1. Introduction
Chemerin is a regulatory adipokine involved in energy metabolism, regulation of immune function, and other physiological processes such as chemotaxis, differentiation, and proliferation. It exerts its action via its G protein-coupled receptors chemokine-like receptor 1 (CMKLR1), G protein-coupled receptor 1 (GPR1), and C-C chemokine receptor-like 2 CCRL2 [
1,
2]. Both clinical, as well as animal studies, have clearly demonstrated that secretion and systemic levels of chemerin rise with overweight and adiposity, and decline after diet, exercise-based weight loss, and bariatric surgery [
3,
4,
5,
6]. Chemerin has been shown to promote the chemotaxis of macrophages and NK cells and to enhance the migration of plasmacytoid dendritic cells [
7,
8,
9]. As a chemoattractant in inflammation, chemerin was reported to exert action on NF-κB signaling, thereby promoting pro-inflammatory, but also anti-inflammatory activities [
10,
11,
12]. In hypertension, chemerin protein levels are elevated, and experimental studies support the role of chemerin in the control of blood pressure, while inhibition of angiotensin-I-converting enzyme lowers chemerin serum levels [
13,
14,
15,
16,
17].
Chemerin has also been associated with several functions of tumor progression, such as growth, invasion, metastasis, recruitment of immunocytes, and formation of new vessels [
18,
19]. In a seminal paper, Pachynski et al. found chemerin to suppress melanoma by recruiting natural killer cells [
20]. In a chemically induced model of skin cancer, the expression of chemerin by keratinocytes has been demonstrated to block the distal phase of tumorigenesis [
21]. Similarly, chemerin was found to counteract tumor progression in hepatocellular carcinoma (HCC) by suppressing IL-6 and GM-CSF expression. Further, it inhibits metastasis in HCC along a signaling pathway via CMKLR1, PTEN, and Akt [
22,
23]. Among patients with HCC, diminished chemerin biosynthesis has been attributed to poor prognosis as well as lowered infiltration of NK cells and dendritic cells [
24]. Notwithstanding antitumor action by chemerin has been reported in a number of cancer types, there are also reports about tumor-enhancing functions. In neuroblastoma cells, inhibition of chemerin-induced CMKLR1 signaling was found to reduce clonal growth and cellular viability in vitro and to inhibit tumor growth in animal experiments [
25]. Likewise, chemerin signals via CMKLR1 and GPR1 to enhance migratory activity and invasion of gastric cancer cells [
26].
Regarding colorectal carcinoma (CRC), chemerin plasma concentration was found to be associated with the risk of incident CRC and to be independent of established CRC risk factors [
27,
28]. In addition, serum chemerin levels turned out to be positively associated with the presence of colorectal adenoma in men [
29]. Furthermore, chemerin receptor CMKLR1 was detected at higher abundance in CRC tumor tissues than in margins [
30].
So far, however, the potential regulation of CRC tumorigenesis and progression has not been investigated in an experimental setting. Recently, our group has reported the development of the metabolically stable high-affinity chemerin peptide agonist CG34 that potently activates both CMKLR1 as well as GPR1. Chelator-linked and radionuclide-loaded CG34 was able to detect via PET/MRI imaging breast cancer in a mouse model that used xenografts of the endogenously CMKLR1-expressing human cell line DU4475 [
31].
In this study, the chemerin analog CG34 was used to investigate the possible regulation of three human CRC cell line models in vitro with regard to proliferation, colony formation, and migration. In addition, CG34 was utilized to study the influence of chemerin receptor signaling on growth and vascularization in two human CRC cell xenograft mouse models. The results of this study represent the first indication of a tumor growth-stimulating effect of chemerin signaling in CRC.
2. Materials and Methods
2.1. Reagents and Cell Culture
The luciferase-expressing cell lines HCT116-luc and HT29-luc were purchased from Caliper (Hopkinton, MA, USA). The cell line SW620-luc cell line was created by transduction in our laboratory. All other cell lines were purchased from ATCC/LGC Standards (Wesel, Germany) or CLS (Eppenheim, Germany). The cell lines were cultured in RPMI 1640 medium (Biochrom AG, Berlin, Germany) or McCoy’s 5A modified medium (Biochrom AG, Berlin, Germany), each supplemented with 10% fetal calf serum (Biochrom AG, Berlin, Germany). All tumor cell lines were cultured in an incubator (Labotect, Rosdorf, Germany) providing a humidified atmosphere at 37 °C with 5% CO2. Cells were passaged every 2–3 days.
2.2. RNA Isolation, Transcription, and RT-qPCR
The preparation of RNA for RT-qPCR experiments was performed according to the manufacturer’s instructions using the RNeasy Plus Mini Kit (Qiagen, Hilden, Germany). Isolated RNA was transcribed into cDNA using the High Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Darmstadt, Germany). For this, 3.2 µg of RNA was transcribed into 80 µL of cDNA (final concentration: 40 ng/µL) according to the manufacturer’s protocol. In addition, as a negative control for each sample, a preparation without reverse transcriptase was analyzed in RT-qPCR. Quantitative real-time human-specific primer sets for TaqMan and CyberGreen amplifications were obtained from Life Technologies (Darmstadt, Germany), SIGMA (Deisenhofen, Germany), or Roche (Mannheim, Germany). Primer sequences, or product numbers, are provided in
Table 1. The Fast Start TaqMan
® Probe Master Kit (Roche) additionally contains Taq DNA Polymerase, reaction buffer, and nucleotides (dATP, dCTP, dGTP, dUTP). For CyberGreen-based PCR, Sso Fast EvaGreen Supermix (Bio-Rad, Düsseldorf, Germany) was used. PCR was performed using the CFX96 real-time system (Bio-Rad). For this purpose, 30 ng of cDNA were added. The analysis was performed using qBase PLUS (Biogazelle, Zwijnaarde, Belgium) according to the ∆∆Ct-method. As multiple reference genes were included in the normalization, the geometric mean of the relative housekeeping expression was first determined and then this value was used to normalize the target gene expression. Subsequently, these data were normalized to a cq value of 34.
2.3. Chemerin ELISA
For the detection of chemerin in cell culture supernatants, ELISA kits from DRG Instruments (Marburg, Germany) were used. Cells were incubated in a full medium at a density of approximately 70% for 24 h; supernatants were immediately used for ELISA or frozen at −80 °C. The ELISA was performed according to the manufacturer’s protocol with the supplied standards. MaxiSorp 96-well plates (Nunc, Thermo Fisher Scientific, Dreieich, Germany) were used. The measurement was performed in the SpectramaxPlus384 reader (Molecular Devices, Biberach an der Riß, Germany) at 650 nm (before the addition of the stop solution) or 450 nm (after addition of the stop solution) and the concentration was determined based on the standard curve using SoftMax Pro 5.3.
2.4. Proliferation Assay Using DAPI Staining of Nuclei
After reaching a confluence level of 60–70%, cells were trypsinized (trypsin/EDTA solution, Biochrom AG, Berlin, Germany) and seeded onto a 96-well plate with transparent, microscopy grade bottom (Becton Dickinson, Heidelberg, Germany). Cell seeding was then performed by pipetting 100 µL containing 10,000 cells per well.
At 1 h after cell seeding, the substances to be tested, including negative controls (medium containing 1.6%, 0.8% or 0.6% FCS for HCT116-luc, HT29-luc, and SW620-luc, respectively, and positive controls (medium containing 10% FCS) were added to the cells in a volume of 100 µL per well. The chemerin analog CG34 (final concentration 10 µM) was diluted in the medium corresponding to the negative controls, as stated above. To avoid loss of substance activity over time, a medium with or without compound was exchanged every 24 h.
After 96 h, cells were fixed for 10 min in a PBS-buffered 4% PFA solution (Herbeta Arzneimittel, Berlin, Germany) pipetted directly into the medium. Then, cells were subjected to 10 min of incubation with 5 µg/mL DAPI (Sigma-Aldrich, Munich, Germany) and 0.1% Triton (Merck, Darmstadt, Germany) in PBS. Plates were washed 2 times with PBS. After the last wash, PBS was left on the plate. The plate was covered with a transparent foil and stored at 4 °C until measurement. The number of nuclei was determined using high-content analysis with the IN Cell Analyzer automated microscope (GE Healthcare, Reading, UK). Data are reported as relative cell numbers in % of the positive control.
2.5. Proliferation Assay Using Bright-Field Microscopy of Growing Cells
After reaching a confluence level of 60–70%, cells were trypsinized and seeded onto a 96-well standard cell culture plate (Sarstedt, Nümbrecht, Germany). Cell seeding was then performed done by pipetting 100 µL each with 10,000 cells per well. Directly after cell seeding, 100 µL per well of RPMI1640 with 10% FCS containing the chemerin analog CG34 were added to the cells. As negative controls, other wells were incubated in RPMI1640 with 10% FCS only. Plates were then placed for up to five days into an automated microscopy system (Incucyte S3, Essen Bioscience, Göttingen, Germany). Bright-field images of each well were taken every two hours. To avoid loss of substance activity over time, a medium with or without compound was exchanged every 48 h. Using the Incucyte software, cell confluence was determined by an adapted segmentation algorithm. Using kinetic confluency data, the rate constant k for cell growth up to three days after seeding was calculated using the exponential growth equation (Y = Y0 × exp(k × X) in GraphPad Prism 7.0 (GraphPad Software, San Diego, CA, USA).
2.6. Colony Formation Assay
Cells were seeded in a flask and incubated for 3 days until reaching 70% confluence. Cells were then trypsinized, suspended in serum-free RPMI1640 medium, and counted using a Neubauer counting chamber. Four ml of a cell suspension containing 30,000 cells per 1 mL of FCS-free medium were prepared. In parallel, a sterile β-mercaptoethanol solution was prepared (5 µL of 2-mercaptoethanol (Sigma-Aldrich, Munich, Germany)) in 8.45 mL of PBS. In addition, methylcellulose aliquots (Sigma-Aldrich, Munich, Germany) were pre-warmed at 37 °C. Under sterile conditions, a mixture of 3.6 mL of methylcellulose, 2.7 mL of FCS, 60 µL of mercaptoethanol solution, 770 µL of Iscove’s medium (Biochrom AG, Berlin, Germany), and 300 µL of the cell suspension was prepared in a tube. The tube was shaken vigorously for approximately 5 min until the preparation took on a pink color. Then, 1.63 mL of agar previously boiled in the microwave and dissolved in the serum-free medium were added to the batch, shaken vigorously repeatedly, and placed in the cell incubator for 20 min. After the incubation period had elapsed, 1 mL of the resulting cell mixture was spread evenly on a gridded 3.5-cm cell culture dish using an insulin syringe, taking care to prevent the formation of air bubbles. For both CG34 treatments as well as the medium control, three small cell culture dishes (2 mm grid, Nalge Nunc International, Rochester, NY, USA) were filled with the cell preparation and placed in a large cell culture dish, which was previously loaded with a small dish filled with PBS to prevent the preparation from drying out. The next day, each cell batch was treated with 100 µL of the substance to be tested for stimulation of colony formation. The negative control consisted of the equivalent treatment with 100 µL of medium containing a concentration of FCS specified for the cell line under investigation (see DAPI assay). CG34 was diluted (100 nM) in the medium of the FCS concentration corresponding to the negative control. Subsequently, compound or negative control additions were made once daily, with only 10 µL added to each batch. The large cell culture dishes containing the preparations were incubated in an incubator for 7 days. On the last day of the experiment, tumor cell colonies were manually counted at a defined size of at least 20 cells per colony under a bright-field microscope at 40× magnification. Data are reported as relative cell numbers in % of the negative control.
2.7. Migration Assay
After reaching a confluence level of 80–90%, cells were trypsinized and seeded in a 96-well standard cell culture plate (Sarstedt, Nümbrecht, Germany). Cell seeding was then performed done by pipetting 100 µL of RPMI1640 with 10% FCS with 75,000 cells per well. The next day, cell monolayers were treated with a 96-head scratch tool. Cells were washed once with a medium. Thereafter, 200 µL per well of RPMI1640 with 10% FCS containing the chemerin analog CG34 (10 µM) was added to the cells. As negative controls, other wells were incubated in RPMI1640 with 10% FCS only. Plates were then placed into an automated microscopy system (Incucyte S3, Essen Bioscience, Göttingen, Germany) for up to 24 h. Using the Incucyte software, the % relative change in wound density from 8 to 20 h after compound addition was determined by an adapted segmentation algorithm.
2.8. Treatment Study
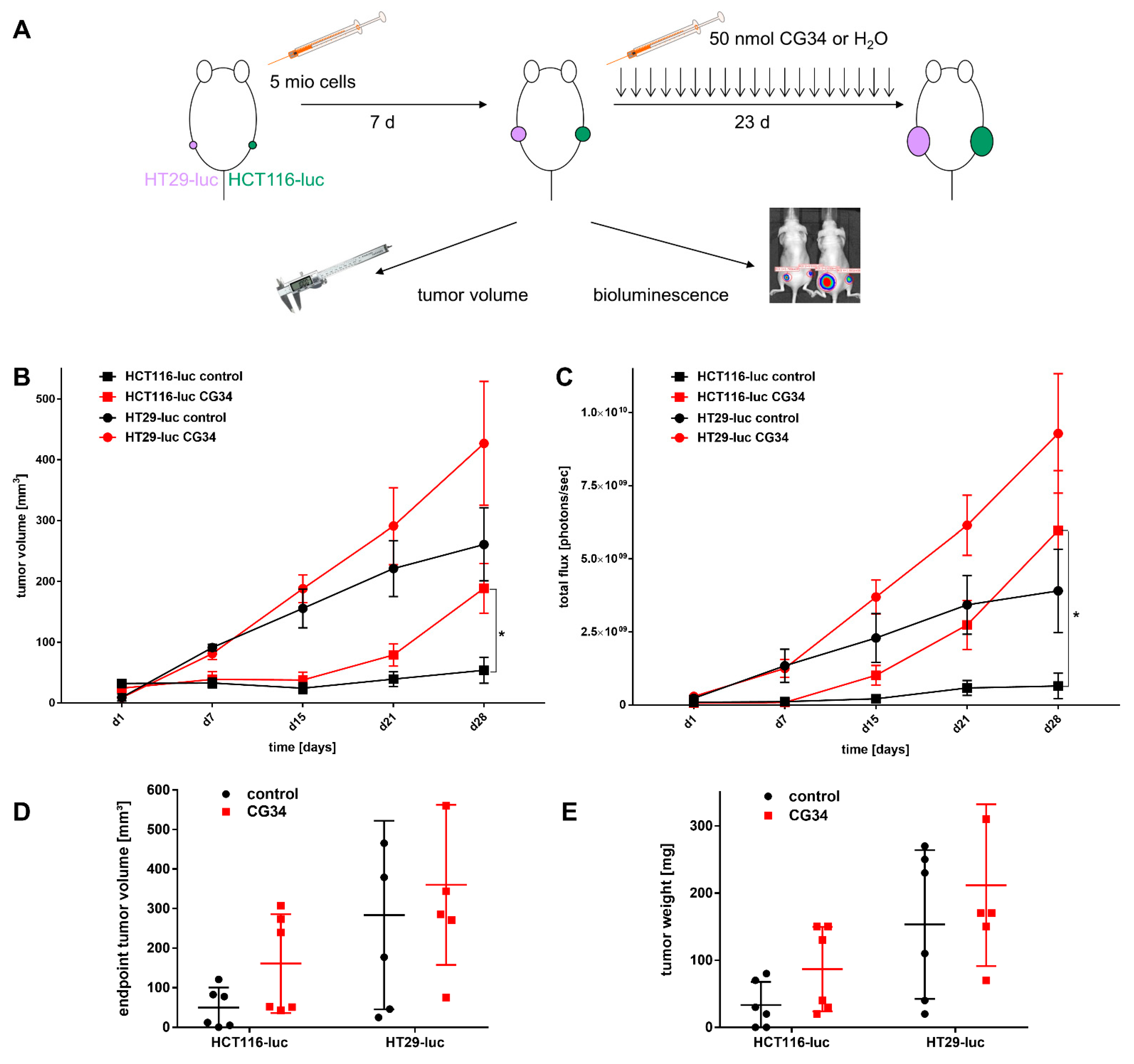
To analyze the potential tumor growth effect of CG34 in vivo, a treatment study was performed. Two luciferase-expressing xenograft mouse models for human colorectal carcinoma were used: HCT116-luc and HT29-luc. 12 female 8–10 weeks old NMRI nude mice were each implanted subcutaneously with 5 × 106 cells in 100 µL RPMI1640 each of the HT29-luc (left flank) or HCT116-luc (right flank). Tumor growth was monitored once weekly from the first day of the experiment using both caliper size measurements and bioluminescence imaging (IVIS Lumina, Caliper [Hopkinton, MA, USA]). On the seventh day, the 12 animals were randomized into two groups with six animals per group. Treatment was started on day eight of the experiment and terminated on day 28. Treatment was administered in a blinded manner (the investigators did not know the assignment of groups until after evaluation), with one group receiving intraperitoneal injections of 200 µL of CG34 (50 nmol) per mouse once daily and the other group receiving equivalent treatment with 200 µL of water. After measuring the length and width of the tumors with a caliper, volume was calculated according to the formula v = 0.5 × (length × width2).
For bioluminescence imaging, each mouse received an intraperitoneal weight-adapted injection of D-luciferin (150 µL) at a dose of 150 µg/g mouse 5–10 min before imaging. Mice were then placed under isoflurane anesthesia and transferred to the imager, where bioluminescence signal detection took place. The exposure time was 1 min at the beginning for small tumors and would be reduced to a minimum of 10 s as the tumor size increased during the experiment. The Living Image 3.1 software (Caliper) was used to count the emitted photons, ultimately determining the photon yield in a region of interest corresponding to the tumor under investigation. In addition, animal weight was monitored twice a week. At the designated experimental endpoint, day 31, animals were anesthetized with isoflurane and euthanized by cervical dislocation. The endpoint tumor volume was determined using a caliper of tumors on sacrificed mice (length, width, and height at autopsy). In addition, the weight of the tumors obtained at autopsy was determined. The excised tumors were frozen in liquid nitrogen and stored at −80 °C.
2.9. CD31 Histology
To visualize tumor vascularization, immunohistochemical staining was performed using an antibody directed against the mouse endothelial cell surface molecule CD31 (JC70A, DAKO, Glostrup, Denmark). 10 µm-thick cryosections were fixed with 4% PFA solution for 20 min at room temperature. To block endogenous tissue peroxidases and prevent the nonspecific conversion of the dye AEC added later, sections were incubated with a 0.3% H2O2 solution for 10 min. Furthermore, an avidin-biotin blockade was performed using the avidin-biotin blocking kit (DAKO, Glostrup, Denmark). To eliminate nonspecific protein interactions with the primary antibody, sections were blocked with 2% skim milk for 30 min. Primary antibody was dissolved 1:50 in 0.1% BSA in PBS and incubated overnight at 4 °C in a humid chamber. As a negative control, the sections were incubated with only the 0.1% BSA solution instead of the primary antibody. In the second step, the biotinylated rabbit anti-rat secondary antibody (DAKO) was applied. After rinsing the sections with PBS, the avidin-biotin complex (Vector Labs, Burlingame, CA, USA) was added for 30 min. Freshly prepared AEC development buffer (50 mM acetate buffer, pH 5.0), AEC solution (Sigma-Aldrich, Munich, Germany), 30% H2O2) was pipetted onto the sections. The gradual red staining of mouse endothelial cells was followed under the microscope and stopped after 10 min by adding distilled water. Counterstaining with hematoxylin for 10 min was performed to better assess tissue structure. To determine the number of vessels in the tumors, 3 to 4 field-of-view images were taken per tumor preparation using a bright-field microscope at 200× objective magnification. In each field of view, the red-stained vessels were counted using ImageJ v145.
2.10. Ki67 Histology
To determine the fraction of proliferating tumor cells, immunohistochemical staining was done with an antibody against human Ki67 (M7240, DAKO). 10 µm-thick tumor cryosections were fixed with a 4% PFA solution. Further treatment of the slides was performed according to the protocol already described for CD31 staining. The anti-human Ki67 antibody was applied to the sections at a concentration of 0.0016 mg/mL. The primary antibody was pretreated with a biotinylation reagent (Animal Research Kit, DAKO) for 20 min. In addition, the primary antibody was mixed with a blocking reagent (DAKO) for 20 min before administration to the cryosections. After incubation overnight at 4 °C, the avidin-biotin complex was applied to the tumor tissue sections for 30 min, which was later developed with AEC. The applied staining reaction was stopped after complete red staining of the proliferating Ki67 containing tumor cells using distilled water. Counterstaining with hematoxylin was used to improve the identification of the non-proliferating tumor cells. Counting of Ki67-labeled cells in 3 to 4 fields of view imaged at 200× magnification was performed using the ImageJ v145.
4. Discussion
Chemerin has been demonstrated to be bound by and to activate two heptahelical plasma membrane receptors, CMKLR1 and GPR1, while a third, CCRL2, binds chemerin and is believed to pass on the ligand to the other receptors [
1,
2]. The expression of the three receptors has been revealed to some degree in healthy organs and tissues, where they act to transmit the various chemerin-mediated physiological functions from immune cell attraction to metabolic regulation [
32]. In cancer, however, the expression of CMKLR1, GPR1, and CCRL2 has not been studied to great extent. In CRC, CMKLR1 was discovered at higher abundance in CRC tumor tissues than in margins [
30]. In addition, CMKLR1 was found to correlate with GDF-15 and VEGF-A levels in CRC tumor-free margin [
33]. Our own previous report revealed CMKLR1 to be highly expressed in the breast cancer cell line DU4475 [
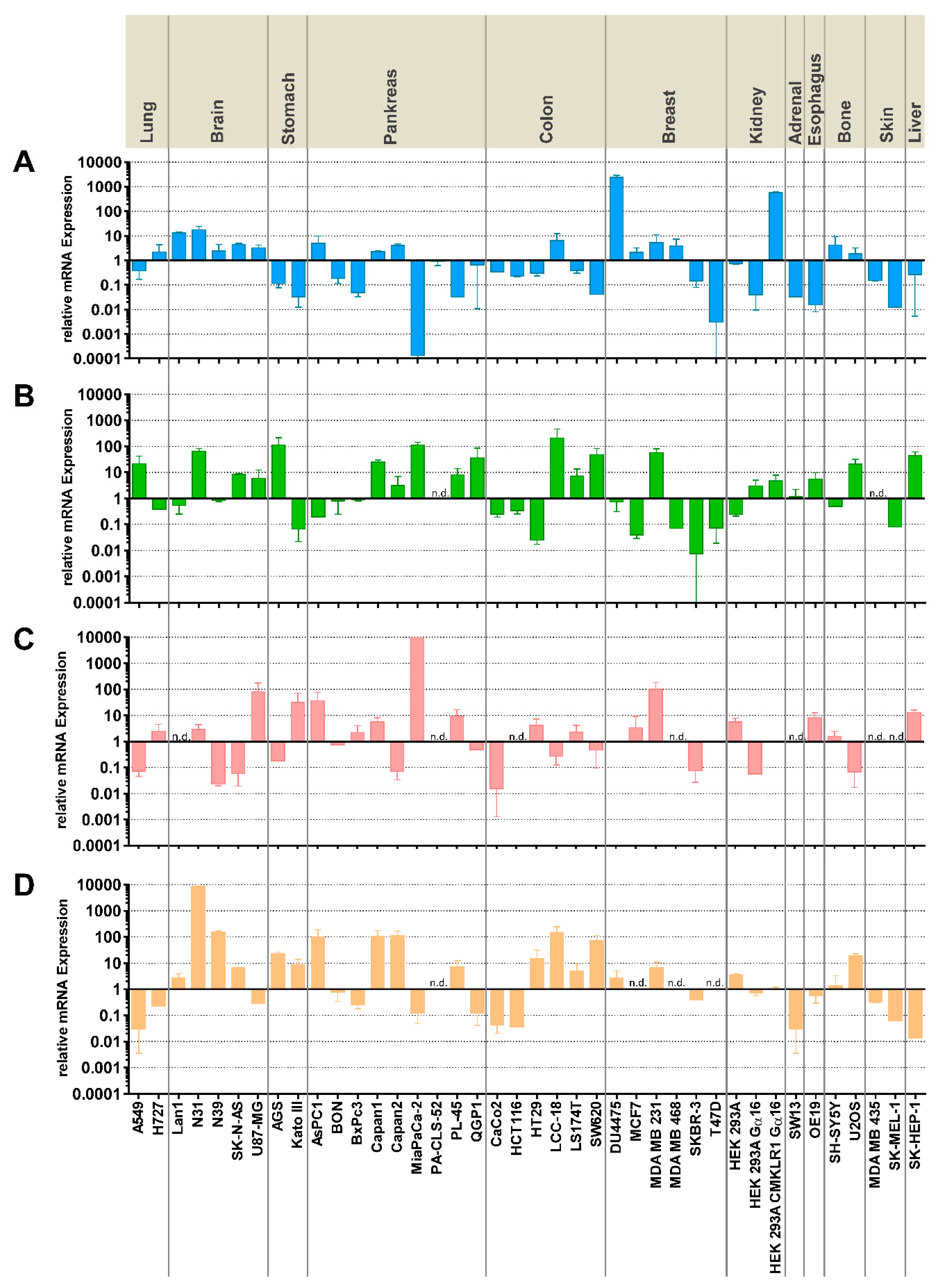
31]. The current study shows quantitative mRNA abundance data for five CRC and 35 other cell lines, revealing the complex and differential expression patterns that do not point to a particular, specific role for any of the receptors in one of the tumor entities under investigation. Rather, CMKLR1 and GPR1 expression levels vary across many orders of magnitude for most tumor types, while CCRL2 is completely missing from seven of the tested cancer cell lines (
Figure 1). While RT-qPCR is a highly specific and very sensitive analytical method to quantify the presence of mRNA, it has limited value in predicting protein levels, in particular with membrane proteins. It represents, therefore, a limitation of this study, that it does not provide evidence of receptor presence at the protein level. In CRC cell lines, the three cell lines HCT116, HT29, and SW620 represent the different expression patterns and were therefore selected for subsequent experiments.
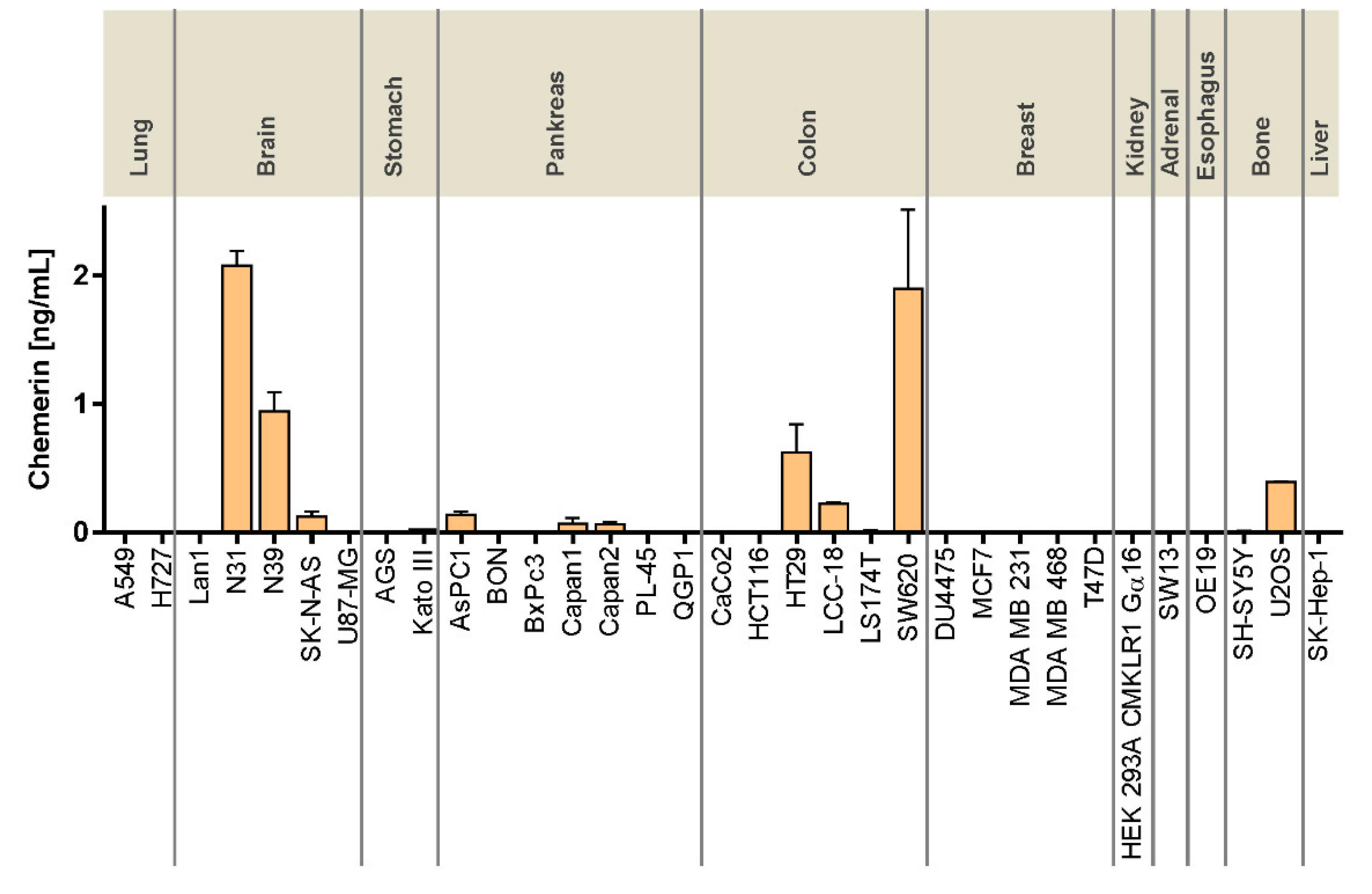
In contrast to the receptors, the ligand chemerin has been extensively characterized with regard to tumor expression and serum levels [
18,
19]. Most research, however, has been focusing on immune cells, cancer-associated fibroblasts, and other components of the tumor microenvironment as sources of chemerin secretion. This study demonstrated significant chemerin mRNA levels in cancer cell lines from the brain, stomach, pancreas, and colon (
Figure 1). Relevant chemerin concentrations in the supernatant of cultured cells, however, were only detected in two glioblastomas as well as in three CRC cell lines, potentially suggesting a role of tumor cell-produced chemerin in the biology of these cancer types. Tumor cells as a source of chemerin so far have been studied in the context of artificial overexpression or intratumoral injection of chemerin [
20,
34], while secretion from cell lines has not been studied so far, to the best of our knowledge.
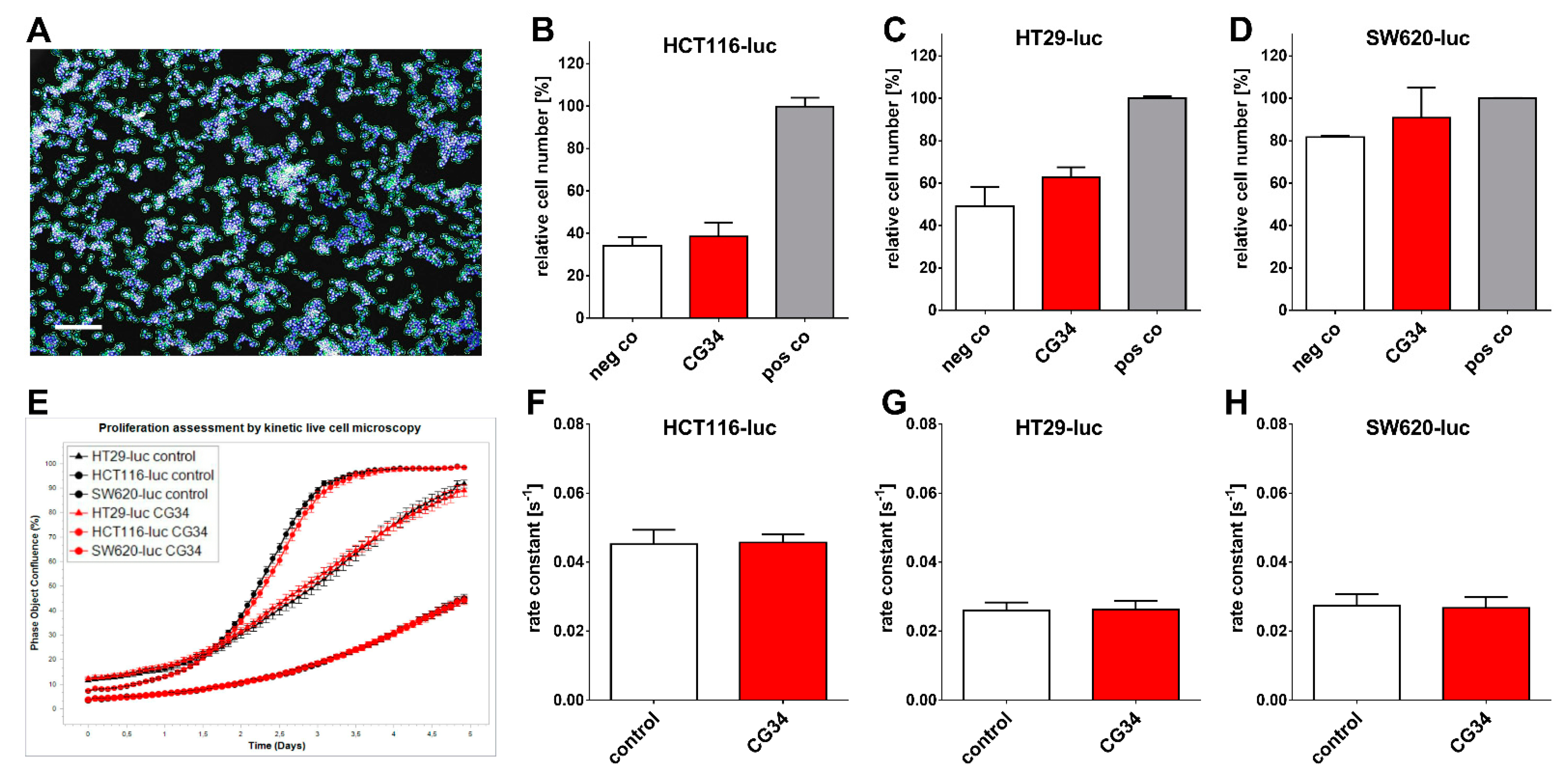
Several tumor types so far have been identified to feature a direct chemerin action on tumor cell proliferation and tumor growth, which may be either stimulating or inhibiting [
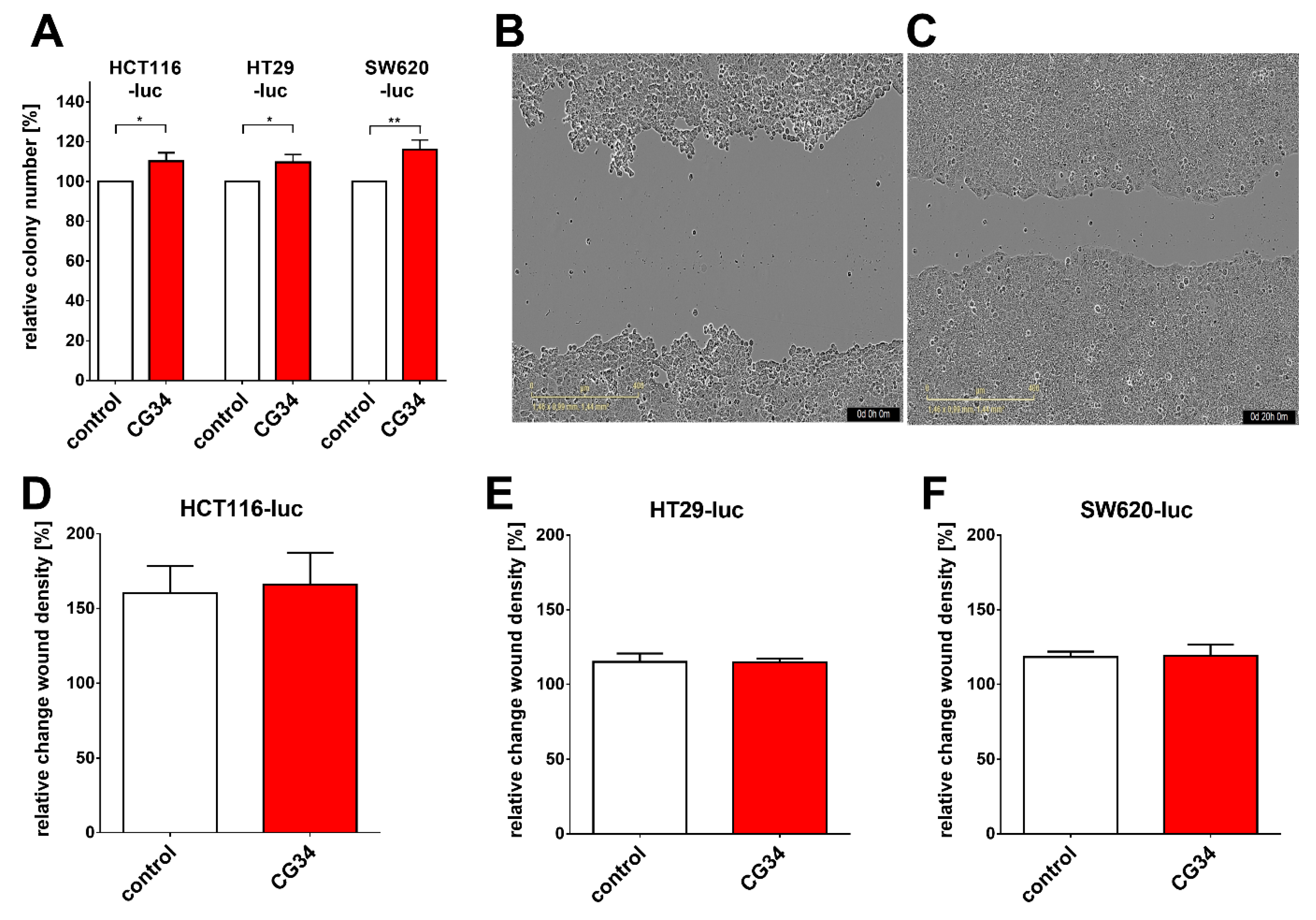
35]. In gastric cancer, e.g., chemerin was observed to stimulate carcinogenesis by inducing phosphorylation of p38 and ERK 1/2 MAPKs. This study did not find a clear stimulatory or inhibitory action of the chemerin analog CG34 on the three CRC cell lines HCT116-luc, HT29-luc, and SW620-luc when grown in a two-dimensional monolayer. However, when these cells were monitored for three-dimensional colony formation, CG34 significantly promoted growth in all three (
Figure 4A). While these results may appear contradictory, it is conceivable that the growth-enhancing effect of the chemerin analog depends on signaling only active in a three-dimensional cell context. It has been established that cells adapt to their environment by reacting to local signals, which in turn results in changes in cell proliferation and other physiological functions [
36]. Still, one limitation of this study is the lack of a mechanistic explanation for the differential regulation by chemerin in 2D versus 3D cultures. Further studies will have to elucidate the signaling processes involved in chemerin-induced enhancement of CRC cell colony formation.
Similar to its action on CRC cell colonies, CG34 clearly stimulated the growth of HCT116-luc as well as HT29-luc xenografts in a subcutaneous nude mouse model, as measured by tumor volume and bioluminescence intensity (
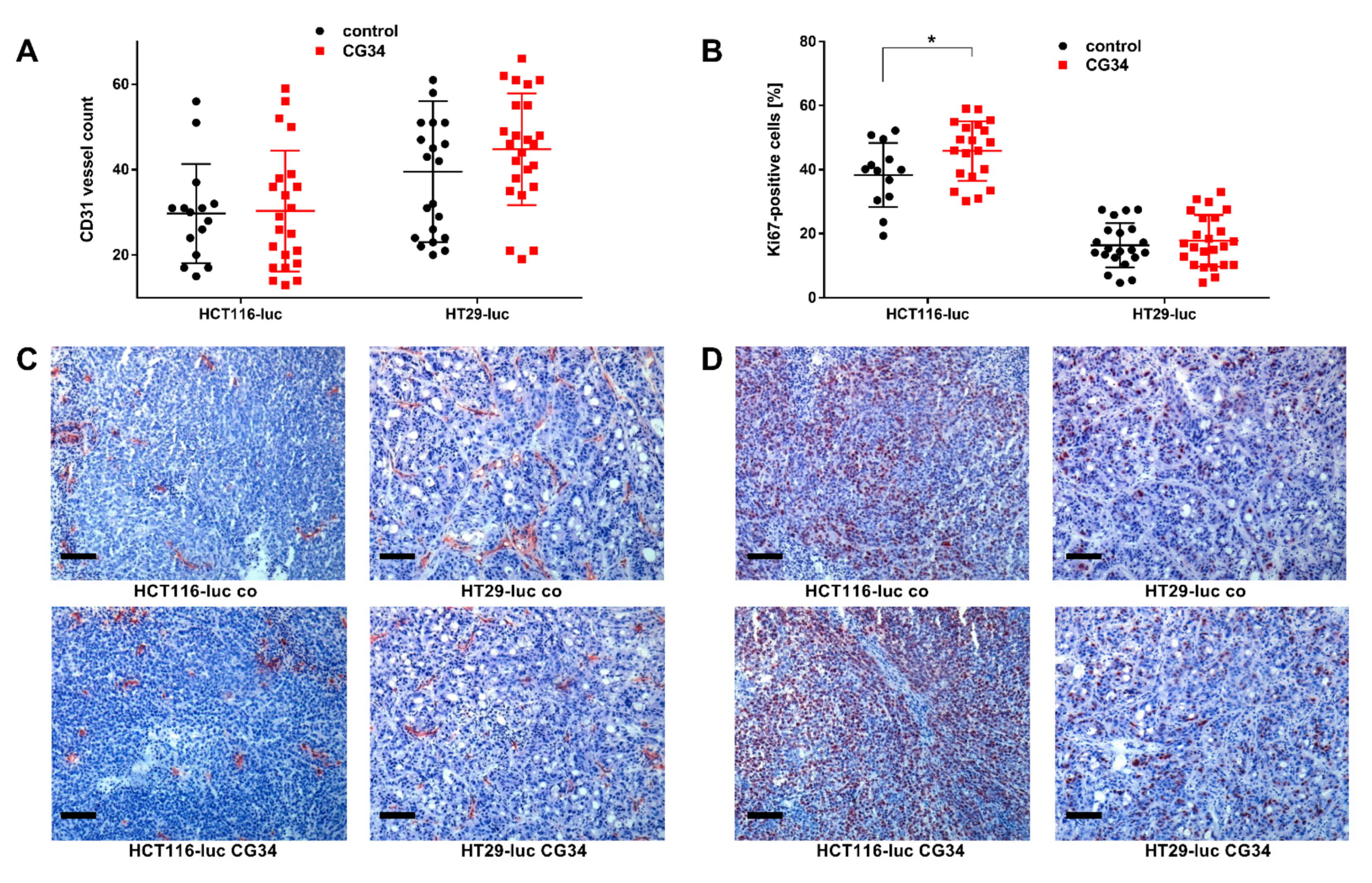
Figure 5). Statistical significance was found for differences between CG34-treated and control groups in HCT116-luc xenografts, while a high variance in values for HT29 precluded a statistically significant result. Similarly, tumor volume and weight were considerably increased. Statistical analysis found significance for the tumor volume differences between HCT116-luc cells treated with CG34 or control resulting from live measurement, but not for the corresponding values measured after the animals were sacrificed. The reason for this remains unclear and may be attributed to measurement error or imprecision. These results are indicative of a strong stimulatory function of chemerin signaling in CRC growth regulation. One of the potential influences of chemerin in regulating tumor growth that has been widely studied is its impact on the formation of new vessels [
18]. Ex-vivo analysis of tumors from the animal study demonstrated only a minor, non-significant enhancement of vessel density in HT29-luc xenografts of the CG34 treatment group versus control (
Figure 6A,C).
Though a correlation of chemerin levels and CRC risk has been established [
27,
28,
29], a regulatory effect has not been reported in the literature to date. Even though this study, hence, provides the first report of a chemerin agonist stimulating CRC in an animal model, it has a number of limitations. As the chemerin analog was administered systemically via a vein, this analysis cannot distinguish direct effects of CG34 on tumor cells from indirect regulation via immune cells, cancer-associated fibroblasts, or other cells of the tumor microenvironment. Indeed, indirect effects dominate in most reports on chemerin effects in cancers [
18,
19,
35]. It is, however, intriguing that both in in vitro colony formation as well as in the animal study, CG34 led to increased growth, potentially suggesting a direct effect of the analog on CRC cells. This is also supported by the detection of a statistically significant increase in the mitosis marker Ki67 in HCT116-luc xenografts of the CG34 treatment group versus tissues from the control group (
Figure 6B,D). Further studies will have to provide confirmation as well as clues about the exact molecular nature of this tumor-promoting activity.