Protein Farnesylation on Nasopharyngeal Carcinoma, Molecular Background and Its Potential as a Therapeutic Target
Abstract
Simple Summary
Abstract
1. Introduction
2. RAS Oncoproteins and Farnesylation
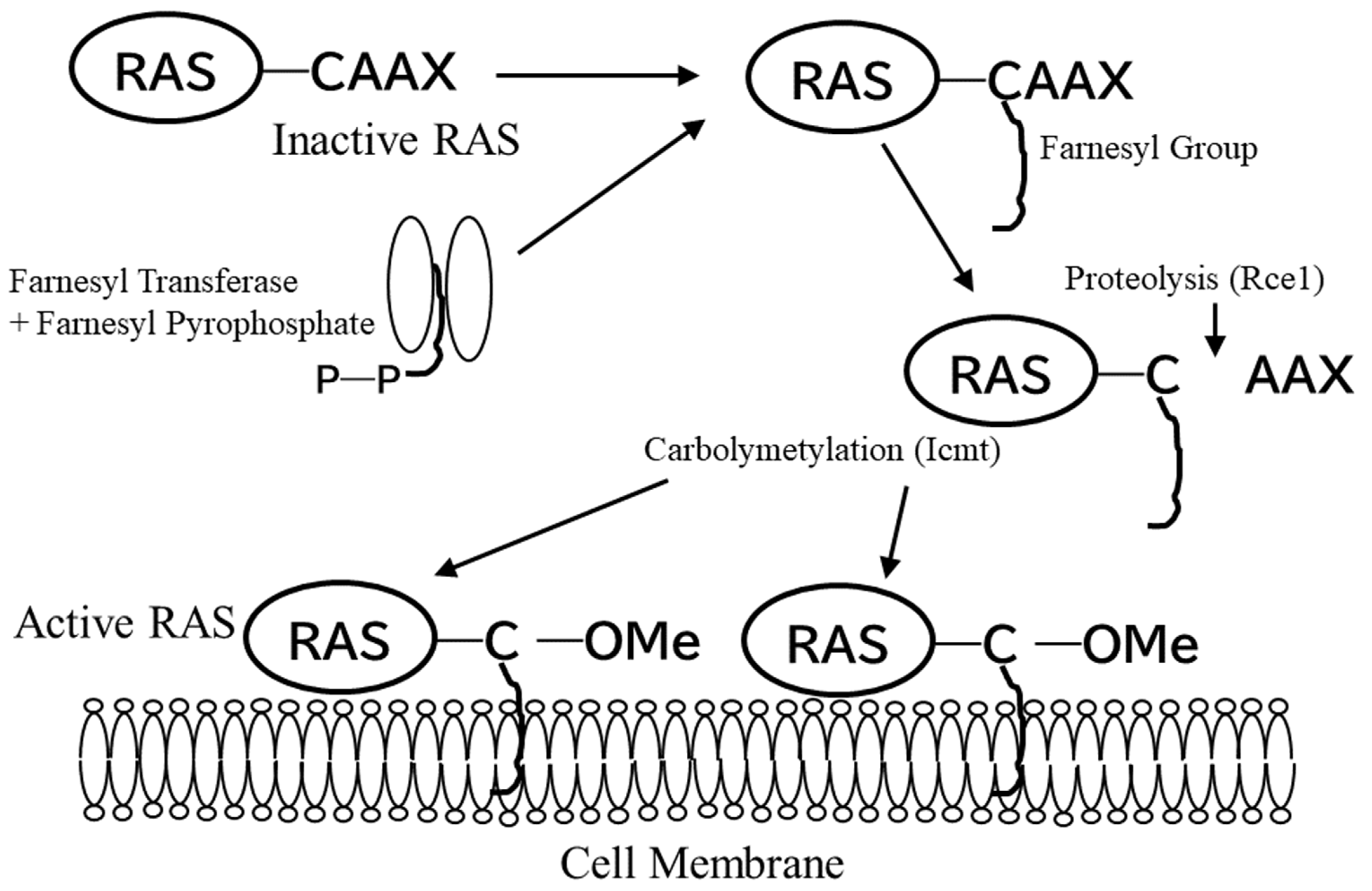
3. Farnesylation, Its Biosynthesis, and Membrane Association by Farnesylation
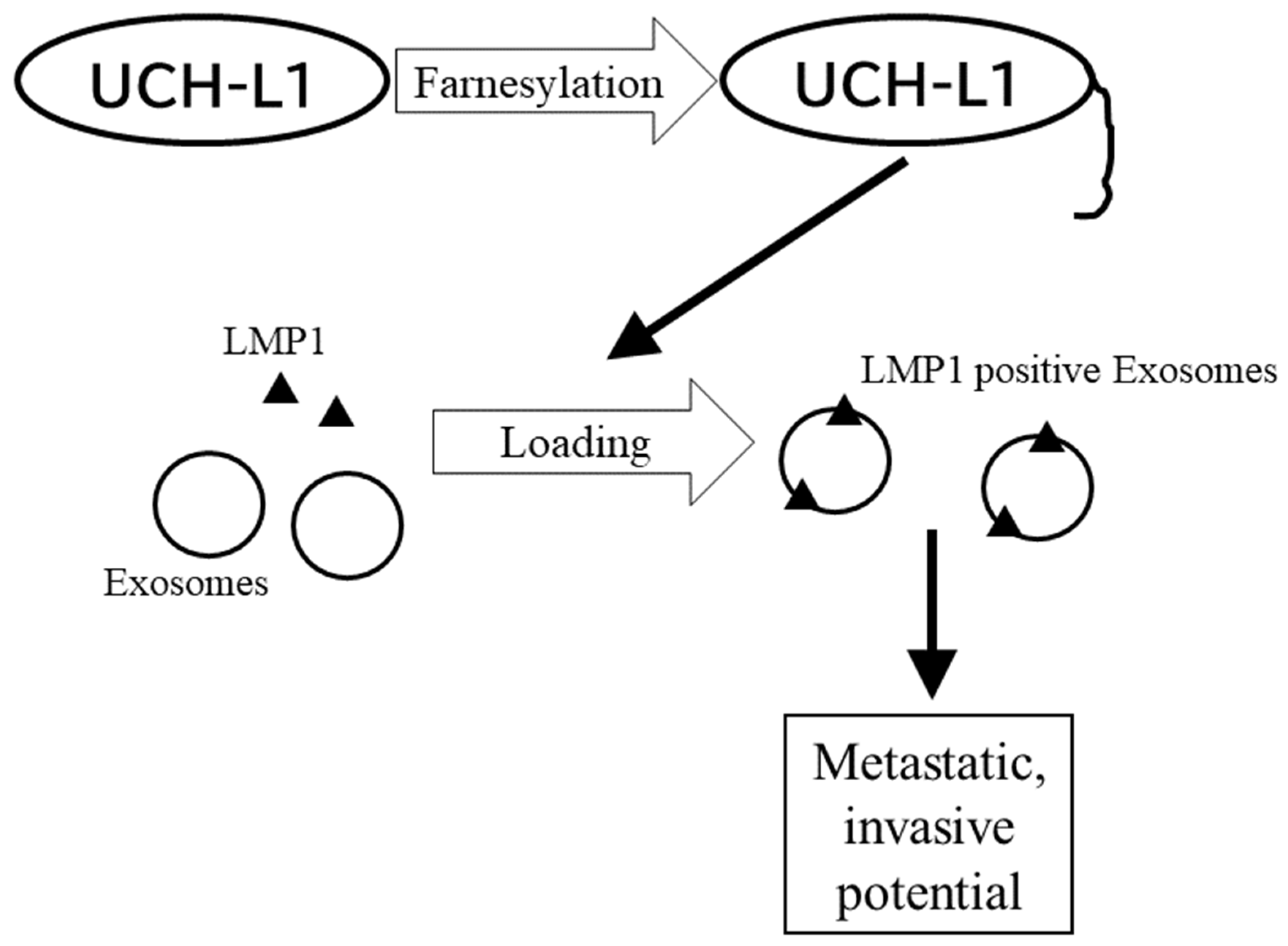
4. Proteins Modified by Farnesylation Other Than RAS
5. Development of Farnesyl Transferase Inhibitors
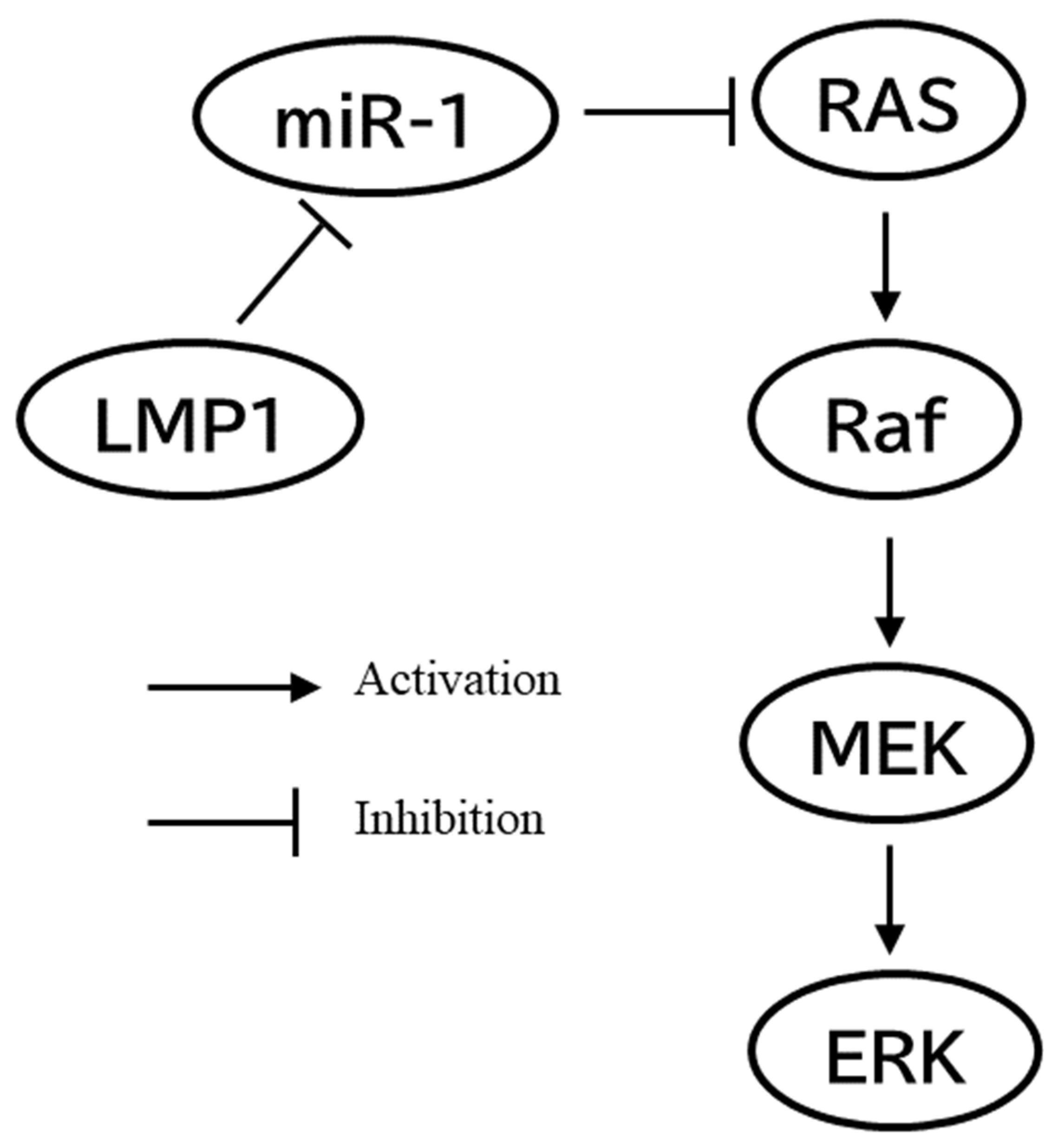
6. Nasopharyngeal Carcinoma and RAS
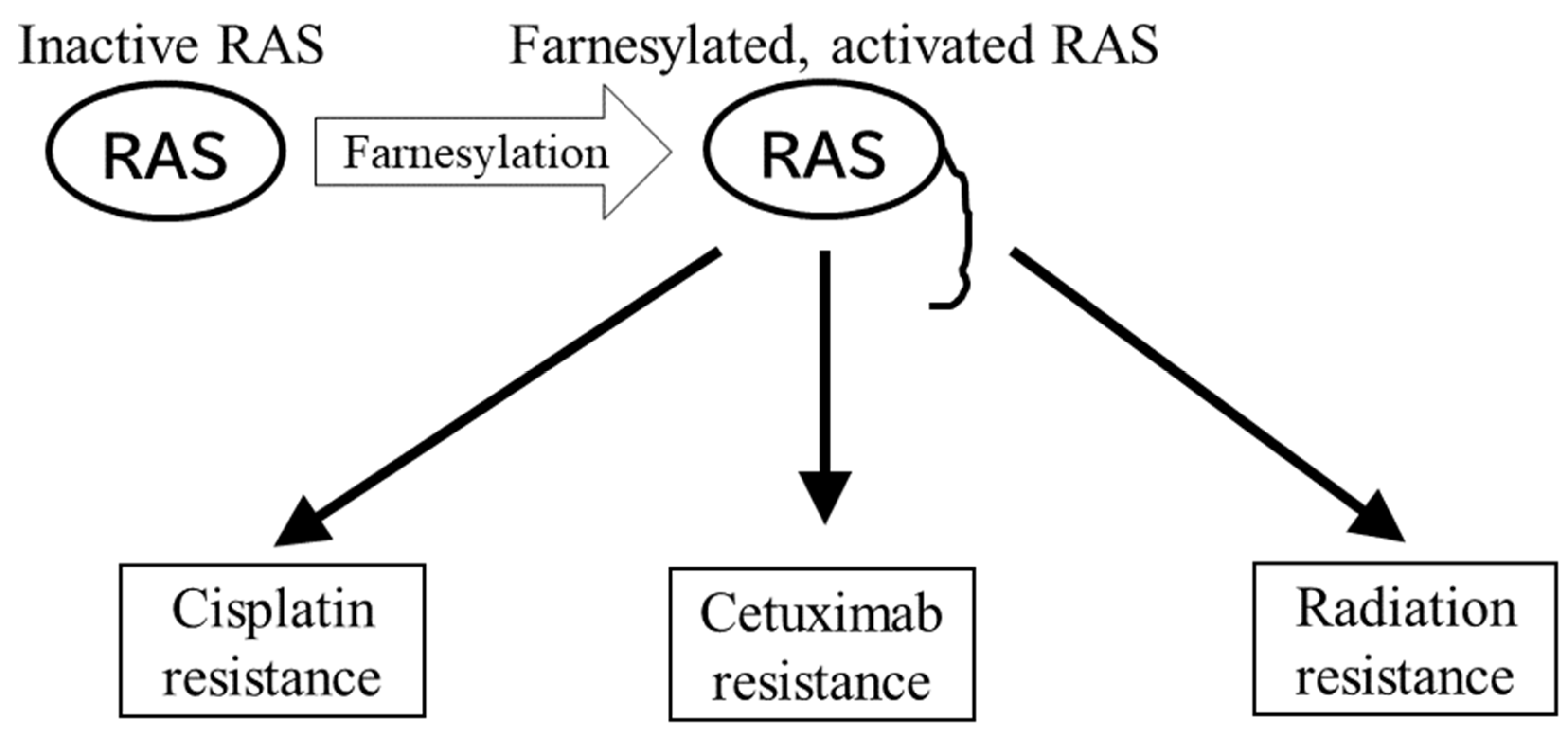
7. Farnesylation and Nasopharyngeal Carcinoma
8. Farnesylation as a Therapeutic Target
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Zanetti, R.; Ferlay, J. Cancer Incidence in Five Continents Volume XI; IARC Scientific Publications: Lyon, France, 2021; Volume XI, ISBN 978-92-832-2219-4.
- Yoshizaki, T.; Kondo, S.; Wakisaka, N.; Murono, S.; Endo, K.; Sugimoto, H.; Nakanishi, S.; Tsuji, A.; Ito, M. Pathogenic Role of Epstein-Barr Virus Latent Membrane Protein-1 in the Development of Nasopharyngeal Carcinoma. Cancer Lett. 2013, 337, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Suzuki, D.; Tokunaga, T.; Takabayashi, T.; Yamada, T.; Wakisaka, N.; Yoshizaki, T.; Murata, H.; Miwa, K.; Shoujaku, H.; et al. Epidemiological Analysis of Nasopharyngeal Carcinoma in the Central Region of Japan during the Period from 1996 to 2005. Auris Nasus Larynx 2011, 38, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Raab-Traub, N. Novel Mechanisms of EBV-Induced Oncogenesis. Curr. Opin. Virol. 2012, 2, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Yoshizaki, T.; Wakisaka, N.; Pagano, J.S. Epstein-Barr Virus, Invasion and Metastasis; Robertson, E.S., Ed.; Caister Academic Press: Norfolk, UK, 2005; ISBN 978-1-904455-03-5. [Google Scholar]
- Shair, K.; Reddy, A.; Cooper, V. New Insights from Elucidating the Role of LMP1 in Nasopharyngeal Carcinoma. Cancers 2018, 10, 86. [Google Scholar] [CrossRef]
- Mainou, B.A.; Everly, D.N.; Raab-Traub, N. Unique Signaling Properties of CTAR1 in LMP1-Mediated Transformation. J. Virol. 2007, 81, 9680–9692. [Google Scholar] [CrossRef]
- Izumi, K.M.; McFarland, E.C.; Ting, A.T.; Riley, E.A.; Seed, B.; Kieff, E.D. The Epstein-Barr Virus Oncoprotein Latent Membrane Protein 1 Engages the Tumor Necrosis Factor Receptor-Associated Proteins TRADD and Receptor-Interacting Protein (RIP) but Does Not Induce Apoptosis or Require RIP for NF-KappaB Activation. Mol. Cell. Biol. 1999, 19, 5759–5767. [Google Scholar] [CrossRef]
- Izumi, K.M.; Kieff, E.D. The Epstein-Barr Virus Oncogene Product Latent Membrane Protein 1 Engages the Tumor Necrosis Factor Receptor-Associated Death Domain Protein to Mediate B Lymphocyte Growth Transformation and Activate NF-KappaB. Proc. Natl. Acad. Sci. USA 1997, 94, 12592–12597. [Google Scholar] [CrossRef]
- Mosialos, G.; Birkenbacht, M.; Yalamanchill, R.; van Arsdale, T.; Ware, C.; Kleff, E. The Epstein-Barr Virus Transforming Protein LMP1 Engages Signaling Proteins for the Tumor Necrosis Factor Receptor Family. Cell 1995, 80, 389–399. [Google Scholar] [CrossRef]
- Paine, E.; Scheinman, R.I.; Baldwin, A.S.; Raab-Traub, N. Expression of LMP1 in Epithelial Cells Leads to the Activation of a Select Subset of NF-Kappa B/Rel Family Proteins. J. Virol. 1995, 69, 4572–4576. [Google Scholar] [CrossRef]
- Thornburg, N.J.; Kulwichit, W.; Edwards, R.H.; Shair, K.H.Y.; Bendt, K.M.; Raab-Traub, N. LMP1 Signaling and Activation of NF-KappaB in LMP1 Transgenic Mice. Oncogene 2006, 25, 288–297. [Google Scholar] [CrossRef]
- Roberts, M.L.; Cooper, N.R. Activation of a Ras–MAPK-Dependent Pathway by Epstein–Barr Virus Latent Membrane Protein 1 Is Essential for Cellular Transformation. Virology 1998, 240, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Eliopoulos, A.G.; Young, L.S. Activation of the CJun N-Terminal Kinase (JNK) Pathway by the Epstein-Barr Virus-Encoded Latent Membrane Protein 1 (LMP1). Oncogene 1998, 16, 1731–1742. [Google Scholar] [CrossRef] [PubMed]
- Mainou, B.A.; Everly, D.N.; Raab-Traub, N. Epstein-Barr Virus Latent Membrane Protein 1 CTAR1 Mediates Rodent and Human Fibroblast Transformation through Activation of PI3K. Oncogene 2005, 24, 6917–6924. [Google Scholar] [CrossRef] [PubMed]
- Everly, D.N.; Mainou, B.A.; Raab-Traub, N. Induction of Id1 and Id3 by Latent Membrane Protein 1 of Epstein-Barr Virus and Regulation of P27/Kip and Cyclin-Dependent Kinase 2 in Rodent Fibroblast Transformation. J. Virol. 2004, 78, 13470–13478. [Google Scholar] [CrossRef]
- Yoshizaki, T.; Sato, H.; Furukawa, M.; Pagano, J.S. The Expression of Matrix Metalloproteinase 9 Is Enhanced by Epstein-Barr Virus Latent Membrane Protein 1. Proc. Natl. Acad. Sci. USA 1998, 95, 3621–3626. [Google Scholar] [CrossRef]
- Yoshizaki, T.; Horikawa, T.; Qing-Chun, R.; Wakisaka, N.; Takeshita, H.; Sheen, T.; Lee, S.; Sato, H.; Furukawa, M. Induction of Interleukin-8 by Epstein-Barr Virus Latent Membrane Protein-1 and Its Correlation to Angiogenesis in Nasopharyngeal Carcinoma. Clin. Cancer Res. 2001, 7, 1946–1951. [Google Scholar]
- Wakisaka, N.; Murono, S.; Yoshizaki, T.; Furukawa, M.; Pagano, J.S. Epstein-Barr Virus Latent Membrane Protein 1 Induces and Causes Release of Fibroblast Growth Factor-2. Cancer Res. 2002, 62, 6337–6344. [Google Scholar]
- Horikawa, T.; Yang, J.; Kondo, S.; Yoshizaki, T.; Joab, I.; Furukawa, M.; Pagano, J.S. Twist and Epithelial-Mesenchymal Transition Are Induced by the EBV Oncoprotein Latent Membrane Protein 1 and Are Associated with Metastatic Nasopharyngeal Carcinoma. Cancer Res. 2007, 67, 1970–1978. [Google Scholar] [CrossRef]
- Murono, S.; Inoue, H.; Tanabe, T.; Joab, I.; Yoshizaki, T.; Furukawa, M.; Pagano, J.S. Induction of Cyclooxygenase-2 by Ep-stein-Barr Virus Latent Membrane Protein 1 Is Involved in Vascular Endothelial Growth Factor Production in Nasopharyn-geal Carcinoma Cells. Proc. Natl. Acad. Sci. USA 2001, 98, 6905–6910. [Google Scholar] [CrossRef]
- Tang, L.L.; Chen, W.Q.; Xue, W.Q.; He, Y.Q.; Zheng, R.S.; Zeng, Y.X.; Jia, W.H. Global Trends in Incidence and Mortality of Nasopharyngeal Carcinoma. Cancer Lett. 2016, 374, 22–30. [Google Scholar] [CrossRef]
- Bossi, P.; Chan, A.T.; Licitra, L.; Trama, A.; Orlandi, E.; Hui, E.P.; Halámková, J.; Mattheis, S.; Baujat, B.; Hardillo, J.; et al. Nasopharyngeal Carcinoma: ESMO-EURACAN Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2021, 32, 452–465. [Google Scholar] [CrossRef] [PubMed]
- Kanno, M.; Narita, N.; Fujimoto, Y.; Wakisaka, N.; Yoshizaki, T.; Kodaira, T.; Makita, C.; Sato, Y.; Yamazaki, K.; Wakaoka, T.; et al. Third Epidemiological Analysis of Nasopharyngeal Carcinoma in the Central Region of Japan from 2006 to 2015. Cancers 2019, 11, 1180. [Google Scholar] [CrossRef] [PubMed]
- Ferris, R.L.; Blumenschein, G.; Fayette, J.; Guigay, J.; Colevas, A.D.; Licitra, L.; Harrington, K.; Kasper, S.; Vokes, E.E.; Even, C.; et al. Nivolumab for Recurrent Squamous-Cell Carcinoma of the Head and Neck. N. Engl. J. Med. 2016, 375, 1856–1867. [Google Scholar] [CrossRef] [PubMed]
- Ferris, R.L.; Blumenschein, G.; Fayette, J.; Guigay, J.; Colevas, A.D.; Licitra, L.; Harrington, K.J.; Kasper, S.; Vokes, E.E.; Even, C.; et al. Nivolumab vs Investigator’s Choice in Recurrent or Metastatic Squamous Cell Carcinoma of the Head and Neck: 2-Year Long-Term Survival Update of CheckMate 141 with Analyses by Tumor PD-L1 Expression. Oral Oncol. 2018, 81, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Burtness, B.; Harrington, K.J.; Greil, R.; Soulières, D.; Tahara, M.; de Castro, G.; Psyrri, A.; Basté, N.; Neupane, P.; Bratland, Å.; et al. Pembrolizumab Alone or with Chemotherapy versus Cetuximab with Chemotherapy for Recurrent or Metastatic Squamous Cell Carcinoma of the Head and Neck (KEYNOTE-048): A Randomised, Open-Label, Phase 3 Study. Lancet 2019, 394, 1915–1928. [Google Scholar] [CrossRef]
- Ma, B.B.Y.; Lim, W.T.; Goh, B.C.; Hui, E.P.; Lo, K.W.; Pettinger, A.; Foster, N.R.; Riess, J.W.; Agulnik, M.; Chang, A.Y.C.; et al. Antitumor Activity of Nivolumab in Recurrent and Metastatic Nasopharyngeal Carcinoma: An International, Multicenter Study of the Mayo Clinic Phase 2 Consortium (NCI-9742). J. Clin. Oncol. 2018, 36, 1412–1418. [Google Scholar] [CrossRef]
- Lerner, E.C.; Qian, Y.; Blaskovich, M.A.; Fossum, R.D.; Vogt, A.; Sun, J.; Cox, A.D.; Der, C.J.; Hamilton, A.D.; Sebti, S.M. Ras CAAX Peptidomimetic FTI-277 Selectively Blocks Oncogenic Ras Signaling by Inducing Cytoplasmic Accumulation of Inactive Ras-Raf Complexes. J. Biol. Chem. 1995, 270, 26802–26806. [Google Scholar] [CrossRef]
- Sebti, S.M.; Hamilton, A.D. Farnesyltransferase and Geranylgeranyltransferase I Inhibitors and Cancer Therapy: Lessons from Mechanism and Bench-to-Bedside Translational Studies. Oncogene 2000, 19, 6584–6593. [Google Scholar] [CrossRef]
- Prendergast, G.C.; Oliff, A. Farnesyltransferase Inhibitors: Antineoplastic Properties, Mechanisms of Action, and Clinical Prospects. Semin. Cancer Biol. 2000, 10, 443–452. [Google Scholar] [CrossRef]
- Hancock, J.F.; Magee, A.I.; Childs, J.E.; Marshall, C.J. All Ras Proteins Are Polyisoprenylated but Only Some Are Palmitoylated. Cell 1989, 57, 1167–1177. [Google Scholar] [CrossRef]
- Casey, P.J.; Solski, P.A.; Der, C.J.; Buss, J.E. P21ras Is Modified by a Farnesyl Isoprenoid. Proc. Natl. Acad. Sci. USA 1989, 86, 8323–8327. [Google Scholar] [CrossRef] [PubMed]
- Adjei, A.A.; Erlichman, C.; Davis, J.N.; Cutler, D.L.; Sloan, J.A.; Marks, R.S.; Hanson, L.J.; Svingen, P.A.; Atherton, P.; Bishop, W.R.; et al. A Phase I Trial of the Farnesyl Transferase Inhibitor SCH66336: Evidence for Biological and Clinical Activity. Cancer Res. 2000, 60, 1871–1877. [Google Scholar] [PubMed]
- Kerklaan, B.M.; Diéras, V.; le Tourneau, C.; Mergui-Roelvink, M.; Huitema, A.D.R.; Rosing, H.; Beijnen, J.H.; Marreaud, S.; Govaerts, A.-S.; Piccart-Gebhart, M.J.; et al. Phase I Study of Lonafarnib (SCH66336) in Combination with Trastuzumab plus Paclitaxel in Her2/Neu Overexpressing Breast Cancer: EORTC Study 16023. Cancer Chemother. Pharmacol. 2013, 71, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Andreopoulou, E.; Vigoda, I.S.; Valero, V.; Hershman, D.L.; Raptis, G.; Vahdat, L.T.; Han, H.S.; Wright, J.J.; Pellegrino, C.M.; Cristofanilli, M.; et al. Phase I–II Study of the Farnesyl Transferase Inhibitor Tipifarnib plus Sequential Weekly Paclitaxel and Doxorubicin–Cyclophosphamide in HER2/Neu-Negative Inflammatory Carcinoma and Non-Inflammatory Estrogen Receptor-Positive Breast Carcinoma. Breast Cancer Res. Treat. 2013, 141, 429–435. [Google Scholar] [CrossRef][Green Version]
- Stieglitz, E.; Ward, A.F.; Gerbing, R.B.; Alonzo, T.A.; Arceci, R.J.; Liu, Y.L.; Emanuel, P.D.; Widemann, B.C.; Cheng, J.W.; Jayaprakash, N.; et al. Phase II/III Trial of a Pre-Transplant Farnesyl Transferase Inhibitor in Juvenile Myelomonocytic Leukemia: A Report from the Children’s Oncology Group. Pediatr. Blood Cancer 2015, 62, 629–636. [Google Scholar] [CrossRef]
- Gilardi, M.; Wang, Z.; Proietto, M.; Chilla, A.; Calleja-Valera, J.L.; Goto, Y.; Vanoni, M.; Janes, M.R.; Mikulski, Z.; Gualberto, A.; et al. Tipifarnib as a Precision Therapy for HRAS-Mutant Head and Neck Squamous Cell Carcinomas. Mol. Cancer Ther. 2020, 19, 1784–1796. [Google Scholar] [CrossRef]
- Ho, A.L.; Brana, I.; Haddad, R.; Bauman, J.; Bible, K.; Oosting, S.; Wong, D.J.; Ahn, M.J.; Boni, V.; Even, C.; et al. Tipifarnib in Head and Neck Squamous Cell Carcinoma with HRAS Mutations. J. Clin. Oncol. 2021, 39, 1856–1864. [Google Scholar] [CrossRef]
- Novelli, G.; D’Apice, M.R. Protein Farnesylation and Disease. J. Inherit. Metab. Dis. 2012, 35, 917–926. [Google Scholar] [CrossRef]
- McTaggart, S.J. Isoprenylated Proteins. Cell. Mol. Life Sci. 2006, 63, 255–267. [Google Scholar] [CrossRef]
- Vicat, J.-M.; Ardila-Osorio, H.; Khabir, A.; Brezak, M.-C.; Viossat, I.; Kasprzyk, P.; Jlidi, R.; Opolon, P.; Ooka, T.; Prevost, G.; et al. Apoptosis and TRAF-1 Cleavage in Epstein-Barr Virus-Positive Nasopharyngeal Carcinoma Cells Treated with Doxorubicin Combined with a Farnesyl-Transferase Inhibitor. Biochem. Pharmacol. 2003, 65, 423–433. [Google Scholar] [CrossRef]
- Kobayashi, E.; Aga, M.; Kondo, S.; Whitehurst, C.; Yoshizaki, T.; Pagano, J.S.; Shackelford, J. C-Terminal Farnesylation of UCH-L1 Plays a Role in Transport of Epstein-Barr Virus Primary Oncoprotein LMP1 to Exosomes. mSphere 2018, 3, e00030-18. [Google Scholar] [CrossRef] [PubMed]
- Malumbres, M.; Barbacid, M. RAS Oncogenes: The First 30 Years. Nat. Rev. Cancer 2003, 3, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Cox, A.D.; Der, C.J. Ras History: The Saga Continues. Small GTPases 2010, 1, 2–27. [Google Scholar] [CrossRef]
- Shimizu, K.; Goldfarb, M.; Suard, Y.; Perucho, M.; Li, Y.; Kamata, T.; Feramisco, J.; Stavnezer, E.; Fogh, J.; Wigler, M.H. Three Human Transforming Genes Are Related to the Viral Ras Oncogenes. Proc. Natl. Acad. Sci. USA 1983, 80, 2112–2116. [Google Scholar] [CrossRef] [PubMed]
- Brunner, T.B.; Hahn, S.M.; Gupta, A.K.; Muschel, R.J.; Mckenna, W.G.; Bernhard, E.J. Farnesyltransferase Inhibitors: An Overview of the Results of Preclinical and Clinical Investigations. Cancer Res. 2003, 63, 5656–5668. [Google Scholar] [PubMed]
- Baum, C.; Kirschmeier, P. Preclinical and Clinical Evaluation of Farnesyltransferase Inhibitors. Curr. Oncol. Rep. 2003, 5, 99–107. [Google Scholar] [CrossRef]
- Rowinsky, E.K.; Windle, J.J.; von Hoff, D.D. Ras Protein Farnesyltransferase: A Strategic Target for Anticancer Therapeutic Development. J. Clin. Oncol. 1999, 17, 3631–3652. [Google Scholar] [CrossRef]
- Adjei, A.A. Blocking Oncogenic Ras Signaling for Cancer Therapy. J. Natl. Cancer Inst. 2001, 93, 1062–1074. [Google Scholar] [CrossRef]
- Scolnick, E.M.; Papageorge, A.G.; Shih, T.Y. Guanine Nucleotide-Binding Activity as an Assay for Src Protein of Rat-Derived Murine Sarcoma Viruses. Proc. Natl. Acad. Sci. USA 1979, 76, 5355–5359. [Google Scholar] [CrossRef]
- Willingham, M.C.; Pastan, I.; Shih, T.Y.; Scolnick, E.M. Localization of the Src Gene Product of the Harvey Strain of MSV to Plasma Membrane of Transformed Cells by Electron Microscopic Immunocytochemistry. Cell 1980, 19, 1005–1014. [Google Scholar] [CrossRef]
- Papageorge, A.; Lowy, D.; Scolnick, E.M. Comparative Biochemical Properties of P21 Ras Molecules Coded for by Viral and Cellular Ras Genes. J. Virol. 1982, 44, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Hurley, J.B.; Simon, M.I.; Teplow, D.B.; Robishaw, J.D.; Gilman, A.G. Homologies between Signal Transducing G Proteins and Ras Gene Products. Science 1984, 226, 860–862. [Google Scholar] [CrossRef] [PubMed]
- Wood, K.W.; Sarnecki, C.; Roberts, T.M.; Blenis, J. Ras Mediates Nerve Growth Factor Receptor Modulation of Three Signal-Transducing Protein Kinases: MAP Kinase, Raf-1, and RSK. Cell 1992, 68, 1041–1050. [Google Scholar] [CrossRef]
- Hagemann, C.; Blank, J.L. The Ups and Downs of MEK Kinase Interactions. Cell. Signal. 2001, 13, 863–875. [Google Scholar] [CrossRef]
- Willumsen, B.M.; Christensen, A.; Hubbert, N.L.; Papageorge, A.G.; Lowy, D.R. The P21 Ras C-Terminus Is Required for Transformation and Membrane Association. Nature 1984, 310, 583–586. [Google Scholar] [CrossRef] [PubMed]
- Willumsen, B.; Norris, K.; Papageorge, A.; Hubbert, N.; Lowy, D. Harvey Murine Sarcoma Virus P21 Ras Protein: Biological and Biochemical Significance of the Cysteine Nearest the Carboxy Terminus. EMBO J. 1984, 3, 2581–2585. [Google Scholar] [CrossRef]
- Schafer, W.R.; Kim, R.; Sterne, R.; Thorner, J.; Kim, S.H.; Rine, J. Genetic and Pharmacological Suppression of Oncogenic Mutations in Ras Genes of Yeast and Humans. Science 1989, 245, 379–385. [Google Scholar] [CrossRef]
- Schafer, W.R.; Trueblood, C.E.; Yang, C.C.; Mayer, M.P.; Rosenberg, S.; Poulter, C.D.; Kim, S.H.; Rine, J. Enzymatic Coupling of Cholesterol Intermediates to a Mating Pheromone Precursor and to the Ras Protein. Science 1990, 249, 1133–1139. [Google Scholar] [CrossRef]
- Nagasu, T.; Yoshimatsu, K.; Rowell, C.; Lewis, M.; Garcia, A. Inhibition of Human Tumor Xenograft Growth by Treatment with the Farnesyl Transferase Inhibitor B956. Cancer Res. 1995, 55, 5310–5314. [Google Scholar]
- Kohl, N.E.; Omer, C.A.; Davide, J.P.; Hamilton, K.; Koblan, K.S.; Kral, A.M.; Miller, P.J.; Mosser, S.D.; O’neill, T.J.; Rands, E.; et al. Inhibition of Farnesyltransferase Induces Regression of Mammary and Salivary Carcinomas in Ras Transgenic Mice. Nat. Med. 1995, 1, 792–797. [Google Scholar] [CrossRef]
- Prior, I.A.; Hancock, J.F. Compartmentalization of Ras Proteins. J. Cell Sci. 2001, 114, 1603–1608. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, J.L.; Brown, M.S. Regulation of the Mevalonate Pathway. Nature 1990, 343, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Hancock, J.F.; Cadwallader, K.; Paterson, H.; Marshall, C.J. A CAAX or a CAAL Motif and a Second Signal Are Sufficient for Plasma Membrane Targeting of Ras Proteins. EMBO J. 1991, 10, 4033. [Google Scholar] [CrossRef]
- Resh, M.D. Trafficking and Signaling by Fatty-Acylated and Prenylated Proteins. Nat. Chem. Biol. 2006, 2, 584–590. [Google Scholar] [CrossRef]
- Lutz, R.J.; Trujillo, M.A.; Denham, K.S.; Wenger, L.; Sinensky, M. Nucleoplasmic Localization of Prelamin A: Implications for Prenylation-Dependent Lamin A Assembly into the Nuclear Lamina. Proc. Natl. Acad. Sci. USA 1992, 89, 3000–3004. [Google Scholar] [CrossRef]
- Zeng, Q.; Si, X.; Horstmann, H.; Xu, Y.; Hong, W.; Pallen, C.J. Prenylation-Dependent Association of Protein-Tyrosine Phosphatases PRL-1, -2, and -3 with the Plasma Membrane and the Early Endosome. J. Biol. Chem. 2000, 275, 21444–21452. [Google Scholar] [CrossRef] [PubMed]
- Tamanoi, F.; Kato-Stankiewicz, J.; Jiang, C.; Machado, I.; Thapar, N. Farnesylated Proteins and Cell Cycle Progression. J. Cell. Biochem. Suppl. 2001, 84 (Suppl. S37), 64–70. [Google Scholar] [CrossRef]
- Ashar, H.R.; James, L.; Gray, K.; Carr, D.; Black, S.; Armstrong, L.; Bishop, W.R.; Kirschmeier, P. Farnesyl Transferase Inhibitors Block the Farnesylation of CENP-E and CENP-F and Alter the Association of CENP-E with the Microtubules. J. Biol. Chem. 2000, 275, 30451–30457. [Google Scholar] [CrossRef]
- Hussein, D.; Taylor, S.S. Farnesylation of Cenp-F Is Required for G2/M Progression and Degradation after Mitosis. J. Cell Sci. 2002, 115, 3403–3414. [Google Scholar] [CrossRef]
- Liu, Z.; Meray, R.K.; Grammatopoulos, T.N.; Fredenburg, R.A.; Cookson, M.R.; Liu, Y.; Logan, T.; Lansbury, P.T. Membrane-Associated Farnesylated UCH-L1 Promotes Alpha-Synuclein Neurotoxicity and Is a Therapeutic Target for Parkinson’s Disease. Proc. Natl. Acad. Sci. USA 2009, 106, 4635–4640. [Google Scholar] [CrossRef]
- Luhtala, N.; Aslanian, A.; Yates, J.R.; Hunter, T. Secreted Glioblastoma Nanovesicles Contain Intracellular Signaling Proteins and Active Ras Incorporated in a Farnesylation-Dependent Manner. J. Biol. Chem. 2017, 292, 611–628. [Google Scholar] [CrossRef] [PubMed]
- Maurer-Stroh, S.; Koranda, M.; Benetka, W.; Schneider, G.; Sirota, F.L.; Eisenhaber, F. Towards Complete Sets of Farnesylated and Geranylgeranylated Proteins. PLoS Comput. Biol. 2007, 3, 634–648. [Google Scholar] [CrossRef] [PubMed]
- Cox, A.D.; Der, C.J. Farnesyltransferase Inhibitors and Cancer Treatment: Targeting Simply Ras? Biochim. Biophys. Acta 1997, 1333, F51–F71. [Google Scholar] [CrossRef]
- Ellis, S.; Mellor, H. Regulation of Endocytic Traffic by Rho Family GTPases. Trends Cell Biol. 2000, 10, 85–88. [Google Scholar] [CrossRef]
- Adamson, P.; Marshall, C.; Hall, A.; Tilbrook, P. Post-Translational Modifications of P21rho Proteins. J. Biol. Chem. 1992, 267, 20033–20038. [Google Scholar] [CrossRef]
- Worman, H.J.; Fong, L.G.; Muchir, A.; Young, S.G. Laminopathies and the Long Strange Trip from Basic Cell Biology to Therapy. J. Clin. Investig. 2009, 119, 1825–1836. [Google Scholar] [CrossRef] [PubMed]
- Leonard, D.M. Ras Farnesyltransferase: A New Therapeutic Target. J. Med. Chem. 1997, 40, 2971–2990. [Google Scholar] [CrossRef]
- Manne, V.; Yan, N.; Carboni, J.; Tuomari, A.; Ricca, C.; Brown, J.; Andahazy, M.; Schmidt, R.; Patel, D.; Zahler, R. Bisubstrate Inhibitors of Farnesyltransferase: A Novel Class of Specific Inhibitors of Ras Transformed Cells. Oncogene 1995, 10, 1763–1779. [Google Scholar]
- Bos, J.L.; de Vries, M.V.; van der Eb, A.J.; Fearon, E.R.; Vogelstein, B.; Hamilton, S.R.; van Boom, J.H. Prevalence of Ras Gene Mutations in Human Colorectal Cancers. Nature 1987, 327, 293–297. [Google Scholar] [CrossRef]
- Forrester, K.; Allmoguera, C.; Perucho, M.; Han, K.; Grizzle, W.E. Detection of High Incidence of K-Ras Oncogenes during Human Colon Tumorigenesis. Nature 1987, 327, 298–303. [Google Scholar] [CrossRef]
- Rodenhuis, S.; van de Wetering, M.L.; Mooi, W.J.; Evers, S.G.; van Zandwijk, N.; Bos, J.L. Mutational Activation of the K-Ras Oncogene. A Possible Pathogenetic Factor in Adenocarcinoma of the Lung. N. Engl. J. Med. 1987, 317, 929–935. [Google Scholar] [CrossRef] [PubMed]
- Smit, V.T.H.B.M.; Boot, A.J.M.; Smits, A.M.M.; Fleuren, G.J.; Cornelisse, C.J.; Bos, J.L. KRAS Codon 12 Mutations Occur Very Frequently in Pancreatic Adenocarcinomas. Nucleic Acids Res. 1988, 16, 7773–7782. [Google Scholar] [CrossRef] [PubMed]
- Almoguera, C.; Shibata, D.; Forrester, K.; Martin, J.; Arnheim, N.; Perucho, M. Most Human Carcinomas of the Exocrine Pancreas Contain Mutant C-K-Ras Genes. Cell 1988, 53, 549–554. [Google Scholar] [CrossRef]
- Yung, W.C.W.; Sham, J.S.T.; Choy, D.T.K.; Ng, M.H. Ras Mutations Are Uncommon in Nasopharyngeal Carcinoma. Eur. J. Cancer B Oral Oncol. 1995, 31B, 399–400. [Google Scholar] [CrossRef]
- Wang, H.Y.; Li, F.; Liu, N.; Liu, X.Y.; Yang, X.H.; Guo, Y.M.; Bei, J.X.; Zeng, Y.X.; Shao, J.Y. Prognostic Implications of a Molecular Classifier Derived from Whole-Exome Sequencing in Nasopharyngeal Carcinoma. Cancer Med. 2019, 8, 2705–2716. [Google Scholar] [CrossRef]
- Li, Y.Y.; Chung, G.T.Y.; Lui, V.W.Y.; To, K.F.; Ma, B.B.Y.; Chow, C.; Woo, J.K.S.; Yip, K.Y.; Seo, J.; Hui, E.P.; et al. Exome and Genome Sequencing of Nasopharynx Cancer Identifies NF-κB Pathway Activating Mutations. Nat. Commun. 2017, 8, 14121. [Google Scholar] [CrossRef]
- Mann, K.M.; Ying, H.; Juan, J.; Jenkins, N.A.; Copeland, N.G. KRAS-Related Proteins in Pancreatic Cancer. Pharmacol. Ther. 2016, 168, 29–42. [Google Scholar] [CrossRef]
- Zhu, G.; Pei, L.; Xia, H.; Tang, Q.; Bi, F. Role of Oncogenic KRAS in the Prognosis, Diagnosis and Treatment of Colorectal Cancer. Mol. Cancer 2021, 20, 143. [Google Scholar] [CrossRef]
- Takahara, M.; Kishibe, K.; Bandoh, N.; Nonaka, S.; Harabuchi, Y. P53, N- and K-Ras, and Beta-Catenin Gene Mutations and Prognostic Factors in Nasal NK/T-Cell Lymphoma from Hokkaido, Japan. Hum. Pathol. 2004, 35, 86–95. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, Y.; Zeng, S.; Hu, X. LMP1 Expression Is Positively Associated with Metastasis of Nasopharyngeal Carcinoma: Evidence from a Meta-Analysis. J. Clin. Pathol. 2012, 65, 41–45. [Google Scholar] [CrossRef]
- Dawson, C.W.; Laverick, L.; Morris, M.A.; Tramoutanis, G.; Young, L.S. Epstein-Barr Virus-Encoded LMP1 Regulates Epithelial Cell Motility and Invasion via the ERK-MAPK Pathway. J. Virol. 2008, 82, 3654–3664. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Shi, J.; Zhong, J.; Huang, Z.; Luo, X.; Huang, Y.; Feng, S.; Shao, J.; Liu, D. MiR-1, Regulated by LMP1, Suppresses Tumour Growth and Metastasis by Targeting K-Ras in Nasopharyngeal Carcinoma. Int. J. Exp. Pathol. 2015, 96, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Al-Sarraf, M.; LeBlanc, M.; Giri, P.G.; Fu, K.K.; Cooper, J.; Vuong, T.; Forastiere, A.A.; Adams, G.; Sakr, W.A.; Schuller, D.E.; et al. Chemoradiotherapy versus Radiotherapy in Patients with Advanced Nasopharyngeal Cancer: Phase III Randomized Intergroup Study 0099. J. Clin. Oncol. 1998, 16, 1310–1317. [Google Scholar] [CrossRef] [PubMed]
- Fuwa, N.; Kodaira, T.; Daimon, T.; Yoshizaki, T. The Long-Term Outcomes of Alternating Chemoradiotherapy for Locoregionally Advanced Nasopharyngeal Carcinoma: A Multiinstitutional Phase II Study. Cancer Med. 2015, 4, 1186–1195. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.-J.; Shi, L.-L.; Hong, X.-H.; Xiao, B.-Y.; Lin, G.-H.; Liu, Q.; Wang, B.-C. A Bayesian Network Meta-Analysis of the Primary Definitive Therapies for Locoregionally Advanced Nasopharyngeal Carcinoma: IC+CCRT, CCRT+AC, and CCRT Alone. PLoS ONE 2022, 17, e0265551. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.P.; Wen, Y.H.; Tang, J.; Wei, Y.; You, R.; Zhu, X.L.; Li, J.; Chen, L.; Ling, L.; Zhang, N.; et al. Endoscopic Surgery Compared with Intensity-Modulated Radiotherapy in Resectable Locally Recurrent Nasopharyngeal Carcinoma: A Multicentre, Open-Label, Randomised, Controlled, Phase 3 Trial. Lancet Oncol. 2021, 22, 381–390. [Google Scholar] [CrossRef]
- Chan, A.T.C.; Hui, E.P.; Ngan, R.K.C.; Tung, S.Y.; Cheng, A.C.K.; Ng, W.T.; Lee, V.H.F.; Ma, B.B.Y.; Cheng, H.C.; Wong, F.C.S.; et al. Analysis of Plasma Epstein-Barr Virus DNA in Nasopharyngeal Cancer After Chemoradiation to Identify High-Risk Patients for Adjuvant Chemotherapy: A Randomized Controlled Trial. J. Clin. Oncol. 2018, 36, 3091–3100. [Google Scholar] [CrossRef]
- Sorich, M.J.; Wiese, M.D.; Rowland, A.; Kichenadasse, G.; McKinnon, R.A.; Karapetis, C.S. Extended RAS Mutations and Anti-EGFR Monoclonal Antibody Survival Benefit in Metastatic Colorectal Cancer: A Meta-Analysis of Randomized, Controlled Trials. Ann. Oncol. 2015, 26, 13–21. [Google Scholar] [CrossRef]
- Liu, F.; Tai, Y.; Ma, J. LncRNA NEAT1/Let-7a-5p Axis Regulates the Cisplatin Resistance in Nasopharyngeal Carcinoma by Targeting Rsf-1 and Modulating the Ras-MAPK Pathway. Cancer Biol. Ther. 2018, 19, 534–542. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, Y.; Liu, L.; Su, H.; Dong, D.; Wang, J.; Zhang, Y.; Chen, Q.; Li, C. MicroRNA-19b Promotes Nasopharyngeal Carcinoma More Sensitive to Cisplatin by Suppressing KRAS. Technol. Cancer Res. Treat. 2018, 17, 1–8. [Google Scholar] [CrossRef]
- Zuo, Q.; Shi, M.; Chen, J.; Liao, W. The Ras Signaling Pathway Mediates Cetuximab Resistance in Nasopharyngeal Carcinoma. Biomed. Pharmacother. 2011, 65, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liang, R.; Zhu, X. Anti-EGFR Therapies in Nasopharyngeal Carcinoma. Biomed. Pharmacother. 2020, 131, 110649. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Hu, Q.; Li, H. Isoprenylcysteine Carboxylmethyltransferase Is Associated with Nasopharyngeal Carcinoma Chemoresistance and Ras Activation. Biochem. Biophys. Res. Commun. 2019, 516, 784–789. [Google Scholar] [CrossRef] [PubMed]
- McKenna, W.G.; Weiss, M.C.; Bakanauskas, V.J.; Sandler, H.; Kelsten, M.L.; Biaglow, J.; Tuttle, S.W.; Endlich, B.; Ling, C.C.; Muschel, R.J. The Role of the H-Ras Oncogene in Radiation Resistance and Metastasis. Int. J. Radiat. Oncol. Biol. Phys. 1990, 18, 849–859. [Google Scholar] [CrossRef]
- McKenna, W.; Weiss, M.; Endlich, B.; Ling, C.; Bakanauskas, V.; Kelsten, M.; Muschel, R.J. Synergistic Effect of the V-Myc Oncogene with H-Ras on Radioresistance. Cancer Res. 1990, 50, 97–102. [Google Scholar]
- Bernhard, E.; McKenna, W.; Hamilton, A.; Sebti, S.; Qian, Y.; Wu, J.; Muschel, R. Inhibiting Ras Prenylation Increases the Radiosensitivity of Human Tumor Cell Lines with Activating Mutations of Ras Oncogenes. Cancer Res. 1998, 58, 1754–1761. [Google Scholar]
- Hermens, A.; Bentvelzen, P.A. Influence of the H-Ras Oncogene on Radiation Responses of a Rat Rhabdomyosarcoma Cell Line. Cancer Res. 1992, 52, 3073–3082. [Google Scholar]
- Bernhard, E.; Stanbridge, E.; Gupta, S.; Gupta, A.; Soto, D.; Bakanauskas, V.; Cerniglia, G.J.; Muschel, R.; McKenna, W. Direct Evidence for the Contribution of Activated N-Ras and K-Ras Oncogenes to Increased Intrinsic Radiation Resistance in Human Tumor Cell Lines. Cancer Res. 2000, 60, 6597–6600. [Google Scholar]
- Kasid, U.; Pfeifer, A.; Brennan, T.; Beckett, M.; Weichselbaum, R.R.; Dritschilo, A.; Mark, G.E. Effect of Antisense C-Raf-1 on Tumorigenicity and Radiation Sensitivity of a Human Squamous Carcinoma. Science 1989, 243, 1354–1356. [Google Scholar] [CrossRef]
- Hagan, M.; Wang, L.; Hanley, J.; Park, J.; Dent, P. Ionizing Radiation-Induced Mitogen-Activated Protein (MAP) Kinase Activation in DU145 Prostate Carcinoma Cells: MAP Kinase Inhibition Enhances Radiation-Induced Cell Killing and G2/M-Phase Arrest. Radiat. Res. 2000, 153, 371–383. [Google Scholar] [CrossRef]
- Gupta, A.; Bernhard, E.; Bakanauskas, V.; Wu, J.; Muschel, R.; McKenna, W.G. RAS-Mediated Radiation Resistance Is Not Linked to MAP Kinase Activation in Two Bladder Carcinoma Cell Lines. Radiat. Res. 2000, 154, 64–72. [Google Scholar] [CrossRef]
- Ruan, L.; Wang, G.L.; Yi, H.; Chen, Y.; Tang, C.E.; Zhang, P.F.; Li, M.Y.; Li, C.; Peng, F.; Li, J.N.; et al. Raf Kinase Inhibitor Protein Correlates with Sensitivity of Nasopharyngeal Carcinoma to Radiotherapy. J. Cell. Biochem. 2010, 110, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Bakanauskas, V.; Cerniglia, G.; Cheng, Y.; Bernhard, E.J.; Muschel, R.; McKenna, W.G. The Ras Radiation Resistance Pathway. Cancer Res. 2001, 61, 4278–4282. [Google Scholar]
- Gupta, A.K.; McKenna, W.G.; Weber, C.N.; Feldman, M.D.; Goldsmith, J.D.; Mick, R.; Machtay, M.; Rosenthal, D.I.; Ba-kanauskas, V.J.; Cerniglia, G.J.; et al. Local Recurrence in Head and Neck Cancer: Relationship to Radiation Resistance and Signal Transduction. Clin. Cancer Res. 2002, 8, 885–892. [Google Scholar] [PubMed]
- Liu, T.; Sun, Q.; Li, Q.; Yang, H.; Zhang, Y.; Wang, R.; Lin, X.; Xiao, D.; Yuan, Y.; Chen, L.; et al. Dual PI3K/MTOR Inhibitors, GSK2126458 and PKI-587, Suppress Tumor Progression and Increase Radiosensitivity in Nasopharyngeal Carcinoma. Mol. Cancer Ther. 2015, 14, 429–439. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Li, Y.; Lu, Y.; Huang, J.; Ren, J.; Zhang, S.; Yin, Z.; Huang, K.; Wu, G.; Yang, K. LZTS2 Inhibits PI3K/AKT Activation and Radioresistance in Nasopharyngeal Carcinoma by Interacting with P85. Cancer Lett. 2018, 420, 38–48. [Google Scholar] [CrossRef]
- Cohen-Jonathan, E.; Evans, S.; Koch, C.; Muschel, R.; McKenna, W.; Wu, J.; Bernhard, E. The Farnesyltransferase Inhibitor L744,832 Reduces Hypoxia in Tumors Expressing Activated H-Ras. Cancer Res. 2001, 61, 2289–2293. [Google Scholar]
- Choi, D.-S.; Kim, D.-K.; Kim, Y.-K.; Gho, Y.S. Proteomics of Extracellular Vesicles: Exosomes and Ectosomes. Mass Spectrom. Rev. 2015, 34, 474–490. [Google Scholar] [CrossRef]
- Lee, M.-J.; Park, D.-H.; Kang, J.-H. Exosomes as the Source of Biomarkers of Metabolic Diseases. Ann. Pediatr. Endocrinol. Metab. 2016, 21, 119. [Google Scholar] [CrossRef]
- van der Pol, E.; Böing, A.N.; Harrison, P.; Sturk, A.; Nieuwland, R. Classification, Functions, and Clinical Relevance of Extracellular Vesicles. Pharmacol. Rev. 2012, 64, 676–705. [Google Scholar] [CrossRef]
- Properzi, F.; Logozzi, M.; Fais, S. Exosomes: The Future of Biomarkers in Medicine. Biomark. Med. 2013, 7, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Raimondo, S.; Corrado, C.; Raimondi, L.; de Leo, G.; Alessandro, R. Role of Extracellular Vesicles in Hematological Malignancies. BioMed Res. Int. 2015, 2015, 821613. [Google Scholar] [CrossRef] [PubMed]
- Ceccarelli, S.; Visco, V.; Raffa, S.; Wakisaka, N.; Pagano, J.S.; Torrisi, M.R. Epstein-Barr Virus Latent Membrane Protein 1 Promotes Concentration in Multivesicular Bodies of Fibroblast Growth Factor 2 and Its Release through Exosomes. Int. J. Cancer 2007, 121, 1494–1506. [Google Scholar] [CrossRef] [PubMed]
- Nanbo, A.; Kawanishi, E.; Yoshida, R.; Yoshiyama, H. Exosomes Derived from Epstein-Barr Virus-Infected Cells Are Internalized via Caveola-Dependent Endocytosis and Promote Phenotypic Modulation in Target Cells. J. Virol. 2013, 87, 10334–10347. [Google Scholar] [CrossRef]
- Meckes, D.G.; Gunawardena, H.P.; Dekroon, R.M.; Heaton, P.R.; Edwards, R.H.; Ozgur, S.; Griffith, J.D.; Damania, B.; Raab-Traub, N. Modulation of B-Cell Exosome Proteins by Gamma Herpesvirus Infection. Proc. Natl. Acad. Sci. USA 2013, 110, E2925–E2933. [Google Scholar] [CrossRef]
- Aga, M.; Bentz, G.L.; Raffa, S.; Torrisi, M.R.; Kondo, S.; Wakisaka, N.; Yoshizaki, T.; Pagano, J.S.; Shackelford, J. Exosomal HIF1α Supports Invasive Potential of Nasopharyngeal Carcinoma-Associated LMP1-Positive Exosomes. Oncogene 2014, 33, 4613–4622. [Google Scholar] [CrossRef]
- Tanaka, T.; Ikegami, Y.; Nakazawa, H.; Kuriyama, N.; Oki, M.; Hanai, J.; Sukhatme, V.P.; Kaneki, M. Low-Dose Farnesyltransferase Inhibitor Suppresses HIF-1α and Snail Expression in Triple-Negative Breast Cancer MDA-MB-231 Cells In Vitro. J. Cell. Physiol. 2017, 232, 192–201. [Google Scholar] [CrossRef]
- Wakisaka, N.; Kondo, S.; Yoshizaki, T.; Murono, S.; Furukawa, M.; Joseph, S.; Pagano, J.S. Epstein-Barr Virus Latent Mem-brane Protein 1 Induces Synthesis of Hypoxia-Inducible Factor 1 α. Mol. Cell. Biol. 2004, 24, 5223–5234. [Google Scholar] [CrossRef]
- Horikawa, T.; Yoshizaki, T.; Kondo, S.; Furukawa, M.; Kaizaki, Y.; Pagano, J.S. Epstein-Barr Virus Latent Membrane Pro-tein 1 Induces Snail and Epithelial-Mesenchymal Transition in Metastatic Nasopharyngeal Carcinoma. Br. J. Cancer 2011, 104, 1160–1167. [Google Scholar] [CrossRef]
- Sinensky, M.; Beck, L.; Leonard, S.; Evans, R. Differential Inhibitory Effects of Lovastatin on Protein Isoprenylation and Sterol Synthesis. J. Biol. Chem. 1990, 265, 19937–19941. [Google Scholar] [CrossRef]
- Macdonald, J.S.; McCoy, S.; Whitehead, R.P.; Iqbal, S.; Wade, J.L.; Giguere, J.K.; Abbruzzese, J.L. A Phase II Study of Farnesyl Transferase Inhibitor R115777 in Pancreatic Cancer: A Southwest Oncology Group (SWOG 9924) Study. Investig. New Drugs 2005, 23, 485–487. [Google Scholar] [CrossRef]
- James, G.L.; Goldstein, J.L.; Brown, M.S. Polylysine and CVIM Sequences of K-RasB Dictate Specificity of Prenylation and Confer Resistance to Benzodiazepine Peptidomimetic In Vitro. J. Biol. Chem. 1995, 270, 6221–6226. [Google Scholar] [CrossRef]
- Fiordalisi, J.J.; Johnson, R.L.; Weinbaum, C.A.; Sakabe, K.; Chen, Z.; Casey, P.J.; Cox, A.D. High Affinity for Farnesyltransferase and Alternative Prenylation Contribute Individually to K-Ras4B Resistance to Farnesyltransferase Inhibitors. J. Biol. Chem. 2003, 278, 41718–41727. [Google Scholar] [CrossRef]
- Whyte, D.B.; Kirschmeier, P.; Hockenberry, T.N.; Nunez-Oliva, I.; James, L.; Catino, J.J.; Bishop, W.R.; Pai, J.K. K- and N-Ras Are Geranylgeranylated in Cells Treated with Farnesyl Protein Transferase Inhibitors. J. Biol. Chem. 1997, 272, 14459–14464. [Google Scholar] [CrossRef]
- Rowell, C.A.; Kowalczyk, J.J.; Lewis, M.D.; Garcia, A.M. Direct Demonstration of Geranylgeranylation and Farnesylation of Ki-Ras In Vivo. J. Biol. Chem. 1997, 272, 14093–14097. [Google Scholar] [CrossRef]
| Proteins | Functions |
|---|---|
| H-, K-, N-RAS | GTPase, signal transduction |
| Rho | GTPase, signal transduction |
| Rheb | GTPase, signal transduction |
| PRL family | Tyrosine phosphatase |
| CENP-E | Kinesin motor protein |
| CENP-F | Chromosome passenger |
| HDJ | Cochaperone |
| Nuclar lamins | Nuclear envelope protein |
| UCH-L1 | De-ubiquitinating enzyme |
| IDs on ClinicalTrials.gov (accessed on 29 May 2022) | Phase | Agents | Tumor Types | References |
|---|---|---|---|---|
| NCT02383927 | Phase 2 | Tipifarnib | HNSCCs with H-ras mutations | [39] |
| NCT03719690 | Phase 2 | Tipifarnib | HNSCCs with H-ras mutations | Ongoing trial |
| NCT04997902 | Phase 1/2 | Tipifarnib with Alpelisib | PI3KCA or H-ras-dependent R/M HNSCCs | Ongoing trial |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kobayashi, E.; Kondo, S.; Dochi, H.; Moriyama-Kita, M.; Hirai, N.; Komori, T.; Ueno, T.; Nakanishi, Y.; Hatano, M.; Endo, K.; et al. Protein Farnesylation on Nasopharyngeal Carcinoma, Molecular Background and Its Potential as a Therapeutic Target. Cancers 2022, 14, 2826. https://doi.org/10.3390/cancers14122826
Kobayashi E, Kondo S, Dochi H, Moriyama-Kita M, Hirai N, Komori T, Ueno T, Nakanishi Y, Hatano M, Endo K, et al. Protein Farnesylation on Nasopharyngeal Carcinoma, Molecular Background and Its Potential as a Therapeutic Target. Cancers. 2022; 14(12):2826. https://doi.org/10.3390/cancers14122826
Chicago/Turabian StyleKobayashi, Eiji, Satoru Kondo, Hirotomo Dochi, Makiko Moriyama-Kita, Nobuyuki Hirai, Takeshi Komori, Takayoshi Ueno, Yosuke Nakanishi, Miyako Hatano, Kazuhira Endo, and et al. 2022. "Protein Farnesylation on Nasopharyngeal Carcinoma, Molecular Background and Its Potential as a Therapeutic Target" Cancers 14, no. 12: 2826. https://doi.org/10.3390/cancers14122826
APA StyleKobayashi, E., Kondo, S., Dochi, H., Moriyama-Kita, M., Hirai, N., Komori, T., Ueno, T., Nakanishi, Y., Hatano, M., Endo, K., Sugimoto, H., Wakisaka, N., & Yoshizaki, T. (2022). Protein Farnesylation on Nasopharyngeal Carcinoma, Molecular Background and Its Potential as a Therapeutic Target. Cancers, 14(12), 2826. https://doi.org/10.3390/cancers14122826






