Small but Challenging Conjunctival Melanoma: New Insights, Paradigms and Future Perspectives
Abstract
Simple Summary
Abstract
1. Introduction
2. Method for Literature Search
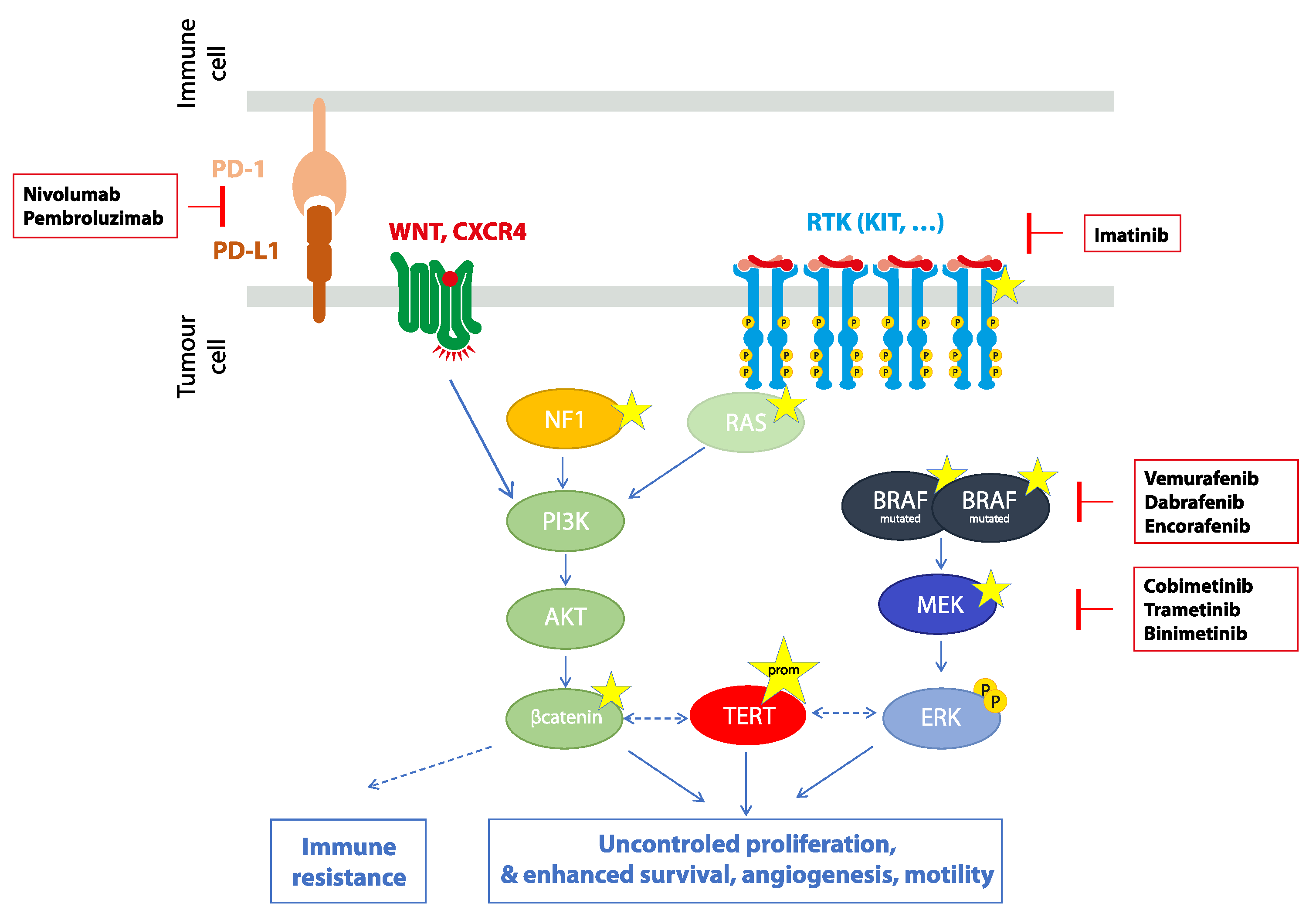
3. Biology of Conjunctival Melanoma
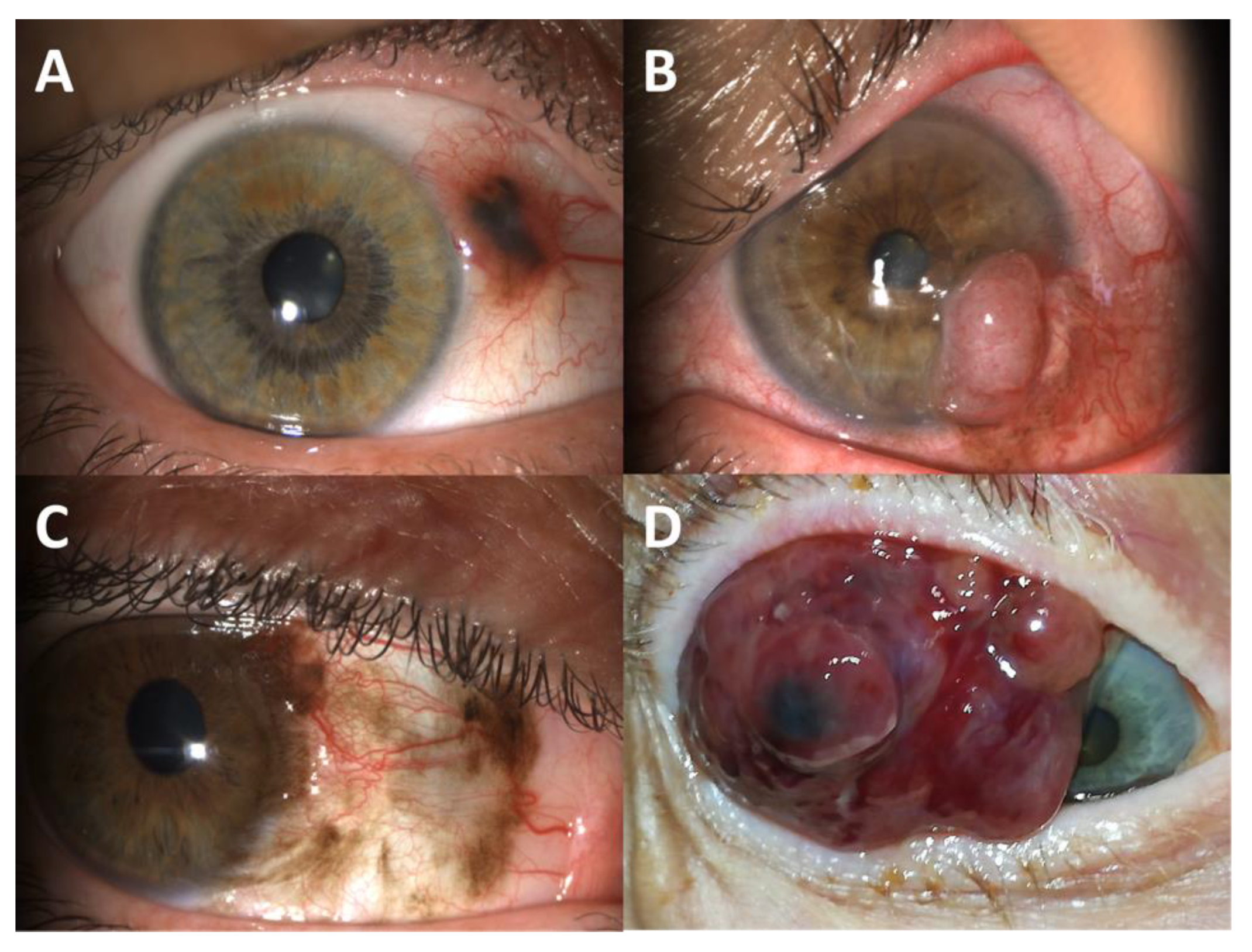
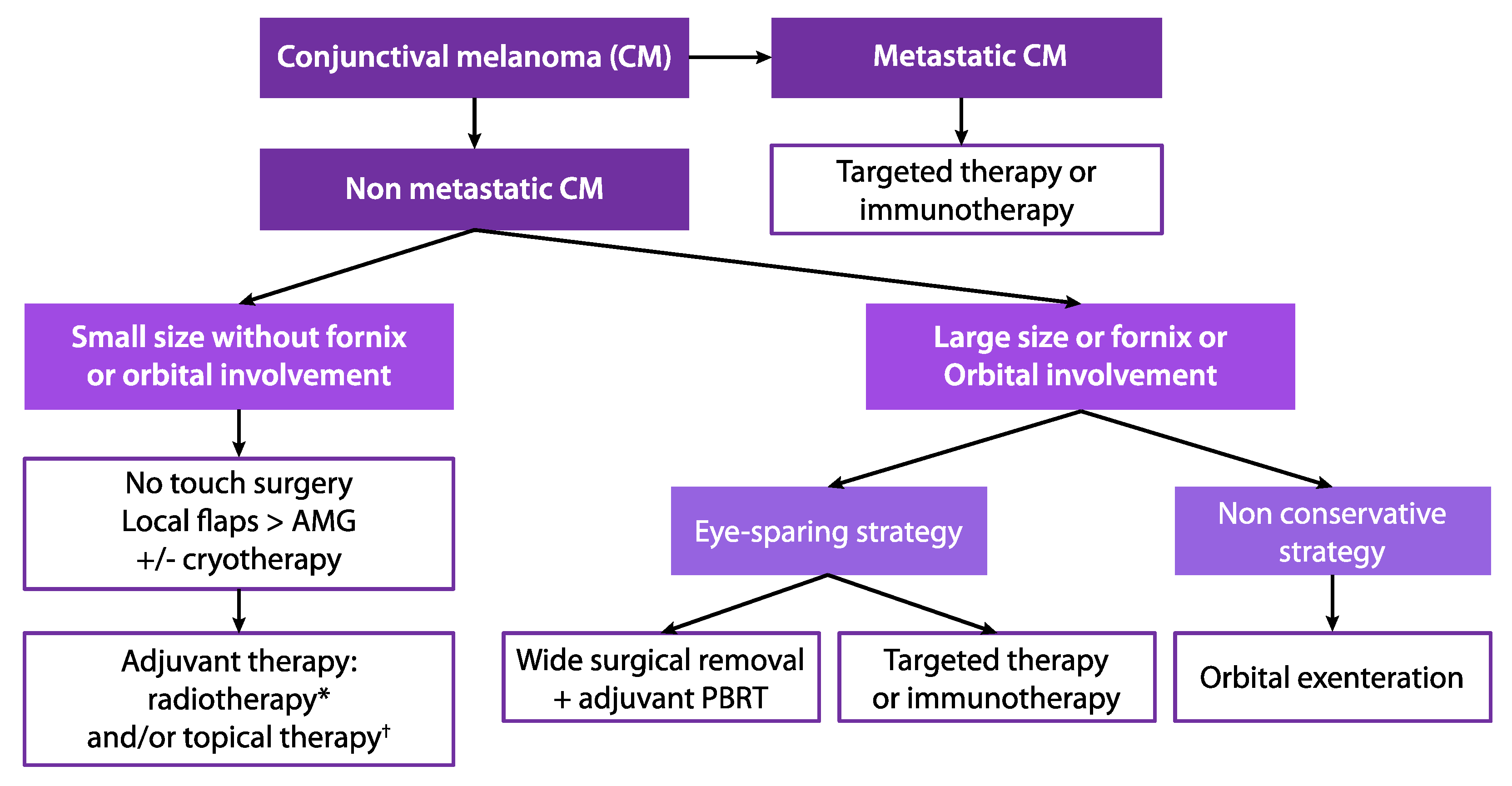
4. Conventional Treatment for Conjunctival Melanoma
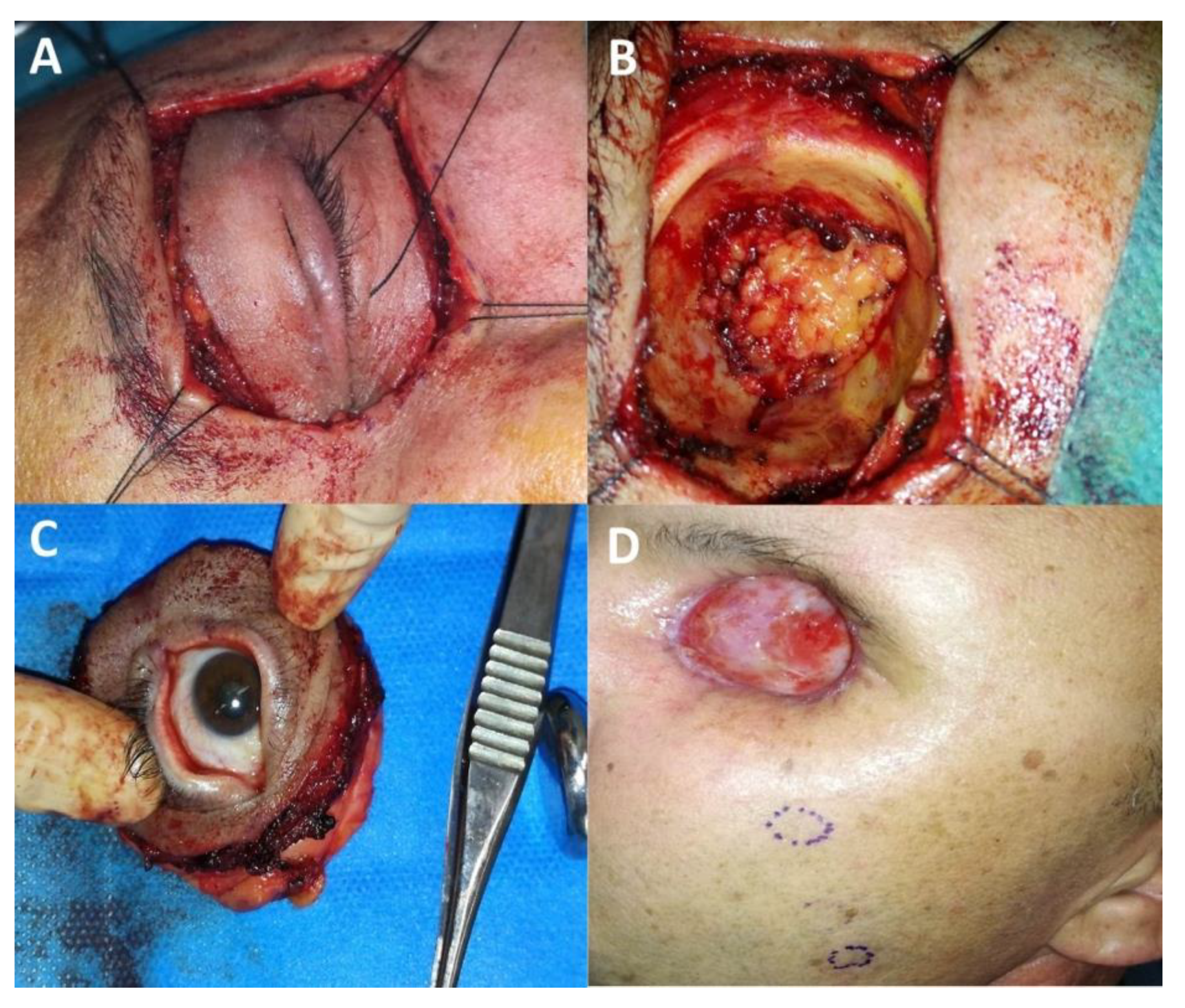
4.1. Surgery
4.2. Adjuvant Therapies
4.2.1. Cryotherapy
4.2.2. Topical Therapy
4.2.3. Adjuvant Radiotherapy
5. Orbital Exenteration for Conjunctival Melanoma
6. Future Perspectives
6.1. Avoiding Orbital Exenteration: Towards the Use of New Eye-Sparing Strategies
- (i)
- the tumour recurrence;
- (ii)
- and locally advanced tumours invading the fornix and/or the orbit.
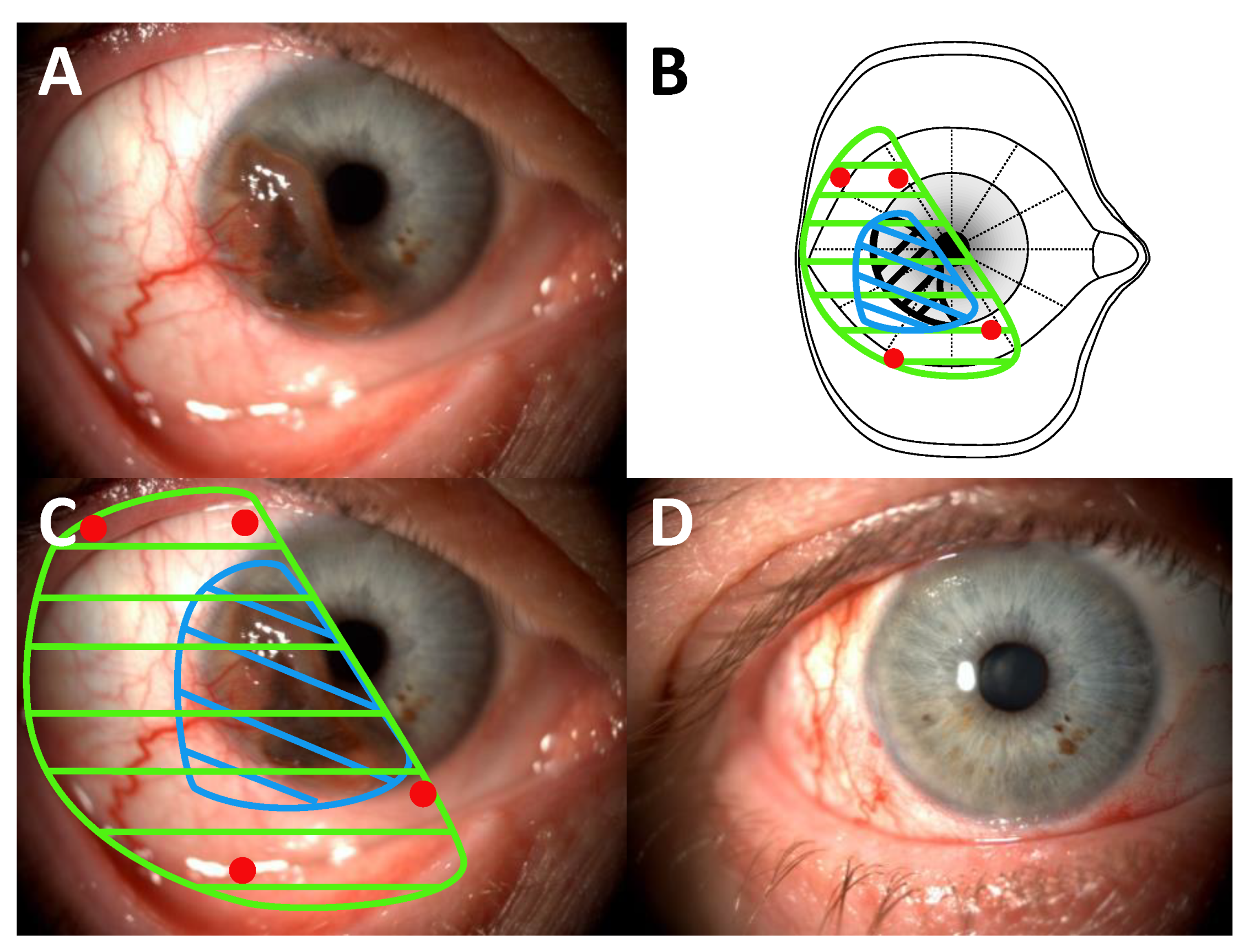
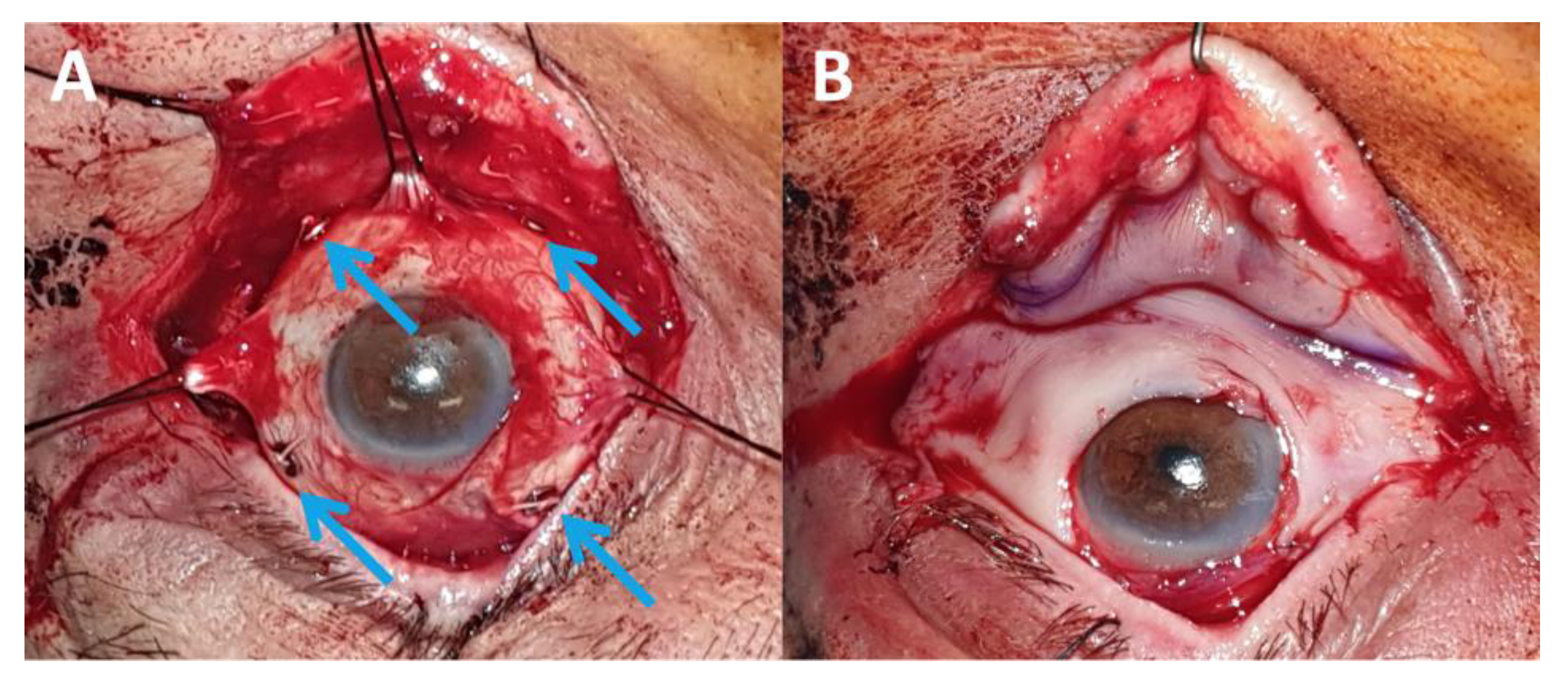
6.1.1. Surgical Excision Followed by Proton Beam Therapy
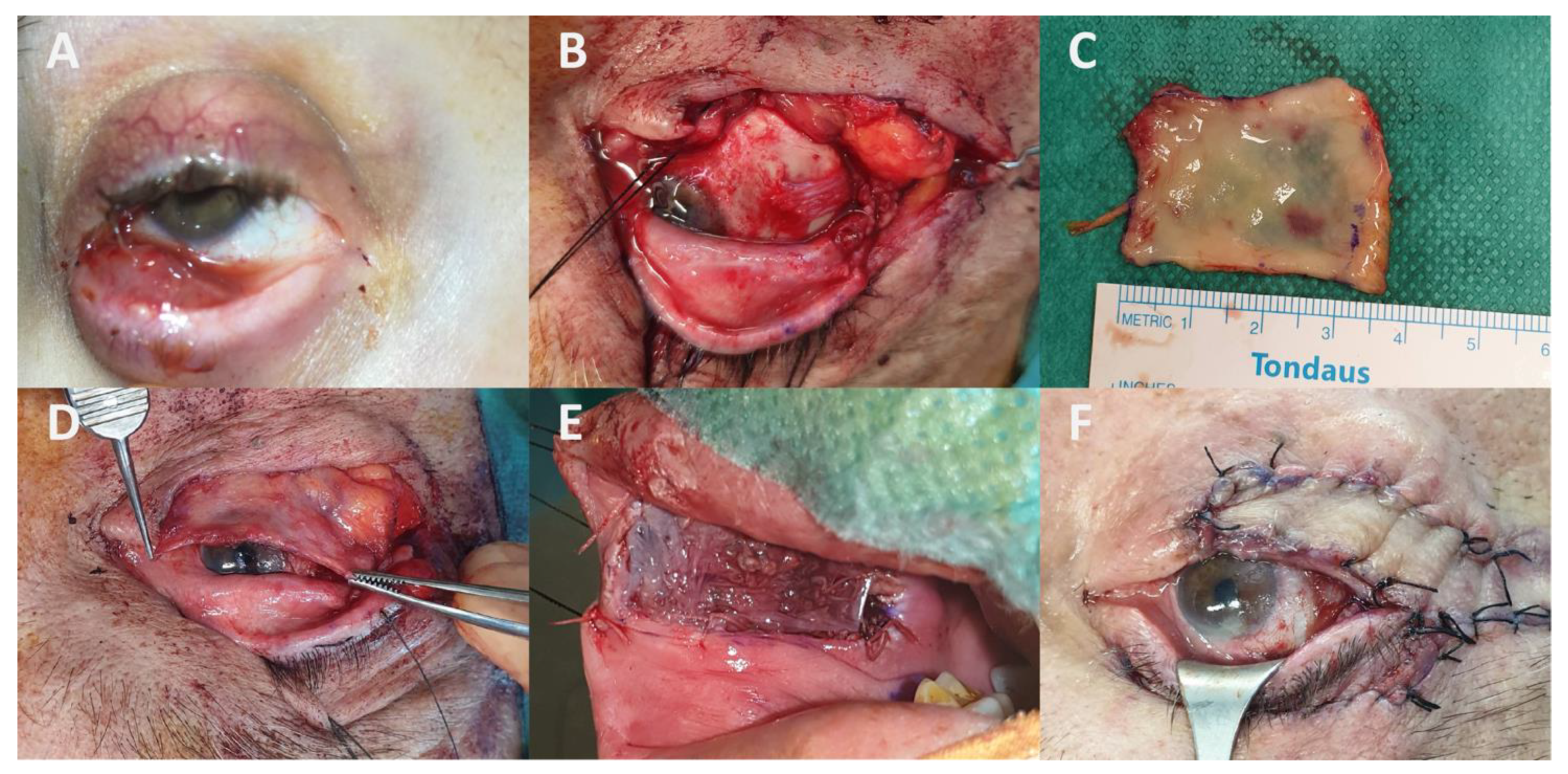
- a close cooperation between the ocular oncologist and the oculoplastic surgeon is essential;
- in the case of CM invading the fornix, the first surgical step is to perform inferior and/or superior cantholysis depending on tumour location to provide adequate surgical exposure (Figure 5);
- wide surgical removal with at least 5-mm free margins is recommended. The oculomotor muscles should be exposed and hooked if necessary. There is still no consensus on whether the anterior lid lamella should be preserved (Figure 5) or removed (Figure 6) in case of CM invading the fornix and the posterior lamella;
- data are currently scarce and are only based on retrospective studies;
- about one third of patients will experience tumour recurrence requiring revision surgeries +/− radiotherapy;
- although the globe is preserved, several patients will progressively lose their vision (secondary glaucoma, limbal cell deficiency); therefore, a distinction should be made between eye-sparing and sight-sparing strategies [98];
- not all CMs are eligible for conservative surgery.
6.1.2. Development of Targeted Therapies and Immunotherapies for Implementing New “Medical” Eye-Sparing Strategies
- the current literature is scarce and may be affected by a publication bias towards treatment. There is currently no ongoing clinical trial investigating MAPK inhibitors and immune checkpoint inhibitors in CM;
- not all CMs are targetable by BRAF and MEK inhibitors. Preliminary data indicate that NRAS-mutated CMs are relatively resistant to targeted therapies [114]. Therefore, only CM carrying a BRAF mutation can be treated with MAPK inhibitors;
- targeted therapy and immunotherapy adverse effects are frequently reported (in about 90% of patients treated with MAPK inhibitors) and can lead to treatment discontinuation;
- as with cutaneous melanoma, initial favourable responses have been reported followed by secondary relapses within a year, especially when BRAF or MEK inhibitors were given alone. Secondary resistance mechanisms are not yet elucidated and studies with a longer follow-up are needed to better assess their incidence in CM. Further studies assessing the rate of secondary resistance to combined BRAF and MEK inhibitors are also needed;
- treatment duration is not consensual;
- cost-effectiveness analyses are currently lacking;
- the treatment protocol remains to be established.
6.2. Treatment of Metastatic Conjunctival Melanoma
| Study | Patient Gender, Age | Disease Sites | Prior Treatments | Mutational Status | Drug, Dosage, Duration (months) | Follow-Up after Treatment (Months) | Clinical Outcome ‡ | Adverse Events (Grade) † |
|---|---|---|---|---|---|---|---|---|
| Targeted therapy | ||||||||
| Kiyohara et al., 2020 [119] | M, 72 | lymph node | lymph node dissection (parotidectomy) | BRAFV600E mutation | dabrafenib + trametinib, NR (6) | 0 (under treatment) | CR | NR |
| Rossi et al., 2019 [120] | M, 70 | lymph node | lymph node dissection (parotidectomy) | BRAFV600E mutation | dabrafenib + trametinib, 150 mg for 2 d + 2 mg for 1 d (8) | 0 (under treatment) | PR | fever hypertransaminasemia (1) |
| Pinto Torres et al., 2017 [118] | F, 56 | hematogenous (orophanryngeal wall) | surgery EBRT (20 Gy/5 fr) | BRAFV600 mutation | vemurafenib, 960 mg for 2d then 480 mg for 2 d due to AE (34) | 6 | CR developed breast cancer | skin rash (1) arthralgia (2) diarrhoea (2) |
| Maleka et al., 2016 [121] | F, 53 | hematogenous (orbit, brain, lung) | enucleation temozolomide (5 m) AdCD40L + cyclophosphamide whole brain EBRT (20 Gy/5 fr) | BRAFV600E mutation | vemurafenib, 960 mg for 2 d then 240 mg for 2 d due to AE (4) | 5 | Progression (for orbital location, PR for other locations) Death | skin rash (2) |
| Griewank et al., 2013 [122] | M, 43 | hematogenous (intramuscular, lungs, brain) | dacarbazine | BRAFV600 mutation | dabrafenib, NR (6) | NR | Progression (initial PR) | NR |
| Weber et al., 2013 [123] | M, 45 | hematogenous (subcutaneous, lungs, bone) | none | BRAFV600E mutation | vemurafenib, 960 mg for 2 d (3) | NR | Progression | NR |
| Immunotherapy | ||||||||
| Hong et al., 2021 [116] | M, 66 | hematogenous (lungs, liver) | none | NR | ipilimumab + nivolumab, 3 mg/kg + 1 mg/kg (6 cycles) | 4 | NR (response without detail) | hypopituitarism (2) |
| Chang et al., 2019 [44] | F, 60 | hematogenous (liver) | none | NRAS mutation | 1: ipilimumab + nivolumab, 3 mg/kg + 1 mg/kg (2 cycles) 2: ipilimumab, 240 mg (2 cycles) then 480 mg (1 cycle) 3: pembrolizumab, 200 mg (9 cycles) | 24 | NR (response without detail) | 1: hepatitis (3) 2: allergy (NR) 3: NR |
| Finger and Pavlik, 2019 [113] | F, 76 | lymph node | lymph node dissection (parotidectomy) + EBRT (cervical + mediastinal) | NRASQ61R mutation | 1: ipilimumab, 3 mg/kg (4 cycles) 2: surgery + EBRT + ipilimumab, 3 mg/kg (4 cycles) 3: surgery + EBRT (50 Gy/20 fr) + pembrolizumab, 2 mg/kg (14 cycles) | 24 | CR | NR |
| F, 72 | hematogenous (lungs, liver, bone, subcutaneous, node) | none | BRAFV600K mutation | ipilimumab + nivolumab, 3 mg/kg + 1 mg/kg (3 cycles) | 36 | CR | liver toxicity (2) colitis (3) pneumonitis (2) | |
| Chaves et al., 2018 [117] | M, 72 | lymph node | lymph node dissection (parotidectomy) | NR | ipilimumab, 3 mg/kg (4 cycles) | 16 | CR | fatigue (2) |
| Sagiv et al., 2018 [112] | F, 58 | hematogenous (lungs, liver) | none | NR | nivolumab, 3 mg/kg (6 cycles) | 9 | CR | biological hepatic failure (3) |
| F, 28 | hematogenous (breast, lungs, clavicle, thigh) | none | NR | nivolumab, 3 mg/kg (7 cycles) | 36 | CR | NR | |
| F, 47 | hematogenous (lungs) | none | NR | nivolumab, 3 mg/kg (10 cycles) | 7 | CR | colitis (3) diarrhoea (3) | |
| M, 74 | hematogenous (lungs) | none | NR | nivolumab, 3 mg/kg (22 cycles) | 1 | PR | colitis (3) | |
| Pinto Torres et al., 2017 [118] | M, 51 | lymph node | cervical lymphadenectomy antiviral therapy for HIV | no BRAF mutation | pembrolizumab, 2 mg/kg (12 cycles) | 0 (under treatment) | CR | NR |
| Combination therapy (immunotherapy and targeted therapy) | ||||||||
| Kiyohara et al., 2020 [119] | M, 71 | lumbar vertebra | Enucleation + vemurafenib | BRAFV600E mutation | 1: dabrafenib + trametinib, NR (6) 2: EBRT + nivolumab, NR (NR) 3: dabrafenib + trametinib, NR (NR) | NR | Death (24 months after initial treatment) | 1: skin rash (2) 2–3: NR |
| Sagiv et al., 2018 [112] | F, 68 | hematogenous (lungs) | none | no BRAFV600E mutation | 1: pembrolizumab, 2 m/kg (13 cycles) 2: ipilimumab + dacarbazine, 3 mg/kg + 800–1000 mg/m2 (2 cycles) | 0 | PR | 1: NR 2: hepatic failure (4) |
| Dagi Glass et al., 2017 [124] | F, 61 | lymph node | lymph node dissection (parotidectomy) + cervical lymphadenectomy | BRAFV600E mutation | 1: dabrafenib + trametinib, NR (1.5) 2: vemurafenib, NR (3.5) 3: pembrolizumab, NR (2) 4: vemurafenib, NR (4) 5: vemurafenib + cobimetinib, NR (24) | 0 (under treatment) | CR | 1: nausea (3) 2–5: NR |
6.3. Perspectives: Towards Personalized Treatment
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Zeng, Y.; Hu, C.; Shu, L.; Pan, Y.; Zhao, L.; Pu, X.; Wu, F. Clinical treatment options for early-stage and advanced conjunctival melanoma. Surv. Ophthalmol. 2021, 66, 461–470. [Google Scholar] [CrossRef]
- Seregard, S. Conjunctival Melanoma. Surv. Ophthalmol. 1998, 42, 321–350. [Google Scholar] [CrossRef]
- Isager, P.; Østerlind, A.; Engholm, G.; Heegaard, S.; Lindegaard, J.; Overgaard, J.; Storm, H.H. Uveal and Conjunctival Malignant Melanoma in Denmark, 1943–1997: Incidence and Validation Study. Ophthalmic Epidemiol. 2005, 12, 223–232. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, C.C.; Wu, X.-C.; Jemal, A.; Martin, H.J.; Roche, L.M.; Chen, V.W. Incidence of noncutaneous melanomas in the U.S. Cancer 2005, 103, 1000–1007. [Google Scholar] [CrossRef]
- Thariat, J.; Salleron, J.; Maschi, C.; Fevrier, E.; Lassalle, S.; Gastaud, L.; Baillif, S.; Claren, A.; Baumard, F.; Herault, J.; et al. Oncologic and visual outcomes after postoperative proton therapy of localized conjunctival melanomas. Radiat. Oncol. 2019, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Missotten, G.S.; Keijser, S.; De Keizer, R.J.W.; De Wolff-Rouendaal, D. Conjunctival Melanoma in The Netherlands: A Nationwide Study. Investig. Opthalmol. Vis. Sci. 2005, 46, 75–82. [Google Scholar] [CrossRef]
- Pacheco, R.R.; Yaghy, A.; Dalvin, L.A.; Vaidya, S.; Perez, A.L.; Lally, S.E.; Shields, J.A.; Shields, C.L. Conjunctival melanoma: Outcomes based on tumour origin in 629 patients at a single ocular oncology centre. Eye 2021, 1–9. [Google Scholar] [CrossRef]
- Martel, A.; Oberic, A.; Moulin, A.; Zografos, L.; Bellini, L.; Almairac, F.; Hamedani, M. Orbital exenteration and conjunctival melanoma: A 14-year study at the Jules Gonin Eye Hospital. Eye 2020, 34, 1897–1902. [Google Scholar] [CrossRef]
- Pandiani, C.; Beranger, G.; Leclerc, J.; Ballotti, R.; Bertolotto, C. Focus on cutaneous and uveal melanoma specificities. Genes Dev. 2017, 31, 724–743. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, M.; De Koning, L.; Coupland, S.E.; Jochemsen, A.G.; Marais, R.; Stern, M.-H.; Valente, A.; Barnhill, R.; Cassoux, N.; Evans, A.; et al. So Close, yet so Far: Discrepancies between Uveal and Other Melanomas. A Position Paper from UM Cure 2020. Cancers 2019, 11, 1032. [Google Scholar] [CrossRef]
- Scholz, S.L.; Cosgarea, I.; Süßkind, D.; Murali, R.; Möller, I.; Reis, H.; Leonardelli, S.; Schilling, B.; Schimming, T.; Hadaschik, E.; et al. NF1 mutations in conjunctival melanoma. Br. J. Cancer 2018, 118, 1243–1247. [Google Scholar] [CrossRef]
- Brouwer, N.J.; Verdijk, R.M.; Heegaard, S.; Marinkovic, M.; Esmaeli, B.; Jager, M.J. Conjunctival melanoma: New insights in tumour genetics and immunology, leading to new therapeutic options. Prog. Retin. Eye Res. 2021, 100971. [Google Scholar] [CrossRef]
- Ghazawi, F.M.; Darwich, R.; Le, M.; Jfri, A.; Rahme, E.; Burnier, J.V.; Sasseville, D.; Burnier, M.N., Jr.; Litvinov, I.V. Incidence trends of conjunctival malignant melanoma in Canada. Br. J. Ophthalmol. 2020, 104, 23–25. [Google Scholar] [CrossRef] [PubMed]
- Kaštelan, S.; Antunica, A.G.; Orešković, L.B.; Rabatić, J.S.; Kasun, B.; Bakija, I. Conjunctival Melanoma—Epidemiological Trends and Features. Pathol. Oncol. Res. 2018, 24, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Virgili, G.; Parravano, M.; Gatta, G.; Capocaccia, R.; Mazzini, C.; Mallone, S.; Botta, L.; RARECAREnet Working Group. Incidence and Survival of Patients With Conjunctival Melanoma in Europe. JAMA Ophthalmol. 2020, 138, 601–608. [Google Scholar] [CrossRef]
- Cisarova, K.; Folcher, M.; El Zaoui, I.; Pescini-Gobert, R.; Peter, V.G.; Royer-Bertrand, B.; Zografos, L.; Schalenbourg, A.; Nicolas, M.; Rimoldi, D.; et al. Genomic and transcriptomic landscape of conjunctival melanoma. PLoS Genet. 2020, 16, e1009201. [Google Scholar] [CrossRef] [PubMed]
- Griewank, K.G.; Murali, R.; Schilling, B.; Scholz, S.; Sucker, A.; Song, M.; Susskind, D.; Grabellus, F.; Zimmer, L.; Hillen, U.; et al. TERT promoter mutations in ocular melanoma distinguish between conjunctival and uveal tumours. Br. J. Cancer 2013, 109, 497–501. [Google Scholar] [CrossRef]
- Mikkelsen, L.H. Molecular biology in conjunctival melanoma and the relationship to mucosal melanoma. Acta Ophthalmol. 2020, 98 (Suppl. 115), 1–27. [Google Scholar] [CrossRef] [PubMed]
- Pleasance, E.D.; Cheetham, R.K.; Stephens, P.J.; McBride, D.J.; Humphray, S.J.; Greenman, C.D.; Varela, I.; Lin, M.-L.; Ordóñez, G.R.; Bignell, G.R.; et al. A comprehensive catalogue of somatic mutations from a human cancer genome. Nat. Cell Biol. 2009, 463, 191–196. [Google Scholar] [CrossRef]
- Mundra, P.A.; Dhomen, N.; Rodrigues, M.; Mikkelsen, L.H.; Cassoux, N.; Brooks, K.; Valpione, S.; Reis-Filho, J.S.; Heegaard, S.; Stern, M.-H.; et al. Ultraviolet radiation drives mutations in a subset of mucosal melanomas. Nat. Commun. 2021, 12, 259. [Google Scholar] [CrossRef]
- Gardrat, S.; Houy, A.; Brooks, K.; Cassoux, N.; Barnhill, R.; Dayot, S.; Bièche, I.; Raynal, V.; Baulande, S.; Marais, R.; et al. Definition of Biologically Distinct Groups of Conjunctival Melanomas According to Etiological Factors and Implications for Precision Medicine. Cancers 2021, 13, 3836. [Google Scholar] [CrossRef] [PubMed]
- Akbani, R.; Akdemir, K.C.; Aksoy, B.A.; Albert, M.; Ally, A.; Amin, S.; Arachchi, H.; Arora, A.; Auman, J.T.; Ayala, B.; et al. Genomic Classification of Cutaneous Melanoma. Cell 2015, 161, 1681–1696. [Google Scholar] [CrossRef] [PubMed]
- International Agency for Research on Cancer. WHO Classification of Skin Tumours, 4th ed.; Elder, D.E., Massi, D., Scolyer, R.A., Willemze, R., Eds.; World Health Organization Classification of Tumours; International Agency for Research on Cancer: Lyon, France, 2018. [Google Scholar]
- Griewank, K.; Westekemper, H.; Murali, R.; Mach, M.; Schilling, B.; Wiesner, T.; Schimming, T.; Livingstone, E.; Sucker, A.; Grabellus, F.; et al. Conjunctival Melanomas Harbor BRAF and NRAS Mutations and Copy Number Changes Similar to Cutaneous and Mucosal Melanomas. Clin. Cancer Res. 2013, 19, 3143–3152. [Google Scholar] [CrossRef] [PubMed]
- Beadling, C.; Jacobson-Dunlop, E.; Hodi, F.S.; Le, C.; Warrick, A.; Patterson, J.; Town, A.; Harlow, A.; Cruz, F.; Azar, S.; et al. KIT Gene Mutations and Copy Number in Melanoma Subtypes. Clin. Cancer Res. 2008, 14, 6821–6828. [Google Scholar] [CrossRef] [PubMed]
- Mikkelsen, L.H.; Maag, E.; Andersen, M.K.; Kruhøffer, M.; Larsen, A.-C.; Melchior, L.C.; Toft, P.B.; Von Buchwald, C.; Wadt, K.; Heegaard, S. The molecular profile of mucosal melanoma. Melanoma Res. 2020, 30, 533–542. [Google Scholar] [CrossRef] [PubMed]
- van Poppelen, N.; van Ipenburg, J.; Bosch, Q.V.D.; Vaarwater, J.; Brands, T.; Eussen, B.; Magielsen, F.; Dubbink, H.; Paridaens, D.; Brosens, E.; et al. Molecular Genetics of Conjunctival Melanoma and Prognostic Value of TERT Promoter Mutation Analysis. Int. J. Mol. Sci. 2021, 22, 5784. [Google Scholar] [CrossRef]
- Spranger, S.; Bao, R.; Gajewski, T.F. Melanoma-intrinsic β-catenin signalling prevents anti-tumour immunity. Nature 2015, 523, 231–235. [Google Scholar] [CrossRef]
- Luke, J.J.; Bao, R.; Sweis, R.F.; Spranger, S.; Gajewski, T.F. WNT/β-catenin Pathway Activation Correlates with Immune Exclusion across Human Cancers. Clin. Cancer Res. 2019, 25, 3074–3083. [Google Scholar] [CrossRef]
- Zimmermann, P.; Dietrich, T.; Bock, F.; Horn, F.K.; Hofmann-Rummelt, C.; EKruse, F.; Cursiefen, C. Tumour-associated lymphangiogenesis in conjunctival malignant melanoma. Br. J. Ophthalmol. 2009, 93, 1529–1534. [Google Scholar] [CrossRef]
- Heindl, L.M.; Hofmann-Rummelt, C.; Adler, W.; Bosch, J.J.; Holbach, L.M.; Naumann, G.O.H.; Kruse, F.E.; Cursiefen, C. Tumor-Associated Lymphangiogenesis in the Development of Conjunctival Melanoma. Investig. Opthalmol. Vis. Sci. 2011, 52, 7074–7083. [Google Scholar] [CrossRef]
- Briceño, C.A.; Elner, V.M.; Demirci, H. Lymphangiogenic and Chemotactic Factors in Conjunctival Melanoma. Ophthalmic Plast. Reconstr. Surg. 2016, 32, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Kakkassery, V.; Winterhalter, S.; Nick, A.-C.; Joachim, S.C.; Joussen, A.M.; Kociok, N. Vascular-Associated Muc4/Vwf Co-Localization in Human Conjunctival Malignant Melanoma Specimens—Tumor Metastasis by Migration? Curr. Eye Res. 2017, 42, 1382–1388. [Google Scholar] [CrossRef]
- Van Ipenburg, J.A.; De Waard, N.E.; Naus, N.C.; Jager, M.J.; Paridaens, D.; Verdijk, R.M. Chemokine Receptor Expression Pattern Correlates to Progression of Conjunctival Melanocytic Lesions. Investig. Ophthalmol. Vis. Sci. 2019, 60, 2950–2957. [Google Scholar] [CrossRef] [PubMed]
- Refaian, N.; Schlereth, S.L.; Koch, K.R.; Notara, M.; Hos, D.; Mescher, M.; Iden, S.; Bosch, J.J.; Jager, M.J.; Cursiefen, C. Comparing the Hem-and Lymphangiogenic Profile of Conjunctival and Uveal Melanoma Cell LinesHem-and Lymphangio-genic Profile of Ocular Melanomas. Investig. Ophthalmol. Vis. Sci. 2015, 56, 5691–5697. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.B. Conjunctival melanomas: Prognostic factors a review and an analysis of a series. Trans. Am. Ophthalmol. Soc. 1980, 78, 467–502. [Google Scholar]
- Folberg, R.; McLean, I.W.; Zimmerman, L.E. Malignant melanoma of the conjunctiva. Hum. Pathol. 1985, 16, 136–143. [Google Scholar] [CrossRef]
- Bobić-Radovanović, A.; Latković, Z.; Marinković, J.; Radovanović, Z. Predictors of Survival in Malignant Melanoma of the Conjunctiva: A Clinico-Pathological and Follow-up Study. Eur. J. Ophthalmol. 1998, 8, 4–7. [Google Scholar] [CrossRef]
- Anastassiou, G.; Esser, M.; Bader, E.; Steuhl, K.-P.; Bornfeld, N. Expression of cell adhesion molecules and tumour infiltrating leucocytes in conjunctival melanoma. Melanoma Res. 2004, 14, 381–385. [Google Scholar] [CrossRef]
- Tuomaala, S.; Toivonen, P.; Al-Jamal, R.; Kivelä, T. Prognostic Significance of Histopathology of Primary Conjunctival Melanoma in Caucasians. Curr. Eye Res. 2007, 32, 939–952. [Google Scholar] [CrossRef]
- Cao, J.; Brouwer, N.J.; Richards, K.E.; Marinkovic, M.; Van Duinen, S.; Hurkmans, D.P.; Verdegaal, E.M.E.; Jordanova, E.S.; Jager, M.J. PD-L1/PD-1 expression and tumor-infiltrating lymphocytes in conjunctival melanoma. Oncotarget 2017, 8, 54722–54734. [Google Scholar] [CrossRef]
- Cao, J.; Brouwer, N.J.; Jordanova, E.S.; Marinkovic, M.; Van Duinen, S.G.; De Waard, N.E.; Ksander, B.R.; Mulder, A.; Claas, F.H.J.; Heemskerk, M.H.M.; et al. HLA Class I Antigen Expression in Conjunctival Melanoma Is Not Associated With PD-L1/PD-1 Status. Investig. Ophthalmol. Vis. Sci. 2018, 59, 1005–1015. [Google Scholar] [CrossRef]
- Lassalle, S.; Nahon-Esteve, S.; Frouin, E.; Boulagnon-Rombi, C.; Josselin, N.; Cassoux, N.; Barnhill, R.; Scheller, B.; Baillif, S.; Hofman, P. PD-L1 Expression in 65 Conjunctival Melanomas and Its Association with Clinical Outcome. Int. J. Mol. Sci. 2020, 21, 9147. [Google Scholar] [CrossRef] [PubMed]
- Shields, C.L.; Chang, M.; Lally, S.E.; Dalvin, L.A.; Orloff, M.M. Conjunctival melanoma with orbital invasion and liver metastasis managed with systemic immune checkpoint inhibitor therapy. Indian J. Ophthalmol. 2019, 67, 2071–2073. [Google Scholar] [CrossRef]
- Shields, J.A.; Shields, C.L.; De Potter, P. Surgical Management of Conjunctival Tumors. Arch. Ophthalmol. 1997, 115, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Finger, P.T.; Milner, M.S.; McCormick, S.A. Topical chemotherapy for conjunctival melanoma. Br. J. Ophthalmol. 1993, 77, 751–753. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Paridaens, D.; Beekhuis, H.; Bosch, W.V.D.; Remeyer, L.; Melles, G. Amniotic membrane transplantation in the management of conjunctival malignant melanoma and primary acquired melanosis with atypia. Br. J. Ophthalmol. 2001, 85, 658–661. [Google Scholar] [CrossRef] [PubMed]
- Shields, C.L.; Shields, J.A.; Armstrong, T. Management of conjunctival and corneal melanoma with surgical excision, amniotic membrane allograft, and topical chemotherapy. Am. J. Ophthalmol. 2001, 132, 576–578. [Google Scholar] [CrossRef]
- Palamar, M.; Yaman, B.; Akalın, T.; Yağcı, A. Amniotic Membrane Transplantation in Surgical Treatment of Conjunctival Melanoma: Long-term Results. Turk. J. Ophthalmol. 2018, 48, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Finger, P.T.; Jain, P.; Mukkamala, S.K. Super-Thick Amniotic Membrane Graft for Ocular Surface Reconstruction. Am. J. Ophthalmol. 2019, 198, 45–53. [Google Scholar] [CrossRef]
- Damato, B.; Coupland, S. An audit of conjunctival melanoma treatment in Liverpool. Eye 2008, 23, 801–809. [Google Scholar] [CrossRef]
- Brouwer, N.J.; Marinkovic, M.; Peters, F.; Hulshof, M.C.C.M.; Pieters, B.R.; De Keizer, R.J.W.; Horeweg, N.; Laman, M.S.; Bleeker, J.C.; Van Duinen, S.G.; et al. Management of conjunctival melanoma with local excision and adjuvant brachytherapy. Eye 2021, 35, 490–498. [Google Scholar] [CrossRef]
- Savar, A.; Esmaeli, B.; Ho, H.; Liu, S.; Prieto, V.G. Conjunctival melanoma: Local-regional control rates, and impact of high-risk histopathologic features. J. Cutan. Pathol. 2010, 38, 18–24. [Google Scholar] [CrossRef]
- Freitag, S.K.; Aakalu, V.K.; Tao, J.P.; Wladis, E.J.; Foster, J.A.; Sobel, R.K.; Yen, M. Sentinel Lymph Node Biopsy for Eyelid and Conjunctival Malignancy. Ophthalmology 2020, 127, 1757–1765. [Google Scholar] [CrossRef] [PubMed]
- Shields, C.L.; Shields, J.A.; Gündüz, K.; Cater, J.; Mercado, G.V.; Gross, N.; Lally, B. Conjunctival MelanomaRisk Factors for Recurrence, Exenteration, Metastasis, and Death in 150 Consecutive Patients. Arch. Ophthalmol. 2000, 118, 1497–1507. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, M.L.; Ozgur, O.K.; Myers, J.N.; Peng, A.; Ning, J.; Zafereo, M.; Thakar, S.; Thuro, B.; Prieto, V.G.; Ross, M.I.; et al. Sentinel lymph node biopsy for ocular adnexal melanoma. Acta Ophthalmol. 2016, 95, e323–e328. [Google Scholar] [CrossRef] [PubMed]
- Cohen, V.; Tsimpida, M.; Hungerford, J.L.; Jan, H.; Cerio, R.; Moir, G. Prospective study of sentinel lymph node biopsy for conjunctival melanoma. Br. J. Ophthalmol. 2013, 97, 1525–1529. [Google Scholar] [CrossRef] [PubMed]
- Ho, V.H.; Ross, M.I.; Prieto, V.G.; Khaleeq, A.; Kim, S.; Esmaeli, B. Sentinel Lymph Node Biopsy for Sebaceous Cell Carcinoma and Melanoma of the Ocular Adnexa. Arch. Otolaryngol. –Head Neck Surg. 2007, 133, 820–826. [Google Scholar] [CrossRef]
- Tuomaala, S. Metastatic pattern and survival in disseminated conjunctival melanoma*1Implications for sentinel lymph node biopsy. Ophthalmology 2004, 111, 816–821. [Google Scholar] [CrossRef]
- Alonso, O.; Damian, A.; Engler, H.; Gaudiano, J. 18F-FDG PET-CT for Staging of Conjunctival Melanoma. World J. Nucl. Med. 2013, 12, 45–47. [Google Scholar] [CrossRef] [PubMed]
- Kurli, M.; Chin, K.; Finger, P.T. Whole-body 18 FDG PET/CT imaging for lymph node and metastatic staging of conjunctival melanoma. Br. J. Ophthalmol. 2008, 92, 479–482. [Google Scholar] [CrossRef]
- Scholz, S.L.; Hérault, J.; Stang, A.; Griewank, K.; Meller, D.; Thariat, J.; Steuhl, K.-P.; Westekemper, H.; Sauerwein, W. Proton radiotherapy in advanced malignant melanoma of the conjunctiva. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 257, 1309–1318. [Google Scholar] [CrossRef] [PubMed]
- Finger, P.T. Cryotherapy of Conjunctival Melanoma. Ophthalmology 1993, 100, 1429. [Google Scholar] [CrossRef]
- Jakobiec, F.A.; Rini, F.J.; Fraunfelder, F.T.; Brownstein, S. Cryotherapy for Conjunctival Primary Acquired Melanosis and Malignant Melanoma. Ophthalmology 1988, 95, 1058–1070. [Google Scholar] [CrossRef]
- Lommatzsch, P.K.; Lommatzsch, R.E.; Kirsch, I.; Fuhrmann, P. Therapeutic outcome of patients suffering from malignant melanomas of the conjunctiva. Br. J. Ophthalmol. 1990, 74, 615–619. [Google Scholar] [CrossRef] [PubMed]
- Jain, P.; Finger, P.T.; Fili, M.; Damato, B.; Coupland, S.E.; Heimann, H.; Kenawy, N.; Brouwer, N.J.; Marinkovic, M.; Van Duinen, S.G.; et al. Conjunctival melanoma treatment outcomes in 288 patients: A multicentre international data-sharing study. Br. J. Ophthalmol. 2020. [Google Scholar] [CrossRef]
- Damato, B.; Coupland, S.E. Management of conjunctival melanoma. Expert Rev. Anticancer. Ther. 2009, 9, 1227–1239. [Google Scholar] [CrossRef]
- Maschi-Cayla, C.; Doyen, J.; Gastaud, P.; Caujolle, J.P. Conjunctival melanomas and proton beam therapy. Acta Ophthalmol. 2013, 91, e647. [Google Scholar] [CrossRef][Green Version]
- Brouwer, N.J.; Marinkovic, M.; Van Duinen, S.G.; Bleeker, J.C.; Jager, M.J.; Luyten, G.P.M. Treatment of conjunctival melanoma in a Dutch referral centre. Br. J. Ophthalmol. 2018, 102, 1277–1282. [Google Scholar] [CrossRef]
- Larsen, A.-C.; Dahmcke, C.M.; Dahl, C.; Siersma, V.D.; Toft, P.B.; Coupland, S.; Prause, J.U.; Guldberg, P.; Heegaard, S. A Retrospective Review of Conjunctival Melanoma Presentation, Treatment, and Outcome and an Investigation of Features Associated WithBRAFMutations. JAMA Ophthalmol. 2015, 133, 1295–1303. [Google Scholar] [CrossRef]
- Cohen, V.M.L.; Papastefanou, V.P.; Liu, S.; Stoker, I.; Hungerford, J.L. The Use of Strontium-90 Beta Radiotherapy as Adjuvant Treatment for Conjunctival Melanoma. J. Oncol. 2013, 2013, 349162. [Google Scholar] [CrossRef]
- Karim, R.; Conway, R.M. Conservative resection and adjuvant plaque brachytherapy for early-stage conjunctival melanoma. Clin. Exp. Ophthalmol. 2011, 39, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Wuestemeyer, H.; Sauerwein, W.; Meller, D.; Chauvel, P.; Schueler, A.; Steuhl, K.-P.; Bornfeld, N.; Anastassiou, G. Proton radiotherapy as an alternative to exenteration in the management of extended conjunctival melanoma. Graefe’s Arch. Clin. Exp. Ophthalmol. 2006, 244, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Werschnik, C.; Lommatzsch, P.K. Long-Term Follow-up of Patients With Conjunctival Melanoma. Am. J. Clin. Oncol. 2002, 25, 248–255. [Google Scholar] [CrossRef]
- Anastassiou, G.; Heiligenhaus, A.; Bechrakis, N.; Bader, E.; Bornfeld, N.; Steuhl, K.-P. Prognostic value of clinical and histopathological parameters in conjunctival melanomas: A retrospective study. Br. J. Ophthalmol. 2002, 86, 163–167. [Google Scholar] [CrossRef]
- Ditta, L.C.; Shildkrot, Y.; Wilson, M.W. Outcomes in 15 Patients with Conjunctival Melanoma Treated with Adjuvant Topical Mitomycin C: Complications and Recurrences. Ophthalmology 2011, 118, 1754–1759. [Google Scholar] [CrossRef] [PubMed]
- Kurli, M.; Finger, P.T. Topical mitomycin chemotherapy for conjunctival malignant melanoma and primary acquired melanosis with atypia: 12 years’ experience. Graefe’s Arch. Clin. Exp. Ophthalmol. 2005, 243, 1108–1114. [Google Scholar] [CrossRef]
- Lee, D.A.; Lee, T.C.; Cortes, A.E.; Kitada, S. Effects of Mithramycin, Mitomycin, Daunorubicin, and Bleomycin on Human Subconjunctival Fibroblast Attachment and Proliferation. Investig. Ophthalmol. Vis. Sci. 1990, 31, 2136–2144. [Google Scholar]
- Yamamoto, T.; Varani, J.; Soong, H.K.; Lighter, P.R. Effects of 5-fluorouracil and Mitomycin C on Cultured Rabbit Subconjunctival Fibroblasts. Ophthalmology 1990, 97, 1204–1210. [Google Scholar] [CrossRef]
- Russell, H.C.; Chadha, V.; Lockington, D.; Kemp, E.G. Topical mitomycin C chemotherapy in the management of ocular surface neoplasia: A 10-year review of treatment outcomes and complications. Br. J. Ophthalmol. 2010, 94, 1316–1321. [Google Scholar] [CrossRef]
- Garip, A.; Schaumberger, M.M.; Wolf, A.; Herold, T.R.; Miller, C.V.; Klingenstein, A.; Schebitz-Walter, K.; Hintschich, C.R. Evaluation of a short-term topical interferon α-2b treatment for histologically proven melanoma and primary acquired melanosis with atypia. Orbit 2015, 35, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, I.; Kase, S.; Ishijima, K.; Ishida, S. Long-term follow-up of conjunctival melanoma treated with topical interferon alpha-2b eye drops as adjunctive therapy following surgical resection. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 2271–2276. [Google Scholar] [CrossRef] [PubMed]
- Coquard, R.; N’Guyen, A.; Mathis, T.; Josserand-Pietri, F.; Khodri, M.; Largeron, G.; Barbet, N.; Grange, J. Adjuvant contact radiotherapy for conjunctival malignancies: Preliminary results of a series of 14 patients treated with the Papillon 50 machine. Cancer Radiother. 2018, 22, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Martel, A.; Baillif, S.; Nahon-Esteve, S.; Gastaud, L.; Bertolotto, C.; Lassalle, S.; Lagier, J.; Hamedani, M.; Poissonnet, G. Orbital exenteration: An updated review with perspectives. Surv. Ophthalmol. 2021, 66, 856–876. [Google Scholar] [CrossRef] [PubMed]
- Martel, A.; Nahon-Esteve, S.; Gastaud, L.; Bertolotto, C.; Lassalle, S.; Baillif, S.; Charles, A. Incidence of Orbital Exenteration: A Nationwide Study in France over the 2006–2017 Period. Ophthalmic Epidemiol. 2021, 28, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Baum, S.H.; Oeverhaus, M.; Saxe, F.; Mohr, C. Modified types of orbital exenteration, survival, and reconstruction. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 2305–2312. [Google Scholar] [CrossRef]
- Aryasit, O.; Preechawai, P.; Kayasut, K. Clinical presentation, treatment, and prognosis of periocular and orbital amyloidosis in a university-based referral center. Clin. Ophthalmol. 2013, 7, 801–805. [Google Scholar] [CrossRef]
- Ali, M.J.; Pujari, A.; Dave, T.V.; Kaliki, S.; Naik, M.N. Clinicopathological profile of orbital exenteration: 14 years of experience from a tertiary eye care center in South India. Int. Ophthalmol. 2016, 36, 253–258. [Google Scholar] [CrossRef]
- Lemaître, S.; Lévy-Gabriel, C.; Dendale, R.; Vincent-Salomon, A.; Rouic, L.L.-L.; Cassoux, N.; Couturaud, B.; Desjardins, L. Secondary orbital exenteration for conjunctival melanoma: A study of 25 cases. J. Français D’ophtalmologie 2021, 44, 415–419. [Google Scholar] [CrossRef]
- Ben Simon, G.J.; Schwarcz, R.M.; Douglas, R.; Fiaschetti, D.; McCann, J.D.; Goldberg, R.A. Orbital exenteration: One size does not fit all. Am. J. Ophthalmol. 2005, 139, 11–17. [Google Scholar] [CrossRef]
- Kobayashi, K.; Mori, T.; Matsumoto, F.; Murakami, N.; Teshima, M.; Fukasawa, M.; Matsumoto, Y.; Matsumura, S.; Itami, J.; Asai, M.; et al. Impact of microscopic orbital periosteum invasion in orbital preservation surgery. Jpn. J. Clin. Oncol. 2017, 47, 321–327. [Google Scholar] [CrossRef]
- Jayaprakasam, A.; Vahdani, K.; Rose, G.E.; Saleh, G.M.; Hussain, B.; Verity, D.H.; Collin, J.R.O. Rapid Rehabilitation With Skin-Muscle Sparing Orbital Exenteration: A Single-Center Series. Ophthalmic Plast. Reconstr. Surg. 2021, 37, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Monjanel, B.; Baillif, S.; Lagier, J.; Gastaud, L.; Poissonnet, G.; Martel, A. Efficacy and safety of an artificial dermal graft for the reconstruction of exenterated sockets: A preliminary report. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 2827–2835. [Google Scholar] [CrossRef] [PubMed]
- Martel, A.; Oberic, A.; Bellini, L.; Almairac, F.; Moulin, A.; Hamedani, M. Is implant placement performed at the same surgical time as orbital exenteration a viable procedure? Int. J. Oral Maxillofac. Implant. 2020, 35, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Bi, Y.; Wu, S.; Zhao, Y.; Bai, S. A new method for fabricating orbital prosthesis with a CAD/CAM negative mold. J. Prosthet. Dent. 2013, 110, 424–428. [Google Scholar] [CrossRef]
- Gill, K.S.; Hsu, D.; Tassone, P.; Pluta, J.; Nyquist, G.; Krein, H.; Bilyk, J.; Murchison, A.P.; Iloreta, A.; Evans, J.J.; et al. Postoperative cerebrospinal fluid leak after microvascular reconstruction of craniofacial defects with orbital exenteration. Laryngoscope 2016, 127, 835–841. [Google Scholar] [CrossRef]
- Paridaens, A.D.; McCartney, A.C.; Minassian, D.C.; Hungerford, J.L. Orbital Exenteration in 95 Cases of Primary Conjunc-tival Malignant Melanoma. Br. J. Ophthalmol. 1994, 78, 520–528. [Google Scholar] [CrossRef]
- Martel, A.; Lassalle, S.; Picard-Gauci, A.; Gastaud, L.; Montaudie, H.; Bertolotto, C.; Nahon-Esteve, S.; Poissonnet, G.; Hofman, P.; Baillif, S. New Targeted Therapies and Immunotherapies for Locally Advanced Periocular Malignant Tumours: Towards a New ‘Eye-Sparing’ Paradigm? Cancers 2021, 13, 2822. [Google Scholar] [CrossRef]
- Shields, C.L.; Chien, J.L.; Surakiatchanukul, T.; Sioufi, K.; Lally, S.E.; Shields, J.A. Conjunctival Tumors: Review of Clinical Features, Risks, Biomarkers, and Outcomes—The 2017 J. Donald M. Gass Lecture. Asia-Pac. J. Ophthalmol. 2017, 6, 109–120. [Google Scholar] [CrossRef]
- Caujolle, J.-P.; Maschi, C.; Chauvel, P.; Herault, J.; Gastaud, P. Association chirurgie-protonthérapie dans le traitement des carcinomes invasifs et récidivants de la conjonctive: Technique et résultats préliminaires. J. Français D’ophtalmologie 2009, 32, 707–714. [Google Scholar] [CrossRef]
- Kumar, S.; Sugandhi, P.; Arora, R.; Pandey, P.K. Amniotic Membrane Transplantation Versus Mucous Membrane Grafting in Anophthalmic Contracted Socket. Orbit 2006, 25, 195–203. [Google Scholar] [CrossRef]
- Oliva, J.; Bardag-Gorce, F.; Niihara, Y. Clinical Trials of Limbal Stem Cell Deficiency Treated with Oral Mucosal Epithelial Cells. Int. J. Mol. Sci. 2020, 21, 411. [Google Scholar] [CrossRef] [PubMed]
- Sherif, M.; Oberic, A.; Tiple, S.; Hamedani, M. Use of Amniotic Membrane for Covering Large Oral Mucosal Defects during Socket Reconstruction Procedures. Klin. Mon. Für Augenheilkd. 2018, 235, 448–449. [Google Scholar] [CrossRef] [PubMed]
- Kar, I.; Singh, A.; Mohapatra, P.; Mohanty, P.; Misra, S. Repair of oral mucosal defects with cryopreserved human amniotic membrane grafts: Prospective clinical study. Int. J. Oral Maxillofac. Surg. 2014, 43, 1339–1344. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Nilsson, J.; Thor, A. Survival and complications of implants to support craniofacial prosthesis: A systematic review. J. Cranio-Maxillofac. Surg. 2016, 44, 1536–1552. [Google Scholar] [CrossRef]
- Leibovitch, I.; McNab, A.; Sullivan, T.; Davis, G.; Selva-Nayagam, D. Orbital Invasion by Periocular Basal Cell Carcinoma. Ophthalmology 2005, 112, 717–723. [Google Scholar] [CrossRef]
- Madge, S.N.; Khine, A.A.; Thaller, V.T.; Davis, G.; Malhotra, R.; McNab, A.; O’Donnell, B.; Selva, D. Globe-Sparing Surgery for Medial Canthal Basal Cell Carcinoma with Anterior Orbital Invasion. Ophthalmology 2010, 117, 2222–2228. [Google Scholar] [CrossRef]
- Larsen, A.-C.; Dahl, C.; Dahmcke, C.M.; Lade-Keller, J.; Siersma, V.D.; Toft, P.B.; Coupland, S.; Prause, J.U.; Guldberg, P.; Heegaard, S. BRAFmutations in conjunctival melanoma: Investigation of incidence, clinicopathological features, prognosis and paired premalignant lesions. Acta Ophthalmol. 2016, 94, 463–470. [Google Scholar] [CrossRef]
- Grimes, J.; Shah, N.V.; Samie, F.H.; Carvajal, R.D.; Marr, B.P. Conjunctival Melanoma: Current Treatments and Future Options. Am. J. Clin. Dermatol. 2020, 21, 371–381. [Google Scholar] [CrossRef]
- Long, G.V.; Hauschild, A.; Santinami, M.; Atkinson, V.; Mandalà, M.; Chiarion-Sileni, V.; Larkin, J.; Nyakas, M.; Dutriaux, C.; Haydon, A.; et al. Adjuvant Dabrafenib plus Trametinib in Stage IIIBRAF-Mutated Melanoma. N. Engl. J. Med. 2017, 377, 1813–1823. [Google Scholar] [CrossRef]
- Larkin, J.; Sileni, V.C.; Gonzalez, R.; Grob, J.-J.; Cowey, C.L.; Lao, C.D.; Schadendorf, D.; Dummer, R.; Smylie, M.; Rutkowski, P.; et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N. Engl. J. Med. 2015, 373, 23–34. [Google Scholar] [CrossRef]
- Sagiv, O.; Thakar, S.D.; Kandl, T.J.; Ford, J.; Sniegowski, M.C.; Hwu, W.-J.; Esmaeli, B. Immunotherapy With Programmed Cell Death 1 Inhibitors for 5 Patients With Conjunctival Melanoma. JAMA Ophthalmol. 2018, 136, 1236–1241. [Google Scholar] [CrossRef] [PubMed]
- Finger, P.T.; Pavlick, A.C. Checkpoint inhibition immunotherapy for advanced local and systemic conjunctival melanoma: A clinical case series. J. Immunother. Cancer 2019, 7, 83. [Google Scholar] [CrossRef]
- El Zaoui, I.; Bucher, M.; Rimoldi, D.; Nicolas, M.; Kaya, G.; Gobert, R.P.; Bedoni, N.; Schalenbourg, A.; Sakina, E.; Zografos, L.; et al. Conjunctival Melanoma Targeted Therapy: MAPK and PI3K/mTOR Pathways Inhibition. Investig. Ophthalmol. Vis. Sci. 2019, 60, 2764–2772. [Google Scholar] [CrossRef] [PubMed]
- Keilholz, U.; Ascierto, P.; Dummer, R.; Robert, C.; Lorigan, P.; van Akkooi, A.; Arance, A.; Blank, C.; Sileni, V.C.; Donia, M.; et al. ESMO consensus conference recommendations on the management of metastatic melanoma: Under the auspices of the ESMO Guidelines Committee. Ann. Oncol. 2020, 31, 1435–1448. [Google Scholar] [CrossRef] [PubMed]
- Hong, B.Y.-B.; Ford, J.R.; Glitza, I.C.; Cabala, C.A.T.; Tetzlaff, M.; Prieto, V.G.; Parker, R.; Daniel, C.; Esmaeli, B. Immune Checkpoint Inhibitor Therapy as an Eye-Preserving Treatment for Locally Advanced Conjunctival Melanoma. Ophthalmic Plast. Reconstr. Surg. 2021, 37, e9–e13. [Google Scholar] [CrossRef] [PubMed]
- Chaves, L.J.; Huth, B.; Augsburger, J.J.; Correa, Z.M. Eye-Sparing Treatment for Diffuse Invasive Conjunctival Melanoma. Ocul. Oncol. Pathol. 2018, 4, 261–266. [Google Scholar] [CrossRef]
- Torres, S.P.; André, T.; Gouveia, E.; Costa, L.; Passos, M.J. Systemic Treatment of Metastatic Conjunctival Melanoma. Case Rep. Oncol. Med. 2017, 2017, 4623964. [Google Scholar] [CrossRef]
- Kiyohara, T.; Tanimura, H.; Miyamoto, M.; Shijimaya, T.; Nagano, N.; Nakamaru, S.; Makimura, K.; Iwai, H. Two cases of BRAF-mutated, bulbar conjunctival melanoma, and review of the published literature. Clin. Exp. Dermatol. 2020, 45, 207–211. [Google Scholar] [CrossRef]
- Rossi, E.; Maiorano, B.A.; Pagliara, M.M.; Sammarco, M.G.; Dosa, T.; Martini, M.; Rindi, G.; Bria, E.; Blasi, M.A.; Tortora, G.; et al. Dabrafenib and Trametinib in BRAF Mutant Metastatic Conjunctival Melanoma. Front. Oncol. 2019, 9, 232. [Google Scholar] [CrossRef]
- Maleka, A.; Åström, G.; Byström, P.; Ullenhag, G.J. A case report of a patient with metastatic ocular melanoma who experienced a response to treatment with the BRAF inhibitor vemurafenib. BMC Cancer 2016, 16, 634. [Google Scholar] [CrossRef]
- Griewank, K.; Westekemper, H.; Schilling, B.; Livingstone, E.; Schimming, T.; Sucker, A.; Hillen, U.; Steuhl, K.-P.; Zimmer, L.; Schadendorf, D. Conjunctival Melanomas Harbor BRAF and NRAS Mutations—Response. Clin. Cancer Res. 2013, 19, 6331–6332. [Google Scholar] [CrossRef] [PubMed]
- Weber, J.L.; Smalley, K.; Sondak, V.K.; Gibney, G.T. Conjunctival Melanomas Harbor BRAF and NRAS Mutations—Letter. Clin. Cancer Res. 2013, 19, 6329–6330. [Google Scholar] [CrossRef]
- Glass, L.R.D.; Lawrence, D.P.; Jakobiec, F.A.; Freitag, S.K. Conjunctival Melanoma Responsive to Combined Systemic BRAF/MEK Inhibitors. Ophthalmic Plast. Reconstr. Surg. 2017, 33, e114–e116. [Google Scholar] [CrossRef] [PubMed]
- Durante, M.A.; Rodriguez, D.A.; Kurtenbach, S.; Kuznetsov, J.N.; Sanchez, M.I.; Decatur, C.L.; Snyder, H.; Feun, L.G.; Livingstone, A.S.; Harbour, J.W. Single-cell analysis reveals new evolutionary complexity in uveal melanoma. Nat. Commun. 2020, 11, 496. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, J.; Nilsson, L.M.; Mitra, S.; Alsén, S.; Shelke, G.V.; Sah, V.R.; Forsberg, E.M.V.; Stierner, U.; All-Eriksson, C.; Einarsdottir, B.; et al. Molecular profiling of driver events in metastatic uveal melanoma. Nat. Commun. 2020, 11, 1894. [Google Scholar] [CrossRef]
- Pandiani, C.; Strub, T.; Nottet, N.; Cheli, Y.; Gambi, G.; Bille, K.; Husser, C.; Dalmasso, M.; Béranger, G.; Lassalle, S.; et al. Single-cell RNA sequencing reveals intratumoral heterogeneity in primary uveal melanomas and identifies HES6 as a driver of the metastatic disease. Cell Death Differ. 2021, 28, 1990–2000. [Google Scholar] [CrossRef]
- Strub, T.; Martel, A.; Nahon-Esteve, S.; Baillif, S.; Ballotti, R.; Bertolotto, C. Translation of single-cell transcriptomic analysis of uveal melanomas to clinical oncology. Prog. Retin. Eye Res. 2021, 100968. [Google Scholar] [CrossRef]

| Study | Cases | Follow-Up in Months (Mean (Range)) | cTNM (n (%)) | Origin of the Tumour (n (%)) | Thickness (mm) (Mean (Range)) | Adjuvant Therapy after Primary Surgery (with or without Cryotherapy) (n (%)) | Target of Initial Treatment | 5-Year Local Recurrence Rates, % |
|---|---|---|---|---|---|---|---|---|
| Pacheco et al., 2021 [7] | 629 | 58 (<1–336) | n = 425 (100) T1 = 266 (63) T2 = 75 (18) T3 = 80 (20) | n = 629 (100) PAM = 476 (76) Naevus = 59 (9) De novo = 94 (15) | n = 476 2.7 (0.2–20.0) | n = 30 (5) † - Topical CT (MMC) = 19 (3) - Topical IT (IFN-a2b) = 1 (<1) - RT = 10 (2)
| NR | Overall = NR PAM = 40 Naevus = 28 De novo = 42 |
| Brouwer et al., 2021 [52] | 58 | 97.3 (9.3–229) | n = 58 (100) T1 = 57 (98) T2 = 1 (2) | n = 58 (100) PAM = 52 (90) | n = 58 0.9 (NR) | n = 58 (100) - Topical CT (MMC) = 15 (26) - RT (plaque) = 58 (100) | - On site = 20 (34) - Other site = 38 (66) | Overall = 21 |
| Jain et al., 2020 [66] | 288 | 52.8 (1–171) | n = 288 (100) T1 = 218 (76) T2 = 34 (12) T3 = 15 (5) Tx = 21 (7) | NR | n = 271 1.9 (0.2–16) | n = 199 (69) - Topical CT = 109 (38)
- RT = 106 (37)
| NR | Overall = 19 |
| Thariat et al., 2019 [5] | 92 | 56.4 (NR) | n = 88 (100) T1 = 63 (72) T2 = 13 (15) T3 = 12 (13) | n = 92 (100) PAM = 60 (65) | n = 92 2.5 (1.0–4.0) | n = 92 (100) - Topical CT (MMC) = 22 (24) - RT (PBRT) = 92 (100) | - On site = 42 (46) - Other site = 50 (54) | Overall = 33 |
| Scholz et al., 2019 [62] | 89 | 50.4 (1–260) | n = 89 (100) T1c/d= 5 (6) T2 = 49 (55) T3 = 35 (39) | n = 89 (100) PAM = 53 (60) | NR | n = 89 (100) - Topical CT = 22 (25) - RT = 89 (100)
- Combination b = 4 (5) | NR | NR |
| Brouwer et al., 2018 [69] | 70 | 70.2 (3–172) | n = 70 (100) T1 = 54 (77) T2 = 16 (23) | n = 70 (100) PAM = 65 (93) | n = 54 2.3 (NR) | n = 39 (56) - Topical CT (MMC) = 1 (1) - RT = 38 (54)
| - On site = 48 (69) - Other site = 22 (31) | Overall = 29 |
| Larsen et al., 2015 [70] | 132 | 73.2 (4–528) | n = 47 (100) T1 = 32 (68) T2 = 11 (23) T3 = 4 (9) | n = 129 (100) PAM = 80 (62) Naevus = 33 (26) Naevus + PAM = 2 (2) De novo = 14 (11) | NR | n = 18 (14) ‡ - Topical CT = 3 (2) - RT (plaque) = 15 (12) | NR | NR |
| Cohen et al., 2013 [71] | 20 | 59 (8–152) | n = 20 (100) T1 = 20 (100) | PAM = 15 (75) De novo = 5 (25) | n = 17 2.1 (0.6–6) | n = 20 (100) - Topical CT (MMC) = 1 (5) - RT (plaque) = 20 (100) | NR | Overall = 18 |
| Karim and Conway, 2011 [72] | 19 | 43.1 (30–54) | n = 19 (100) T1 = 19 (100) | PAM = 19 (100) | n = 19 0.7 (median) (0.2–1.6) | n = 19 (100) - RT (plaque) = 19 (100) | NR | 0 |
| Savar et al., 2011 [53] | 26 | 32 (2.4–84) | n = 26 (100) T1 = 9 (35) T2 = 10 (38) T3 = 7 (27) | NR | n = 23 2.7 (0.23–12) | n = 9 (35) - Topical CT (MMC) = 5 (19) - Topical IT (IFN-a2b) = 1 (4) - RT (EBRT) = 3 (12) | - On site = 20 (69) - Other site = 6 (21) | Overall = 9 |
| Damato and Coupland, 2009 [51] | 76 | 52.8 (median) for patients initially treated on site 38.4 (median) (8–167) for referred patients | NR a | NR | NR | NR | - On site = 40 (53) - Other site = 36 (47) | NR |
| Wuestemeyer et al., 2006 [73] | 20 | 38.1 (NR) | n = 20 (100) T1 = 2 (10) T2 = 14 (70) T3 = 4 (20) | PAM = 2 (10) De novo = 2 (10) NR = 16 (80) (recurrence) | NR | n = 20 (100) - Topical CT = 2 (10) - RT = 4 (20)
- Combination b = 2 (10) | NR | Overall = 40 (but mortality at 3 years) |
| Missotten et al., 2005 [6] | 194 | 81.6 (1–618) | NR a | n = 194 (100) PAM = 111 (57) Naevus = 3 (2) Naevus + PAM = 9 (5) De novo = 50 (26) Inconclusive = 21 (11) | n = 152 2.07 (NR) | n = 35 (18) - Topical CT = 4 (2) - RT = 31 (16)
| NR | Overall = 39 |
| Tuomaala et al., 2002 [40] | 85 | 75.6 (3–396) | NR a | n = 77 (100) PAM = 53 (69) Naevus = 23 (30) NR = 1 (1) | n = 72 1.3 (0.2–8.8) | n = 6 (7) - Topical CT = 5 (6) | NR | Overall = 36 |
| Werschnik and Lommatzsch, 2002 [74] | 85 | 165.6 (NR) | n = 85 (100) T1 = 48 (56) T2 = 37 (44) | n = 85 (100) PAM = 22 (26) Naevus = 29 (34) De novo = 34 (40) | NR | n = 38 (45) c - RT (plaque) = 38 (45) | NR | Overall = 40 |
| Anastassiou et al., 2002 [75] | 69 | 67 (median) (15–360) | NR a | n = 69 (100) PAM = 29 (42) Naevus = 27 (39) De novo = 11 (16) Inconclusive = 2 (3) | NR | n = 40 (58) - Topical CT = 3 (4) - RT = 34 (49)
- Combination b = 1 (1) | NR | NR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nahon-Estève, S.; Bertolotto, C.; Picard-Gauci, A.; Gastaud, L.; Baillif, S.; Hofman, P.; Groulier, A.; Maschi, C.; Caujolle, J.-P.; Lassalle, S.; et al. Small but Challenging Conjunctival Melanoma: New Insights, Paradigms and Future Perspectives. Cancers 2021, 13, 5691. https://doi.org/10.3390/cancers13225691
Nahon-Estève S, Bertolotto C, Picard-Gauci A, Gastaud L, Baillif S, Hofman P, Groulier A, Maschi C, Caujolle J-P, Lassalle S, et al. Small but Challenging Conjunctival Melanoma: New Insights, Paradigms and Future Perspectives. Cancers. 2021; 13(22):5691. https://doi.org/10.3390/cancers13225691
Chicago/Turabian StyleNahon-Estève, Sacha, Corine Bertolotto, Alexandra Picard-Gauci, Lauris Gastaud, Stéphanie Baillif, Paul Hofman, Anaïs Groulier, Célia Maschi, Jean-Pierre Caujolle, Sandra Lassalle, and et al. 2021. "Small but Challenging Conjunctival Melanoma: New Insights, Paradigms and Future Perspectives" Cancers 13, no. 22: 5691. https://doi.org/10.3390/cancers13225691
APA StyleNahon-Estève, S., Bertolotto, C., Picard-Gauci, A., Gastaud, L., Baillif, S., Hofman, P., Groulier, A., Maschi, C., Caujolle, J.-P., Lassalle, S., & Martel, A. (2021). Small but Challenging Conjunctival Melanoma: New Insights, Paradigms and Future Perspectives. Cancers, 13(22), 5691. https://doi.org/10.3390/cancers13225691








