Mouse Preclinical Cancer Immunotherapy Modeling Involving Anti-PD-1 Therapies Reveals the Need to Use Mouse Reagents to Mirror Clinical Paradigms
Abstract
Simple Summary
Abstract
1. Introduction
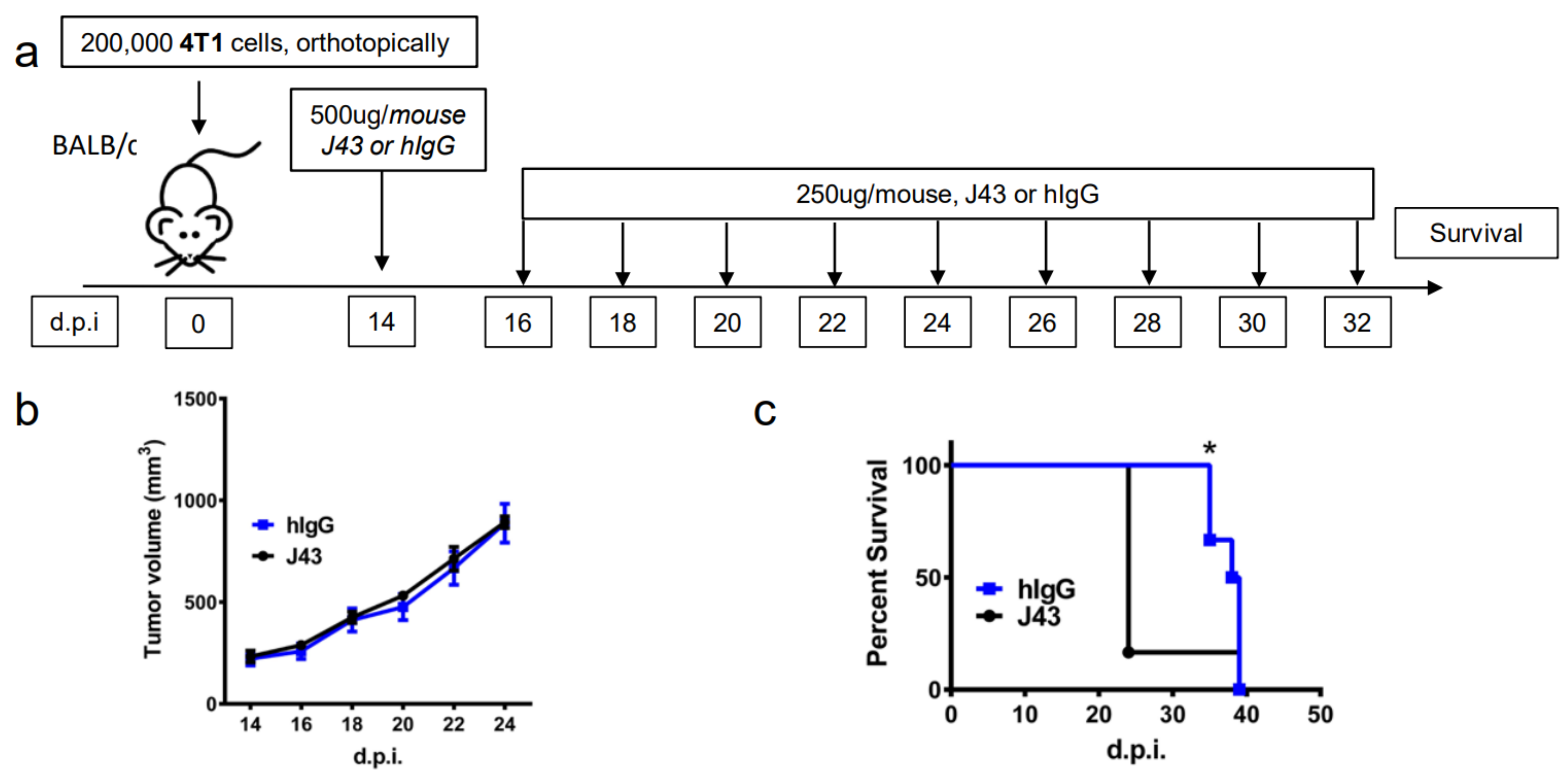
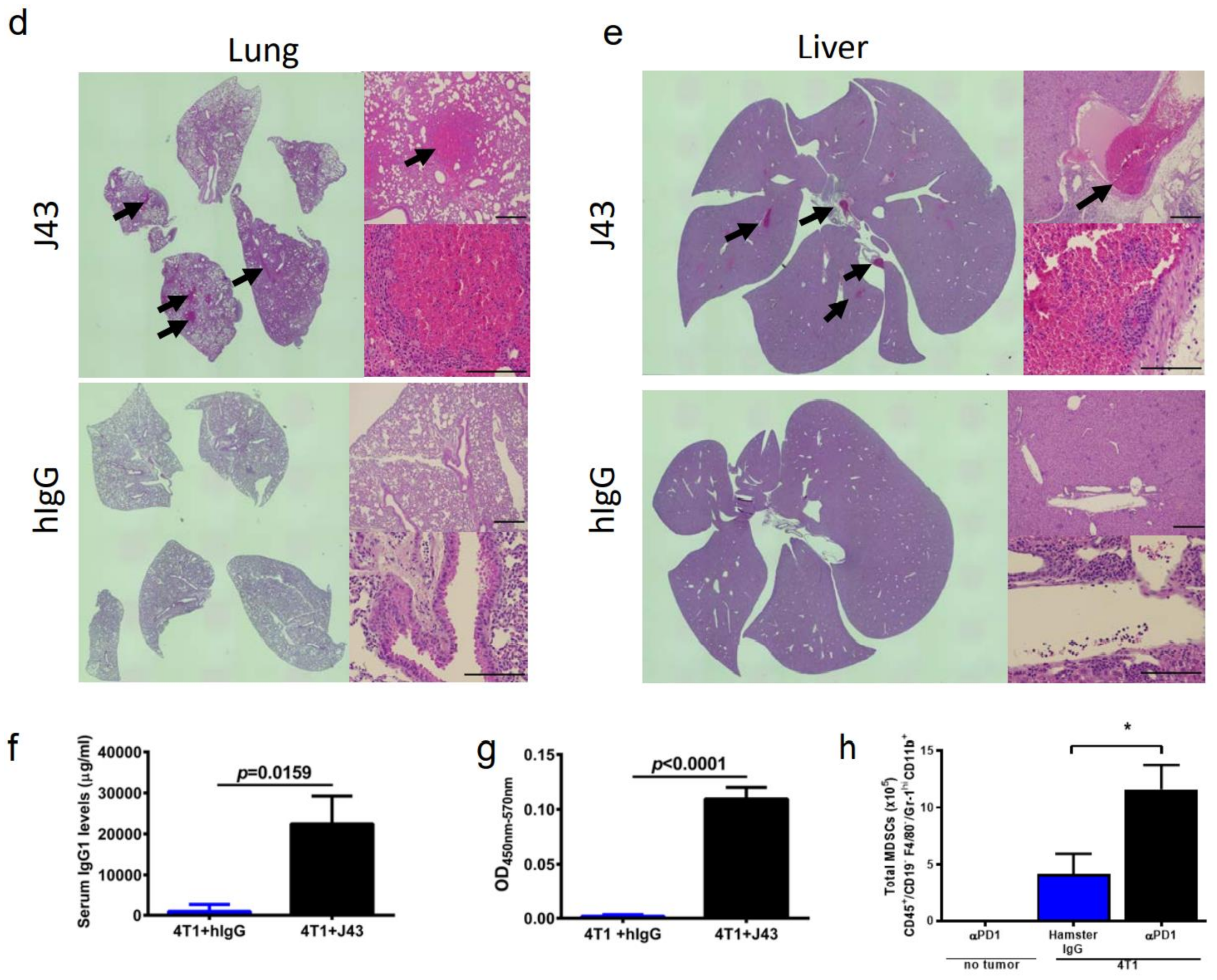
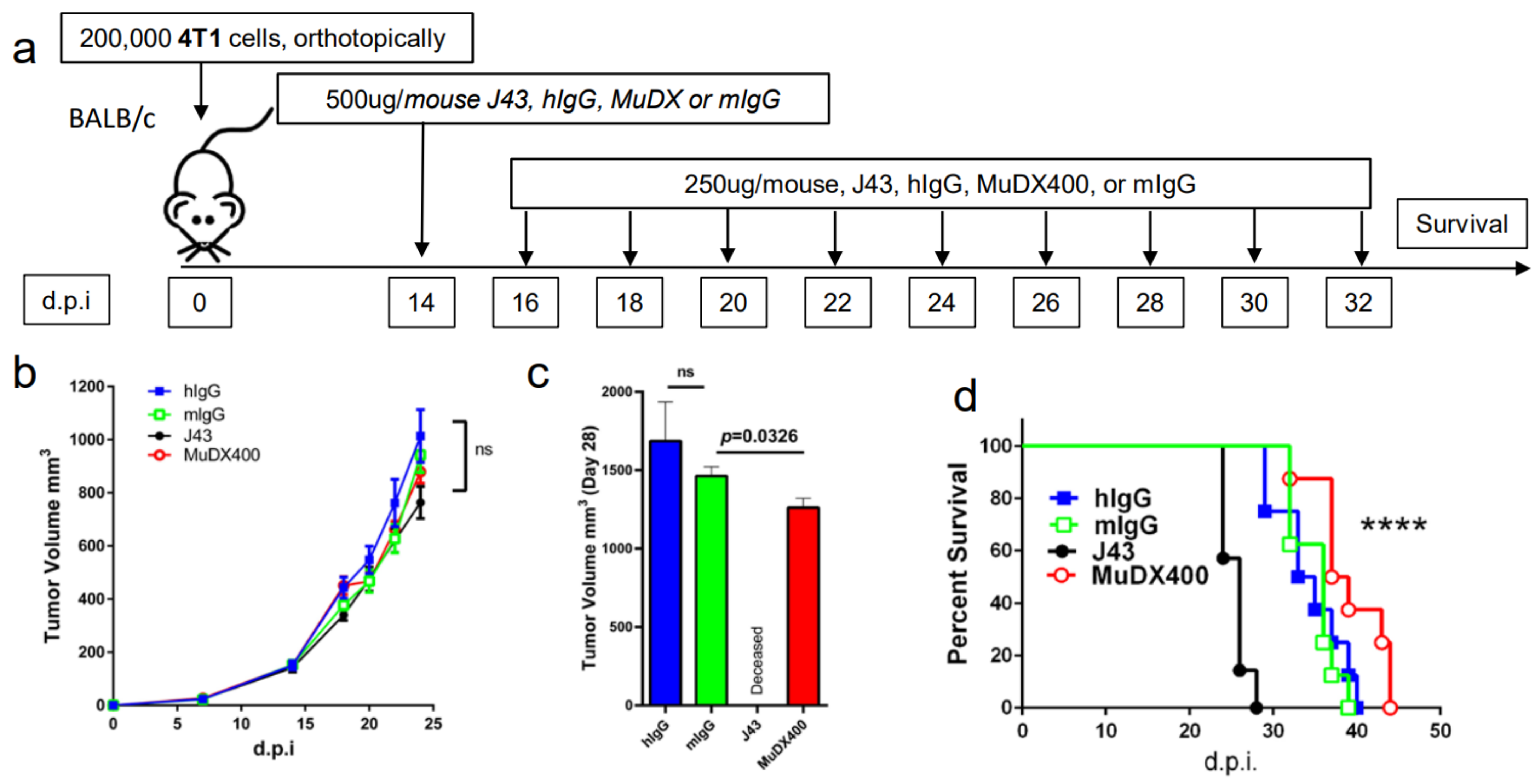
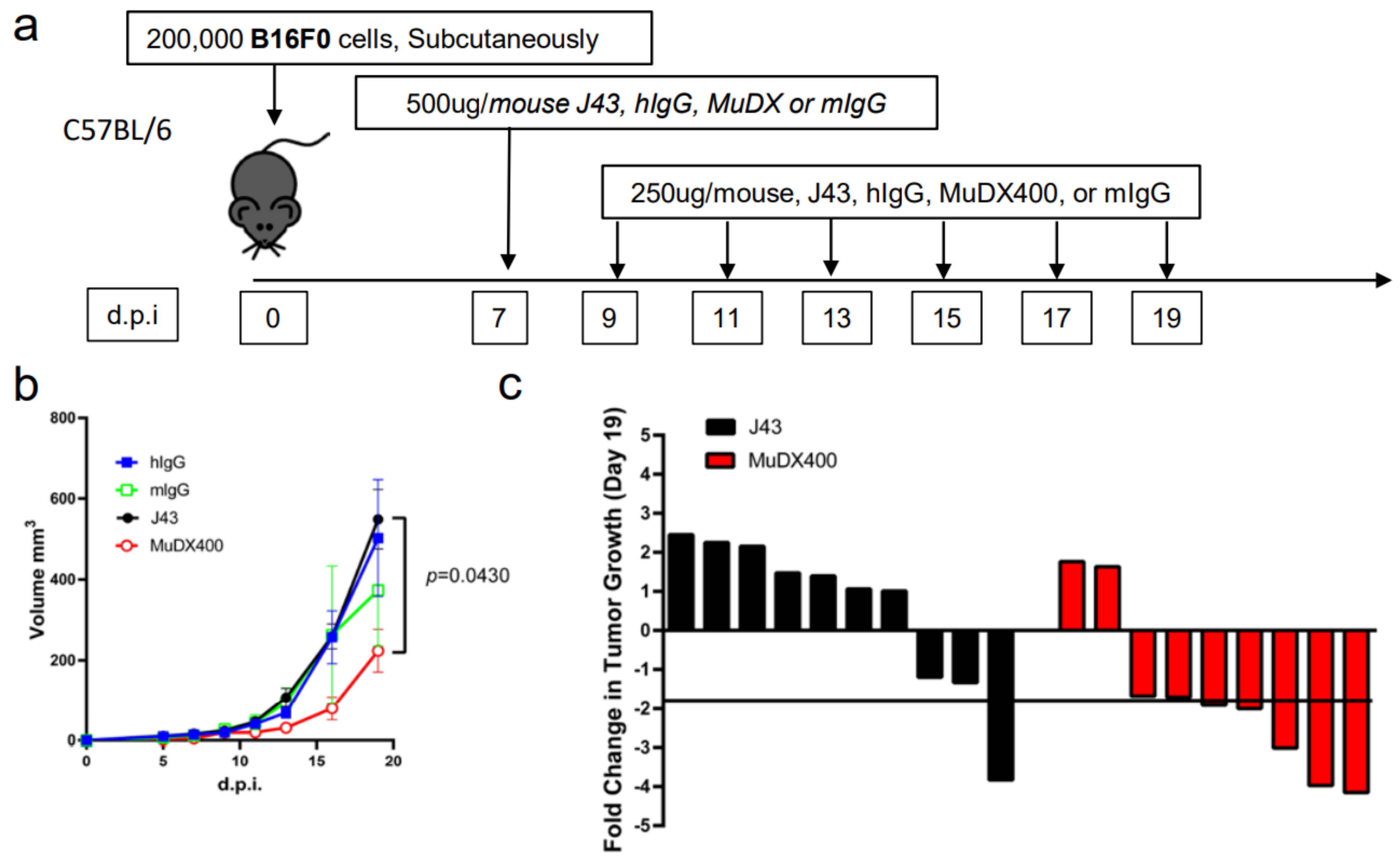
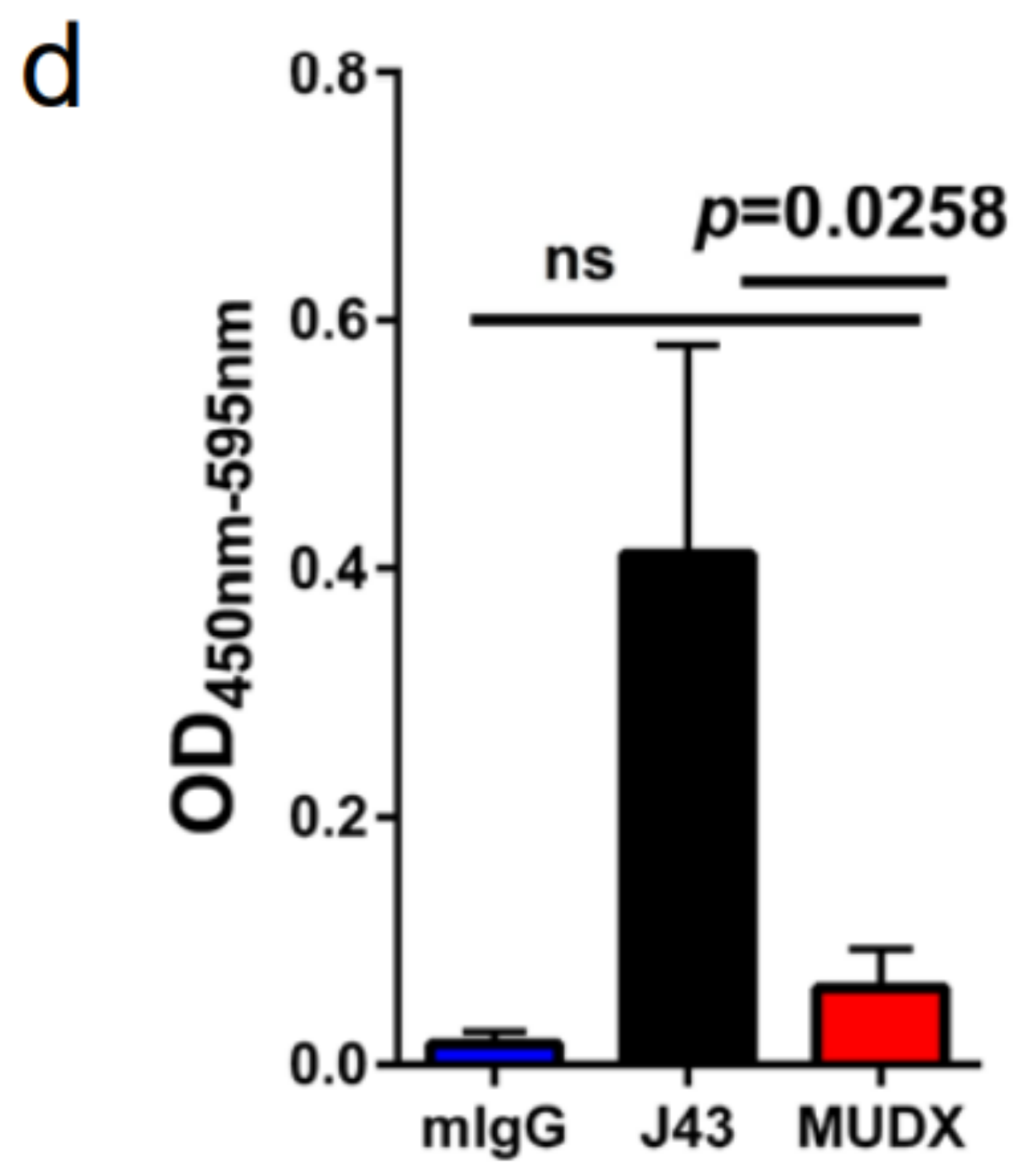
2. Results
3. Discussion
4. Materials and Methods
4.1. Mice
4.2. Tumor Cell Line and Treatment
4.3. Mouse Lung Whole-Mount Preparation
4.4. H&E Staining
4.5. ELISA
4.6. Statistics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sanmamed, F.M.; Chen, A.L. Paradigm shift in cancer immunotherapy: From enhancement to normalization. Cell 2018, 175, 313–326. [Google Scholar] [CrossRef]
- Sharpe, A.H.; Wherry, E.J.; Ahmed, R.; Freeman, G.J. The function of programmed cell death 1 and its ligands in regulating autoimmunity and infection. Nat. Immunol. 2007, 8, 239. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, H.S.; Freeman, J.G.; Dranoff, G.; Sharpe, H.A. Coinhibitory pathways in immunotherapy for cancer. Annu. Rev. Immunol. 2016, 34, 539–573. [Google Scholar] [CrossRef] [PubMed]
- Chen, L. Co-inhibitory molecules of the B7–CD28 family in the control of T-cell immunity. Nat. Rev. Immunol. 2004, 4, 336. [Google Scholar] [CrossRef] [PubMed]
- Greenwald, R.J.; Freeman, G.J.; Sharpe, A.H. The B7 family revisited. Annu Rev. Immunol. 2005, 23, 515–548. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, T.; Honjo, T. The PD-1–PD-L pathway in immunological tolerance. Trends Immunol. 2006, 27, 195–201. [Google Scholar] [CrossRef]
- Nakae, S.; Suto, H.; Iikura, M.; Kakurai, M.; Sedgwick, J.D.; Tsai, M.; Galli, S.J. Mast cells enhance T cell activation: Importance of mast cell costimulatory molecules and secreted TNF. J. Immunol. 2006, 176, 2238–2248. [Google Scholar] [CrossRef]
- Latchman, Y.; Wood, C.R.; Chernova, T.; Chaudhary, D.; Borde, M.; Chernova, I.; Freeman, G. J PD-L2 is a second ligand for PD-1 and inhibits T cell activation. Nat. Immunol. 2001, 2, 261. [Google Scholar] [CrossRef]
- Brown, J.A.; Dorfman, D.M.; Ma, F.R.; Sullivan, E.L.; Munoz, O.; Wood, C.R.; Freeman, G.J. Blockade of programmed death-1 ligands on dendritic cells enhances T cell activation and cytokine production. J. Immunol. 2003, 170, 1257–1266. [Google Scholar] [CrossRef]
- LaFleur, M.W.; Muroyama, Y.; Drake, C.G.; Sharpe, A.H. Inhibitors of the PD-1 pathway in tumor therapy. J. Immunol. 2018, 200, 375–383. [Google Scholar] [CrossRef]
- Twyman-Saint Victor, C.; Rech, A.J.; Maity, A.; Rengan, R.; Pauken, K.E.; Stelekati, E.; Minn, A.J. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature 2015, 520, 373. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.; Schachter, J.; Long, G.V.; Arance, A.; Grob, J.J.; Mortier, L.; Ribas, A. Pembrolizumab versus ipilimumab in advanced melanoma. N. Engl. J. Med. 2015, 372, 2521–2532. [Google Scholar] [CrossRef]
- Garon, E.B.; Rizvi, N.A.; Hui, R.; Leighl, N.; Balmanoukian, A.S.; Eder, J.P.; Gandhi, L. Pembrolizumab for the treatment of non–small-cell lung cancer. N. Engl. J. Med. 2015, 372, 2018–2028. [Google Scholar] [CrossRef] [PubMed]
- Powles, T.; Fine, G.D.; Braiteh, F.S.; Loriot, Y.; Cruz, C.; Vogelzang, N.J. MPDL3280A (anti-PD-L1) treatment leads to clinical activity in metastatic bladder cancer. Nature 2014, 515, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Rangarajan, A.; Weinberg, R.A. Comparative biology of mouse versus human cells: Modelling human cancer in mice. Nat. Rev. Cancer 2003, 3, 952. [Google Scholar] [CrossRef] [PubMed]
- Masopust, D.; Sivula, C.P.; Jameson, S.C. Of mice, dirty mice, and men: Using mice to understand human immunology. J. Immunol. 2017, 199, 383–388. [Google Scholar] [CrossRef]
- Moore, K.J. Utilization of mouse models in the discovery of human disease genes. Drug Discov. Today 1999, 4, 123–128. [Google Scholar] [CrossRef]
- Mall, C.; Sckisel, G.D.; Proia, D.A.; Mirsoian, A.; Grossenbacher, S.K.; Pai, C.C.S.; Murphy, W.J. Repeated PD-1/PD-L1 monoclonal antibody administration induces fatal xenogeneic hypersensitivity reactions in a murine model of breast cancer. Oncoimmunology 2016, 5, e1075114. [Google Scholar] [CrossRef]
- Brüggemann, M.; Winter, G.; Waldmann, H.; Neuberger, M.S. The immunogenicity of chimeric antibodies. J. Exp. Med. 1989, 170, 2153–2157. [Google Scholar] [CrossRef] [PubMed]
- Hunter, K.W., Jr. Murine mammary carcinoma 4T1 induces a leukemoid reaction with splenomegaly: Association with tumor-derived growth factors. Exp. Mol. Pathol. 2007, 82, 12–24. [Google Scholar]
- Heppner, G.H.; Miller, F.R.; Shekhar, P.M. Nontransgenic models of breast cancer. Breast Cancer Res. 2000, 2, 331. [Google Scholar] [CrossRef] [PubMed]
- Lelekakis, M.; Moseley, J.M.; Martin, T.J.; Hards, D.; Williams, E.; Ho, P.; Anderson, R.L. A novel orthotopic model of breast cancer metastasis to bone. Clin. Exp. Metastasis 1999, 17, 163–170. [Google Scholar] [CrossRef]
- De Souza Garcia, C.M.; de Araújo, M.R.; Lopes, M.T.P.; Ferreira, M.; Cassali, G.D. Morphological and immunophenotipical characterization of murine mammary carcinoma 4t1. Braz. J. Vet. Pathol. 2014, 7, 158–165. [Google Scholar]
- McMaster, P.D.; Kruse, H. Peripheral vascular reactions in anaphylaxis of the mouse. J. Exp. Med. 1949, 89, 583–596. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Weiser, R.S.; Golub, O.J.; Hamre, D.M. Studies on anaphylaxis in the mouse. J. Infect. Dis. 1941, 68, 97–112. [Google Scholar] [CrossRef]
- Cameron, J. The effect of aspirin, cortisone and other compounds on susceptibility to anaphylactic shock in mice. Br. J. Exp. Pathol. 1957, 38, 512. [Google Scholar]
- Presta, L.G. Engineering of therapeutic antibodies to minimize immunogenicity and optimize function. Adv. Drug Deliv. Rev. 2006, 58, 640–656. [Google Scholar] [CrossRef] [PubMed]
- Khodoun, M.V.; Strait, R.; Armstrong, L.; Yanase, N.; Finkelman, F.D. Identification of markers that distinguish IgE-from IgG-mediated anaphylaxis. Proc. Natl. Acad. Sci. USA 2011, 108, 12413–12418. [Google Scholar] [CrossRef]
- Jönsson, F.; Mancardi, D.A.; Kita, Y.; Karasuyama, H.; Iannascoli, B.; Van Rooijen, N.; Bruhns, P. Mouse and human neutrophils induce anaphylaxis. J. Clin. Invest. 2011, 121, 1484–1496. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monjazeb, A.M.; Wang, Z.; Vick, L.V.; Dunai, C.; Minnar, C.; Khuat, L.T.; Murphy, W.J. Mouse Preclinical Cancer Immunotherapy Modeling Involving Anti-PD-1 Therapies Reveals the Need to Use Mouse Reagents to Mirror Clinical Paradigms. Cancers 2021, 13, 729. https://doi.org/10.3390/cancers13040729
Monjazeb AM, Wang Z, Vick LV, Dunai C, Minnar C, Khuat LT, Murphy WJ. Mouse Preclinical Cancer Immunotherapy Modeling Involving Anti-PD-1 Therapies Reveals the Need to Use Mouse Reagents to Mirror Clinical Paradigms. Cancers. 2021; 13(4):729. https://doi.org/10.3390/cancers13040729
Chicago/Turabian StyleMonjazeb, Arta M., Ziming Wang, Logan V. Vick, Cordelia Dunai, Christine Minnar, Lam T. Khuat, and William J. Murphy. 2021. "Mouse Preclinical Cancer Immunotherapy Modeling Involving Anti-PD-1 Therapies Reveals the Need to Use Mouse Reagents to Mirror Clinical Paradigms" Cancers 13, no. 4: 729. https://doi.org/10.3390/cancers13040729
APA StyleMonjazeb, A. M., Wang, Z., Vick, L. V., Dunai, C., Minnar, C., Khuat, L. T., & Murphy, W. J. (2021). Mouse Preclinical Cancer Immunotherapy Modeling Involving Anti-PD-1 Therapies Reveals the Need to Use Mouse Reagents to Mirror Clinical Paradigms. Cancers, 13(4), 729. https://doi.org/10.3390/cancers13040729





