Prognostic Significance of Prostate-Specific Antigen Persistence after Radical Prostatectomy: A Systematic Review and Meta-Analysis
Abstract
Simple Summary
Abstract
1. Introduction
2. Results
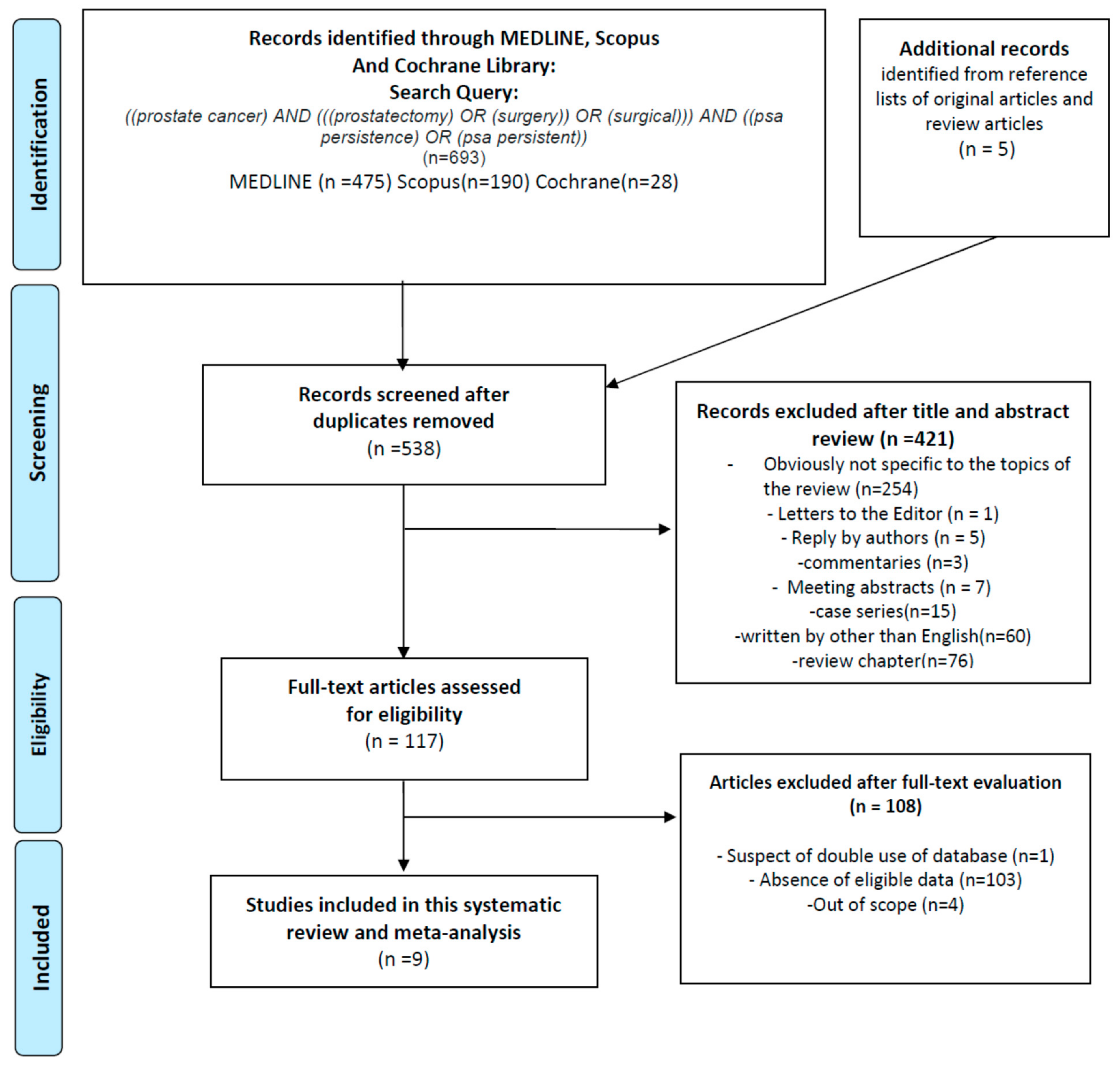
2.1. Study Selection and Characteristics
2.2. Meta-Analysis
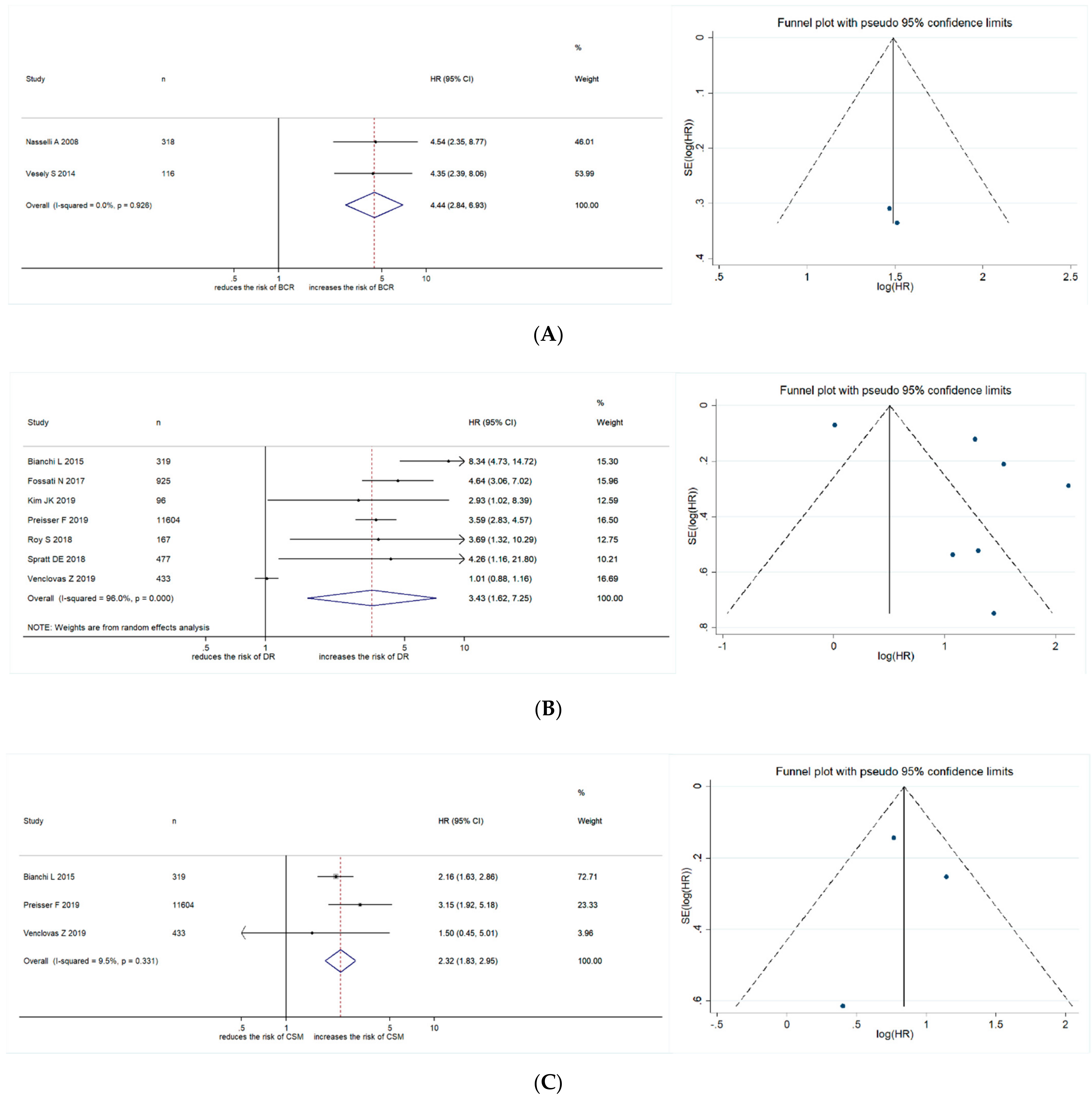
2.2.1. Association between PSA Persistence and BCR
2.2.2. Association between PSA Persistence and Disease Recurrence
2.2.3. Association between PSA Persistence and CSM
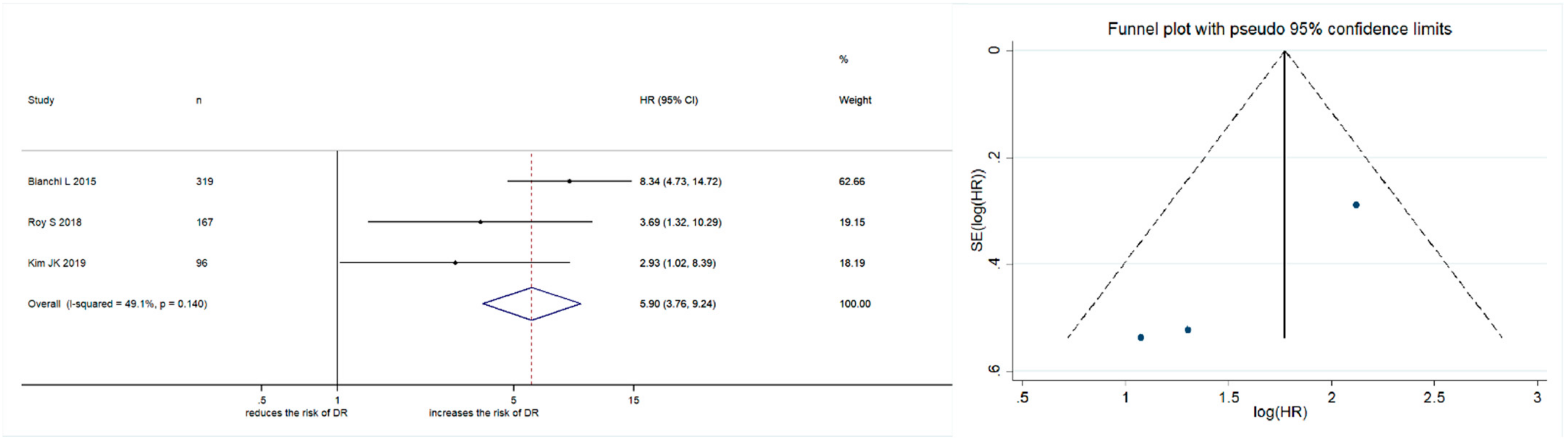
2.2.4. Subgroup Analysis
3. Discussion
4. Materials and Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA A Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef]
- Gallina, A.; Chun, F.K.-H.; Suardi, N.; Eastham, J.A.; Perrotte, P.; Graefen, M.; Hutterer, G.; Huland, H.; Klein, E.A.; Reuther, A.; et al. Comparison of stage migration patterns between Europe and the USA: An analysis of 11 350 men treated with radical prostatectomy for prostate cancer. BJU Int. 2008, 101, 1513–1518. [Google Scholar] [CrossRef] [PubMed]
- EAU-ESTRO-SIOG Guidelines on Prostate Cancer. 2020. Available online: https://uroweb.org/guidelines/ (accessed on 28 October 2020).
- Pound, C.R.; Partin, A.W.; Eisenberger, M.A.; Chan, D.W.; Pearson, J.D.; Walsh, P.C. Natural history of progression after PSA elevation following radical prostatectomy. JAMA 1999, 281, 1591–1597. [Google Scholar] [CrossRef] [PubMed]
- Shariat, S.F.; Kattan, M.W.; Vickers, A.J.; Karakiewicz, P.I.; Scardino, P.T. Critical review of prostate cancer predictive tools. Futur. Oncol. 2009, 5, 1555–1584. [Google Scholar] [CrossRef]
- Stamey, T.A.; Kabalin, J.N.; McNeal, J.E.; Johnstone, I.M.; Freiha, F.; Redwine, E.A.; Yang, N. Prostate Specific Antigen in the Diagnosis and Treatment of Adenocarcinoma of the Prostate. II. Radical Prostatectomy Treated Patients. J. Urol. 1989, 141, 1076–1083. [Google Scholar] [CrossRef]
- Bianchi, L.; Nini, A.; Bianchi, M.; Gandaglia, G.; Fossati, N.; Suardi, N.; Moschini, M.; Dell’Oglio, P.; Schiavina, R.; Montorsi, F.; et al. The Role of Prostate-specific Antigen Persistence after Radical Prostatectomy for the Prediction of Clinical Progression and Cancer-specific Mortality in Node-positive Prostate Cancer Patients. Eur. Urol. 2016, 69, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Fossati, N.; Karnes, R.J.; Colicchia, M.; Boorjian, S.A.; Bossi, A.; Seisen, T.; Di Muzio, N.; Cozzarini, C.; Chiorda, B.N.; Fiorino, C.; et al. Impact of Early Salvage Radiation Therapy in Patients with Persistently Elevated or Rising Prostate-specific Antigen After Radical Prostatectomy. Eur. Urol. 2018, 73, 436–444. [Google Scholar] [CrossRef]
- Kim, J.K.; Jeong, C.W.; Ku, J.H.; Kim, H.H.; Kwak, C. Prostate specific antigen (PSA) persistence 6 weeks after radical prostatectomy and pelvic lymph node dissection as predictive factor of radiographic progression in node-positive prostate cancer patients. J. Cancer 2019, 10, 2237–2242. [Google Scholar] [CrossRef]
- Naselli, A.; Introini, C.; Andreatta, R.; Spina, B.; Truini, M.; Puppo, P. Prognostic factors of persistently detectable PSA after radical prostatectomy. Int. J. Urol. 2009, 16, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Preisser, F.; Chun, F.K.; Pompe, R.S.; Heinze, A.; Salomon, G.; Graefen, M.; Huland, H.; Tilki, D. Persistent Prostate-Specific Antigen After Radical Prostatectomy and Its Impact on Oncologic Outcomes. Eur. Urol. 2019, 76, 106–114. [Google Scholar] [CrossRef]
- Roy, S.; Sia, M.; Tyldesley, S.; Bahl, G. Pathologically Node-Positive Prostate Carcinoma—Prevalence, Pattern of Care and Outcome from a Population-Based Study. Clin. Oncol. 2019, 31, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Spratt, D.E.; Dai, D.L.; Den, R.B.; Troncoso, P.; Yousefi, K.; Ross, A.E.; Schaeffer, E.M.; Haddad, Z.; Davicioni, E.; Mehra, R.; et al. Performance of a Prostate Cancer Genomic Classifier in Predicting Metastasis in Men with Prostate-specific Antigen Persistence Postprostatectomy. Eur. Urol. 2018, 74, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Venclovas, Z.; Jievaltas, M.; Milonas, D. Significance of Time Until PSA Recurrence After Radical Prostatectomy Without Neo- or Adjuvant Treatment to Clinical Progression and Cancer-Related Death in High-Risk Prostate Cancer Patients. Front. Oncol. 2019, 9. [Google Scholar] [CrossRef] [PubMed]
- Vesely, S.; Jarolím, L.; Duskova, K.; Schmidt, M.; Dusek, P.; Babjuk, M. The use of early postoperative prostate-specific antigen to stratify risk in patients with positive surgical margins after radical prostatectomy. BMC Urol. 2014, 14, 79. [Google Scholar] [CrossRef]
- Partin, A.W.; Oesterling, J.E. The Clinical Usefulness of Prostate Specific Antigen: Update 1994. J. Urol. 1994, 152, 1358–1368. [Google Scholar] [CrossRef]
- Abdollah, F.; Suardi, N.; Gallina, A.; Bianchi, M.; Tutolo, M.; Passoni, N.; Fossati, N.; Sun, M.; Dell’Oglio, P.; Salonia, A.; et al. Extended pelvic lymph node dissection in prostate cancer: A 20-year audit in a single center. Ann. Oncol. 2013, 24, 1459–1466. [Google Scholar] [CrossRef]
- Abdollah, F.; Sun, M.; Thuret, R.; Budäus, L.; Jeldres, C.; Graefen, M.; Briganti, A.; Perrotte, P.; Rigatti, P.; Montorsi, F.; et al. Decreasing Rate and Extent of Lymph Node Staging in Patients Undergoing Radical Prostatectomy May Undermine the Rate of Diagnosis of Lymph Node Metastases in Prostate Cancer. Eur. Urol. 2010, 58, 882–892. [Google Scholar] [CrossRef] [PubMed]
- Briganti, A.; Blute, M.L.; Eastham, J.H.; Graefen, M.; Heidenreich, A.; Karnes, J.R.; Montorsi, F.; Studer, U.E. Pelvic Lymph Node Dissection in Prostate Cancer. Eur. Urol. 2009, 55, 1251–1265. [Google Scholar] [CrossRef]
- Abdollah, F.; Karnes, R.J.; Suardi, N.; Cozzarini, C.; Gandaglia, G.; Fossati, N.; Bianchi, M.; Boorjian, S.A.; Sun, M.; Karakiewicz, P.I.; et al. Predicting Survival of Patients with Node-positive Prostate Cancer Following Multimodal Treatment. Eur. Urol. 2014, 65, 554–562. [Google Scholar] [CrossRef] [PubMed]
- Briganti, A.; Karnes, J.R.; Da Pozzo, L.F.; Cozzarini, C.; Gallina, A.; Suardi, N.; Bianchi, M.; Freschi, M.; Doglioni, C.; Fazio, F.; et al. Two positive nodes represent a significant cut-off value for cancer specific survival in patients with node positive prostate cancer. A new proposal based on a two-institution experience on 703 consecutive N+ patients treated with radical prostatectomy, extended pelvic lymph node dissection and adjuvant therapy. Eur. Urol. 2009, 55, 261–270. [Google Scholar]
- Schumacher, M.C.; Burkhard, F.C.; Thalmann, G.N.; Fleischmann, A.; Studer, U.E. Good Outcome for Patients with Few Lymph Node Metastases After Radical Retropubic Prostatectomy. Eur. Urol. 2008, 54, 344–352. [Google Scholar] [CrossRef]
- Brockman, J.A.; Alanee, S.; Vickers, A.J.; Scardino, P.T.; Wood, D.P.; Kibel, A.S.; Lin, D.W.; Bianco, F.J., Jr.; Rabah, D.M.; Klein, E.A.; et al. Nomogram Predicting Prostate Cancer–specific Mortality for Men with Biochemical Recurrence After Radical Prostatectomy. Eur. Urol. 2015, 67, 1160–1167. [Google Scholar] [CrossRef]
- Walz, J.; Chun, F.K.-H.; Klein, E.A.; Reuther, A.; Saad, F.; Graefen, M.; Huland, H.; Karakiewicz, P.I. Nomogram Predicting the Probability of Early Recurrence After Radical Prostatectomy for Prostate Cancer. J. Urol. 2009, 181, 601–608. [Google Scholar] [CrossRef]
- D’Amico, A.V.; Whittington, R.; Malkowicz, S.B.; Cote, K.; Loffredo, M.; Schultz, D.; Chen, M.H.; Tomaszewski, J.E.; Renshaw, A.A.; Wein, A.; et al. Biochemical outcome after radical prostatectomy or external beam radiation therapy for patients with clinically localized prostate carcinoma in the prostate specific antigen era. Cancer 2002, 95, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Verze, P.; Scuzzarella, S.; Martina, G.R.; Giummelli, P.; Cantoni, F.; Mirone, V. Long-term oncological and functional results of extraperitoneal laparoscopic radical prostatectomy: One surgical team’s experience on 1,600 consecutive cases. World J. Urol. 2013, 31, 529–534. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P. Cochrane Handbook for Systematic Reviews of Intervensions Version 5.1.0 (Updated March 2011). Cochrane Collab, 2011. Available online: https://handbook-5-1.cochrane.org (accessed on 17 October 2020).
- DerSimonian, R.; Kacker, R. Random-effects model for meta-analysis of clinical trials: An update. Contemp. Clin. Trials 2007, 28, 105–114. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; Van Der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing Bias in Studies of Prognostic Factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Dinnes, J.; D’Amico, R.; Sowden, A.J.; Sakarovitch, C.; Song, F.; Petticrew, M.; Altman, D.G. Evaluating non-randomised intervention studies. Heal. Technol. Assess. 2003, 7, 1–173. [Google Scholar] [CrossRef] [PubMed]
| Author and Year | Region | Design | Recruitment Period | No. pts | Operation Modality | Reported Outcomes | NOS | Funding Source |
|---|---|---|---|---|---|---|---|---|
| Nasselli A 2008 | Italy | R cohort | 2002–2007 | 318 | ORP | BCR | 6 | NR |
| Vesely S 2014 | Czech | R case-control | 2001–2012 | 116 | ORP or LRP | BCR | 5 | NR |
| Bianchi L 2015 | Italy | R cohort | 1998–2013 | 319 | NR | Disease recurrence, CSM | 7 | None |
| Fossati N 2017 | EU | R cohort | 1996–2009 | 925 | NR | Disease recurrence | 7 | None |
| Roy S 2018 | Canada | R cohort e | 2005–2014 | 167 | NR | Disease recurrence | 6 | Sanofi and Bayer Health Care Pharmaceuticals |
| Spratt DE 2018 | US | R cohort | 1990–2015 | 477 | NR | Disease recurrence | 6 | GenomeDx Biosciences |
| Kim JK 2019 | Korea | R cohort | 2002–2014 | 96 | ORP or RARP | Disease recurrence | 6 | The National Research Foundation of Korea |
| Preisser F 2019 | Germany | R cohort | 1992–2016 | 11,604 | ORP or RARP | Disease recurrence, CSM, OM | 7 | None |
| Venclovas Z 2019 | Lithuania | R case-control | 2001–2017 | 433 | ORP | Disease recurrence, CSM | 5 | NR |
| Author and Year | Median F/U (Overall or Undetectable vs. Persistence) | Median age (Overall or Undetectable vs. Persistence) | Median iPSA (IQR) <Overall or Undetectable vs. Persistence> | GS ≥ 8 | ≥pT3a | PSM | pN+ | n. PSA Persistence | n. Postoperative RT |
|---|---|---|---|---|---|---|---|---|---|
| Nasselli A 2008 | NR | 65 | 7 (NR) | 77(24.2%) (GS ≥ 4 + 3) | 79(24.8%) | 89(28.0%) | 20(6.3%) | 33(10.4%) | NR |
| Vesely S 2014 | 31.4 months | 64 | 9.2(2.9–38.2) | 59(51%) (GS ≥ 3 + 4) | 62(53.4%) | 116(100%) | NR | NR | NR |
| Bianchi L 2015 | 53 months | 65 | 11.1(7–23.3) | 156(52.5%) | 278(87.1%) | 169(53.0%) | 319(100%) | 83(26%) | ART 200(62.7%) |
| Fossati N 2017 | 8 years | 65 | 8.0(5.6–13.5) | 228(24%) | 519(56%) | 403(44%) | 0 | 224 (24.2%) | 925(100%) |
| Roy S 2018 | 48 months | 64 | 12.5(8.2–21.5) | 102(61.3%) | 156(94%) | 117(70%) | 167(100%) | NR | 63(37.7%) |
| Spratt DE 2018 | 57 months | 60 | 6.4 (NR) | NR | 242(51.6%) | 229(48.0%) | 38(8.0%) | 150(31.4%) | NR |
| Kim JK 2019 | 45 months | 67 | 30.5 (NR) vs. 30.6 (NR) | 39(40.6%) | 89(92.7%) | 73(76%) | 96(100%) | 52(54.2%) | ART 20(20.8%) |
| Preisser F 2019 | 61.8 months vs. 46.4 months | 64.6 vs. 64.2 | 6.6 (4.7–9.7) vs. 11.2 (6.8–19.8) | NR | 3764(32.5%) | 2042(17.6%) | 699(6.0%) | 1025(8.8%) | 1815(15.6%) |
| Venclovas Z 2019 | 64 months | 65 | NR | 189(43.6%) | 295(68.1%) | 188(43.4%) | 56(12.9%) | 130(30%) | NR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kimura, S.; Urabe, F.; Sasaki, H.; Kimura, T.; Miki, K.; Egawa, S. Prognostic Significance of Prostate-Specific Antigen Persistence after Radical Prostatectomy: A Systematic Review and Meta-Analysis. Cancers 2021, 13, 948. https://doi.org/10.3390/cancers13050948
Kimura S, Urabe F, Sasaki H, Kimura T, Miki K, Egawa S. Prognostic Significance of Prostate-Specific Antigen Persistence after Radical Prostatectomy: A Systematic Review and Meta-Analysis. Cancers. 2021; 13(5):948. https://doi.org/10.3390/cancers13050948
Chicago/Turabian StyleKimura, Shoji, Fumihiko Urabe, Hiroshi Sasaki, Takahiro Kimura, Kenta Miki, and Shin Egawa. 2021. "Prognostic Significance of Prostate-Specific Antigen Persistence after Radical Prostatectomy: A Systematic Review and Meta-Analysis" Cancers 13, no. 5: 948. https://doi.org/10.3390/cancers13050948
APA StyleKimura, S., Urabe, F., Sasaki, H., Kimura, T., Miki, K., & Egawa, S. (2021). Prognostic Significance of Prostate-Specific Antigen Persistence after Radical Prostatectomy: A Systematic Review and Meta-Analysis. Cancers, 13(5), 948. https://doi.org/10.3390/cancers13050948







