Augmented Reality and Image-Guided Robotic Liver Surgery
Abstract
:Simple Summary
Abstract
1. Introduction
2. Augmented Reality
2.1. External Robot-Assisted Liver Ablation
2.2. Augmented Reality in Clinical Practice
3. Image-Guided Robotic Liver Surgery
3.1. Preoperative Imaging and 3D Rendering
3.2. Intra-Operative Robotic Ultrasound Application
3.3. Indocyanine Green Fluorescence
4. Future Prospective
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ciria, R.; Cherqui, D.; Geller, D.A.; Briceno, J.; Wakabayashi, G. Comparative Short-term Benefits of Laparoscopic Liver Resection. Ann. Surg. 2016, 263, 761–777. [Google Scholar] [CrossRef]
- Wakabayashi, G.; Cherqui, D.; Geller, D.A.; Buell, J.F.; Kaneko, H.; Han, H.S.; Asbun, H.; O’rourke, N.; Tanabe, M.; Koffron, A.J.; et al. Recommendations for laparoscopic liver resection: A report from the second international consensus conference held in Morioka. Ann. Surg. 2015, 261, 619–629. [Google Scholar] [CrossRef] [PubMed]
- Kasai, M.; Cipriani, F.; Gayet, B.; Aldrighetti, L.; Ratti, F.; Sarmiento, J.M.; Scatton, O.; Kim, K.-H.; Dagher, I.; Topal, B.; et al. Laparoscopic versus open major hepatectomy: A systematic review and meta-analysis of individual patient data. Surgery 2018, 163, 985–995. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machairas, N.; Kostakis, I.D.; Schizas, D.; Kykalos, S.; Nikiteas, N.; Sotiropoulos, G.C. Meta-analysis of laparoscopic versus open liver resection for intrahepatic cholangiocarcinoma. Updates Surg. 2020, 73, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Guerrini, G.P.; Esposito, G.; Tarantino, G.; Serra, V.; Olivieri, T.; Catellani, B.; Assirati, G.; Guidetti, C.; Ballarin, R.; Magistri, P.; et al. Laparoscopic versus open liver resection for intrahepatic cholangiocarcinoma: The first meta-analysis. Langenbeck’s Arch. Surg. 2020, 405, 265–275. [Google Scholar] [CrossRef]
- Sotiropoulos, G.C.; Prodromidou, A.; Kostakis, I.D.; Machairas, N. Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. Updates Surg. 2017, 69, 291–311. [Google Scholar] [CrossRef]
- Syn, N.L.; Kabir, T.; Koh, Y.X.; Tan, H.L.; Wang, L.Z.; Chin, B.Z.; Wee, I.; Teo, J.Y.; Tai, B.C.; Goh, B.K.P. Survival Advantage of Laparoscopic Versus Open Resection For Colorectal Liver Metastases. Ann. Surg. 2019, 272, 253–265. [Google Scholar] [CrossRef]
- Schmelzle, M.; Krenzien, F.; Schöning, W.; Pratschke, J. Laparoscopic liver resection: Indications, limitations, and economic aspects. Langenbeck’s Arch. Surg. 2020, 405, 725–735. [Google Scholar] [CrossRef]
- Tsung, A.; Geller, D.A.; Sukato, D.C.; Sabbaghian, S.; Tohme, S.; Steel, J.; Marsh, W.; Reddy, S.K.; Bartlett, D.L. Robotic Versus Laparoscopic Hepatectomy. Ann. Surg. 2014, 259, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Gavriilidis, P.; Roberts, K.J.; Aldrighetti, L.; Sutcliffe, R.P. A comparison between robotic, laparoscopic and open hepatectomy: A systematic review and network meta-analysis. Eur. J. Surg. Oncol. 2020, 46, 1214–1224. [Google Scholar] [CrossRef]
- Zhao, Z.; Yin, Z.; Li, M.; Jiang, N.; Liu, R. State of the art in robotic liver surgery: A meta-analysis. Updates Surg. 2020, 73, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yuan, Q.; Xu, Y.; Wang, W. Comparative clinical outcomes of robot-assisted liver resection versus laparoscopic liver resection: A meta-analysis. PLoS ONE 2020, 15, e0240593. [Google Scholar] [CrossRef]
- Machairas, N.; Papaconstantinou, D.; Tsilimigras, D.I.; Moris, D.; Prodromidou, A.; Paspala, A.; Spartalis, E.; Kostakis, I.D. Comparison between robotic and open liver resection: A systematic review and meta-analysis of short-term outcomes. Updates Surg. 2019, 71, 39–48. [Google Scholar] [CrossRef]
- Tsilimigras, D.I.; Moris, D.; Vagios, S.; Merath, K.; Pawlik, T.M. Safety and oncologic outcomes of robotic liver resections: A systematic review. J. Surg. Oncol. 2018, 117, 1517–1530. [Google Scholar] [CrossRef]
- Liu, R.; Wakabayashi, G.; Kim, H.-J.; Choi, G.-H.; Yiengpruksawan, A.; Fong, Y.; He, J.; Boggi, U.; Troisi, R.I.; Efanov, M.; et al. International consensus statement on robotic hepatectomy surgery in 2018. World J. Gastroenterol. 2019, 25, 1432–1444. [Google Scholar] [CrossRef] [PubMed]
- Giménez, M.; Gallix, B.; Costamagna, G.; Vauthey, J.-N.; Moche, M.; Wakabayashi, G.; Bale, R.; Swanström, L.; Futterer, J.; Geller, D.; et al. Definitions of Computer-Assisted Surgery and Intervention, Image-Guided Surgery and Intervention, Hybrid Operating Room, and Guidance Systems. Ann. Surg. Open 2020, 1, e21. [Google Scholar] [CrossRef] [PubMed]
- Okuda, Y.; Taura, K.; Seo, S.; Yasuchika, K.; Nitta, T.; Ogawa, K.; Hatano, E.; Uemoto, S. Usefulness of operative planning based on 3-dimensional CT cholangiography for biliary malignancies. Surgery 2015, 158, 1261–1271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, C.-H.; Tao, H.-S.; Yang, J.; Fang, Z.-S.; Cai, W.; Liu, J.; Fan, Y.-F. Impact of Three-Dimensional Reconstruction Technique in the Operation Planning of Centrally Located Hepatocellular Carcinoma. J. Am. Coll. Surg. 2014, 220, 28–37. [Google Scholar] [CrossRef]
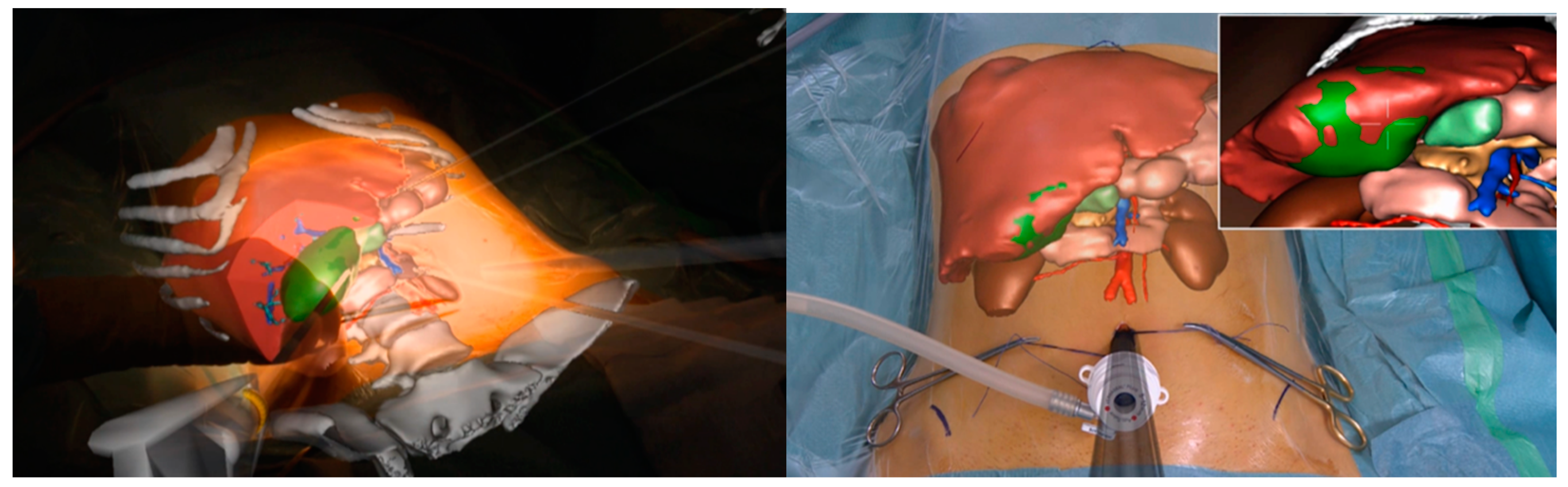
- Hallet, J.; Soler, L.; Diana, M.; Mutter, D.; Baumert, T.F.; Habersetzer, F.; Marescaux, J.; Pessaux, P. Trans-Thoracic Minimally Invasive Liver Resection Guided by Augmented Reality. J. Am. Coll. Surg. 2015, 220, e55–e60. [Google Scholar] [CrossRef] [PubMed]
- Phutane, P.; Buc, E.; Poirot, K.; Ozgur, E.; Pezet, D.; Bartoli, A.; Le Roy, B. Preliminary trial of augmented reality performed on a laparoscopic left hepatectomy. Surg. Endosc. 2017, 32, 514–515. [Google Scholar] [CrossRef]
- Mise, Y.; Hasegawa, K.; Satou, S.; Shindoh, J.; Miki, K.; Akamatsu, N.; Arita, J.; Kaneko, J.; Sakamoto, Y.; Kokudo, N. How Has Virtual Hepatectomy Changed the Practice of Liver Surgery? Ann. Surg. 2018, 268, 127–133. [Google Scholar] [CrossRef]
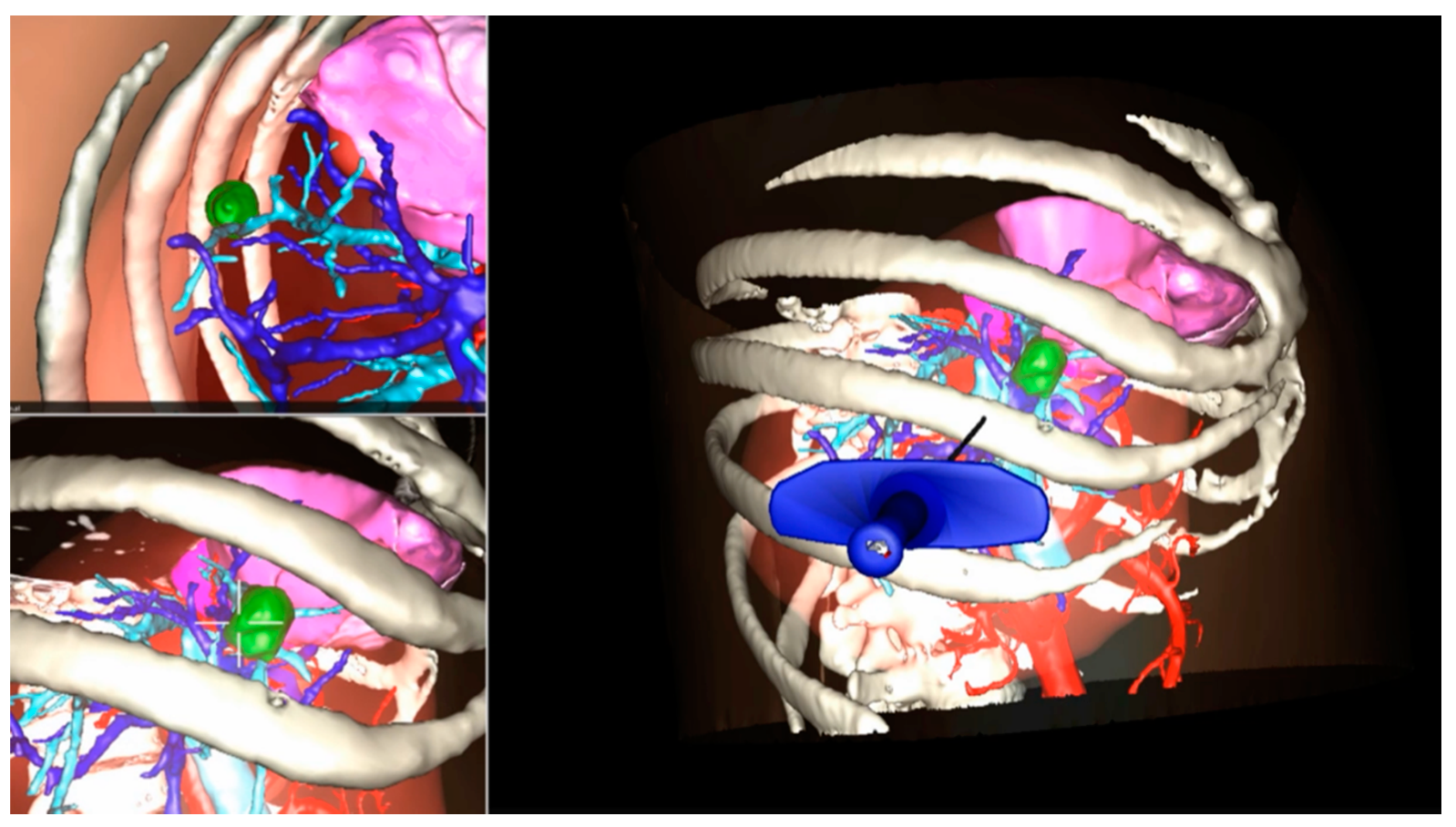
- Buchs, N.C.; Volonte, F.; Pugin, F.; Toso, C.; Fusaglia, M.; Gavaghan, K.; Majno, P.E.; Peterhans, M.; Weber, S.; Morel, P. Augmented environments for the targeting of hepatic lesions during image-guided robotic liver surgery. J. Surg. Res. 2013, 184, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Ntourakis, D.; Memeo, R.; Soler, L.; Marescaux, J.; Mutter, D.; Pessaux, P. Augmented Reality Guidance for the Resection of Missing Colorectal Liver Metastases: An Initial Experience. World J. Surg. 2015, 40, 419–426. [Google Scholar] [CrossRef]
- Kingham, T.P.; Pak, L.M.; Simpson, A.L.; Leung, U.; Doussot, A.; D’Angelica, M.I.; DeMatteo, R.P.; Allen, P.J.; Jarnagin, W.R. 3D image guidance assisted identification of colorectal cancer liver metastases not seen on intraoperative ultrasound: Results from a prospective trial. HPB 2017, 20, 260–267. [Google Scholar] [CrossRef] [Green Version]
- Banz, V.M.; Müller, P.C.; Tinguely, P.; Inderbitzin, D.; Ribes, D.; Peterhans, M.; Candinas, D.; Weber, S. Intraoperative image-guided navigation system: Development and applicability in 65 patients undergoing liver surgery. Langenbeck’s Arch. Surg. 2016, 401, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Diana, M.; Soler, L.; Agnus, V.; D’Urso, A.; Vix, M.; Dallemagne, B.; Faucher, V.; Roy, C.; Mutter, D.; Marescaux, J.; et al. Prospective Evaluation of Precision Multimodal Gallbladder Surgery Navigation. Ann. Surg. 2017, 266, 890–897. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, Y.; Kaneko, H.; Cleary, S.P.; Buell, J.F.; Cai, X.; Wakabayashi, G. What is the best technique in parenchymal transection in laparoscopic liver resection? Comprehensive review for the clinical question on the 2nd International Consensus Conference on Laparoscopic Liver Resection. J. Hepato-Biliary-Pancreat. Sci. 2015, 22, 363–370. [Google Scholar] [CrossRef]
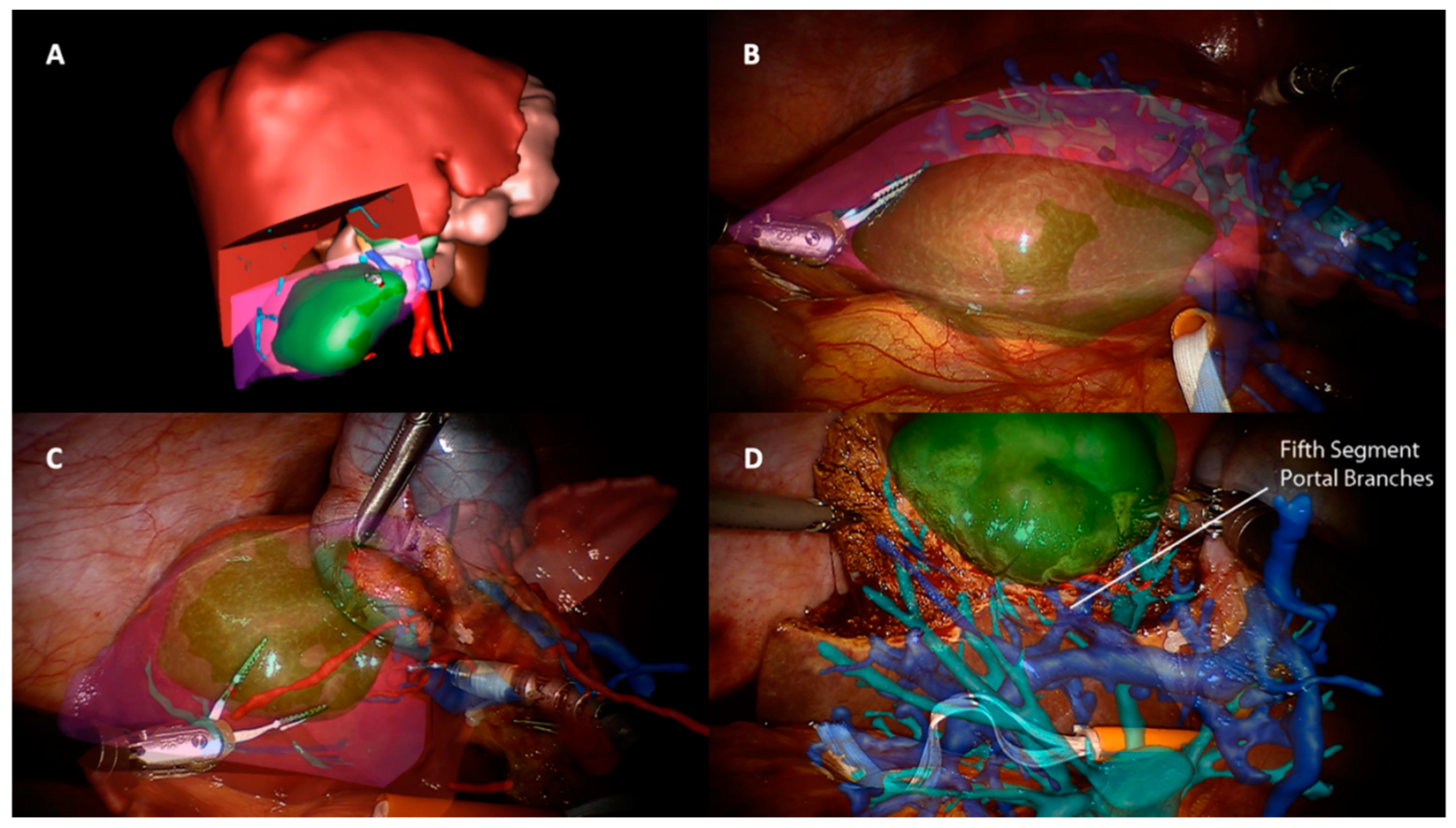
- Pessaux, P.; Diana, M.; Soler, L.; Piardi, T.; Mutter, D.; Marescaux, J. Towards cybernetic surgery: Robotic and augmented reality-assisted liver segmentectomy. Langenbeck’s Arch. Surg. 2014, 400, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Hao, W.; Binbin, J.; Wei, Y.; Kun, Y. Can Radiofrequency Ablation Replace Liver Resection for Solitary Colorectal Liver Metastasis? A Systemic Review and Meta-Analysis. Front. Oncol. 2020, 10, 561669. [Google Scholar] [CrossRef]
- Wen, R.; Chui, C.-K.; Ong, S.-H.; Lim, K.-B.; Chang, S.K.-Y. Projection-based visual guidance for robot-aided RF needle insertion. Int. J. Comput. Assist. Radiol. Surg. 2013, 8, 1015–1025. [Google Scholar] [CrossRef] [PubMed]
- Wen, R.; Tay, W.-L.; Nguyen, B.P.; Chng, C.-B.; Chui, C.-K. Hand gesture guided robot-assisted surgery based on a direct augmented reality interface. Comput. Methods Programs Biomed. 2014, 116, 68–80. [Google Scholar] [CrossRef] [PubMed]
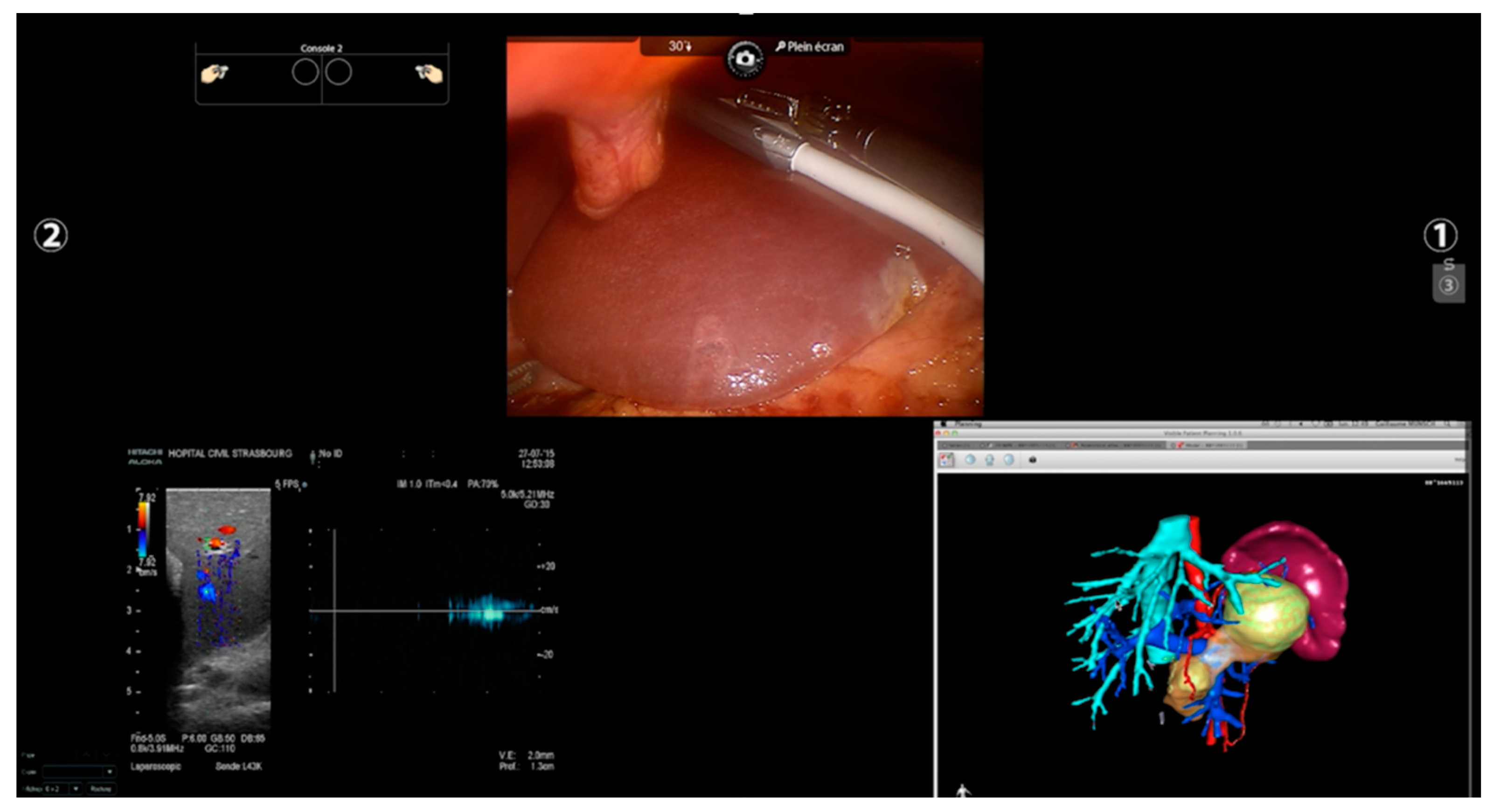
- Woo, Y.; Choi, G.H.; Min, B.S.; Hyung, W.J. Novel application of simultaneous multi-image display during complex robotic abdominal procedures. BMC Surg. 2014, 14, 13. [Google Scholar] [CrossRef] [Green Version]
- Marescaux, J.; Clément, J.-M.; Tassetti, V.; Koehl, C.; Cotin, S.; Russier, Y.; Mutter, D.; Delingette, H.; Ayache, N. Virtual Reality Applied to Hepatic Surgery Simulation: The Next Revolution. Ann. Surg. 1998, 228, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Palomar, R.; Cheikh, F.A.; Edwin, B.; Fretland, Å.; Beghdadi, A.; Elle, O.J. A novel method for planning liver resections using deformable Bézier surfaces and distance maps. Comput. Methods Programs Biomed. 2017, 144, 135–145. [Google Scholar] [CrossRef]
- Xiang, N.; Fang, C.; Fan, Y.; Yang, J.; Zeng, N.; Liu, J.; Zhu, W. Application of liver three-dimensional printing in hepatectomy for complex massive hepatocarcinoma with rare variations of portal vein: Preliminary experience. Int. J. Clin. Exp. Med. 2015, 8, 18873–18878. [Google Scholar] [PubMed]
- Li, P.; Wang, M.; Yang, Y.; Liu, H.; Pan, Z.; Jiang, B.; Lau, W.Y.; Huang, G.; Zhou, W. Preoperative three-dimensional versus two-dimensional evaluation in assessment of patients undergoing major liver resection for hepatocellular carcinoma: A propensity score matching study. Ann. Transl. Med. 2020, 8, 182. [Google Scholar] [CrossRef]
- Fang, C.; An, J.; Bruno, A.; Cai, X.; Fan, J.; Fujimoto, J.; Golfieri, R.; Hao, X.; Jiang, H.; Jiao, L.R.; et al. Consensus recommendations of three-dimensional visualization for diagnosis and management of liver diseases. Hepatol. Int. 2020, 14, 437–453. [Google Scholar] [CrossRef]
- Araki, K.; Conrad, C.; Ogiso, S.; Kuwano, H.; Gayet, B. Intraoperative Ultrasonography of Laparoscopic Hepatectomy: Key Technique for Safe Liver Transection. J. Am. Coll. Surg. 2013, 218, e37–e41. [Google Scholar] [CrossRef] [PubMed]
- Ferrero, A.; Langella, S.; Giuliante, F.; Viganò, L.; Vellone, M.; Zimmitti, G.; Ardito, F.; Nuzzo, G.; Capussotti, L. Intraoperative Liver Ultrasound Still Affects Surgical Strategy for Patients with Colorectal Metastases in the Modern Era. World J. Surg. 2013, 37, 2655–2663. [Google Scholar] [CrossRef]
- Langella, S.; Ardito, F.; Russolillo, N.; Panettieri, E.; Perotti, S.; Mele, C.; Giuliante, F.; Ferrero, A. Intraoperative Ultrasound Staging for Colorectal Liver Metastases in the Era of Liver-Specific Magnetic Resonance Imaging: Is It Still Worthwhile? J. Oncol. 2019, 2019, 1369274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Hondt, M.; Vandenbroucke-Menu, F.; Préville-Ratelle, S.; Turcotte, S.; Chagnon, M.; Plasse, M.; Létourneau, R.; Dagenais, M.; Roy, A.; Lapointe, R. Is intra-operative ultrasound still useful for the detection of a hepatic tumour in the era of modern pre-operative imaging? HPB 2011, 13, 665–669. [Google Scholar] [CrossRef] [Green Version]
- Viganò, L.; Ferrero, A.; Amisano, M.; Russolillo, N.; Capussotti, L. Comparison of laparoscopic and open intraoperative ultrasonography for staging liver tumours. BJS 2013, 100, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Langella, S.; Russolillo, N.; D’Eletto, M.; Forchino, F.; Tesoriere, R.L.; Ferrero, A. Oncological safety of ultrasound-guided laparoscopic liver resection for colorectal metastases: A case–control study. Updates Surg. 2015, 67, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Ferrero, A.; Russolillo, N.; Langella, S.; Forchino, F.; Stasi, M.; Fazio, F.; Tesoriere, R.L. Ultrasound liver map technique for laparoscopic liver resections: Perioperative outcomes are not impaired by technical complexity. Updates Surg. 2019, 71, 49–56. [Google Scholar] [CrossRef]
- Russolillo, N.; Borello, A.; Langella, S.; Casella, M.; Tesoriere, R.L.; Ferrero, A. Comparison of laparoscopic ultrasound and liver-specific magnetic resonance imaging for staging colorectal liver metastases. Surg. Endosc. 2020, 35, 3547–3553. [Google Scholar] [CrossRef]
- Cho, J.Y. Outcomes of Laparoscopic Liver Resection for Lesions Located in the Right Side of the Liver. Arch. Surg. 2009, 144, 25–29. [Google Scholar] [CrossRef] [Green Version]
- Casciola, L.; Patriti, A.; Ceccarelli, G.; Bartoli, A.; Ceribelli, C.; Spaziani, A. Robot-assisted parenchymal-sparing liver surgery including lesions located in the posterosuperior segments. Surg. Endosc. 2011, 25, 3815–3824. [Google Scholar] [CrossRef]
- Pesi, B.; Moraldi, L.; Guerra, F.; Tofani, F.; Nerini, A.; Annecchiarico, M.; Coratti, A. Surgical and oncological outcomes after ultrasound-guided robotic liver resections for malignant tumor. Analysis of a prospective database. Int. J. Med. Robot. Comput. Assist. Surg. 2019, 15, e2002. [Google Scholar] [CrossRef] [PubMed]
- Guerra, F.; Guadagni, S.; Pesi, B.; Furbetta, N.; Di Franco, G.; Palmeri, M.; Annecchiarico, M.; Eugeni, E.; Coratti, A.; Patriti, A.; et al. Outcomes of robotic liver resections for colorectal liver metastases. A multi-institutional analysis of minimally invasive ultrasound-guided robotic surgery. Surg. Oncol. 2018, 28, 14–18. [Google Scholar] [CrossRef]
- Schneider, C.M.; Peng, P.D.; Taylor, R.H.; Dachs, G.W.; Hasser, C.J.; DiMaio, S.P.; Choti, M.A. Robot-assisted laparoscopic ultrasonography for hepatic surgery. Surgery 2012, 151, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Boctor, E.M.; Choti, M.A.; Burdette, E.C.; Webster, R.J., III. Three-dimensional ultrasound-guided robotic needle placement: An experimental evaluation. Int. J. Med. Robot. Comput. Assist. Surg. 2008, 4, 180–191. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Jia, Z.-Z.; Song, Z.-J.; Yang, X.-D.; Chen, K.; Liang, P. Three-dimensional ultrasound image-guided robotic system for accurate microwave coagulation of malignant liver tumours. Int. J. Med. Robot. Comput. Assist. Surg. 2010, 6, 256–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Majlesara, A.; Golriz, M.; Hafezi, M.; Saffari, A.; Stenau, E.; Maier-Hein, L.; Müller-Stich, B.P.; Mehrabi, A. Indocyanine green fluorescence imaging in hepatobiliary surgery. Photodiagnosis Photodyn. Ther. 2017, 17, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Reinhart, M.B.; Huntington, C.R.; Blair, L.J.; Heniford, B.T.; Augenstein, V.A. Indocyanine Green. Surg. Innov. 2015, 23, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Daskalaki, D.; Aguilera, F.; Patton, K.; Giulianotti, P.C. Fluorescence in robotic surgery. J. Surg. Oncol. 2015, 112, 250–256. [Google Scholar] [CrossRef]
- Handgraaf, H.; Boogerd, L.; Höppener, D.; Peloso, A.; Mulder, B.S.; Hoogstins, C.; Hartgrink, H.; van de Velde, C.; Mieog, J.; Swijnenburg, R.; et al. Long-term follow-up after near-infrared fluorescence-guided resection of colorectal liver metastases: A retrospective multicenter analysis. Eur. J. Surg. Oncol. 2017, 43, 1463–1471. [Google Scholar] [CrossRef] [PubMed]
- Marino, M.V.; Podda, M.; Fernandez, C.C.; Ruiz, M.G.; Fleitas, M.G. The application of indocyanine green-fluorescence imaging during robotic-assisted liver resection for malignant tumors: A single-arm feasibility cohort study. HPB 2020, 22, 422–431. [Google Scholar] [CrossRef]
- Van Der Vorst, J.R.; Schaafsma, B.E.; Hutteman, M.; Msc, F.P.R.V.; Liefers, G.-J.; Hartgrink, H.H.; Smit, V.T.H.B.M.; Löwik, C.W.G.M.; Van De Velde, C.J.H.; Frangioni, J.V.; et al. Near-infrared fluorescence-guided resection of colorectal liver metastases. Cancer 2013, 119, 3411–3418. [Google Scholar] [CrossRef]
- Hoekstra, L.T.; de Graaf, W.; Nibourg, G.A.A.; Heger, M.; Bennink, R.J.; Stieger, B.; van Gulik, T.M. Physiological and Biochemical Basis of Clinical Liver Function Tests. Ann. Surg. 2013, 257, 27–36. [Google Scholar] [CrossRef] [Green Version]
- Cheung, T.T.; Ma, K.W.; She, W.H.; Dai, W.C.; Tsang, S.H.Y.; Chan, A.C.Y.; Chok, K.S.H.; Lo, C.M. Pure laparoscopic hepatectomy with augmented reality-assisted indocyanine green fluorescence versus open hepatectomy for hepatocellular carcinoma with liver cirrhosis: A propensity analysis at a single center. Asian J. Endosc. Surg. 2018, 11, 104–111. [Google Scholar] [CrossRef] [Green Version]
- Chiow, A.K.H.; Rho, S.Y.; Wee, I.J.; Lee, L.S.; Choi, G.H. Robotic ICG guided anatomical liver resection in a multi-centre cohort: An evolution from “positive staining” into “negative staining” method. HPB 2020, 23, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Ishizawa, T.; Fukushima, N.; Shibahara, J.; Masuda, K.; Tamura, S.; Aoki, T.; Hasegawa, K.; Beck, Y.; Fukayama, M.; Kokudo, N. Real-time identification of liver cancers by using indocyanine green fluorescent imaging. Cancer 2009, 115, 2491–2504. [Google Scholar] [CrossRef] [PubMed]
- Boogerd, L.S.F.; Handgraaf, H.; Lam, H.-D.; Huurman, V.A.L.; Sarasqueta, A.F.; Frangioni, J.V.; Van De Velde, C.J.H.; Braat, A.E.; Vahrmeijer, A.L. Laparoscopic detection and resection of occult liver tumors of multiple cancer types using real-time near-infrared fluorescence guidance. Surg. Endosc. 2016, 31, 952–961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peloso, A.; Franchi, E.; Canepa, M.C.; Barbieri, L.; Briani, L.; Ferrario, J.; Bianco, C.; Quaretti, P.; Brugnatelli, S.; Dionigi, P.; et al. Combined use of intraoperative ultrasound and indocyanine green fluorescence imaging to detect liver metastases from colorectal cancer. HPB 2013, 15, 928–934. [Google Scholar] [CrossRef] [Green Version]
- Li, C.-G.; Zhou, Z.-P.; Tan, X.-L.; Wang, Z.-Z.; Liu, Q.; Zhao, Z.-M. Robotic resection of liver focal nodal hyperplasia guided by indocyanine green fluorescence imaging: A preliminary analysis of 23 cases. World J. Gastrointest. Oncol. 2020, 12, 1407–1415. [Google Scholar] [CrossRef]
- Mehdorn, A.-S.; Beckmann, J.; Braun, F.; Becker, T.; Egberts, J.-H. Usability of Indocyanine Green in Robot-Assisted Hepatic Surgery. J. Clin. Med. 2021, 10, 456. [Google Scholar] [CrossRef] [PubMed]
- Marino, M.V.; Di Saverio, S.; Podda, M.; Ruiz, M.G.; Fleitas, M.G. The Application of Indocyanine Green Fluorescence Imaging During Robotic Liver Resection: A Case-Matched Study. World J. Surg. 2019, 43, 2595–2606. [Google Scholar] [CrossRef]
- Okamoto, T.; Onda, S.; Yanaga, K.; Suzuki, N.; Hattori, A. Clinical application of navigation surgery using augmented reality in the abdominal field. Surg. Today 2014, 45, 397–406. [Google Scholar] [CrossRef]
- Meola, A.; Cutolo, F.; Carbone, M.; Cagnazzo, F.; Ferrari, M.; Ferrari, V. Augmented reality in neurosurgery: A systematic review. Neurosurg. Rev. 2016, 40, 537–548. [Google Scholar] [CrossRef]
- Jud, L.; Fotouhi, J.; Andronic, O.; Aichmair, A.; Osgood, G.; Navab, N.; Farshad, M. Applicability of augmented reality in orthopedic surgery—A systematic review. BMC Musculoskelet. Disord. 2020, 21, 103. [Google Scholar] [CrossRef]
- Ayoub, A.; Pulijala, Y. The application of virtual reality and augmented reality in Oral & Maxillofacial Surgery. BMC Oral Health 2019, 19, 238. [Google Scholar] [CrossRef] [Green Version]
- Teatini, A.; de Frutos, J.P.; Eigl, B.; Pelanis, E.; Aghayan, D.L.; Lai, M.; Kumar, R.P.; Palomar, R.; Edwin, B.; Elle, O.J. Influence of sampling accuracy on augmented reality for laparoscopic image-guided surgery. Minim. Invasive Ther. Allied Technol. 2020, 30, 229–238. [Google Scholar] [CrossRef] [Green Version]
- Kenngott, H.G.; Wagner, M.; Gondan, M.; Nickel, F.; Nolden, M.; Fetzer, A.; Weitz, J.; Fischer, L.; Speidel, S.; Meinzer, H.-P.; et al. Real-time image guidance in laparoscopic liver surgery: First clinical experience with a guidance system based on intraoperative CT imaging. Surg. Endosc. 2013, 28, 933–940. [Google Scholar] [CrossRef]
- Luo, H.; Yin, D.; Zhang, S.; Xiao, D.; He, B.; Meng, F.; Zhang, Y.; Cai, W.; He, S.; Zhang, W.; et al. Augmented reality navigation for liver resection with a stereoscopic laparoscope. Comput. Methods Programs Biomed. 2019, 187, 105099. [Google Scholar] [CrossRef]
- Nam, W.H.; Kang, D.-G.; Lee, D.; Lee, J.Y.; Ra, J.B. Automatic registration between 3D intra-operative ultrasound and pre-operative CT images of the liver based on robust edge matching. Phys. Med. Biol. 2011, 57, 69–91. [Google Scholar] [CrossRef]
- Kong, S.-H.; Haouchine, N.; Soares, R.; Klymchenko, A.S.; Andreiuk, B.; Marques, B.; Shabat, G.; Piechaud, T.; Diana, M.; Cotin, S.; et al. Robust augmented reality registration method for localization of solid organs’ tumors using CT-derived virtual biomechanical model and fluorescent fiducials. Surg. Endosc. 2016, 31, 2863–2871. [Google Scholar] [CrossRef] [Green Version]
- Vera, A.M.; Russo, M.; Mohsin, A.; Tsuda, S. Augmented reality telementoring (ART) platform: A randomized controlled trial to assess the efficacy of a new surgical education technology. Surg. Endosc. 2014, 28, 3467–3472. [Google Scholar] [CrossRef]
- Kowalewski, K.-F.; Garrow, C.; Proctor, T.; Preukschas, A.A.; Friedrich, M.; Müller, P.C.; Kenngott, H.G.; Fischer, L.; Müller-Stich, B.P.; Nickel, F. LapTrain: Multi-modality training curriculum for laparoscopic cholecystectomy—results of a randomized controlled trial. Surg. Endosc. 2018, 32, 3830–3838. [Google Scholar] [CrossRef]
- Lee, J.H.; Tanaka, E.; Woo, Y.; Ali, G.; Son, T.; Kim, H.; Hyung, W.J. Advanced real-time multi-display educational system (ARMES): An innovative real-time audiovisual mentoring tool for complex robotic surgery. J. Surg. Oncol. 2017, 116, 894–897. [Google Scholar] [CrossRef]
- Lai, E.C.; Tang, C.N. Training robotic hepatectomy: The Hong Kong experience and perspective. Hepatobiliary Surg. Nutr. 2017, 6, 222–229. [Google Scholar] [CrossRef] [Green Version]
- Fong, Y.; Buell, J.F.; Collins, J.; Martinie, J.; Bruns, C.; Tsung, A.; Clavien, P.-A.; Nachmany, I.; Edwin, B.; Pratschke, J.; et al. Applying the Delphi process for development of a hepatopancreaticobiliary robotic surgery training curriculum. Surg. Endosc. 2020, 34, 4233–4244. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giannone, F.; Felli, E.; Cherkaoui, Z.; Mascagni, P.; Pessaux, P. Augmented Reality and Image-Guided Robotic Liver Surgery. Cancers 2021, 13, 6268. https://doi.org/10.3390/cancers13246268
Giannone F, Felli E, Cherkaoui Z, Mascagni P, Pessaux P. Augmented Reality and Image-Guided Robotic Liver Surgery. Cancers. 2021; 13(24):6268. https://doi.org/10.3390/cancers13246268
Chicago/Turabian StyleGiannone, Fabio, Emanuele Felli, Zineb Cherkaoui, Pietro Mascagni, and Patrick Pessaux. 2021. "Augmented Reality and Image-Guided Robotic Liver Surgery" Cancers 13, no. 24: 6268. https://doi.org/10.3390/cancers13246268
APA StyleGiannone, F., Felli, E., Cherkaoui, Z., Mascagni, P., & Pessaux, P. (2021). Augmented Reality and Image-Guided Robotic Liver Surgery. Cancers, 13(24), 6268. https://doi.org/10.3390/cancers13246268





