin. Cancer Res. 2016, 22, 5729–5737. [Google Scholar] [CrossRef] [Green Version]
- Marra, A.; Viale, G.; Curigliano, G. Recent advances in triple negative breast cancer: The immunotherapy era. BMC Med. 2019, 17, 90. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Tian, Q.; Zhang, M.; Wang, H.; Wu, L.; Yang, J. Immune-related biomarkers in triple-negative breast cancer. Breast Cancer 2021, 28, 792–805. [Google Scholar] [CrossRef]
- Xiao, Y.; Ma, D.; Zhao, S.; Suo, C.; Shi, J.; Xue, M.Z.; Ruan, M.; Wang, H.; Zhao, J.; Li, Q.; et al. Multi-Omics Profiling Reveals Distinct Microenvironment Characterization and Suggests Immune Escape Mechanisms of Triple-Negative Breast Cancer. Clin. Cancer Res. 2019, 25, 5002–5014. [Google Scholar] [CrossRef] [Green Version]
- Gumusay, O.; Callan, J.; Rugo, H.S. Immunotherapy toxicity: Identification and management. Breast Cancer Res. Treat. 2022, 192, 1–17. [Google Scholar] [CrossRef]
- Miles, D.; Gligorov, J.; André, F.; Cameron, D.; Schneeweiss, A.; Barrios, C.; Xu, B.; Wardley, A.; Kaen, D.; Andrade, L.; et al. Primary results from IMpassion131, a double-blind, placebo-controlled, randomised phase III trial of first-line paclitaxel with or without atezolizumab for unresectable locally advanced/metastatic triple-negative breast cancer. Ann. Oncol. 2021, 32, 994–1004. [Google Scholar] [CrossRef]
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04148911?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=3 (accessed on 7 January 2022).
- Wang, H.; Ma, H.; Sové, R.J.; Emens, L.A.; Popel, A.S. Quantitative systems pharmacology model predictions for efficacy of atezolizumab and nab-paclitaxel in triple-negative breast cancer. J. Immunother. Cancer 2021, 9, e002100. [Google Scholar] [CrossRef]
- Adams, S.; Diéras, V.; Barrios, C.H.; Winer, E.P.; Schneeweiss, A.; Iwata, H.; Loi, S.; Patel, S.; Henschel, V.; Chui, S.Y.; et al. Patient-reported outcomes from the phase III IMpassion130 trial of atezolizumab plus nab-paclitaxel in metastatic triple-negative breast cancer. Ann. Oncol. 2020, 31, 582–589. [Google Scholar] [CrossRef]
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03281954?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=2 (accessed on 7 January 2022).
- Kyte, J.A.; Røssevold, A.; Falk, R.S.; Naume, B. ALICE: A randomized placebo-controlled phase II study evaluating atezolizumab combined with immunogenic chemotherapy in patients with metastatic triple-negative breast cancer. J. Transl. Med. 2020, 18, 252. [Google Scholar] [CrossRef]
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04690855?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=11 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT04584112?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=5 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03498716?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=6 (accessed on 7 January 2022).
- Mittendorf, E.A.; Zhang, H.; Barrios, C.H.; Saji, S.; Jung, K.H.; Hegg, R.; Koehler, A.; Sohn, J.; Iwata, H.; Telli, M.L.; et al. Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early-stage triple-negative breast cancer (IMpassion031): A randomised, double-blind, phase 3 trial. Lancet 2020, 396, 1090–1100. [Google Scholar] [CrossRef]
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04177108?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=10 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03256344?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=12 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03292172?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=14 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04739670?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=15 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03371017?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=7 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04770272?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=13 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03206203?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=16 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03756298?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=17 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02530489?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=27&view=results (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04408118?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=18 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03853707?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=28 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03483012?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=23 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03101280?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=20 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT01898117?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=25 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03464942?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=24 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02883062?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=22 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04249167?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=21 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02322814?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=26 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04434040?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=19 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03800836?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=29 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03961698?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=31 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02620280?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=32 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04849364?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=30 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04639245?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=35 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02708680?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=37 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03915678?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=34 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03424005?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=33 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03289962?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=36 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT05001347?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=38 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03829501?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=40 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02543645?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=42 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03170960?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=41 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04638751?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=43 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03232593?term=NCT03232593&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03952325?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=47 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04102618?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=48 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04954599?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=49 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT05069935?term=atezolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=46 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04683679?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04095689?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=2 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04427293?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=3 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04024800?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=4 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT02977468?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=5 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03362060?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=5 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04191135?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=7 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02768701?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=8 (accessed on 7 January 2022).
- Schmid, P.; Salgado, R.; Park, Y.H.; Muñoz-Couselo, E.; Kim, S.B.; Sohn, J.; Im, S.A.; Foukakis, T.; Kuemmel, S.; Dent, R.; et al. Pembrolizumab plus chemotherapy as neoadjuvant treatment of high-risk, early-stage triple-negative breast cancer: Results from the phase 1b open-label, multicohort KEYNOTE-173 study. Ann. Oncol. 2020, 31, 569–581. [Google Scholar] [CrossRef] [PubMed]
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03720431?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=10 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03121352?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=11 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03036488?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=12 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03145961?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=13 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03567720?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=15 (accessed on 7 January 2022).
- Winer, E.P.; Lipatov, O.; Im, S.A.; Goncalves, A.; Muñoz-Couselo, E.; Lee, K.S.; Schmid, P.; Tamura, K.; Testa, L.; Witzel, I.; et al. KEYNOTE-119 investigators. Pembrolizumab versus investigator-choice chemotherapy for metastatic triple-negative breast cancer (KEYNOTE-119): A randomised, open-label, phase 3 trial. Lancet Oncol. 2021, 22, 499–511. [Google Scholar] [CrossRef]
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03639948?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=17 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03184558?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=18 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04986852?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=19 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04468061?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=20 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02734290?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03752723?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02981303?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=23 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03644589?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=24 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02755272?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=25 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04373031?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02971761?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=28 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT02513472?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=29 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03310957?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=30 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03599453?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=32 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03106415?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=33 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT02730130?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=34 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04634747?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=35 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03225547?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=36 (accessed on 7 January 2022).
- Vinayak, S.; Tolaney, S.M.; Schwartzberg, L.; Mita, M.; McCann, G.; Tan, A.R.; Wahner-Hendrickson, A.E.; Forero, A.; Anders, C.; Wulf, G.M.; et al. Open-label Clinical Trial of Niraparib Combined With Pembrolizumab for Treatment of Advanced or Metastatic Triple-Negative Breast Cancer. JAMA Oncol. 2019, 5, 1132–1140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03012230?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=38 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02411656?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=39 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT01676753?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=40 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04301011?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=41 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04348747?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=42 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04879849?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=43 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT05082259?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=44 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04230109?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=45 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03197389?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=46 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04443348?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=47 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT05112536?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=48 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03775850?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=49 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03289819?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT04432857?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=51 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03396445?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=52 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT01986426?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=53 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03761914?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=54 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03797326?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=55 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04265872?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=56 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04332653?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=57 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04429542?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=58 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT05082610?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=59 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02644369?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=60 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT05094804?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=61 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT05070247?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=63 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04725331?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=64 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03454451?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=65 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03849469?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=66 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04234113?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=67 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02178722?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=68 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT05007106?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=70 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03621982?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=71 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04348916?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=73 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT01042379?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=74 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04060342?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=75 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT03366844?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=76 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04148937?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=77 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03277352?term=pembrolizumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=78 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT04331067?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT02393794?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=2 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT03818685?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=3 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT03487666?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=4 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT03414684?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=5 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/results/NCT03316586?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=6 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT02499367?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=7 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/results/NCT03098550?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=8 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT04159818?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=9 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/results/NCT04142931?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=10 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/results/NCT02834247?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=11 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT03546686?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=12 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT03435640?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=14 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT02637531?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=15 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT03829436?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=16 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT04423029?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=17 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT03667716?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=18 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT04561362?term=Nivolumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=19 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT02926196?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT04360941?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=2 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT04188119?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=3 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT03971409?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=5 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/results/NCT03387085?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=7 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT03861403?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=9 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT02630368?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=10 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/record/NCT02554812?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=12 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT04551885?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=14 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://www.clinicaltrials.gov/ct2/show/results/NCT02222922?term=avelumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=15 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT04243616?term=cemiplimab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03199040?term=Durvalumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03167619?term=Durvalumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=2 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT02826434?term=NCT02826434&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT02489448?term=Tremelimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=4 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02527434?term=Tremelimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03982173?term=Tremelimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=3 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03616886?term=Durvalumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=4 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03356860?term=Durvalumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=5 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03742102?term=NCT03742102&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT04176848?term=NCT04176848&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03801369?term=Durvalumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=9 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03606967?term=ipilimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=10 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03740893?term=Durvalumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=14 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03739931?term=Durvalumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=17 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT04504669?term=NCT04504669&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03983954?term=NCT03983954&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT04556773?term=NCT04556773&draw=2&rank=1 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03544125?term=NCT03544125&draw=2&rank=1 (accessed on 7 January 2022).
- Ghebeh, H.; Al-Sayed, A.; Eiada, R.; Cabangon, L.; Ajarim, D.; Suleman, K.; Tulbah, A.; Al-Tweigeri, T. Weekly Paclitaxel given concurrently with Durvalumab has a favorable safety profile in triple-negative metastatic breast cancer. Sci. Rep. 2021, 11, 19154. [Google Scholar] [CrossRef] [PubMed]
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT02658214?term=Tremelimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=5 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03872505?term=durvalumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=3 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03752398?term=ipilimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=7 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT04434560?term=ipilimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=5 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02983045?term=ipilimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=6 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03126110?term=ipilimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=8 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03241173?term=ipilimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=9 (accessed on 7 January 2022).
- Bernal-Estévez, D.; Sánchez, R.; Tejada, R.E.; Parra-López, C. Chemotherapy and radiation therapy elicits tumor specific T-cell responses in a breast cancer patient. BMC Cancer 2016, 16, 591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT04879888?term=ipilimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=11 (accessed on 7 January 2022).
- Clinical Trials. Available online: https://clinicaltrials.gov/ct2/show/NCT03674827?term=Tremelimumab&cond=TNBC+-+Triple-Negative+Breast+Cancer&draw=2&rank=6 (accessed on 7 January 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).