Long-Term Outcomes of Lymph Node Transfer in Secondary Lymphedema and Its Correlation with Flap Characteristics
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
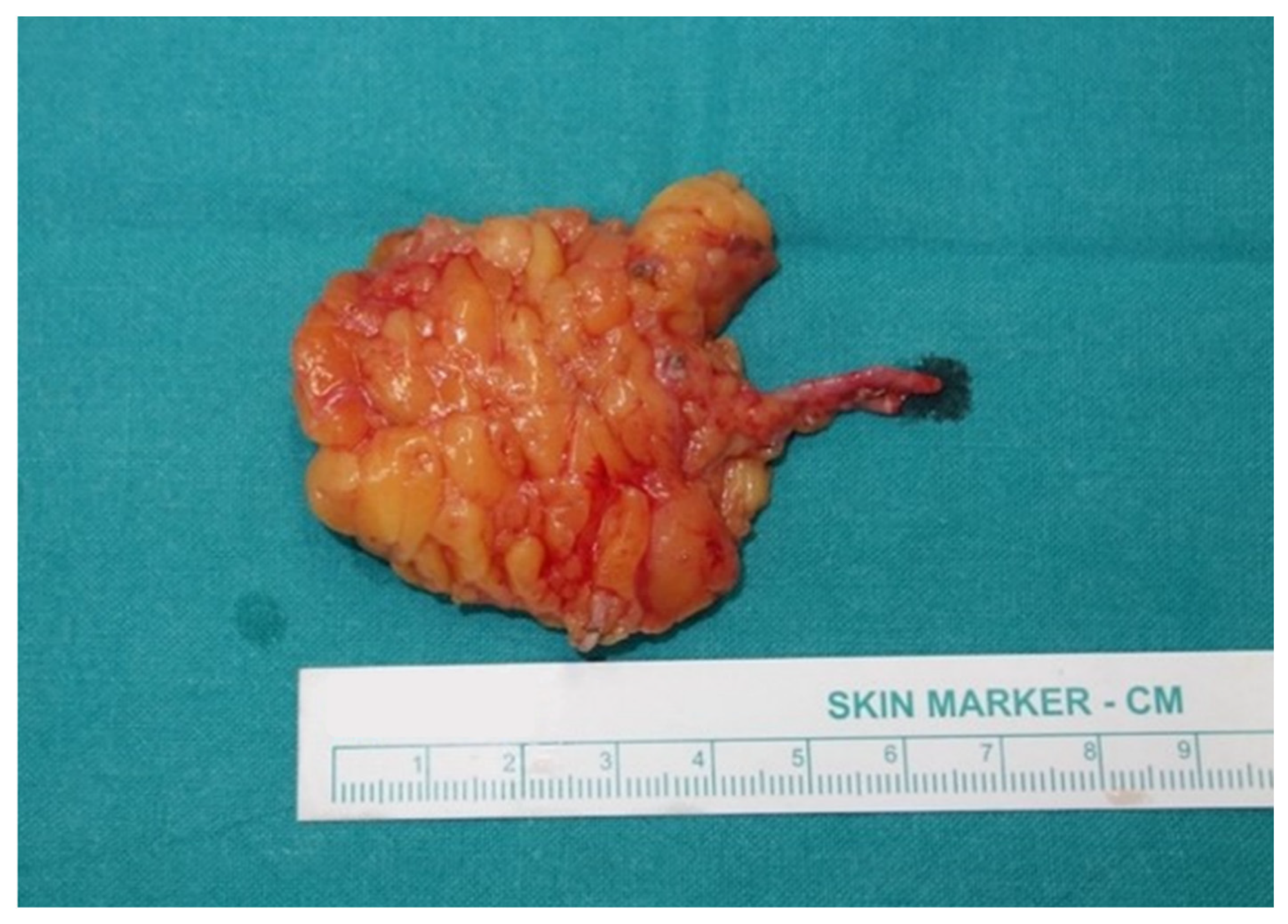
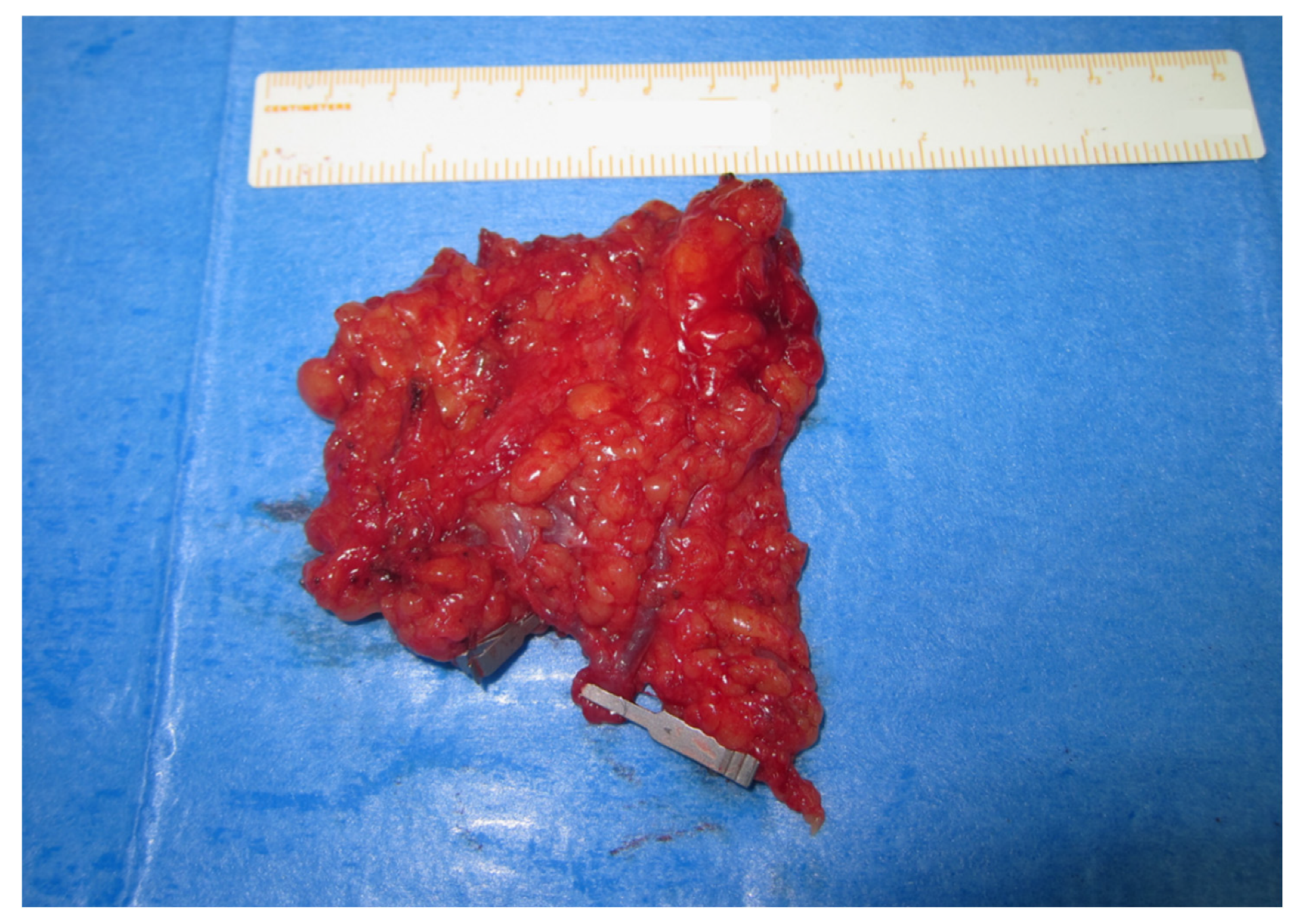
2.2. Treatment Protocol, Surgical Technique, and Management
2.3. Statistical Analysis
3. Results
3.1. Patients
3.2. Lymph Node Flap Characteristics—Correlation with Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Executive Committee of the International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology 2020, 53, 3–19. [Google Scholar]
- Szuba, A.; Rockson, S.G. Lymphedema: Classification, diagnosis and therapy. Vasc. Med. 1998, 3, 145–156. [Google Scholar] [CrossRef] [Green Version]
- Lee, B.B.; Andrade, M.; Antignani, P.L.; Boccardo, F.; Bunke, N.; Campisi, C.; Damstra, R.; Flour, M.; Forner-Cordero, I.; Gloviczki, P.; et al. Diagnosis and treatment of primary lymphedema. Consensus Document of the International Union of Phlebology (IUP)-2013. Int. Angiol. 2013, 32, 541–574. [Google Scholar] [PubMed]
- Damstra, R.J.; Voesten, H.G.; van Schelven, W.D.; van der Lei, B. Lymphatic venous anastomosis (LVA) for treatment of secondary arm lymphedema: A prospective study of 11 LVA procedures in 10 patients with breast cancer related lymphedema and a critical review of the literature. Breast Cancer Res. Treat. 2009, 113, 199–206. [Google Scholar] [CrossRef]
- Brennan, M.J.; DePompolo, R.W.; Garden, F.H. Focused review: Postmastectomy lymphedema. Arch. Phys. Med. Rehabil. 1996, 77, s74–s80. [Google Scholar] [CrossRef]
- Shih, Y.C.; Xu, Y.; Cormier, J.N.; Giordano, S.; Ridner, S.H.; Buchholz, T.A.; Perkins, G.H.; Elting, L.S. Incidence, treatment costs and complications of lymphedema after breast cancer among women of working age: A 2-year follow-up study. J. Clin. Oncol. 2009, 27, 2007–2014. [Google Scholar] [CrossRef]
- Becker, C.; Vasile, J.V.; Levine, J.L.; Batista, B.N.; Studinger, R.M.; Chen, C.M.; Riquet, M. Microlymphatic Surgery for the Treatment of Iatrogenic Lymphedema. Clin. Plast. Surg. 2012, 39, 385–398. [Google Scholar] [CrossRef] [PubMed]
- Viitanen, T.P.; Visuri, M.T.; Hartiala, P.; Mäki, M.T.; Seppänen, M.P.; Suominen, E.A.; Saaristo, A.M. Lymphatic Vessel Function and Lymphatic Growth Factor Secretion after Microvascular lymph Node Transfer in Lymphedema Patients. Plast. Reconstr. Surg. Glob. Open 2013, 1, 1–9. [Google Scholar] [CrossRef]
- Dionyssiou, D.; Demiri, E.; Tsimponis, A.; Sarafis, A.; Mpalaris, V.; Tatsidou, G.; Arsos, G. A randomized control study of treating secondary stage II breast cancer-related lymphoedema with free lymph node transfer. Breast Cancer Res. Treat. 2016, 156, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Ito, R.; Suami, H. Overview of Lymph Node Transfer for Lymphedema Treatment. Plast. Reconstr. Surg. 2014, 134, 548–556. [Google Scholar] [CrossRef]
- Demiri, E.; Dionyssiou, D.; Tsimponis, A.; Goula, O.C.; Mιlothridis, P.; Pavlidis, L.; Spyropoulou, G.A.; Foroglou, P. Donor Site Lymphedema following Lymph Node Transfer for Breast Cancer Related Lymphedema. A Systematic Review of the Literature. Lymphat. Res. Biol. 2018, 16, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Dionyssiou, D.; Demiri, E.; Sarafis, A.; Goula, C.O.; Tsimponis, A.; Arsos, G. Functional lymphatic reconstruction with the “Selected Lymph Node” technique guided by a SPECT-CT lymphoscintigraphy. J. Surg. Oncol. 2019, 120, 911–918. [Google Scholar] [CrossRef]
- Tourani, S.; Taylor, G.; Ashton, M. Vascularized Lymph Node Transfer: A Review of the Current Evidence. Plast. Reconstr. Surg. 2016, 137, 985–993. [Google Scholar] [CrossRef] [PubMed]
- Becker, C.; Assouad, J.; Riquet, M.; Hidden, G. Postmastectomy Lymphedema. Long-term Results Following Microsurgical Lymph Node Transplantation. Ann. Surg. 2006, 243, 313–315. [Google Scholar] [CrossRef]
- Brorson, H.; Hoijer, P. Standardized measurements used to order compression garments can be used to calculate arm volumes to evaluate lymphoedema treatment. J. Plast. Surg. Hand Surg. 2012, 46, 410–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garza, R., 3rd; Skoracki, R.; Hock, K.; Povoski, S.P. A comprehensive overview on the surgical management of secondary lymphedema of the upper and lower extremities related to prior oncologic therapies. BMC Cancer 2017, 17, 468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Brucker, B.; Zeltzer, A.; Seidenstuecker, K.; Hendrickx, B.; Adriaenssens, N.; Hamdi, M. Breast Cancer-Related Lymphedema: Quality of life after lymph node transfer. Plast. Recon. Surg. 2016, 137, 1673–1680. [Google Scholar] [CrossRef]
- Coriddi, M.; Dayan, J.; Sobti, N.; Nash, D.; Goldberg, J.; Klassen, A.; Pusic, A.; Mehrara, B. Systematic Review of Patient-Reported Outcomes following Surgical Treatment of Lymphedema. Cancers 2020, 12, 565. [Google Scholar] [CrossRef] [Green Version]
- Leung, N.; Furniss, D.; Giele, H. Modern surgical management of breast cancer therapy related upper limb and breast cancer lymphoedema. Maturitas 2015, 80, 384–390. [Google Scholar] [CrossRef]
- Patel, K.M.; Chu, S.Y.; Huang, J.J.; Wu, C.W.; Lin, C.Y.; Cheng, M.H. Preplanning Vascularized Lymph Node Transfer with Duplex Ultrasonography: An Evaluation of 3 Donor Sites. Plast. Recon. Surg. Glob. Open 2014, 2, e193. [Google Scholar] [CrossRef]
- Cheng, M.H.; Chen, S.C.; Henry, S.L.; Tan, B.K.; Lin, M.C.; Huang, J.J. Vascularized Groin Lymph Node Flap Transfer for Postmastecomy Upper Limb Lymphoedema: Flap Anatomy, Recipient Sites, and Outcomes. Plast. Recon. Surg. 2013, 131, 286–298. [Google Scholar] [CrossRef] [PubMed]
- Vignes, S.; Blanchard, M.; Yannoutsos, A.; Arrault, M. Complications of Autologous Lymph-node Transplantation for Limb Lymphoedema. Eur. J. Vasc. Endovasc. Surg. 2013, 45, 516–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scaglioni, M.F.; Arvanitakis, M.; Chen, Y.C.; Giovanoli, P.; Chia-Shen Yang, J.; Chang, E.I. Comprehensive review of vascularized lymph node transfers for lymphedema: Outcomes and complications. Microsurgery 2018, 38, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Cibula, D.; Borčinová, M.; Marnitz, S.; Jarkovský, J.; Klát, J.; Pilka, R.; Torné, A.; Zapardiel, I.; Petiz, A.; Lay, L.; et al. Lower-Limb Lymphedema after Sentinel Lymph Node Biopsy in Cervical Cancer Patients. Cancers 2021, 13, 2360. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Ali, R.; Chen, C.H.; Wallace, C.; Chang, Y.C.; Chen, H.C.; Cheng, M.H. Vascularized Groin Lymph Node Transfer Using the Wrist as a Recipient Site for Management of Postmastectomy Upper Extremity Lymphedema. Plast. Recon. Surg. 2009, 123, 1265–1275. [Google Scholar] [CrossRef] [Green Version]
- Spratt, J. Groin dissection. J. Surg. Oncol. 2000, 73, 243–262. [Google Scholar] [CrossRef]
- Gharb, B.B.; Rampazzo, A.; Spanio di Spilimbergo, S.; Xu, E.S.; Chung, K.P.; Chen, H.C. Vascularized lymph node transfer based on the hilar perforators improves the outcome in upper limb lymphedema. Ann. Plast. Surg. 2011, 67, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Becker, C.; (European University Hospital Georges-Pompidou, Paris, France). Personal communication, 2011.
- Saaristo, A.M.; Niemi, T.S.; Viitanen, T.P.; Tervala, T.V.; Hartiala, P.; Suominen, E.A. Microvascular Breast Reconstruction and Lymph Node Transfer for Postmastectomy Lymphedema Patients. Ann. Surg. 2012, 255, 468–473. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.I.; Ibrahim, A.; Liu, J.; Robe, C.; Suami, H.; Hanasono, M.M.; Nguyen, A.T. Optimizing Quality of Life for Patients with Breast Cancer Related Lymphedema: A Prospective Study Combining DIEP Flap Breast Reconstruction and Lymphedema Surgery. Plast. Recon. Surg. 2020, 145, 676e–685e. [Google Scholar] [CrossRef] [PubMed]
- Forte, A.; Cinotto, G.; Boczar, D.; Huayllani, M.T.; Lu, X.; Manrique, O.J.; McLaughlin, S.A. Lymph node transfer combined with deep inferior epigastric perforators and transverse rectus abdominis myocutaneous procedures: A systematic review. Gland. Surg. 2020, 9, 521–527. [Google Scholar] [CrossRef]

| Flap Size (cm2) | Number of LNs | Harvested Flap | Vascular Pedicle | Lymphedema Stage | Preop VD% | Postop VD% | VDR |
|---|---|---|---|---|---|---|---|
| 13.0 | 2 | LNT | SIEA | 2 | 23 | 12 | 48 |
| 13.3 | 2 | LNT | SIEA | 2 | 30 | 20 | 33 |
| 14.0 | 2 | LNT | SCIA | 1 | 15 | 8 | 47 |
| 14.4 | 2 | LNT | SCIA | 2 | 30 | 22 | 27 |
| 15.1 | 2 | LNT + FALD | SCIA | 1 | 16 | 12 | 25 |
| 16.1 | 3 | LNT | SCIA | 2 | 35 | 5 | 86 |
| 16.1 | 2 | LNT + DIEP | SCIA | 1 | 14 | 24 | −71 |
| 17.1 | 3 | LNT | SCIP | 1 | 11 | 2 | 82 |
| 17.1 | 3 | LNT | SCIA | 2 | 41 | 15 | 63 |
| 17.2 | 2 | LNT | SIEA | 1 | 26 | 21 | 19 |
| 18.1 | 3 | LNT | SCIP | 2 | 93 | 32 | 66 |
| 18.2 | 2 | LNT | SCIP | 2 | 27 | 22 | 18 |
| 19.7 | 3 | LNT | SCIP | 2 | 25 | 18 | 28 |
| 20.2 | 2 | LNT | SIEA | 2 | 49 | 21 | 57 |
| 20.7 | 3 | LNT + DIEP | SIEA | 2 | 28 | 17 | 39 |
| 20.7 | 2 | LNT | SCIP | 2 | 27 | 7 | 74 |
| 21.0 | 3 | LNT | SCIA | 2 | 27 | 17 | 37 |
| 21.2 | 2 | LNT | SCIP | 1 | 20 | 9 | 55 |
| 21.7 | 2 | LNT | SCIP | 2 | 21 | 7 | 67 |
| 21.8 | 4 | LNT + FALD | SCIA | 2 | 12 | 1 | 92 |
| 21.8 | 3 | LNT | SCIP | 3 | 31 | 13 | 58 |
| 22.0 | 3 | LNT | SIEA | 2 | 40 | 27 | 33 |
| 22.2 | 4 | LNT | SIEA | 2 | 30 | 8 | 73 |
| 22.4 | 5 | LNT | SIEA | 2 | 35 | 14 | 60 |
| 22.8 | 3 | LNT | SIEA | 3 | 28 | 2 | 93 |
| 23.2 | 4 | LNT | SCIA | 3 | 37 | 11 | 70 |
| 23.2 | 2 | LNT + DIEP | SIEA | 3 | 57 | 26 | 54 |
| 23.4 | 5 | LNT + DIEP | SIEA | 3 | 13 | 5 | 62 |
| 23.8 | 4 | LNT + DIEP | SIEA | 3 | 32 | 14 | 56 |
| 24.2 | 2 | LNT | SIEA | 3 | 27 | 14 | 48 |
| 24.4 | 3 | LNT | SCIA | 3 | 21 | 11 | 48 |
| 24.5 | 3 | LNT + DIEP | SIEA | 3 | 41 | 25 | 39 |
| 19.8 | 2.8 | 49.6 |
| Flap Size (cm2) | Number of LNs | Harvested Flap | Vascular Pedicle | Lymphedema Stage | Preop VD% | Postop VD% | VDR |
|---|---|---|---|---|---|---|---|
| 25.2 | 3 | LNT | SCIP | 1 | 38 | 16 | 58 |
| 25.5 | 4 | LNT | SCIA | 3 | 67 | 24 | 64 |
| 25.6 | 4 | LNT + FALD | SCIP | 1 | 12 | 3 | 75 |
| 26.6 | 4 | LNT + DIEP | SIEA | 1 | 30 | 13 | 57 |
| 27.2 | 3 | LNT + FALD | SCIA | 2 | 27 | 14 | 48 |
| 27.3 | 3 | LNT | SIEA | 3 | 63 | 26 | 59 |
| 27.3 | 2 | LNT | SIEA | 3 | 41 | 13 | 68 |
| 28.1 | 3 | LNT | SIEA | 1 | 16 | 4 | 75 |
| 28.4 | 3 | LNT + FALD | SCIP | 3 | 33 | 16 | 52 |
| 29.9 | 5 | LNT + DIEP | SCIA | 2 | 33 | 10 | 70 |
| 31.3 | 4 | LNT + FALD | SCIA | 2 | 18 | 4 | 78 |
| 31.6 | 3 | LNT | SIEA | 2 | 26 | 11 | 58 |
| 33.8 | 4 | LNT | SCIA | 2 | 29 | 18 | 38 |
| 34.5 | 4 | LNT | SCIP | 2 | 43 | 20 | 53 |
| 34.6 | 4 | LNT + DIEP | SIEA | 2 | 30 | 12 | 60 |
| 36.9 | 4 | LNT + DIEP | SIEA | 2 | 28 | 15 | 46 |
| 36.9 | 4 | LNT | SCIA | 2 | 44 | 19 | 57 |
| 37.0 | 3 | LNT | SCIA | 2 | 41 | 13 | 68 |
| 37.2 | 4 | LNT + DIEP | SCIA | 2 | 38 | 8 | 79 |
| 39.1 | 5 | LNT + DIEP | SCIA | 2 | 36 | 14 | 61 |
| 39.1 | 5 | LNT + DIEP | SCIA | 2 | 35 | 13 | 63 |
| 39.6 | 4 | LNT | SCIA | 3 | 39 | 13 | 67 |
| 39.6 | 4 | LNT | SIEA | 3 | 30 | 10 | 67 |
| 39.8 | 4 | LNT | SCIP | 2 | 35 | 17 | 51 |
| 39.8 | 4 | LNT | SCIA | 2 | 61 | 29 | 52 |
| 39.8 | 3 | LNT | SIEA | 2 | 31 | 13 | 58 |
| 40.6 | 4 | LNT | SCIP | 2 | 34 | 10 | 71 |
| 41.0 | 4 | LNT + DIEP | SIEA | 3 | 30 | 14 | 53 |
| 41.9 | 4 | LNT + DIEP | SIEA | 3 | 48 | 20 | 69 |
| 42.3 | 4 | LNT + DIEP | SCIP | 3 | 28 | 8 | 72 |
| 44.6 | 4 | LNT + DIEP | SCIP | 3 | 40 | 14 | 65 |
| 47.5 | 4 | LNT + DIEP | SIEA | 1 | 36 | 12 | 67 |
| 35.0 | 3.8 | 61.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dionyssiou, D.; Sarafis, A.; Tsimponis, A.; Kalaitzoglou, A.; Arsos, G.; Demiri, E. Long-Term Outcomes of Lymph Node Transfer in Secondary Lymphedema and Its Correlation with Flap Characteristics. Cancers 2021, 13, 6198. https://doi.org/10.3390/cancers13246198
Dionyssiou D, Sarafis A, Tsimponis A, Kalaitzoglou A, Arsos G, Demiri E. Long-Term Outcomes of Lymph Node Transfer in Secondary Lymphedema and Its Correlation with Flap Characteristics. Cancers. 2021; 13(24):6198. https://doi.org/10.3390/cancers13246198
Chicago/Turabian StyleDionyssiou, Dimitrios, Alexandros Sarafis, Antonios Tsimponis, Asterios Kalaitzoglou, Georgios Arsos, and Efterpi Demiri. 2021. "Long-Term Outcomes of Lymph Node Transfer in Secondary Lymphedema and Its Correlation with Flap Characteristics" Cancers 13, no. 24: 6198. https://doi.org/10.3390/cancers13246198
APA StyleDionyssiou, D., Sarafis, A., Tsimponis, A., Kalaitzoglou, A., Arsos, G., & Demiri, E. (2021). Long-Term Outcomes of Lymph Node Transfer in Secondary Lymphedema and Its Correlation with Flap Characteristics. Cancers, 13(24), 6198. https://doi.org/10.3390/cancers13246198






