Combination of Modern Radiotherapy and New Targeted Treatments for Breast Cancer Management
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
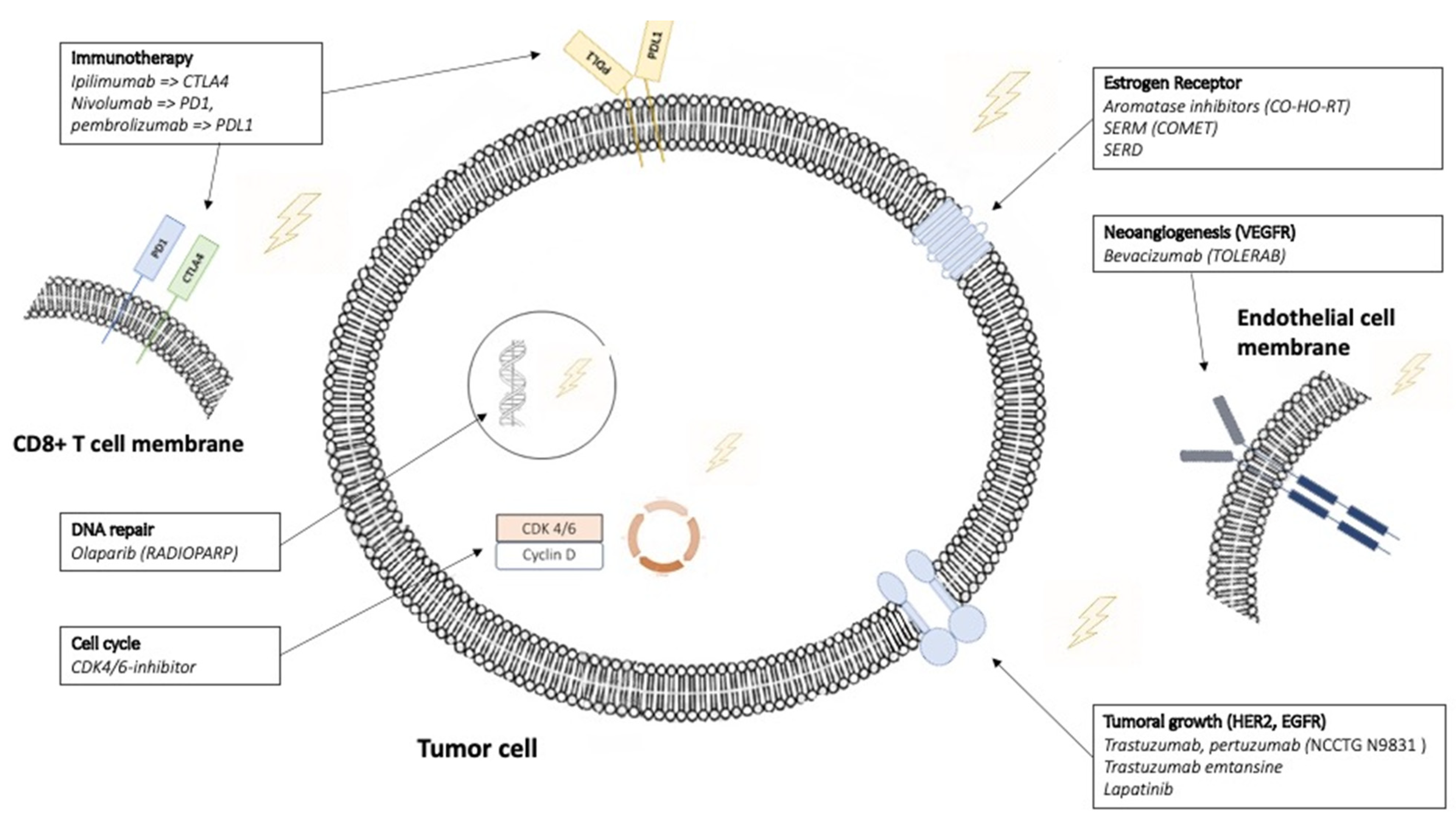
3.1. Hormonotherapy
3.2. Target the Tumor Growth: HER-2 Inhibitor
3.3. Target the Tumor Angiogenesis: VEGF-Inhibitor
3.4. Immunotherapy
3.5. Target the Cell Cycle: CDK-Inhibitor
3.6. Target the DNA Repair: PARP-Inhibitor
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ADC | antibody–drug conjugate |
| BC | breast cancer |
| BM | brain metastases |
| CDK-I | CDK inhibitor |
| EGFR | epidermal growth factor |
| ER | estrogen receptor |
| GnRH | gonadotropin hormone analogues |
| ICI | immune checkpoint inhibitors |
| LHRH | luteinizing hormone−releasing hormone |
| LVEF | Left ventricular ejection fraction |
| PD | pharmacodynamic |
| PF | pulmonary fibrosis |
| PK | pharmacokinetic |
| RT | radiation therapy |
| SBRT | stereotactic body RT |
| SERD | selective estrogen receptor degradants |
| SERM | selective estrogen receptor modulators |
| T-DM1 | Trastuzumab emtansine |
| TKI | tyrosine kinase inhibitor |
| WBRT | whole-brain RT |
References
- EBCTCG. Effect of Radiotherapy after Breast-Conserving Surgery on 10-Year Recurrence and 15-Year Breast Cancer Death: Meta-Analysis of Individual Patient Data for 10 801 Women in 17 Randomised Trials. Lancet 2011, 378, 1707–1716. [Google Scholar] [CrossRef]
- Patel, H.K.; Bihani, T. Selective Estrogen Receptor Modulators (SERMs) and Selective Estrogen Receptor Degraders (SERDs) in Cancer Treatment. Pharmacol. Ther. 2018, 186, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Anzic, M.; Marinko, T. Effect of Adjuvant Hormonal Therapy on the Development of Pulmonary Fibrosis after Postoperative Radiotherapy for Breast Cancer. J. Breast Cancer 2020, 23, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Butta, A.; MacLennan, K.; Flanders, K.C.; Sacks, N.P.; Smith, I.; McKinna, A.; Dowsett, M.; Wakefield, L.M.; Sporn, M.B.; Baum, M. Induction of Transforming Growth Factor Beta 1 in Human Breast Cancer in Vivo Following Tamoxifen Treatment. Cancer Res. 1992, 52, 4261–4264. [Google Scholar] [PubMed]
- Yavas, G.; Yavas, C.; Acar, H.; Toy, H.; Yuce, D.; Ata, O. Comparison of the Effects of Aromatase Inhibitors and Tamoxifen on Radiation-Induced Lung Toxicity: Results of an Experimental Study. Support Care Cancer 2013, 21, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Bentzen, S.M.; Skoczylas, J.Z.; Overgaard, M.; Overgaard, J. Radiotherapy-Related Lung Fibrosis Enhanced by Tamoxifen. J. Natl. Cancer Inst. 1996, 88, 918–922. [Google Scholar] [CrossRef] [PubMed]
- Varga, Z.; Cserháti, A.; Kelemen, G.; Boda, K.; Thurzó, L.; Kahán, Z. Role of Systemic Therapy in the Development of Lung Sequelae after Conformal Radiotherapy in Breast Cancer Patients. Int. J. Radiat. Oncol. Biol. Phys. 2011, 80, 1109–1116. [Google Scholar] [CrossRef]
- Dörr, W.; Bertmann, S.; Herrmann, T. Radiation Induced Lung Reactions in Breast Cancer Therapy. Modulating Factors and Consequential Effects. Strahlenther. Onkol. 2005, 181, 567–573. [Google Scholar] [CrossRef]
- Pierce, L.J.; Hutchins, L.F.; Green, S.R.; Lew, D.L.; Gralow, J.R.; Livingston, R.B.; Osborne, C.K.; Albain, K.S. Sequencing of Tamoxifen and Radiotherapy after Breast-Conserving Surgery in Early-Stage Breast Cancer. J. Clin. Oncol. 2005, 23, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Harris, E.E.R.; Christensen, V.J.; Hwang, W.-T.; Fox, K.; Solin, L.J. Impact of Concurrent versus Sequential Tamoxifen with Radiation Therapy in Early-Stage Breast Cancer Patients Undergoing Breast Conservation Treatment. J. Clin. Oncol. 2005, 23, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Munshi, A.; Gupta, D. Concurrent versus Sequential Radiotherapy and Tamoxifen in Breast Cancer—The CONSET Trial Is Launched. Acta Oncol. 2011, 50, 154–155. [Google Scholar] [CrossRef] [PubMed]
- Arimidex, Tamoxifen, Alone or in Combination Trialists’ Group; Buzdar, A.; Howell, A.; Cuzick, J.; Wale, C.; Distler, W.; Hoctin-Boes, G.; Houghton, J.; Locker, G.Y.; Nabholtz, J.M. Comprehensive Side-Effect Profile of Anastrozole and Tamoxifen as Adjuvant Treatment for Early-Stage Breast Cancer: Long-Term Safety Analysis of the ATAC Trial. Lancet Oncol. 2006, 7, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Bollet, M.A.; Kirova, Y.M.; Antoni, G.; Pierga, J.-Y.; Sigal-Zafrani, B.; Laki, F.; Campana, F.; Dendale, R.; Salmon, R.; Cottu, P.; et al. Responses to Concurrent Radiotherapy and Hormone-Therapy and Outcome for Large Breast Cancers in Post-Menopausal Women. Radiother. Oncol. 2007, 85, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Azria, D.; Belkacemi, Y.; Romieu, G.; Gourgou, S.; Gutowski, M.; Zaman, K.; Moscardo, C.L.; Lemanski, C.; Coelho, M.; Rosenstein, B.; et al. Concurrent or Sequential Adjuvant Letrozole and Radiotherapy after Conservative Surgery for Early-Stage Breast Cancer (CO-HO-RT): A Phase 2 Randomised Trial. Lancet Oncol. 2010, 11, 258–265. [Google Scholar] [CrossRef]
- Chargari, C.; Castro-Pena, P.; Toledano, I.; Bollet, M.A.; Savignoni, A.; Cottu, P.; Laki, F.; Campana, F.; De Cremoux, P.; Fourquet, A.; et al. Concurrent Use of Aromatase Inhibitors and Hypofractionated Radiation Therapy. World J. Radiol. 2012, 4, 318–323. [Google Scholar] [CrossRef]
- Loap, P.; Kirova, Y.; Takanen, S.; Créhange, G.; Fourquet, A. Breast radiation therapy during COVID-19 outbreak: Practical advice. Cancer Radiother. 2020, 24, 196–198. [Google Scholar] [CrossRef] [PubMed]
- Rozeboom, B.; Dey, N.; De, P. ER+ Metastatic Breast Cancer: Past, Present, and a Prescription for an Apoptosis-Targeted Future. Am. J. Cancer Res. 2019, 9, 2821–2831. [Google Scholar]
- Metcalfe, C.; Ingalla, E.; Blake, R.; Chang, J.; Daemen, A.; De Bruyn, T.; Giltnane, J.; Guan, J.; Hafner, M.; Hartman, S.; et al. Abstract P5-04-07: GDC-9545: A Novel ER Antagonist and Clinical Candidate That Combines Desirable Mechanistic and Pre-Clinical DMPK Attributes. Cancer Res. 2019, 79, P5-04-07. [Google Scholar] [CrossRef]
- Bihani, T.; Patel, H.K.; Arlt, H.; Tao, N.; Jiang, H.; Brown, J.L.; Purandare, D.M.; Hattersley, G.; Garner, F. Elacestrant (RAD1901), a Selective Estrogen Receptor Degrader (SERD), Has Antitumor Activity in Multiple ER+ Breast Cancer Patient-Derived Xenograft Models. Clin. Cancer Res. 2017, 23, 4793–4804. [Google Scholar] [CrossRef]
- Patel, H.K.; Tao, N.; Lee, K.-M.; Huerta, M.; Arlt, H.; Mullarkey, T.; Troy, S.; Arteaga, C.L.; Bihani, T. Elacestrant (RAD1901) Exhibits Anti-Tumor Activity in Multiple ER+ Breast Cancer Models Resistant to CDK4/6 Inhibitors. Breast Cancer Res. 2019, 21, 146. [Google Scholar] [CrossRef]
- Gombos, A. Selective Oestrogen Receptor Degraders in Breast Cancer: A Review and Perspectives. Curr. Opin. Oncol. 2019, 31, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Kümler, I.; Tuxen, M.K.; Nielsen, D.L. A Systematic Review of Dual Targeting in HER2-Positive Breast Cancer. Cancer Treat. Rev. 2014, 40, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Pietras, R.J.; Poen, J.C.; Gallardo, D.; Wongvipat, P.N.; Lee, H.J.; Slamon, D.J. Monoclonal Antibody to HER-2/Neureceptor Modulates Repair of Radiation-Induced DNA Damage and Enhances Radiosensitivity of Human Breast Cancer Cells Overexpressing This Oncogene. Cancer Res. 1999, 59, 1347–1355. [Google Scholar]
- Hou, J.; Zhou, Z.; Chen, X.; Zhao, R.; Yang, Z.; Wei, N.; Ni, Q.; Feng, Y.; Yu, X.; Ma, J.; et al. HER2 Reduces Breast Cancer Radiosensitivity by Activating Focal Adhesion Kinase in Vitro and in Vivo. Oncotarget 2016, 7, 45186–45198. [Google Scholar] [CrossRef] [PubMed]
- Denduluri, N.; Somerfield, M.R.; Eisen, A.; Holloway, J.N.; Hurria, A.; King, T.A.; Lyman, G.H.; Partridge, A.H.; Telli, M.L.; Trudeau, M.E.; et al. Selection of Optimal Adjuvant Chemotherapy Regimens for Human Epidermal Growth Factor Receptor 2 (HER2)-Negative and Adjuvant Targeted Therapy for HER2-Positive Breast Cancers: An American Society of Clinical Oncology Guideline Adaptation of the Cancer Care Ontario Clinical Practice Guideline. J. Clin. Oncol. 2016, 34, 2416–2427. [Google Scholar] [CrossRef] [PubMed]
- Lidbrink, E.; Chmielowska, E.; Otremba, B.; Bouhlel, A.; Lauer, S.; Liste Hermoso, M.; Nüesch, E.; Shing, M.; Misra, V. A Real-World Study of Cardiac Events in >3700 Patients with HER2-Positive Early Breast Cancer Treated with Trastuzumab: Final Analysis of the OHERA Study. Breast Cancer Res. Treat. 2019, 174, 187–196. [Google Scholar] [CrossRef]
- Bergom, C.; Bradley, J.A.; Ng, A.K.; Samson, P.; Robinson, C.; Lopez-Mattei, J.; Mitchell, J.D. Past, Present, and Future of Radiation-Induced Cardiotoxicity: Refinements in Targeting, Surveillance, and Risk Stratification. JACC CardioOncol. 2021, 3, 343–359. [Google Scholar] [CrossRef] [PubMed]
- Jacob, J.; Belin, L.; Pierga, J.Y.; Gobillion, A.; Vincent-Salomon, A.; Dendale, R.; Beuzeboc, P.; Campana, F.; Fourquet, A.; Kirova, Y.M. Concurrent Administration of Trastuzumab with Locoregional Breast Radiotherapy: Long-Term Results of a Prospective Study. Breast Cancer Res. Treat. 2014, 148, 345–353. [Google Scholar] [CrossRef]
- Caussa, L.; Kirova, Y.M.; Gault, N.; Pierga, J.-Y.; Savignoni, A.; Campana, F.; Dendale, R.; Fourquet, A.; Bollet, M.A. The Acute Skin and Heart Toxicity of a Concurrent Association of Trastuzumab and Locoregional Breast Radiotherapy Including Internal Mammary Chain: A Single-Institution Study. Eur. J. Cancer 2011, 47, 65–73. [Google Scholar] [CrossRef]
- Halyard, M.Y.; Pisansky, T.M.; Dueck, A.C.; Suman, V.; Pierce, L.; Solin, L.; Marks, L.; Davidson, N.; Martino, S.; Kaufman, P.; et al. Radiotherapy and Adjuvant Trastuzumab in Operable Breast Cancer: Tolerability and Adverse Event Data from the NCCTG Phase III Trial N9831. J. Clin. Oncol. 2009, 27, 2638–2644. [Google Scholar] [CrossRef] [PubMed]
- Aboudaram, A.; Loap, P.; Loirat, D.; Dhia, S.B.; Cao, K.; Fourquet, A.; Kirova, Y. Pertuzumab and Trastuzumab Combination with Concomitant Locoregional Radiotherapy for the Treatment of Breast Cancers with HER2 Receptor Overexpression. Cancers 2021, 13, 4790. [Google Scholar] [CrossRef]
- Belkacémi, Y.; Gligorov, J.; Ozsahin, M.; Marsiglia, H.; De Lafontan, B.; Laharie-Mineur, H.; Aimard, L.; Antoine, E.-C.; Cutuli, B.; Namer, M.; et al. Concurrent Trastuzumab with Adjuvant Radiotherapy in HER2-Positive Breast Cancer Patients: Acute Toxicity Analyses from the French Multicentric Study. Ann. Oncol. 2008, 19, 1110–1116. [Google Scholar] [CrossRef] [PubMed]
- Ben Dhia, S.; Loap, P.; Loirat, D.; Vincent-Salomon, A.; Cao, K.; Escalup, L.; Fourquet, A.; Kirova, Y. Concurrent radiation therapy and dual HER2 blockade in breast cancer: Assessment of toxicity. Cancer Radiother. 2021, 25, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Ajgal, Z.; de Percin, S.; Diéras, V.; Pierga, J.Y.; Campana, F.; Fourquet, A.; Kirova, Y.M. Combination of Radiotherapy and Double Blockade HER2 with Pertuzumab and Trastuzumab for HER2-Positive Metastatic or Locally Recurrent Unresectable and/or Metastatic Breast Cancer: Assessment of Early Toxicity. Cancer Radiother. 2017, 21, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Alvarez, A.; Papakonstantinou, A.; Oliveira, M. Brain Metastases in HER2-Positive Breast Cancer: Current and Novel Treatment Strategies. Cancers 2021, 13, 2927. [Google Scholar] [CrossRef]
- Chargari, C.; Idrissi, H.R.; Pierga, J.-Y.; Bollet, M.A.; Diéras, V.; Campana, F.; Cottu, P.; Fourquet, A.; Kirova, Y.M. Preliminary Results of Whole Brain Radiotherapy with Concurrent Trastuzumab for Treatment of Brain Metastases in Breast Cancer Patients. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 631–636. [Google Scholar] [CrossRef]
- Krop, I.; Winer, E.P. Trastuzumab Emtansine: A Novel Antibody-Drug Conjugate for HER2-Positive Breast Cancer. Clin. Cancer Res. 2014, 20, 15–20. [Google Scholar] [CrossRef]
- Stumpf, P.K.; Cittelly, D.M.; Robin, T.P.; Carlson, J.A.; Stuhr, K.A.; Contreras-Zarate, M.J.; Lai, S.; Ormond, D.R.; Rusthoven, C.G.; Gaspar, L.E.; et al. Combination of Trastuzumab Emtansine and Stereotactic Radiosurgery Results in High Rates of Clinically Significant Radionecrosis and Dysregulation of Aquaporin-4. Clin. Cancer Res. 2019, 25, 3946–3953. [Google Scholar] [CrossRef]
- Geraud, A.; Xu, H.P.; Beuzeboc, P.; Kirova, Y.M. Preliminary Experience of the Concurrent Use of Radiosurgery and T-DM1 for Brain Metastases in HER2-Positive Metastatic Breast Cancer. J. Neurooncol. 2017, 131, 69–72. [Google Scholar] [CrossRef]
- von Minckwitz, G.; Huang, C.-S.; Mano, M.S.; Loibl, S.; Mamounas, E.P.; Untch, M.; Wolmark, N.; Rastogi, P.; Schneeweiss, A.; Redondo, A.; et al. Trastuzumab Emtansine for Residual Invasive HER2-Positive Breast Cancer. N. Engl. J. Med. 2019, 380, 617–628. [Google Scholar] [CrossRef]
- Denduluri, N.; Somerfield, M.R.; Chavez-MacGregor, M.; Comander, A.H.; Dayao, Z.; Eisen, A.; Freedman, R.A.; Gopalakrishnan, R.; Graff, S.L.; Hassett, M.J.; et al. Selection of Optimal Adjuvant Chemotherapy and Targeted Therapy for Early Breast Cancer: ASCO Guideline Update. J. Clin. Oncol. 2020, 39, 685–693. [Google Scholar] [CrossRef]
- Mignot, F. In Vitro Effects of Trastuzumab Emtansine (T-DM1) and Concurrent Irradiation on HER2-Positive Breast Cancer Cells. Cancer/Radiothérapie 2021, 25, 126–134. [Google Scholar] [CrossRef]
- Zolcsák, Z.; Loirat, D.; Fourquet, A.; Kirova, Y.M. Adjuvant Trastuzumab Emtansine (T-DM1) and Concurrent Radiotherapy for Residual Invasive HER2-Positive Breast Cancer: Single-Center Preliminary Results. Am. J. Clin. Oncol. 2020, 43, 895–901. [Google Scholar] [CrossRef] [PubMed]
- Sambade, M.J.; Kimple, R.J.; Camp, J.T.; Peters, E.; Livasy, C.A.; Sartor, C.I.; Shields, J.M. Lapatinib in Combination with Radiation Diminishes Tumor Regrowth in HER2+ and Basal-Like/EGFR+ Breast Tumor Xenografts. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 575–581. [Google Scholar] [CrossRef][Green Version]
- Christodoulou, C.; Kalogera-Fountzila, A.; Karavasilis, V.; Kouvatseas, G.; Papandreou, C.N.; Samantas, E.; Varaki, K.; Papadopoulos, G.; Bobos, M.; Rallis, G.; et al. Lapatinib with Whole Brain Radiotherapy in Patients with Brain Metastases from Breast and Non-Small Cell Lung Cancer: A Phase II Study of the Hellenic Cooperative Oncology Group (HeCOG). J. Neurooncol. 2017, 134, 443–451. [Google Scholar] [CrossRef]
- Kim, J.M.; Miller, J.A.; Kotecha, R.; Chao, S.T.; Ahluwalia, M.S.; Peereboom, D.M.; Mohammadi, A.M.; Barnett, G.H.; Murphy, E.S.; Vogelbaum, M.A.; et al. Stereotactic Radiosurgery with Concurrent HER2-Directed Therapy Is Associated with Improved Objective Response for Breast Cancer Brain Metastasis. Neuro-Oncology 2019, 21, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Pierga, J.-Y.; Petit, T.; Delozier, T.; Ferrero, J.-M.; Campone, M.; Gligorov, J.; Lerebours, F.; Roché, H.; Bachelot, T.; Charafe-Jauffret, E.; et al. Neoadjuvant Bevacizumab, Trastuzumab, and Chemotherapy for Primary Inflammatory HER2-Positive Breast Cancer (BEVERLY-2): An Open-Label, Single-Arm Phase 2 Study. Lancet Oncol. 2012, 13, 375–384. [Google Scholar] [CrossRef]
- Robert, N.J.; Diéras, V.; Glaspy, J.; Brufsky, A.M.; Bondarenko, I.; Lipatov, O.N.; Perez, E.A.; Yardley, D.A.; Chan, S.Y.T.; Zhou, X.; et al. RIBBON-1: Randomized, Double-Blind, Placebo-Controlled, Phase III Trial of Chemotherapy with or without Bevacizumab for First-Line Treatment of Human Epidermal Growth Factor Receptor 2-Negative, Locally Recurrent or Metastatic Breast Cancer. J. Clin. Oncol. 2011, 29, 1252–1260. [Google Scholar] [CrossRef]
- Schueneman, A.J.; Himmelfarb, E.; Geng, L.; Tan, J.; Donnelly, E.; Mendel, D.; McMahon, G.; Hallahan, D.E. SU11248 Maintenance Therapy Prevents Tumor Regrowth after Fractionated Irradiation of Murine Tumor Models. Cancer Res. 2003, 63, 4009–4016. [Google Scholar] [PubMed]
- Huber, P.E.; Bischof, M.; Jenne, J.; Heiland, S.; Peschke, P.; Saffrich, R.; Gröne, H.-J.; Debus, J.; Lipson, K.E.; Abdollahi, A. Trimodal Cancer Treatment: Beneficial Effects of Combined Antiangiogenesis, Radiation, and Chemotherapy. Cancer Res. 2005, 65, 3643–3655. [Google Scholar] [CrossRef]
- Goyal, S.; Rao, M.S.; Khan, A.; Huzzy, L.; Green, C.; Haffty, B.G. Evaluation of Acute Locoregional Toxicity in Patients with Breast Cancer Treated with Adjuvant Radiotherapy in Combination with Bevacizumab. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 408–413. [Google Scholar] [CrossRef]
- Pernin, V.; Belin, L.; Cottu, P.; Bontemps, P.; Lemanski, C.; De La Lande, B.; Baumann, P.; Missohou, F.; Levy, C.; Peignaux, K.; et al. Radiotherapy Associated with Concurrent Bevacizumab in Patients with Non-Metastatic Breast Cancer. Breast 2014, 23, 816–820. [Google Scholar] [CrossRef]
- Clément-Zhao, A.; Tanguy, M.-L.; Cottu, P.; De La Lande, B.; Bontemps, P.; Lemanski, C.; Baumann, P.; Savignoni, A.; Levy, C.; Peignaux, K.; et al. Toxicity of Locoregional Radiotherapy in Combination with Bevacizumab in Patients with Non-Metastatic Breast Cancer (TOLERAB): Final Long-Term Evaluation. PLoS ONE 2019, 14, e0221816. [Google Scholar] [CrossRef]
- Demaria, S.; Kawashima, N.; Yang, A.M.; Devitt, M.L.; Babb, J.S.; Allison, J.P.; Formenti, S.C. Immune-Mediated Inhibition of Metastases after Treatment with Local Radiation and CTLA-4 Blockade in a Mouse Model of Breast Cancer. Clin. Cancer Res. 2005, 11, 728–734. [Google Scholar] [PubMed]
- Verbrugge, I.; Hagekyriakou, J.; Sharp, L.L.; Galli, M.; West, A.; McLaughlin, N.M.; Duret, H.; Yagita, H.; Johnstone, R.W.; Smyth, M.J.; et al. Radiotherapy Increases the Permissiveness of Established Mammary Tumors to Rejection by Immunomodulatory Antibodies. Cancer Res. 2012, 72, 3163–3174. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Liang, H.; Burnette, B.; Beckett, M.; Darga, T.; Weichselbaum, R.R.; Fu, Y.-X. Irradiation and Anti-PD-L1 Treatment Synergistically Promote Antitumor Immunity in Mice. J. Clin. Investig. 2014, 124, 687–695. [Google Scholar] [CrossRef]
- Ho, A.Y.; Barker, C.A.; Arnold, B.B.; Powell, S.N.; Hu, Z.I.; Gucalp, A.; Lebron-Zapata, L.; Wen, H.Y.; Kallman, C.; D’Agnolo, A.; et al. A Phase 2 Clinical Trial assessing the efficacy and Safety of Pembrolizumab and Radiotherapy in Patients with Metastatic Triple-Negative Breast Cancer. Cancer 2020, 126, 850–860. [Google Scholar] [CrossRef]
- Barroso-Sousa, R.; Krop, I.E.; Trippa, L.; Tan-Wasielewski, Z.; Li, T.; Osmani, W.; Andrews, C.; Dillon, D.; Richardson, E.T.; Pastorello, R.G.; et al. A Phase II Study of Pembrolizumab in Combination With Palliative Radiotherapy for Hormone Receptor-Positive Metastatic Breast Cancer. Clin. Breast Cancer 2020, 20, 238–245. [Google Scholar] [CrossRef]
- Cao, K.; Abbassi, L.; Romano, E.; Kirova, Y. Radiation Therapy and Immunotherapy in Breast Cancer Treatment: Preliminary Data and Perspectives. Expert Rev. Anticancer Ther. 2021, 21, 501–510. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, E.; Chargari, C.; Galluzzi, L.; Kroemer, G. Optimising Efficacy and Reducing Toxicity of Anticancer Radioimmunotherapy. Lancet Oncol. 2019, 20, e452–e463. [Google Scholar] [CrossRef]
- Finn, R.S.; Martin, M.; Rugo, H.S.; Jones, S.; Im, S.-A.; Gelmon, K.; Harbeck, N.; Lipatov, O.N.; Walshe, J.M.; Moulder, S.; et al. Palbociclib and Letrozole in Advanced Breast Cancer. N. Engl. J. Med. 2016, 375, 1925–1936. [Google Scholar] [CrossRef]
- Iwata, H.; Im, S.-A.; Masuda, N.; Im, Y.-H.; Inoue, K.; Rai, Y.; Nakamura, R.; Kim, J.H.; Hoffman, J.T.; Zhang, K.; et al. PALOMA-3: Phase III Trial of Fulvestrant With or Without Palbociclib in Premenopausal and Postmenopausal Women With Hormone Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Metastatic Breast Cancer That Progressed on Prior Endocrine Therapy-Safety and Efficacy in Asian Patients. J. Glob. Oncol. 2017, 3, 289–303. [Google Scholar] [CrossRef]
- Finn, R.S.; Dering, J.; Conklin, D.; Kalous, O.; Cohen, D.J.; Desai, A.J.; Ginther, C.; Atefi, M.; Chen, I.; Fowst, C.; et al. PD 0332991, a Selective Cyclin D Kinase 4/6 Inhibitor, Preferentially Inhibits Proliferation of Luminal Estrogen Receptor-Positive Human Breast Cancer Cell Lines in Vitro. Breast Cancer Res. 2009, 11, R77. [Google Scholar] [CrossRef]
- Michaud, K.; Solomon, D.A.; Oermann, E.; Kim, J.-S.; Zhong, W.-Z.; Prados, M.D.; Ozawa, T.; James, C.D.; Waldman, T. Pharmacologic Inhibition of Cyclin-Dependent Kinases 4 and 6 Arrests the Growth of Glioblastoma Multiforme Intracranial Xenografts. Cancer Res. 2010, 70, 3228–3238. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, S.; Madani, D.; Joshi, S.; Chung, S.A.; Johns, T.; Day, B.; Khasraw, M.; McDonald, K.L. Combination of Palbociclib and Radiotherapy for Glioblastoma. Cell Death Discov. 2017, 3, 17033. [Google Scholar] [CrossRef] [PubMed]
- Hashizume, R.; Zhang, A.; Mueller, S.; Prados, M.D.; Lulla, R.R.; Goldman, S.; Saratsis, A.M.; Mazar, A.P.; Stegh, A.H.; Cheng, S.-Y.; et al. Inhibition of DNA Damage Repair by the CDK4/6 Inhibitor Palbociclib Delays Irradiated Intracranial Atypical Teratoid Rhabdoid Tumor and Glioblastoma Xenograft Regrowth. Neuro-Oncology 2016, 18, 1519–1528. [Google Scholar] [CrossRef] [PubMed]
- Bosacki, C.; Bouleftour, W.; Sotton, S.; Vallard, A.; Daguenet, E.; Ouaz, H.; Cojoracu, I.; Moslemi, D.; Molekzadehmoghani, M.; Magné, N. CDK 4/6 Inhibitors Combined with Radiotherapy: A Review of Literature. Clin. Transl. Radiat. Oncol. 2021, 26, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Hans, S.; Cottu, P.; Kirova, Y.M. Preliminary Results of the Association of Palbociclib and Radiotherapy in Metastatic Breast Cancer Patients. Radiother. Oncol. 2018, 126, 181. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, T.; Shikama, N.; Sasai, K. Severe Acute Radiation-Induced Enterocolitis after Combined Palbociclib and Palliative Radiotherapy Treatment. Radiother. Oncol. 2018, 131, 240–241. [Google Scholar] [CrossRef] [PubMed]
- Chowdhary, M.; Sen, N.; Chowdhary, A.; Usha, L.; Cobleigh, M.A.; Wang, D.; Patel, K.R.; Barry, P.N.; Rao, R.D. Safety and Efficacy of Palbociclib and Radiation Therapy in Patients With Metastatic Breast Cancer: Initial Results of a Novel Combination. Adv. Radiat. Oncol. 2019, 4, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Gil-Gil, M.; Alba, E.; Gavilá, J.; de la Haba-Rodríguez, J.; Ciruelos, E.; Tolosa, P.; Candini, D.; Llombart-Cussac, A. The Role of CDK4/6 Inhibitors in Early Breast Cancer. Breast 2021, 58, 160–169. [Google Scholar] [CrossRef]
- Pesch, A.M.; Hirsh, N.H.; Chandler, B.C.; Michmerhuizen, A.R.; Ritter, C.L.; Androsiglio, M.P.; Wilder-Romans, K.; Liu, M.; Gersch, C.L.; Larios, J.M.; et al. Short-Term CDK4/6 Inhibition Radiosensitizes Estrogen Receptor-Positive Breast Cancers. Clin. Cancer Res. 2020, 26, 6568–6580. [Google Scholar] [CrossRef] [PubMed]
- Petroni, G.; Buqué, A.; Yamazaki, T.; Bloy, N.; Liberto, M.D.; Chen-Kiang, S.; Formenti, S.C.; Galluzzi, L. Radiotherapy Delivered before CDK4/6 Inhibitors Mediates Superior Therapeutic Effects in ER+ Breast Cancer. Clin. Cancer Res. 2021, 27, 1855–1863. [Google Scholar] [CrossRef] [PubMed]
- Beddok, A.; Xu, H.P.; Henry, A.A.; Porte, B.; Fourquet, A.; Cottu, P.; Kirova, Y. Concurrent Use of Palbociclib and Radiation Therapy: Single-Centre Experience and Review of the Literature. Br. J. Cancer 2020, 123, 905–908. [Google Scholar] [CrossRef] [PubMed]
- Bryant, H.E.; Schultz, N.; Thomas, H.D.; Parker, K.M.; Flower, D.; Lopez, E.; Kyle, S.; Meuth, M.; Curtin, N.J.; Helleday, T. Specific Killing of BRCA2-Deficient Tumours with Inhibitors of Poly(ADP-Ribose) Polymerase. Nature 2005, 434, 913–917. [Google Scholar] [CrossRef] [PubMed]
- Farmer, H.; McCabe, N.; Lord, C.J.; Tutt, A.N.J.; Johnson, D.A.; Richardson, T.B.; Santarosa, M.; Dillon, K.J.; Hickson, I.; Knights, C.; et al. Targeting the DNA Repair Defect in BRCA Mutant Cells as a Therapeutic Strategy. Nature 2005, 434, 917–921. [Google Scholar] [CrossRef]
- Lesueur, P.; Chevalier, F.; Austry, J.-B.; Waissi, W.; Burckel, H.; Noël, G.; Habrand, J.-L.; Saintigny, Y.; Joly, F. Poly-(ADP-Ribose)-Polymerase Inhibitors as Radiosensitizers: A Systematic Review of Pre-Clinical and Clinical Human Studies. Oncotarget 2017, 8, 69105–69124. [Google Scholar] [CrossRef] [PubMed]
- Cerrato, A.; Morra, F.; Celetti, A. Use of Poly ADP-Ribose Polymerase [PARP] Inhibitors in Cancer Cells Bearing DDR Defects: The Rationale for Their Inclusion in the Clinic. J. Exp. Clin. Cancer Res. 2016, 35, 179. [Google Scholar] [CrossRef] [PubMed]
- Feng, F.Y.; Speers, C.; Liu, M.; Jackson, W.C.; Moon, D.; Rinkinen, J.; Wilder-Romans, K.; Jagsi, R.; Pierce, L.J. Targeted Radiosensitization with PARP1 Inhibition: Optimization of Therapy and Identification of Biomarkers of Response in Breast Cancer. Breast Cancer Res. Treat. 2014, 147, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Michmerhuizen, A.R.; Pesch, A.M.; Moubadder, L.; Chandler, B.C.; Wilder-Romans, K.; Cameron, M.; Olsen, E.; Thomas, D.G.; Zhang, A.; Hirsh, N.; et al. PARP1 Inhibition Radiosensitizes Models of Inflammatory Breast Cancer to Ionizing Radiation. Mol. Cancer Ther. 2019, 18, 2063–2073. [Google Scholar] [CrossRef]
- Jagsi, R.; Griffith, K.A.; Moran, J.M.; Ficaro, E.; Marsh, R.; Dess, R.T.; Chung, E.; Liss, A.L.; Hayman, J.A.; Mayo, C.S.; et al. A Randomized Comparison of Radiation Therapy Techniques in the Management of Node-Positive Breast Cancer: Primary Outcomes Analysis. Int. J. Radiat. Oncol. Biol. Phys. 2018, 101, 1149–1158. [Google Scholar] [CrossRef] [PubMed]
- Jagsi, R.; Griffith, K.A.; Bellon, J.R.; Woodward, W.A.; Horton, J.K.; Ho, A.; Feng, F.Y.; Speers, C.; Overmoyer, B.; Sabel, M.; et al. Concurrent Veliparib With Chest Wall and Nodal Radiotherapy in Patients With Inflammatory or Locoregionally Recurrent Breast Cancer: The TBCRC 024 Phase I Multicenter Study. J. Clin. Oncol. 2018, 36, 1317–1322. [Google Scholar] [CrossRef] [PubMed]
- Loap, P.; Loirat, D.; Berger, F.; Ricci, F.; Vincent-Salomon, A.; Ezzili, C.; Mosseri, V.; Fourquet, A.; Ezzalfani, M.; Kirova, Y. Combination of Olaparib and Radiation Therapy for Triple Negative Breast Cancer: Preliminary Results of the RADIOPARP Phase 1 Trial. Int. J. Radiat. Oncol. Biol. Phys. 2021, 109, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Loap, P.; Loirat, D.; Berger, F.; Cao, K.; Ricci, F.; Jochem, A.; Raizonville, L.; Mosseri, V.; Fourquet, A.; Kirova, Y. Combination of Olaparib with Radiotherapy for Triple-Negative Breast Cancers: One-Year Toxicity Report of the RADIOPARP Phase I Trial. Int. J. Cancer 2021, 149, 1828–1832. [Google Scholar] [CrossRef] [PubMed]
- Dewan, M.Z.; Galloway, A.E.; Kawashima, N.; Dewyngaert, J.K.; Babb, J.S.; Formenti, S.C.; Demaria, S. Fractionated but Not Single-Dose Radiotherapy Induces an Immune-Mediated Abscopal Effect When Combined with Anti-CTLA-4 Antibody. Clin. Cancer Res. 2009, 15, 5379–5388. [Google Scholar] [CrossRef] [PubMed]
| Target | Name | Number | Recruitment Status | Endpoint |
|---|---|---|---|---|
| Estrogen receptor (ER) | ||||
| Tamoxifen + locoregional RT | CONSET trial | NCT00896155 | Unknown | Pulmonary fibrosis |
| Tumor growth | ||||
| Trastuzumab Emtansine (T-DM1) + brain RT | BIRTH trial | NCT02135159 | Completed | Brain radionecrosis |
| Tumor angiogenesis | ||||
| Bevacizumab + brain RT | A-Plus | NCT02185352 | Active, not recruiting | Brain-specific progression free survival |
| Cell cycle | ||||
| Palbociclib + locoregional RT | PALATINE | NCT03870919 | Recruiting | Overall survival |
| DNA repair | ||||
| Olaparib +/− locoregional RT | NCT03598257 | Recruiting | Invasive Disease-Free Survival |
| Studies | Prospective/ Retrospective | Number of Patients | Mono or Double HER2 Blockage | IMC Irradiation | Anthracyclines | Grade 2 Cardiac Toxicity | Grade 2 Skin Toxicity | Grade 2 Esophagitis |
|---|---|---|---|---|---|---|---|---|
| Belkacémi et al. 2008 [32] | Prospective | 146 | Trastuzumab | 76% | NA | 10% | 51% | 12% |
| Halyard et al. 2009 [30] | Prospective | 982 | Trastuzumab | 0% | 100% | 2.1% | 6.2% | NA |
| Caussa et al. 2011 [29] | Prospective | 106 | Trastuzumab | 83% | 92% | 5.7% | 15.1% | 3.8% |
| Jacob et al. 2014 [28] | Prospective | 308 | Trastuzumab | 73.7% | 90.9% | 25.8% | 2.9% | 1.6% |
| Aboudaram et al. 2021 [31] | Retrospective | 55 | Trastuzumab-Pertuzumab | NA | NA | 0% | 30.9% | 1.8% |
| Targeted Treatments | Main Preclinical Results | Ref. | Main Clinical Results | Ref. |
|---|---|---|---|---|
| Estrogen receptor | ||||
| SERM (Tamoxifen) | In in vivo model: high frequency of RIPF in concurrent administration of tamoxifen and RT | [5] | In retrospective and prospetive studies: high frequency of RIPF in concurrent administration of tamoxifen and RT | [6,7,8] |
| Aromatase Inhibitor | In in vivo model: low frequency of RIPF in concurrent administration of AI and RT | [5] | In retrospective studies: low frequency of any grade 3 toxicity (incuding RIPF) | [13,14,15] |
| HER2-inhibitor | ||||
| Tastuzumab, Pertuzumab (both humanized monoclonal antibodies, directed against the extracellular domain of the receptor) | In in vitro models: HER2 reduces breast cancer celles radiosensitivity | [23,24] | In retrospective and prospetive studies: low frequency of cardiac toxicity in concurrent administration of HER2-inhibitor and locoregional RT and low frequency of brain toxicity in concurrent administration of HER2-inhibitor and brain RT | [28,29,30,31,32,36] |
| T-DM1 (antibody–drug conjugate) | In in vitro models: T-DM1 was not a radiation-sensitizer on HER2-positive breast cancer cells | [42] | In retrospective studie: high frequency of brain radionecrosis in concurrent administration of T-DM1 and brain SBRT, low frequency of cardiac toxicity in concurrent administration of T-DM1 and locoregional RT | [38,39,43] |
| Lapatinib, pyrotinib * and neratinib * (tyrosine kinase inhibitor targeting the epidermal growth factor (EGFR, ErbB-1) and HER2 (ErbB-2)) | In in vitro and in vivo models: lapatinib increased the radiosensitivity of BC cells lines and BC xenografts | [44,85] | In retrospective studie: low frequency of brain radionecrosis in concurrent administration of lapatinib and brain RT | [45,46] |
| VEGFR inhibitor | ||||
| Bevacizumab | In in vitro and in vivo models: VEGF inhibitor has a radiosensitizing effect when it is combined with RT | [49,50] | In retrospective studies; low frequency of any grade 3 toxicity in concurrent administration of bevacizumab and RT | [51,53] |
| Immunotherapy | ||||
| Ipilimumab (anti-CTLA-4 antibody) | In in vivo model: Increase overall survival in immunogenic murine model of metastatic BC | [54] | N/A | |
| Nivolumab and pembrolizumab (antibody PD-1/PD-L1 antibody) | In in vivo model: Antitumor effects of concurrent administration of RT and nivolumab in established triple-negative breast tumors | [55] | In prospective study: outcomes improvements in concurrent administration of pertuzumab and RT for metastatic BC, no data for toxicity | [57,58] |
| CDK inhibitor | ||||
| Palbociclib, ribociclib, abemaciclib (tyrosine kinase inhibitor targeting CDK4/6 cyclin D) | In in vitro and in vivo models: Coucurrent administration of CDK4/6 inhibition and RT led to significant radiosensitization in multiple BC models | [72,73] | In retrospective studies: several cases of grade 3 toxicity | [69,70,74] |
| PARP-inhibitor | ||||
| Olaparib, velaparib, rucaparib *, niraparib * | In in vitro study: Concurrent administration of PARPi and RT induce more DNA damages in particular in BRCA mutated BC cell lines | [80] | In retrospective and prospective studies: high frequency of late toxicity with velaparib, low frequence of late toxicity with olaparib | [82,84] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beddok, A.; Cottu, P.; Fourquet, A.; Kirova, Y. Combination of Modern Radiotherapy and New Targeted Treatments for Breast Cancer Management. Cancers 2021, 13, 6358. https://doi.org/10.3390/cancers13246358
Beddok A, Cottu P, Fourquet A, Kirova Y. Combination of Modern Radiotherapy and New Targeted Treatments for Breast Cancer Management. Cancers. 2021; 13(24):6358. https://doi.org/10.3390/cancers13246358
Chicago/Turabian StyleBeddok, Arnaud, Paul Cottu, Alain Fourquet, and Youlia Kirova. 2021. "Combination of Modern Radiotherapy and New Targeted Treatments for Breast Cancer Management" Cancers 13, no. 24: 6358. https://doi.org/10.3390/cancers13246358
APA StyleBeddok, A., Cottu, P., Fourquet, A., & Kirova, Y. (2021). Combination of Modern Radiotherapy and New Targeted Treatments for Breast Cancer Management. Cancers, 13(24), 6358. https://doi.org/10.3390/cancers13246358






