Traditional Systemic Treatment Options in Advanced Low-Grade Serous Ovarian Cancer after Successful Cytoreduction: A Systematic Review and Meta-Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Study Selection
2.2. Study Selection
2.3. We Excluded Studies That
- Did not report specific information about type of adjuvant treatment;
- Did not include survival data;
- Included patients who did receive neoadjuvant treatment;
- Included other new targeted therapies: Poly-ADP ribose polymerase (PARP) inhibitors, MEK inhibitors, and antiangiogenics;
- Included patients who received intraperitoneal chemotherapy;
- Grey Literature was not considered—case reports, letters, and comments were excluded.
2.4. Statistical Analysis
2.5. Quality Assessment of Studies
3. Results
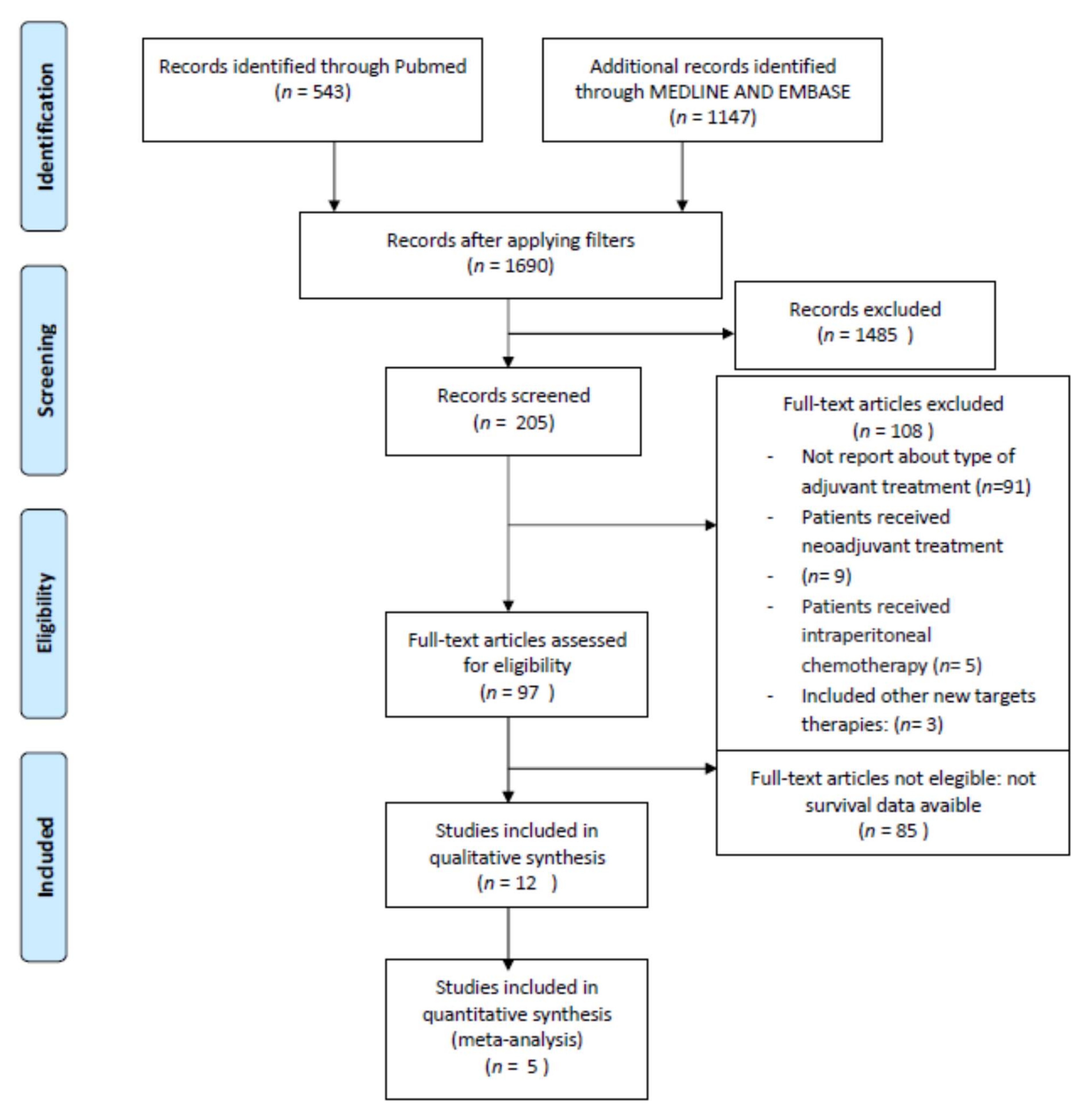
3.1. Evidence Acquisition
3.2. Study Characteristics
3.3. Qualitative Synthesis
First-Line Setting (Primary Treatment)
3.4. Recurrent Setting
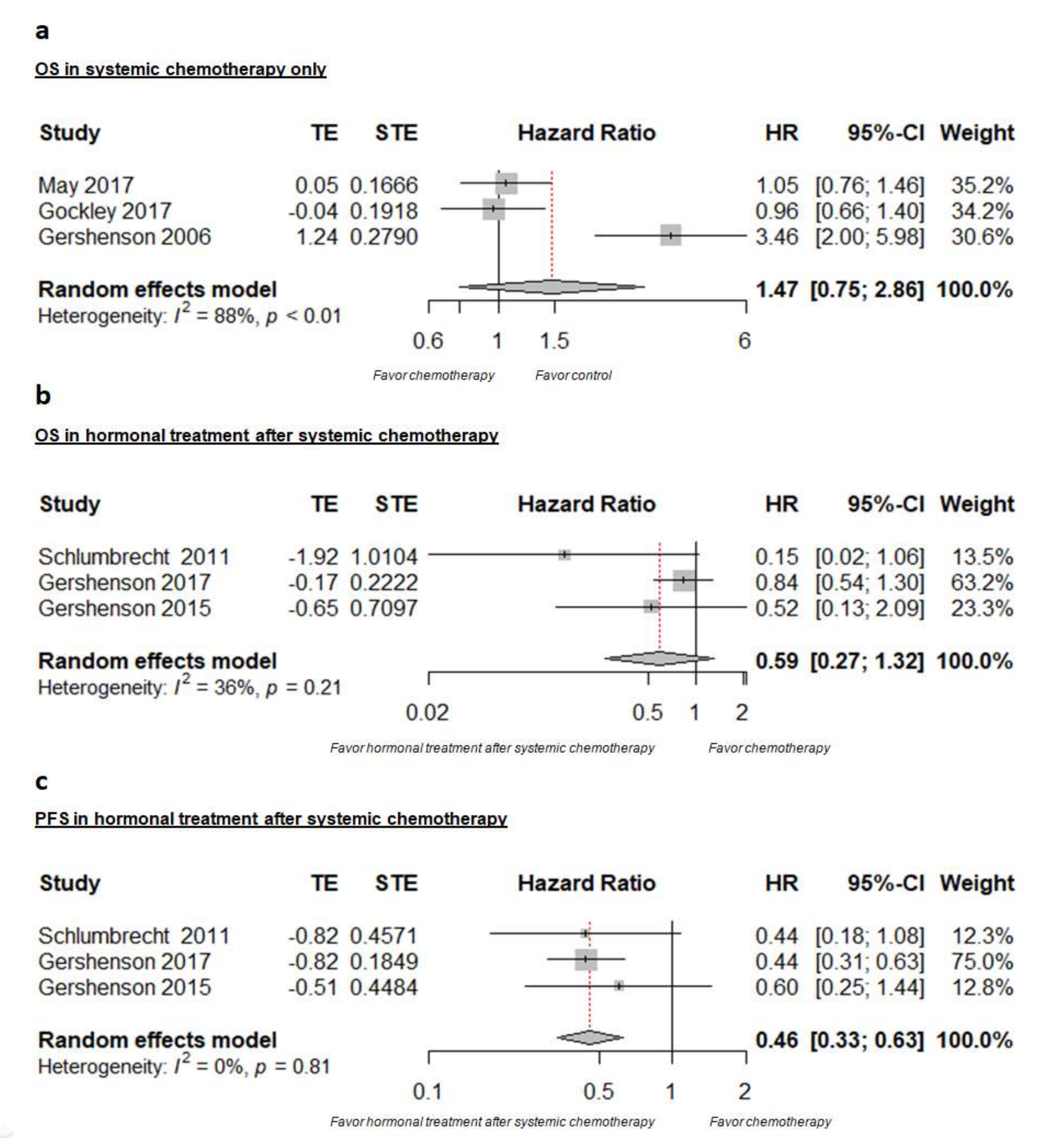
3.5. Quantitative Synthesis
3.6. Quality Assessments
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Malpica, A.; Deavers, M.T.; Lu, K.; Bodurka, D.; Atkinson, E.N.; Gershenson, D.M.; Silva, E.G. Grading Ovarian Serous Carcinoma Using a Two-Tier System. Am. J. Surg. Pathol. 2004, 28, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Gadducci, A.; Cosio, S. Therapeutic Approach to Low-Grade Serous Ovarian Carcinoma: State of Art and Perspectives of Clinical Research. Cancers 2020, 12, 1336. [Google Scholar] [CrossRef] [PubMed]
- Bogani, G.; Maggiore, U.L.R.; Paolini, B.; Diito, A.; Martinelli, F.; Lorusso, D.; Raspagliesi, F. The detrimental effect of adopting interval debulking surgery in advanced stage low-grade serous ovarian cancer. J. Gynecol. Oncol. 2019, 30, e4. [Google Scholar] [CrossRef] [PubMed]
- Cobb, L.P.; Sun, C.C.; Iyer, R.; Nick, A.M.; Fleming, N.D.; Westin, S.N.; Sood, A.K.; Wong, K.K.; Silva, E.G.; Gershenson, D.M. The role of neoadjuvant chemotherapy in the management of low-grade serous carcinoma of the ovary and peritoneum: Further evidence of relative chemoresistance. Gynecol. Oncol. 2020, 158, 653–658. [Google Scholar] [CrossRef]
- Crane, E.K.; Sun, C.C.; Ramirez, P.T.; Schmeler, K.M.; Malpica, A.; Gershenson, D.M. The role of secondary cytoreduction in low-grade serous ovarian cancer or peritoneal cancer. Gynecol. Oncol. 2014, 136, 25–29. [Google Scholar] [CrossRef] [Green Version]
- Gershenson, D.M.; Sun, C.C.; Bodurka, D.; Coleman, R.L.; Lu, K.H.; Sood, A.K.; Deavers, M.; Malpica, A.L.; Kavanagh, J.J. Recurrent low-grade serous ovarian carcinoma is relatively chemoresistant. Gynecol. Oncol. 2009, 114, 48–52. [Google Scholar] [CrossRef]
- Armstrong, D.K.; Alvarez, R.D.; Bakkum-Gamez, J.N.; Barroilhet, L.; Behbakht, K.; Berchuck, A.; Chen, L.M.; Cristea, M.; DeRosa, M.; Eisenhauer, E.L.; et al. Ovarian Cancer, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2021, 19, 191–226. [Google Scholar] [CrossRef]
- Colombo, N.; Sessa, C.; Du Bois, A.; Ledermann, J.; McCluggage, W.G.; McNeish, I.; Morice, P.; Pignata, S.; Ray-Coquard, I.; Vergote, I.; et al. ESMO–ESGO consensus conference recommendations on ovarian cancer: Pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease. Ann. Oncol. 2019, 30, 672–705. [Google Scholar] [CrossRef] [Green Version]
- Study Quality Assessment Tools|NHLBI, NIH. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 9 October 2021).
- Tang, M.; O’Connell, R.L.; Amant, F.; Beale, P.; McNally, O.; Sjoquist, K.M.; Grant, P.; Davis, A.; Sykes, P.; Mileshkin, L.; et al. PARAGON: A Phase II study of anastrozole in patients with estrogen receptor-positive recurrent/metastatic low-grade ovarian cancers and serous borderline ovarian tumors. Gynecol. Oncol. 2019, 154, 531–538. [Google Scholar] [CrossRef]
- Gershenson, D.M.; Bodurka, D.; Coleman, R.L.; Lu, K.H.; Malpica, A.; Sun, C.C. Hormonal Maintenance Therapy for Women With Low-Grade Serous Cancer of the Ovary or Peritoneum. J. Clin. Oncol. 2017, 35, 1103–1111. [Google Scholar] [CrossRef]
- Gershenson, D.M.; Bodurka, D.C.; Lu, K.H.; Nathan, L.C.; Milojevic, L.; Wong, K.K.; Malpica, A.; Sun, C.C. Impact of Age and Primary Disease Site on Outcome in Women With Low-Grade Serous Carcinoma of the Ovary or Peritoneum: Results of a Large Single-Institution Registry of a Rare Tumor. J. Clin. Oncol. 2015, 33, 2675–2682. [Google Scholar] [CrossRef] [Green Version]
- May, T.; Lheureux, S.; Bernardini, M.; Jiang, H.; Tone, A. Clinical behavior of low grade serous ovarian carcinoma: Ananalysis of 714 patients from the Ovarian Cancer Association Consortium (OCAC). Gynecol. Oncol. 2017, 145, 14. [Google Scholar] [CrossRef]
- Gockley, A.; Melamed, A.; Bregar, A.J.; Clemmer, J.T.; Birrer, M.; Schorge, J.O.; Del Carmen, M.G.; Rauh-Hain, J.A. Outcomes of Women With High-Grade and Low-Grade Advanced-Stage Serous Epithelial Ovarian Cancer. Obstet. Gynecol. 2017, 129, 439–447. [Google Scholar] [CrossRef] [Green Version]
- Schlumbrecht, M.P.; Sun, C.C.; Wong, K.N.; Broaddus, R.R.; Gershenson, D.M.; Bodurka, D.C. Clinicodemographic factors influencing outcomes in patients with low-grade serous ovarian carcinoma. Cancer 2011, 117, 3741–3749. [Google Scholar] [CrossRef] [Green Version]
- Grabowski, J.P.; Harter, P.; Heitz, F.; Pujade-Lauraine, E.; Reuss, A.; Kristensen, G.; Ray-Coquard, I.; Heitz, J.; Traut, A.; Pfisterer, J.; et al. Operability and chemotherapy responsiveness in advanced low-grade serous ovarian cancer. An analysis of the AGO Study Group metadatabase. Gynecol. Oncol. 2016, 140, 457–462. [Google Scholar] [CrossRef]
- Gershenson, D.M.; Sun, C.C.; Lu, K.H.; Coleman, R.L.; Sood, A.K.; Malpica, A.; Deavers, M.T.; Silva, E.G.; Bodurka, D.C. Clinical Behavior of Stage II-IV Low-Grade Serous Carcinoma of the Ovary. Obstet. Gynecol. 2006, 108, 361–368. [Google Scholar] [CrossRef]
- Fader, A.N.; Java, J.; Ueda, S.; Bristow, R.E.; Armstrong, D.K.; Bookman, M.A.; Gershenson, D.M.; Gynecologic Oncology Group (GOG). Survival in Women With Grade 1 Serous Ovarian Carcinoma. Obstet. Gynecol. 2013, 122, 225–232. [Google Scholar] [CrossRef] [Green Version]
- Fader, A.N.; Bergstrom, J.; Jernigan, A.; Tanner, E.J.; Roche, K.L.; Stone, R.L.; Levinson, K.L.; Ricci, S.; Wethingon, S.; Wang, T.-L.; et al. Primary cytoreductive surgery and adjuvant hormonal monotherapy in women with advanced low-grade serous ovarian carcinoma: Reducing overtreatment without compromising survival? Gynecol. Oncol. 2017, 147, 85–91. [Google Scholar] [CrossRef]
- Gershenson, D.M.; Sun, C.C.; Iyer, R.B.; Malpica, A.L.; Kavanagh, J.J.; Bodurka, D.C.; Schmeler, K.; Deavers, M. Hormonal therapy for recurrent low-grade serous carcinoma of the ovary or peritoneum. Gynecol. Oncol. 2012, 125, 661–666. [Google Scholar] [CrossRef] [Green Version]
- Zantow, E.; Chen, A.; Zhao, D.; Mashburn, S.; Underwood, H.; Subia, M.B.; Zuna, R.; Moore, K.; Holman, L. Clinical Factors Associated with Short- and Long-Term Survival in Low Grade Ovarian Carcinoma. Gynecol. Oncol. 2017, 147, 216. [Google Scholar] [CrossRef]
- Coleman, R.L.; Spirtos, N.M.; Enserro, D.; Herzog, T.J.; Sabbatini, P.; Armstrong, D.K.; Kim, J.-W.; Park, S.-Y.; Kim, B.-G.; Nam, J.-H.; et al. Secondary Surgical Cytoreduction for Recurrent Ovarian Cancer. N. Engl. J. Med. 2019, 381, 1929–1939. [Google Scholar] [CrossRef]
- Harter, P.; Sehouli, J.; Vergote, I.; Ferron, G.; Reuss, A.; Meier, W.; Greggi, S.; Mosgaard, B.J.; Selle, F.; Guyon, F.; et al. Randomized Trial of Cytoreductive Surgery for Relapsed Ovarian Cancer. N. Engl. J. Med. 2021, 385, 2123–2131. [Google Scholar] [CrossRef]
- Tropé, C.; Marth, C.; Kaern, J. Tamoxifen in the treatment of recurrent ovarian carcinoma. Eur. J. Cancer 2000, 36, 59–61. [Google Scholar] [CrossRef]
- Langdon, S.P.; Gourley, C.; Gabra, H.; Stanley, B. Endocrine therapy in epithelial ovarian cancer. Expert Rev. Anticancer Ther. 2016, 17, 109–117. [Google Scholar] [CrossRef]
- Alavi, S.; Harter, P.; Richter, R.; Keller, M.; Oskay Özcelik, G.; Mustea, A.; Schmalfeldt, B.; Wimberger, P.; Trillsch, F.; Mahner, S.; et al. Monitor VII: Treatment Strategies of Low Grade Ovarian Carcinomas—A German Survey Of The Charité—Berlin and Kliniken Essen Mitte with Support of the Study Groups Noggo and Ago. Ann. Oncol. 2018, 29, VIII355. [Google Scholar] [CrossRef]
- Hsu, C.-Y.; Bristow, R.; Cha, M.S.; Wang, B.G.; Ho, C.-L.; Kurman, R.J.; Wang, T.-L.; Shih, I.-M. Characterization of Active Mitogen-Activated Protein Kinase in Ovarian Serous Carcinomas. Clin. Cancer Res. 2004, 10, 6432–6436. [Google Scholar] [CrossRef] [Green Version]
- Farley, J.; Brady, W.; Vathipadiekal, V.; A Lankes, H.; Coleman, R.; Morgan, M.; Mannel, R.; Yamada, S.D.; Mutch, D.; Rodgers, W.H.; et al. Selumetinib in women with recurrent low-grade serous carcinoma of the ovary or peritoneum: An open-label, single-arm, phase 2 study. Lancet Oncol. 2012, 14, 134–140. [Google Scholar] [CrossRef] [Green Version]
- Gershenson, D.M.; Miller, A.; E Brady, W.; Paul, J.; Carty, K.; Rodgers, W.; Millan, D.; Coleman, R.L.; Moore, K.N.; Banerjee, S.; et al. Trametinib versus standard of care in patients with recurrent low-grade serous ovarian cancer (GOG 281/LOGS): An international, randomised, open-label, multicentre, phase 2/3 trial. Lancet 2022, 399, 541–553. [Google Scholar] [CrossRef]
- Monk, B.J.; Grisham, R.N.; Banerjee, S.; Kalbacher, E.; Mirza, M.R.; Romero, I.; Vuylsteke, P.; Coleman, R.L.; Hilpert, F.; Oza, A.M.; et al. MILO/ENGOT-ov11: Binimetinib Versus Physician’s Choice Chemotherapy in Recurrent or Persistent Low-Grade Serous Carcinomas of the Ovary, Fallopian Tube, or Primary Peritoneum. J. Clin. Oncol. 2020, 38, 3753–3762. [Google Scholar] [CrossRef]
- Gershenson, D.M.; Gourley, C.; Paul, J. MEK Inhibitors for the Treatment of Low-Grade Serous Ovarian Cancer: Expanding Therapeutic Options for a Rare Ovarian Cancer Subtype. J. Clin. Oncol. 2020, 38, 3731–3734. [Google Scholar] [CrossRef]
- Letrozole with or without Paclitaxel and Carboplatin in Treating Patients with Stage II-IV Ovarian, Fallopian Tube, or Primary Peritoneal Cancer. NRG-GY019 Trial. Available online: https://clinicaltrials.gov/ct2/show/NCT04095364 (accessed on 9 October 2021).
| Study (Year) | Design | Setting | Arms | Follow-up (Months) | Patients (n) | Population | Age (Years) | Histology |
|---|---|---|---|---|---|---|---|---|
| May (2017) [13] | Retrospective | multicenter | adjuvant chemo vs no adjuvant chemo | Median 58.8 | 439 | Stage I–IV with PCRS | Median 54 | LGSOC |
| Gockley (2017) [14] | Retrospective | National Cancer Database | adjuvant chemo vs no adjuvant chemo | Median 72.9 | 280 | Stage IIIc–IV with PCRS | Mean 53.6 | LGSOC |
| Schlumbrecht (2011) [15] | Retrospective | Single Cancer Center (MDACC) | adjuvant chemo + hormonal therapy vs adjuvant chemo only | Median 60.9 | 194 | Newly diagnosed PCRS | Mean 44.9 | LGSOC |
| Gershenson (2017) [11] | Retrospective and prospective | Single Cancer Center (MDACC) | adjuvant chemo + hormonal therapy vs adjuvant chemo only | Median 70.8 | 203 | Stage II–IV with PCRS | Median 47.5 | LGSOC LGSPC |
| Gershenson (2015) [12] | Retrospective and prospective | Single Cancer Center (MDACC) | adjuvant chemo + hormonal therapy vs adjuvant chemo only | Median 72.5 | 287 | Stage I–IV with PCRS | Median 46.1 | LGSOC GSPC |
| Grabowski (2016) [16] | Retrospective | AGO Database of 4 RT | Adjuvant chemo | --- | 145 | Stage IIIb–IV with CCRS | Median 48 | LGSOC |
| Gershenson (2006) [17] | Retrospective | Single Cancer Center (MDACC) | Adjuvant chemo | Mean 71 | 112 | Stage II–IV with PCRS | Median 43 | LGSOC |
| Fader (2013) [18] | Retrospective | multicenter | Adjuvant chemo | Median 47.1 | 47 | stage III–IV with MRCRS | Median 56.5 | LGSOC |
| Fader (2017) [19] | Retrospective | multicenter | Adjuvant hormonal therapy | Median 41 | 27 | Stage II–IV with PCRS | Median 47.5 | LGSOC |
| Study (Year) | Design | Setting | Arms | Follow-up (Months) | Patients (n) | Population | Age (Years) | Histology |
|---|---|---|---|---|---|---|---|---|
| Tang (2019) [10] | Phase II trial | Multicenter | Only HT (anastrozole) | Mean 31.1 | 36 | Recurrent LGSOC | Mean 57 | LGSOC |
| Gershenson (2012) [20] | Retrospective | Single Cancer Center | Only HT | - | 64 | Recurrent LGSOC and LGSPC | Median 49.4 | LGSOC LGSPC |
| Gershenson (2009) [6] | Retrospective | Single Cancer Center | Only chemo | - | 58 | Recurrent LGSOC | Median 43.2 | LGSOC |
| Study, Date | Control Arm | Intervention Arm | Primary Endpoint | Median PFS (Mo) | HR | 95%CI | Median OS (Mo) | HR | 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| PRIMARY | |||||||||
| May 2017 [13] | no AC (269) | PBAC (170) | Response to ACT | - | - | - | 106.8 | 1.05 | 0.76–1.46 |
| Gockley 2017 [14] | no AC (140) | PBAC (140) | OutcomeSurvival factors | - | - | - | 88.2 | 0.96 | 0.66–1.40 |
| Schlumbrecht 2011 [15] | ACT (170) | ACT +HC (9) | effect of demographics and treatment on survival | 76.4 | 0.44 | 0.18–1.08 | - | 0.15 | 0.02–1.06 |
| Gershenson 2017 [11] | PBACT (133) | PBACT +HMT (70) | outcome | 64.9 | 0.44 | 0.31–0.64 | 115.7 | 0.84 | 0.54–1.30 |
| Gershenson 2015 [12] | ACT (159) | ACT +HMT (50) | outcome | - | 0.92 | 0.64–1.32 | - | 1.05 | 0.64–1.73 |
| Grabowski 2016 [16] | - | PBACT (145) | efficacy of PBACT after CCRS | 92.0 | - | - | 97.0 | - | - |
| Gershenson 2006 [17] | - | PBACT (112) | Clinical Behavior Analysis | 19.5 | - | - | 81.8 | - | - |
| Fader 2013 [18] | - | PBACT (47) | Evaluation of Clinicopathological variables | 33.2 | 96.9 | ||||
| Fader 2017 [19] | - | PCRS + HT (26)NACT + PCRS + HT (1) | Outcome | - | - | - | - | - | - |
| RECURRENT DISEASE | |||||||||
| Tang 2019 [10] | - | Anastrozole | Clinical Benefit Rates | 11.1 | - | 3.2–11.9 | - | - | - |
| Gershenson 2012 [20] | - | HT | Efficacy of HT | - | - | - | 78.2 | - | - |
| Gershenson 2009 [6] | - | Chemotherapy | Evaluate chemoresistance of recurrent LGSOC | - | - | - | 87.1 | - | 56.8–117.3 |
| Study, Year | Criteria | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
| Primary Treatment | ||||||||||||||
| May, 2017 [13] | NA | NA | NA | NA | NA | |||||||||
| Gockley, 2017 [14] | NA | NA | NA | NA | NA | |||||||||
| Schlumbrecht, 2011 [15] | NA | NA | NA | NA | NA | |||||||||
| Gershenson, 2017 [11] | NA | NA | NA | NA | NA | |||||||||
| Gershenson, 2015 [12] | NA | NA | NA | NA | NA | |||||||||
| Grabowski, 2016 [16] | NA | NA | NA | NA | NA | |||||||||
| Gershenson, 2006 [17] | NA | NA | NA | NA | NA | |||||||||
| Fader, 2013 [18] | NA | NA | NA | NA | NA | |||||||||
| Fader, 2017 [19] | NA | NA | NA | NA | NA | |||||||||
| Recurrence Treatment | ||||||||||||||
| Tang, 2019 [10] | NA | NA | NA | NA | NA | |||||||||
| Gershenson, 2012 [20] | NA | NA | NA | NA | NA | |||||||||
| Gershenson, 2009 [6] | NA | NA | NA | NA | NA | |||||||||
 , no:
, no:  .
.Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montero-Macías, R.; Rigolet, P.; Mikhael, E.; Krell, J.; Villefranque, V.; Lecuru, F.; Fotopoulou, C. Traditional Systemic Treatment Options in Advanced Low-Grade Serous Ovarian Cancer after Successful Cytoreduction: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 3681. https://doi.org/10.3390/cancers14153681
Montero-Macías R, Rigolet P, Mikhael E, Krell J, Villefranque V, Lecuru F, Fotopoulou C. Traditional Systemic Treatment Options in Advanced Low-Grade Serous Ovarian Cancer after Successful Cytoreduction: A Systematic Review and Meta-Analysis. Cancers. 2022; 14(15):3681. https://doi.org/10.3390/cancers14153681
Chicago/Turabian StyleMontero-Macías, Rosa, Pascal Rigolet, Elie Mikhael, Jonathan Krell, Vincent Villefranque, Fabrice Lecuru, and Christina Fotopoulou. 2022. "Traditional Systemic Treatment Options in Advanced Low-Grade Serous Ovarian Cancer after Successful Cytoreduction: A Systematic Review and Meta-Analysis" Cancers 14, no. 15: 3681. https://doi.org/10.3390/cancers14153681
APA StyleMontero-Macías, R., Rigolet, P., Mikhael, E., Krell, J., Villefranque, V., Lecuru, F., & Fotopoulou, C. (2022). Traditional Systemic Treatment Options in Advanced Low-Grade Serous Ovarian Cancer after Successful Cytoreduction: A Systematic Review and Meta-Analysis. Cancers, 14(15), 3681. https://doi.org/10.3390/cancers14153681






