The Role of VEGF Receptors as Molecular Target in Nuclear Medicine for Cancer Diagnosis and Combination Therapy
Abstract
Simple Summary
Abstract
1. Introduction
2. VEGF/VEGFRs System in Angiogenesis and AAT
2.1. VEGF Glycoproteins
2.2. VEGF Receptors and Their Co-Receptors
2.3. Anti-Angiogenic Therapy Strategies for Tumour Treatment
3. The Role of VEGFR and Their Ligands in Combination Targeted Radionuclide Tumour Treatment
3.1. Radiolabelled VEGF Ligands and Their Derivatives
3.2. Radiolabelled Anti-VEGF and Anti-VEGFR Antibodies
3.3. Radiolabelled Peptide-Like Structure Ligands Used for VEGF/VEGFR Imaging
3.4. Radiolabelled Small Molecular Inhibitors of VEGFR Tyrosine Kinase
3.5. Radiolabelled Peptide-Like Ligands for NRP-1 Imaging
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| AATs | anti-angiogenic therapies |
| AKT | protein kinase B |
| BSA | bovine serum albumin |
| BV | bevacizumab |
| C-tag | cysteine-tag |
| DAG | diacylglicerole |
| DIPG | diffuse intrinsic pontine glioma |
| EC | ethylene dicysteine |
| eNOS | endothelial nitric oxide synthase |
| Fab | antigen-binding fragment |
| FAK | focal adhesion kinase |
| HIF-1 | hypoxia inducible factor-1 |
| hnTf | human transferrin |
| IL-1b | interleukin 1b |
| IP3 | inositol triphosphate |
| mAb | monoclonal antibody |
| MBs | microbubbles |
| NIRF | near-infrared fluorescent |
| NRP | neuropilin |
| NSCLC | non-small cell lung cancer |
| N-suc-Df | N-succinyl-desferrioxamine |
| PIP2 | phosphatidylinositol bisphosphate |
| PLC-γ | phospholipase C-gamma |
| PlGF | placental growth factor |
| PKC | protein kinase C |
| PS | polymersome |
| QD | quantum dot |
| Ram | ramucirumab |
| Ran | ranibizumab |
| RTKs | receptor tyrosine kinases |
| scVEGF | single-chain vascular endothelial growth factor |
| SFB | N-succinimidyl-4-fluorobenzoate |
| sVEGFR | soluble vascular endothelial growth factor receptor |
| TNF-α | tumour necrosis factor alpha |
| TPPs | tumour penetrating peptides |
| VEGF | vascular endothelial growth factor |
| VEGFR | vascular endothelial growth factor receptor |
| VHL | von Hippel–Lindau |
| VRAPs | VEGFR-associated proteins |
References
- Ferrara, N. VEGF and the quest for tumour angiogenesis factors. Nat. Rev. Cancer 2002, 2, 795–803. [Google Scholar] [CrossRef]
- Ferrara, N.; Gerber, H.P.; LeCouter, J. The biology of VEGF and its receptors. Nat. Med. 2003, 9, 669–676. [Google Scholar] [CrossRef]
- Zhu, L.; Niu, G.; Fang, X.; Chen, X. Preclinical molecular imaging of tumor angiogenesis. Q. J. Nucl. Med. Mol. Imaging 2010, 54, 291–308. [Google Scholar] [PubMed]
- Rahimi, N. Vascular endothelial growth factor receptors: Molecular mechanisms of activation and therapeutic potentials. Exp. Eye Res. 2006, 83, 1005–1016. [Google Scholar] [CrossRef]
- Kiselyov, A.; Balakin, K.V.; Tkachenko, S.E. VEGF/VEGFR signalling as a target for inhibiting angiogenesis. Expert Opin. Investig. Drugs 2007, 16, 83–107. [Google Scholar] [CrossRef]
- Zhang, L.; Xu, J.S.; Sanders, V.M.; Letson, A.D.; Roberts, C.J.; Xu, R.X. Multifunctional microbubbles for image-guided antivascular endothelial growth factor therapy. J. Biomed. Opt. 2010, 15, 030515. [Google Scholar] [CrossRef]
- Arjaans, M.; Schröder, C.P.; Oosting, S.F.; Dafni, U.; Kleibeuker, J.E.; de Vries, E.G. VEGF pathway targeting agents, vessel normalization and tumor drug uptake: From bench to bedside. Oncotarget 2016, 7, 21247–21258. [Google Scholar] [CrossRef]
- Tortora, G.; Melisi, D.; Ciardiello, F. Angiogenesis: A target for cancer therapy. Curr. Pharm. Des. 2004, 10, 11–26. [Google Scholar] [CrossRef] [PubMed]
- Kubo, K.; Shimizu, T.; Ohyama, S.; Murooka, H.; Iwai, A.; Nakamura, K.; Hasegawa, K.; Kobayashi, Y.; Takahashi, N.; Takahashi, K.; et al. Novel Potent Orally Active Selective VEGFR-2 Tyrosine Kinase Inhibitors: Synthesis, Structure—Activity Relationships, and Antitumor Activities of N-Phenyl-N′-{4-(4-quinolyloxy)phenyl}ureas. J. Med. Chem. 2005, 48, 1359–1366. [Google Scholar] [CrossRef]
- Wedge, S.R.; Kendrew, J.; Hennequin, L.F.; Valentine, P.J.; Barry, S.T.; Brave, S.R.; Smith, N.R.; James, N.H.; Dukes, M.; Curwen, J.O.; et al. AZD2171: A highly potent, orally bioavailable, vascular endothelial growth factor receptor-2 tyrosine kinase inhibitor for the treatment of cancer. Cancer Res. 2005, 65, 4389–4400. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, A.; von Wronski, M.A.; Sato, A.K.; Dransfield, D.T.; Sexton, D.; Bogdan, N.; Pillai, R.; Nanjappan, P.; Song, B.; Marinelli, E.; et al. A distinct strategy to generate high-affinity peptide binders to receptor tyrosine kinases. Protein Eng. Des. Sel. 2005, 18, 417–424. [Google Scholar] [CrossRef]
- Roskoski, R., Jr. Sunitinib: A VEGF and PDGF receptor protein kinase and angiogenesis inhibitor. BioChem. Biophys. Res. Commun. 2007, 356, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Rüegg, C.; Hasmim, M.; Lejeune, F.J.; Alghisi, G.C. Antiangiogenic peptides and proteins: From experimental tools to clinical drugs. Biochim. Biophys. Acta 2006, 1765, 155–177. [Google Scholar] [CrossRef]
- Le Tourneau, C.; Raymond, E.; Faivre, S. Sunitinib: A novel tyrosine kinase inhibitor. A brief review of its therapeutic potential in the treatment of renal carcinoma and gastrointestinal stromal tumors (GIST). Ther. Clin. Risk Manag. 2007, 3, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Murukesh, N.; Dive, C.; Jayson, G.C. Biomarkers of angiogenesis and their role in the development of VEGF inhibitors. Br. J. Cancer 2010, 102, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Backer, M.V.; Backer, J.M. Imaging key biomarkers of tumor angiogenesis. Theranostics 2012, 2, 502–515. [Google Scholar] [CrossRef]
- Muñoz, C.; Adasen, F.; Alzate-Morales, J.; Vergara, A.; Kniess, T.; Caballero, J. Study of differences in the VEGFR2 inhibitory activities between semaxanib and SU5205 using 3D-QSAR, docking, and molecular dynamics simulations. J. Mol. Graph. Model. 2012, 32, 39–48. [Google Scholar] [CrossRef]
- Feliz, L.R.; Tsimberidou, A.M. Anti-vascular endothelial growth factor therapy in the era of personalized medicine. Cancer Chemother. Pharmacol. 2013, 72, 1–12. [Google Scholar] [CrossRef]
- Zhao, Y.; Adjei, A.A. Targeting Angiogenesis in Cancer Therapy: Moving Beyond Vascular Endothelial Growth Factor. Oncologist 2015, 20, 660–673. [Google Scholar] [CrossRef]
- Bueno, M.J.; Mouron, S.; Quintela-Fandino, M. Personalising and targeting antiangiogenic resistance: A complex and multifactorial approach. Br. J. Cancer 2017, 116, 1119–1125. [Google Scholar] [CrossRef]
- Simon, T.; Gagliano, T.; Giamas, G. Direct Effects of Anti-Angiogenic Therapies on Tumor Cells: VEGF Signaling. Trends Mol. Med. 2017, 23, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Zirlik, K.; Duyster, J. Anti-Angiogenics: Current Situation and Future Perspectives. Oncol. Res. Treat. 2018, 41, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Quintanilla, L.; Luaces-Rodríguez, A.; Gil-Martínez, M.; Mondelo-García, C.; Maroñas, O.; Mangas-Sanjuan, V.; González-Barcia, M.; Zarra-Ferro, I.; Aguiar, P.; Otero-Espinar, F.J.; et al. Pharmacokinetics of Intravitreal Anti-VEGF Drugs in Age-Related Macular Degeneration. Pharmaceutics 2019, 11, 365. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, N.; Hillan, K.J.; Gerber, H.P.; Novotny, W. Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat. Rev. Drug Discov. 2004, 3, 391–400. [Google Scholar] [CrossRef]
- Haubner, R.; Beer, A.J.; Wang, H.; Chen, X. Positron emission tomography tracers for imaging angiogenesis. Eur. J. Nucl. Med. Mol. Imaging 2010, 37 (Suppl. 1), S86–S103. [Google Scholar] [CrossRef]
- Kniess, T. Radiolabeled small molecule inhibitors of VEGFR—Recent advances. Curr. Pharm. Des. 2012, 18, 2867–2874. [Google Scholar] [CrossRef]
- Bernard-Gauthier, V.; Bailey, J.J.; Berke, S.; Schirrmacher, R. Recent Advances in the Development and Application of Radiolabeled Kinase Inhibitors for PET Imaging. Molecules 2015, 20, 22000–22027. [Google Scholar] [CrossRef]
- Yoshimoto, M.; Kurihara, H.; Fujii, H. Theragnostic Imaging Using Radiolabeled Antibodies and Tyrosine Kinase Inhibitors. Sci. World J. 2015, 842101. [Google Scholar] [CrossRef]
- Schenone, S.; Bondavalli, F.; Botta, M. Antiangiogenic Agents: An update on small molecule VEGFR inhibitors. Curr. Med. Chem. 2007, 14, 2495–2516. [Google Scholar] [CrossRef]
- Casaletto, J.B.; McClatchey, A.I. Spatial regulation of receptor tyrosine kinases in development and cancer. Nat. Rev. Cancer 2012, 12, 387–400. [Google Scholar] [CrossRef]
- Binétruy-Tournaire, R.; Demangel, C.; Malavaud, B.; Vassy, R.; Rouyre, S.; Kraemer, M.; Plouët, J.; Derbin, C.; Perret, G.; Mazie, J.C. Identification of a peptide blocking vascular endothelial growth factor (VEGF)-mediated angiogenesis. EMBO J. 2000, 19, 1525–1533. [Google Scholar] [CrossRef]
- Starzec, A.; Vassy, R.; Martin, A.; Lecouvey, M.; Di Benedetto, M.; Crépin, M.; Perret, G.Y. Antiangiogenic and antitumor activities of peptide inhibiting the vascular endothelial growth factor binding to neuropilin-1. Life Sci. 2006, 79, 2370–2381. [Google Scholar] [CrossRef]
- Teesalu, T.; Sugahara, K.N.; Kotamraju, V.R.; Ruoslahti, E. C-end rule peptides mediate neuropilin-1-dependent cell, vascular, and tissue penetration. Proc. Natl. Acad. Sci. USA 2009, 106, 16157–16162. [Google Scholar] [CrossRef]
- Sugahara, K.N.; Teesalu, T.; Karmali, P.P.; Kotamraju, V.R.; Agemy, L.; Girard, O.M.; Hanahan, D.; Mattrey, R.F.; Ruoslahti, E. Tissue-penetrating delivery of compounds and nanoparticles into tumors. Cancer Cell 2009, 16, 510–520. [Google Scholar] [CrossRef]
- Simón-Gracia, L.; Hunt, H.; Teesalu, T. Peritoneal carcinomatosis targeting with tumor homing peptides. Molecules 2018, 23, 1190. [Google Scholar] [CrossRef]
- Jarvis, A.; Allerston, C.K.; Jia, H.; Herzog, B.; Garza-Garcia, A.; Winfield, N.; Ellard, K.; Aqil, R.; Lynch, R.; Chapman, C.; et al. Small molecule inhibitors of the neuropilin-1 vascular endothelial growth factor A (VEGF-A) interaction. J. Med. Chem. 2010, 53, 2215–2226. [Google Scholar] [CrossRef]
- Jia, H.; Aqil, R.; Cheng, L.; Chapman, C.; Shaikh, S.; Jarvis, A.; Chan, A.W.; Hartzoulakis, B.; Evans, I.M.; Frolov, A.; et al. N-terminal modification of VEGF-A C terminus-derived peptides delineates structural features involved in neuropilin-1 binding and functional activity. ChemBioChem 2014, 15, 1161–1170. [Google Scholar] [CrossRef]
- Tymecka, D.; Puszko, A.K.; Lipiński, P.F.; Fedorczyk, B.; Wilenska, B.; Sura, K.; Perret, G.Y.; Misicka, A. Branched pentapeptides as potent inhibitors of the vascular endothelial growth factor 165 binding to Neuropilin-1: Design, synthesis and biological activity. Eur. J. Med. Chem. 2018, 158, 453–462. [Google Scholar] [CrossRef]
- Puszko, A.K.; Sosnowski, P.; Tymecka, D.; Raynaud, F.; Hermine, O.; Lepelletier, Y.; Misicka, A. Neuropilin-1 peptide-like ligands with proline mimetics, tested using the improved chemiluminescence affinity detection method. MedChemComm 2019, 10, 332–340. [Google Scholar] [CrossRef]
- Puszko, A.K.; Sosnowski, P.; Raynaud, F.; Hermine, O.; Hopfgartner, G.; Lepelletier, Y.; Misicka, A. Does Cysteine Rule (CysR) Complete the CendR Principle? Increase in Affinity of Peptide Ligands for NRP-1 through the Presence of N-Terminal Cysteine. Biomolecules 2020, 10, 448. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.Q.; Lepelletier, Y.; Montès, M.; Borriello, L.; Jarray, R.; Grépin, R.; Leforban, B.; Loukaci, A.; Benhida, R.; Hermine, O.; et al. NRPa-308, a new neuropilin-1 antagonist, exerts in vitro anti-angiogenic and anti-proliferative effects and in vivo anti-cancer effects in a mouse xenograft model. Cancer Lett. 2018, 414, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Longo, R.; Gasparini, G. Challenges for patient selection with VEGF inhibitors. Cancer Chemother. Pharmacol. 2007, 60, 151–170. [Google Scholar] [CrossRef]
- Samén, E.; Thorell, J.O.; Lu, L.; Tegnebratt, T.; Holmgren, L.; Stone-Elander, S. Synthesis and preclinical evaluation of [11C]PAQ as a PET imaging tracer for VEGFR-2. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, 1283–1295. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Wang, R.F. A concise review of current radiopharmaceuticals in tumor angiogenesis imaging. Curr. Pharm. Des. 2012, 18, 1032–1040. [Google Scholar] [CrossRef] [PubMed]
- Tolmachew, V.; Stone-Elander, S.; Orlova, A. Radiolabelled receptor-tyrosine-kinase targeting drugs for patient stratification and monitoring of therapy response: Prospects and pitfalls. Lancet Oncol. 2010, 11, 992–1000. [Google Scholar] [CrossRef]
- Taurone, S.; Galli, F.; Signore, A.; Agostinelli, E.; Dierckx, R.A.J.O.; Minni, A.; Pucci, M.; Artico, M. VEGF in nuclear medicine: Clinical application in cancer and future perspectives (Review). Int. J. Oncol. 2016, 49, 437–447. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bahce, I.; Yaqub, M.; Smit, E.F.; Lammertsma, A.A.; van Dongen, G.A.M.S.; Hendrikse, N.H. Personalizing NSCLC therapy by characterizing tumors using TKI-PETand immuno-PET. Lung Cancer 2017, 107, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Senger, D.R.; Galli, S.J.; Dvorak, A.M.; Perruzzi, C.A.; Harvey, V.S.; Dvorak, H.F. Tumor cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Science 1983, 219, 983–985. [Google Scholar] [CrossRef]
- Plouet, J.; Schilling, J.; Gospodarowicz, D. Isolation and characterization of a newly identified endothelial cell mitogen produced by AtT-20 cells. EMBO J. 1989, 8, 3801–3806. [Google Scholar] [CrossRef]
- Ferrara, N.; Hanzel, W.J. Pituitary folicular cells secrete a novel heparinbinding growth factor specific for vascular endothelial cells. BioChem. Biophys. Res. Commun. 1989, 161, 851–858. [Google Scholar] [CrossRef]
- Holmes, D.I.R.; Zachary, I. The vascular endothelial growth factor (VEGF) family: Angiogenic factors in health and disease. Genome Biol. 2005, 6, 209. [Google Scholar] [CrossRef][Green Version]
- Yamazaki, Y.; Matsunaga, Y.; Tokunaga, Y.; Obayashi, S.; Saito, M.; Morita, T. Snake Venom Vascular Endothelial Growth Factors (VEGF-Fs) Exclusively Vary Their Structures and Functions among Species. J. Biol. Chem. 2009, 284, 9885–9891. [Google Scholar] [CrossRef] [PubMed]
- Pötgens, A.J.; Lubsen, N.H.; van Altena, M.C.; Vermeulen, R.; Bakker, A.; Schoenmakers, J.G.; Ruiter, D.J.; de Waal, R.M. Covalent Dimerization of Vascular Permeability Factor/Vascular Endothelial Growth Factor Is Essential for Its Biological Activity. J. Biol. Chem. 1994, 269, 32879–32885. [Google Scholar] [CrossRef]
- Nowak, D.G.; Woolard, J.; Amin, E.M.; Konopatskaya, O.; Saleem, M.A.; Churchill, A.J.; Ladomery, M.R.; Harper, S.J.; Bates, D.O. Expression of pro- and anti-angiogenic isoforms of VEGF is differentially regulated by splicing and growth factors. J. Cell Sci. 2008, 121, 3487–3495. [Google Scholar] [CrossRef]
- Peach, C.J.; Mignone, V.W.; Arruda, M.A.; Alcobia, D.C.; Hill, S.J.; Kilpatrick, L.E.; Woolard, J. Molecular Pharmacology of VEGF-A Isoforms: Binding and Signalling at VEGFR2. Int. J. Mol. Sci. 2018, 19, 1264. [Google Scholar] [CrossRef]
- Houck, K.A.; Leung, D.W.; Rowland, A.M.; Winer, J.; Ferrara, N. Dual regulation of vascular endothelial growth factor bioavailability by genetic and proteolytic mechanisms. J. Biol. Chem. 1992, 267, 26031–26037. [Google Scholar] [CrossRef]
- Ferrara, N.; Davis-Smith, T. The Biology of Vascular Endothelial Growth Factor. Endocr. Rev. 1997, 18, 4–25. [Google Scholar] [CrossRef] [PubMed]
- Gerber, H.P.; McMurtrey, S.; Kowalski, J.; Yan, M.; Keyt, B.A.; Dixit, V.; Ferrara, N. Vascular Endothelial Growth Factor Regulates Endothelial Cell Survival through the Phosphatidylinositol 3′-Kinase/Akt Signal Transduction Pathway. Requirement for Flk-1/KDR activation. J. Biol. Chem. 1998, 273, 30336–30343. [Google Scholar] [CrossRef]
- Dvorak, H.F.; Brown, L.F.; Detmar, M.; Dvorak, A.M. Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am. J. Pathol. 1995, 146, 1029–1039. [Google Scholar]
- Cluass, M.; Gerlach, M.; Gerlach, H.; Brett, J.; Wang, F.; Familletti, P.C.; Pan, Y.C.; Olander, J.V.; Connolly, D.T.; Stern, D. Vascular Permeability Factor: A Tumor-derived Polypeptide that Induces Endothelial Cell and Monocyte Procoagulant Activity, and Promotes Monocyte Migration. J. Exp. Med. 1990, 172, 1535–1545. [Google Scholar] [CrossRef]
- Broxmeyer, H.E.; Cooper, S.; Li, Z.H.; Lu, L.; Song, H.Y.; Kwon, B.S.; Warren, R.E.; Donner, D.B. Myeloid progenitor cell regulatory effects of vascular endothelial cell growth factor. Int. J. Hematol. 1995, 62, 203–215. [Google Scholar] [CrossRef]
- Hattori, K.; Dias, S.; Heissig, B.; Hackett, N.R.; Lyden, D.; Tateno, M.; Hicklin, D.J.; Zhu, Z.; Witte, L.; Crystal, R.G.; et al. Vascular Endothelial Growth Factor and Angiopoietin-1 Stimulate Postnatal Hematopoiesis by Recruitment of Vasculogenic and Hematopoietic Stem Cells. J. Exp. Med. 2001, 193, 1005–1014. [Google Scholar] [CrossRef] [PubMed]
- Storkebaum, E.; Carmeliet, P. VEGF: A critical player in neurodegeneration. J. Clin. Investig. 2004, 113, 14–18. [Google Scholar] [CrossRef]
- Berse, B.; Brown, L.F.; Van de Water, L.; Dvorak, H.F.; Senger, D.R. Vascular Permeability Factor (Vascular Endothelial Growth Factor) Gene is Expressed Differentially in Normal Tissues, Macrophages, and Tumors. Mol. Biol. Cell 1992, 3, 211–220. [Google Scholar] [CrossRef]
- Dvorak, H.F.; Sioussat, T.M.; Brown, L.F.; Berse, B.; Nagy, J.A.; Sotrel, A.; Manseau, E.J.; Van de Water, L.; Senger, D.R. Distribution of Vascular Permeability Factor (Vascular Endothelial Growth Factor) in Tumors: Concentration in Tumor Blood Vessels. J. Exp. Med. 1991, 174, 1275–1278. [Google Scholar] [CrossRef] [PubMed]
- Semenza, G. Angiogenesis in ischemic and neoplastic disorders. Annu. Rev. Med. 2003, 54, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Forsythe, J.A.; Jiang, B.H.; Iyer, N.V.; Agani, F.; Leung, S.W.; Koos, R.D.; Semenza, G.L. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol. Cell. Biol. 1996, 16, 4604–4613. [Google Scholar] [CrossRef] [PubMed]
- Warren, R.S.; Yuan, H.; Matli, M.R.; Ferrara, N.; Donner, D.B. Induction of vascular endothelial growth factor by insulin-like growth factor 1 in colorectal carcinoma. J. Biol. Chem. 1996, 271, 29483–29488. [Google Scholar] [CrossRef]
- Ben-Av, P.; Crofford, L.J.; Wilder, R.L.; Hla, T. Induction of vascular endothelial growth factor expression in synovial fibroblasts by prostaglandin E and interleukin-l: A potential mechanism for inflammatory angiogenesis. FEBS Lett. 1995, 372, 83–87. [Google Scholar] [CrossRef]
- Enholm, B.; Paavonen, K.; Ristimäki, A.; Kumar, V.; Gunji, Y.; Klefstrom, J.; Kivinen, L.; Laiho, M.; Olofsson, B.; Joukov, V.; et al. Comparison of VEGF, VEGF-B, VEGF-C and Ang-1 mRNA regulation by serum, growth factors, oncoproteins and hypoxia. Oncogene 1997, 14, 2475–2483. [Google Scholar] [CrossRef]
- Siemesiter, G.; Weindel, K.; Mohrs, K.; Barleon, B.; Martiny-Baron, G.; Marmé, D. Reversion of deregulated expression of vascular endothelial growth factor in human renal carcinoma cells by von Hippel-Lindau tumor suppressor protein. Cancer Res. 1996, 56, 2299–2301. [Google Scholar]
- Eliceiri, B.P.; Paul, R.; Schwartzberg, P.L.; Hood, J.D.; Leng, J.; Cheresh, D.A. Selective requirement for Src kinases during VEGF-induced angiogenesis and vascular permeability. Mol. Cell 1999, 4, 915–924. [Google Scholar] [CrossRef]
- Kimura, H.; Esumi, H. Reciprocal regulation between nitric oxide and vascular endothelial growth factor in angiogenesis. Acta Biochim. Pol. 2003, 50, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Ushio-Fukai, M.; Nakamura, Y. Reactive oxygen species and angiogenesis: NADPH oxidase as target for cancer therapy. Cancer Lett. 2008, 266, 37–52. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Tjwa, M.; Van Hove, I.; Enholm, B.; Neven, E.; Paavonen, K.; Jeltsch, M.; Juan, T.D.; Sievers, R.E.; Chorianopoulos, E.; et al. Reevaluation of the Role of VEGF-B Suggests a Restricted Role in the Revascularization of the Ischemic Myocardium. Arter. Thromb. Vasc. Biol. 2008, 28, 1614–1620. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, C.E.; Falkevall, A.; Wang, X.; Larsson, E.; Huusko, J.; Nilsson, I.; van Meeteren, L.A.; Samen, E.; Lu, L.; Vanwildemeersch, M.; et al. Vascular endothelial growth factor B controls endothelial fatty acid uptake. Nature 2010, 464, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, C.E.; Mehlem, A.; Falkevall, A.; Muhl, L.; Fam, B.C.; Orstäter, H.; Scotney, P.; Nyqvist, D.; Samen, E.; Lu, L.; et al. Targeting VEGF-B as a novel treatment for insulin resistance and type 2 diabetes. Nature 2012, 490, 426–430. [Google Scholar] [CrossRef]
- Arjunan, P.; Lin, X.; Tang, Z.; Du, Y.; Kumar, A.; Liu, L.; Yin, X.; Huang, L.; Chen, W.; Chen, Q.; et al. VEGF-B is a potent antioxidant. Proc. Natl. Acad. Sci. USA 2018, 115, 10351–10356. [Google Scholar] [CrossRef]
- Dhondt, J.; Peeraer, E.; Verheyen, A.; Nuydens, R.; Buysschaert, I.; Poesen, K.; Van Geyte, K.; Beerens, M.; Shibuya, M.; Haigh, J.J.; et al. Neuronal FLT1 receptor and its selective ligand VEGF-B protect against retrograde degeneration of sensory neurons. FASEB J. 2011, 25, 1461–1473. [Google Scholar] [CrossRef]
- Yue, X.; Hariri, D.J.; Caballero, B.; Zhang, S.; Bartlett, M.J.; Kaut, O.; Mount, D.W.; Wullner, U.; Sherman, S.J.; Falk, T. Comparative study of the neurotrophic effects elicited by VEGF-B and GDNF in preclinical in vivo models of Parkinson’s disease. Neuroscience 2014, 258, 385–400. [Google Scholar] [CrossRef] [PubMed]
- De Falco, S. The discovery of placenta growth factor and its biological activity. Exp. Mol. Med. 2012, 44, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Carmeliet, P.; Moons, L.; Luttun, A.; Vincenti, V.; Compernolle, V.; De Mol, M.; Wu, Y.; Bono, F.; Devy, L.; Beck, H.; et al. Synergism between vascular endothelial growth factor and placental growth factor contributes to angiogenesis and plasma extravasation in pathological conditions. Nat. Med. 2001, 7, 575–583. [Google Scholar] [CrossRef]
- Oura, H.; Bertoncini, J.; Velasco, P.; Brown, L.F.; Carmeliet, P.; Detmar, M. A critical role of placental growth factor in the induction of inflammation and edema formation. Blood 2003, 101, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Rolny, C.; Mazzone, M.; Tugues, S.; Laoui, D.; Johansson, I.; Coulon, C.; Squadrito, M.L.; Segura, I.; Li, X.; Knevels, E.; et al. HRG inhibits tumor growth and metastasis by inducing macrophage polarization and vessel normalization through down-regulation of PlGF. Cancer Cell. 2011, 19, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Jussila, L.; Alitalo, K. Vascular growth factors and lymphangiogenesis. Physiol. Rev. 2002, 82, 673–700. [Google Scholar] [CrossRef] [PubMed]
- Tsurusaki, T.; Kanda, S.; Sakai, H.; Kanetake, H.; Saito, Y.; Alitalo, K.; Koji, T. Vascular endothelial growth factor-C expression in human prostatic carcinoma and its relationship to lymph node metastasis. Br. J. Cancer 1999, 80, 309–313. [Google Scholar] [CrossRef]
- Mandriota, S.J.; Jussila, L.; Jeltsch, M.; Compagni, A.; Baetens, D.; Prevo, R.; Banerji, S.; Huarte, J.; Montesano, R.; Jackson, D.G.; et al. Vascular endothelial growth factor-C-mediated lymphangiogenesis promotes tumour metastasis. EMBO J. 2001, 20, 672–682. [Google Scholar] [CrossRef]
- Stacker, S.A.; Caesar, C.; Baldwin, M.E.; Thornton, G.E.; Williams, R.A.; Prevo, R.; Jackson, D.G.; Nishikawa, S.; Kubo, H.; Achen, M.G. VEGF-D promotes the metastatic spread of tumor cells via the lymphatics. Nat. Med. 2001, 7, 186–191. [Google Scholar] [CrossRef]
- Shibuya, M.; Claesson-Welsh, L. Signal transduction by VEGF receptors in regulation of angiogenesis and lymphangiogenesis. Exp. Cell Res. 2006, 312, 549–560. [Google Scholar] [CrossRef]
- Soker, S.; Fidder, H.; Neufeld, G.; Klagsbrun, M. Characterization of novel vascular endothelial growth factor (VEGF) receptors on tumor cells that bind VEGF165 via its exon 7-encoded domain. J. Biol. Chem. 1996, 271, 5761–5767. [Google Scholar] [CrossRef]
- Soker, S.; Takashima, S.; Miao, H.Q.; Neufeld, G.; Klagsbrun, M. Neuropilin-1 is expressed by endothelial and tumor cells as an isoform-specific receptor for vascular endothelial growth factor. Cell 1998, 92, 735–745. [Google Scholar] [CrossRef]
- Pan, Q.; Chathery, Y.; Wu, Y.; Rathore, N.; Tong, R.K.; Peale, F.; Bagri, A.; Tessier-Lavigne, M.; Koch, A.W.; Watts, R.J. Neuropilin-1 binds to VEGF121 and regulates endothelial cell migration and sprouting. J. Biol. Chem. 2007, 282, 24049–24056. [Google Scholar] [CrossRef]
- Jakeman, L.B.; Armanini, M.; Philips, H.S.; Ferrara, N. Developmental expression of binding sites and mRNA for vascular endothelial growth factor suggests a role for this protein in vasculogenesis and angiogenesis. Endocrinology 1993, 133, 848–859. [Google Scholar] [CrossRef]
- Shen, H.; Clauss, M.; Ryan, J.; Schmidt, A.M.; Tijburg, P.; Borden, L.; Connolly, D.; Stern, D.; Kao, J. Characterization of vascular permeability factor/vascular endothelial growth factor receptors on mononuclear phagocytes. Blood 1993, 81, 2767–2773. [Google Scholar] [CrossRef]
- Walter, J.W.; North, P.E.; Waner, M.; Mizeracki, A.; Blei, F.; Walker, J.W.; Reinisch, J.F.; Marchuk, D.A. Somatic mutation of vascular endothelial growth factor receptors in juvenile hemangioma. Genes Chromosomes Cancer 2002, 33, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Colbert, L.S.; Fuller, M.; Zhang, Y.; Gonzalez-Perez, R.R. Vascular endothelial growth factor receptor-2 in breast cancer. Biochim. Biophys. Acta 2010, 1806, 108–121. [Google Scholar] [CrossRef] [PubMed]
- Pajusola, K.; Aprelikova, O.; Korhonen, J.; Kaipainen, A.; Pertovaara, L.; Alitalo, R.; Alitalo, K. FLT4 receptor tyrosine kinase contains seven immunoglobulin-like loops and is expressed in multiple human tissues and cell lines. Cancer Res. 1992, 52, 5738–5743. [Google Scholar]
- Yuan, L.; Moyon, D.; Pardanaud, L.; Breant, C.; Karkkainen, M.J.; Alitalo, K.; Eichmann, A. Abnormal lymphatic vessel development in neuropilin 2 mutant mice. Development 2002, 129, 4797–4806. [Google Scholar] [PubMed]
- Mac Gabhann, F.; Popel, A.S. Dimerization of VEGF receptors and implications for signal transduction: A computational study. Biophys. Chem. 2007, 128, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Waltenberger, J.; Claesson-Welsh, L.; Siegbahn, A.; Shibuya, M.; Heldin, C.H. Different signal transduction properties of KDR and Flt1, two receptors for vascular endothelial growth factor. J. Biol. Chem. 1994, 269, 26988–26995. [Google Scholar] [CrossRef]
- Sondell, M.; Lundborg, G.; Kanje, M. Vascular endothelial growth factor has neurotrophic activity and stimulates axonal outgrowth, enhancing cell survival and Schwann cell proliferation in the peripheral nervous system. J. Neuro Sci. 1999, 19, 5731–5740. [Google Scholar] [CrossRef]
- De Vries, C.; Escobedo, J.A.; Ueno, H.; Houck, K.; Ferrara, N.; Williams, L.T. The fms-like tyrosine kinase, a receptor for vascular endothelial growth factor. Science 1992, 255, 989–991. [Google Scholar] [CrossRef]
- Olsson, A.K.; Dimberg, A.; Kreuger, J.; Claesson-Welsh, L. VEGF receptor signaling—In control of vascular function. Nat. Rev. Mol. Cell. Biol. 2006, 7, 359–371. [Google Scholar] [CrossRef] [PubMed]
- Autiero, M.; Waltenberger, J.; Communi, D.; Kranz, A.; Moons, L.; Lambrechts, D.; Kroll, J.; Plaisance, S.; De Mol, M.; Bono, F.; et al. Role of PlGF in the intra- and intermolecular cross talk between the VEGF receptors Flt1 and Flk1. Nat. Med. 2003, 9, 936–943. [Google Scholar] [CrossRef]
- Matsumoto, K.; Yoshitomi, H.; Rossant, J.; Zaret, K.S. Liver organogenesis promoted by endothelial cells prior to vascular function. Science 2001, 294, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Byzova, T.V.; Goldman, C.K.; Pampori, N.; Thomas, K.A.; Bett, A.; Shattil, S.J.; Plow, E.F. A mechanism for modulation of cellular responses to VEGF: Activation of the integrins. Mol. Cell 2000, 6, 851–860. [Google Scholar] [CrossRef]
- Le Boeuf, F.; Houle, F.; Huot, J. Regulation of Vascular Endothelial Growth Factor Receptor 2-mediated Phosphorylation of Focal Adhesion Kinase by Heat Shock Protein 90 and Src Kinase Activities. J. Biol. Chem. 2004, 279, 39175–39185. [Google Scholar] [CrossRef]
- Kendall, R.L.; Thomas, K.A. Inhibition of vascular endothelial cell growth factor activity by an endogenously encoded soluble receptor. Proc. Natl. Acad. Sci. USA 1993, 90, 10705–10709. [Google Scholar] [CrossRef]
- Murga, M.; Fernandez-Capetillo, O.; Tosato, G. Neuropilin-1 regulates attachment in human endothelial cells independently of vascular endothelial growth factor receptor-2. Blood 2005, 105, 1992–1999. [Google Scholar] [CrossRef] [PubMed]
- Horing, C.; Weich, H.A. Soluble VEGF receptors. Angiogenesis 1999, 3, 33–39. [Google Scholar] [CrossRef]
- Ebos, J.M.L.; Bocci, G.; Man, S.; Thrope, P.E.; Hicklin, D.J.; Zhou, D.; Jia, X.; Kerbel, R.S. A naturally occurring soluble form of vascular endothelial growth factor receptor 2 detected in mouse and human plasma. Mol. Cancer Res. 2004, 2, 315–326. [Google Scholar]
- Cai, J.; Jiang, W.G.; Grant, M.B.; Boulton, M. Pigment epithelium-derived factor inhibits angiogenesis via regulated intracellular proteolysis of vascular endothelial growth factor receptor 1. J. Biol. Chem. 2006, 281, 3604–3613. [Google Scholar] [CrossRef]
- Albuquerque, R.J.C.; Hayashi, T.; Cho, W.G.; Kleinman, M.E.; Dridi, S.; Takeda, A.; Baffi, J.Z.; Yamada, K.; Kaneko, H.; Green, M.G.; et al. Alternatively spliced vascular endothelial growth factor receptor-2 is an essential endogenous inhibitor of lymphatic vessel growth. Nat. Med. 2009, 15, 1023–1030. [Google Scholar] [CrossRef]
- Barleon, B.; Totzke, F.; Herzog, C.; Blanke, S.; Kremmer, E.; Siemeister, G.; Marmé, D.; Martiny-Baron, G. Mapping of sites for ligand binding and receptor dimerization at the extracellular domain of the vascular endothelial growth factor receptor FLT-1. J. Biol. Chem. 1997, 272, 10382–10388. [Google Scholar] [CrossRef]
- Lorquet, S.; Berndt, S.; Blacher, S.; Gengoux, E.; Peulen, O.; Maquoi, E.; Noël, A.; Foidart, J.M.; Munaut, C.; Péqueux, C. Soluble forms of VEGF receptor-1 and -2 promote vascular maturation via mural cell recruitment. FASEB J. 2010, 24, 3782–3795. [Google Scholar] [CrossRef]
- Goldman, C.K.; Kendall, R.L.; Cabrera, G.; Soroceanu, L.; Heike, Y.; Gillespie, G.Y.; Siegal, G.P.; Mao, X.; Bett, A.J.; Huckle, W.R.; et al. Paracrine expression of a native soluble vascular endothelial growth factor receptor inhibits tumor growth, metastasis, and mortality rate. Proc. Natl. Acad. Sci. USA 1998, 95, 8795–8800. [Google Scholar] [CrossRef]
- Harris, A.L.; Reusch, P.; Barleon, B.; Hang, C.; Dobbs, N.; Marme, D. Soluble Tie2 and Flt1 extracellular domains in serum of patients with renal cancer and response to antiangiogenic therapy. Clin. Cancer Res. 2001, 7, 1992–1997. [Google Scholar]
- Toi, M.; Bando, H.; Ogawa, T.; Muta, M.; Hornig, C.; Weich, H.A. Significance of vascular endothelial growth factor (VEGF)/soluble VEGF receptor-1 relationship in breast cancer. Int. J. Cancer 2002, 98, 14–18. [Google Scholar] [CrossRef]
- Bando, H.; Weich, H.A.; Brokelmann, M.; Horiguchi, S.; Funata, N.; Ogawa, T.; Toi, M. Association between intratumoral free and total VEGF, soluble VEGFR-1, VEGFR-2 and prognosis in breast cancer. Br. J. Cancer 2005, 92, 553–561. [Google Scholar] [CrossRef]
- Aref, S.; El Sherbiny, M.; Goda, T.; Fouda, M.; Al Askalany, H.; Abdalla, D. Soluble VEGF/sFLt1 ratio is an independent predictor of AML patient outcome. Hematology 2005, 10, 131–134. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Bando, H.; Mori, T.; Takahashi, K.; Matsumoto, H.; Yasutome, M.; Weich, H.; Toi, M. Overexpression of soluble vascular endothalial growth factor receptor 1 in colorectal cancer: Association with progression and prognosis. Cancer Sci. 2007, 98, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Kopczyńska, E.; Dancewicz, M.; Kowalewski, J.; Makarewicz, R.; Kardymowicz, H.; Kaczmarczyk, A.; Tyrakowski, T. Time-dependent changes of plasma concentrations of angiopoietins, vascular endothelial growth factor, and soluble forms of their receptors in nonsmall cell lung cancer patients following surgical resection. ISRN Oncol. 2012, 2012, 638352. [Google Scholar] [CrossRef][Green Version]
- Kou, B.; Li, Y.; Zhang, L.; Zhu, G.; Wang, X.; Li, Y.; Xia, J.; Shi, Y. In vivo inhibition of tumor angiogenesis by a soluble VEGFR-2 fragment. Exp. Mol. Pathol. 2004, 76, 129–137. [Google Scholar] [CrossRef]
- Faderl, S.; Do, K.A.; Johnson, M.M.; Keating, M.; O’Brien, S.; Jilani, I.; Ferrajoli, A.; Ravandi-Kashani, F.; Aguilar, C.; Dey, A.; et al. Angiogenic factors may have a different prognostic role in adult acute lymphoblastic leukemia. Blood 2005, 106, 4303–4307. [Google Scholar] [CrossRef]
- Jayasinghe, C.; Simiantonaki, N.; Michel-Schmidt, R.; Kirkpatrick, C.J. Comparative study of human colonic tumor-derives endothelial cells (HCTEC) and normal colonic microvascular endothelial cells (HCMEC): Hypoxia-induces sVEGFR-1 and sVEGFR-2 levels. Oncol. Rep. 2009, 21, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, S.; Obata, Y.; Yagyu, K.; Lin, Y.; Nakajima, T.; Kobayashi, O.; Kikuichi, M.; Ushijima, R.; Kurosawa, M.; Ueda, J. Reduced serum vascular endothelial growth factor receptor-2 (sVEGFR-2) and sVEGFR-1 levels in gastric cancer patients. Cancer Sci. 2011, 102, 866–869. [Google Scholar] [CrossRef] [PubMed]
- Folkman, J. What is the evidence that tumors are angiogenesis dependent? J. Natl. Cancer Inst. 1990, 82, 4–6. [Google Scholar] [CrossRef]
- Skobe, M.; Rockwell, P.; Goldstein, N.; Vosseler, S.; Fusenig, N.E. Halting angiogenesis suppresses carcinoma cell invasion. Nat. Med. 1997, 3, 1222–1227. [Google Scholar] [CrossRef]
- Yang, J.C.; Haworth, L.; Sherry, R.M.; Hwu, P.; Schwartzentruber, D.J.; Topalian, S.L.; Steinberg, S.M.; Chen, H.X.; Rosenberg, S.A. A randomized trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cancer. N. Engl. J. Med. 2003, 349, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Stephen, R.M.; Gilles, R.J. Promise and progress for functional and molecular imaging of response to targeted therapies. Pharm. Res. 2007, 24, 1172–1185. [Google Scholar] [CrossRef]
- Stacy, M.R.; Maxfield, M.W.; Sinusas, A.J. Targeted Molecular Imaging of Angiogenesis in PET and SPECT: A review. Yale J. Biol. Med. 2012, 85, 75–86. [Google Scholar] [PubMed]
- Wang, H.; Cai, W.; Chen, K.; Li, Z.B.; Kashefi, A.; He, L.; Chen, X. A new PET tracer specific for vascular endothelial growth factor receptor 2. Eur. J. Nucl. Med. Mol. Imaging 2007, 34, 2001–2010. [Google Scholar] [CrossRef]
- Cai, W.; Chen, K.; Mohamedali, K.A.; Cao, Q.; Gambhir, S.S.; Rosenblum, M.G.; Chen, X. PET of vascular endothelial growth factor receptor expression. J. Nucl. Med. 2006, 47, 2048–2056. [Google Scholar]
- Backer, M.V.; Levashova, Z.; Patel, V.; Jehning, B.T.; Claffey, K.; Blankenberg, F.G.; Backer, J.M. Molecular imaging of VEGF receptors in angiogenic vasculature with single-chain VEGF-based probes. Nat. Med. 2007, 13, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Goel, S.; Duda, D.G.; Xu, L.; Munn, L.L.; Boucher, Y.; Fukumura, D.; Jain, R.K. Normalization of the vasculature for treatment of cancer and other diseases. Physiol. Rev. 2011, 91, 1071–7121. [Google Scholar] [CrossRef] [PubMed]
- Blankenberg, F.G.; Levashova, Z.; Goris, M.G.; Hamby, C.V.; Backer, M.V.; Backer, J.M. Targeted systemic radiotherapy with scVEGF/177Lu leads to sustained disruption of the tumor vasculature and intratumoral apoptosis. J. Nucl. Med. 2011, 52, 1630–1637. [Google Scholar] [CrossRef]
- Rusckowski, M.; Wang, Y.; Blankenberg, F.G.; Levashova, Z.; Backer, M.V.; Backer, J.M. Targeted scVEGF/177 Lu radiopharmaceutical inhibits growth of metastases and can be effectively combined with chemotherapy. EJNMMI Res. 2016, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Feng, S.; Liu, J.; Li, Q.; Zheng, L.; Xie, L.; Li, H.; Huang, D. Novel small peptides derived from VEGF 125-136: Potential drugs for radioactive diagnosis and therapy in A549 tumor-bearing nude mice. Sci. Rep. 2017, 7, 1–13. [Google Scholar] [CrossRef]
- Levashova, Z.; Backer, M.; Hamby, C.V.; Pizzonia, J.; Backer, J.M.; Blankenberg, F.G. Molecular imaging of changes in the prevalence of vascular endothelial growth factor receptor in sunitinib-treated murine mammary tumors. J. Nucl. Med. 2010, 51, 959–966. [Google Scholar] [CrossRef]
- Wang, H.; Gao, H.; Guo, N.; Niu, G.; Ma, Y.; Kiesewetter, D.O.; Chen, X. Site-specific labeling of scVEGF with fluorine-18 for positron emission tomography imaging. Theranostics 2012, 2, 607. [Google Scholar] [CrossRef]
- Yoshimoto, M.; Kinuya, S.; Kawashima, A.; Nishii, R.; Yokoyama, K.; Kawai, K. Radioiodinated VEGF to image tumor angiogenesis in a LS180 tumor xenograft model. Nucl. Med. Biol. 2006, 33, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Tekabe, Y.; Kollaros, M.; Zerihoun, A.; Zhang, G.; Backer, M.V.; Backer, J.M.; Johnson, L.L. Imaging VEGF receptor expression to identify accelerated atherosclerosis. EJNMMI Res. 2014, 4, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Rainer, E.; Wang, H.; Traub-Weidinger, T.; Widhalm, G.; Fueger, B.; Chang, J.; Zhu, Z.; Marosi, C.; Haug, A.; Hacker, M.; et al. The prognostic value of [123 I]-vascular endothelial growth factor ([123 I]-VEGF) in glioma. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 2396–2403. [Google Scholar] [CrossRef] [PubMed]
- Vaisman, N.; Gospodarowicz, D.; Neufeld, G. Characterization of the receptors for vascular endothelial growth factor. J. Biol. Chem. 1990, 265, 19461–19466. [Google Scholar] [CrossRef]
- Jakeman, L.B.; Winer, J.; Bennett, G.L.; Altar, C.A.; Ferrara, N. Binding sites for vascular endothelial growth factor are localized on endothelial cells in adult rat tissues. J. Clin. Investig. 1992, 89, 244–253. [Google Scholar] [CrossRef] [PubMed]
- Cohen, T.; Gitay-Goren, H.; Sharon, R.; Shibuya, M.; Halaban, R.; Levi, B.Z.; Neufeld, G. VEGF121, a vascular endothelial growth factor (VEGF) isoform lacking heparin binding ability, requires cell-surface heparan sulfates for efficient binding to the VEGF receptors of human melanoma cells. J. Biol. Chem. 1995, 270, 11322–11326. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.; Röckl, W.; Hornig, C.; Gröne, E.F.; Theis, H.; Weich, H.A.; Fuchs, E.; Yayon, A.; Gröne, H.J. Receptors of vascular endothelial growth factor/vascular permeability factor (VEGF/VPF) in fetal and adult human kidney: Localization and [125I] VEGF binding sites. JASN 1998, 9, 1032–1044. [Google Scholar]
- Cooper, M.E.; Vranes, D.; Youssef, S.; Stacker, S.A.; Cox, A.J.; Rizkalla, B.; Casley, D.J.; Bach, L.A.; Kelly, D.J.; Gilbert, R.E. Increased renal expression of vascular endothelial growth factor (VEGF) and its receptor VEGFR-2 in experimental diabetes. Diabetes 1999, 48, 2229–2239. [Google Scholar] [CrossRef]
- Backer, M.V.; Backer, J.M. Functionally active VEGF fusion proteins. Protein Expr. Purif. 2001, 23, 1–7. [Google Scholar] [CrossRef]
- Cai, W.; Guzman, R.; Hsu, A.R.; Wang, H.; Chen, K.; Sun, G.; Gera, A.; Choi, R.; Bliss, T.; He, L.; et al. Positron emission tomography imaging of poststroke angiogenesis. Stroke 2009, 40, 270–277. [Google Scholar] [CrossRef]
- Willmann, J.K.; Chen, K.; Wang, H.; Paulmurugan, R.; Rollins, M.; Cai, W.; Wang, D.S.; Chen, I.Y.; Gehysens, O.; Rodriguez-Porcel, M.; et al. Monitoring of the biological response to murine hindlimb ischemia with 64Cu-labeled vascular endothelial growth factor-121 positron emission tomography. Circulation 2008, 117, 915. [Google Scholar] [CrossRef]
- Rodriguez-Porcel, M.; Cai, W.; Gheysens, O.; Willmann, J.K.; Chen, K.; Wang, H.; Chen, I.Y.; He, L.; Wu, J.C.; Li, Z.B.; et al. Imaging of VEGF receptor in a rat myocardial infarction model using PET. J. Nucl. Med. 2008, 49, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Cai, W.; Li, Z.B.; Wang, H.; Chen, X. Quantitative PET imaging of VEGF receptor expression. Mol. Imaging Biol. 2009, 11, 15–22. [Google Scholar] [CrossRef]
- Kang, C.M.; Kim, S.M.; Koo, H.J.; Yim, M.S.; Lee, K.H.; Ryu, E.K.; Choe, Y.S. In vivo characterization of 68 Ga-NOTA-VEGF 121 for the imaging of VEGF receptor expression in U87MG tumor xenograft models. Eur. J Nucl. Med Mol. Imaging 2013, 40, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.M.; Koo, H.J.; Choe, Y.S.; Choi, J.Y.; Lee, K.H.; Kim, B.T. 68Ga-NODAGA-VEGF121 for in vivo imaging of VEGF receptor expression. Nucl. Med. Biol. 2014, 41, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Peck-Radosavljevic, M.; Koller, E.; Koller, F.; Kaserer, K.; Kreil, A.; Kapiotis, S.; Hamwi, A.; Weich, H.A.; Valent, P.; et al. Characterization of 123I-vascular endothelial growth factor–binding sites expressed on human tumour cells: Possible implication for tumour scintigraphy. Int. J. Cancer 2001, 91, 789–796. [Google Scholar] [CrossRef]
- Lu, E.; Wagner, W.R.; Schellenberger, U.; Abraham, J.A.; Klibanov, A.L.; Woulfe, S.R.; Csikari, M.M.; Fisher, D.; Schreiner, G.F.; Brandenburger, G.H.; et al. Targeted in vivo labeling of receptors for vascular endothelial growth factor: Approach to identification of ischemic tissue. Circulation 2003, 108, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Gitay-Goren, H.; Cohen, T.; Tessler, S.; Soker, S.; Gengrinovitch, S.; Rockwell, P.; Klaksburg, M.; Levi, B.Z.; Neufeld, G. Selective binding of VEGF to one of the three vascular endothelial growth factor receptors of vascular endothelial cells. J. Biol. Chem. 1996, 271, 5519–5523. [Google Scholar] [CrossRef] [PubMed]
- Blankenberg, F.G.; Backer, M.V.; Levashova, Z.; Patel, V.; Backer, J.M. In vivo tumor angiogenesis imaging with site-specific labeled 99m Tc-HYNIC-VEGF. Eur. J. Nucl. Med. Mol. Imaging 2006, 33, 841–848. [Google Scholar] [CrossRef] [PubMed]
- Backer, M.V.; Levashova, Z.; Levenson, R.; Blankenberg, F.G.; Backer, J.M. Cysteine-containing fusion tag for site-specific conjugation of therapeutic and imaging agents to targeting proteins. In Peptide-Based Drug Design. Methods In Molecular Biology™; Otvos, L., Ed.; Humana Press: Totowa, NJ, USA, 2008; Volume 494, pp. 275–294. [Google Scholar] [CrossRef]
- Levashova, Z.; Backer, M.; Backer, J.M.; Blankenberg, F.G. Direct site-specific labeling of the Cys-tag moiety in scVEGF with technetium 99m. Bioconjugate Chem. 2008, 19, 1049–1054. [Google Scholar] [CrossRef] [PubMed]
- Levashova, Z.; Backer, M.; Backer, J.M.; Blankenberg, F.G. Imaging vascular endothelial growth factor (VEGF) receptors in turpentine-induced sterile thigh abscesses with radiolabeled single-chain VEGF. J. Nucl. Med. 2009, 50, 2058–2063. [Google Scholar] [CrossRef]
- Blankenberg, F.G.; Levashova, Z.; Sarkar, S.K.; Pizzonia, J.; Backer, M.V.; Backer, J.M. Noninvasive assessment of tumor VEGF receptors in response to treatment with pazopanib: A molecular imaging study. Transl Oncol. 2010, 3, 56–64. [Google Scholar] [CrossRef]
- Eder, M.; Krivoshein, A.V.; Backer, M.; Backer, J.M.; Haberkorn, U.; Eisenhut, M. ScVEGF-PEG-HBED-CC and scVEGF-PEG-NOTA conjugates: Comparison of easy-to-label recombinant proteins for [68Ga] PET imaging of VEGF receptors in angiogenic vasculature. Nucl. Med. Biol. 2010, 37, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Blom, E.; Velikyan, I.; Monazzam, A.; Razifar, P.; Nair, M.; Razifar, P.; Vaderheyden, J.L.; Krivoshein, A.V.; Backer, M.; Backer, J.; et al. Synthesis and characterization of scVEGF-PEG-[68Ga] NOTA and scVEGF-PEG-[68Ga] DOTA PET tracers. J. Labelled Comp. Radio Pharm. 2011, 54, 685–692. [Google Scholar] [CrossRef]
- Meyer, J.P.; Edwards, K.J.; Kozlowski, P.; Backer, M.V.; Backer, J.M.; Lewis, J.S. Selective imaging of VEGFR-1 and VEGFR-2 using 89Zr-labeled single-chain VEGF mutants. J. Nucl. Med. 2016, 57, 1811–1816. [Google Scholar] [CrossRef]
- Tekabe, Y.; Johnson, L.L.; Rodriquez, K.; Li, Q.; Backer, M.; Backer, J.M. Selective imaging of vascular endothelial growth factor receptor-1 and receptor-2 in atherosclerotic lesions in diabetic and non-diabetic ApoE−/− mice. Mol. Imaging Biol. 2018, 20, 85–93. [Google Scholar] [CrossRef]
- Zhang, Y.; Hong, H.; Niu, G.; Valdovinos, H.F.; Orbay, H.; Nayak, T.R.; Chen, X.; Barnhart, T.E.; Cai, W. Positron emission tomography imaging of vascular endothelial growth factor receptor expression with 61Cu-labeled lysine-tagged VEGF121. Mol. Pharm. 2012, 9, 3586–3594. [Google Scholar] [CrossRef][Green Version]
- Blankenberg, F.G.; Mandl, S.; Cao, Y.A.; O’Connell-Rodwell, C.; Contag, C.; Mari, C.; Gaynutdinov, T.I.; Vanderheyden, J.L.; Backer, M.V.; Backer, J.M. Tumor imaging using a standardized radiolabeled adapter protein docked to vascular endothelial growth factor. J. Nucl. Med. 2004, 45, 1373–1380. [Google Scholar] [PubMed]
- Chen, K.; Li, Z.B.; Wang, H.; Cai, W.; Chen, X. Dual-modality optical and positron emission tomography imaging of vascular endothelial growth factor receptor on tumor vasculature using quantum dots. Eur. J. Nucl. Med. Mol. Imaging 2008, 35, 2235–2244. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.M.; Koo, H.J.; Lee, K.C.; Choe, Y.S.; Choi, J.Y.; Lee, K.H.; Kim, B.T. A vascular endothelial growth factor 121 (VEGF121)-based dual PET/optical probe for in vivo imaging of VEGF receptor expression. Biomaterials 2013, 34, 6839–6845. [Google Scholar] [CrossRef]
- Hsu, A.R.; Cai, W.; Veeravagu, A.; Mohamedali, K.A.; Chen, K.; Kim, S.; Vogel, H.; Hou, L.C.; Tse, V.; Rosenblum, M.G.; et al. Multimodality molecular imaging of glioblastoma growth inhibition with vasculature-targeting fusion toxin VEGF121/rGel. J. Nucl. Med. 2007, 48, 445–454. [Google Scholar] [PubMed]
- Veenendaal, L.M.; Jin, H.; Ran, S.; Cheung, L.; Navone, N.; Marks, J.W.; Waltenberger, J.; Thorpe, P.; Rosenblum, M.G. In vitro and in vivo studies of a VEGF121/rGelonin chimeric fusion toxin targeting the neovasculature of solid tumors. Proc. Natl. Acad. Sci. USA 2002, 99, 7866–7871. [Google Scholar] [CrossRef]
- Akiyama, H.; Mohamedali, K.A.; e Silva, R.L.; Kachi, S.; Shen, J.; Hatara, C.; Umeda, N.; Hackett, S.F.; Aslam, S.; Krause, M.; et al. Vascular targeting of ocular neovascularization with a vascular endothelial growth factor121/gelonin chimeric protein. Mol. Pharmacol. 2005, 68, 1543–1550. [Google Scholar] [CrossRef]
- Ran, S.; Mohamedali, K.A.; Luster, T.A.; Thorpe, P.E.; Rosenblum, M.G. The vascular-ablative agent VEGF121/rGel inhibits pulmonary metastases of MDA-MB-231 breast tumors. Neoplasia 2005, 7, 486–496. [Google Scholar] [CrossRef]
- Fine, B.A.; Valente, P.T.; Feinstein, G.I.; Dey, T. VEGF, flt-1, and KDR/flk-1 as prognostic indicators in endometrial carcinoma. Gynecol. Oncol. 2000, 76, 33–39. [Google Scholar] [CrossRef]
- Li, S.; Peck-Radosavljevic, M.; Kienast, O.; Preitfellner, J.; Hamilton, G.; Kurtaran, A.; Pirich, C.; Angelberger, P.; Dudczak, R. Imaging gastrointestinal tumours using vascular endothelial growth factor-165 (VEGF165) receptor scintigraphy. Ann. Oncol. 2003, 14, 1274–1277. [Google Scholar] [CrossRef]
- Li, S.; Kienast, O.; Beheshti, M.; Preitfellner, J.; Traub-Weidinger, T.; Dudczak, R.; Peck-Radosavljevic, M.; Schmid, M.; Hamilton, G.; Schima, W.; et al. Iodine-123-vascular endothelial growth factor-165 (123 I-VEGF 165): Biodistribution, safety and radiation dosimetry in patients with pancreatic cancer. Nuklearmedizin 2003, 42, A180. [Google Scholar]
- Holzer, G.; Hamilton, G.; Angelberger, P.; Lai, D.; Ubl, P.; Dudczak, R.; Dominkus, M.; Li, S. Imaging of highly malignant osteosarcoma with iodine-123-vascular endothelial growth factor. Oncology 2012, 83, 45–49. [Google Scholar] [CrossRef]
- Cornelissen, B.; Oltenfreiter, R.; Kersemans, V.; Staelens, L.; Frankenne, F.; Foidart, J.M.; Slegers, G. In vitro and in vivo evaluation of [123I]-VEGF165 as a potential tumor marker. Nucl. Med. Biol. 2005, 32, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Galli, F.; Artico, M.; Taurone, S.; Manni, I.; Bianchi, E.; Piaggio, G.; Weintraub, B.D.; Szkudlinski, M.W.; Agostinelli, E.; Signore, A. Radiolabeling of VEGF165 with 99mTc to evaluate VEGFR expression in tumor angiogenesis. Int. J. Oncol. 2017, 50, 2171–2179. [Google Scholar] [CrossRef]
- Chan, C.; Sandhu, J.; Guha, A.; Scollard, D.A.; Wang, J.; Chen, P.; Bai, K.; Lee, L.; Reilly, R.M. A human transferrin-vascular endothelial growth factor (hnTf-VEGF) fusion protein containing an integrated binding site for 111In for imaging tumor angiogenesis. J. Nucl. Med. 2005, 46, 1745–1752. [Google Scholar] [PubMed]
- Chan, C.; Cai, Z.; Su, R.; Reilly, R.M. 111In-or 99mTc-labeled recombinant VEGF bioconjugates: In vitro evaluation of their cytotoxicity on porcine aortic endothelial cells overexpressing Flt-1 receptors. Nucl. Med. Biol. 2010, 37, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Qin, Z.X.; Li, Q.W.; Liu, G.Y.; Luo, C.X.; Xie, G.F.; Zheng, L. Imaging targeted at tumor with 188Re-labeled VEGF189 exon 6-encoded peptide and effects of the transfecting truncated KDR gene in tumor-bearing nude mice. Nucl. Med. Biol. 2009, 36, 535–543. [Google Scholar] [CrossRef]
- Bodei, L.; Cremonesi, M.; Zoboli, S.; Grana, C.; Bartolomei, M.; Rocca, P.; Caracciolo, M.; Maäcke, H.R.; Chinol, M.; Paganelli, G. Receptor-mediated radionuclide therapy with 90 Y-DOTATOC in association with amino acid infusion: A phase I study. Eur. J. Nucl. Med. 2003, 30, 207–216. [Google Scholar] [CrossRef]
- Rolleman, E.J.; Bernard, B.F.; Breeman, W.A.P.; Forrer, F.; de Blois, E.; Hoppin, J.; Gotthardt, M.; Boerman, O.C.; Krenning, E.P.; de Jong, M. Molecular imaging of reduced renal uptake of radiolabelled [DOTA0, Tyr3] octreotate by the combination of lysine and Gelofusine in rats. Nuklearmedizin 2008, 47, 110–115. [Google Scholar] [CrossRef]
- Melis, M.; Bijster, M.; de Visser, M.; Konijnenberg, M.W.; de Swart, J.; Rolleman, E.J.; Boerman, O.C.; Krenning, E.P.; de Jong, M. Dose-response effect of Gelofusine on renal uptake and retention of radiolabelled octreotate in rats with CA20948 tumours. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, 1968. [Google Scholar] [CrossRef]
- Jayson, G.C.; Zweit, J.; Jackson, A.; Mulatero, C.; Julyan, P.; Ranson, M.; Broughton, L.; Wagstaff, J.; Hakannson, L.; Groenewegen, G.; et al. Molecular imaging and biological evaluation of HuMV833 anti-VEGF antibody: Implications for trial design of antiangiogenic antibodies. J. Natl. Cancer Inst. 2002, 94, 1484–1493. [Google Scholar] [CrossRef]
- Cai, W.; Chen, X. Multimodality imaging of vascular endothelial growth factor and vascular endothelial growth factor receptor expression. Front. Biosci. 2007, 12, 4267–4279. [Google Scholar] [CrossRef]
- Choe, Y.S.; Lee, K.H. Targeted In Vivo Imaging of Angiogenesis: Present Status and Perspectives. Curr. Pharm. Des. 2007, 13, 17–31. [Google Scholar] [CrossRef]
- Cai, W.; Chen, X. Multimodality Molecular Imaging of Tumor Angiogenesis. J. Nucl. Med. 2008, 49, 113S–128S. [Google Scholar] [CrossRef]
- Michalski, M.H.; Chen, X. Molecular imaging in cancer treatment. Eur. J. Nucl. Med. Mol. Imaging 2011, 38, 358–377. [Google Scholar] [CrossRef]
- Collingridge, D.R.; Carroll, V.A.; Glaser, M.; Aboagye, E.O.; Osman, S.; Hutchinson, O.C.; Barthel, H.; Luthra, S.K.; Brady, F.; Bicknell, R.; et al. The Development of [124I]Iodinated-VG76e: A Novel Tracer for Imaging Vascular Endothelial Growth Factor in Vivo Using Positron Emission Tomography. Cancer Res. 2002, 62, 5912–5919. [Google Scholar]
- Bouziotis, P.; Psimadas, D.; Fani, M.; Gourni, E.; Loudos, G.; Xanthopoulos, S.; Archimandritis, S.C.; Varvarigou, A.D. Radiolabeled biomolecules for early cancer detection and therapy via angiogenesis targeting. Nucl. Instrum. Methods Phys. Res. A 2006, 569, 492–496. [Google Scholar] [CrossRef]
- Fani, M.; Bouziotis, P.; Harris, A.L.; Psimadas, D.; Gourni, E.; Loudos, G.; Varvarigou, A.D.; Maecke, H.R. 177Lu-labeled-VG76e monoclonal antibody in tumor angiogenesis: A comparative study using DOTA and DTPA chelating systems. Radiochim. Acta 2007, 95, 351–357. [Google Scholar] [CrossRef]
- Willmann, J.K.; Paulmurugan, R.; Chen, K.; Gheysens, O.; Rodriguez-Porcel, M.; Lutz, A.M.; Chen, I.Y.; Chen, X.; Gambhir, S.S. US imaging of tumor angiogenesis with microbubbles targeted to vascular endothelial growth factor receptor type 2 in mice. Radiology 2008, 246, 508–518. [Google Scholar] [CrossRef]
- Willmann, J.K.; Cheng, Z.; Davis, C.; Lutz, A.M.; Schipper, M.L.; Nielsen, C.H.; Gambhir, S.S. Targeted microbubbles for imaging tumor angiogenesis: Assessment of whole-body biodistribution with dynamic micro-PET in mice. Radiology 2008, 249, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.M.; Kim, E.M.; Cheong, S.J.; Kim, D.W.; Lim, S.T.; Sohn, M.H.; Jeong, H.J. Targeted molecular imaging of VEGF receptors overexpressed in ischemic microvasculature using chitosan-DC101 conjugates. J. Biomed. Mater. Res. A 2010, 92, 1510–1517. [Google Scholar] [CrossRef]
- Desar, I.M.E.; Stillebroer, A.B.; Oosterwijk, E.; Leenders, W.P.J.; van Herpen, C.M.L.; van der Graaf, W.T.A.; Boerman, O.C.; Mulders, P.F.A.; Oyen, W.J.G. 111In-Bevacizumab Imaging of Renal Cell Cancer and Evaluation of Neoadjuvant Treatment with the Vascular Endothelial Growth Factor Receptor Inhibitor Sorafenib. J. Nucl. Med. 2010, 51, 1707–1715. [Google Scholar] [CrossRef]
- Chang, A.J.; Sohn, R.; Lu, Z.H.; Arbeit, J.M.; Lapi, S.E. Detection of Rapalog-Mediated Therapeutic Response in Renal Cancer Xenografts Using 64Cu-bevacizumab ImmunoPET. PLoS ONE 2013, 8, e58949. [Google Scholar] [CrossRef]
- Cea, V.; Sala, C.; Verpelli, C. Antiangiogenic Therapy for Glioma. J. Signal Transduct. 2012, 483040. [Google Scholar] [CrossRef] [PubMed]
- Gerstner, E.R.; Batchelor, T.T. Antiangiogenic therapy for glioblastoma. Cancer J. 2012, 18, 45–50. [Google Scholar] [CrossRef]
- Batchelor, T.T.; Reardon, D.A.; de Groot, J.F.; Wick, W.; Weller, M. Antiangiogenic therapy for glioblastoma: Current status and future prospects. Clin. Cancer Res. 2014, 20, 5612–5619. [Google Scholar] [CrossRef]
- Kozakiewicz, P.; Kordzińska-Cisek, I.; Król-Woch, K.; Stachyra, P. Anti-angiogenic therapy in glioblastoma multiforme. Oncol. Radiother. 2018, 2, 17–22. [Google Scholar]
- Nagengast, W.B.; de Vries, E.G.E.; Hospers, G.A.; Mulder, N.H.; de Jong, J.R.; Hollema, H.; Brouwers, A.H.; van Dongen, G.A.; Perk, L.R.; Lub-de Hooge, M.N. In Vivo VEGF Imaging with Radiolabeled Bevacizumab in a Human Ovarian Tumor Xenograft. J. Nucl. Med. 2007, 48, 1313–1319. [Google Scholar] [CrossRef] [PubMed]
- Scheer, M.G.; Stollman, T.H.; Boerman, O.C.; Verrijp, K.; Sweep, F.C.G.J.; Leenders, W.P.J.; Ruers, T.J.M.; Oyen, W.J.G. Imaging liver metastases of colorectal cancer patients with radiolabelled bevacizumab: Lack of correlation with VEGF-A expression. Eur. J. Cancer 2008, 44, 1835–1840. [Google Scholar] [CrossRef] [PubMed]
- Nagengast, W.B.; Lub-de Hooge, M.N.; van Straten, E.M.E.; Kruijff, S.; Brouwers, A.H.; den Dunnen, W.F.A.; de Jong, J.R.; Hollema, H.; Dierckx, R.A.; Mulder, N.H.; et al. VEGF-SPECT with 111In-bevacizumab in stage III/IV melanoma patients. Eur. J. Cancer 2011, 47, 1595–1602. [Google Scholar] [CrossRef]
- Stollman, T.H.; Scheer, M.G.W.; Leenders, W.P.J.; Verrijp, K.C.N.; Soede, A.C.; Oyen, W.J.G.; Ruers, T.J.M.; Boerman, O.C. Specific imaging of VEGF-A expression with radiolabeled anti-VEGF monoclonal antibody. Int. J. Cancer 2008, 122, 2310–2314. [Google Scholar] [CrossRef]
- Stollman, T.H.; Scheer, M.G.; Franssen, G.M.; Verrijp, K.N.; Oyen, W.J.G.; Ruers, T.J.M.; Leenders, W.P.J.; Boerman, O.C. Tumor accumulation of radiolabeled bevacizumab due to targeting of cell- and matrix-associated VEGF-A isoforms. Cancer Biother. Radiopharm. 2009, 24, 195–200. [Google Scholar] [CrossRef]
- Hosseinimehr, S.J.; Orlova, A.; Tolmachev, V. Preparation and in vitro evaluation of 111In-CHX-A″-DTPA-labeled anti-VEGF monoclonal antibody bevacizumab. Hum. Antibodies 2010, 19, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Nayak, T.K.; Garmestani, K.; Baidoo, K.E.; Milenic, D.E.; Brechbiel, M.W. PET imaging of tumor angiogenesis in mice with VEGF-A targeted 86Y-CHX-A″-DTPA-bevacizumab. Int. J. Cancer 2011, 128, 920–926. [Google Scholar] [CrossRef]
- Van Dongen, G.A.M.S.; Poot, A.J.; Vugt, D.J. PET imaging with radiolabeled antibodies and tyrosine kinase inhibitors: Immuno-PET and TKI-PET. Tumor Biol. 2012, 33, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Kameswaran, M.; Pandey, U.; Gamre, N.; Vimalnath, K.V.; Sarma, H.D.; Dash, A. Evaluation of (177)Lu-CHX-A’’-DTPA-Bevacizumab as a radioimmunotherapy agent targeting VEGF expressing cancers. Appl. Radiat. Isot. 2016, 114, 196–201. [Google Scholar] [CrossRef]
- Patel, N.; Able, S.; Allen, D.; Fokas, E.; Cornelissen, B.; Gleeson, F.V.; Harris, A.L.; Vallis, K.A. Monitoring response to anti-angiogenic mTOR inhibitor therapy in vivo using 111In-bevacizumab. EJNMMI Res. 2017, 7, 49. [Google Scholar] [CrossRef] [PubMed]
- Yudistiro, R.; Hanaoka, H.; Katsumata, N.; Yamaguchi, A.; Tsushima, Y. Bevacizumab Radioimmunotherapy (RIT) with Accelerated Blood Clearance Using the Avidin Chase. Mol. Pharm. 2018, 15, 2165–2173. [Google Scholar] [CrossRef]
- Nagengast, W.B.; de Korte, M.A.; Munnink, T.H.O.; Timmer-Bosscha, H.; den Dunnen, W.F.; Hollema, H.; de Jong, J.R.; Jensen, M.R.; Quadt, C.; Garcia-Echeverria, C.; et al. 89Zr-Bevacizumab PET of Early Antiangiogenic Tumor Response to Treatment with HSP90 Inhibitor NVP-AUY922. J. Nucl. Med. 2010, 51, 761–767. [Google Scholar] [CrossRef]
- Van der Bilt, A.R.; Terwisscha van Scheltinga, A.G.; Timmer-Bosscha, H.; Schröder, C.P.; Pot, L.; Kosterink, J.G.W.; van der Zee, A.G.J.; Lub-de Hooge, M.N.; de Jong, S.; de Vries, E.G.E.; et al. Measurement of tumor VEGF-A levels with 89Zr-bevacizumab PET as an early biomarker for the antiangiogenic effect of everolimus treatment in an ovarian cancer xenograft model. Clin. Cancer Res. 2012, 18, 6306–6314. [Google Scholar] [CrossRef] [PubMed]
- Van Asselt, S.J.; Oosting, S.F.; Brouwers, A.H.; Bongaerts, A.H.H.; de Jong, J.R.; Lub-de Hooge, M.N.; Munnink, T.H.O.; Fiebrich, H.B.; Sluiter, W.J.; Links, T.P.; et al. Everolimus Reduces (89)Zr-Bevacizumab Tumor Uptake in Patients with Neuroendocrine Tumors. J. Nucl. Med. 2014, 55, 1087–1092. [Google Scholar] [CrossRef] [PubMed]
- Van Es, S.C.; Brouwers, A.H.; Mahesh, S.V.K.; Leliveld-Kors, A.M.; de Jong, I.J.; Lub-de Hooge, M.N.; de Vries, E.G.E.; Gietema, J.A.; Oosting, S.F. 89Zr-Bevacizumab PET: Potential Early Indicator of Everolimus Efficacy in Patients with Metastatic Renal Cell Carcinoma. J. Nucl. Med. 2017, 58, 905–910. [Google Scholar] [CrossRef] [PubMed]
- Gaykema, S.B.M.; Brouwers, A.H.; Lub-de Hooge, M.N.; Timmer-Bosscha, H.; Pot, L.; van Dam, G.M.; Pleijhuis, R.G.; van der Meulen, S.B.; Bart, J.; de Vries, J.; et al. 89Zr-Bevacizumab PET Imaging in Primary Breast Cancer. J. Nucl. Med. 2013, 54, 1014–1018. [Google Scholar] [CrossRef]
- Bahce, I.; Huisman, M.C.; Verwer, E.E.; Ooijevaar, R.; Boutkourt, F.; Vugts, D.J.; van Dongen, G.A.; Boellaard, R.; Smit, E.F. Pilot study of 89Zr-bevacizumab positron emission tomography in, patients with advanced non-small cell lung cancer. EJNMMI Res. 2014, 4, 35. [Google Scholar] [CrossRef] [PubMed]
- Oosting, S.; Brouwers, A.H.; Van Es, S.C.; Nagengast, W.B.; Munnink, T.H.O.; Hooge, M.N.L.-D.; Hollema, H.; De Jong, J.R.; De Jong, I.J.; De Haas, S.; et al. 89 Zr-bevacizumab PET imaging in metastatic renal cell carcinoma patients before and during antiangiogenic treatment. J. Clin. Oncol. 2012, 30, 10581. [Google Scholar] [CrossRef]
- Oosting, S.F.; Brouwers, A.H.; Van Es, S.C.; Nagengast, W.B.; Munnink, T.H.O.; Hooge, M.N.L.-D.; Hollema, H.; De Jong, J.R.; De Jong, I.J.; De Haas, S.; et al. 89Zr-bevacizumab PET visualizes heterogeneous tracer accumulation in tumour lesions of renal cell carcinoma patients and differential effects of antiangiogenic treatment. J. Nucl. Med. 2015, 56, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Oosting, F.S.; van Asselt, S.J.; Brouwers, A.H.; Bongaerts, A.H.H.; Steinberg, J.D.J.; de Jong, J.R.; Lub-de Hooge, M.N.; van der Horst-Schrivers, A.N.A.; Walenkamp, A.M.E.; Hoving, E.W.; et al. 89Zr-Bevacizumab PET Visualizes Disease Manifestations in Patients with von Hippel–Lindau Disease. J. Nucl. Med. 2016, 57, 1244–1250. [Google Scholar] [CrossRef] [PubMed]
- Camacho, X.; García, M.F.; Calzada, V.; Fernández, M.; Porcal, W.; Alonso, O.; Gambini, J.P.; Cabral, P. Synthesis and evaluation of (99m)Tc chelate-conjugated bevacizumab. Curr. Radiopharm 2013, 6, 12–19. [Google Scholar] [CrossRef]
- Camacho, X.; García, M.F.; Calzada, V.; Fernández, M.; Chabalgoity, J.A.; Moreno, M.; de Aguiar, R.B.; Alonso, O.; Gambini, J.P.; Chammas, R.; et al. [99mTc(CO)3]-Radiolabeled Bevacizumab: In vitro and in vivo Evaluation in a Melanoma Model. Oncology 2013, 84, 200–209. [Google Scholar] [CrossRef]
- Camacho, X.; García, M.F.; Calzada, V.; Fernández, M.; Alonso, O.; Gambini, J.P.; de Aguiar, R.B.; Machado, C.M.L.; Chamms, R.; Porcal, W.; et al. 99mTc-Labeled Bevacizumab via HYNIC for Imaging of Melanoma. J. Anal. Oncol. 2014, 3, 53–64. [Google Scholar] [CrossRef]
- Kameswaran, M.; Pandey, U.; Sarma, H.D.; Samuel, G. Preparation of 99mTc carbonyl DTPA-bevacizumab and its bioevaluation in a melanoma model. Ann. Nucl. Med. 2014, 28, 911–916. [Google Scholar] [CrossRef]
- Cohen, R.; Stammes, M.A.; de Roos, I.H.; Stigter-van Walsum, M.; Visser, G.W.; van Dongen, G.A. Inert coupling of IRDye800CW to monoclonal antibodies for clinical optical imaging of tumor targets. EJNMMI Res. 2011, 1, 31. [Google Scholar] [CrossRef]
- Cohen, R.; Vugts, D.J.; Stigter-van Walsum, M.; Visser, G.W.; van Dongen, G.A. Inert coupling of IRDye800CW and zirconium-89 to monoclonal antibodies for single- or dual-mode fluorescence and PET imaging. Nat. Protoc. 2013, 8, 1010–1018. [Google Scholar] [CrossRef]
- Jansen, M.H.; Lagerweij, T.; Sewing, A.C.; Vugts, D.J.; van Vuurden, D.G.; Molthoff, C.F.M.; Caretti, V.; Veringa, S.J.E.; Petersen, N.; Carcaboso, A.M.; et al. Bevacizumab Targeting Diffuse Intrinsic Pontine Glioma: Results of 89Zr-Bevacizumab PET Imaging in Brain Tumor Models. Mol. Cancer Ther. 2016, 15, 2166–2174. [Google Scholar] [CrossRef]
- Jansen, M.H.; Veldhuijzen van Zanten, S.E.M.; van Vuurden, D.G.; Huisman, M.C.; Vugts, D.J.; Hoekstra, O.S.; van Dongen, G.A.; Kaspers, G.J.L. Molecular Drug Imaging: 89Zr-Bevacizumab PET in Children with Diffuse Intrinsic Pontine Glioma. J. Nucl. Med. 2017, 58, 711–716. [Google Scholar] [CrossRef]
- Veldhuijzen van Zanten, S.E.M.; Sewing, A.C.P.; van Lingen, A.; Hoekstra, O.S.; Wesseling, P.; Meel, M.H.; van Vuurden, D.G.; Kaspers, G.J.L.; Hulleman, E.; Bugiani, M. Multiregional Tumor Drug-Uptake Imaging by PET and Microvascular Morphology in End-Stage Diffuse Intrinsic Pontine Glioma. J. Nucl. Med. 2018, 59, 612–615. [Google Scholar] [CrossRef] [PubMed]
- Ashrafi, S.A.; Hosseinimehr, S.J.; Varmira, K.; Abedi, S.M. Radioimmunotherapy with 131I-bevacizumab as a specific molecule for cells with overexpression of the vascular endothelial growth factor. Cancer Biother. Radiopharm. 2012, 27, 420–425. [Google Scholar] [CrossRef]
- Kameswaran, M.; Sarma, H.D.; Dash, A. Preclinical evaluation of 131I-Bevacizumab—A prospective agent for radioimmunotherapy in VEGF expressing cancers. Appl. Radiat. Isot. 2017, 123, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Christoforidis, J.B.; Carlton, M.M.; Knopp, M.V.; Hinkle, G.H. PET/CT imaging of I-124-radiolabeled bevacizumab and ranibizumab after intravitreal injection in a rabbit model. Invest. Ophthalmol. Vis. Sci. 2011, 52, 5899–5903. [Google Scholar] [CrossRef] [PubMed]
- Christoforidis, J.B.; Carlton, M.M.; Wang, J.; Jiang, A.; Pratt, C.; Abdel-Rasoul, M.; Hinkle, G.H.; Knopp, M.V. Anatomic and pharmacokinetic properties of intravitreal bevacizumab and ranibizumab after vitrectomy and lensectomy. Retina 2013, 33, 946–952. [Google Scholar] [CrossRef]
- Christoforidis, J.B.; Briley, K.; Binzel, K.; Bhatia, P.; Wei, L.; Kumar, K.; Knopp, M.V. Systemic Biodistribution and Intravitreal Pharmacokinetic Properties of Bevacizumab, Ranibizumab, and Aflibercept in a Nonhuman Primate Model. Invest. Ophthalmol. Vis. Sci. 2017, 58, 5636–5645. [Google Scholar] [CrossRef]
- Paudyal, B.; Paudyal, P.; Oriuchi, N.; Hanaoka, H.; Tominaga, H.; Endo, K. Positron emission tomography imaging and biodistribution of vascular endothelial growth factor with 64Cu-labeled bevacizumab in colorectal cancer xenografts. Cancer Sci. 2011, 102, 117–121. [Google Scholar] [CrossRef]
- Zhang, Y.; Hong, H.; Engle, J.W.; Yang, Y.; Barnhart, T.E.; Cai, W. Positron emission tomography and near-infrared fluorescence imaging of vascular endothelial growth factor with dual-labeled bevacizumab. Am. J. Nucl. Med. Mol. Imaging 2012, 2, 1–13. [Google Scholar]
- Zhang, Y.; Hong, H.; Cai, W. PET tracers based on Zirconium-89. Curr. Radiopharm. 2011, 4, 131–139. [Google Scholar] [CrossRef]
- Wei, W.; Ni, D.; Ehlerding, E.B.; Luo, Q.-Y.; Cai, W. PET Imaging of Receptor Tyrosine Kinases in Cancer. Mol. Cancer Ther. 2018, 17, 1625–1636. [Google Scholar] [CrossRef]
- Luo, H.; England, C.G.; Graves, S.A.; Sun, H.; Liu, G.; Nickles, R.J.; Cai, W. PET Imaging of VEGFR-2 Expression in Lung Cancer with 64Cu-Labeled Ramucirumab. J. Nucl. Med. 2016, 57, 285–290. [Google Scholar] [CrossRef]
- Laffon, E.; Marthan, R. A three-time-point method for assessing kinetic parameters of 64Cu-labeled Ramucirumab trapping in VEGFR-2 positive lung tumors. Phys. Med. 2017, 43, 1–5. [Google Scholar] [CrossRef]
- Li, M.; Jiang, D.; Barnhart, T.E.; Cao, T.; Engle, J.W.; Chen, W.; Cai, W. Immuno-PET imaging of VEGFR-2 expression in prostate cancer with 89Zr-labeled ramucirumab. Am. J. Cancer Res. 2019, 9, 2037–2046. [Google Scholar] [PubMed]
- Janousek, J.; Barta, P.; Novy, Z.; Zilkova, K.; Trejtnar, F. Antiangiogenic Human Monoclonal Antibody Ramucirumab Radiolabelling: In Vitro Evaluation on VEGFR2-positive Cell Lines. Anticancer Res. 2019, 39, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Nagengast, W.B.; Lub-de Hooge, M.N.; Oosting, S.F.; den Dunnen, W.F.A.; Warnders, F.J.; Brouwers, A.H.; de Jong, J.R.; Price, P.M.; Hollema, H.; Hospers, G.A.P.; et al. VEGF-PET Imaging Is a Noninvasive Biomarker Showing Differential Changes in the Tumor during Sunitinib Treatment. Cancer Res. 2011, 71, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Christoforidis, J.B.; Williams, M.M.; Kothandaraman, S.; Kumar, K.; Epitropoulos, F.J.; Knopp, M.V. Pharmacokinetic properties of intravitreal I-124-aflibercept in a rabbit model using PET/CT. Curr. Eye Res. 2012, 37, 1171–1174. [Google Scholar] [CrossRef] [PubMed]
- Hao, G.; Hajibeigi, A.; León-Rodríguez, L.M.; Oz, O.K.; Sun, X. Peptoid-based PET imaging of vascular endothelial growth factor receptor (VEGFR) expression. Am. J. Nucl. Med. Mol. Imaging 2011, 1, 65–75. [Google Scholar]
- Cai, W.; Hong, H. Peptoid and positron emission tomography: An appealing combination. Am. J. Nucl. Med. Mol. Imaging 2011, 1, 76–79. [Google Scholar]
- Rezazadeh, F.; Sadeghzadeh, N.; Abedi, S.M.; Abediankenari, S. 99mTc-D (LPR): A novel retro-inverso peptide for VEGF receptor-1 targeted tumor imaging. Nucl. Med. Biol. 2018, 2. [Google Scholar] [CrossRef] [PubMed]
- Giordano, R.J.; Cardó-Vila, M.; Salameh, A.; Anobom, C.D.; Zeitlin, B.D.; Hawke, D.H.; Valente, A.P.; Almeida, F.C.L.; Nör, J.E.; Sidman, R.L.; et al. From combinatorial peptide selection to drug prototype (I): Targeting the vascular endothelial growth factor receptor pathway. Proc. Natl. Acad. Sci. USA 2010, 107, 5112–5117. [Google Scholar] [CrossRef]
- Hicks, J.W.; VanBrocklin, H.F.; Wilson, A.A.; Houle, S.; Vasdev, N. Radiolabeled small molecule protein kinase inhibitors for imaging with PET or SPECT. Molecules 2010, 15, 8260–8278. [Google Scholar] [CrossRef]
- Kuchar, M.; Oliveira, M.C.; Gano, L.; Santos, I.; Kniess, T. Radioiodinated sunitinib as a potential radiotracer for imaging angiogenesis-radiosynthesis and first radiopharmacological evaluation of 5-[125I]Iodo-sunitinib. Bioorg. Med. Chem. Lett. 2012, 22, 2850–2855. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.Q.; Miller, K.D.; Sledge, G.; Zheng, Q.H. Synthesis of [F-18]SU11248, a new potential PET tracer for imaging cancer tyrosine kinase. Bioorg. Med. Chem. Lett. 2005, 15, 4380–4384. [Google Scholar] [CrossRef]
- Kniess, T.; Bergmann, R.; Steinbach, J. Synthesis and metabolic stability of 11C-labelled SU11248 derivative as inhibitor of tyrosine kinases. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, S310. [Google Scholar]
- Caballero, J.; Muñoz, C.; Alzate-Morales, J.H.; Cunha, S.; Gano, L.; Bergmann, R.; Steinbach, J.; Kniess, T. Synthesis, in silico, in vitro, and in vivo investigation of 5-[11C]methoxy-substituted sunitinib, a tyrosine kinase inhibitor of VEGFR-2. Eur. J. Med. Chem. 2012, 58, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Kniess, T.; Bergmann, R.; Kuchar, M.; Steinbach, J.; Wuest, F. Synthesis and radiopharmacological investigation of 3-[4′-[(18)F]fluorobenzylidene]indolin-2-one as possible tyrosine kinase inhibitor. Bioorg. Med. Chem. 2009, 17, 7732–7742. [Google Scholar] [CrossRef]
- Sakr, T.M.; El-Safoury, D.M.; Awad, G.A.; Motaleb, M.A. Biodistribution of 99mTc-sunitinib as a potential radiotracer for tumor hypoxia imaging. J. Label. Comp. Radiopharm. 2013, 56, 392–395. [Google Scholar] [CrossRef] [PubMed]
- Schuller, H.M.; Kabalka, G.W.; Schuller, H.M. Diagnosis by Determination of Hyperactivity or Increased Expression of Members of Cell Signaling Pathways. U.S. Patent 2006/0233705 A1, 19 October 2006. [Google Scholar]
- Asakawa, C.; Ogawa, M.; Kumata, K.; Fujinaga, M.; Kato, K.; Yamasaki, T.; Yui, J.; Kawamura, K.; Hatori, A.; Fukumura, T.; et al. [11C]Sorafenib: Radiosynthesis and preliminary PET study of brain uptake in P-gp/Bcrp knockout mice. Bioorg. Med. Chem. Lett. 2011, 21, 2220–2223. [Google Scholar] [CrossRef] [PubMed]
- Poot, A.J.; van der Wildt, B.; Stigter-van Walsum, M.; Rongen, M.; Schuit, R.C.; Hendrikse, N.H.; Eriksson, J.; van Dongen, G.A.M.S.; Windhorst, A.D. [11C]Sorafenib: Radiosynthesis and preclinical evaluation in tumor-bearing mice of a new TKI-PET tracer. Nucl. Med. Biol. 2013, 40, 488–497. [Google Scholar] [CrossRef]
- Ilovich, O.; Jacobson, O.; Aviv, Y.; Litchi, A.; Chisin, R.; Mishani, E. Formation of fluorine-18 labeled diaryl ureas-labeled VEGFR-2/PDGFR dual inhibitors as molecular imaging agents for angiogenesis. Bioorg. Med. Chem. 2008, 16, 4242–4251. [Google Scholar] [CrossRef]
- Ilovich, O.; Åberg, O.; Langstrom, B.; Mishani, E. Rhodium-mediated [11C]Carbonylation: A library of N-phenyl-N′-{4-(4-quinolyloxy)-phenyl}-[11C]-urea derivatives as potential PET angiogenic probes. J. Label. Compd. Radiopharm. 2009, 52, 151–157. [Google Scholar] [CrossRef]
- Sun, W. Angiogenesis in metastatic colorectal cancer and the benefits of targeted therapy. J. Hematol. Oncol. 2012, 5, 63. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Lola, C.M.; Wang, M.; Miller, K.D.; Sledge, G.W.; Zheng, Q.H. Radiosynthesis of [11C]Vandetanib and [11C]chloro-Vandetanib as new potential PET agents for imaging of VEGFR in cancer. Bioorg. Med. Chem. Lett. 2011, 21, 3222–3226. [Google Scholar] [CrossRef]
- Dischino, D.; Tran, T.; Donnelly, D.; Bonacorsi, S.; Chow, P.; Roache, R.; Kukral, D.; Kim, J.; Hayes, W. Radiosynthesis of a F-18 labeled fluoro analog of brivanib. J. Label. Compd. Radiopharm. 2011, 54, S444. [Google Scholar]
- Ilovich, O.; Billauer, H.; Dotan, S.; Mishani, E. Labeled 3-aryl-4-indolylmaleimide derivatives and their potential as angiogenic PET biomarkers. Bioorg. Med. Chem. 2010, 18, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Hirata, M.; Asanom, A.; Magata, Y.; Ohmomo, Y.; Temma, T. Synthesis and evaluation of novel radioiodinated anthranilate derivatives for in vivo imaging of vascular endothelial growth factor receptor with single-photon emission computed tomography. Ann. Nucl. Med. 2020, 34, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Mitran, B.; Güler, R.; Roche, F.P.; Lindström, E.; Selvaraju, R.M.; Fleetwood, F.; Rinne, S.S.; Claesson-Welsh, L.; Tolmachev, V.; Stahl, S.; et al. Radionuclide imaging of VEGFR2 in glioma vasculature using biparatopic affibody conjugate: Proof-of-principle in a murine model. Theranostics 2018, 8, 4462–4476. [Google Scholar] [CrossRef] [PubMed]
- Niland, S.; Eble, J.A. Neuropilin: Handyman and Power Broker in the Tumor Microenvironment. Advances in Experimental Medicine and Biology. In Tumor Microenvironment; Birbrair, A., Ed.; Springer: Cham, Switzerland, 2020; Volume 1223, pp. 31–67. [Google Scholar] [CrossRef]
- Mota, F.; Fotinou, C.; Rana, R.R.; Chan, A.E.; Yelland, T.; Arooz, M.T.; O’Leary, A.P.; Hutton, J.; Frankel, P.; Zachary, I.; et al. Architecture and hydration of the arginine-binding site of neuropilin-1. FEBS J. 2018, 285, 1290–1304. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.; Bai, Y.; Zhu, Q.; Hu, B.; Xu, Y. Targeting VEGF–neuropilin interactions: A promising antitumor strategy. Drug Discov. Today 2019, 24, 656–664. [Google Scholar] [CrossRef]
- Vander Kooi, C.W.; Jusino, M.A.; Perman, B.; Neau, D.B.; Bellamy, H.D.; Leahy, D.J. Structural basis for ligand and heparin binding to neuropilin B domains. Proc. Natl. Acad. Sci. USA 2007, 104, 6152–6157. [Google Scholar] [CrossRef] [PubMed]
- Jia, H.; Bagherzadeh, A.; Hartzoulakis, B.; Jarvis, A.; Löhr, M.; Shaikh, S.; Aqil, R.; Cheng, L.; Tickner, M.; Esposito, D.; et al. Characterization of a bicyclic peptide neuropilin-1 (NP-1) antagonist (EG3287) reveals importance of vascular endothelial growth factor exon 8 for NP-1 binding and role of NP-1 in KDR signaling. J. Biol. Chem. 2006, 281, 13493–13502. [Google Scholar] [CrossRef]
- Starzec, A.; Ladam, P.; Vassy, R.; Badache, S.; Bouchemal, N.; Navaza, A.; du Penhoat, C.H.; Perret, G.Y. Structure–function analysis of the antiangiogenic ATWLPPR peptide inhibiting VEGF165 binding to neuropilin-1 and molecular dynamics simulations of the ATWLPPR/neuropilin-1 complex. Peptides 2007, 28, 2397–2402. [Google Scholar] [CrossRef] [PubMed]
- Teesalu, T.; Sugahara, K.N.; Ruoslahti, E. Tumor-penetrating peptides. Front. Oncol. 2013, 3, 216. [Google Scholar] [CrossRef]
- Perret, G.Y.; Starzec, A.; Hauet, N.; Vergote, J.; Le Pecheur, M.; Vassy, R.; Léger, G.; Verbeke, K.A.; Bormans, G.; Nicolas, P.; et al. In vitro evaluation and biodistribution of a 99mTc-labeled anti-VEGF peptide targeting neuropilin-1. Nucl. Med. Biol. 2004, 31, 575–581. [Google Scholar] [CrossRef]
- Lan, X.L.; Gao, Z.R.; Sun, L. An experimental study on radionuclide imaging with radiolabeled blood vessel polypeptide in diagnosis for malignant tumor. J. Oncol. 2008, 14, 627–630. [Google Scholar]
- Wu, H.; Chen, H.; Pan, D.; Ma, Y.; Liang, S.; Wan, Y.; Fang, Y. Imaging integrin α v β 3 and NRP-1 positive gliomas with a novel fluorine-18 labeled RGD-ATWLPPR heterodimeric peptide probe. Mol. Imaging Biol. 2014, 16, 781–792. [Google Scholar] [CrossRef]
- Liang, S.; Ma, Y.; Guo, J.; Guo, R.; Wang, H. 18 F-radiolabeled analogs of peptide RGD-A7R for simultaneous PET imaging of both αvβ3 and VEGF in tumors. J. Radioanal. Nucl. Chem. 2015, 303, 1891–1896. [Google Scholar] [CrossRef]
- Ma, Y.; Liang, S.; Guo, J.; Guo, R.; Wang, H. 18F labeled RGD-A7R peptide for dual integrin and VEGF-targeted tumor imaging in mice bearing U87MG tumors. J. Label. Compd. Radio Pharm. 2014, 57, 627–631. [Google Scholar] [CrossRef]
- Ma, Y.; Liang, S.; Guo, J.; Wang, H. 18 F-radiolabeled RGD-A7R-conjugated nano-particles for integrin and VEGF-targeted tumor imaging. J. Radioanal. Nucl. Chem. 2016, 308, 741–746. [Google Scholar] [CrossRef]
- Alberici, L.; Roth, L.; Sugahara, K.N.; Agemy, L.; Kotamraju, V.R.; Teesalu, T.; Bordignon, C.; Traversari, C.; Rizzardi, G.P.; Ruoslahti, E. De novo design of a tumor-penetrating peptide. Cancer Res. 2013, 73, 804–812. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Yang, W.; Zhang, M.; Li, G.; Wang, S.; Wang, Z.; Ma, X.; Kang, F.; Wang, J. Evaluation of 68 Ga-labeled iNGR peptide with tumor-penetrating motif for microPET imaging of CD13-positive tumor xenografts. Tumor Biol. 2016, 37, 12123–12131. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Zhu, L.; Ma, Y.; Niu, G.; Chen, X. Synthesis and evaluation of new iRGD peptide analogs for tumor optical imaging. Bioorg. Med. Chem. Lett. 2011, 21, 1146–1150. [Google Scholar] [CrossRef] [PubMed]
- Satpati, D.; Vats, K.; Sharma, R.; Sarma, H.D.; Dash, A. 68Ga-labeling of internalizing RGD (iRGD) peptide functionalized with DOTAGA and NODAGA chelators. J. Pept. Sci. 2020, 26, e3241. [Google Scholar] [CrossRef] [PubMed]
- Carlsen, J.; Gildehaus, F.J.; Pfeiffer, S.; Oos, R.; Haubner, R.; Bormann-Giglmaier, K.; Schumacher, G.; Bartenstein, P. iRGD peptides labelled with 68-Ga as diagnostic tracers for human cancers using μPET and for future therapy labelled with 177-Lu. J. Nucl. Med. 2013, 54 (Suppl. 2), 1327. [Google Scholar]
- Zhao, M.; Kang, F.; Zhang, M.; Wang, S.; Yang, W.; Wang, J. Evaluation of 68Ga-labeled iNGR peptide with tumor penetrating motif for microPET imaging of CD13-positive tumor xenografts. J. Nucl. Med. 2015, 56 (Suppl. 3), 1157. [Google Scholar] [CrossRef]
- Adhikari, A.; Tiwari, A.K.; Shukla, A.; Mishra, A.K.; Datta, A. Synthesis and Preclinical Evaluation of Radioligand, 99mTc-DO3A-Et-RPAR for Imaging NRP-1 Specific Tumor. ChemistrySelect 2019, 4, 12950–12954. [Google Scholar] [CrossRef]
- Dong, P.; Cai, H.; Chen, L.; Li, Y.; Yuan, C.; Wu, X.; Shen, G.; Zhou, H.; Zhang, W.; Li, L. Biodistribution and evaluation of 131I-labeled neuropilin-binding peptide for targeted tumor imaging. Contrast Media Mol. Imaging 2016, 11, 467–474. [Google Scholar] [CrossRef]
- Simón-Gracia, L.; Scodeller, P.; Fuentes, S.S.; Vallejo, V.G.; Ríos, X.; San Sebastián, E.; Sidorenko, V.; Di Silvo, D.; Suck, M.; De Lorenzi, F.; et al. Application of polymersomes engineered to target p32 protein for detection of small breast tumors in mice. Oncotarget 2018, 9, 18682. [Google Scholar] [CrossRef] [PubMed]
- Feng, G.K.; Liu, R.B.; Zhang, M.Q.; Ye, X.X.; Zhong, Q.; Xia, Y.F.; Li, M.Z.; Wang, J.; Song, E.W.; Zhang, X.; et al. SPECT and near-infrared fluorescence imaging of breast cancer with a neuropilin-1-targeting peptide. J. Control. Release 2014, 192, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Luo, F.; Wang, S.; Ni, E.; Tang, X.; Lv, H.; Chen, X.; Chen, L.; Yan, J. Monoclonal antibody against NRP-1 b1b2. Hybridoma 2011, 30, 369–373. [Google Scholar] [CrossRef]
- Chen, L.; Miao, W.; Tang, X.; Zhang, H.; Wang, S.; Luo, F.; Yan, J. Inhibitory effect of neuropilin-1 monoclonal antibody (NRP-1 MAb) on glioma tumor in mice. J. Biomed. Nanotechnol. 2013, 9, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Zeng, F.; Luo, F.; Lv, S.; Zhang, H.; Cao, C.; Chen, X.; Wang, S.; Li, Z.; Wang, X.; Dou, X.; et al. A monoclonal antibody targeting neuropilin-1 inhibits adhesion of MCF7 breast cancer cells to fibronectin by suppressing the FAK/p130cas signaling pathway. Anticancer Drugs 2014, 25, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Dou, X.; Yan, J.; Zhang, Y.; Liu, P.; Jiang, Y.; Lv, S.; Zeng, F.; Chen, X.; Wang, S.; Zhang, H.; et al. SPECT imaging of neuropilin receptor type-1 expression with 131I-labeled monoclonal antibody. Int. J. Oncol. 2016, 49, 961–970. [Google Scholar] [CrossRef] [PubMed]
- Bumbaca, D.; Xiang, H.; Boswell, C.A.; Port, R.E.; Stainton, S.L.; Mundo, E.E.; Ulufatu, S.; Bagri, A.; Theil, F.P.; Fielder, P.J.; et al. Maximizing tumour exposure to anti-neuropilin-1 antibody requires saturation of non-tumour tissue antigenic sinks in mice. Br. J. Pharmacol. 2012, 166, 368–377. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov Identifier: NCT01859234. Available online: clinicaltrials.gov/ct2/show/NCT01859234 (accessed on 22 October 2020).
- ClinicalTrials.gov Identifier: NCT01894451. Available online: clinicaltrials.gov/ct2/show/NCT01894451 (accessed on 22 October 2020).
- Ferrara, N.; Kerbel, R.S. Angiogenesis as a therapeutic target. Nature 2005, 438, 967–974. [Google Scholar] [CrossRef]
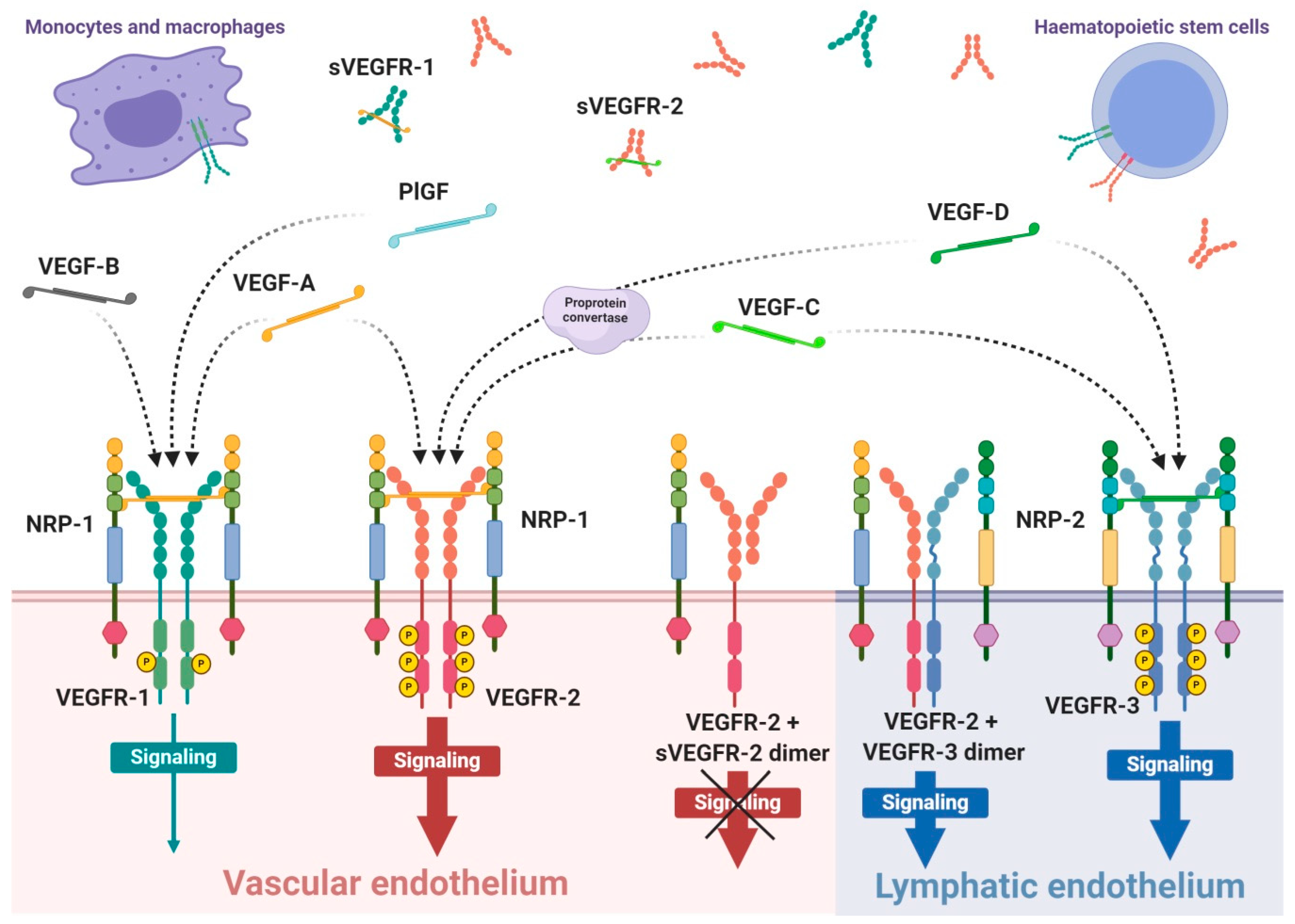
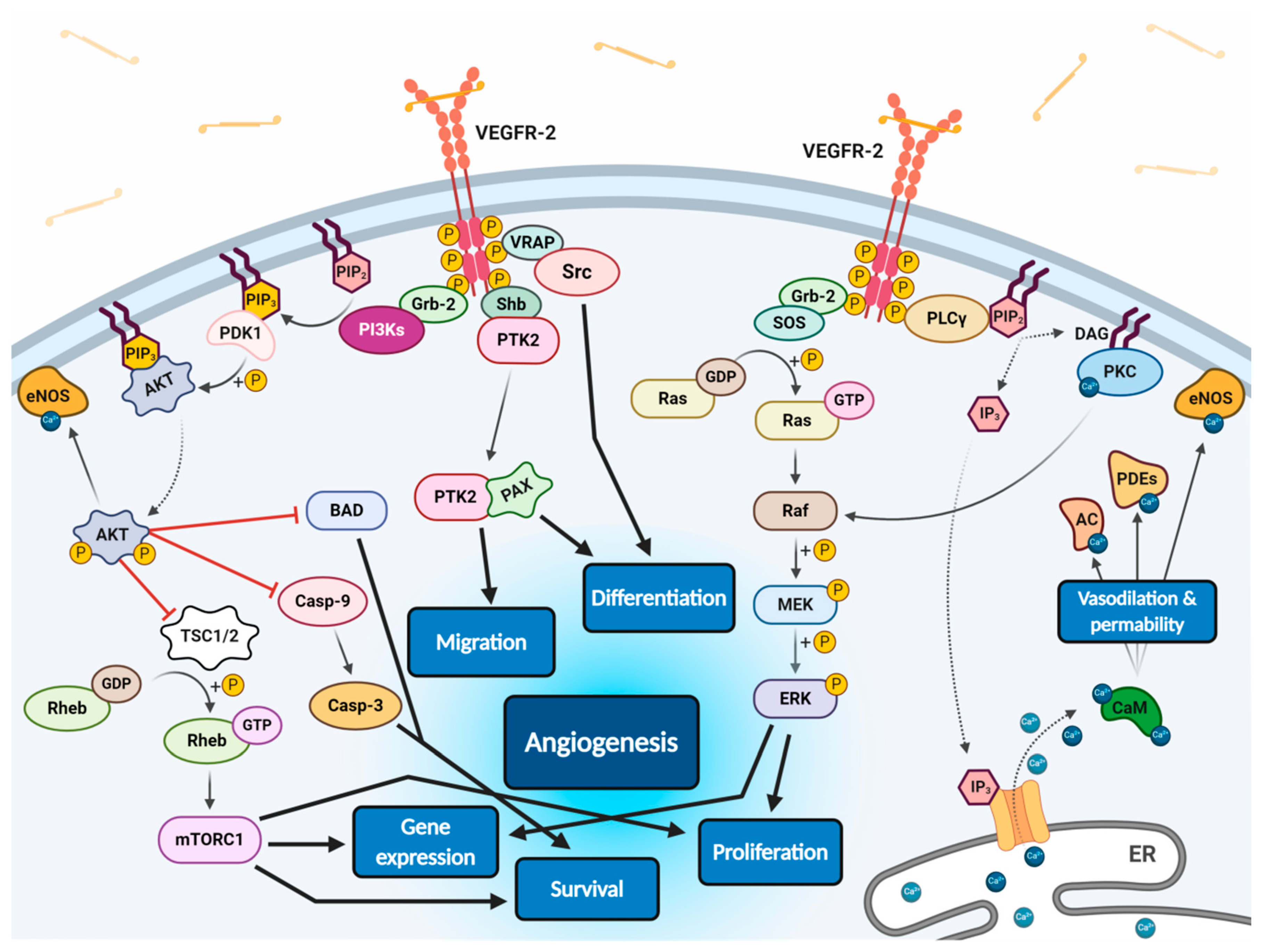
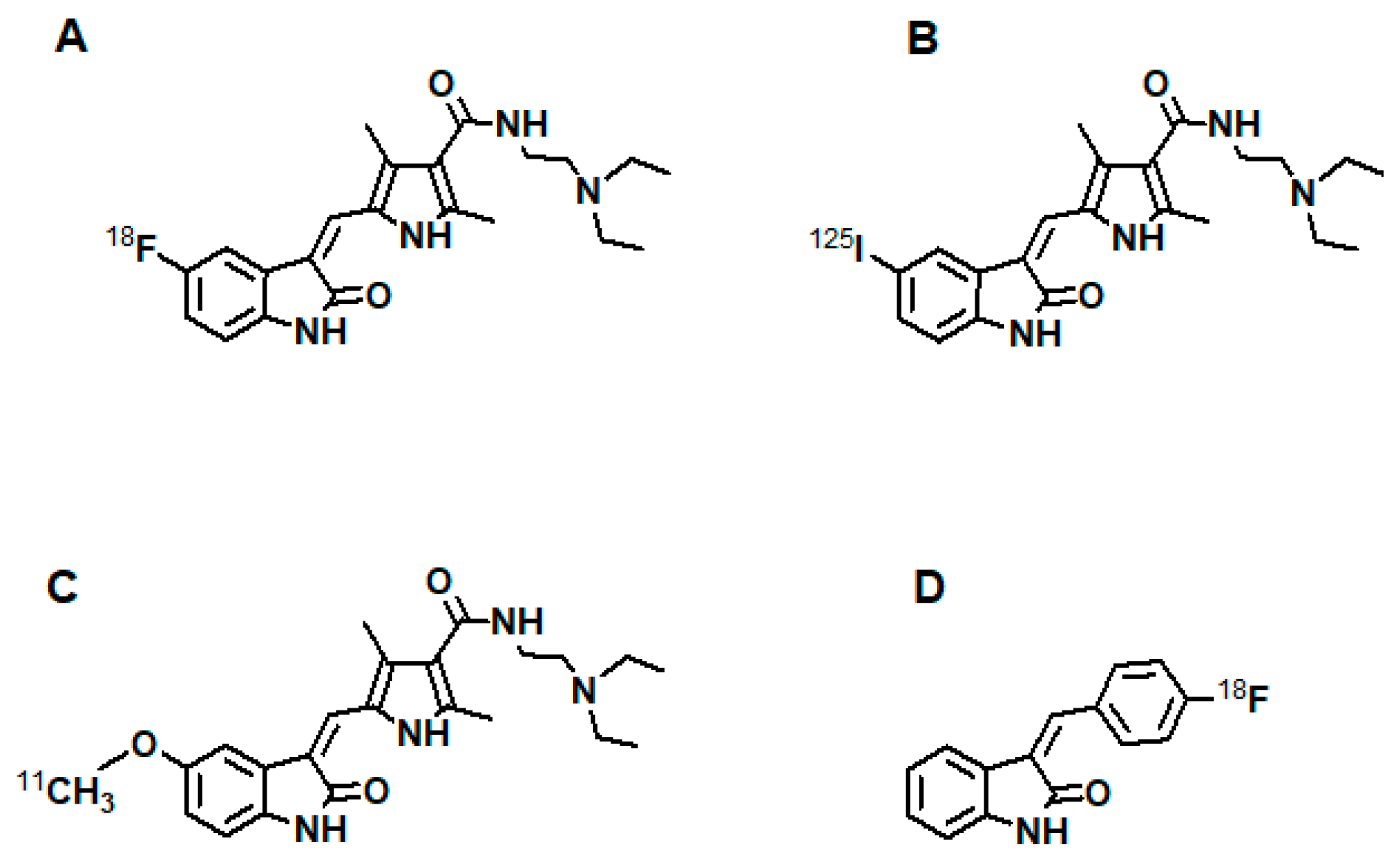
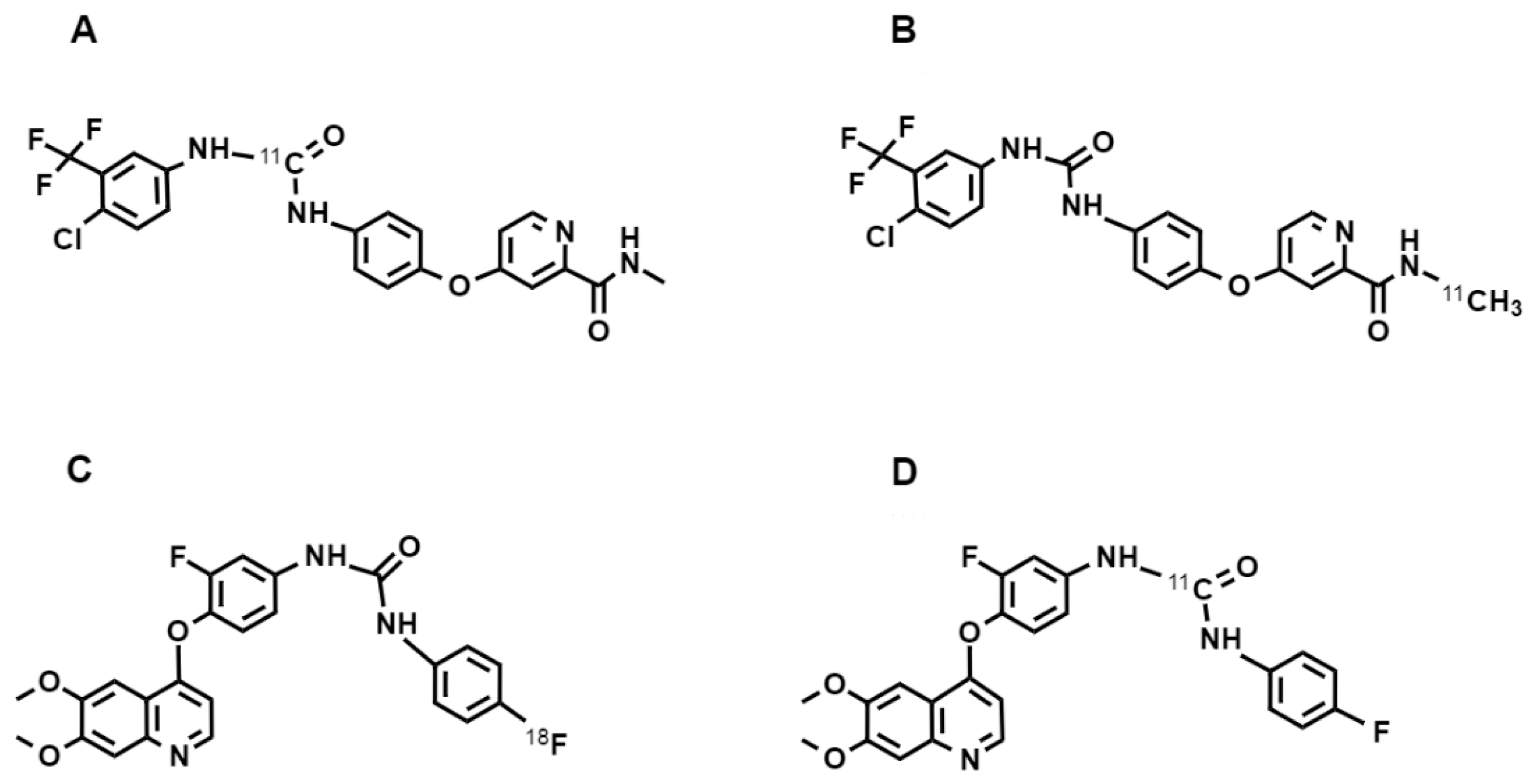
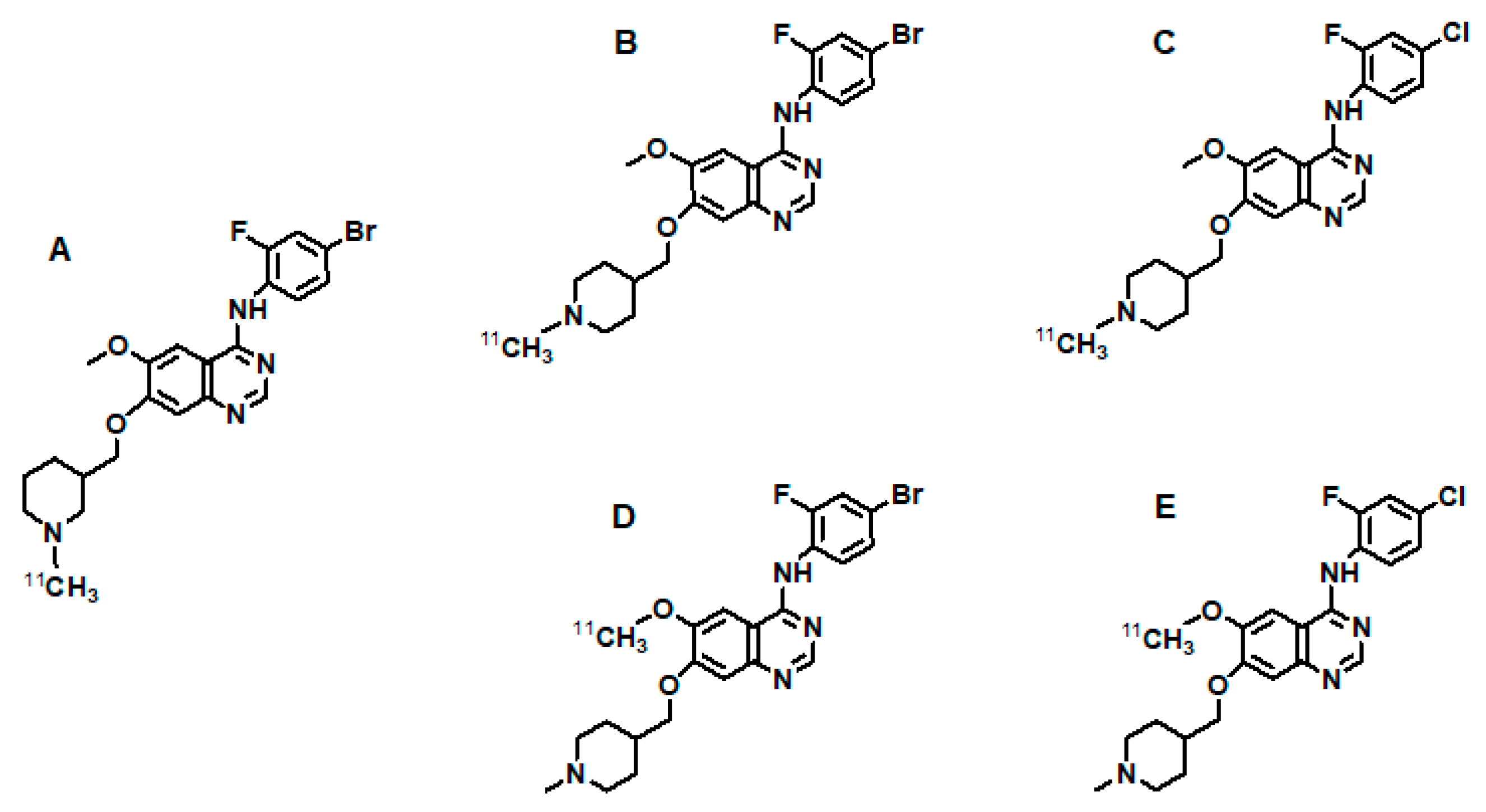
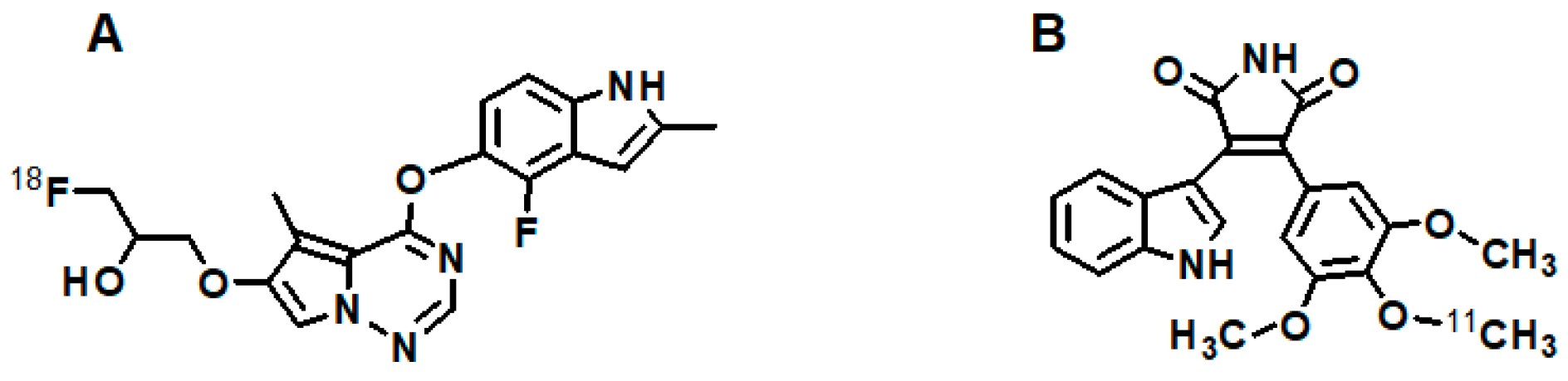
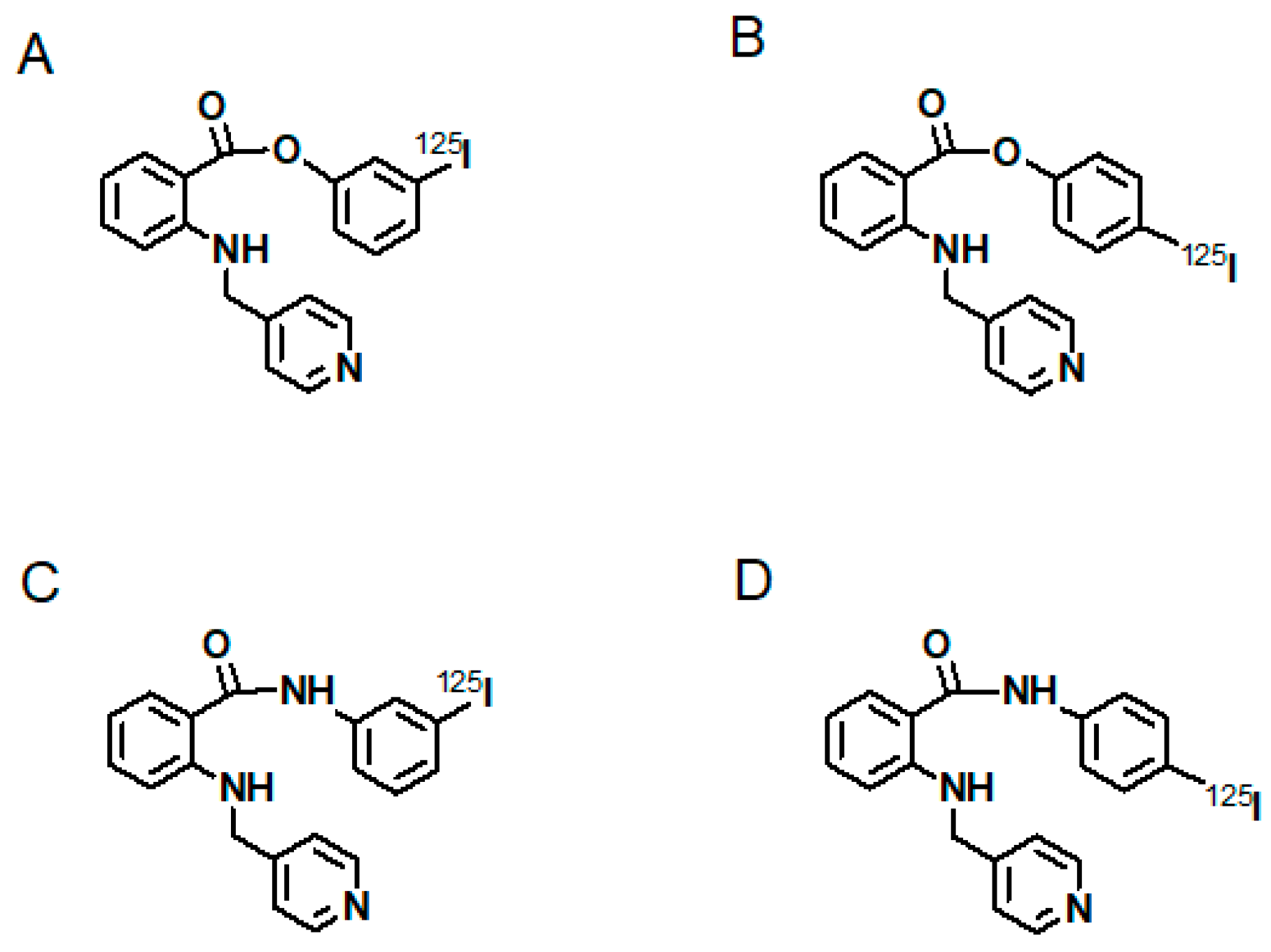
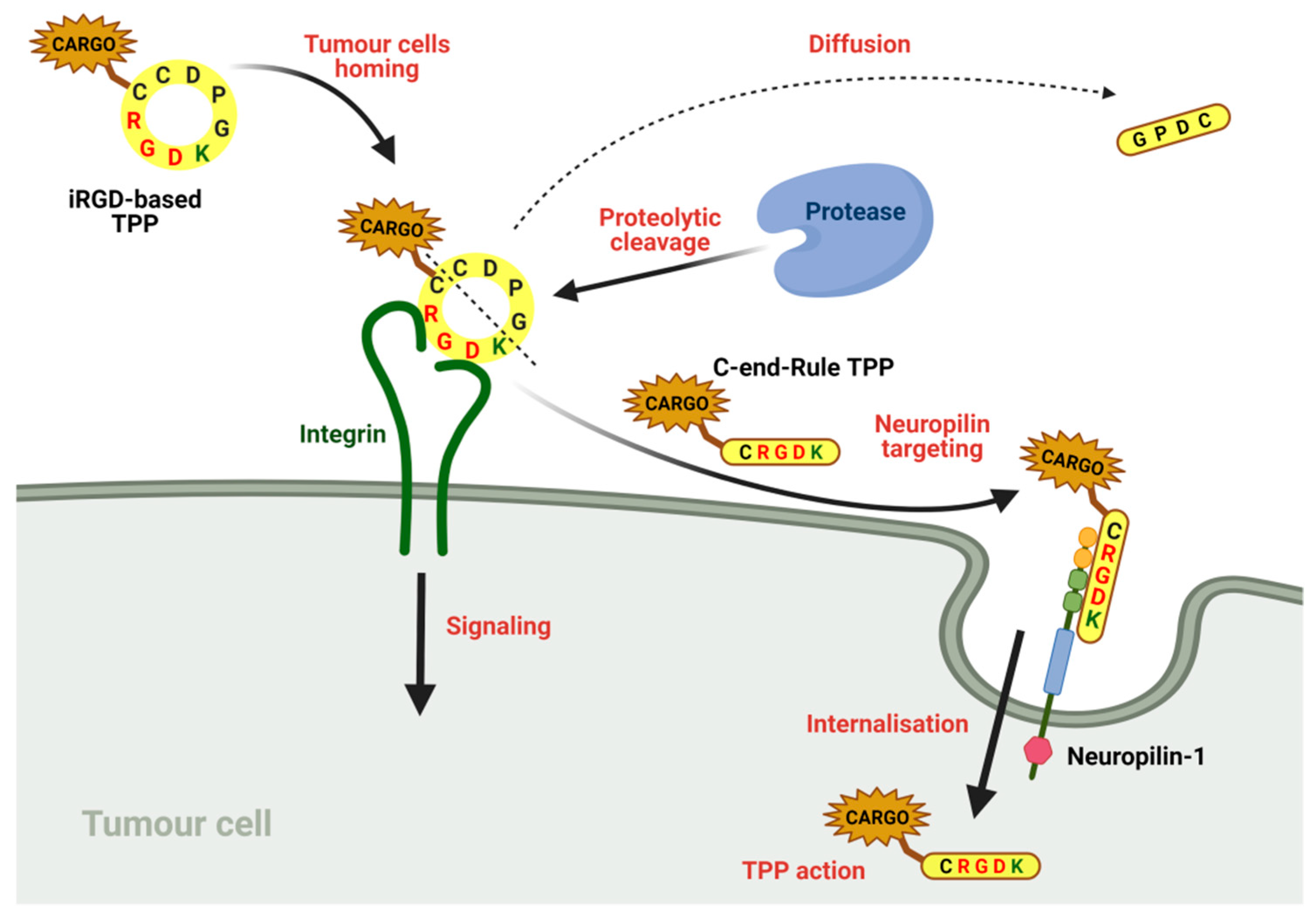
| Radiocompound | Aim of Study | References |
|---|---|---|
| [125I]I-VEGF | identification and characterisation of VEGFR | [144] |
| [125I]I-VEGF-A121 | investigation of the heparin effect on binding of VEGF-A121/165 to VEGFRs; study of the induction of VEGFR-2 tyrosine autophosphorylation by VEGF-A | [146,149] |
| [125I]I-VEGF-A165 | investigation of the heparin effect on VEGF-A121/165 binding to VEGFRs; localisation of VEGFR and quantification of VEGF binding in human kidney; study of VEGF binding to neuropilin-1; study of renal expression of VEGF and VEGFR-2 in experimental diabetes; study on induction of VEGFR-2 tyrosine autophosphorylation by VEGF-A; identification of VEGFR binding sites for VEGF-A165 | [91,145,146,147,148,149] |
| [111In]In-DTPA-VEGF-A121 | detection of ischemia related with VEGFRs | [157] |
| [64Cu]Cu-DOTA-VEGF-A121 | examination of VEGFR expression on different sized human glioblastoma U87MG tumours, in rats myocardial infractions, post-stroke angiogenesis and ischemia; development of VEGFR-2-specific tracer with low renal toxicity | [132,133,150,151,152,153] |
| [64Cu]Cu-DOTA-VEGFmutant | ||
| [64Cu]Cu-DOTA-VEGFDEE | ||
| [68Ga]Ga-NOTA-VEGF-A121 | examination of VEGFR overexpression in U87MG tumour xenograft models | [154,155] |
| [68Ga]Ga-NODAGA-VEGF-A121 | ||
| [123I]I/[125I]I-VEGF-A121 | examination of VEGFR overexpression on various types of human and cancer cells; examination of angiogenesis in LS180 tumour xenograft model | [141,156] |
| [123I]I/[125I]I-VEGF-A165 | ||
| [99mTc]Tc-HuS/Hu-VEGF | examination of VEGFR-2 overexpression in subcutaneous and pulmonary adenocarcinoma tumours | [169] |
| [99mTc]Tc-HYNIC-C-tagged-VEGF | imaging of tumour vasculature during cyclophosphamide treatment | [159] |
| [99mTc]Tc-HYNIC-scVEGF | multimodal imaging of VEGFRs; description of site-specific protein modification and labelling; identification of accelerated atherosclerosis in diabetes via VEGFRs imaging | [134,142,160] |
| [64Cu]Cu-DOTA-PEG-scVEGF | ||
| [99mTc]Tc-scVEGF-PEG-DOTA | ||
| [64Cu]Cu-DOTA-QD-VEGF | dual-modality optical and PET imaging of VEGFR overexpression on U87MG tumour model | [170,171] |
| [64Cu]Cu-DOTA-(AF)-SAv/biotin-PEG-VEGF-A121 | ||
| [99mTc]Tc-scVEGF | usefulness of direct labelled VEGF-radiocompound; imaging of VEGFR expression changes in breast cancer xenografts under sunitinib treatment and HT29 xenografts during pazopanib treatment | [139,161,162,163] |
| [68Ga]Ga-HBED-CC-PEG-scVEGF | imaging of VEGFRs in different human xenografts in mice | [164,165] |
| [68Ga]Ga-NOTA/DOTA-PEG-scVEGF | ||
| [18F]FBEM-scVEGF | VEGFRs imaging on mouse models with xenografts of various tumour cell lines | [140] |
| [89Zr]Zr-DFO-PEG-scVR1 | independent imaging of VEGFR-1 and VEGFR-2 on breast cancer on 4T1luc mice model | [166] |
| [89Zr]Zr-DFO-PEG-scVR2 | ||
| [99mTc]Tc-scVR1-PEG-DOTA | selective imaging of VEGFR-1 and VEGFR-2 in atherosclerotic lesions on diabetic and non-diabetic mice | [167] |
| [99mTc]Tc-scVR2-PEG-DOTA | ||
| [61Cu]Cu-NOTA-K3-VEGF-A121 | PET/CT imaging of VEGFR expression on 4T1 tumour-bearing mice | [168] |
| [177Lu]Lu-DOTA-PEG-scVEGF | synthesis and study of therapeutic radiocompound for targeted systemic radiotherapy on MDA231luc tumour-bearing mice; investigation on effectiveness of combinational therapy with doxorubicin | [136,137] |
| [64Cu]Cu-DOTA-VEGF-A121/rGel | determination of anti-angiogenic and anti-tumour effects of a vasculature-targeting fusion toxin on orthotopic glioblastoma mice model by multimodal imaging | [172] |
| [123I]I/[125I]I-VEGF-A165 | examination of tumour localisation in patients with gastrointestinal tumours; evaluation of tumour therapy efficiency on athymic mice models; imaging of highly malignant VEGFR-positive osteosarcoma; investigation of prognostic value of imaging in patients with histologically verified brain tumours | [143,177,178,179,180] |
| [99mTc]Tc-HYNIC-VEGF-A165 | evaluation of VEGFR overexpressions on various xenograft tumours in mice | [181] |
| [111In]In-hnTf-VEGF-A165 | imaging of athymic mice bearing U87MG human glioblastoma xenografts by new human-transferin recombinant protein | [182] |
| [99mTc]Tc/[111In]In-DTPA-VEGF-2K | synthesis of new recombinant proteins and comparison their cytotoxicity on overexpressing VEGFR-1 PAE cells | [183] |
| [99mTc]Tc/[111In]In-DTPA-VEGF-2K-NLS | ||
| [188Re]Re-MAG3-QKRKRKKSRYKS | evaluation of in vivo distribution and tumour imaging in two groups of human ovarian tumour-bearing mice | [184] |
| [99mTc]Tc-HYNIC-QKRKRKKSRKKH | synthesis and study of novel small peptides as potential drugs for radioactive diagnosis and therapy in A549 tumour-bearing mice | [138] |
| [99mTc]Tc-HYNIC-RKRKRKKSRYIVLS | ||
| [188Re]Re-EC-QKRKRKKSRKKH | ||
| [188Re]Re-EC-RKRKRKKSRYIVLS |
| Radiocompound | Aim of Study | References |
|---|---|---|
| [124I]I-HuMV833 | antibody distribution study in patients treated with HuMV833 | [188] |
| [125I]I-VG76e | VEGFs level imaging in human fibrosarcoma; patient classification for AAT | [193] |
| [125I]SIB-VG76e | ||
| [125I]I-SHPP-VG76e | ||
| [124I]I-SHPP-VG76e | ||
| [99mTc]Tc-VG76e | detection and inhibition of human breast adenocarcinoma | [194] |
| [153Sm]Sm-DTPA-VG76e | ||
| [177Lu]Lu-DTPA-VG76e | ||
| [177Lu]Lu-DOTA-VG76e | synthesis and evaluation of novel potential therapeutic anti-angiogenic radioagents | [195] |
| [177Lu]Lu-DTPA-VG76e | ||
| [125I]MBs-I-Bt-Avas12a1 | studies of biological aspects of angiogenesis | [196] |
| [18F]MBs-SFB-Avas12a1 | VEGFR overexpression and tumour angiogenesis imaging | [197] |
| [99mTc]Tc-HYNIC-chtiosan-Cy5.5-DC101 | ischemia monitoring of umbilical vein endothelial cells studied on mice with surgically induced ischemia | [198] |
| [64Cu]Cu-NOTA-BV | imaging of VEGF overexpressing renal carcinoma; monitoring of tumour response to cancer everolimus treatment | [200] |
| [111In]In-DTPA-BV | assessment of new radiotracers‘ application as markers for non-invasive VEGF imaging in tumour microenvironment | [205] |
| [89Zr]Zr-N-suc-Df-BV | ||
| [111In]In-DTPA-BV | research on correlation between radiotracer tumour uptake and level of VEGF-A expression, studied on colon cancer metastases to liver and melanoma lesions treated with BV | [206,207] |
| [111In]In-DTPA-BV | visualisation of VEGF-A for prediction of chemotherapy response and patient classification for anti-VEGF AAT | [208] |
| [125I]I-BV | ||
| [111In]In-DTPA-BV | imaging of different VEGF isoforms expression | [209] |
| study of radiotracer tumour uptake during sorafenib treatment regading to VEGF expression | [199] | |
| [111In]In-CHX-A″-DTPA-BV | scintigraphic imaging of VEGF expression; patient stratification for anti-VEGF AAT | [210] |
| [86Y]Y-CHX-A″-DTPA-BV | application for non-invasive assessment of VEGF-A tumour angiogenesis status; possibility of application as a marker in radioimmunotherapy conducted with the use of therapeutic radioconjugate [90Y]Y-CHX-A″-DTPA-BV | [211] |
| [177Lu]Lu-CHX-A″-DTPA-BV | application as therapeutic agent for anti-VEGF AAT | [213] |
| [111In]In-DTPA-BV | VEGF expression imaging and radiotracer application for assessment of response to rapamycin renal and breast cancer treatment | [214] |
| [111In]In-DTPA-Bt-BV | application of avidin chase strategy for [90Y]Y-DTPA-Bt-BV therapy | [215] |
| [90Y]Y-DTPA-Bt-BV | ||
| [89Zr]Zr-N-suc-Df-BV | in vivo non-invasive visualisation of early changes in VEGF levels during treatment with synthetic inhibitor NVPAUY922 | [216] |
| application as an early biomarker of everolimus AAT | [217,218,219] | |
| VEGF expression imaging in primary breast cancer and non-small cell lung cancer; study on correlation between radiotracer uptake and of VEGF-A level | [220,221] | |
| VEGF-A expression imaging before and during AAT with BV/IFNα and sunitinib | [222,223,224] | |
| [99mTc]Tc-HYNIC-BV | scintigraphic imaging of VEGF levels in tumour | [225,226,227] |
| [99mTc]Tc(CO)3-BV | ||
| [99mTc]Tc-DTPA-BV | evaluation of VEGF binding and application in radioimmunoscintigraphy of various cancers | [228] |
| [89Zr]Zr-N-suc-Df-BV/cetuximab-800CW | early photo- and radio-detection of small, established tumours which cannot be identified by current radiological and nuclear techniques | [229,230] |
| [89Zr]Zr-N-suc-Df-BV/cetuximab | ||
| [89Zr]Zr-N-suc-Df-BV | study on VEGFR expression in adult and childhood HGG, including DIPG tumours; identification of heterogeneity of pontine glioma lesions smaller than a centimeter; stratification patients for BV treatment | [231,232,233] |
| [131I]I-BV | tumour-targeting evaluation for cancer imaging and treatment | [234] |
| targeting VEGF overexpressing cancers therapy; evaluation of application as potential diagnostic and radioimmunotherapeutic agent | [235] | |
| [124I]I-Ran | application in age-related macular degeneration treatment | [236,237,238] |
| [124I]I-BV | ||
| [64Cu]Cu-DOTA-BV | study on correlation between VEGF expression and tumour uptake of radiotracer; evaluation of possibility for patient stratification for AAT | [239] |
| [64Cu]Cu-NOTA-BV-800CW | VEGF imaging in human glioblastoma; application in disease diagnosis, patient stratification and treatment monitoring | [240] |
| [64Cu]Cu-NOTA-RamAb | VEGFR-2 binding studies of radiopreparation | [243] |
| [89Zr]Zr-N-suc-Df-Ram | radiotracer application for AAT monitoring and patient stratification for AAT | [245] |
| [99mTc]Tc-Ram | evaluation of affinity to VEGFR-2 receptor | [246] |
| [99mTc]Tc-HYNIC-Ram | ||
| [99mTc]Tc-DTPA-Ram | ||
| [89Zr]Zr-N-suc-Df-Ran | non-invasive dynamic visualisation and quantification of VEGF signaling; radiotracer application for AAT monitoring | [247] |
| Radiocompound | Aim of Study | References |
|---|---|---|
| [124I]I-aflibercept | examination of pharmacokinetic properties of intravitreally applied [124I]I-aflibercept in the vitreous cavity | [238] |
| [64Cu]Cu-DOTA-GU40C4 | evaluation of diagnostic and therapeutic abilities on VEGFR-2 positive prostate cancer | [249,250] |
| [131I]I-Tyr-RRL | angiogenesis imaging in tumour AAT | [44] |
| [99mTc]Tc-peptide1 | application of retro-inverso peptidomimetic derivatives for synthesis of radiotracers with high affinity towards VEGFR-1 and NRP-1 | [251,252] |
| [99mTc]Tc-peptide2 | ||
| ([99mTc]Tc-HYNIC-retro-inverso peptidomimetic) |
| Radiocompound | Aim of Study | References |
|---|---|---|
| [125I]5-I-sunitinib | imaging of VEGFR expressing tumours and angiogenic processes | [254] |
| [18F]5-F-sunitinib | RTKs in vivo imaging | [255] |
| [99mTc]Tc-sunitinib | potential radiopharmaceutical for tumour hypoxia imaging | [259] |
| [methoxy-11C]5-methoxy-sunitinib | RTKs in vivo imaging and evaluation of AAT efficiency | [256,257] |
| [18F]3-[4′-fluorobenzylidene]indolin-2-one | RTKs in vivo imaging | [258] |
| [18F]sorafenib | imaging of increased expression of VEGFRs | [260] |
| [124I]I-sorafenib | ||
| [carbamate-11C]-sorafenib | VEGFR expressing tumours in vivo imaging | [261,262] |
| [carbamate-11C]-sorafenib | ||
| [N-methyl-11C]-sorafenib | ||
| [18F]F-diaryl urea | VEGFR-positive tumours in vivo imaging in AAT | [263] |
| [carbamate-11C]-diaryl urea | [264] | |
| [N-methyl-11C]-PAQ | imaging of VEGFR-2 expression fluctuations and angiogenesis | [43] |
| [N-methyl-11C]vandetanib | VEGFR imaging and monitoring of effectiveness of vandetanib orchloro-vandetanib therapy | [266] |
| [N-methyl-11C]chloro-vandetanib [O-methyl-11C]vandetanib | ||
| [O-methyl-11C]chloro-vandetanib | ||
| [18F]F-brivanib | VEGFR in vivo imaging and angiogenic processes visualisation | [267] |
| [methoxy-11C-](trimethoxy-phenyl)-indolyl-maleimide | VEGFR in vivo imaging and visualisation of angiogenic processes | [268] |
| [125I]m-I-NPAE | VEGFR in vivo imaging in AAT | [269] |
| [125I]p-I-NPAE | ||
| [125I]m-I-NPAM | ||
| [125I]p-I-NPAM | ||
| [111In]In-NODAGA-ZVEGFR2-Bp2 | VEGFR-2 expression imaging and visualisation of tumour angiogenesis in GBM | [270] |
| Radiocompound | Aim of Study | References |
|---|---|---|
| [99mTc]Tc-MA-A7R | determination of peptide binding to NRP-1 and NRP-2 | [278] |
| [99mTc]Tc-HYNIC-A7R | imaging of NRP-1 positive tumours | [279] |
| [18F]F-Al-NOTA-RGD-A7R | investigation of diagnostic ability on dual αvβ3 and NRP-1 positive glioblastoma tumours | [280,281,282,283] |
| [18F]F-Al-NOTA-A7R | ||
| [18F]-benzoate-RGD-A7R | ||
| [18F]F-n-BSA-RGD-A7R | ||
| [68Ga]Ga-DOTAGA-Ahx-iRGD | investigation of diagnostic ability on dual αvβ3 and NRP-1 positive tumours | [287,288] |
| [68Ga]Ga-NODAGA-Ahx-iRGD | ||
| 68Ga labelled iRGD | ||
| [68Ga]Ga-NOTA/DOTA-NGR [68Ga]Ga-NOTA/DOTA-iNGR | comparison of diagnostic abilities on CD13-positive tumour xenografts | [285,289] |
| 99mTc and RPAR derivative complex | investigation of diagnostic ability on different NRP-1 positive tumours | [290] |
| [131I]I-Tyr-tLyp-1 | [291] | |
| 99mTc labelled CK3 | [293] | |
| [124I]I-Tyr-LinTT1-PS | investigation of diagnostic ability of polymersomes conjugated with LinTT1 peptide on triple negative breast cancer | [292] |
| [131I]I-A6-11-26 | investigation of delivery ability on NRP-1 positive tumours | [297] |
| [111In]In-DOTA-MNRP1685A | [298] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Masłowska, K.; Halik, P.K.; Tymecka, D.; Misicka, A.; Gniazdowska, E. The Role of VEGF Receptors as Molecular Target in Nuclear Medicine for Cancer Diagnosis and Combination Therapy. Cancers 2021, 13, 1072. https://doi.org/10.3390/cancers13051072
Masłowska K, Halik PK, Tymecka D, Misicka A, Gniazdowska E. The Role of VEGF Receptors as Molecular Target in Nuclear Medicine for Cancer Diagnosis and Combination Therapy. Cancers. 2021; 13(5):1072. https://doi.org/10.3390/cancers13051072
Chicago/Turabian StyleMasłowska, Katarzyna, Paweł Krzysztof Halik, Dagmara Tymecka, Aleksandra Misicka, and Ewa Gniazdowska. 2021. "The Role of VEGF Receptors as Molecular Target in Nuclear Medicine for Cancer Diagnosis and Combination Therapy" Cancers 13, no. 5: 1072. https://doi.org/10.3390/cancers13051072
APA StyleMasłowska, K., Halik, P. K., Tymecka, D., Misicka, A., & Gniazdowska, E. (2021). The Role of VEGF Receptors as Molecular Target in Nuclear Medicine for Cancer Diagnosis and Combination Therapy. Cancers, 13(5), 1072. https://doi.org/10.3390/cancers13051072







