Exploring Older Women’s Attitudes to and Experience of Treatment for Advanced Ovarian Cancer: A Qualitative Phenomenological Study
Abstract
Simple Summary
Abstract
1. Introduction
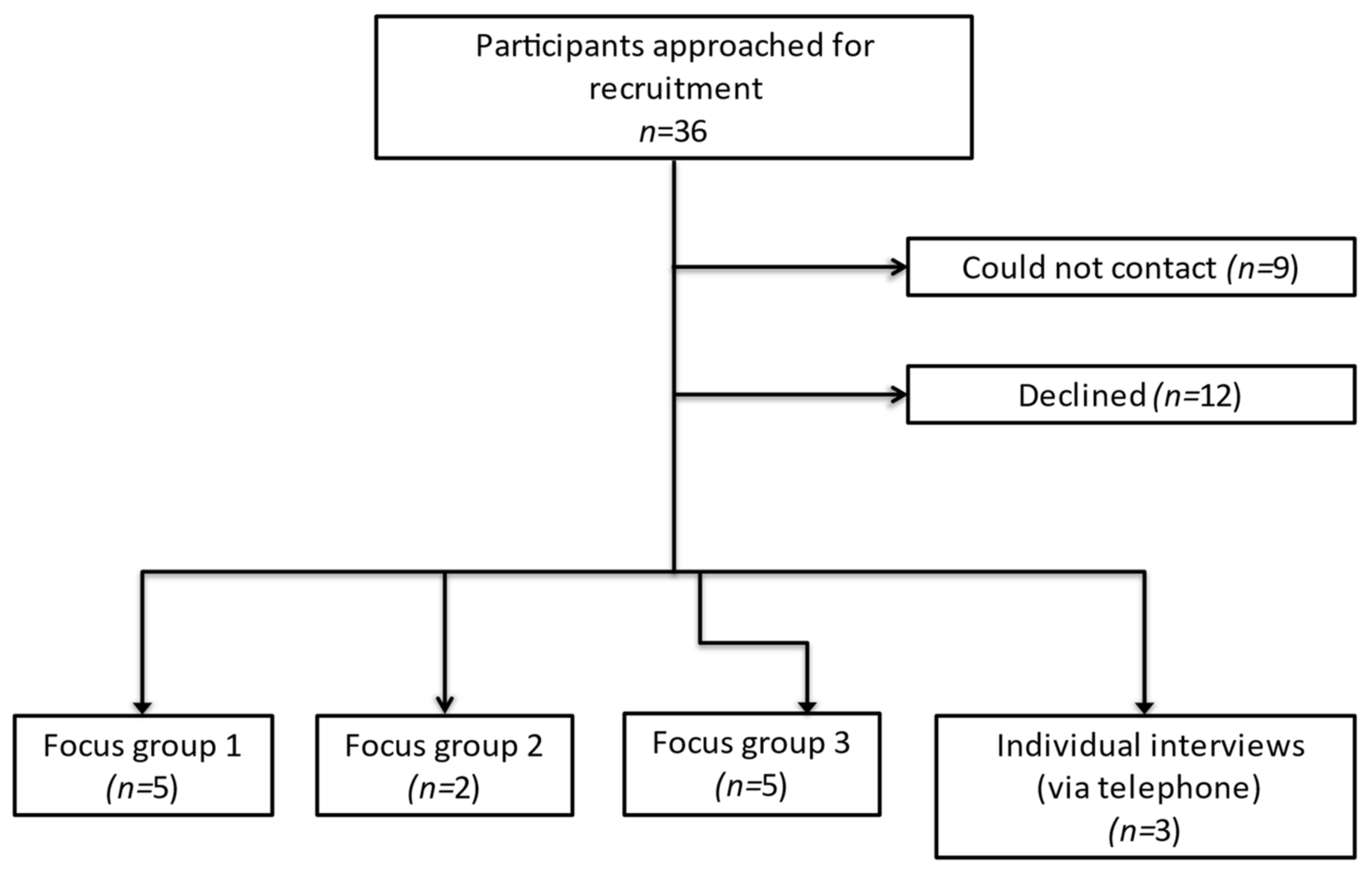
2. Materials and Methods
3. Results
3.1. Theme: Multifactorial Decision-Making
3.1.1. Subtheme: Reception and Retention of Information Clouds Decisions
“When you’re first diagnosed, it’s such a shock to you, you don’t absorb everything that’s being said.”(Patient 4, 82 years at diagnosis, receiving first-line chemotherapy)
“I sort of went into zombie mode, it never occurred to me to say no.”(Patient 12, 70 years at diagnosis, in follow up from first-line chemotherapy)
“I was desperately tired at this stage and an awful lot of information is given to you”.(Patient 14, 72 years at diagnosis, in follow up from first-line chemotherapy)
“Well I had to make the decision on the spot…so there was no time to think about it.”(Patient 14, 72 years at diagnosis, in follow up from first-line chemotherapy)
“I can’t bear looking on the internet, I just don’t want to know.”(Patient 8, 69 years at diagnosis, receiving chemotherapy for relapsed disease)
“You’ve gone through six months of chemo feeling blimmin awful for no … you know, nobody knows the answer.”(Patient 2, 78 years at diagnosis, receiving chemotherapy for relapsed disease)
3.1.2. Subtheme: Lengthening Life Expectancy
“I was told I could go profoundly deaf … but I had to take that chance.”(Patient 7, 74 years at diagnosis, in follow up from first-line chemotherapy)
“I would have done anything to have treatment, gone through anything.”(Patient 1, 77 years at diagnosis, in follow up from first-line chemotherapy)
“I’d still want to be alive because there’s other things I’m sure I’d be able to do.”(Patient 1, 77 years at diagnosis, in follow up from first-line chemotherapy)
3.1.3. Subtheme: Family Influence
“They didn’t want me to have six months or less to live, it’s not nice for them knowing one’s going to die so that’s why they said yes to chemo, to see how much longer it would give them.”(Patient 2, 78 years at diagnosis, receiving chemotherapy for relapsed disease)
“I think the thing that put most pressure on me was my husband being ill.”(Patient 13, 76 years at diagnosis, in follow up after first-line chemotherapy)
“I want to be here for him, rather than leaving him for my family to look after”(Patient 2, 78years at diagnosis, receiving chemotherapy for relapsed disease)
3.2. Theme: Burden of Logistical Issues
3.2.1. Subtheme: Care Coordination
“It’s like a blanket around you isn’t it.”(Patient 1, 77 years at diagnosis, in follow up from first-line chemotherapy)
“It’s just these things on the ground that you have to do as a patient when you’re feeling exhausted.”(Patient 14, 72 years at diagnosis, in follow up after first-line chemotherapy)
“I don’t actually know who my doctor is.”(Patient 4, 82 years at diagnosis, receiving first-line chemotherapy)
3.2.2. Subtheme: Transport
3.2.3. Subtheme: Informal Support
“Oh your family back you up don’t they.”(Patient 2, 78 years at diagnosis, receiving chemotherapy for relapsed disease)
“The only thing I can do is put my hand in the hand of god and you, I can’t do anything more”(Patient 8, 69 years at diagnosis, receiving chemotherapy for relapsed disease)
3.3. Theme: Side-Effects
3.3.1. Subtheme: Weighed Down by Side-Effects
“I was incredibly weak and then you still have to do things and you can’t manage it.”(Patient 11, 70 years at diagnosis, in follow up after first-line chemotherapy)
“It’s a matter of dragging my body around to keep up with essentials.”(Patient 14, 72 years at diagnosis, in follow up from first-line chemotherapy)
3.3.2. Subtheme: Determination Not to Let Cancer Interfere
“I just carry on as normal, I do my Pilates, I go to a club, but I’ve forgotten what it’s like to feel normal.”(Patient 1, 77 years at diagnosis, in follow up from first-line chemotherapy)
“I live life normally and I will go on like that until it’s my time to go.”(Patient 11, 70 years at diagnosis, in follow up after first-line chemotherapy)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cabasag, C.J.; Butler, J.; Arnold, M.; Rutherford, M.; Bardot, A.; Ferlay, J.; Morgan, E.; Møller, B.; Gavin, A.; Norell, C.H.; et al. Exploring variations in ovarian cancer survival by age and stage (ICBP SurvMark-2): A population-based study. Gynecol. Oncol. 2020, 157, 234–244. [Google Scholar] [CrossRef]
- Dumas, L.; Bowen, R.; Butler, J.; Banerjee, S. Under treatment of older patients with newly diagnosed epithelial ovarian cancer remains an issue. Cancers 2021, 13, 952. [Google Scholar] [CrossRef] [PubMed]
- Ferrero, A.; Fuso, L.; Tripodi, E.; Tana, R.; Daniele, A.; Zanfagnin, V.; Perotto, S.; Gadducci, A. Ovarian cancer in elderly patients: Patterns of care and treatment outcomes according to age and modified frailty index. Int. J. Gynecol. Cancer 2017, 27, 1863–1871. [Google Scholar] [CrossRef]
- Fourcadier, E.; Trétarre, B.; Gras-Aygon, C.; Ecarnot, F.; Daurès, J.P.; Bessaoud, F. Under-treatment of elderly patients with ovarian cancer: A population based study. BMC Cancer 2015, 15, 937. [Google Scholar] [CrossRef] [PubMed]
- Tew, W.P.; Muss, H.B.; Kimmick, G.G.; Von Gruenigen, V.E.; Lichtman, S.M. Breast and ovarian cancer in the older woman. J. Clin. Oncol. 2014, 32, 2553–2561. [Google Scholar] [CrossRef] [PubMed]
- Tew, W.P.; Fleming, G.F. Treatment of ovarian cancer in the older woman. Gynecol. Oncol. 2015, 136, 136–142. [Google Scholar] [CrossRef]
- Mohile, S.G.; Dale, W.; Somerfield, M.R.; Schonberg, M.A.; Boyd, C.M.; Burhenn, P.S.; Canin, B.; Cohen, H.J.; Holmes, H.M.; Hopkins, J.O.; et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J. Clin. Oncol. 2018, 36, 2326. [Google Scholar] [CrossRef]
- Woodard, S.; Nadella, P.C.; Kotur, L.; Wilson, J.; Burak, W.E.; Shapiro, C.L. Older women with breast carcinoma are less likely to receive adjuvant chemotherapy: Evidence of possible age bias? Cancer 2003, 98, 1141–1149. [Google Scholar] [CrossRef]
- Falandry, C.; Savoye, A.M.; Stefani, L.; Tinquaut, F.; Lorusso, D.; Herrstedt, J.; Bourbouloux, E.; Floquet, A.; Brachet, P.E.; Zannetti, A.; et al. EWOC-1: A randomized trial to evaluate the feasibility of three different first-line chemotherapy regimens for vulnerable elderly women with ovarian cancer (OC): A GCIG-ENGOT-GINECO study. J. Clin. Oncol. 2019, 37, 5508. [Google Scholar] [CrossRef]
- Nordin, A.J.; Chinn, D.J.; Moloney, I.; Naik, R.; de Barros Lopes, A.; Monaghan, J.M. Do elderly cancer patients care about cure? Attitudes to radical gynecologic oncology surgery in the elderly. Gynecol. Oncol. 2001, 81, 447–455. [Google Scholar] [CrossRef]
- Sattar, S.; Alibhai, S.M.H.; Fitch, M.; Krzyzanowska, M.; Leighl, N.; Puts, M.T.E. Chemotherapy and radiation treatment decision-making experiences of older adults with cancer: A qualitative study. J. Geriatr. Oncol. 2018, 9, 47–52. [Google Scholar] [CrossRef]
- Meropol, N.J.; Egleston, B.L.; Buzaglo, J.S.; Benson, A.B., III; Cegala, D.J.; Diefenbach, M.A.; Fleisher, L.; Miller, S.M.; Sulmasy, D.P.; Weinfurt, K.P.; et al. Cancer patient preferences for quality and length of life. Cancer 2008, 113, 3459–3466. [Google Scholar] [CrossRef]
- De Celis, E.S.P.; Li, D.; Sun, C.-L.; Kim, H.; Twardowski, P.; Fakih, M. Patient-defined goals and preferences among older adults with cancer starting chemotherapy (CT). J. Clin. Oncol. 2018, 36, 10009. [Google Scholar] [CrossRef]
- Shrestha, A.; Martin, C.; Burton, M.; Walters, S.; Collins, K.; Wyld, L. Quality of life versus length of life considerations in cancer patients: A systematic literature review. Psychooncology 2019, 28, 1367–1380. [Google Scholar] [CrossRef]
- Committee for Human Medicinal Products. Adequacy of Guidance on the Elderly Regarding Medicinal Products for Human Use; European Medicines Agency: London, UK, 2007; pp. 1–28. [Google Scholar]
- Lambert, S.D.; Loiselle, C.G. Combining individual interviews and focus groups to enhance data richness. J. Adv. Nurs. 2008, 62, 228–237. [Google Scholar] [CrossRef]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic Analysis: Striving to Meet the Trustworthiness Criteria. Int. J. Qual. Methods 2017, 16, 1609406917733847. [Google Scholar] [CrossRef]
- Saldaña, J. The Coding Manual for Qualitative Researchers; Sage: Los Angeles, CA, USA, 2015. [Google Scholar]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Sun, C.L.; Kim, H.; Chung, V.; Koczywas, M.; Fakih, M.; Chao, J.; Chien, L.; Charles, K.; Fernandes Dos Santos Hughes, S.; et al. Geriatric assessment-driven intervention (GAIN) on chemotherapy toxicity in older adults with cancer: A randomized controlled trial. J. Clin. Oncol. 2020, 38, 12010. [Google Scholar] [CrossRef]
- Mohile, S.G.; Mohamed, M.R.; Culakova, E.; Xu, H.; Loh, K.P.; Magnuson, A.; Flannery, M.A.; Ramsdale, E.E.; Dunne, R.F.; Gilmore, N.; et al. A geriatric assessment (GA) intervention to reduce treatment toxicity in older patients with advanced cancer: A University of Rochester Cancer Center NCI community oncology research program cluster randomized clinical trial (CRCT). J. Clin. Oncol. 2020, 38, 12009. [Google Scholar] [CrossRef]
- Fabi, A.; Bhargava, R.; Fatigoni, S.; Guglielmo, M.; Horneber, M.; Roila, F.; Weis, J.; Jordan, K.; Ripamonti, C.I. Cancer-related fatigue: ESMO Clinical Practice Guidelines for diagnosis and treatment. Ann. Oncol. 2020, 31, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Tate, A.R.; Nicholson, A.; Cassell, J.A. Are GPs under-investigating older patients presenting with symptoms of ovarian cancer Observational study using General Practice Research Database. Br. J. Cancer 2010, 102, 947–951. [Google Scholar] [CrossRef]
- National Cancer Intelligence Network. Routes to Diagnosis 2015 Update: Ovarian Cancer n.d. Available online: http://www.ncin.org.uk/publications/data_briefings/ (accessed on 19 November 2019).
- Gaston, C.M.; Mitchell, G. Information giving and decision-making in patients with advanced cancer: A systematic review. Soc. Sci. Med. 2005, 61, 2252–2264. [Google Scholar] [CrossRef]
- Costanzo, E.S.; Lutgendorf, S.K.; Rothrock, N.E.; Anderson, B. Coping and quality of life among women extensively treated for gynecologic cancer. Psychooncology 2006, 15, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Baitar, A.; Buntinx, F.; De Burghgraeve, T.; Deckx, L.; Schrijvers, D.; Wildiers, H.; van den Akker, M. The influence of coping strategies on subsequent wellbeing in older patients with cancer: A comparison with 2 control groups. Psychooncology 2018, 27, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Hernández, R.; Calderon, C.; Carmona-Bayonas, A.; Rodríguez Capote, A.; Jara, C.; Padilla Álvarez, A.; Gómez-Camacho, M.D.L.N.; Beato, C.; Castelo, B.; Majem, M.; et al. Differences in coping strategies among young adults and the elderly with cancer. Psychogeriatrics 2019, 19, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Long Roche, K.; Angarita, A.M.; Cristello, A.; Lippitt, M.; Haider, A.H.; Bowie, J.V.; Fader, A.N.; Tergas, A.I. “Little big things”: A qualitative study of ovarian cancer survivors and their experiences with the health care system. J. Oncol. Pract. 2016, 12, e974–e980. [Google Scholar] [CrossRef]
- Leppin, A.; Montori, V.; Gionfriddo, M. Minimally Disruptive Medicine: A Pragmatically Comprehensive Model for Delivering Care to Patients with Multiple Chronic Conditions. Healthcare 2015, 3, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Ridgeway, J.L.; Egginton, J.S.; Tiedje, K.; Linzer, M.; Boehm, D.; Poplau, S.; de Oliveira, D.R.; Odell, L.; Montori, V.M.; Eton, D.T. Factors that lessen the burden of treatment in complex patients with chronic conditions: A qualitative study. Patient Prefer Adherence 2014, 8, 339–351. [Google Scholar] [CrossRef]
| Question |
|---|
| 1. What were the biggest challenges you faced while receiving treatment? |
| 2. Do you feel, before starting treatment, that you had a good idea of the potential risks and benefits of treatment? |
| 3. Is there any information you wish you had received that you didn’t prior to starting chemotherapy? |
| 4. What were your main goals of treatment/Why did you decide to have treatment? |
| 5. How much did the opinions of your clinicians impact on your decision to have treatment? |
| 6. How much did the feelings and opinions of your family and friends impact on your decision to have treatment? |
| 7. Knowing now the side-effects you have experienced, would you make the same decision again to undergo treatment? |
| 8. When you think about your health, what would you say the term quality of life means to you? |
| 9. With that in mind, in what ways has your diagnosis and treatment for ovarian cancer affected your quality of life? |
| 10. If you experienced side effects during treatment, did you feel well-supported? |
| 11. How well do you think your GP * and other community teams were kept informed of your progress during treatment? |
| Patient Characteristic | n | (%) |
|---|---|---|
| Living situation | ||
| Lives alone | 6 | (40.0) |
| Lives with spouse | 6 | (40.0) |
| Lives with other family members | 2 | (13.3) |
| Lives in sheltered accommodation | 1 | (6.7) |
| Has caring responsibilities | 4 | (26.7) |
| Employment status | ||
| Retired | 14 | (93.3) |
| Financial impact | ||
| Cancer has had no financial impact | 13 | (86.7) |
| Cancer has had a little financial impact | 2 | (13.3) |
| Stage at diagnosis | ||
| 1 | 0 | (0) |
| 2 | 4 | (26.7) |
| 3 | 9 | (60.0) |
| 4 | 2 | (13.3) |
| Primary treatment | ||
| Platinum doublet chemotherapy | 12 | (80.0) |
| Single-agent carboplatin | 3 | (20.0) |
| Surgery | 11 | (73.3) |
| Primary treatment tolerance | ||
| No delays | 6 | (40.0) |
| Delay 1 week or less | 3 | (20.0) |
| Delay >/= 2 weeks | 2 | (13.3) |
| Dose reduction at beginning | 0 | (0) |
| Dose reduction during chemotherapy | 4 | (26.7) |
| Has had disease recurrence | 8 | (53.3) |
| Second line treatment | ||
| Chemotherapy (doublet) | 3 | (20.0) |
| Chemotherapy (single agent) | 2 | (13.3) |
| Clinical Trial | 2 | (13.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dumas, L.; Lidington, E.; Appadu, L.; Jupp, P.; Husson, O.; Banerjee, S. Exploring Older Women’s Attitudes to and Experience of Treatment for Advanced Ovarian Cancer: A Qualitative Phenomenological Study. Cancers 2021, 13, 1207. https://doi.org/10.3390/cancers13061207
Dumas L, Lidington E, Appadu L, Jupp P, Husson O, Banerjee S. Exploring Older Women’s Attitudes to and Experience of Treatment for Advanced Ovarian Cancer: A Qualitative Phenomenological Study. Cancers. 2021; 13(6):1207. https://doi.org/10.3390/cancers13061207
Chicago/Turabian StyleDumas, Lucy, Emma Lidington, Laura Appadu, Philippa Jupp, Olga Husson, and Susana Banerjee. 2021. "Exploring Older Women’s Attitudes to and Experience of Treatment for Advanced Ovarian Cancer: A Qualitative Phenomenological Study" Cancers 13, no. 6: 1207. https://doi.org/10.3390/cancers13061207
APA StyleDumas, L., Lidington, E., Appadu, L., Jupp, P., Husson, O., & Banerjee, S. (2021). Exploring Older Women’s Attitudes to and Experience of Treatment for Advanced Ovarian Cancer: A Qualitative Phenomenological Study. Cancers, 13(6), 1207. https://doi.org/10.3390/cancers13061207







