The Current Landscape of Clinical Trials for Systemic Treatment of HCC
Abstract
Simple Summary
Abstract
1. Introduction
| Trial Name | Treatment Arms | Line of Therapy | Primary Endpoint | ORR | PFS | OS |
|---|---|---|---|---|---|---|
| SHARP [5] | Sorafenib vs. Placebo | First | OS | 2 vs. 1% | 5.5 vs. 2.8 months | 10.7 vs. 7.9 months (HR 0.69) |
| REFLECT [20] | Lenvatinib vs. Sorafenib | First | OS | 24.1 vs. 9.2% | 7.4 vs. 3.7 months | 13.6 vs. 12.3 months (HR 0.92) |
| IMbrave150 [25,26] | Atezolizumab+bevacizumab vs. sorafenib | First | OS and PFS | 29.8 vs. 11.3% | 6.8 vs. 4.3 months | 19.2 vs. 13.4 months (HR 0.66) |
| RESORCE [21] | Regorafenib vs. Placebo | Second | OS | 11 vs. 4% | 3.1 vs. 1.5 months | 10.6 vs. 7.8 months (HR 0.63) |
| CELESTIAL [22] | Cabozantinib vs. Placebo | Second and third | OS | 4 vs. 1% | 5.2 vs. 1.9 months | 10.2 vs. 8.0 months (HR 0.76) |
| REACH-2 [24] | Ramucirumab vs. Placebo (in patients with AFP > 400 ng/mL) | Second | OS | 5 vs. 1% | 2.8 vs. 1.6 months | 8.5 vs. 7.3 months (HR 0.71) |
| CHECKMATE 040 [16] | Nivolumab * single arm | Second | ORR | 15% | N/A | N/A |
| KEYNOTE 224 [17] | Pembrolizumab * single arm | Second | ORR | 17% | N/A | N/A |
| CHECKMATE 040 [27] | Nivolumab + ipilimumab * single arm | Second | ORR | 32% | N/A | N/A |
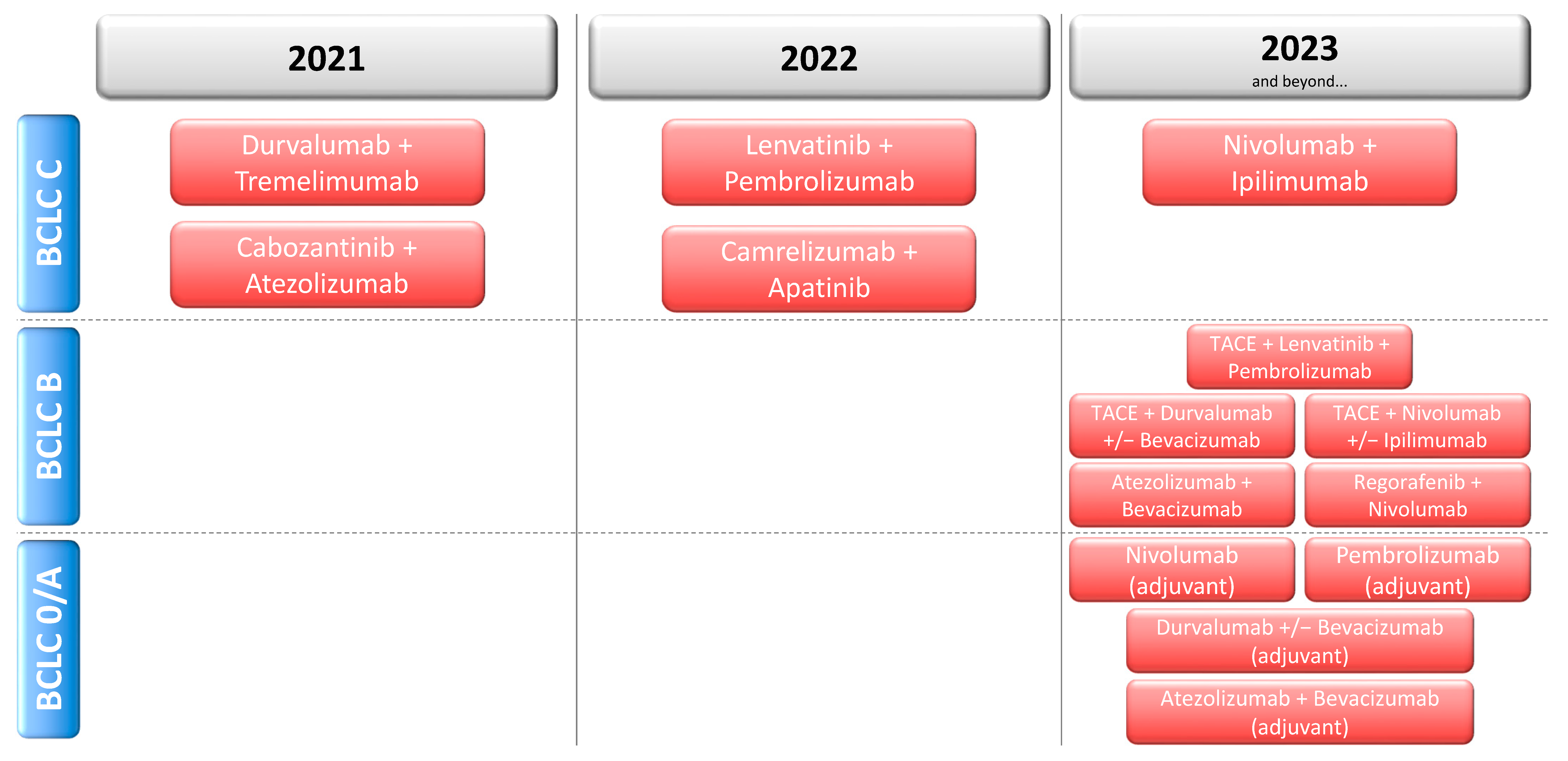
2. Systemic Treatment in the First- and Second-Line for Advanced HCC
3. Systemic Treatment for Intermediate HCC
4. Adjuvant Systemic Treatment
5. Neoadjuvant Systemic Treatment
6. Systemic Treatment beyond Immune Checkpoint Inhibition
7. Outlook and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- European Association For The Study Of The Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Kulik, L.M.; Finn, R.S.; Sirlin, C.B.; Abecassis, M.M.; Roberts, L.R.; Zhu, A.X.; Murad, M.H.; Marrero, J.A. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018, 67, 358–380. [Google Scholar] [CrossRef]
- Finn, R.S.; Zhu, A.X. Evolution of Systemic Therapy for Hepatocellular Carcinoma. Hepatology 2020. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Villanueva, A.; Marrero, J.A.; Schwartz, M.; Meyer, T.; Galle, P.R.; Lencioni, R.; Greten, T.F.; Kudo, M.; Mandrekar, S.J.; et al. Trial Design and Endpoints in Hepatocellular Carcinoma: AASLD Consensus Conference. Hepatology 2020. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Ricci, S.; Mazzaferro, V.; Hilgard, P.; Gane, E.; Blanc, J.F.; de Oliveira, A.C.; Santoro, A.; Raoul, J.L.; Forner, A.; et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008, 359, 378–390. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.J.; Qin, S.; Park, J.W.; Poon, R.T.; Raoul, J.L.; Philip, P.A.; Hsu, C.H.; Hu, T.H.; Heo, J.; Xu, J.; et al. Brivanib versus sorafenib as first-line therapy in patients with unresectable, advanced hepatocellular carcinoma: Results from the randomized phase III BRISK-FL study. J. Clin. Oncol. 2013, 31, 3517–3524. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Decaens, T.; Raoul, J.L.; Boucher, E.; Kudo, M.; Chang, C.; Kang, Y.K.; Assenat, E.; Lim, H.Y.; Boige, V.; et al. Brivanib in patients with advanced hepatocellular carcinoma who were intolerant to sorafenib or for whom sorafenib failed: Results from the randomized phase III BRISK-PS study. J. Clin. Oncol. 2013, 31, 3509–3516. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.L.; Kang, Y.K.; Lin, D.Y.; Park, J.W.; Kudo, M.; Qin, S.; Chung, H.C.; Song, X.; Xu, J.; Poggi, G.; et al. Sunitinib versus sorafenib in advanced hepatocellular cancer: Results of a randomized phase III trial. J. Clin. Oncol. 2013, 31, 4067–4075. [Google Scholar] [CrossRef] [PubMed]
- Cainap, C.; Qin, S.; Huang, W.T.; Chung, I.J.; Pan, H.; Cheng, Y.; Kudo, M.; Kang, Y.K.; Chen, P.J.; Toh, H.C.; et al. Linifanib versus Sorafenib in patients with advanced hepatocellular carcinoma: Results of a randomized phase III trial. J. Clin. Oncol. 2015, 33, 172–179. [Google Scholar] [CrossRef]
- Zhu, A.X.; Rosmorduc, O.; Evans, T.R.; Ross, P.J.; Santoro, A.; Carrilho, F.J.; Bruix, J.; Qin, S.; Thuluvath, P.J.; Llovet, J.M.; et al. SEARCH: A phase III, randomized, double-blind, placebo-controlled trial of sorafenib plus erlotinib in patients with advanced hepatocellular carcinoma. J. Clin. Oncol. 2015, 33, 559–566. [Google Scholar] [CrossRef]
- Zhu, A.X.; Kudo, M.; Assenat, E.; Cattan, S.; Kang, Y.K.; Lim, H.Y.; Poon, R.T.; Blanc, J.F.; Vogel, A.; Chen, C.L.; et al. Effect of everolimus on survival in advanced hepatocellular carcinoma after failure of sorafenib: The EVOLVE-1 randomized clinical trial. JAMA 2014, 312, 57–67. [Google Scholar] [CrossRef]
- Rimassa, L.; Assenat, E.; Peck-Radosavljevic, M.; Pracht, M.; Zagonel, V.; Mathurin, P.; Rota Caremoli, E.; Porta, C.; Daniele, B.; Bolondi, L.; et al. Tivantinib for second-line treatment of MET-high, advanced hepatocellular carcinoma (METIV-HCC): A final analysis of a phase 3, randomised, placebo-controlled study. Lancet Oncol. 2018, 19, 682–693. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Qin, S.; Ryoo, B.Y.; Lu, S.N.; Yen, C.J.; Feng, Y.H.; Lim, H.Y.; Izzo, F.; Colombo, M.; Sarker, D.; et al. Phase III randomized study of second line ADI-PEG 20 plus best supportive care versus placebo plus best supportive care in patients with advanced hepatocellular carcinoma. Ann. Oncol. 2018, 29, 1402–1408. [Google Scholar] [CrossRef] [PubMed]
- Abou-Alfa, G.K.; Shi, Q.; Knox, J.J.; Kaubisch, A.; Niedzwiecki, D.; Posey, J.; Tan, B.R., Jr.; Kavan, P.; Goel, R.; Lammers, P.E.; et al. Assessment of Treatment With Sorafenib Plus Doxorubicin vs Sorafenib Alone in Patients With Advanced Hepatocellular Carcinoma: Phase 3 CALGB 80802 Randomized Clinical Trial. JAMA Oncol. 2019. [Google Scholar] [CrossRef]
- Merle, P.; Blanc, J.F.; Phelip, J.M.; Pelletier, G.; Bronowicki, J.P.; Touchefeu, Y.; Pageaux, G.; Gerolami, R.; Habersetzer, F.; Nguyen-Khac, E.; et al. Doxorubicin-loaded nanoparticles for patients with advanced hepatocellular carcinoma after sorafenib treatment failure (RELIVE): A phase 3 randomised controlled trial. Lancet Gastroenterol. Hepatol. 2019, 4, 454–465. [Google Scholar] [CrossRef]
- El-Khoueiry, A.B.; Sangro, B.; Yau, T.; Crocenzi, T.S.; Kudo, M.; Hsu, C.; Kim, T.-Y.; Choo, S.-P.; Trojan, J.; Welling, T.H.; et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): An open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 2017, 389, 2492–2502. [Google Scholar] [CrossRef]
- Zhu, A.X.; Finn, R.S.; Edeline, J.; Cattan, S.; Ogasawara, S.; Palmer, D.; Verslype, C.; Zagonel, V.; Fartoux, L.; Vogel, A.; et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): A non-randomised, open-label phase 2 trial. Lancet Oncol. 2018, 19, 940–952. [Google Scholar] [CrossRef]
- Finn, R.S.; Ryoo, B.Y.; Merle, P.; Kudo, M.; Bouattour, M.; Lim, H.Y.; Breder, V.; Edeline, J.; Chao, Y.; Ogasawara, S.; et al. Pembrolizumab As Second-Line Therapy in Patients With Advanced Hepatocellular Carcinoma in KEYNOTE-240: A Randomized, Double-Blind, Phase III Trial. J. Clin. Oncol. 2020, 38, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Yau, T.; Park, J.W.; Finn, R.S.; Cheng, A.L.; Mathurin, P.; Edeline, J.; Kudo, M.; Han, K.H.; Harding, J.J.; Merle, P.; et al. CheckMate 459: A randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann. Oncol. 2019, 30, v874–v875. [Google Scholar] [CrossRef]
- Kudo, M.; Finn, R.S.; Qin, S.; Han, K.-H.; Ikeda, K.; Piscaglia, F.; Baron, A.; Park, J.-W.; Han, G.; Jassem, J.; et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomised phase 3 non-inferiority trial. Lancet 2018, 391, 1163–1173. [Google Scholar] [CrossRef]
- Bruix, J.; Qin, S.; Merle, P.; Granito, A.; Huang, Y.-H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Breder, V.; et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 389, 56–66. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Meyer, T.; Cheng, A.-L.; El-Khoueiry, A.B.; Rimassa, L.; Ryoo, B.-Y.; Cicin, I.; Merle, P.; Chen, Y.; Park, J.-W.; et al. Cabozantinib in Patients with Advanced and Progressing Hepatocellular Carcinoma. N. Engl. J. Med. 2018, 379, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Zhu, A.X.; Park, J.O.; Ryoo, B.Y.; Yen, C.J.; Poon, R.; Pastorelli, D.; Blanc, J.F.; Chung, H.C.; Baron, A.D.; Pfiffer, T.E.; et al. Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): A randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2015, 16, 859–870. [Google Scholar] [CrossRef]
- Zhu, A.X.; Kang, Y.K.; Yen, C.J.; Finn, R.S.; Galle, P.R.; Llovet, J.M.; Assenat, E.; Brandi, G.; Pracht, M.; Lim, H.Y.; et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased alpha-fetoprotein concentrations (REACH-2): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 2019, 20, 282–296. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Richard, S.F.; Shukui, Q.; Masafumi, I.; Peter, R.G.; Michel, D.; Tae-You, K.; Ho Yeong, L.; Masatoshi, K.; Valeriy Vladimirovich, B.; Philippe, M.; et al. IMbrave150: Updated overall survival (OS) data from a global, randomized, open-label phase III study of atezolizumab (atezo) + bevacizumab (bev) versus sorafenib (sor) in patients (pts) with unresectable hepatocellular carcinoma (HCC). J. Clin. Oncol. 2021, 39, 267. [Google Scholar] [CrossRef]
- Yau, T.; Kang, Y.K.; Kim, T.Y.; El-Khoueiry, A.B.; Santoro, A.; Sangro, B.; Melero, I.; Kudo, M.; Hou, M.M.; Matilla, A.; et al. Efficacy and Safety of Nivolumab Plus Ipilimumab in Patients With Advanced Hepatocellular Carcinoma Previously Treated With Sorafenib: The CheckMate 040 Randomized Clinical Trial. JAMA Oncol. 2020. [Google Scholar] [CrossRef]
- Rimassa, L.; Cheng, A.; Braiteh, F.; Benzaghou, F.; Hazra, S.; Borgman, A.; Sinha, R.; Kayali, Z.; Zhu, A.; Kelley, R. Phase 3 (COSMIC-312) study of cabozantinib in combination with atezolizumab vs sorafenib in patients with advanced hepatocellular carcinoma (aHCC) who have not received previous systemic anticancer therapy. Ann. Oncol. 2019, 30, iv65–iv66. [Google Scholar] [CrossRef]
- Josep, M.L.; Masatoshi, K.; Ann-Lii, C.; Richard, S.F.; Peter, R.G.; Shuichi, K.; Tim, M.; Shukui, Q.; Corina, E.D.; Erluo, C.; et al. Lenvatinib (len) plus pembrolizumab (pembro) for the first-line treatment of patients (pts) with advanced hepatocellular carcinoma (HCC): Phase 3 LEAP-002 study. J. Clin. Oncol. 2019, 37, TPS4152. [Google Scholar] [CrossRef]
- Ghassan, K.A.-A.; Stephen Lam, C.; Junji, F.; Peter, R.G.; Robin Kate, K.; Shukui, Q.; Jon, A.; Annie, D.; Gordana, V.; Alejandra, N.; et al. A randomized, multicenter phase 3 study of durvalumab (D) and tremelimumab (T) as first-line treatment in patients with unresectable hepatocellular carcinoma (HCC): HIMALAYA study. J. Clin. Oncol. 2018, 36, TPS4144. [Google Scholar] [CrossRef]
- Qin, S.; Finn, R.S.; Kudo, M.; Meyer, T.; Vogel, A.; Ducreux, M.; Macarulla, T.M.; Tomasello, G.; Boisserie, F.; Hou, J.; et al. RATIONALE 301 study: Tislelizumab versus sorafenib as first-line treatment for unresectable hepatocellular carcinoma. Future Oncol. 2019, 15, 1811–1822. [Google Scholar] [CrossRef]
- Llovet, J.M.; El-Khoueiry, A.B.; Vogel, A.; Madoff, D.C.; Finn, R.S.; Ogasawara, S.; Ren, Z.; Mody, K.; Li, J.J.; Siegel, A.B.; et al. 1016TiP LEAP-012 trial in progress: Pembrolizumab plus lenvatinib and transarterial chemoembolization (TACE) in patients with intermediate-stage hepatocellular carcinoma (HCC) not amenable to curative treatment. Ann. Oncol. 2020, 31, S702–S703. [Google Scholar] [CrossRef]
- Bruix, J.; Takayama, T.; Mazzaferro, V.; Chau, G.Y.; Yang, J.; Kudo, M.; Cai, J.; Poon, R.T.; Han, K.H.; Tak, W.Y.; et al. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): A phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2015, 16, 1344–1354. [Google Scholar] [CrossRef]
- Exposito, M.J.; Akce, M.; Alvarez, J.; Assenat, E.; Balart, L.; Baron, A.; Decaens, T.; Heurgue-Berlot, A.; Martin, A.; Paik, S.; et al. Abstract No. 526 CheckMate-9DX: Phase 3, randomized, double-blind study of adjuvant nivolumab vs placebo for patients with hepatocellular carcinoma (HCC) at high risk of recurrence after curative resection or ablation. J. Vasc. Interv. Radiol. 2019, 30, S227–S228. [Google Scholar] [CrossRef]
- Zhu, A.; Kudo, M.; Vogel, A.; Yau, T.; Zhou, J.; Kim, E.; Malhotra, U.; Siegel, A.B.; Cheng, A.-L. Abstract CT284: Phase 3 KEYNOTE-937: Adjuvant pembrolizumab versus placebo in patients with hepatocellular carcinoma and complete radiologic response after surgical resection or local ablation. Cancer Res. 2020, 80, CT284. [Google Scholar] [CrossRef]
- Hack, S.P.; Spahn, J.; Chen, M.; Cheng, A.L.; Kaseb, A.; Kudo, M.; Lee, H.C.; Yopp, A.; Chow, P.; Qin, S. IMbrave 050: A Phase III trial of atezolizumab plus bevacizumab in high-risk hepatocellular carcinoma after curative resection or ablation. Future Oncol. 2020, 16, 975–989. [Google Scholar] [CrossRef] [PubMed]
- Knox, J.; Cheng, A.; Cleary, S.; Galle, P.; Kokudo, N.; Lencioni, R.; Park, J.; Zhou, J.; Mann, H.; Morgan, S.; et al. A phase 3 study of durvalumab with or without bevacizumab as adjuvant therapy in patients with hepatocellular carcinoma at high risk of recurrence after curative hepatic resection or ablation: EMERALD-2. Ann. Oncol. 2019, 30, iv59–iv60. [Google Scholar] [CrossRef]
- Gassmann, D.; Weiler, S.; Mertens, J.C.; Reiner, C.S.; Vrugt, B.; Nageli, M.; Mangana, J.; Mullhaupt, B.; Jenni, F.; Misselwitz, B. Liver Allograft Failure After Nivolumab Treatment-A Case Report With Systematic Literature Research. Transpl. Direct 2018, 4, e376. [Google Scholar] [CrossRef] [PubMed]
- Moehler, M.; Heo, J.; Lee, H.C.; Tak, W.Y.; Chao, Y.; Paik, S.W.; Yim, H.J.; Byun, K.S.; Baron, A.; Ungerechts, G.; et al. Vaccinia-based oncolytic immunotherapy Pexastimogene Devacirepvec in patients with advanced hepatocellular carcinoma after sorafenib failure: A randomized multicenter Phase IIb trial (TRAVERSE). Oncoimmunology 2019, 8, 1615817. [Google Scholar] [CrossRef] [PubMed]
- Ghassan, K.A.-A.; Peter, R.G.; Yee, C.; Karen, T.B.; Jeong, H.; Mitesh, J.B.; Angelo, L.; Adina, P.; Delphine, A.; Monika, L.; et al. PHOCUS: A phase 3 randomized, open-label study comparing the oncolytic immunotherapy Pexa-Vec followed by sorafenib (SOR) vs SOR in patients with advanced hepatocellular carcinoma (HCC) without prior systemic therapy. J. Clin. Oncol. 2016, 34, TPS4146. [Google Scholar] [CrossRef]
- Peter, R.G.; Richard, S.F.; Shukui, Q.; Masafumi, I.; Andrew, X.Z.; Tae-You, K.; Masatoshi, K.; Valeriy Vladimirovich, B.; Philippe, M.; Ahmed Omar, K.; et al. Patient-reported outcomes (PROs) from the Phase III IMbrave150 trial of atezolizumab (atezo) + bevacizumab (bev) vs sorafenib (sor) as first-line treatment (tx) for patients (pts) with unresectable hepatocellular carcinoma (HCC). J. Clin. Oncol. 2020, 38, 476. [Google Scholar] [CrossRef]
- Foerster, F.; Hess, M.; Gerhold-Ay, A.; Marquardt, J.U.; Becker, D.; Galle, P.R.; Schuppan, D.; Binder, H.; Bockamp, E. The immune contexture of hepatocellular carcinoma predicts clinical outcome. Sci. Rep. 2018, 8, 5351. [Google Scholar] [CrossRef] [PubMed]
- Sia, D.; Jiao, Y.; Martinez-Quetglas, I.; Kuchuk, O.; Villacorta-Martin, C.; Castro de Moura, M.; Putra, J.; Camprecios, G.; Bassaganyas, L.; Akers, N.; et al. Identification of an Immune-specific Class of Hepatocellular Carcinoma, Based on Molecular Features. Gastroenterology 2017, 153, 812–826. [Google Scholar] [CrossRef] [PubMed]
- Kurebayashi, Y.; Ojima, H.; Tsujikawa, H.; Kubota, N.; Maehara, J.; Abe, Y.; Kitago, M.; Shinoda, M.; Kitagawa, Y.; Sakamoto, M. Landscape of immune microenvironment in hepatocellular carcinoma and its additional impact on histological and molecular classification. Hepatology 2018, 68, 1025–1041. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Lou, Y.; Yang, J.; Wang, J.; Feng, J.; Zhao, Y.; Wang, L.; Huang, X.; Fu, Q.; Ye, M.; et al. Integrated multiomic analysis reveals comprehensive tumour heterogeneity and novel immunophenotypic classification in hepatocellular carcinomas. Gut 2019, 68, 2019–2031. [Google Scholar] [CrossRef] [PubMed]
- Harding, J.J.; Nandakumar, S.; Armenia, J.; Khalil, D.N.; Albano, M.; Ly, M.; Shia, J.; Hechtman, J.F.; Kundra, R.; El Dika, I.; et al. Prospective Genotyping of Hepatocellular Carcinoma: Clinical Implications of Next-Generation Sequencing for Matching Patients to Targeted and Immune Therapies. Clin. Cancer Res. 2019, 25, 2116–2126. [Google Scholar] [CrossRef]
- Pinyol, R.; Sia, D.; Llovet, J.M. Immune Exclusion-Wnt/CTNNB1 Class Predicts Resistance to Immunotherapies in HCC. Clin. Cancer Res. 2019, 25, 2021–2023. [Google Scholar] [CrossRef] [PubMed]
- Ayers, M.; Lunceford, J.; Nebozhyn, M.; Murphy, E.; Loboda, A.; Kaufman, D.R.; Albright, A.; Cheng, J.D.; Kang, S.P.; Shankaran, V.; et al. IFN-gamma-related mRNA profile predicts clinical response to PD-1 blockade. J. Clin. Investig. 2017, 127, 2930–2940. [Google Scholar] [CrossRef]
- Havel, J.J.; Chowell, D.; Chan, T.A. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat. Rev. Cancer 2019, 19, 133–150. [Google Scholar] [CrossRef]
- Rimassa, L.; Personeni, N.; Czauderna, C.; Foerster, F.; Galle, P. Systemic Treatment of Hcc in Special Populations. J. Hepatol. 2020. [Google Scholar] [CrossRef]
| Trial | Identifier | Phase | BCLC Stage | Treatment Arms | Primary Endpoint(s) | Setting |
|---|---|---|---|---|---|---|
| COSMIC-312 | NCT03755791 | Phase 3 | B or C | Cabozantinib + atezolizumab Sorafenib Cabozantinib | PFS per RECIST 1.1 OS | First-line |
| LEAP-002 | NCT03713593 | Phase 3 | B or C | Lenvatinib + pembrolizumab Lenvatinib | PFS per RECIST 1.1 OS | First-line |
| HIMALAYA | NCT03298451 | Phase 3 | B or C | Durvalumab Durvalumab + trevelimumab (2 regimens) Sorafenib | OS | First-line |
| CheckMate 9DW | NCT04039607 | Phase 3 | C | Nivolumab + ipilimumab Sorafenib or lenvatinib | OS | First-line |
| N/A | NCT03764293 | Phase 3 | B or C | Camrelizumab (SHR-1210) + apatinib Sorafenib | PFS OS | First-line |
| RATIONALE-301 | NCT03412773 | Phase 3 | B or C | Tislelizumab Sorafenib | OS | First-line |
| GOING | NCT04170556 | Phase 1/2 | BCLC C | Regorafenib (monotherapy for the first 8 weeks) + nivolumab | Safety | Second-line |
| RENOBATE | NCT04310709 | Phase 2 | B or C | Regorafenib + nivolumab | ORR per RECIST 1.1 | First-line |
| Bayer 19497 | NCT03347292 | Phase 1b/2 | B or C | Regorafenib + pembrolizumab | Safety | First-line |
| N/A | NCT04183088 | Phase 2 | B or C | Part 1: Regorafenib + tislelizumab Part 2: Regorafenib + tislelizumab Regorafenib | Part 1: Safety Part 2: PFS per RECIST 1.1 ORR per RECIST 1.1 | First-line |
| N/A | NCT04442581 | Phase 2 | B or C | Cabozantinib + pembrolizumab | ORR per RECIST 1.1 | First-line |
| N/A | NCT03941873 | Phase 1/2 | B or C | Phase 1: Sitravatinib Sitravatinib + tislelizumab Phase 2: Sitravatinib Sitravatinib + tislelizumab | Phase 1: Safety Phase 2: ORR per RECIST 1.1 | First- and later line |
| Trial | Identifier | Phase | BCLC Stage | Treatment Arms | Primary Endpoint(s) | Setting |
|---|---|---|---|---|---|---|
| LEAP-012 | NCT04246177 | Phase 3 | B |
|
| First-line |
| EMERALD-1 | NCT03778957 | Phase 3 | B |
|
| First-line |
| CheckMate 74W | NCT04340193 | Phase 3 | B |
|
| First-line |
| ABC-HCC | NCT04803994 | Phase 3 | B |
|
| First-line |
| RENOTACE | NCT04777851 | Phase 3 | B |
|
| First-line |
| Trial | Identifier | Phase | BCLC Stage | Treatment Arms | Primary Endpoint(s) | Setting |
|---|---|---|---|---|---|---|
| CheckMate 9DX | NCT03383458 | Phase 3 | 0 or A |
|
| Adjuvant |
| KEYNOTE-937 | NCT03867084 | Phase 3 | 0 or A |
|
| Adjuvant |
| IMbrave050 | NCT04102098 | Phase 3 | 0 or A |
|
| Adjuvant |
| EMERALD-2 | NCT03847428 | Phase 3 | 0 or A |
|
| Adjuvant |
| Trial | Identifier | Phase | BCLC Stage | Treatment Arms | Primary Endpoint(s) | Setting |
|---|---|---|---|---|---|---|
| NIVOLEP | NCT03630640 | Phase 2 | A or B |
|
| Neoadjuvant & adjuvant |
| CaboNivo | NCT03299946 | Phase 1b | N/A * |
|
| Neoadjuvant |
| N/A | NCT03337841 | Phase 2 | 0 or A |
|
| Neoadjuvant & adjuvant |
| PLENTY202001 | NCT04425226 | Phase 2 | N/A ** |
|
| Neoadjuvant |
| Identifier | Phase | BCLC Stage | Treatment Arms | Primary Endpoint(s) | Setting |
|---|---|---|---|---|---|
| NCT02905188 | Phase 1 | C |
|
| Palliative |
| NCT03980288 | Phase 1 | C |
|
| Palliative |
| NCT04011033 | Phase 2 | C |
|
| Palliative |
| NCT03319459 | Phase 1 | C |
|
| Palliative |
| NCT03841110 | Phase 1 | C |
|
| Palliative |
| NCT03071094 | Phase 1/2 | C |
|
| Palliative |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foerster, F.; Galle, P.R. The Current Landscape of Clinical Trials for Systemic Treatment of HCC. Cancers 2021, 13, 1962. https://doi.org/10.3390/cancers13081962
Foerster F, Galle PR. The Current Landscape of Clinical Trials for Systemic Treatment of HCC. Cancers. 2021; 13(8):1962. https://doi.org/10.3390/cancers13081962
Chicago/Turabian StyleFoerster, Friedrich, and Peter Robert Galle. 2021. "The Current Landscape of Clinical Trials for Systemic Treatment of HCC" Cancers 13, no. 8: 1962. https://doi.org/10.3390/cancers13081962
APA StyleFoerster, F., & Galle, P. R. (2021). The Current Landscape of Clinical Trials for Systemic Treatment of HCC. Cancers, 13(8), 1962. https://doi.org/10.3390/cancers13081962






