Prognostic Impact of Neutropenia in Cancer Patients with Septic Shock: A 2009–2017 Nationwide Cohort Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Study Patients and Data Definitions
2.3. Statistical Analysis
3. Results
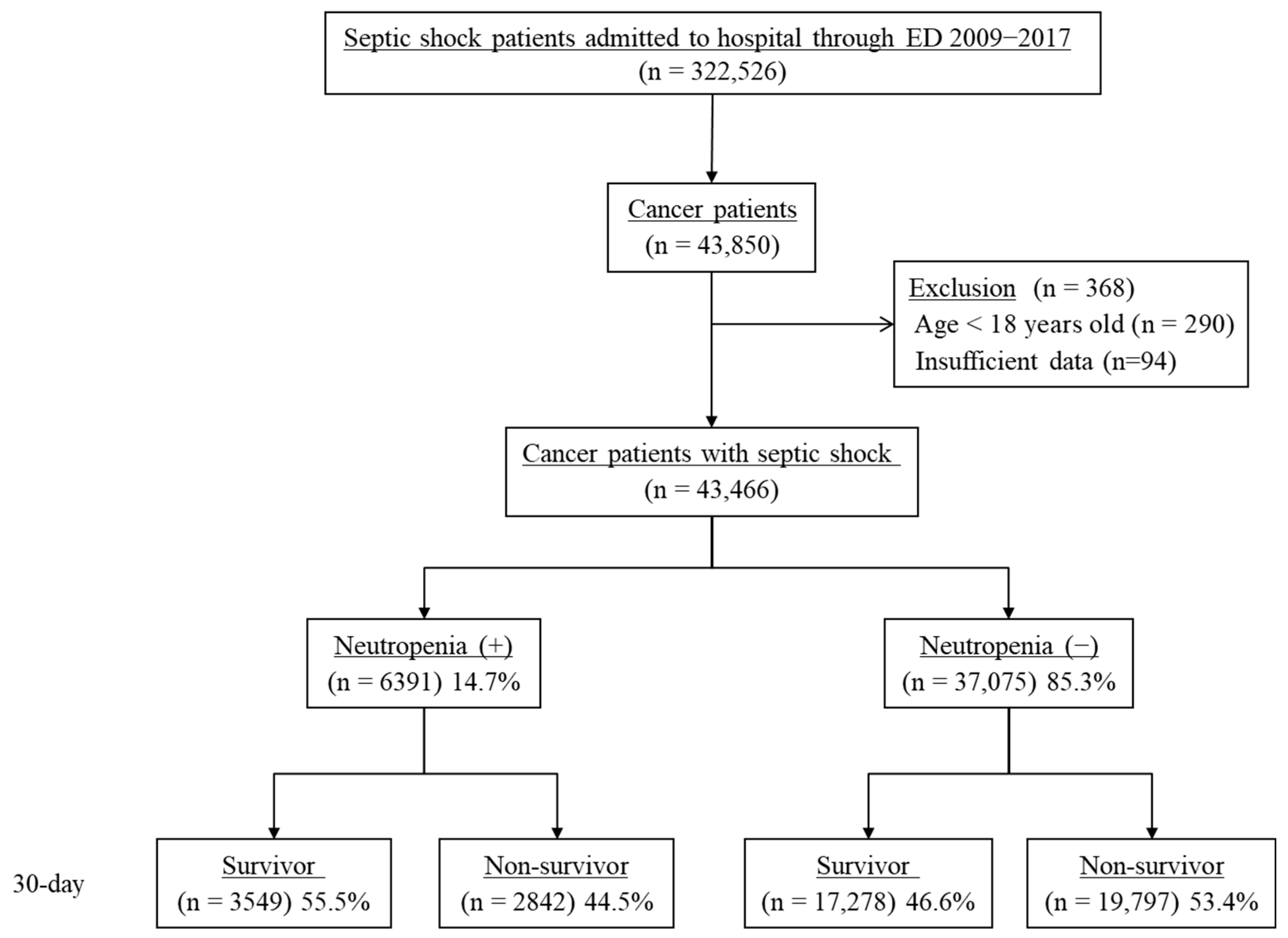
3.1. Study Population
3.2. Baseline and Clinical Characteristics of the Study Population
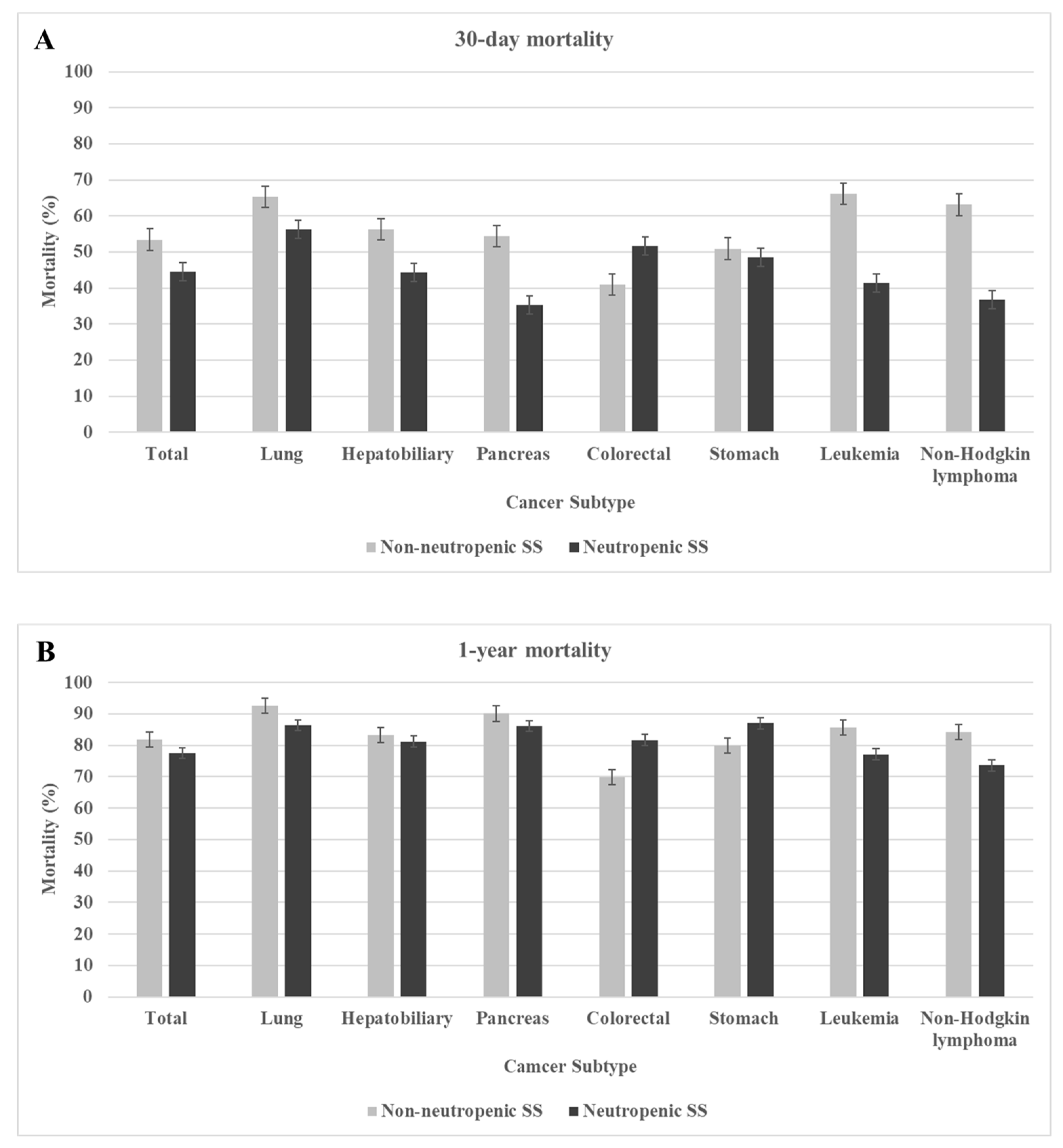
3.3. Mortality Rate of Septic Shock According to Cancer Subtype and Prevalence Rate of Neutropenic Septic Shock According to Chemotherapy Status
3.4. Factors Associated with 30-Day and 1-Year Mortality in Septic Shock Survivors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Azoulay, E.; Mokart, D.; Pène, F.; Lambert, J.; Kouatchet, A.; Mayaux, J.; Vincent, F.; Nyunga, M.; Bruneel, F.; Laisne, L.M.; et al. Outcomes of critically ill patients with hematologic malignancies: Prospective multicenter data from France and Belgium—a groupe de recherche respiratoire en réanimation onco-hématologique study. J. Clin. Oncol. 2013, 31, 2810–2818. [Google Scholar] [CrossRef]
- Soares, M.; Bozza, F.A.; Azevedo, L.C.; Silva, U.V.; Corrêa, T.D.; Colombari, F.; Torelly, A.P.; Varaschin, P.; Viana, W.N.; Knibel, M.F.; et al. Effects of Organizational Characteristics on Outcomes and Resource Use in Patients with Cancer Admitted to Intensive Care Units. J. Clin. Oncol. 2016, 34, 3315–3324. [Google Scholar] [CrossRef] [PubMed]
- Georges, Q.; Azoulay, E.; Mokart, D.; Soares, M.; Jeon, K.; Oeyen, S.; Rhee, C.K.; Gruber, P.; Ostermann, M.; Hill, Q.A.; et al. Influence of neutropenia on mortality of critically ill cancer patients: Results of a meta-analysis on individual data. Crit. Care 2018, 22, 326. [Google Scholar] [CrossRef] [PubMed]
- Azoulay, E.; Pène, F.; Darmon, M.; Lengliné, E.; Benoit, D.; Soares, M.; Vincent, F.; Bruneel, F.; Perez, P.; Lemiale, V.; et al. Managing critically Ill hematology patients: Time to think differently. Blood Rev. 2015, 29, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Mokart, D.; Pastores, S.M.; Darmon, M. Has survival increased in cancer patients admitted to the ICU? Yes. Intensive Care Med. 2014, 40, 1570–1572. [Google Scholar] [CrossRef] [PubMed]
- de Montmollin, E.; Tandjaoui-Lambiotte, Y.; Legrand, M.; Lambert, J.; Mokart, D.; Kouatchet, A.; Lemiale, V.; Pène, F.; Bruneel, F.; Vincent, F.; et al. Outcomes in critically ill cancer patients with septic shock of pulmonary origin. Shock 2013, 39, 250–254. [Google Scholar] [CrossRef]
- Mokart, D.; Lambert, J.; Schnell, D.; Fouché, L.; Rabbat, A.; Kouatchet, A.; Lemiale, V.; Vincent, F.; Lengliné, E.; Bruneel, F.; et al. Delayed intensive care unit admission is associated with increased mortality in patients with cancer with acute respiratory failure. Leuk. Lymphoma 2013, 54, 1724–1729. [Google Scholar] [CrossRef]
- Bouteloup, M.; Perinel, S.; Bourmaud, A.; Azoulay, E.; Mokart, D.; Darmon, M. Outcomes in adult critically ill cancer patients with and without neutropenia: A systematic review and meta-analysis of the Groupe de Recherche en Réanimation Respiratoire du patient d’Onco-Hématologie (GRRR-OH). Oncotarget 2017, 8, 1860–1870. [Google Scholar] [CrossRef]
- Kochanek, M.; Schalk, E.; von Bergwelt-Baildon, M.; Beutel, G.; Buchheidt, D.; Hentrich, M.; Henze, L.; Kiehl, M.; Liebregts, T.; von Lilienfeld-Toal, M.; et al. Management of sepsis in neutropenic cancer patients: 2018 guidelines from the Infectious Diseases Working Party (AGIHO) and Intensive Care Working Party (iCHOP) of the German Society of Hematology and Medical Oncology (DGHO). Ann. Hematol. 2019, 98, 1051–1069. [Google Scholar] [CrossRef]
- Cheol Seong, S.; Kim, Y.Y.; Khang, Y.H.; Heon Park, J.; Kang, H.J.; Lee, H.; Do, C.H.; Song, J.S.; Hyon Bang, J.; Ha, S.; et al. Data Resource Profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 2017, 46, 799–800. [Google Scholar] [CrossRef]
- Kim, J.A.; Yoon, S.; Kim, L.Y.; Kim, D.S. Towards Actualizing the Value Potential of Korea Health Insurance Review and Assessment (HIRA) Data as a Resource for Health Research: Strengths, Limitations, Applications, and Strategies for Optimal Use of HIRA Data. J. Korean Med. Sci. 2017, 32, 718–728. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.; Murphy, M.V.; Li, L.; Platt, R.; Klompas, M. Comparison of trends in sepsis incidence and coding using administrative claims versus objective clinical data. Clin. Infect. Dis. 2015, 60, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Seo, H.J.; Oh, I.H.; Yoon, S.J. A comparison of the cancer incidence rates between the national cancer registry and insurance claims data in Korea. Asian Pac. J. Cancer Prev. 2012, 13, 6163–6168. [Google Scholar] [CrossRef]
- Hong, S.; Won, Y.J.; Park, Y.R.; Jung, K.W.; Kong, H.J.; Lee, E.S. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2017. Cancer Res. Treat. 2020, 52, 335–350. [Google Scholar] [CrossRef]
- Kim, Y.-J.; Kim, M.-J.; Kim, Y.-J.; Kim, W.Y. Short and Long-Term Mortality Trends for Cancer Patients with Septic Shock Stratified by Cancer Type from 2009 to 2017: A Population-Based Cohort Study. Cancers 2021, 13, 657. [Google Scholar] [CrossRef]
- Li, Y.; Guo, J.; Yang, H.; Li, H.; Shen, Y.; Zhang, D. Comparison of culture-negative and culture-positive sepsis or septic shock: A systematic review and meta-analysis. Crit. Care 2021, 25, 167. [Google Scholar] [CrossRef] [PubMed]
- Kadri, S.S.; Rhee, C.; Strich, J.R.; Morales, M.K.; Hohmann, S.; Menchaca, J.; Suffredini, A.F.; Danner, R.L.; Klompas, M. Estimating Ten-Year Trends in Septic Shock Incidence and Mortality in United States Academic Medical Centers Using Clinical Data. Chest 2017, 151, 278–285. [Google Scholar] [CrossRef]
- Kuderer, N.M.; Dale, D.C.; Crawford, J.; Cosler, L.E.; Lyman, G.H. Mortality, morbidity, and cost associated with febrile neutropenia in adult cancer patients. Cancer 2006, 106, 2258–2266. [Google Scholar] [CrossRef]
- Chindaprasirt, J.; Wanitpongpun, C.; Limpawattana, P.; Thepsuthammarat, K.; Sripakdee, W.; Sookprasert, A.; Wirasorn, K. Mortality, length of stay, and cost associated with hospitalized adult cancer patients with febrile neutropenia. Asian Pac. J. Cancer Prev. 2013, 14, 1115–1119. [Google Scholar] [CrossRef]
- Kozma, C.M.; Dickson, M.; Chia, V.; Legg, J.; Barron, R. Trends in neutropenia-related inpatient events. J. Oncol. Pract. 2012, 8, 149–155. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lingaratnam, S.; Thursky, K.A.; Slavin, M.A.; Kirsa, S.W.; Bennett, C.A.; Worth, L.J. The disease and economic burden of neutropenic fever in adult patients in Australian cancer treatment centres 2008: Analysis of the Victorian Admitted Episodes Dataset. J. Intern. Med. 2011, 41, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Weycker, D.; Sofrygin, O.; Seefeld, K.; Deeter, R.G.; Legg, J.; Edelsberg, J. Technical evaluation of methods for identifying chemotherapy-induced febrile neutropenia in healthcare claims databases. BMC Health Serv. Res. 2013, 13, 60. [Google Scholar] [CrossRef]
- Kim, D.; Lee, S.; Youk, T.; Hong, S. Incidence and Clinical Outcomes of Febrile Neutropenia in Adult Cancer Patients with Chemotherapy Using Korean Nationwide Health Insurance Database. Yonsei Med. J. 2021, 62, 479–486. [Google Scholar] [CrossRef]
- Maschmeyer, G.; Beinert, T.; Buchheidt, D.; Cornely, O.A.; Einsele, H.; Heinz, W.; Heussel, C.P.; Kahl, C.; Kiehl, M.; Lorenz, J.; et al. Diagnosis and antimicrobial therapy of lung infiltrates in febrile neutropenic patients: Guidelines of the infectious diseases working party of the German Society of Haematology and Oncology. Eur. J. Cancer 2009, 45, 2462–2472. [Google Scholar] [CrossRef]
- Soares, M.; Salluh, J.I.F.; Torres, V.B.L.; Leal, J.V.R.; Spector, N. Short- and long-term outcomes of critically ill patients with cancer and prolonged ICU length of stay. Chest 2008, 134, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.S.; Suh, G.Y.; Ryu, J.A.; Chung, C.R.; Yang, J.H.; Park, C.M.; Jeon, K. Effect of Early Intervention on Long-Term Outcomes of Critically Ill Cancer Patients Admitted to ICUs. Crit. Care Med. 2015, 43, 1439–1448. [Google Scholar] [CrossRef] [PubMed]
- Kalil, A.C.; Opal, S.M. Sepsis in the severely immunocompromised patient. Curr. Infect. Dis. Rep. 2015, 17, 487. [Google Scholar] [CrossRef] [PubMed]
- Regazzoni, C.J.; Khoury, M.; Irrazabal, C.; Myburg, C.; Galvalisi, N.R.; O’Flaherty, M.; Sarquis, S.G.; Poderoso, J.J. Neutropenia and the development of the systemic inflammatory response syndrome. Intensive Care Med. 2003, 29, 135–138. [Google Scholar] [CrossRef]
- Talcott, J.A.; Finberg, R.; Mayer, R.J.; Goldman, L. The medical course of cancer patients with fever and neutropenia. Clinical identification of a low-risk subgroup at presentation. Arch. Intern. Med. 1988, 148, 2561–2568. [Google Scholar] [CrossRef]
- Reilly, J.P.; Anderson, B.J.; Hudock, K.M.; Dunn, T.G.; Kazi, A.; Tommasini, A.; Charles, D.; Shashaty, M.G.; Mikkelsen, M.E.; Christie, J.D.; et al. Neutropenic sepsis is associated with distinct clinical and biological characteristics: A cohort study of severe sepsis. Crit. Care 2016, 20, 222. [Google Scholar] [CrossRef] [PubMed]
- Laserna, A.; Fowler, C.; O’Connell, K.; Manjappachar, N.; Martin, P.; Cuenca, J.; Urso, C.; Gutierrez, C.; Malik, I.; Erfe, R.; et al. 1670: NEUTROPENIC SEPTIC SHOCK OUTCOMES IN CANCER PATIENTS AND THE INFLUENCE OF COLONY-STIMULATING FACTOR. Crit. Care Med. 2020, 48, 810. [Google Scholar] [CrossRef]
- Souza-Dantas, V.C.; Salluh, J.I.F.; Soares, M. Impact of neutropenia on the outcomes of critically ill patients with cancer: A matched case-control study. Ann. Oncol. 2011, 22, 2094–2100. [Google Scholar] [CrossRef]
- Lemiale, V.; Pons, S.; Mirouse, A.; Tudesq, J.J.; Hourmant, Y.; Mokart, D.; Pène, F.; Kouatchet, A.; Mayaux, J.; Nyunga, M.; et al. Sepsis and Septic Shock in Patients with Malignancies: A Groupe de Recherche Respiratoire en Réanimation Onco-Hématologique Study. Crit. Care Med. 2020, 48, 822–829. [Google Scholar] [CrossRef]
- de Vries, V.A.; Müller, M.C.A.; Arbous, M.S.; Biemond, B.J.; Blijlevens, N.M.A.; Kusadasi, N.; Span, L.R.F.; Vlaar, A.P.J.; van Westerloo, D.J.; Kluin-Nelemans, H.C.; et al. Long-Term Outcome of Patients with a Hematologic Malignancy and Multiple Organ Failure Admitted at the Intensive Care. Crit. Care Med. 2019, 47, e120–e128. [Google Scholar] [CrossRef] [PubMed]
- Vincent, F.; Soares, M.; Mokart, D.; Lemiale, V.; Bruneel, F.; Boubaya, M.; Gonzalez, F.; Cohen, Y.; Azoulay, E.; Darmon, M. In-hospital and day-120 survival of critically ill solid cancer patients after discharge of the intensive care units: Results of a retrospective multicenter study-A Groupe de recherche respiratoire en réanimation en Onco-Hématologie (Grrr-OH) study. Ann. Intensive Care 2018, 8, 40. [Google Scholar] [CrossRef]
- Hohenberger, P.; Buchheidt, D. Surgical interventions in patients with hematologic malignancies. Crit. Rev. Oncol. Hematol. 2005, 55, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Mokart, D.; Darmon, M.; Resche-Rigon, M.; Lemiale, V.; Pène, F.; Mayaux, J.; Rabbat, A.; Kouatchet, A.; Vincent, F.; Nyunga, M.; et al. Prognosis of neutropenic patients admitted to the intensive care unit. Intensive Care Med. 2015, 41, 296–303. [Google Scholar] [CrossRef]
- Theyab, A.; Algahtani, M.; Alsharif, K.F.; Hawsawi, Y.M.; Alghamdi, A.; Alghamdi, A.; Akinwale, J. New insight into the mechanism of granulocyte colony-stimulating factor (G-CSF) that induces the mobilization of neutrophils. Hematology 2021, 26, 628–636. [Google Scholar] [CrossRef]
- Klastersky, J.; de Naurois, J.; Rolston, K.; Rapoport, B.; Maschmeyer, G.; Aapro, M.; Herrstedt, J. Management of febrile neutropaenia: ESMO Clinical Practice Guidelines. Ann. Oncol. 2016, 27, v111–v118. [Google Scholar] [CrossRef]
- Smith, T.J.; Bohlke, K.; Lyman, G.H.; Carson, K.R.; Crawford, J.; Cross, S.J.; Goldberg, J.M.; Khatcheressian, J.L.; Leighl, N.B.; Perkins, C.L.; et al. Recommendations for the Use of WBC Growth Factors: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2015, 33, 3199–3212. [Google Scholar] [CrossRef] [PubMed]
- National Collaborating Centre for Cancer. National Collaborating Centre for Cancer. National Institute for Health and Care Excellence: Guidelines. In Neutropenic Sepsis: Prevention and Management of Neutropenic Sepsis in Cancer Patients; National Institute for Health and Clinical Excellence (NICE): London, UK, 2012. [Google Scholar]
- Cooper, A.J.; Keller, S.P.; Chan, C.; Glotzbecker, B.E.; Klompas, M.; Baron, R.M.; Rhee, C. Improvements in Sepsis-associated Mortality in Hospitalized Patients with Cancer versus Those without Cancer. A 12-Year Analysis Using Clinical Data. Ann. Am. Thorac. Soc. 2020, 17, 466–473. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Kang, J.; Kim, M.J.; Ryoo, S.M.; Kang, G.H.; Shin, T.G.; Park, Y.S.; Choi, S.H.; Kwon, W.Y.; Chung, S.P.; et al. Development and validation of the VitaL CLASS score to predict mortality in stage IV solid cancer patients with septic shock in the emergency department: A multi-center, prospective cohort study. BMC Med. 2020, 18, 390. [Google Scholar] [CrossRef] [PubMed]
- Azoulay, E.; Soares, M.; Darmon, M.; Benoit, D.; Pastores, S.; Afessa, B. Intensive care of the cancer patient: Recent achievements and remaining challenges. Ann. Intensive Care 2011, 1, 5. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | All Patients (n = 43,466) | Non-Neutropenic SS (n = 37,075) | Neutropenic SS (n = 6391) | p-Value |
|---|---|---|---|---|
| Age, years | 67.0 ± 12.7 | 67.8 ± 12.6 | 62.6 ± 12.9 | <0.001 |
| Sex, male | 28,067 (64.6) | 24,166 (65.2) | 3901 (61.0) | <0.001 |
| Comorbidities | ||||
| Hypertension | 23,136 (53.2) | 20,091 (54.2) | 3045 (47.7) | <0.001 |
| Diabetes mellitus | 16,977 (39.1) | 14,758 (39.8) | 2219 (34.7) | <0.001 |
| Congestive heart failure | 5745 (13.2) | 5008 (13.5) | 737 (11.5) | <0.001 |
| Chronic lung disease | 5008 (11.5) | 4301 (11.6) | 707 (11.1) | 0.213 |
| Renal failure | 2783 (6.4) | 2397 (6.5) | 386 (6.0) | 0.199 |
| Liver cirrhosis | 4974 (11.4) | 4705 (12.7) | 269 (4.2) | <0.001 |
| CCI (mean) | 6.30 ± 3.89 | 6.29 ± 3.91 | 6.36 ± 3.80 | 0.186 |
| CCI (subgroup) | ||||
| 0–2 | 7816 (18.0) | 6709 (18.1) | 1107 (17.3) | |
| 3–4 | 9652 (22.2) | 8160 (22.0) | 1492 (23.4) | |
| 5–7 | 8256 (19.0) | 7231 (19.5) | 1025 (16.0) | |
| 8+ | 17,742 (40.8) | 14,975 (40.4) | 2767 (43.3) | |
| Cancer type | <0.001 | |||
| Brain | 772 (1.8) | 736 (2.0) | 36 (0.6) | |
| Lung | 6657 (15.3) | 5646 (15.2) | 1011 (15.8) | |
| Liver | 6238 (14.4) | 6074 (16.4) | 164 (2.6) | |
| Colon | 4494 (10.3) | 4122 (11.1) | 372 (5.8) | |
| Stomach | 3684 (8.5) | 3284 (8.9) | 400 (6.3) | |
| Gall bladder | 1981 (4.6) | 1911 (5.2) | 70 (1.1) | |
| Pancreas | 1943 (4.5) | 1799 (4.9) | 144 (2.3) | |
| Leukemia | 1917 (4.4) | 1,053 (2.8) | 864 (13.5) | |
| Non-Hodgkin’s lymphoma | 1475 (3.4) | 724 (2.0) | 751 (11.8) | |
| Female reproductive system | 1249 (2.9) | 862 (2.3) | 387 (6.0) | |
| Breast | 1112 (2.6) | 752 (2.0) | 360 (5.6) | |
| Kidney/bladder | 1095 (2.5) | 1010 (2.7) | 85 (1.3) | |
| Multiple myeloma | 923 (2.1) | 635 (1.7) | 288 (4.5) | |
| Male reproductive system | 754 (1.7) | 641 (1.7) | 113 (1.8) | |
| Oropharynx | 439 (1.0) | 364 (1.0) | 75 (1.2) | |
| Esophagus | 391 (0.9) | 324 (0.9) | 67 (1.0) | |
| Thyroid | 169 (0.4) | 160 (0.4) | 9 (0.1) | |
| Larynx | 149 (0.3) | 131 (0.4) | 18 (0.3) | |
| Hodgkin lymphoma | 50 (0.1) | 28 (0.1) | 22 (0.3) | |
| Other, unspecified | 2995 (6.9) | 2564 (6.9) | 431 (6.7) | |
| Multiple | 4979 (11.5) | 4255 (11.5) | 724 (11.3) | |
| Treatment | ||||
| Radiotherapy within 30 days | 1607 (3.7) | 1272 (3.4) | 335 (5.2) | <0.001 |
| Chemotherapy within 30 days | 8310 (19.1) | 4693 (12.7) | 3617 (56.6) | <0.001 |
| Radiotherapy within 90 days | 3723 (8.6) | 3019 (8.1) | 704 (11.0) | <0.001 |
| Chemotherapy within 90 days | 13,831 (31.8) | 9425 (25.4) | 4406 (68.9) | <0.001 |
| Outcome | ||||
| 30-day mortality | 22,639 (52.1) | 19,797 (53.4) | 2842 (44.5) | <0.001 |
| 1-year mortality | 35,325 (81.3) | 30,369 (81.9) | 4956 (77.5) | <0.001 |
| Characteristics | 30-Day Mortality | 1-Year Mortality | ||||
|---|---|---|---|---|---|---|
| Adjusted HR | 95% CI | p-Value | Adjusted HR | 95% CI | p-Value | |
| Neutropenia | 0.811 | 0.779–0.844 | <0.001 | 0.861 | 0.836–0.888 | <0.001 |
| Age | 1.007 | 1.006–1.008 | <0.001 | 1.009 | 1.008–1.010 | <0.001 |
| Female sex | 0.919 | 0.894–0.945 | <0.001 | 0.919 | 0.899–0.939 | <0.001 |
| CCI | ||||||
| 0–2 | Reference | Reference | ||||
| 3–4 | 1.356 | 1.296–1.419 | <0.001 | 1.312 | 1.267–1.359 | <0.001 |
| 5–7 | 1.431 | 1.366–1.499 | <0.001 | 1.405 | 1.355–1.456 | <0.001 |
| 8+ | 1.840 | 1.767–1.915 | <0.001 | 1.862 | 1.805–1.921 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-M.; Kim, Y.-J.; Kim, Y.-J.; Kim, W.-Y. Prognostic Impact of Neutropenia in Cancer Patients with Septic Shock: A 2009–2017 Nationwide Cohort Study. Cancers 2022, 14, 3601. https://doi.org/10.3390/cancers14153601
Kim S-M, Kim Y-J, Kim Y-J, Kim W-Y. Prognostic Impact of Neutropenia in Cancer Patients with Septic Shock: A 2009–2017 Nationwide Cohort Study. Cancers. 2022; 14(15):3601. https://doi.org/10.3390/cancers14153601
Chicago/Turabian StyleKim, Sang-Min, Youn-Jung Kim, Ye-Jee Kim, and Won-Young Kim. 2022. "Prognostic Impact of Neutropenia in Cancer Patients with Septic Shock: A 2009–2017 Nationwide Cohort Study" Cancers 14, no. 15: 3601. https://doi.org/10.3390/cancers14153601
APA StyleKim, S.-M., Kim, Y.-J., Kim, Y.-J., & Kim, W.-Y. (2022). Prognostic Impact of Neutropenia in Cancer Patients with Septic Shock: A 2009–2017 Nationwide Cohort Study. Cancers, 14(15), 3601. https://doi.org/10.3390/cancers14153601






