Signature and Prediction of Perigastric Lymph Node Metastasis in Patients with Gastric Cancer and Total Gastrectomy: Is Total Gastrectomy Always Necessary?
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Eligibility Criteria
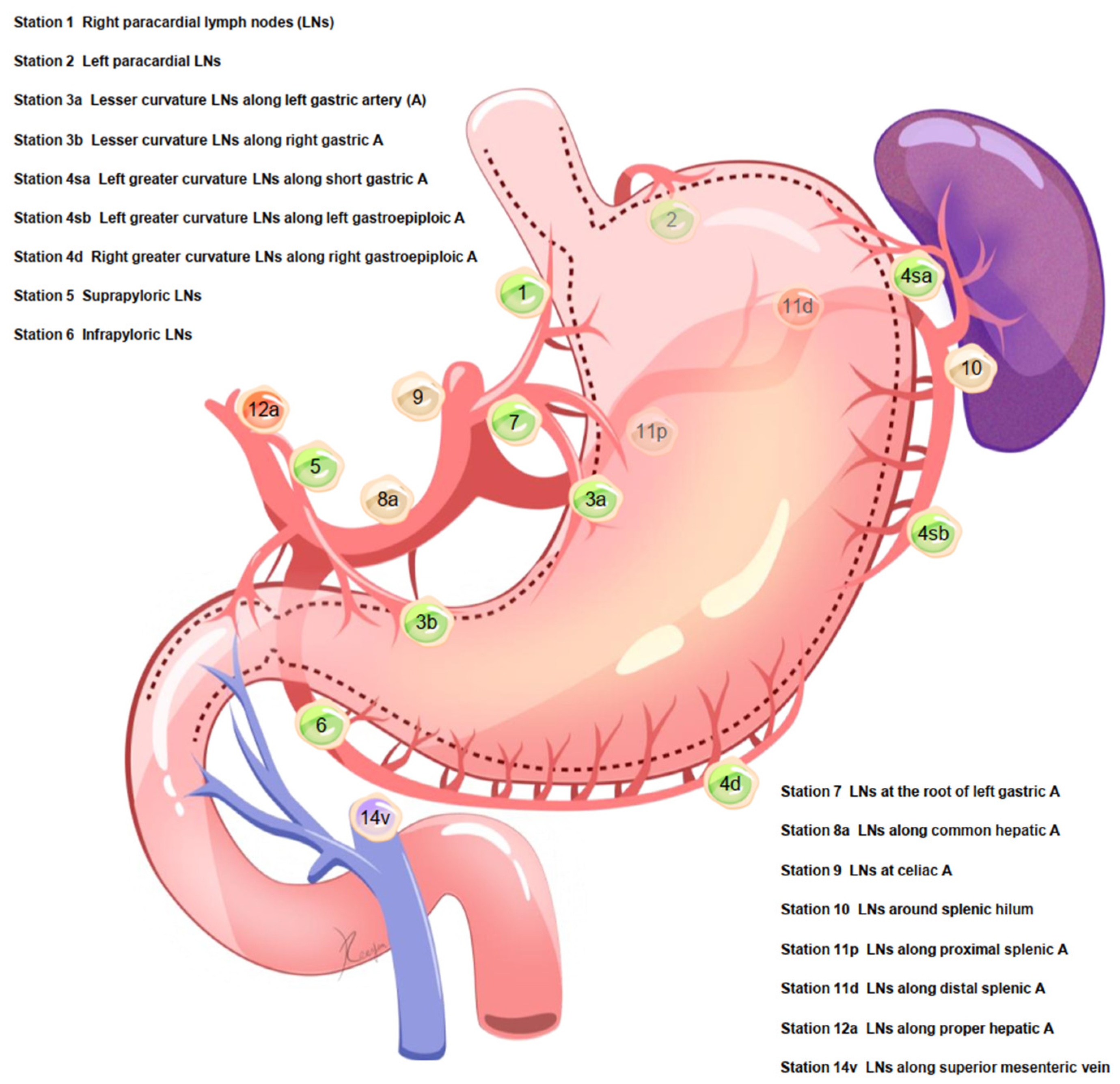
2.2. Lymph Node Dissection for Total Gastrectomy
2.3. Clinical and Pathological Factors
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Tumor Location May Determine pLNM Risk
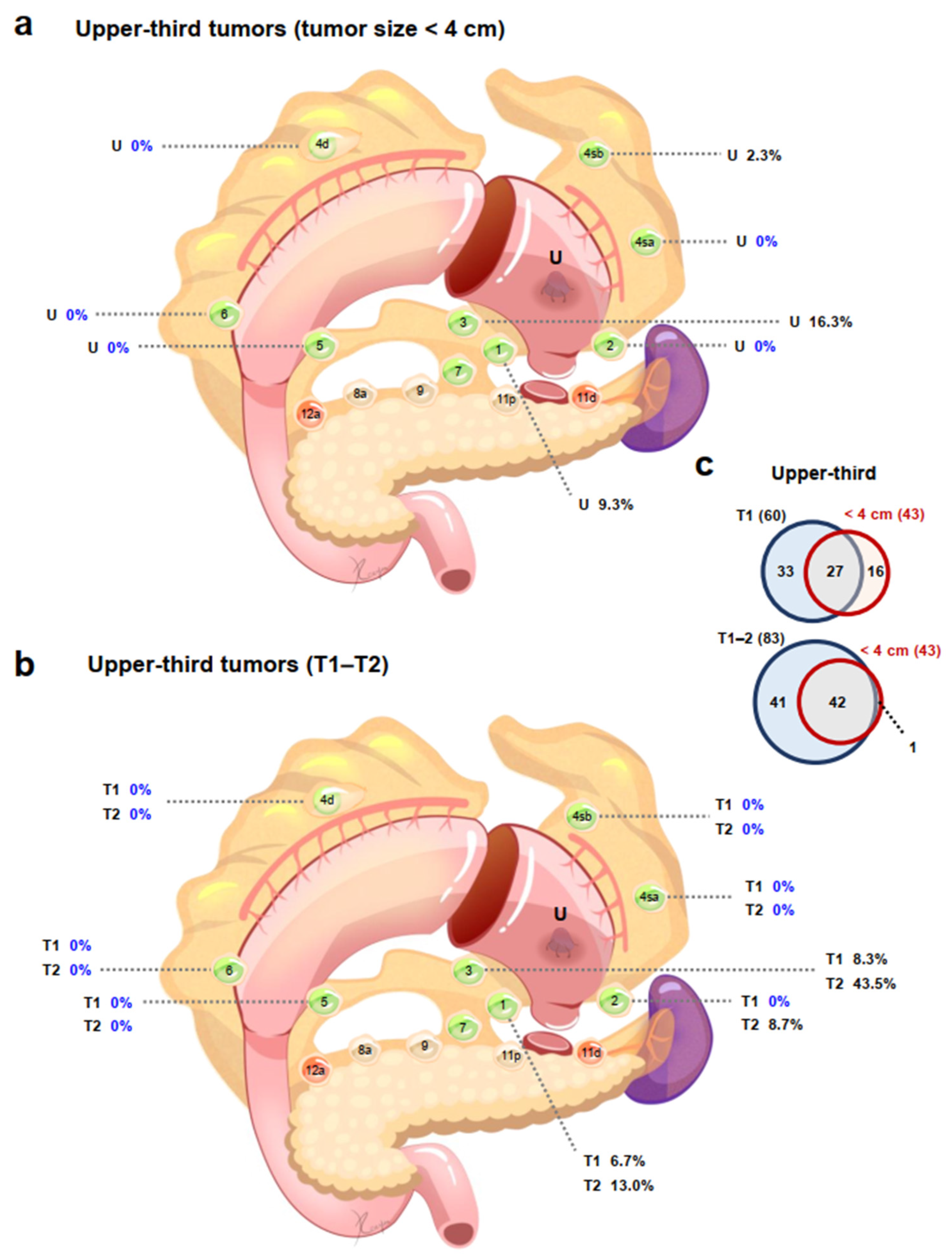
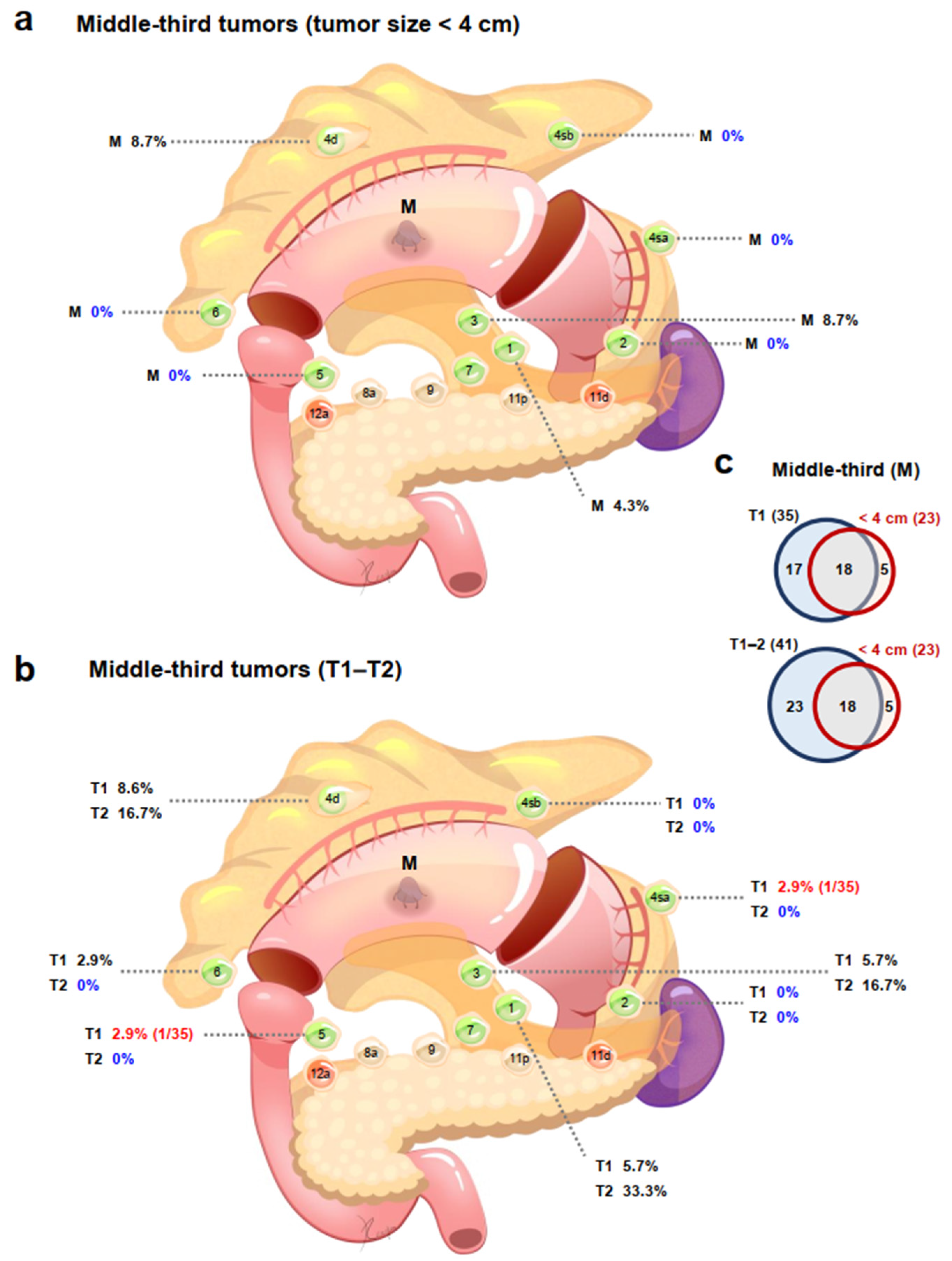
3.3. Tumor Location Combined with Tumor Size May Determine pLNM Risk
3.4. Tumor Location Combined with T Stage May Determine pLNM Risk
3.5. Identification of Independent Predictive Factors and Models of pLNMs
3.6. Models for pLNM Showed Good Predictive Performance
3.7. Indications for Proximal Gastrectomy Could Be Expanded
3.8. Indications for PPG May Need Reevaluating
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rizzo, A.; Mollica, V.; Ricci, A.D.; Maggio, I.; Massucci, M.; Rojas Limpe, F.L.; Fabio, F.D.; Ardizzoni, A. Third- and later-line treatment in advanced or metastatic gastric cancer: A systematic review and meta-analysis. Future Oncol. 2020, 16, 4409–4418. [Google Scholar] [CrossRef] [PubMed]
- Ricci, A.D.; Rizzo, A.; Rojas Llimpe, F.L.; Di Fabio, F.; De Biase, D.; Rihawi, K. Novel HER2-Directed Treatments in Advanced Gastric Carcinoma: AnotHER Paradigm Shift? Cancers 2021, 13, 1664. [Google Scholar] [CrossRef]
- Rihawi, K.; Ricci, A.D.; Rizzo, A.; Brocchi, S.; Marasco, G.; Pastore, L.V.; Llimpe, F.L.R.; Golfieri, R.; Renzulli, M. Tumor-Associated Macrophages and Inflammatory Microenvironment in Gastric Cancer: Novel Translational Implications. Int. J. Mol. Sci. 2021, 22, 3805. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.D.; Yamashita, H.; Seto, Y. Gastric cancer surgery: Historical background and perspective in Western countries versus Japan. Ann. Transl. Med. 2019, 7, 493. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Jiang, Y.; Chen, C.; Zheng, H.; Huang, W.; Xu, B.; Tang, W.; Yuan, Q.; Zhou, K.; Liang, X.; et al. Radiomics signature based on computed tomography images for the preoperative prediction of lymph node metastasis at individual stations in gastric cancer: A multicenter study. Radiother. Oncol. 2021, 165, 179–190. [Google Scholar] [CrossRef]
- Tatsumi, Y.; Tanigawa, N.; Nishimura, H.; Nomura, E.; Mabuchi, H.; Matsuki, M.; Narabayashi, I. Preoperative diagnosis of lymph node metastases in gastric cancer by magnetic resonance imaging with ferumoxtran-10. Gastric Cancer 2006, 9, 120–128. [Google Scholar] [CrossRef]
- Chen, S.; Yu, Y.; Li, T.; Ruan, W.; Wang, J.; Peng, Q.; Yu, Y.; Cao, T.; Xue, W.; Liu, X.; et al. A novel DNA methylation signature associated with lymph node metastasis status in early gastric cancer. Clin. Epigenetics 2022, 14, 18. [Google Scholar] [CrossRef]
- Wei, J.; Zhang, Y.; Liu, Y.; Wang, A.; Fan, B.; Fu, T.; Jia, Z.; He, L.; Ji, K.; Ji, X.; et al. Construction and Validation of a Risk-Scoring Model that Preoperatively Predicts Lymph Node Metastasis in Early Gastric Cancer Patients. Ann. Surg. Oncol. 2021, 28, 6665–6672. [Google Scholar] [CrossRef]
- Son, T.; Hyung, W.J.; Kim, J.W.; Kim, H.I.; An, J.Y.; Cheong, J.H.; Choi, S.H.; Noh, S.H. Anatomic extent of metastatic lymph nodes: Still important for gastric cancer prognosis. Ann. Surg. Oncol. 2014, 21, 899–907. [Google Scholar] [CrossRef]
- Jin, C.; Jiang, Y.; Yu, H.; Wang, W.; Li, B.; Chen, C.; Yuan, Q.; Hu, Y.; Xu, Y.; Zhou, Z.; et al. Deep learning analysis of the primary tumour and the prediction of lymph node metastases in gastric cancer. Br. J. Surg. 2021, 108, 542–549. [Google Scholar] [CrossRef]
- Rawicz-Pruszyński, K.; Mielko, J.; Ciseł, B.; Skórzewska, M.; Pikuła, A.; Gęca, K.; Skoczylas, T.; Kubiatowski, T.; Kurylcio, A.; Polkowski, W.P. Blast from the past: Perioperative use of the Maruyama computer program for prediction of lymph node involvement in the surgical treatment of gastric cancer following neoadjuvant chemotherapy. Eur. J. Surg. Oncol. 2019, 45, 1957–1963. [Google Scholar] [CrossRef]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer 2021, 24, 1–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamashita, H.; Seto, Y.; Sano, T.; Makuuchi, H.; Ando, N.; Sasako, M.; Japanese Gastric Cancer Association; the Japan Esophageal Society. Results of a nation-wide retrospective study of lymphadenectomy for esophagogastric junction carcinoma. Gastric Cancer 2017, 20, 69–83. [Google Scholar] [CrossRef] [Green Version]
- Yura, M.; Yoshikawa, T.; Otsuki, S.; Yamagata, Y.; Morita, S.; Katai, H.; Nishida, T.; Yoshiaki, T. Oncological safety of proximal gastrectomy for T2/T3 proximal gastric cancer. Gastric Cancer 2019, 22, 1029–1035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugoor, P.; Shah, S.; Dusane, R.; Desouza, A.; Goel, M.; Shrikhande, S.V. Proximal gastrectomy versus total gastrectomy for proximal third gastric cancer: Total gastrectomy is not always necessary. Langenbecks Arch. Surg. 2016, 401, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, M.; Honda, M.; Hiki, N.; Kinoshita, T.; Yabusaki, H.; Nunobe, S.; Shibasaki, H.; Matsuki, A.; Watanabe, M.; Abe, T. Oncological outcomes of function-preserving gastrectomy for early gastric cancer: A multicenter propensity score matched cohort analysis comparing pylorus-preserving gastrectomy versus conventional distal gastrectomy. Gastric Cancer 2017, 20, 709–717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, D.J.; Kim, Y.W.; Yang, H.K.; Ryu, K.W.; Han, S.U.; Kim, H.H.; Hyung, W.J.; Park, J.H.; Suh, Y.S.; Kwon, O.K.; et al. Short-term outcomes of a multicentre randomized clinical trial comparing laparoscopic pylorus-preserving gastrectomy with laparoscopic distal gastrectomy for gastric cancer (the KLASS-04 trial). Br. J. Surg. 2021, 108, 1043–1049. [Google Scholar] [CrossRef]
- Zhu, C.C.; Cao, H.; Berlth, F.; Xu, J.; Park, S.H.; Choe, H.N.; Suh, Y.S.; Kong, S.H.; Lee, H.J.; Kim, W.H.; et al. Pylorus-preserving gastrectomy for early cancer involving the upper third: Can we go higher? Gastric Cancer 2019, 22, 881–891. [Google Scholar] [CrossRef] [Green Version]
- Suh, Y.S.; Han, D.S.; Kong, S.H.; Kwon, S.; Shin, C.I.; Kim, W.H.; Kim, H.H.; Lee, H.J.; Yang, H.K. Laparoscopy-assisted pylorus-preserving gastrectomy is better than laparoscopy-assisted distal gastrectomy for middle-third early gastric cancer. Ann. Surg. 2014, 259, 485–493. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [Green Version]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 2017, 20, 1–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control. 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Khalayleh, H.; Kim, Y.W.; Man Yoon, H.; Ryu, K.W.; Kook, M.C. Evaluation of Lymph Node Metastasis Among Adults with Gastric Adenocarcinoma Managed with Total Gastrectomy. JAMA Netw. Open 2021, 4, e2035810. [Google Scholar] [CrossRef] [PubMed]
- Haruta, S.; Shinohara, H.; Hosogi, H.; Ohkura, Y.; Kobayashi, N.; Mizuno, A.; Okamura, R.; Ueno, M.; Sakai, Y.; Udagawa, H. Proximal gastrectomy with exclusion of no. 3b lesser curvature lymph node dissection could be indicated for patients with advanced upper-third gastric cancer. Gastric Cancer 2017, 20, 528–535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ri, M.; Kumagai, K.; Namikawa, K.; Atsumi, S.; Hayami, M.; Makuuchi, R.; Ida, S.; Ohashi, M.; Sano, T.; Nunobe, S. Is proximal gastrectomy indicated for locally advanced cancer in the upper third of the stomach? Ann. Gastroenterol. Surg. 2021, 5, 767–775. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, W.; Yu, Y.; Liu, J.J.; Jiang, L.; Xue, H.D.; Lei, J.; Jin, Z.; Yu, J.C. Prediction of the Depth of Tumor Invasion in Gastric Cancer: Potential Role of CT Radiomics. Acad. Radiol. 2020, 27, 1077–1084. [Google Scholar] [CrossRef]
- Mocellin, S.; Pasquali, S. Diagnostic accuracy of endoscopic ultrasonography (EUS) for the preoperative locoregional staging of primary gastric cancer. Cochrane Database Syst. Rev. 2015, 2015, CD009944. [Google Scholar] [CrossRef]
- Wang, J.; Li, X.; Zhang, Z.; Jing, C.; Li, J. Clinical Research of Combined Application of DCEUS and Dynamic Contrast-Enhanced MSCT in Preoperative cT Staging of Gastric Cancer. J. Oncol. 2021, 2021, 9868585. [Google Scholar] [CrossRef]
| Station | Upper Third | Middle Third | Lower Third | |||
|---|---|---|---|---|---|---|
| Tumor < 4 cm | Tumor ≥ 4 cm | Tumor < 4 cm | Tumor ≥ 4 cm | Tumor < 4 cm | Tumor ≥ 4 cm | |
| 1 | 9.3% (4/43) | 31.6% (42/133) | 4.3% (1/23) | 28.4% (21/74) | 11.1% (1/9) | 38.9% (7/18) |
| 2 | 0% (0/43) | 18.8% (25/133) | 0% (0/23) | 6.8% (5/74) | 0% (0/9) | 5.6% (1/18) |
| 3 | 16.3% (7/43) | 34.6% (46/133) | 8.7% (2/23) | 40.5% (30/74) | 0% (0/9) | 38.9% (7/18) |
| 4sa | 0% (0/43) | 5.3% (7/133) | 0% (0/23) | 16.2% (12/74) | 0% (0/9) | 5.6% (1/18) |
| 4sb | 2.3% (1/43) | 8.3% (11/133) | 0% (0/23) | 12.2% (9/74) | 0% (0/9) | 5.6% (1/18) |
| 4d | 0% (0/43) | 6.0% (8/133) | 8.7% (2/23) | 31.1% (23/74) | 0% (0/9) | 38.9% (7/18) |
| 5 | 0% (0/43) | 0.8% (1/133) | 0% (0/23) | 10.8% (8/74) | 0% (0/9) | 11.1% (2/18) |
| 6 | 0% (0/43) | 0% (0/133) | 0% (0/23) | 16.2% (12/74) | 0% (0/9) | 44.4% (8/18) |
| Station | Upper Third | Middle Third | Lower Third | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T1 | T2 | T3 | T4 | T1 | T2 | T3 | T4 | |
| 1 | 6.7% | 13.0% | 39.6% | 45.0% | 5.7% | 33.3% | 9.5% | 45.7% | 14.3% | 0% | 25.0% | 42.9% |
| (4/60) | (3/23) | (21/53) | (18/40) | (2/35) | (2/6) | (2/21) | (16/35) | (1/7) | (0/2) | (1/4) | (6/14) | |
| 2 | 0% | 8.7% | 17.0% | 35.0% | 0% | 0% | 0% | 14.3% | 0% | 0% | 0% | 7.1% |
| (0/60) | (2/23) | (9/53) | (14/40) | (0/35) | (0/6) | (0/21) | (5/35) | (0/7) | (0/2) | (0/4) | (1/14) | |
| 3 | 8.3% | 43.5% | 39.6% | 42.5% | 5.7% | 16.7% | 33.3% | 62.9% | 0% | 0% | 25.0% | 42.9% |
| (5/60) | (10/23) | (21/53) | (17/40) | (2/35) | (1/6) | (7/21) | (22/35) | (0/7) | (0/2) | (1/4) | (6/14) | |
| 4sa | 0% | 0% | 3.8% | 12.5% | 2.9% | 0% | 14.3% | 22.9% | 0% | 0% | 0% | 7.1% |
| (0/60) | (0/23) | (2/53) | (5/40) | (1/35) | (0/6) | (3/21) | (8/35) | (0/7) | (0/2) | (0/4) | (1/14) | |
| 4sb | 0% | 0% | 5.7% | 22.5% | 0% | 0% | 14.3% | 17.1% | 0% | 0% | 0% | 7.1% |
| (0/60) | (0/23) | (3/53) | (9/40) | (0/35) | (0/6) | (3/21) | (6/35) | (0/7) | (0/2) | (0/4) | (1/14) | |
| 4d | 0% | 0% | 3.8% | 15.0% | 8.6% | 16.7% | 19.0% | 48.6% | 0% | 0% | 0% | 50.0% |
| (0/60) | (0/23) | (2/53) | (6/40) | (3/35) | (1/6) | (4/21) | (17/35) | (0/7) | (0/2) | (0/4) | (7/14) | |
| 5 | 0% | 0% | 0% | 2.5% | 2.9% | 0% | 4.8% | 17.1% | 0% | 0% | 0% | 14.3% |
| (0/60) | (0/23) | (0/53) | (1/40) | (1/35) | (0/6) | (1/21) | (6/35) | (0/7) | (0/2) | (0/4) | (2/14) | |
| 6 | 0% | 0% | 0% | 0% | 2.9% | 0% | 4.8% | 28.6% | 0% | 50.0% | 0% | 50.0% |
| (0/60) | (0/23) | (0/53) | (0/40) | (1/35) | (0/6) | (1/21) | (10/35) | (0/7) | (1/2) | (0/4) | (7/14) | |
| Station | Multivariate Analysis (2nd) | Tumor Size (Continuous) | sDPD (Continuous) | Pathological Type | UICC 8th T Stage | Lymphatic Invasion | Venous Invasion |
|---|---|---|---|---|---|---|---|
| 1 | OR | 1.010 | 1.025 | 1.254 | 1.406 | 2.575 | 1.945 |
| (95% CI) | (1.001–1.018) | (0.962–1.092) | (0.868–1.810) | (1.030–1.918) | (1.172–5.653) | (0.769–4.916) | |
| p value | 0.021 | 0.445 | 0.228 | 0.032 | 0.018 | 0.160 | |
| 2 | OR | 1.004 | 1.121 | 1.221 | 2.478 | 2.523 | 3.283 |
| (95% CI) | (0.993–1.014) | (1.024–1.228) | (0.716–2.083) | (1.417–4.333) | (0.673–9.455) | (0.387–27.85) | |
| p value | 0.485 | 0.014 | 0.463 | 0.001 | 0.170 | 0.276 | |
| 3 | OR | 1.007 | 0.997 | 1.404 | 1.416 | 2.110 | 1.493 |
| (95% CI) | (0.999–1.015) | (0.940–1.058) | (0.999–1.972) | (1.059–1.893) | (1.050–4.242) | (0.665–3.349) | |
| p value | 0.080 | 0.925 | 0.051 | 0.019 | 0.036 | 0.331 | |
| 4sa | OR | 1.019 | 1.032 | 1.109 | 1.739 | 2.647 | 0.728 |
| (95% CI) | (1.008–1.030) | (0.923–1.154) | (0.558–2.204) | (0.913–3.314) | (0.501–13.97) | (0.149–3.555) | |
| p value | 0.001 | 0.577 | 0.768 | 0.092 | 0.252 | 0.695 | |
| 4sb | OR | 1.006 | 1.074 | 1.273 | 2.468 | 5.283 | 1.735 |
| (95% CI) | (0.994–1.017) | (0.970–1.190) | (0.672–2.410) | (1.265–4.816) | (0.645–43.29) | (0.194–15.48) | |
| p value | 0.319 | 0.170 | 0.458 | 0.008 | 0.121 | 0.622 | |
| 4d | OR | 1.009 | 0.882 | 1.214 | 1.480 | 2.414 | 4.543 |
| (95% CI) | (1.000–1.018) | (0.808–0.962) | (0.720–2.048) | (0.972–2.251) | (0.736–7.925) | (0.884–23.34) | |
| p value | 0.045 | 0.005 | 0.466 | 0.067 | 0.146 | 0.070 | |
| 5 | OR | 0.983 | 0.761 | 1.199 | 2.454 | 0.964 | 1.263 |
| (95% CI) | (0.963–1.003) | (0.633–0.914) | (0.489–2.940) | (1.050–5.739) | (0.146–6.359) | (0.102–15.65) | |
| p value | 0.097 | 0.004 | 0.692 | 0.038 | 0.969 | 0.856 | |
| 6 | OR | 0.993 | 0.676 | 0.885 | 1.782 | 1.860 | 9.466 |
| (95% CI) | (0.981–1.006) | (0.567–0.804) | (0.431–1.817) | (1.011–3.142) | (0.405–8.533) | (0.575–155.8) | |
| p value | 0.280 | <0.001 | 0.739 | 0.046 | 0.425 | 0.116 |
| Perigastric Lymph Node Metastasis (pLNM) Prediction | AUC (95% CI) | AIC |
|---|---|---|
| Station 1 pLNM | ||
| Tumor size | 0.706 (0.650–0.757) | 320 |
| UICC 8th T stage | 0.727 (0.673–0.777) | 307 |
| Lymphatic invasion | 0.682 (0.626–0.734) | 309 |
| Model: Tumor size + UICC 8th T stage + lymphatic invasion | 0.774 (0.723–0.820) | 297 |
| Station 2 pLNM | ||
| sDPD | 0.553 (0.495–0.610) | 203 |
| UICC 8th T stage | 0.775 (0.724–0.821) | 174 |
| Model: sDPD + UICC 8th T stage | 0.811 (0.763–0.854) | 171 |
| Station 3 pLNM | ||
| UICC 8th T stage | 0.719 (0.665–0.770) | 322 |
| Lymphatic invasion | 0.667 (0.611–0.720) | 342 |
| Model: UICC 8th T stage + lymphatic invasion | 0.742 (0.689–0.791) | 317 |
| Station 4sa pLNM | ||
| Tumor size | 0.813 (0.765–0.856) | 126 |
| Station 4sb pLNM | ||
| UICC 8th T stage | 0.794 (0.744–0.839) | 136 |
| Station 4d pLNM | ||
| Tumor size | 0.757 (0.704–0.804) | 213 |
| sDPD | 0.725 (0.671–0.775) | 218 |
| Model: Tumor size + sDPD | 0.819 (0.771–0.861) | 206 |
| Station 5 pLNM | ||
| sDPD | 0.741 (0.687–0.790) | 85 |
| UICC 8th T stage | 0.752 (0.699–0.800) | 90 |
| Model: sDPD + UICC 8th T stage | 0.791 (0.740–0.835) | 85 |
| Station 6 pLNM | ||
| sDPD | 0.873 (0.829–0.908) | 112 |
| UICC 8th T stage | 0.804 (0.755–0.848) | 127 |
| Model: sDPD + UICC 8th T stage | 0.909 (0.871–0.939) | 103 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, C.-D.; Yamashita, H.; Okumura, Y.; Yagi, K.; Aikou, S.; Seto, Y. Signature and Prediction of Perigastric Lymph Node Metastasis in Patients with Gastric Cancer and Total Gastrectomy: Is Total Gastrectomy Always Necessary? Cancers 2022, 14, 3409. https://doi.org/10.3390/cancers14143409
Zhang C-D, Yamashita H, Okumura Y, Yagi K, Aikou S, Seto Y. Signature and Prediction of Perigastric Lymph Node Metastasis in Patients with Gastric Cancer and Total Gastrectomy: Is Total Gastrectomy Always Necessary? Cancers. 2022; 14(14):3409. https://doi.org/10.3390/cancers14143409
Chicago/Turabian StyleZhang, Chun-Dong, Hiroharu Yamashita, Yasuhiro Okumura, Koichi Yagi, Susumu Aikou, and Yasuyuki Seto. 2022. "Signature and Prediction of Perigastric Lymph Node Metastasis in Patients with Gastric Cancer and Total Gastrectomy: Is Total Gastrectomy Always Necessary?" Cancers 14, no. 14: 3409. https://doi.org/10.3390/cancers14143409
APA StyleZhang, C.-D., Yamashita, H., Okumura, Y., Yagi, K., Aikou, S., & Seto, Y. (2022). Signature and Prediction of Perigastric Lymph Node Metastasis in Patients with Gastric Cancer and Total Gastrectomy: Is Total Gastrectomy Always Necessary? Cancers, 14(14), 3409. https://doi.org/10.3390/cancers14143409






