The Vulvar Cancer Risk in Differentiated Vulvar Intraepithelial Neoplasia: A Systematic Review
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Study Selection
2.3. Data Extraction and Analysis
2.4. Critical Appraisal
3. Results
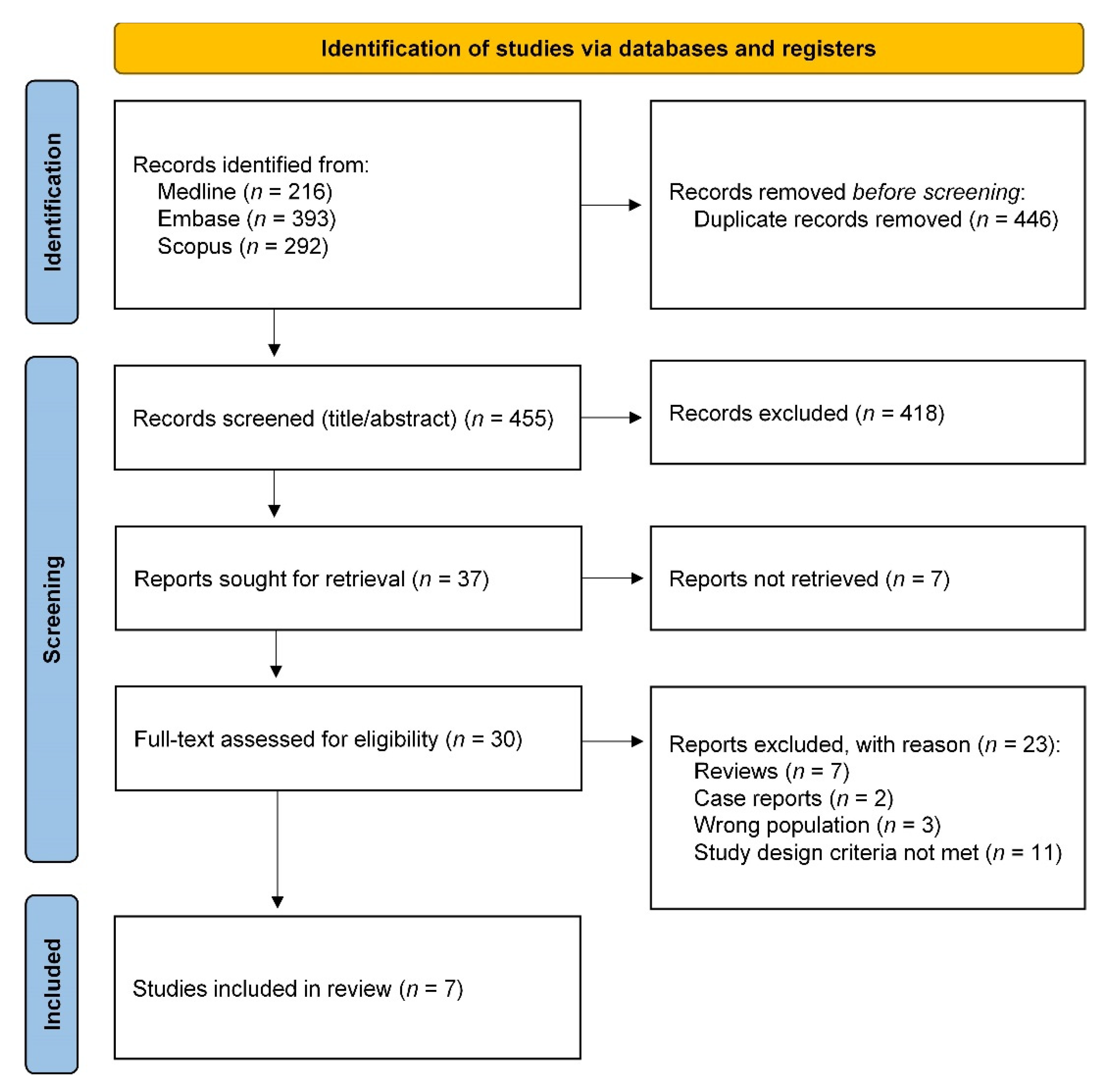
3.1. Search Results
3.2. Study Characteristics
3.3. Risk of Bias of All Included Studies
3.4. Outcome of Objectives
3.4.1. Primary VSCC Risk in dVIN
3.4.2. Recurrent VSCC Risk in dVIN
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cohen, P.A.; Anderson, L.; Eva, L.; Scurry, J. Clinical and molecular classification of vulvar squamous pre-cancers. Int. J. Gynecol. Cancer 2019, 29, 821–828. [Google Scholar] [CrossRef] [PubMed]
- De Sanjose, S.; Alemany, L.; Ordi, J.; Tous, S.; Alejo, M.; Bigby, S.M.; Joura, E.A.; Maldonado, P.; Laco, J.; Bravo, I.G.; et al. Worldwide human papillomavirus genotype attribution in over 2000 cases of intraepithelial and invasive lesions of the vulva. Eur. J. Cancer 2013, 49, 3450–3461. [Google Scholar] [CrossRef] [PubMed]
- Faber, M.T.; Sand, F.L.; Albieri, V.; Norrild, B.; Kjaer, S.K.; Verdoodt, F. Prevalence and type distribution of human papillomavirus in squamous cell carcinoma and intraepithelial neoplasia of the vulva. Int. J. Cancer 2017, 141, 1161–1169. [Google Scholar] [CrossRef] [Green Version]
- Hinten, F.; Molijn, A.; Eckhardt, L.; Massuger, L.; Quint, W.; Bult, P.; Bulten, J.; Melchers, W.J.G.; de Hullu, J.A. Vulvar cancer: Two pathways with different localization and prognosis. Gynecol. Oncol. 2018, 149, 310–317. [Google Scholar] [CrossRef]
- Nooij, L.S.; Ter Haar, N.T.; Ruano, D.; Rakislova, N.; van Wezel, T.; Smit, V.; Trimbos, B.; Ordi, J.; van Poelgeest, M.I.E.; Bosse, T. Genomic Characterization of Vulvar (Pre)cancers Identifies Distinct Molecular Subtypes with Prognostic Significance. Clin. Cancer Res. 2017, 23, 6781–6789. [Google Scholar] [CrossRef] [Green Version]
- Fehr, M.K.; Baumann, M.; Mueller, M.; Fink, D.; Heinzl, S.; Imesch, P.; Dedes, K. Disease progression and recurrence in women treated for vulvovaginal intraepithelial neoplasia. J. Gynecol. Oncol. 2013, 24, 236–241. [Google Scholar] [CrossRef] [Green Version]
- Thuijs, N.B.; van Beurden, M.; Bruggink, A.H.; Steenbergen, R.D.M.; Berkhof, J.; Bleeker, M.C.G. Vulvar intraepithelial neoplasia: Incidence and long-term risk of vulvar squamous cell carcinoma. Int. J. Cancer 2020, 148, 90–98. [Google Scholar] [CrossRef]
- Bigby, S.M.; Eva, L.J.; Fong, K.L.; Jones, R.W. The Natural History of Vulvar Intraepithelial Neoplasia, Differentiated Type: Evidence for Progression and Diagnostic Challenges. Int. J. Gynecol. Pathol. 2016, 35, 574–584. [Google Scholar] [CrossRef]
- Van Seters, M.; van Beurden, M.; de Craen, A.J. Is the assumed natural history of vulvar intraepithelial neoplasia III based on enough evidence? A systematic review of 3322 published patients. Gynecol. Oncol. 2005, 97, 645–651. [Google Scholar] [CrossRef]
- Allbritton, J.I. Vulvar Neoplasms, Benign and Malignant. Obstet. Gynecol. Clin. N. Am. 2017, 44, 339–352. [Google Scholar] [CrossRef] [PubMed]
- Abell, M.R.; Gosling, J.R. Intraepithelial and infiltrative carcinoma of vulva: Bowen’s type. Cancer 1961, 14, 318–329. [Google Scholar] [CrossRef]
- Wilkinson, E.J.; Kneale, B.; Lynch, P.J. Report of the Issvd Terminology Committee. J. Reprod. Med. 1986, 31, 973–974. [Google Scholar]
- Bornstein, J.; Bogliatto, F.; Haefner, H.K.; Stockdale, C.K.; Preti, M.; Bohl, T.G.; Reutter, J.; Committee, I.T. The 2015 International Society for the Study of Vulvovaginal Disease (ISSVD) Terminology of Vulvar Squamous Intraepithelial Lesions. J. Low Genit. Tract. Dis. 2016, 20, 11–14. [Google Scholar] [CrossRef]
- Hart, W.R. Vulvar intraepithelial neoplasia: Historical aspects and current status. Int. J. Gynecol. Pathol. 2001, 20, 16–30. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hayden, J.A.; van der Windt, D.A.; Cartwright, J.L.; Cote, P.; Bombardier, C. Assessing bias in studies of prognostic factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef]
- Te Grootenhuis, N.C.; Pouwer, A.W.; de Bock, G.H.; Hollema, H.; Bulten, J.; van der Zee, A.G.J.; de Hullu, J.A.; Oonk, M.H.M. Margin status revisited in vulvar squamous cell carcinoma. Gynecol. Oncol. 2019, 154, 266–275. [Google Scholar] [CrossRef]
- Van de Nieuwenhof, H.P.; Massuger, L.F.; van der Avoort, I.A.; Bekkers, R.L.; Casparie, M.; Abma, W.; van Kempen, L.C.; de Hullu, J.A. Vulvar squamous cell carcinoma development after diagnosis of VIN increases with age. Eur. J. Cancer 2009, 45, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Regauer, S.; Eberz, B.; Reich, O. Human Papillomavirus-Induced Squamous Intraepithelial Lesions in Vulvar Lichen Planus. J. Low Genit. Tract. Dis. 2016, 20, 360–364. [Google Scholar] [CrossRef]
- McAlpine, J.N.; Kim, S.Y.; Akbari, A.; Eshragh, S.; Reuschenbach, M.; von Knebel Doeberitz, M.; Prigge, E.S.; Jordan, S.; Singh, N.; Miller, D.M.; et al. HPV-independent Differentiated Vulvar Intraepithelial Neoplasia (dVIN) is Associated With an Aggressive Clinical Course. Int. J. Gynecol. Pathol. 2017, 36, 507–516. [Google Scholar] [CrossRef]
- Eva, L.J.; Ganesan, R.; Chan, K.K.; Honest, H.; Malik, S.; Luesley, D.M. Vulval squamous cell carcinoma occurring on a background of differentiated vulval intraepithelial neoplasia is more likely to recur: A review of 154 cases. J. Reprod. Med. 2008, 53, 397–401. [Google Scholar]
- Yang, B.; Hart, W.R. Vulvar intraepithelial neoplasia of the simplex (differentiated) type: A clinicopathologic study including analysis of HPV and p53 expression. Am. J. Surg. Pathol. 2000, 24, 429–441. [Google Scholar] [CrossRef]
- Nederlandse Vereniging voor Obstetrie en Gynaecologie. Landelijke Richtlijn Intra-Epitheliale Neoplasieën van de vulva (VIN). 2010. Available online: https://richtlijnendatabase.nl/richtlijn/vin (accessed on 23 August 2021).
- Lee, A.; Bradford, J.; Fischer, G. Long-term Management of Adult Vulvar Lichen Sclerosus: A Prospective Cohort Study of 507 Women. JAMA Dermatol. 2015, 151, 1061–1067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Werkgroep Oncologische Gynaecologie (WOG). Landelijke richtlijn Vulvacarcinoom. 2018. Available online: https://richtlijnendatabase.nl/richtlijn/vulvacarcinoom (accessed on 23 August 2021).
- Morrison, J.; Baldwin, P.; Buckley, L.; Cogswell, L.; Edey, K.; Faruqi, A.; Ganesan, R.; Hall, M.; Hillaby, K.; Reed, N.; et al. British Gynaecological Cancer Society (BGCS) vulval cancer guidelines: Recommendations for practice. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 502–525. [Google Scholar] [CrossRef]
- Oonk, M.H.M.; Planchamp, F.; Baldwin, P.; Bidzinski, M.; Brannstrom, M.; Landoni, F.; Mahner, S.; Mahantshetty, U.; Mirza, M.; Petersen, C.; et al. European Society of Gynaecological Oncology Guidelines for the Management of Patients With Vulvar Cancer. Int. J. Gynecol. Cancer 2017, 27, 832–837. [Google Scholar] [CrossRef] [PubMed]
- Kurman, R.J.; Carcangiu, M.L.; Herrington, C.S.; Young, R.H. WHO Classification of Tumours of Female Reproductive Organs, 4th ed.; International Agency for Research on Cancer: Lyon, France, 2014; Volume 6. [Google Scholar]
- Nascimento, A.F.; Granter, S.R.; Cviko, A.; Yuan, L.; Hecht, J.L.; Crum, C.P. Vulvar acanthosis with altered differentiation: A precursor to verrucous carcinoma? Am. J. Surg. Pathol. 2004, 28, 638–643. [Google Scholar] [CrossRef] [PubMed]
- Watkins, J.C.; Howitt, B.E.; Horowitz, N.S.; Ritterhouse, L.L.; Dong, F.; MacConaill, L.E.; Garcia, E.; Lindeman, N.I.; Lee, L.J.; Berkowitz, R.S.; et al. Differentiated exophytic vulvar intraepithelial lesions are genetically distinct from keratinizing squamous cell carcinomas and contain mutations in PIK3CA. Mod. Pathol. 2017, 30, 448–458. [Google Scholar] [CrossRef] [Green Version]
- Akbari, A.; Pinto, A.; Amemiya, Y.; Seth, A.; Mirkovic, J.; Parra-Herran, C. Differentiated exophytic vulvar intraepithelial lesion: Clinicopathologic and molecular analysis documenting its relationship with verrucous carcinoma of the vulva. Mod. Pathol. 2020, 33, 2011–2018. [Google Scholar] [CrossRef]
- Dasgupta, S.; Ewing-Graham, P.C.; van Kemenade, F.J.; van Doorn, H.C.; Noordhoek Hegt, V.; Koljenovic, S. Differentiated vulvar intraepithelial neoplasia (dVIN): The most helpful histological features and the utility of cytokeratins 13 and 17. Virchows Arch. 2018, 473, 739–747. [Google Scholar] [CrossRef] [Green Version]
- Jin, C.; Liang, S. Differentiated Vulvar Intraepithelial Neoplasia: A Brief Review of Clinicopathologic Features. Arch. Pathol. Lab. Med. 2019, 143, 768–771. [Google Scholar] [CrossRef] [Green Version]
- Reutter, J.C.; Walters, R.A.; Selim, M.A. Differentiated Vulvar Intraepithelial Neoplasia: What Criteria Do We Use in Practice? J. Low Genit. Tract. Dis. 2016, 20, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Van de Nieuwenhof, H.P.; Bulten, J.; Hollema, H.; Dommerholt, R.G.; Massuger, L.F.; van der Zee, A.G.; de Hullu, J.A.; van Kempen, L.C. Differentiated vulvar intraepithelial neoplasia is often found in lesions, previously diagnosed as lichen sclerosus, which have progressed to vulvar squamous cell carcinoma. Mod. Pathol. 2011, 24, 297–305. [Google Scholar] [CrossRef]
- Van den Einden, L.C.; de Hullu, J.A.; Massuger, L.F.; Grefte, J.M.; Bult, P.; Wiersma, A.; van Engen-van Grunsven, A.C.; Sturm, B.; Bosch, S.L.; Hollema, H.; et al. Interobserver variability and the effect of education in the histopathological diagnosis of differentiated vulvar intraepithelial neoplasia. Mod. Pathol. 2013, 26, 874–880. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoang, L.N.; Park, K.J.; Soslow, R.A.; Murali, R. Squamous precursor lesions of the vulva: Current classification and diagnostic challenges. Pathology 2016, 48, 291–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Study (Year) | Country | Study Design | Type of Cohort | Inclusion Period | Number and Type of Cases | Inclusion Criteria dVIN |
|---|---|---|---|---|---|---|
| Yang et al. (2000) [22] | USA | Retrospective cohort study | Center-based | NA | 8 dVIN 1 | Revision of pathology slides |
| Van de Nieuwenhof et al. (2009) [18] | The Netherlands | Retrospective cohort study | Population-based | 1992–2005 | 67 dVIN | Pathology reports describing dVIN as differentiated VIN, VIN simplex type, VIN NOS with LS and/or a high-risk HPV-negative result |
| Regauer et al. (2016) [19] | Austria | Retrospective cohort study | Center-based | 2004–2016 | 16 dVIN | Revision of pathology slides |
| Thuijs et al. (2020) [7] | The Netherlands | Retrospective cohort study | Population-based | 1991–2011 | 12 dVIN | Pathology reports describing dVIN as differentiated VIN, vulvar dystrophy with atypia or simplex VIN |
| McAlpine et al. (2017) [20] | Canada | Retrospective cohort study | Center-based | 1985–2005 | 7 dVIN18 dVIN/VSCC | Revision of pathology slides |
| Eva et al. (2008) [21] | UK | Retrospective cohort study | Center-based | 2000–2005 | 44 dVIN/VSCC | Pathology reports describing dVIN adjacent to VSCC |
| Te Grootenhuis et al. (2019) [17] | The Netherlands | Retrospective cohort study | Center-based | 2000–2010 | 197 dVIN/VSCC | Revision of pathology slides |
| Study (Year) | Study Participation | Study Attrition | Prognostic Factor Measurement | Outcome Measurement | Study Confounding | Statistical Analysis and Reporting |
|---|---|---|---|---|---|---|
| Yang et al. (2000) [22] | High | High | Moderate | Low | Moderate | Moderate |
| Van de Nieuwenhof et al. (2009) [18] | Low | Low | Moderate | Low | High | Low |
| Regauer et al. (2016) [19] | High | High | Moderate | High | High | High |
| Thuijs et al. (2020) [7] | Low | Low | Moderate | Low | High | Low |
| McAlpine et al. (2017) [20] | Low | Moderate | Low | Low | Moderate | Low |
| Eva et al. (2008) [21] | Moderate | High | Moderate | High | High | Moderate |
| Te Grootenhuis et al. (2019) [17] | Low | Moderate | Low | Low | Moderate | Low |
| Study (Year) | Number and Type of Cases | Age | Follow-Up Time | Primary VSCC Risk in dVIN | Recurrent VSCC Risk in dVIN/VSCC | ||||
|---|---|---|---|---|---|---|---|---|---|
| Risk of Primary VSCC | Time to Progression | Risk of Recurrent VSCC | Time to Progression | ||||||
| Years, Median (Range) | Months, Median (Range) | Number of Primary VSCC | Absolute Risk (%) | Months, Median (Range) | Number of Recurrent VSCC | Absolute Risk (%) | Months, Median (Range) | ||
| Yang et al. (2000) [22] | 8 dVIN 1 | 67.5 (55–82) | 48.5 (14–121) | 3 | 37.5 | 9 (6–55) | - | - | - |
| Van de Nieuwenhof et al. (2009) [18] | 67 dVIN | 67 | NA | 22 | 32.8 | 22.8 (3–84) | - | - | - |
| Regauer et al. (2016) [19] | 16 dVIN | NA | NA | 9 | 56.3 | NA | - | - | - |
| Thuijs et al. (2020) [7] | 12 dVIN | 70.3 (40.3–85.3) | 167 (4–329) 2 | 7 | 58.3 | 16.8 | - | - | - |
| McAlpine et al. (2017) [20] | 7 dVIN 18 dVIN/VSCC | 75.1 3 75.8 3 | 72 NA | 6 - | 85.7 - | 22.8 - | - 17 | - 94.4 | - 13.2 |
| Eva et al. (2008) [21] | 44 dVIN/VSCC | NA | NA | - | - | - | 14 | 31.8 | NA |
| Te Grootenhuis et al. (2019) [17] | 197 dVIN/VSCC | 73 (26–100) 4 | 80 (0–204) | - | - | - | 94 5 | 47.7 | 32 (0–202) 6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Voss, F.O.; Thuijs, N.B.; Vermeulen, R.F.M.; Wilthagen, E.A.; van Beurden, M.; Bleeker, M.C.G. The Vulvar Cancer Risk in Differentiated Vulvar Intraepithelial Neoplasia: A Systematic Review. Cancers 2021, 13, 6170. https://doi.org/10.3390/cancers13246170
Voss FO, Thuijs NB, Vermeulen RFM, Wilthagen EA, van Beurden M, Bleeker MCG. The Vulvar Cancer Risk in Differentiated Vulvar Intraepithelial Neoplasia: A Systematic Review. Cancers. 2021; 13(24):6170. https://doi.org/10.3390/cancers13246170
Chicago/Turabian StyleVoss, Féline O., Nikki B. Thuijs, Ravi F. M. Vermeulen, Erica A. Wilthagen, Marc van Beurden, and Maaike C. G. Bleeker. 2021. "The Vulvar Cancer Risk in Differentiated Vulvar Intraepithelial Neoplasia: A Systematic Review" Cancers 13, no. 24: 6170. https://doi.org/10.3390/cancers13246170
APA StyleVoss, F. O., Thuijs, N. B., Vermeulen, R. F. M., Wilthagen, E. A., van Beurden, M., & Bleeker, M. C. G. (2021). The Vulvar Cancer Risk in Differentiated Vulvar Intraepithelial Neoplasia: A Systematic Review. Cancers, 13(24), 6170. https://doi.org/10.3390/cancers13246170






