Clinical Implications of Androgen-Positive Triple-Negative Breast Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Clinical Characteristics of AR-Positive Tnbc
3. Potential Diagnostic and Prognostic Biomarkers
3.1. SOX10 and GATA3
3.2. Programmed Cell Death Ligand (PDL1) and Forkhead Box 1 (FOXA1)
3.3. ER-Beta Receptor
4. Clinical Imaging and AR Positivity
5. Prognosis
5.1. AR as an Independent Prognostic Marker
5.2. Discordance Rate of AR Positivity
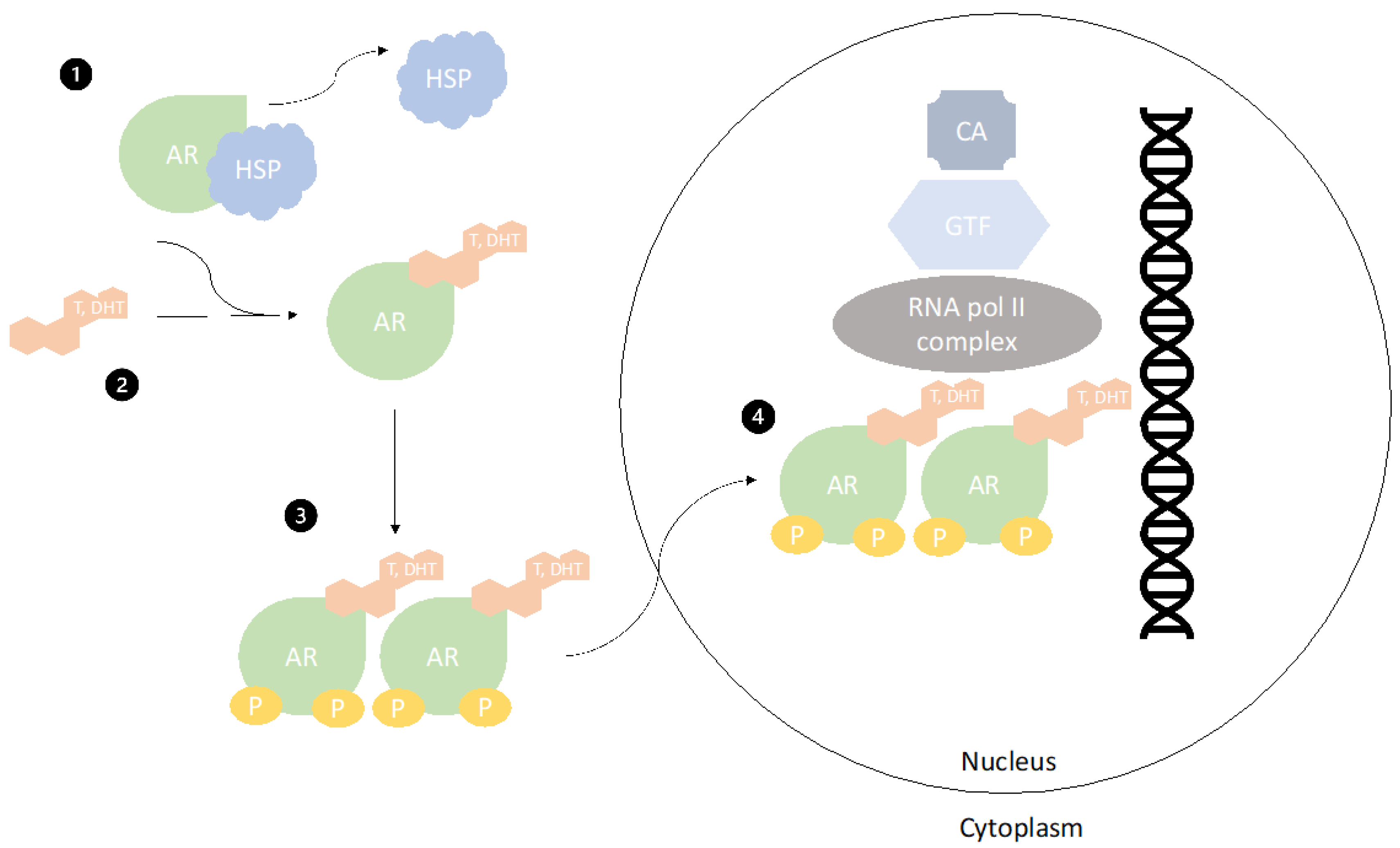
6. Androgen Receptors as a Therapeutic Target
Interplay of Signaling Pathways with Androgen Receptors
7. Discussion
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lehmann, B.D.; Pietenpol, J.A. Clinical implications of molecular heterogeneity in triple negative breast cancer. Breast 2015, 24, S36–S40. [Google Scholar] [CrossRef]
- Safarpour, D.; Tavassoli, F.A. A targetable androgen receptor-Positive breast cancer subtype hidden among the triple-negative cancers. Arch. Pathol. Lab. Med. 2015, 139, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, B.D.; Bauer, J.A.; Chen, X.; Sanders, M.E.; Chakravarthy, A.B.; Shyr, Y.; Pietenpol, J.A. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J. Clin. Investig. 2011, 121, 2750–2767. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Ma, D.; Xiao, Y.; Li, X.; Ma, J.; Zhang, H.; Xu, X.; Lv, H.; Jiang, W.; Yang, W.; et al. Molecular Subtyping of Triple-Negative Breast Cancers by Immunohistochemistry: Molecular Basis and Clinical Relevance. Oncologist 2020, 25, e1481. [Google Scholar] [CrossRef] [PubMed]
- Jézéquel, P.; Loussouarn, D.; Guérin-Charbonnel, C.; Campion, L.; Vanier, A.; Gouraud, W.; Lasla, H.; Guette, C.; Valo, I.; Verrièle, V.; et al. Gene-expression molecular subtyping of triple-negative breast cancer tumours: Importance of immune response. Breast Cancer Res. 2015, 17, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Bareche, Y.; Venet, D.; Ignatiadis, M.; Aftimos, P.; Piccart, M.; Rothe, F.; Sotiriou, C. Unravelling triple-negative breast cancer molecular heterogeneity using an integrative multiomic analysis. Ann. Oncol. 2018, 29, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.C.; Steele, L.; Warden, C.; Wilczynski, S.; Mortimer, J.; Yuan, Y.; Neuhausen, S.L. Molecular subtypes of triple-negative breast cancer in women of different race and ethnicity. Oncotarget 2019, 10, 198–208. [Google Scholar] [CrossRef] [PubMed]
- Burstein, M.D.; Tsimelzon, A.; Poage, G.M.; Covington, K.R.; Contreras, A.; Fuqua, S.A.W.; Savage, M.I.; Osborne, C.K.; Hilsenbeck, S.G.; Chang, J.C.; et al. Comprehensive genomic analysis identifies novel subtypes and targets of triple-negative breast cancer. Clin. Cancer Res. 2015, 21, 1688–1698. [Google Scholar] [CrossRef]
- Prado-Vázquez, G.; Gámez-Pozo, A.; Trilla-Fuertes, L.; Arevalillo, J.M.; Zapater-Moros, A.; Ferrer-Gómez, M.; Díaz-Almirón, M.; López-Vacas, R.; Navarro, H.; Maín, P.; et al. A novel approach to triple-negative breast cancer molecular classification reveals a luminal immune-positive subgroup with good prognoses. Sci. Rep. 2019, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.R.; Jiang, Y.Z.; Xu, X.E.; Yu, K.D.; Jin, X.; Hu, X.; Zuo, W.J.; Hao, S.; Wu, J.; Liu, G.Y.; et al. Comprehensive transcriptome analysis identifies novel molecular subtypes and subtype-specific RNAs of triple-negative breast cancer. Breast Cancer Res. 2016, 18, 1–10. [Google Scholar] [CrossRef]
- Kim, J.; Yu, D.; Kwon, Y.; Lee, K.S.; Sim, S.H.; Kong, S.Y.; Lee, E.S.; Park, I.H.; Park, C. Genomic characteristics of triple-negative breast cancer nominate molecular subtypes that predict chemotherapy response. Mol. Cancer Res. 2020, 18, 253–263. [Google Scholar] [CrossRef]
- Tang, P.; Tse, G.M. Immunohistochemical surrogates for molecular classification of breast carcinoma: A 2015 update. Arch. Pathol. Lab. Med. 2016, 140, 806–814. [Google Scholar] [CrossRef] [PubMed]
- McGhan, L.J.; McCullough, A.E.; Protheroe, C.A.; Dueck, A.C.; Lee, J.J.; Nunez-Nateras, R.; Castle, E.P.; Gray, R.J.; Wasif, N.; Goetz, M.P.; et al. Androgen receptor-positive triple negative breast cancer: A unique breast cancer subtype. Ann. Surg. Oncol. 2014, 21, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Tozbikian, G.H.; Zynger, D.L. A combination of GATA3 and SOX10 is useful for the diagnosis of metastatic triple-negative breast cancer. Hum. Pathol. 2019, 85, 221–227. [Google Scholar] [CrossRef]
- Hu, R.; Dawood, S.; Holmes, M.D.; Collins, L.C.; Schnitt, S.J.; Cole, K.; Marotti, J.D.; Hankinson, S.E.; Colditz, G.A.; Tamimi, R.M. Androgen receptor expression and breast cancer survival in postmenopausal women. Clin. Cancer Res. 2011, 17, 1867–1874. [Google Scholar] [CrossRef]
- Kensler, K.H.; Beca, F.; Baker, G.M.; Heng, Y.J.; Beck, A.H.; Schnitt, S.J.; Hazra, A.; Rosner, B.A.; Eliassen, A.H.; Hankinson, S.E.; et al. Androgen receptor expression in normal breast tissue and subsequent breast cancer risk. NPJ Breast Cancer 2018, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yarid, N.; McMahon, L.; Yang, Q.; Hicks, D.G. Expression of androgen receptor and its association with estrogen receptor and androgen receptor downstream proteins in normal/benign breast luminal epithelium. Appl. Immunohistochem. Mol. Morphol. 2014, 22, 498–504. [Google Scholar] [CrossRef]
- Brünnert, D.; Langer, C.; Zimmermann, L.; Bargou, R.C.; Burchardt, M.; Chatterjee, M.; Stope, M.B. The heat shock protein 70 inhibitor VER155008 suppresses the expression of HSP27, HOP and HSP90β and the androgen receptor, induces apoptosis, and attenuates prostate cancer cell growth. J. Cell. Biochem. 2020, 121, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.D.; Gucalp, A.; Traina, T.A. The role of the androgen receptor in triple-negative breast cancer. Women’s Health 2013, 9, 351–360. [Google Scholar] [CrossRef]
- Solomon, J.Z.; Mirabal, R.J.; Manzur, D.J.; Kohn, T.P.; Lipshultz, L.I.; Pastuszak, A.W. Selective Androgen Receptor Modulators: Current Knowledge and Clinical Applications. Sex Med. Rev. 2019, 7, 84–94. [Google Scholar] [CrossRef]
- Coussy, F.; Lavigne, M.; de Koning, L.; El Botty, R.; Nemati, F.; Naguez, A.; Bataillon, G.; Ouine, B.; Dahmani, A.; Montaudon, E.; et al. Response to mTOR and PI3K inhibitors in enzalutamide-resistant luminal androgen receptor triple-negative breast cancer patient-derived xenografts. Theranostics 2020, 10, 1531–1543. [Google Scholar] [CrossRef] [PubMed]
- McNamara, K.M.; Yoda, T.; Miki, Y.; Chanplakorn, N.; Wongwaisayawan, S.; Incharoen, P.; Kongdan, Y.; Wang, L.; Takagi, K.; Mayu, T.; et al. Androgenic pathway in triple negative invasive ductal tumors: Its correlation with tumor cell proliferation. Cancer Sci. 2013, 104, 639–646. [Google Scholar] [CrossRef]
- Angajala, A.; Mothershed, E.; Davis, M.B.; Tripathi, S.; He, Q.; Bedi, D.; Dean-Colomb, W.; Yates, C. Quadruple Negative Breast Cancers (QNBC) Demonstrate Subtype Consistency among Primary and Recurrent or Metastatic Breast Cancer. Transl. Oncol. 2019, 12, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Lee, K.H.; Yun, J.S.; Park, Y.L.; Park, C.H.; Do, S.I.; Chae, S.W. Clinicopathologic significance of androgen receptor expression and discordant receptor status during progression in breast cancer. Int. J. Clin. Exp. Pathol. 2017, 10, 7929–7939. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.E.; Kang, S.H.; Lee, S.J.; Bae, Y.K. Androgen Receptor Expression Predicts Decreased Survival in Early Stage Triple-Negative Breast Cancer. Ann. Surg. Oncol. 2015, 22, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Guiu, S.; Charon-Barra, C.; Vernerey, D.; Fumoleau, P.; Campone, M.; Spielmann, M.; Roché, H.; Mesleard, C.; Arnould, L.; Lemonnier, J.; et al. Coexpression of androgen receptor and FOXA1 in nonmetastatic triple-negative breast cancer: Ancillary study from PACS08 trial. Futur. Oncol. 2015, 11, 2283–2297. [Google Scholar] [CrossRef]
- Tung, N.; Garber, J.E.; Hacker, M.R.; Torous, V.; Freeman, G.J.; Poles, E.; Rodig, S.; Alexander, B.; Lee, L.; Collins, L.C.; et al. Prevalence and predictors of androgen receptor and programmed death-ligand 1 in BRCA1-associated and sporadic triple-negative breast cancer. NPJ Breast Cancer 2016, 2, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Dieci, M.V.; Tsvetkova, V.; Griguolo, G.; Miglietta, F.; Mantiero, M.; Tasca, G.; Cumerlato, E.; Giorgi, C.A.; Giarratano, T.; Faggioni, G.; et al. Androgen receptor expression and association with distant disease-free survival in triple negative breast cancer: Analysis of 263 patients treated with standard therapy for stage I-III disease. Front. Oncol. 2019, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Astvatsaturyan, K.; Yue, Y.; Walts, A.E.; Bose, S. Androgen receptor positive triple negative breast cancer: Clinicopathologic, prognostic, and predictive features. PLoS ONE 2018, 13, e0197827. [Google Scholar] [CrossRef] [PubMed]
- Sunar, V.; Dogan, H.T.; Sarici, F.; Ates, O.; Akin, S.; Baspinar, B.; Aksoy, S.; Altundag, K. Association between androgen receptor status and prognosis in triple negative breast cancer. J. BUON 2018, 23, 1325–1330. [Google Scholar] [PubMed]
- Pistelli, M.; Caramanti, M.; Biscotti, T.; Santinelli, A.; Pagliacci, A.; De Lisa, M.; Ballatore, Z.; Ridolfi, F.; Maccaroni, E.; Bracci, R.; et al. Androgen receptor expression in early triple-negative breast cancer: Clinical significance and prognostic associations. Cancers 2014, 6, 1351–1362. [Google Scholar] [CrossRef] [PubMed]
- Jongen, L.; Floris, G.; Wildiers, H.; Claessens, F.; Richard, F.; Laenen, A.; Desmedt, C.; Ardui, J.; Punie, K.; Smeets, A.; et al. Tumor characteristics and outcome by androgen receptor expression in triple-negative breast cancer patients treated with neo-adjuvant chemotherapy. Breast Cancer Res. Treat. 2019, 176, 699–708. [Google Scholar] [CrossRef] [PubMed]
- Ma, D.; Jiang, Y.Z.; Xiao, Y.; Xie, M.D.; Zhao, S.; Jin, X.; Xu, X.E.; Shao, Z.M. Integrated molecular profiling of young and elderly patients with triple-negative breast cancer indicates different biological bases and clinical management strategies. Cancer 2020, 126, 3209–3218. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.Q.; Chen, W.L.; Ma, H.G.; Jiang, K. Androgen receptor expression identifies patient with favorable outcome in operable triple negative breast cancer. Oncotarget 2017, 8, 56364–56374. [Google Scholar] [CrossRef]
- Mohammed, A.A.; Elsayed, F.M.; Algazar, M.; Rashed, H.E.; Anter, A.H. Neoadjuvant Chemotherapy in Triple Negative Breast Cancer: Correlation between Androgen Receptor Expression and Pathological Response. Asian Pac. J. Cancer Prev. 2020, 21, 563–568. [Google Scholar] [CrossRef]
- Müller, M.; Güth, U.; Varga, Z.; Reeve, K.; Bjelic-Radisic, V.; Fleisch, M.; Tausch, C.J.; Elfgen, C. Clinical imaging of the heterogeneous group of triple-negative breast cancer. Anticancer Res. 2020, 40, 2125–2131. [Google Scholar] [CrossRef]
- Collina, F.; Cerrone, M.; Peluso, V.; de Laurentiis, M.; Caputo, R.; De Cecio, R.; Liguori, G.; Botti, G.; Cantile, M.; Di Bonito, M. Downregulation of androgen receptor is strongly associated with diabetes in triple negative breast cancer patients. Am. J. Transl. Res. 2016, 8, 3530–3539. [Google Scholar]
- Asano, Y.; Kashiwagi, S.; Goto, W.; Tanaka, S.; Morisaki, T.; Takashima, T.; Noda, S.; Onoda, N.; Ohsawa, M.; Hirakawa, K.; et al. Expression and clinical significance of androgen receptor in triple-negative breast cancer. Cancers 2017, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Rakha, E.A.; El-Sayed, M.E.; Green, A.R.; Lee, A.H.S.; Robertson, J.F.; Ellis, I.O. Prognostic markers in triple-negative breast cancer. Cancer 2007, 109, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Thike, A.A.; Chong, L.Y.Z.; Cheok, P.Y.; Li, H.H.; Yip, G.W.C.; Bay, B.H.; Tse, G.M.K.; Iqbal, J.; Tan, P.H. Loss of androgen receptor expression predicts early recurrence in triple-negative and basal-like breast cancer. Mod. Pathol. 2014, 27, 352–360. [Google Scholar] [CrossRef]
- Shen, Y.; Yang, F.; Zhang, W.; Song, W.; Liu, Y.; Guan, X. The Androgen Receptor Promotes Cellular Proliferation by Suppression of G-Protein Coupled Estrogen Receptor Signaling in Triple-Negative Breast Cancer. Cell. Physiol. Biochem. 2018, 43, 2047–2061. [Google Scholar] [CrossRef]
- Bae, M.S.; Park, S.Y.; Song, S.E.; Kim, W.H.; Lee, S.H.; Han, W.; Park, I.A.; Noh, D.Y.; Moon, W.K. Heterogeneity of triple-negative breast cancer: Mammographic, US, and MR imaging features according to androgen receptor expression. Eur. Radiol. 2015, 25, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Candelaria, R.P.; Adrada, B.E.; Wei, W.; Thompson, A.M.; Santiago, L.; Lane, D.L.; Huang, M.L.; Arribas, E.M.; Rauch, G.M.; Symmans, W.F.; et al. Imaging features of triple-negative breast cancers according to androgen receptor status. Eur. J. Radiol. 2019, 114, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Moon, B.I.; Lim, W.; Park, S.; Cho, M.S.; Sung, S.H. Feasibility of Classification of Triple Negative Breast Cancer by Immunohistochemical Surrogate Markers. Clin. Breast Cancer 2018, 18, e1123–e1132. [Google Scholar] [CrossRef] [PubMed]
- Santonja, A.; Sánchez-Muñoz, A.; Lluch, A.; Chica-Parrado, M.R.; Albanell, J.; Chacón, J.I.; Antolín, S.; Jerez, J.M.; de la Haba, J.; de Luque, V.; et al. Triple negative breast cancer subtypes and pathologic complete response rate to neoadjuvant chemotherapy. Oncotarget 2018, 9, 26406–26416. [Google Scholar] [CrossRef]
- Abd-Elazeem, M.A.; Abd-Elazeem, M.A. Claudin 4 expression in triple-negative breast cancer: Correlation with androgen receptors and Ki-67 expression. Ann. Diagn. Pathol. 2015, 19, 37–42. [Google Scholar] [CrossRef] [PubMed]
- McNamara, K.M.; Yoda, T.; Miki, Y.; Nakamura, Y.; Suzuki, T.; Nemoto, N.; Miyashita, M.; Nishimura, R.; Arima, N.; Tamaki, K.; et al. Androgen receptor and enzymes in lymph node metastasis and cancer reoccurrence in triple-negative breast cancer. Int. J. Biol. Markers 2015, 30, e184–e189. [Google Scholar] [CrossRef]
- Davis, D.G.; Siddiqui, M.T.; Oprea-Ilies, G.; Stevens, K.; Osunkoya, A.O.; Cohen, C.; Li, X. GATA-3 and FOXA1 expression is useful to differentiate breast carcinoma from other carcinomas. Hum. Pathol. 2016, 47, 26–31. [Google Scholar] [CrossRef]
- Harbhajanka, A.; Chahar, S.; Miskimen, K.; Silverman, P.; Harris, L.; Williams, N.; Varadan, V.; Gilmore, H. Clinicopathological, immunohistochemical and molecular correlation of neural crest transcription factor SOX10 expression in triple-negative breast carcinoma. Hum. Pathol. 2018, 80, 163–169. [Google Scholar] [CrossRef]
- Al-Zahrani, K.N.; Cook, D.P.; Vanderhyden, B.C.; Sabourin, L.A. Assessing the efficacy of androgen receptor and Sox10 as independent markers of the triple-negative breast cancer subtype by transcriptome profiling. Oncotarget 2018, 9, 33348–33359. [Google Scholar] [CrossRef] [PubMed]
- Chou, J.; Provot, S.; Werb, Z. GATA3 in development and cancer differentiation: Cells GATA have it! J. Cell Physiol. 2010, 222, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Moon, B.I.; Lim, W.; Park, S.; Cho, M.S.; Sung, S.H. Expression patterns of GATA3 and the androgen receptor are strongly correlated in patients with triple-negative breast cancer. Hum. Pathol. 2016, 55, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Boto, A.; Harigopal, M. Strong androgen receptor expression can aid in distinguishing GATA3+ metastases. Hum. Pathol. 2018, 75, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Wasserman, J.K.; Williams, P.A.; Islam, S.; Robertson, S.J. GATA-3 expression is not associated with complete pathological response in triple negative breast cancer patients treated with neoadjuvant chemotherapy. Pathol. Res. Pract. 2016, 212, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Mangia, A.; Saponaro, C.; Vagheggini, A.; Opinto, G.; Centonze, M.; Vicenti, C.; Popescu, O.; Pastena, M.; Giotta, F.; Silvestris, N. Should tumor infiltrating lymphocytes, androgen receptor, and FOXA1 expression predict the clinical outcome in triple negative breast cancer patients? Cancers 2019, 11, 1393. [Google Scholar] [CrossRef]
- Guiu, S.; Mollevi, C.; Charon-Barra, C.; Boissière, F.; Crapez, E.; Chartron, E.; Lamy, P.J.; Gutowski, M.; Bourgier, C.; Romieu, G.; et al. Prognostic value of androgen receptor and FOXA1 co-expression in non-metastatic triple negative breast cancer and correlation with other biomarkers. Br. J. Cancer 2018, 119, 76–79. [Google Scholar] [CrossRef]
- Mansouri, H.; Alcaraz, L.B.; Mollevi, C.; Mallavialle, A.; Jacot, W.; Boissière-Michot, F.; Simony-Lafontaine, J.; Laurent-Matha, V.; Roger, P.; Liaudet-Coopman, E.; et al. Co-expression of androgen receptor and cathepsin d defines a triple-negative breast cancer subgroup with poorer overall survival. Cancers 2020, 12, 1244. [Google Scholar] [CrossRef]
- Nakashoji, A.; Matsui, A.; Nagayama, A.; Iwata, Y.; Sasahara, M.; Murata, Y. Clinical predictors of pathological complete response to neoadjuvant chemotherapy in triple-negative breast cancer. Oncol. Lett. 2017, 14, 4135–4141. [Google Scholar] [CrossRef] [PubMed]
- Anestis, A.; Sarantis, P.; Theocharis, S.; Zoi, I.; Tryfonopoulos, D.; Korogiannos, A.; Koumarianou, A.; Xingi, E.; Thomaidou, D.; Kontos, M.; et al. Estrogen receptor beta increases sensitivity to enzalutamide in androgen receptor-positive triple-negative breast cancer. J. Cancer Res. Clin. Oncol. 2019, 145, 1221–1233. [Google Scholar] [CrossRef]
- Song, W.; Tang, L.; Xu, Y.; Sun, Q.; Yang, F.; Guan, X. ERβ1 inhibits metastasis of androgen receptor-positive triple-negative breast cancer by suppressing ZEB1. J. Exp. Clin. Cancer Res. 2017, 36, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Roubaud, G.; Liaw, B.C.; Oh, W.K.; Mulholland, D.J. Strategies to avoid treatment-induced lineage crisis in advanced prostate cancer. Nat. Rev. Clin. Oncol. 2017, 14, 269–283. [Google Scholar] [CrossRef] [PubMed]
- Li, J.W.; Zhang, K.; Shi, Z.T.; Zhang, X.; Xie, J.; Liu, J.Y.; Chang, C. Triple-negative invasive breast carcinoma: The association between the sonographic appearances with clinicopathological feature. Sci. Rep. 2018, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Elfgen, C.; Varga, Z.; Reeve, K.; Moskovszky, L.; Bjelic-Radisic, V.; Tausch, C.; Güth, U. The impact of distinct triple-negative breast cancer subtypes on misdiagnosis and diagnostic delay. Breast Cancer Res. Treat. 2019, 177, 67–75. [Google Scholar] [CrossRef]
- Sartor, H.; Zackrisson, S.; Elebro, K.; Hartman, L.; Borgquist, S. Mammographic density in relation to tumor biomarkers, molecular subtypes, and mode of detection in breast cancer. Cancer Causes Control 2015, 26, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Doane, A.S.; Danso, M.; Lal, P.; Donaton, M.; Zhang, L.; Hudis, C.; Gerald, W.L. An estrogen receptor-negative breast cancer subset characterized by a hormonally regulated transcriptional program and response to androgen. Oncogene 2006, 25, 3994–4008. [Google Scholar] [CrossRef] [PubMed]
- Asano, Y.; Kashiwagi, S.; Onoda, N.; Kurata, K.; Morisaki, T.; Noda, S.; Takashima, T.; Ohsawa, M.; Kitagawa, S.; Hirakawa, K. Clinical verification of sensitivity to preoperative chemotherapy in cases of androgen receptor-expressing positive breast cancer. Br. J. Cancer 2016, 114, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Adamo, B.; Ricciardi, G.R.R.; Ieni, A.; Franchina, T.; Fazzari, C.; Sanò, M.V.; Angelico, G.; Caruso, M.; Tuccari, G.; Adamo, V. Correction: The prognostic significance of combined androgen receptor, E-Cadherin, Ki67 and CK5/6 expression in patients with triple negative breast cancer (Oncotarget (2017) 8 (76974-76986) doi:10.18632/oncotarget.20293). Oncotarget 2019, 10, 917. [Google Scholar] [CrossRef]
- Ricciardi, G.R.R.; Adamo, B.; Ieni, A.; Licata, L.; Cardia, R.; Ferraro, G.; Franchina, T.; Tuccari, G.; Adamo, V. Androgen receptor (AR), E-Cadherin, and Ki-67 as emerging targets and novel prognostic markers in triple-negative breast cancer (TNBC) patients. PLoS ONE 2015, 10, e0128368. [Google Scholar] [CrossRef]
- Luo, X.; Shi, Y.X.; Li, Z.M.; Jiang, W.Q. Expression and clinical significance of androgen receptor in triple negative breast cancer. Chin. J. Cancer 2010, 29, 585–590. [Google Scholar] [CrossRef]
- Liu, Y.X.; Zhang, K.J.; Tang, L.L. Clinical significance of androgen receptor expression in triple negative breast cancer-an immunohistochemistry study. Oncol. Lett. 2018, 15, 10008–10016. [Google Scholar] [CrossRef] [PubMed]
- Foulkes, W.D.; Smith, I.E.; Reis-Filho, J.S. Triple-Negative Breast Cancer. N. Engl. J. Med. 2010, 363, 1938–1948. [Google Scholar] [CrossRef]
- Gasparini, P.; Fassan, M.; Cascione, L.; Guler, G.; Balci, S.; Irkkan, C.; Paisie, C.; Lovat, F.; Morrison, C.; Zhang, J.; et al. Androgen receptor status is a prognostic marker in non-basal triple negative breast cancers and determines novel therapeutic options. PLoS ONE 2014, 9, e88525. [Google Scholar] [CrossRef] [PubMed]
- Thakkar, A.; Wang, B.; Picon-Ruiz, M.; Buchwald, P.; Ince, T.A. Vitamin D and androgen receptor-targeted therapy for triple-negative breast cancer. Breast Cancer Res. Treat. 2016, 157, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Figee, M.; Mayberg, H. The future of personalized brain stimulation. Nat. Med. 2021, 27, 198–199. [Google Scholar] [CrossRef]
- Hickey, T.E.; Selth, L.A.; Chia, K.M.; Laven-Law, G.; Milioli, H.H.; Roden, D.; Jindal, S.; Hui, M.; Finlay-Schultz, J.; Ebrahimie, E.; et al. The androgen receptor is a tumor suppressor in estrogen receptor–positive breast cancer. Nat. Med. 2021, 27, 310–320. [Google Scholar] [CrossRef]
- D’Amato, N.C.; Gordon, M.A.; Babbs, B.; Spoelstra, N.S.; Carson Butterfield, K.T.; Torkko, K.C.; Phan, V.T.; Barton, V.N.; Rogers, T.J.; Sartorius, C.A.; et al. Cooperative Dynamics of AR and ER Activity in Breast Cancer. Mol. Cancer Res. 2016, 14, 1054–1067. [Google Scholar] [CrossRef]
- Barton, V.N.; D’Amato, N.C.; Gordon, M.A.; Lind, H.T.; Spoelstra, N.S.; Babbs, B.L.; Heinz, R.E.; Elias, A.; Jedlicka, P.; Jacobsen, B.M.; et al. Multiple molecular subtypes of triple-negative breast cancer critically rely on androgen receptor and respond to enzalutamide in vivo. Mol. Cancer Ther. 2015, 14, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Kwilas, A.R.; Ardiani, A.; Gameiro, S.R.; Richards, J.; Hall, A.B.; Hodge, J.W. Androgen deprivation therapy sensitizes triple negative breast cancer cells to immune-mediated lysis through androgen receptor independent modulation of osteoprotegerin. Oncotarget 2016, 7, 23498–23511. [Google Scholar] [CrossRef]
- Differentiation, H.; Embryonic, H.; Cells, S.; Dynamic, T.-D.; Culture, P.; Toshio, C.; Ring, A.; Medicine, R.; Virchow-Clinic, C.; Miki, T. Page 1 of 38 1. Tissue Eng. Part C Methods 2011, 17, 557–568. [Google Scholar] [CrossRef]
- Luo, J.; Jin, J.; Yang, F.; Sun, Z.; Zhang, W.; Shi, Y.; Xu, J.; Guan, X. The correlation between PARP1 and BRCA1 in AR positive triple-negative breast cancer. Int. J. Biol. Sci. 2016, 12, 1500–1510. [Google Scholar] [CrossRef]
- Giovannelli, P.; Di Donato, M.; Auricchio, F.; Castoria, G.; Migliaccio, A. Androgens Induce Invasiveness of Triple Negative Breast Cancer Cells Through AR/Src/PI3-K Complex Assembly. Sci. Rep. 2019, 9, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Gordon, M.A.; D’Amato, N.C.; Gu, H.; Babbs, B.; Wulfkuhle, J.; Petricoin, E.F.; Gallagher, I.; Dong, T.; Torkko, K.; Liu, B.; et al. Synergy between Androgen Receptor Antagonism and Inhibition of mTOR and HER2 in Breast Cancer. Mol. Cancer Ther. 2017, 16, 1389–1400. [Google Scholar] [CrossRef] [PubMed]
- Traina, T.A.; Miller, K.; Yardley, D.A.; Eakle, J.; Schwartzberg, L.S.; O’Shaughnessy, J.; Gradishar, W.; Schmid, P.; Winer, E.; Kelly, C.; et al. Enzalutamide for the treatment of androgen receptor-expressing triple-negative breast cancer. J. Clin. Oncol. 2018, 36, 884–890. [Google Scholar] [CrossRef]
- Sang, M.; Meng, L.; Ma, C.; Liu, S.; Sang, M.; Chang, S.; Liu, F.; Lian, Y.; Geng, C. Effect of AR antagonist combined with PARP1 inhibitor on sporadic triple-negative breast cancer bearing AR expression and methylation-mediated BRCA1 dysfunction. Biomed. Pharmacother. 2019, 111, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Speers, C.; Zhao, S.G.; Chandler, B.; Liu, M.; Wilder-Romans, K.; Olsen, E.; Nyati, S.; Ritter, C.; Alluri, P.G.; Kothari, V.; et al. Androgen receptor as a mediator and biomarker of radioresistance in triple-negative breast cancer. NPJ Breast Cancer 2017, 3, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tamae, D.; Mostaghel, E.; Montgomery, B.; Nelson, P.S.; Balk, S.P.; Kantoff, P.W.; Taplin, M.-E.; Penning, T.M. The DHEA-sulfate depot following P450c17 inhibition supports the case for AKR1C3 inhibition in high risk localized and advanced castration resistant prostate cancer. Chem. Biol. Interact. 2015, 234, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Toren, P.J.; Kim, S.; Pham, S.; Mangalji, A.; Adomat, H.; Guns, E.S.T.; Zoubeidi, A.; Moore, W.; Gleave, M.E. Anticancer activity of a novel selective CYP17A1 inhibitor in preclinical models of castrate-resistant prostate cancer. Mol. Cancer Ther. 2015, 14, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Michmerhuizen, A.R.; Chandler, B.; Olsen, E.; Wilder-Romans, K.; Moubadder, L.; Liu, M.; Pesch, A.M.; Zhang, A.; Ritter, C.; Ward, S.T.; et al. Seviteronel, a Novel CYP17 Lyase Inhibitor and Androgen Receptor Antagonist, Radiosensitizes AR-Positive Triple Negative Breast Cancer Cells. Front. Endocrinol. 2020, 11, 1–13. [Google Scholar] [CrossRef]
- Khatun, A.; Shimozawa, M.; Kito, H.; Kawaguchi, M.; Fujimoto, M.; Ri, M.; Kajikuri, J.; Niwa, S.; Fujii, M.; Ohya, S. Transcriptional repression and protein degradation of the Ca2+-activated K+ channel KCa1.1 by androgen receptor inhibition in human breast cancer cells. Front. Physiol. 2018, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.P.; Mostaghel, E.A.; Nelson, P.S.; Montgomery, B. Androgen deprivation therapy: Progress in understanding mechanisms of resistance and optimizing androgen depletion. Nat. Clin. Pract. Urol. 2009, 6, 76–85. [Google Scholar] [CrossRef]
- Grellety, T.; Callens, C.; Richard, E.; Briaux, A.; Velasco, V.; Pulido, M.; Gonçalves, A.; Gestraud, P.; MacGrogan, G.; Bonnefoi, H.; et al. Enhancing Abiraterone Acetate Efficacy in Androgen Receptor–positive Triple-negative Breast Cancer: Chk1 as a potential target. Clin. Cancer Res. 2019, 25, 856–867. [Google Scholar] [CrossRef]
- Elfgen, C.; Reeve, K.; Moskovszky, L.; Güth, U.; Bjelic-Radisic, V.; Fleisch, M.; Tausch, C.; Varga, Z. Prognostic impact of PIK3CA protein expression in triple negative breast cancer and its subtypes. J. Cancer Res. Clin. Oncol. 2019, 145, 2051–2059. [Google Scholar] [CrossRef]
- Millis, S.Z.; Gatalica, Z.; Winkler, J.; Vranic, S.; Kimbrough, J.; Reddy, S.; O’Shaughnessy, J.A. Predictive biomarker profiling of >6000 breast cancer patients shows heterogeneity in TNBC, with treatment implications. Clin. Breast Cancer 2015, 15, 473–481.e3. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, B.D.; Bauer, J.A.; Schafer, J.M.; Pendleton, C.S.; Tang, L.; Johnson, K.C.; Chen, X.; Balko, J.M.; Gómez, H.; Arteaga, C.L.; et al. PIK3CA mutations in androgen receptor-positive triple negative breast cancer confer sensitivity to the combination of PI3K and androgen receptor inhibitors. Breast Cancer Res. 2014, 16, 1–14. [Google Scholar] [CrossRef]
- Cuenca-López, M.D.; Montero, J.C.; Morales, J.C.; Prat, A.; Pandiella, A.; Ocana, A. Phospho-kinase profile of triple negative breast cancer and androgen receptor signaling. BMC Cancer 2014, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, B.D.; Abramson, V.G.; Sanders, M.E.; Mayer, E.L.; Haddad, T.C.; Nanda, R.; Van Poznak, C.; Storniolo, A.M.; Nangia, J.R.; Gonzalez-Ericsson, P.I.; et al. TBCRC 032 IB/II Multicenter Study: Molecular Insights to AR Antagonist and PI3K Inhibitor Efficacy in Patients with AR+ Metastatic Triple-Negative Breast Cancer. Clin. Cancer Res. 2020, 26, 2111–2123. [Google Scholar] [CrossRef] [PubMed]
- Pistelli, M.; Ballatore, Z.; Santinelli, A.; Biscotti, T.; Piva, F.; Occhipinti, G.; Della Mora, A.; Pagliacci, A.; Battelli, N.; Bastianelli, L.; et al. Phosphorylated mTOR is associated to androgen receptor expression in early triple-negative breast cancer. Oncol. Rep. 2016, 36, 755–762. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Robles, A.J.; Cai, S.; Cichewicz, R.H.; Mooberry, S.L. Selective activity of deguelin identifies therapeutic targets for androgen receptor-positive breast cancer. Breast Cancer Res. Treat. 2016, 157, 475–488. [Google Scholar] [CrossRef] [PubMed]
- Fry, D.W.; Harvey, P.J.; Keller, P.R.; Elliott, W.L.; Meade, M.A.; Trachet, E.; Albassam, M.; Zheng, X.X.; Leopold, W.R.; Pryer, N.K.; et al. Specific inhibition of cyclin-dependent kinase 4/6 by PD 0332991 and associated antitumor activity in human tumor xenografts. Mol. Cancer Ther. 2004, 3, 1427–1437. [Google Scholar] [PubMed]
- Toogood, P.L.; Harvey, P.J.; Repine, J.T.; Sheehan, D.J.; Vanderwel, S.N.; Zhou, H.; Keller, P.R.; Mcnamara, D.J.; Sherry, D.; Zhu, T.; et al. Discovery of a potent and selective inhibitor of cyclin-dependent kinase 4/6. J. Med. Chem. 2005, 48, 2388–2406. [Google Scholar] [CrossRef] [PubMed]
- Asghar, U.S.; Barr, A.R.; Cutts, R.; Beaney, M.; Babina, I.; Giltnane, J.; Lacap, J.A.; Crocker, L.; Young, A.; Herrera-abreu, M.T.; et al. Europe PMC Funders Group Single-cell dynamics determines response to CDK4/6 inhibition in triple negative breast cancer. Clin. Cancer Res. 2018, 23, 5561–5572. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Koo, J.; Park, H.S.; Kim, J.H.; Choi, S.Y.; Lee, J.H.; Park, B.W.; Lee, K.S. Expression of androgen receptors in primary breast cancer. Ann. Oncol. 2009, 21, 488–492. [Google Scholar] [CrossRef]
- Roseweir, A.K.; McCall, P.; Scott, A.; Liew, B.; Lim, Z.; Mallon, E.A.; Edwards, J. Phosphorylation of androgen receptors at serine 515 is a potential prognostic marker for triple negative breast cancer. Oncotarget 2017, 8, 37172–37185. [Google Scholar] [CrossRef] [PubMed]
- Koryakina, Y.; Ta, H.Q.; Gioeli, D. Androgen receptor phosphorylation: Biological context and functional consequences. Endocr. Relat. Cancer 2014, 21, T131–T145. [Google Scholar] [CrossRef] [PubMed]
- Bhattarai, S.; Klimov, S.; Mittal, K.; Krishnamurti, U.; Li, X.B.; Oprea-Ilies, G.; Wetherilt, C.S.; Riaz, A.; Aleskandarany, M.A.; Green, A.R.; et al. Prognostic role of androgen receptor in triple negative breast cancer: A multi-institutional study. Cancers 2019, 11, 995. [Google Scholar] [CrossRef]
- Collina, F.; Aquino, G.; Brogna, M.; Cipolletta, S.; Buonfanti, G.; De Laurentiis, M.; Di Bonito, M.; Cantile, M.; Botti, G. LncRNA HOTAIR up-regulation is strongly related with lymph nodes metastasis and LAR subtype of triple negative breast cancer. J. Cancer 2019, 10, 2018–2024. [Google Scholar] [CrossRef] [PubMed]
| First Author | Type of Study | n | AR threshold for Positivity | Method of AR Assessment | % of AR-Positive/LAR Tumors | Clinical Features (Only Results Relevant to Our Review are Presented) |
|---|---|---|---|---|---|---|
| Lehmann et al. [3] | Analysis of breast cancer data sets | 587 | No value applied | Gene expression analysis | 11% LAR | Patients in the LAR group were significantly older at diagnosis. |
| Kim et al. [24] | Retrospective study | 55 | Allred scoring method | IHC | 14.5% AR-positive | AR expression in TNBC was associated with older age at diagnosis (p = 0.006), smaller tumor size (p = 0.032) and lower histologic grade (p = 0.003). |
| Choi et al. [25] | Retrospective study | 492 | 1% | IHC | 17.7% AR-positive | AR expression showed significant correlation with older age (p < 0.001), lower histologic grade (p < 0.001). Poor prognostic marker for OS in univariate (p = 0.026) and multivariate (p = 0.008) analysis. |
| Guiu et al. [26] | Prospective study | 592 | 10% | IHC | 26% | AR-positive tumors had lower nuclear grades, appeared more often in older and postmenopausal women, exhibited less often lymphocytic infiltrate. No association between AR expression and tumor size, node involvement. |
| Tung et al. [27] | Retrospective study | 197 | Negative: <1% Weakly positive: 1–10% Positive: >10% | IHC | 18% | AR expression was less common in BRCA1. Factors predicting AR expression were: lower histologic grade, older age at diagnosis and PDL-1 expression. |
| Dieci et al. [28] | Retrospective study | 263 | 1% | IHC | 29.7% | AR expression was presented more frequently with older age (p > 0.001), G1-G2 (p = 0.003), lower Ki-67 (p < 0.001). |
| Astvatsaturyan et al. [29] | Retrospective study | 135 | 1%, 10%, 20%, 25%, 30% | IHC | 41% at 1% threshold | AR immunoreactivity in at least 1% of tumor cell nuclei was considered the most appropriate threshold to define AR positivity. Using this threshold AR-positive tumors were more frequently in older women, inverse relationship between Ki-67 and AR expression was found. |
| Sunar et al. [30] | Retrospective study | 84 | 1% | IHC | 29.8% | No statistically significant differences in terms of age, tumor size, lymph node metastasis. Grade 3 tumors were less frequent in AR-positive tumors. |
| Pistelli et al. [31] | Retrospective study | 81 | 10% | IHC | 18.8% | AR expression was inversely correlated with a higher Ki-67 and a lymphovascular invasion, but no other variables (age, menopausal status, size of tumor, histological features). |
| Park et al. [102] | Retrospective study | 413 | 10% | IHC | 35% | AR was significantly expressed in patients with smaller tumor size (p = 0.035) and lower histologic grade (p < 0.001). There were no statistically significant differences between AR expression and age at diagnosis, BMI, menopausal status, lymph node involvement. |
| Hu et al. [34] | Retrospective study | 360 | 10% | IHC | 31.4% | AR-positive tumors were more likely to have low Ki-67 (p = 0.007), observed in post-menopausal patients (p = 0.037), grade 3 (p = 0.007). AR expression was not correlated to patient age, tumor size, node status and vascular invasion. |
| Jongen et al. [32] | Retrospective study | 71 | AR-high: >34% AR-low: 1–34% >1%, >10%, <1% | IHC | 1% cut-off: 32% 10% cut-off: 27% Degrees: 15% AR-low 17% AR-high | Younger and premenopausal patients carried more AR-low tumors, AR-high tumors observed more frequent in older and postmenopausal patients. AR-negative in the middle regarding age. |
| Mohammed et al. [35] | Retrospective study | 89 | 1% | IHC | 32.6% | Ki-67 and histological grade were lower in AR-positive group. No significant association was observed between pCR and clinical-pathological features in AR-positive TNBC. |
| Mueller et al. [36] | Retrospective study | 135 | Not applicable | Subtyping using a panel of antibodies | 27.4% were LAR TNBC | Mammographic margins of LAR TNBC more often spiculated or presented as a mass with calcifications. |
| Collina et al. [37] | Retrospective study | 238 | 1% | IHC and expression of luminal cytokeratin for identification of LAR | LAR: 19% AR: 23% | AR expression was not correlated to menopausal condition, both in AR-positive and LAR TNBC patients. No correlation was also found with BMI, but a strong association between AR downregulation and diabetes was found. |
| Asano et al. [38] | Retrospective study | 190 | 1% | IHC | 29.5% | No correlation was found between clinicopathological characteristics and AR expression. |
| Rakha et al. [39] | Retrospective study | 1944 (of which 282 were TNBC) | 0% (negative) | IHC | 23% of TNBC cases | Absence of AR was associated with higher histological grade (p < 0.001), development of recurrences (p = 0.038) and distant metastasis (p = 0.049). |
| Thike et al. [40] | Retrospective study | 699 | 1% | IHC | 38% AR-positive | Androgen receptor expression was inversely correlated with histologic grade and mitotic score. |
| Shen et al. [41] | Retrospective study | 165 | 10% | IHC | 35.8% high levels of AR and 64.2% low levels of AR | Expression of AR was positively associated with tumor size, lymph node metastasis and high-grade tumor. |
| Bae et al. [42] | Retrospective study | 125 | 10% | IHC | 26.4% AR-positive | AR-positive TNBC is associated with calcifications, spiculated masses, and non-mass enhancement. |
| Candelaria et al. [43] | Prospective study | 144 | 10% | IHC | 31.2% AR-positive | AR-positive TNBC was significantly associated with heterogeneously dense breast composition on mammography, mass with calcifications, irregular mass shape on mammography, and irregular mass shape on sonography. |
| Kim et al. [44] | Retrospective study | 200 | 1% | IHC | 11% LAR | LAR subtype was associated with older patient age, apocrine histological features, low density of stromal tumor-infiltrating lymphocytes and low Ki-67 labeling index. |
| Santonja et al. [45] | retrospective study | 125 | 1% | IHC | 11.2% | LAR is the least proliferative subtype and the most chemoresistant one. |
| McNamara et al. [47] | Retrospective study | 39 | H score | IHC | Data not shown | AR status was concordant between primary and recurrent/metastatic disease, but coordinated expression of AR and androgenic enzymes was lost. There was an inverse association between AR and Ki-67. |
| Elfgen et al. [63] | Observational study | 166 | Semi-quantitative scoring system | IHC | 28.3% LAR | Lowest rate of missed malignant diagnoses on mammography was found in LAR. Lymph node metastasis was significantly more frequent in LAR. |
| Luo et al. [69] | Retrospective study | 137 TNBC and 132 non-TNBC | 1% (different scores were given to the percentage of positive cells and staining intensity) | IHC | 27.7% in TNBC and 83.3% in non-TNBC | Positive rate of AR was significantly lower in TNBC than non-TNBC. AR expression was correlated with menorrheal status (p = 0.009), tumor grade (p = 0.023), node status (p = 0.005), but was not correlated with clinicopathologic parameters and survival in non-TNBC. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brumec, M.; Sobočan, M.; Takač, I.; Arko, D. Clinical Implications of Androgen-Positive Triple-Negative Breast Cancer. Cancers 2021, 13, 1642. https://doi.org/10.3390/cancers13071642
Brumec M, Sobočan M, Takač I, Arko D. Clinical Implications of Androgen-Positive Triple-Negative Breast Cancer. Cancers. 2021; 13(7):1642. https://doi.org/10.3390/cancers13071642
Chicago/Turabian StyleBrumec, Maša, Monika Sobočan, Iztok Takač, and Darja Arko. 2021. "Clinical Implications of Androgen-Positive Triple-Negative Breast Cancer" Cancers 13, no. 7: 1642. https://doi.org/10.3390/cancers13071642
APA StyleBrumec, M., Sobočan, M., Takač, I., & Arko, D. (2021). Clinical Implications of Androgen-Positive Triple-Negative Breast Cancer. Cancers, 13(7), 1642. https://doi.org/10.3390/cancers13071642









