Simple Summary
Breast cancer is the most common cancer affecting women, and the importance of NR function in breast cancer biology has been recognized since the turn of the 20th century. The nuclear receptor family of transcription factors is associated with cancer development and progression, informs diagnostic and prognostic outcomes, and is an established therapeutic target. Across all subtypes of breast cancer, crosstalk between NR pathways and other signalling pathways has also been demonstrated. Recent critical findings into modulating these NRs, particularly Type 1 NRs, have led to clinical trials and a greater understanding of their mechanism of action. Here, we reviewed the current preclinical insights into the role of Type 1 NRs in breast cancer that have served as a catalyst for clinical translation.
Abstract
The nuclear receptor (NR) family of transcription factors is intimately associated with the development, progression and treatment of breast cancer. They are used diagnostically and prognostically, and crosstalk between nuclear receptor pathways and growth factor signalling has been demonstrated in all major subtypes of breast cancer. The majority of breast cancers are driven by estrogen receptor α (ER), and anti-estrogenic therapies remain the backbone of treatment, leading to clinically impactful improvements in patient outcomes. This serves as a blueprint for the development of therapies targeting other nuclear receptors. More recently, pivotal findings into modulating the progesterone (PR) and androgen receptors (AR), with accompanying mechanistic insights into NR crosstalk and interactions with other proliferative pathways, have led to clinical trials in all of the major breast cancer subtypes. A growing body of evidence now supports targeting other Type 1 nuclear receptors such as the glucocorticoid receptor (GR), as well as Type 2 NRs such as the vitamin D receptor (VDR). Here, we reviewed the existing preclinical insights into nuclear receptor activity in breast cancer, with a focus on Type 1 NRs. We also discussed the potential to translate these findings into improving patient outcomes.
Keywords:
nuclear receptor; steroid hormone; oestrogen; progesterone; androgen; glucocorticoid; breast cancer 1. Nuclear Receptors in Breast Cancer
An appreciation of the fundamental importance of nuclear receptor (NR) function in breast cancer biology can be initially traced back to Beatson’s pivotal work in 1896 demonstrating that oophorectomy in young women with unresectable breast cancer could cause tumour regression [1]. Fast-forward to the 1960s, Jensen followed by Toft and Gorski used murine models to confirm the existence of an intracellular hormone-binding entity that we now recognise as a subset of NR called the steroid hormone receptor [2]. Historically, the study of NR function in breast cancer has largely focused on characterising and therapeutically targeting the oestrogen (ER) and, to a lesser extent, the progesterone (PR) and androgen receptors (AR). However, recognising that ER/PR-negative breast cancers, and indeed a subset of ER/PR-positive breast cancers, do not benefit from ER-targeted therapies has provided a clinical imperative to evaluate the therapeutic impact of modulating non-oestrogen NR-signalling pathways as well. A list of the main nuclear receptors in breast cancer can be found in Table 1.

Table 1.
Main nuclear receptors involved in breast cancer and their natural ligands.
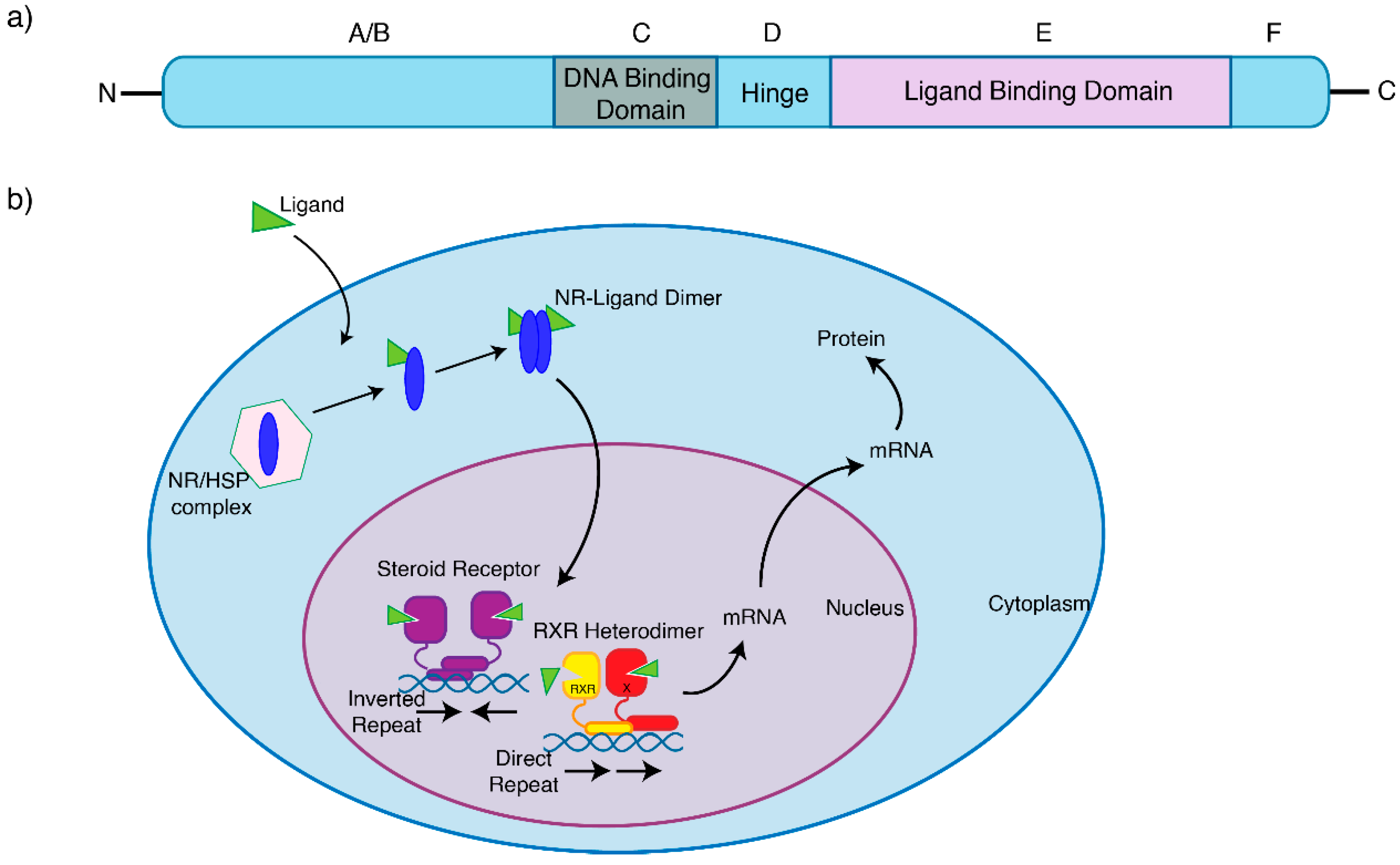
NRs are ligand-activated intracellular proteins or DNA-binding transcription factors, [3,4,5] that play a crucial role in key aspects of human physiology and pathophysiology, such as breast cancer. The NR family of transcription factors consists of 48 different genes, including the closely related steroid hormone receptors. Typically, nuclear hormone receptors consist of several domains, which share a similar structure and are differentially conserved between each receptor (Figure 1a). Typically, ligands (such as hormones, vitamins, or nutrients [6]) bind to their cognate NRs, which in turn regulate the transcription of a subset of genes expressed by a cell, resulting in what is typically considered ‘classical’ hormone signalling. Some NRs, however, can remain constitutively active. To enable these pathways and provide an added layer of regulation, NRs recruit protein coregulators into transcriptional complexes that bind to the DNA. These are either coactivators, which enhance transcription, or corepressors, which repress transcription [4]. These coregulators are essential to the underlying mechanism of NR action by mediating their transcriptional potency [7] and therefore modulating gene expression [8].
Figure 1.
Nuclear receptors share the similar structural domains. (a) Most NRs contain an N-terminal region (A/B), a conserved DNA-binding domain (C), a variable hinge (D), a conserved ligand-binding domain (E), and a variable C-terminal region (F). (b) The NRs involved in breast cancer are bound to heat-shock proteins (HSP) in the cytoplasm, and are activated by binding of ligands, whereby canonical signalling is initiated. This NR–ligand complex will either form a heterodimer (steroid receptors), or form an RXR heterodimer, and translocate to the nucleus, binding to target genes and initiating transcription.
NRs are classically divided into two subsets based on their subcellular location and function [3]. Type 1 nuclear receptors include the sex steroid hormone receptors AR, ER and PR, as well as the corticosteroids GR and the mineralocorticoid receptor (MR). Broadly, sex steroids control the development of the urogenital tracts, secondary sexual characteristics and behaviour, as well as gametogenesis in both males and females. Corticosteroids control our physiological, developmental and behavioural responses to stress, as well as play a critical role in regulating salt and water balance. Unliganded, Type 1 NRs share a similar structure [6,9]. With classical direct genomic signalling, Type 1 NRs are located in the cytoplasm, but translocate to the nucleus upon hormone binding as homodimers, where they associate with chromatin and regulate gene transcription (Figure 1b). However, particularly with ER signalling, we now recognize that indirect regulation of gene expression can also occur via genomic, nongenomic and ligand-independent pathways, comprehensively reviewed by Fuentes et al. [10] and Siersbaek et al. [11]. These insights into the interplay between intracellular kinases, transcription and growth factors, membrane receptors, coregulators and both natural and synthetic ligands with NR signalling have helped in the design of practice-changing therapeutic strategies. In contrast, Type 2 NRs, which include the thyroid hormone, vitamin D and retinoic acid receptors, reside in the nucleus constitutively bound to DNA as RXR heterodimers, and typically act to repress transcription in the absence of ligands [3,12].
While this review focuses predominantly on recent preclinical insights into Type 1 NRs with translational potential in ER+ breast cancer, this is a rapidly evolving space in molecular biology and the clinic that is becoming increasingly relevant across all breast cancer subtypes.
2. Nuclear Receptor Autoregulation and Crosstalk
NR autoregulation describes classical single nuclear receptor activity, or the standard regulation of expression of a NR gene by its hormone-bound protein product [3]. The autoregulation of NR genes can lead to induction (upregulation) or repression (downregulation). Autoinduction leads to the cellular biosynthesis of more NRs and enhanced hormone responsiveness, while autorepression is a homeostatic mechanism that modulates hormonal signalling by downregulating the hormone receptor. Mechanisms for NR autoregulation can be broadly transcriptional or posttranscriptional.
In addition to ligands autoregulating the expression of their own receptor, another important means for modulating cellular responsiveness to different hormonal signals is through the cross-regulation of expression of other NRs. This ‘crosstalk’ between nuclear receptors can be defined as the interplay between different nuclear receptors or even between their overlapping signalling pathways [6]. DNA crosstalk mechanisms can be classified as either indirect (where NRs do not physically interact) or direct (where NRs physically interact to jointly regulate specific target gene subsets). Broadly, when these NR-induced signalling pathways either indirectly or directly interplay, this creates unique signalling and gene expression profiles. An understanding of the different NR crosstalk mechanisms provides us with novel opportunities to therapeutically target oncogenic pathways. For deeper mechanistic insights into co-regulators, nuclear receptor signalling and crosstalk, we direct the reader to other comprehensive reviews from Bagamasbad et al. [3], Conzen et al. [5], De Bosscher et al. [6], O’Malley et al. [7], Sikora et al. [8], and Doan et al. [13].
Biological insights into the underlying mechanisms of this complex NR interplay, both at the level of the cistrome and the interactome, have been gained from techniques such as Chromatin Immunoprecipitation coupled with high-throughput Sequencing (ChIP-seq) and Rapid Immunoprecipitation Mass spectrometry of Endogenous protein (RIME) [14,15,16,17,18]. How these insights impact the targeting of NRs as a therapeutic pathway in breast cancer, and highlight potential combinatorial strategies, are addressed in this review.
3. Oestrogen Receptor Signalling
The action of oestrogen is mediated by two ERs encoded on different chromosomes but sharing sequence homology, the Estrogen Receptor alpha (ERα, NR3A1) and Estrogen Receptor beta (ERβ, NR3A2) nuclear hormone receptors [19]. Meanwhile, the role of ERβ in breast cancer remains unclear and is not specifically assessed by immunohistochemistry in the clinical setting [20]. ERα has been intensely studied due to its integral role in breast tumorigenesis, where it can initiate gene expression changes that promote cell cycle progression [21]. In modern-day epidemiological studies, exposure to oestrogen (and progestogens) has been consistently linked to an increase in breast cancer risk [22], particularly ER+ breast cancer [23]. Around 75% of breast cancers are defined and driven by ERα transcriptional activity and for decades, anti-oestrogen therapies targeting ER have formed the cornerstone of therapy for the management of ER+ breast cancer. ERα inhibition is achieved either by the direct blockade of ERα activation through competitive inhibition of oestradiol (selective ER modulators, SERMS, i.e. tamoxifen), degrading ER (selective ER degraders, SERDs, i.e. fulvestrant) or by preventing peripheral oestrogen synthesis using aromatase inhibitors (AIs). However, clinical outcomes vary considerably, and a proportion of women with early breast cancer driven by ERα transcriptional activity develop drug resistance and relapse with incurable, metastatic disease.
More recently, the targeting of cell cycle progression with cyclin-dependant kinase 4/6 (CDK4/6) inhibitors in combination with anti-oestrogen therapy has become the standard first-line therapy in de novo or recurrent breast cancer [24,25]. While this approach has prolonged the progression-free and overall survival of patients with metastatic disease [26,27,28,29], when patients develop resistance to this treatment combination, there are currently no equally robust therapeutic strategies in the second line [30]. Second-line treatment options include fulvestrant, cytotoxic chemotherapy, or anti-oestrogen therapy combined with inhibitors of the mammalian target of rapamycin (mTORi). Additionally, growing evidence supports the use of next-generation oral SERDs (Table 2) and combinatorial strategies with alpha-selective phosphoinositide 3-kinase inhibitors (PI3Ki) in patients harbouring somatic, activating PIK3CA mutations [31,32]. The optimal sequencing of this repertoire of therapeutic strategies, however, remains the subject of ongoing clinical trials such as the SONIA study (ClinicalTrials.gov identifier NCT03425838), and the growing use of commercially available tissue and liquid biopsy-based companion diagnostic panels is leading to a surge in biomarker-driven treatment strategies post-CDK4/6-inhibitor therapy in ER+ metastatic breast cancer.

Table 2.
Clinical trials in progress that are investigating nuclear receptor-directed therapies in breast cancer.
As a member of the nuclear receptor superfamily of transcription factors, ERα is composed of functional domains and structural regions in common with other nuclear receptors (Figure 1a). The A/B region represents the N-terminal domain, involved in gene transcription transactivation, and containing a zinc finger that mediates binding to target sequences [10]. Significant progress has been made in understanding how wild-type ERα interacts with DNA. Using genomic technologies in breast cancer cell lines, it has been shown that ERα is able to bind to specific DNA sequences known as estrogen response elements (EREs, with a consensus motif GGTCAnnnTGACC) within the chromatin [33,34]. The C region of ERα is the DNA binding domain which contributes to ER dimerization and binds to these canonical EREs. The D region is the hinge region that binds chaperone proteins and allows for receptor–ligand complexes to translocate to the nucleus, and the E/F region is the ligand binding domain, which binds oestrogen, coactivators and corepressors (Figure 1a). Additional regulators of ER transcriptional activity known as activation function domains AF1 and AF2 are located in the N-terminal and DNA binding domains, respectively [35].
Genomic analyses have shown that ERα rarely acts through associations with promoter regions of target genes. Instead, genome-wide maps of ERα binding in breast cancer confirm that ERα binding events mostly occur at distal cis-regulatory enhancer elements at significant distances from the transcription start sites [33,36]. DNA-looping occurs, bringing enhancers in spatial proximity to promoter regions of target genes, and transcription is initiated [37]. It is also now clear that, in addition to oestrogens, ER function is modulated by other steroid receptors, with the interaction between ER and both PR and AR being the best-characterized models of nuclear receptor crosstalk in breast cancer. In addition, multiple signalling pathways (e.g., growth factor and cytokine signalling pathways) may also have a substantial impact on the efficacy of anti-oestrogen therapies [8,11].
It has been proposed that resistance to endocrine therapies may be the result of both genetic and epigenetic factors [38,39,40,41]. While gain-of-function mutations in ESR1, the gene encoding ERα, are relatively rare in primary breast cancer [42], 11–55% of metastatic cancers have point mutations in the ligand-binding domain of ER, especially in amino acids Y537 and D538 [42]. These mutations generate a constitutively active ER that is less dependent on oestrogen for activity [43,44,45]. The highest prevalence of ESR1 mutations has been reported in the cell-free DNA (cfDNA) of AI-resistant metastatic ER+ breast cancer patients using droplet digital PCR [46,47,48]. At a cistromic level, not only are ESR1 mutants distinct from oestrogen-stimulated wild-type ER, Y537S and D538G ESR mutants also have distinct cistromes and transcriptomes [49]. These mutations cluster in the ligand-binding domain of ER and lead to ligand-independent ER activity that promotes tumour growth, partial resistance to endocrine therapy and enhanced metastatic capacity. However, tumours bearing ESR1 mutations can retain relative sensitivity to SERDs. A retrospective analysis of plasma samples from the phase III SoFEA study in patients resistant to nonsteroidal aromatase inhibitors confirmed significantly improved outcomes with fulvestrant-containing regimens compared with exemestane in the 39.1% of patients found to be harbouring an ESR1 mutation [47]. This highlights the imperative to accelerate the development and rollout of more effective, potent and orally bioavailable next-generation SERDs, which have been shown to act through slowing intra-nuclear ER mobility, resulting in the limitation of both chromatin accessibility and downstream proliferative activity [50]. A number of these next-generation SERDs are currently being investigated in phase I–III clinical trials in early- and advanced-stage breast cancer, both alone and in combination with CDK4/6 inhibitors (ClinicalTrials.gov identifiers NCT04647487, NCT03455270, NCT04669587 and NCT04711252).
The novel selective estrogen receptor covalent antagonists (SERCAs) are another therapeutic alternative in overcoming endocrine resistance. This class of drugs targets the cysteine residue at amino acid 530 (C530) that exists only in ER, to promote a unique antagonist conformation. Specifically, the SERCAs H3B-5942 and H3B-6545 have been demonstrated to covalently bind to C530 of both wild-type and mutant ERα proteins, and have been shown to be superior to standard-of-care therapies in in vitro and in vivo models of endocrine resistance [51,52]. Currently, H3B-6545 is being investigated in phase I–II clinical trials in advanced, metastatic breast cancer either alone or in combination with CDK4/6 inhibitors (ClinicalTrials.gov identifiers NCT04568902, NCT04288089 and NCT03250676).
Emerging data have revealed that alterations in the epigenome can result in ER-directed therapy resistance. Aromatase inhibitor-induced DNA hypermethylation at estrogen-responsive elements (EREs) is associated with a reduction in ER binding and activity [41,53]. As a result, decreased gene expression of key ER regulators and reduced ER binding cause the cell to become less dependent on oestrogen for survival, and therefore less sensitive to ER-directed therapies [41]. Moreover, ER+ breast cancers that have relapsed following endocrine therapy exhibit higher DNA methylation at enhancer loci [41]. ER-directed therapy resistance can also emerge from altered methylation patterns at promoter regions of genes [54,55]. For example, hypermethylation at the PTEN, PIXT2 and HOXC10 promoters have been found to be predictive biomarkers of resistance in both cell lines and tumour tissues [55,56,57]. While demethylation therapies such as decitabine have been demonstrated to be efficacious in reversing hypermethylation in preclinical models, they have not yet been translated into clinical use [58].
Post-translational histone modifications have also been shown to induce chromatin remodelling that favour the repression of ER and promotion of signalling pathways associated with endocrine resistance. Histone variants have been linked to oestrogen signalling and endocrine resistance. For example, overexpression of the H2A variant H2A.Z has been linked to oestrogen-independent proliferation, and thus ER-targeted therapy resistance [59]. Another study demonstrated that the H2B variant HIST1H2BE is overexpressed in both resistant cell lines and tumours treated with aromatase inhibitors derived from patients [60]. Finally, variations in histones by histone deacetylases (HDACs) have also been associated with the loss of ER expression, also conferring endocrine resistance. In early-phase clinical trials, combinations of an aromatase inhibitor or tamoxifen with HDAC inhibitors such as vorinostat or entinostat demonstrated improvements in overall survival, with the potential to re-sensitize tumours to endocrine therapy in women with resistant disease [61,62]. Disappointingly, results from the positive phase II ENCORE301 study were not replicated in the phase III E2112 study of entinostat plus exemestane, which failed to demonstrate improved survival compared to exemestane alone in aromatase inhibitor-resistant patients with advanced disease [63]. Unlike ENCORE301, many patients in the E2112 study had received prior fulvestrant and/or CDK4/6-inhibitors, likely impacting the final outcome, while simultaneously strengthening the trial’s relevance in a more ‘current’ therapeutic context where CDK4/6-inhibitors are now the standard first-line treatment. We are awaiting results from exploratory analyses to identify a predictive biomarker of response to this class of therapy.
4. Progesterone Receptor Signalling
In combination with oestrogen, progesterone plays a major role in normal breast development, as well as changes in the mammary gland during the menstrual cycle, pregnancy and lactation [64]. Mouse mammary studies have revealed that PR (NR3C3) is essential in the mammary epithelium for ductal side-branching and alveologenesis [65]. In the adult mouse, 17β-oestradiol induces the expression of PR, and stimulation with progesterone (e.g., during the luteal phase of the menstrual cycle) triggers cell proliferation. Progestogens, which are any natural or artificial substance that exerts progesterone-like activity via activation of PR [66], have long been employed as contraceptive agents, or components of Menopausal Hormonal Therapy (MHT) in combination with oestrogen as they prevent hyperplastic or malignant consequences of chronic, unopposed oestrogen exposure on the endometrium [67].
PR is both a member of the NR family and an ERα target gene, co-expressed in over two-thirds of ER+ breast cancers [68]. PR exists in two isoforms, PR-A and PR-B [69]. Historically, the accepted explanation for PR activity in ER+ breast cancer cells was that PR expression was a passive consequence of a functional oestrogen receptor. PR was therefore established as a biomarker of ERα functionality in breast cancer and a predictive marker of response to ERα-directed agents [70]. Therefore, functional studies into the role of progesterone and its receptor have lagged significantly behind those of ERα and have in fact been the subject of heated debate. Epidemiological studies and clinical MHT trials have implicated that synthetic progestins were associated with an increased risk of breast cancer [22,23,71,72]. Additionally, progesterone-initiated PR signalling has been shown to contribute to mammary tumourigenesis in murine models [73]. On the other hand, multiple studies have demonstrated the improved prognosis of PR+ breast cancers [74,75,76,77,78,79], and a Combined Endocrine Receptor (CER) score averaging the Allred score of both ER and PR has been demonstrated to be a more powerful discriminator of patient outcome than either ER or PR alone [80]. In support of this, the heterozygous or homozygous deletion of PR occurs more often in the luminal B breast cancer subtype that is associated with a higher proliferation rate and poorer prognosis compared with luminal A breast cancers [81].
Importantly, the role of PR in breast cancer is context-dependent and highlights the importance of the hormonal milieu. Pivotal studies have emphasised that the function of PR in breast cancer has to be considered in the context of the presence of oestrogen and ERα signalling [15,82]. In the absence of a functional oestrogen-activated ER complex, PR activation might have modest pro-proliferative effects, and differing effects in malignant and normal breast tissue contingent on oestrogenic status. This emphasizes the importance of further delineating the precise mechanisms through which PR regulates tumours compared with mammary gland proliferation.
In breast cancer cell lines, the administration of progestogens has been shown to inhibit ERα transcriptional activity and oestrogen-induced cell proliferation [83,84,85]. Additionally, progestogens alone oppose the oestrogen-induced proliferation of MCF7 and T47D cell line and ER+/PR+ patient-derived xenografts [15,86]. Interestingly, the combination of tamoxifen and progesterone had an even greater suppressive effect on tumour growth. Clinically, benefits have been demonstrated from a single injection of progesterone administered before surgery [87], and the use of a single agent progestogen has consistently shown to be clinically beneficial either as a first-line therapy in de novo metastatic ER+ breast cancer, or in advanced disease when ER-directed endocrine agents have failed [88,89,90,91,92,93,94,95,96,97,98,99,100].
Taken together, existing data imply that PR can play an anti-proliferative role in ER+ breast cancer. Mechanistically, the stimulation of PR by progestins regulates distinct cistromes and transcriptomes in breast cancer cells compared to normal breast cells [101,102], and can function as a molecular rheostat to control ERα binding and transcriptional activity. In the presence of agonist ligands, insights gained from ChIP-seq experiments have confirmed that PR causes the rapid redistribution or sequestration of ERα away from its pro-proliferative gene targets in breast cancer cells, resulting in a unique gene expression program that is associated with a good clinical outcome and culminating in cell cycle arrest [15,103]. The potential clinical significance of exploiting this interaction between ERα and PR signalling in breast cancer affords the possibility that the addition of a progesterone agonist might enhance the anti-proliferative effect of anti-oestrogen therapies and therefore provide a more effective combination therapy. Indeed, two short-term, pre-operative window-of-opportunity studies, PIONEER and WinPRO (ClinicalTrials.gov identifiers NCT03306472 and NCT03906669), are currently testing this hypothesis clinically in early-stage breast cancer.
Paradoxically, PR antagonists have also proven to be antiproliferative in cell line and murine models of ER+ breast cancer [104,105,106,107,108,109,110,111]. It has indeed been hypothesized that PR antagonists may also interfere with ER transcriptional activity, similarly to agonists [66]. However, clinical trials of agents such as mifepristone and onapristone have recruited poorly, have shown either a lack of reproducible efficacy or unacceptable hepatotoxicity [112,113,114], and have therefore not progressed to routine clinical use.
5. Androgen Receptor Signalling
AR (NR3C4) is essential for the development of male reproductive organs, and it is also expressed in the majority of breast cancers. Two isoforms and several alternative splicing variants, encoded by the same gene, have been described. While AR is currently not routinely assessed immunohistochemically in biopsies and surgical excision specimens from our breast cancer patients, it is in fact the most widely expressed hormone receptor in all stages of breast cancer [115,116]. AR expression varies between breast cancer subtypes, and the function of AR in breast cancer is highly context-dependant, contingent on the co-expression of ER, the AR:ER protein ratio, the menopausal status of the patient and the hormonal milieu [8].
AR is expressed in up to 85% of ER+ breast cancer and is an independent clinico-pathological prognostic factor associated with favourable outcomes in this setting [117,118]. AR and ER co-localize at select genomic loci within the nuclei of breast cancer cells [119], and functional crosstalk between the hormone receptors has been well-described [120]. Controversially, both AR agonists and antagonists have been shown to inhibit growth in ER+ preclinical models, by inhibiting ER function at a genomic level [119,121,122,123,124]. However, the bulk of positive evidence supports an anti-proliferative role of androgens in ER+ breast cancers, with androgenic signalling via AR generally antagonistic of oestrogen activity [116,119,125]. Indeed, the historic use of androgens as a treatment in breast cancer clinically supports this [126,127]. Major reasons that have limited its clinical utility include virilising side effects, concerns regarding the aromatisation of androgens to oestrogen and the development of effective ER-directed approaches.
More recently, there has been a resurgence of interest in the role of the AR signalling axis in ER+ breast cancer. The activation of AR by its natural ligand DHT in endocrine-sensitive ER+ cell lines in vitro inhibited proliferation and ER signalling [119,128], consistent with aforementioned clinical studies, supporting the premise that androgens inhibit proliferation and induce tumour regression. AR agonism has also been shown to retain its anti-ER signalling and growth inhibitory effects in endocrine therapy-naïve and -resistant in vivo patient-derived xenograft (PDX) models [129], including those harbouring genomic aberrations of ESR1 and CCND1 [16]. The anticancer effect was a result of an upregulation of AR target genes, including tumour suppressors, the reprogramming of the binding of ER and its co-activators on chromatin, and the redistribution of E2-stimulated p300 binding sites, resulting in inhibition of the expression of critical ER-regulated cell cycle and survival genes [16].
Therapeutically, the development of selective androgen receptor modulators (SARMs), such as enobosarm and RAD140, now offers a novel approach for targeting AR in breast cancer [16,130]. SARMs exhibit a high specificity of binding to AR and have the advantage that they dissociate the anabolic from androgenic effects of AR and therefore lack the virilising effects seen with the historical use of androgens [131]. A phase II study has demonstrated that enobosarm was well tolerated and conferred clinical benefit in heavily pre-treated patients with ER+/AR+ metastatic breast cancer [132]. Enobosarm in combination with CDK4/6 inhibitors has also been shown to be efficacious in the setting of endocrine or CDK4/6 inhibitor-resistant breast cancer models (which retain the expression of AR), suggesting that AR agonism may partially restore sensitivity to CDK4/6 inhibitors, thus positing that this combination may be an effective therapeutic strategy in the second-line treatment of ER+ metastatic breast cancer [16]. Together, these findings provided the motivation behind the phase III registration ARTEST study (ClinicalTrials.gov identifier NCT04869943) of enobosarm in endocrine therapy and CDK4/6 inhibitor-resistant ER+ metastatic breast cancer patients [133].
A transdermal preparation of 4-OH-testosterone, CR1447, has also demonstrated efficacy and a favourable toxicity profile in phase I/II studies [134]. Another alternative AR agonist includes oral testosterone undecanoate, which utilises a self-emulsifying drug delivery system to minimise pharmacokinetic variability experienced with other formulations [135], maximising free testosterone levels and AR interaction while potentially reducing the risk of androgenisation by more predictably maintaining testosterone levels in the eugonadal range [136]. Window-of-opportunity studies using this compound are also currently under development.
In contrast to ER+ breast cancer, high AR expression is associated with a poor prognosis in triple-negative breast cancers (TNBC) [137]. AR is expressed in 15–35% of TNBCs [138], primarily in the luminal androgen receptor (LAR) subtype. These tumours demonstrate a gene expression signature resembling that of endocrine-responsive tumours [139], are characterised by both AR expression and androgen-dependant growth [140], and are classically less responsive to conventional cytotoxic chemotherapy. AR-antagonism in this setting, with antiandrogens such as bicalutamide, have been investigated in clinical trials [141]. The second-generation AR antagonist enzalutamide has been shown to be well-tolerated in combination with exemestane, with clinical efficacy in this subset of TNBC that expresses AR [142], as well as in a cohort of ER+ patients with high levels of AR mRNA and low levels of ER mRNA on mRNA-sequencing [143]. This provides a rationale to explore combinatorial strategies of AR antagonists with agents such as CDK4/6i [144,145] and PI3K inhibitors [146]. Growing evidence also supports the utility of other next-generation AR-targeted agents such as abiraterone acetate with prednisone in AR+ TNBC, as well as the novel CYP17 lyase inhibitor and potent AR antagonist seviteronel (VT-464/INO-464), which is about to enter clinical trials in combination with chemotherapy in the phase I/II 4CAST study (ClinicalTrials.gov identifier NCT04947189). Furthermore, seviteronel has been shown to induce DNA damage following radiation in AR+ TNBC models, demonstrating a unique radiosensitizing effect [147].
6. Glucocorticoid Receptor Signalling
As with AR, GR (NR3C1) expression is not routinely evaluated in breast carcinomas. GR is expressed in ~70% of ER+ breast cancers and >60% of all breast cancers [148]. Clinically, synthetic glucocorticoids (GR agonists) such as dexamethasone are ubiquitously used in breast cancer in conjunction with chemotherapy to mitigate hypersensitivity reactions, and for their antiemetic, anti-inflammatory, as well as orexigenic properties. However, dexamethasone triggers different effects depending on the breast cancer subtype [149].
Similarly to the trend observed with AR expression, retrospective meta-analyses of patients with ER+ breast cancer have determined that high GR mRNA levels are associated with low tumour grade [148] and better prognosis [150,151] compared to low or negligible GR expression, independent of PR expression. Again, the opposite was observed in ER- breast cancer where high tumour GR expression was associated with a worse prognosis [150]. Therefore, mirroring AR, the tumour suppressor vs. oncogenic potential of GR is dependent upon ER expression. Mechanistically in ER+ disease, both ER and GR undergo crosstalk upon co-treatment with oestradiol and dexamethasone [151,152], with reciprocal reprogramming of both receptors occurring via the Hager lab’s well-described assisted loading mechanism [152,153]. This model involves chromatin remodelling by one receptor followed by recruitment of the other receptor. Upon co-stimulation of ER and GR in MCF7 cells with oestradiol and glucocorticoids, transcriptional changes in genes linked to cell proliferation and differentiation occur [151], inhibiting growth. Despite these preclinical findings, clinical studies in ER+ breast cancer patients have demonstrated varied effects of glucocorticoid use on breast cancer patient survival, with modest effects when used as a single agent and no additive effect in combination with other drugs, including anti-oestrogens [154,155]. However, given the widespread use of glucocorticoids in cancer, further exploration of the full therapeutic potential of activating GR in ER+ breast cancer warrants further investigation.
By contrast, GR activation with glucocorticoid has been shown to inhibit chemotherapy-induced cell apoptosis [156], and drives the expression of pro-tumorigenic genes in TNBC [157,158]. This raises the concern that the routine administration of high doses of synthetic glucocorticoids as a chemotherapy premedication has the potential to activate GR-mediated cell survival pathways and diminish the effectiveness of chemotherapy in this setting. More recently, an extensive study using both patient-derived and TNBC cell line-derived xenograft models also suggested that activation of GR with glucocorticoid treatment increases tumour heterogeneity and promotes breast cancer metastasis [159]. The suggested mechanism was the upregulation of the expression of a receptor tyrosine kinase-like orphan receptor-1 (ROR-1). With GR identified as a target in this setting, preclinical findings of the potentiated cytotoxic efficacy of paclitaxel chemotherapy with the addition of the GR antagonist Mifepristone [156] has now led to the translation of these findings to the clinical research setting. Consistent with these observations, a randomised phase I clinical trial combined mifepristone with nab-paclitaxel, confirming disease activity and manageable toxicity [160], and a randomised phase II trial is currently recruiting (NCT02788981).
7. Other Nuclear Receptors
The mineralocorticoid receptor (MR, NR3C2) is another receptor of interest, given that it is most likely expressed in the majority of breast cancers (up to 90%) [161]. Aldosterone, the primary ligand for MR, is typically used in the management of hypertension and cardiac failure. As with GR, MR can undergo crosstalk with PR to induce significant growth inhibition, and many glucocorticoids also bind to MR with high affinity [162]. An interaction between ER and MR has not been directly explored in breast cancer models; however, high MR and retinoic acid receptor (RAR) expression is associated with improved ER+ breast cancer-specific survival. A tumour-suppressive relationship between these nuclear receptors was illustrated by co-treatment with mineralocorticoids and retinoic acid receptor-stimulating retinoids [163], highlighting another potential therapeutic pathway worth characterising in the setting of breast cancer resistant to standard ER-targeted therapies. Independently, RAR expression can predict for resistance to tamoxifen [164]. While the results of combinatorial therapeutic strategies with retinoids in patients with breast cancer have been generally disappointing [165], retinoids have been shown to inhibit the expansion of chemoresistant cytokeratin 5-positive (CK5+) cells through RAR/PR crosstalk [166].
The relationship between Vitamin D and breast cancer remains controversial. A recent meta-analysis demonstrated that while there is no relationship between nuclear VDR (NR1I1) expression and overall survival in patients with breast cancer, high total nuclear and cytoplasmic VDR expression was associated with improved survival outcomes [167]. Both the VDR and vitamin D 1-hydroxylase, the enzyme that generates the active Vitamin D3 ligand 1,25-dihydroxycholecalciferol, are expressed in the human breast. Additionally, VDR expression correlates with the expression of ER. Interest has been provoked by growing evidence suggesting that adequate Vitamin D levels and intake inversely correlate with breast cancer risk [168,169,170], and that low levels of vitamin D are associated with an increased risk of recurrence or death in breast cancer patients [167,171]. This is arguably enough evidence to suggest that early breast cancer patients should at least supplement vitamin D if found to be deficient. 1,25-dihydroxycholecalciferol inhibits the proliferation of breast cancer cell lines and promotes differentiation and apoptosis in vitro [172,173,174], but clinical data regarding tumour responsiveness to vitamin D are limited and remain inconclusive [174,175]. The impact of vitamin D supplementation in the neoadjuvant setting on the rate of pathological complete response is being investigated in TNBC (ClinicalTrials.gov identifier NCT04677816).
8. Conclusions
Given that the prominent nuclear receptors in breast cancer all share similar consensus DNA binding motifs, as well as mechanisms of co-activation, it is not surprising that there is substantial functional crosstalk between these receptors. Additionally, given that most nuclear receptors are regulated by ligands and are often highly co-expressed, this renders them susceptible to external control over their gene regulatory activities [6], and therefore ideal druggable targets.
In ER+ breast cancer, steroid hormone receptors are certainly not bystanders in ER signalling pathways. Modulation of their activity can alter or reprogram ER DNA binding to dramatically modify target gene expression. Such a modulation of hormone receptor function in combination with anti-oestrogen therapy can either modify the response or alter the trajectory of developing resistance to therapy, and certainly highlights the imperative to improve our understanding of how other steroid hormone receptors influence ER function in the context of standard anti-oestrogen therapy. However, the fact that AR and GR have opposite functions in the presence and absence of ER highlights the importance of characterising the functional interplay between different steroid hormone receptor signalling pathways in both luminal and nonluminal breast cancer subtypes, to fully exploit their therapeutic potential. Overwhelmingly, the modulation of nuclear receptor activity beyond targeting the ER provides us with novel approaches to manage patients with breast cancer.
Given the crosstalk of pathways triggered between different nuclear receptors, it may be possible that in the near future, breast cancer therapeutic decisions may require consideration of the expression of all four major steroid hormone receptors in breast cancer— ER, PR, AR and GR. This opens the prospect of the deeper characterisation of breast cancers for both prognostic purposes and as predictive biomarkers of response to a new array of endocrine therapies.
Author Contributions
Conceptualisation, S.K.; data curation, S.K.; writing, S.K., A.F. and E.L.; funding acquisition, E.L. All authors have read and agreed to the published version of the manuscript.
Funding
E.L. is supported by a National Breast Cancer Foundation Endowed Chair (Grant number NBCF EC17-02) and Love Your Sister. E.L. and S.K. are supported by the Balnaves Foundation. A.F. is supported by the Australian Commonwealth Government Research Training Program.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Beatson, G.T. On the treatment of inoperable cases of carcinoma of the mamma. Lancet 1896, 2, 1–14. [Google Scholar]
- Jensen, E.V.; Jacobson, H.I.; Walf, A.A.; Frye, C.A. Estrogen action: A historic perspective on the implications of considering al-ternative approaches. Physiol. Behav. 2010, 99, 151–162. [Google Scholar] [CrossRef]
- Bagamasbad, P.; Denver, R.J. Mechanisms and significance of nuclear receptor auto- and cross-regulation. Gen. Comp. Endocrinol. 2011, 170, 3–17. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, B.W. 90 YEARS of PROGESTERONE: Reminiscing on the origins of the field of progesterone and estrogen receptor action. J. Mol. Endocrinol. 2020, 65, C1–C4. [Google Scholar] [CrossRef]
- Conzen, S.D. Minireview: Nuclear Receptors and Breast Cancer. Mol. Endocrinol. 2008, 22, 2215–2228. [Google Scholar] [CrossRef] [PubMed]
- De Bosscher, K.; Desmet, S.J.; Clarisse, D.; Estébanez-Perpiña, E.; Brunsveld, L. Nuclear receptor crosstalk—Defining the mecha-nisms for therapeutic innovation. Nat. Rev. Endocrinol. 2020, 16, 363–377. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, B.W. Coregulators: From whence came these ‘master genes’. Mol. Endocrinol. 2007, 21, 1009–1013. [Google Scholar] [CrossRef] [PubMed]
- Sikora, M.J. Family Matters: Collaboration and Conflict Among the Steroid Receptors Raises a Need for Group Therapy. Endocrinology 2016, 157, 4553–4560. [Google Scholar] [CrossRef]
- A Lamb, C.; I Vanzulli, S.; Lanari, C. Hormone receptors in breast cancer: More than estrogen receptors. Medicina 2019, 79, 540–545. [Google Scholar] [PubMed]
- Fuentes, N.; Silveyra, P. Estrogen receptor signaling mechanisms. Adv. Protein Chem. Struct. Biol. 2019, 116, 135–170. [Google Scholar] [CrossRef]
- Siersbæk, R.D.; Kumar, S.; Carroll, J. Signaling pathways and steroid receptors modulating estrogen receptor α function in breast cancer. Genes Dev. 2018, 32, 1141–1154. [Google Scholar] [CrossRef] [PubMed]
- Mangelsdorf, D.; Thummel, C.; Beato, M.; Herrlich, P.; Schütz, G.; Umesono, K.; Blumberg, B.; Kastner, P.; Mark, M.; Chambon, P.; et al. The nuclear receptor superfamily: The second decade. Cell 1995, 83, 835–839. [Google Scholar] [CrossRef]
- Doan, T.B.; Graham, J.D.; Clarke, C. Emerging functional roles of nuclear receptors in breast cancer. J. Mol. Endocrinol. 2017, 58, R169–R190. [Google Scholar] [CrossRef]
- Schmidt, D.; Wilson, M.D.; Spyrou, C.; Brown, G.D.; Odom, D.T. Europe PMC Funders Group ChIP-seq: Using high-throughput sequencing to discover protein-DNA interactions. Methods 2014, 48, 240–248. [Google Scholar] [CrossRef]
- Mohammed, H.; Russell, I.A.; Stark, R.; Rueda, O.M.; Hickey, T.; Tarulli, G.; Serandour, A.A.A.; Birrell, S.N.; Bruna, A.; Saadi, A.; et al. Progesterone receptor modulates ERα action in breast cancer. Nat. Cell Biol. 2015, 523, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Hickey, T.E.; Selth, L.A.; Chia, K.M.; Laven-Law, G.; Milioli, H.H.; Roden, D.; Jindal, S.; Hui, M.; Finlay-Schultz, J.; Ebrahimie, E.; et al. The androgen receptor is a tumor suppressor in estrogen receptor–positive breast cancer. Nat. Med. 2021, 27, 310–320. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, H.; Taylor, C.; Brown, G.D.; Papachristou, E.; Carroll, J.; D’Santos, C.S. Rapid immunoprecipitation mass spectrometry of endogenous proteins (RIME) for analysis of chromatin complexes. Nat. Protoc. 2016, 11, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Papachristou, E.K.; Kishore, K.; Holding, A.N.; Harvey, K.; Roumeliotis, T.I.; Chilamakuri, C.S.R.; Omarjee, S.; Chia, K.M.; Swarbrick, A.; Lim, E.; et al. A quantitative mass spectrometry-based approach to monitor the dynamics of endogenous chromatin-associated protein complexes. Nat. Commun. 2018, 9, 1–13. [Google Scholar] [CrossRef]
- Gburcik, V.; Picard, D. The cell-specific activity of the estrogen receptor a may be fine-tuned by phosphorylation-induced structural gymnastics. Nucl. Recept. Signal. 2006, 4, e005. [Google Scholar] [CrossRef]
- Ström, A.; Hartman, J.; Foster, J.S.; Kietz, S.; Wimalasena, J.; Gustafsson, J. Estrogen receptor beta inhibits 17beta-estradiol-stimulated proliferation of the breast cancer cell line T47D. Proc. Natl. Acad. Sci. USA 2004, 101, 1566–1571. [Google Scholar] [CrossRef]
- Carroll, J.S.; Liu, X.S.; Brodsky, A.S.; Li, W.; Meyer, C.A.; Szary, A.J.; Eeckhoute, J.; Shao, W.; Hestermann, E.V.; Geistlinger, T.R.; et al. Chromosome-wide mapping of estrogen receptor binding reveals long-range regulation requiring the fork-head protein FoxA1. Cell 2005, 122, 33–43. [Google Scholar] [CrossRef]
- Group, C.; Cancer, B. Type and timing of menopausal hormone therapy and breast cancer risk: Individual participant meta-analysis of the worldwide epidemiological evidence. Lancet 2019, 394, 1159–1168. [Google Scholar]
- Althuis, M.D.; Fergenbaum, J.H.; Garcia-Closas, M.; A Brinton, L.; Madigan, M.P.; E Sherman, M. Etiology of hormone receptor-defined breast cancer: A systematic review of the literature. Cancer Epidemiol. Biomark. Prev. 2004, 13, 1558–1568. [Google Scholar]
- Finn, R.S.; Martin, M.; Rugo, H.S.; Jones, S.; Im, S.-A.; Gelmon, K.; Harbeck, N.; Lipatov, O.N.; Walshe, J.M.; Moulder, S.; et al. Palbociclib and Letrozole in Advanced Breast Cancer. N. Engl. J. Med. 2016, 375, 1925–1936. [Google Scholar] [CrossRef] [PubMed]
- Cristofanilli, M.; Turner, N.C.; Bondarenko, I.; Ro, J.; Im, S.-A.; Masuda, N.; Colleoni, M.; DeMichele, A.; Loi, S.; Verma, S.; et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): Final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016, 17, 425–439. [Google Scholar] [CrossRef]
- Turner, N.C.; Jungsil PALOMA3 Study Group; Andre, F.; Loi, S.; Verma, S.; Iwata, H.; Harbeck, N.; Loibl, S.; Bartlett, C.H.; Zhang, K.; et al. Palbociclib in Hormone-Receptor–Positive Advanced Breast Cancer. N. Engl. J. Med. 2015, 373, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Hortobagyi, G.; Stemmer, S.; Burris, H.; Yap, Y.-S.; Sonke, G.; Paluch-Shimon, S.; Campone, M.; Petrakova, K.; Blackwell, K.; Winer, E.; et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann. Oncol. 2018, 29, 1541–1547. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.J.; Cheng, J.; Bloomquist, E.; Sanchez, J.; Wedam, S.B.; Singh, H.; Amiri-Kordestani, L.; Ibrahim, A.; Sridhara, R.; Goldberg, K.B.; et al. CDK4/6 inhibitor treatment for patients with hormone receptor-positive, HER2-negative, advanced or metastatic breast cancer: A US Food and Drug Administration pooled analysis. Lancet Oncol. 2020, 21, 250–260. [Google Scholar] [CrossRef]
- Schettini, F.; Giudici, F.; Giuliano, M.; Cristofanilli, M.; Arpino, G.; del Mastro, L.; Puglisi, F.; de Placido, S.; Paris, I.; de Placido, P.; et al. Overall Survival of CDK4/6-Inhibitor-Based Treatments in Clinically Relevant Subgroups of Metastatic Breast Cancer: Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2020, 112, 1089–1097. [Google Scholar] [CrossRef]
- Schettini, F.; Giuliano, M.; Giudici, F.; Conte, B.; De Placido, P.; Venturini, S.; Rognoni, C.; Di Leo, A.; Locci, M.; Jerusalem, G.; et al. Endocrine-Based Treatments in Clinically-Relevant Subgroups of Hormone Receptor-Positive/HER2-Negative Metastatic Breast Cancer: Systematic Review and Meta-Analysis. Cancers 2021, 13, 1458. [Google Scholar] [CrossRef]
- Rugo, H.S.; Rugo, H.S.; Lerebours, F.; Ciruelos, E.; Drullinsky, P.; Ruiz-Borrego, M.; Neven, P.; Park, Y.H.; Prat, A.; Bachelot, T.; et al. Alpelisib plus fulvestrant in PIK3CA-mutated, hormone receptor-positive advanced breast cancer after a CDK4/6 inhibitor (BYLieve): One cohort of a phase 2, multicentre, open-label, non-comparative study. Lancet Oncol. 2021, 22, 489–498. [Google Scholar] [CrossRef]
- Turner, S.; Chia, S.; Kanakamedala, H.; Hsu, W.; Park, J.; Chandiwana, D.; Ridolfi, A.; Yu, C.; Zarate, J.P.; Rugo, H.S. Effectiveness of Alpelisib + Fulvestrant Compared with Real-World Standard Treatment Among Patients with HR+, HER2-, PIK3CA-Mutated Breast Cancer. Oncologist 2021, 26, e1133–e1142. [Google Scholar] [CrossRef]
- Carroll, J.; A Meyer, C.; Song, J.; Li, W.; Geistlinger, T.R.; Eeckhoute, J.; Brodsky, A.S.; Keeton, E.K.; Fertuck, K.C.; Hall, G.F.; et al. Genome-wide analysis of estrogen receptor binding sites. Nat. Genet. 2006, 38, 1289–1297. [Google Scholar] [CrossRef]
- Klinge, C.M. Estrogen receptor interaction with estrogen response elements. Nucleic Acids Res. 2001, 29, 2905–2919. [Google Scholar] [CrossRef]
- Kumar, R.; Zakharov, M.N.; Khan, S.H.; Miki, R.; Jang, H.; Toraldo, G.; Singh, R.; Bhasin, S.; Jasuja, R. The Dynamic Structure of the Estrogen Receptor. J. Amino Acids 2011, 2011, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ross-Innes, C.S.; Stark, R.; Teschendorff, A.E.; Holmes, K.A.; Ali, H.R.; Dunning, M.; Brown, G.D.; Gojis, O.; Ellis, I.; Green, A.; et al. Differential oestrogen receptor binding is associated with clinical outcome in breast cancer. Nature 2012, 481, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Fullwood, M.; Liu, M.H.; Pan, Y.F.; Liu, J.; Xu, H.; Bin Mohamed, Y.; Orlov, Y.; Velkov, S.; Thoreau, H.; Mei, P.H.; et al. An oestrogen-receptor-α-bound human chromatin interactome. Nature 2009, 462, 58–64. [Google Scholar] [CrossRef]
- Ellis, M.J.; Ding, L.; Shen, D.; Luo, J.; Suman, V.J.; Wallis, J.W.; Van Tine, B.A.; Hoog, J.; Goiffon, R.; Goldstein, T.C.; et al. Whole-genome analysis informs breast cancer response to aromatase inhibition. Nature 2012, 486, 353–360. [Google Scholar] [CrossRef]
- Fuqua, S.A.W.; Gu, G.; Rechoum, Y. Estrogen receptor (ER) α mutations in breast cancer: Hidden in plain sight. Breast Cancer Res. Treat. 2014, 144, 11–19. [Google Scholar] [CrossRef]
- Jeselsohn, R.; Buchwalter, G.; DE Angelis, C.; Brown, M.; Schiff, R. ESR1 mutations—A mechanism for acquired endocrine resistance in breast cancer. Nat. Rev. Clin. Oncol. 2015, 12, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Stone, A.; Zotenko, E.; Locke, W.; Korbie, D.; Millar, E.; Pidsley, R.; Stirzaker, C.; Graham, P.; Trau, M.; Musgrove, E.A.; et al. DNA methylation of oestrogen-regulated enhancers defines endocrine sensitivity in breast cancer. Nat. Commun. 2015, 6, 7758. [Google Scholar] [CrossRef]
- Atlas, T.C.G. Comprehensive molecular portraits of human breast tumours. Nature 2012, 490, 61–70. [Google Scholar]
- Merenbakh-Lamin, K.; Ben-Baruch, N.; Yeheskel, A.; Dvir, A.; Soussan-Gutman, L.; Jeselsohn, R.; Yelensky, R.; Brown, M.; Miller, V.A.; Sarid, D.; et al. D538G Mutation in Estrogen Receptor-α: A Novel Mechanism for Acquired Endocrine Resistance in Breast Cancer. Cancer Res. 2013, 73, 6856–6864. [Google Scholar] [CrossRef] [PubMed]
- Robinson, D.R.; Wu, Y.-M.; Vats, P.; Su, F.; Lonigro, R.J.; Cao, X.; Kalyana-Sundaram, S.; Wang, R.; Ning, Y.; Hodges, L.; et al. Activating ESR1 mutations in hormone-resistant metastatic breast cancer. Nat. Genet. 2013, 45, 1446–1451. [Google Scholar] [CrossRef]
- Toy, W.; Weir, H.; Razavi, P.; Lawson, M.; Goeppert, A.U.; Mazzola, A.M.; Smith, A.; Wilson, J.; Morrow, C.; Wong, W.L.; et al. Activating ESR1 Mutations Differentially Affect the Efficacy of ER Antagonists. Cancer Discov. 2016, 7, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Chandarlapaty, S.; Chen, D.; He, W.; Sung, P.; Samoila, A.; You, D.; Bhatt, T.; Patel, P.; Voi, M.; Gnant, M.; et al. Prevalence of ESR1 Mutations in Cell-Free DNA and Outcomes in Metastatic Breast Cancer: A Secondary Analysis of the BOLERO-2 Clinical Trial. JAMA Oncol. 2016, 2, 1310–1315. [Google Scholar] [CrossRef]
- Fribbens, C.; O’Leary, B.; Kilburn, L.; Hrebien, S.; Garcia-Murillas, I.; Beaney, M.; Cristofanilli, M.; Andre, F.; Loi, S.; Loibl, S.; et al. Plasma ESR1 Mutations and the Treatment of Estrogen Receptor–Positive Advanced Breast Cancer. J. Clin. Oncol. 2016, 34, 2961–2968. [Google Scholar] [CrossRef] [PubMed]
- Spoerke, J.M.; Gendreau, S.; Walter, K.; Qiu, J.; Wilson, T.R.; Savage, H.; Aimi, J.; Derynck, M.K.; Chen, M.; Chan, I.T.; et al. Heterogeneity and clinical significance of ESR1 mutations in ER-positive metastatic breast cancer patients re-ceiving fulvestrant. Nat. Commun. 2016, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jeselsohn, R.; Bergholz, J.S.; Pun, M.; Cornwell, M.; Liu, W.; Nardone, A.; Xiao, T.; Li, W.; Qiu, X.; Buchwalter, G.; et al. Allele-Specific Chromatin Recruitment and Therapeutic Vulnerabilities of ESR1 Activating Mutations. Cancer Cell 2018, 33, 173–186.e5. [Google Scholar] [CrossRef] [PubMed]
- Guan, J.; Zhou, W.; Hafner, M.; Blake, R.A.; Chalouni, C.; Chen, I.; De Bruyn, T.; Giltnane, J.M.; Hartman, S.; Heidersbach, A.; et al. Therapeutic Ligands Antagonize Estrogen Receptor Function by Impairing Its Mobility. Cell 2019, 178, 949–963.e18. [Google Scholar] [CrossRef]
- Puyang, X.; Furman, C.; Zheng, G.Z.; Wu, Z.J.; Banka, D.; B, K.A.; Agoulnik, S.; Bolduc, D.M.; Buonamici, S.; Caleb, B.; et al. Discovery of Selective Estrogen Receptor Covalent Antagonists for the Treatment of ERαWT and ERαMUT Breast Cancer. Cancer Discov. 2018, 8, 1176–1193. [Google Scholar] [CrossRef]
- Hamilton, E.P.; Wang, J.S.; Pluard, T.; Johnston, S.; Morikawa, A.A.; Dees, C.E.; Jones, R.H.; Haley, B.; Armstrong, A.; Cohen, A.L.; et al. Abstract PD8-06: Phase I/II trial of H3B-6545, a novel selective estrogen receptor covalent antagonist (SER-CA), in estrogen receptor positive (ER+), human epidermal growth factor receptor 2 negative (HER2-) advanced breast cancer. Cancer Res. 2021, 81, PD8-06 LP. [Google Scholar]
- Stone, A.; Valdes-Mora, F.; Gee, J.M.W.; Farrow, L.; McClelland, R.A.; Fiegl, H.; Dutkowski, C.; McCloy, R.; Sutherland, R.L.; Musgrove, E.A.; et al. Tamoxifen-Induced Epigenetic Silencing of Oestrogen-Regulated Genes in Anti-Hormone Resistant Breast Cancer. PLoS ONE 2012, 7, e40466. [Google Scholar] [CrossRef]
- Fan, M.; Yan, P.S.; Hartman-Frey, C.; Chen, L.; Paik, H.; Oyer, S.L.; Salisbury, J.D.; Cheng, A.; Li, L.; Abbosh, P.H.; et al. Diverse Gene Expression and DNA Methylation Profiles Correlate with Differential Adaptation of Breast Cancer Cells to the Antiestrogens Tamoxifen and Fulvestrant. Cancer Res. 2006, 66, 11954–11966. [Google Scholar] [CrossRef]
- Phuong, N.T.T.; Kim, S.K.; Lim, S.C.; Kim, H.S.; Kim, T.H.; Lee, K.Y.; Ahn, S.-G.; Yoon, J.-H.; Kang, K.W. Role of PTEN promoter methylation in tamoxifen-resistant breast cancer cells. Breast Cancer Res. Treat. 2010, 130, 73–83. [Google Scholar] [CrossRef]
- Maier, S.; Nimmrich, I.; Koenig, T.; Eppenberger-Castori, S.; Bohlmann, I.; Paradiso, A.; Spyratos, F.; Thomssen, C.; Mueller, V.; Nährig, J.; et al. DNA-methylation of the homeodomain transcription factor PITX2 reliably predicts risk of distant disease recur-rence in tamoxifen-treated, node-negative breast cancer patients--Technical and clinical validation in a multi-centre setting in collaboration wi. Eur. J. Cancer 2007, 43, 1679–1686. [Google Scholar] [CrossRef] [PubMed]
- Pathiraja, T.N.; Nayak, S.R.; Xi, Y.; Jiang, S.; Garee, J.P.; Edwards, D.P.; Lee, A.V.; Chen, J.; Shea, M.J.; Santen, R.J.; et al. Epigenetic Reprogramming of HOXC10 in Endocrine-Resistant Breast Cancer. Sci. Transl. Med. 2014, 6, 229ra41. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Achinger-Kawecka, J.; Stirzaker, C.; Chia, K.; Portman, N.; Campbell, E.; Du, Q.; Laven-Law, G.; Nair, S.S.; Yong, A.; Wilkinson, A.; et al. Epigenetic therapy suppresses endocrine-resistant breast tumour growth by re-wiring ER-mediated 3D chromatin interactions. bioRxiv 2021. [Google Scholar] [CrossRef]
- Svotelis, A.; Gévry, N.; Grondin, G.; Gaudreau, L. H2A.Z overexpression promotes cellular proliferation of breast cancer cells. Cell Cycle 2010, 9, 364–370. [Google Scholar] [CrossRef]
- Nayak, S.R.; Harrington, E.; Boone, D.; Hartmaier, R.; Chen, J.; Pathiraja, T.N.; Cooper, K.L.; Fine, J.L.; Sanfilippo, J.; Davidson, N.E.; et al. A Role for Histone H2B Variants in Endocrine-Resistant Breast Cancer. Horm. Cancer 2015, 6, 214–224. [Google Scholar] [CrossRef]
- Munster, P.N.; Thurn, K.T.; Thomas, S.; Raha, P.; Lacevic, M.; Miller, A.; Melisko, M.; Ismail-Khan, R.; Rugo, H.; Moasser, M.; et al. A phase II study of the histone deacetylase inhibitor vorinostat combined with tamoxifen for the treatment of patients with hormone therapy-resistant breast cancer. Br. J. Cancer 2011, 104, 1828–1835. [Google Scholar] [CrossRef] [PubMed]
- Yardley, D.A.; Ismail-Khan, R.R.; Melichar, B.; Lichinitser, M.; Munster, P.N.; Klein, P.M.; Cruickshank, S.; Miller, K.D.; Lee, M.J.; Trepel, J.B. Randomized phase II, double-blind, placebo-controlled study of exemestane with or without entinostat in postmenopausal women with locally recurrent or metastatic estrogen receptor-positive breast cancer progressing on treat-ment with a nonsteroidal aromat. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 2128–2135. [Google Scholar] [CrossRef] [PubMed]
- Connolly, R.M.; Zhao, F.; Miller, K.D.; Lee, M.-J.; Piekarz, R.L.; Smith, K.L.; Brown-Glaberman, U.A.; Winn, J.S.; Faller, B.A.; Onitilo, A.A.; et al. E2112: Randomized Phase III Trial of Endocrine Therapy Plus Entinostat or Placebo in Hormone Receptor–Positive Advanced Breast Cancer. A Trial of the ECOG-ACRIN Cancer Research Group. J. Clin. Oncol. 2021, 81. [Google Scholar] [CrossRef]
- Pasqualini, J.R. Breast cancer and steroid metabolizing enzymes: The role of progestogens. Maturitas 2009, 65, S17–S21. [Google Scholar] [CrossRef] [PubMed]
- Brisken, C.; Hess, K.; Jeitziner, R. Progesterone and Overlooked Endocrine Pathways in Breast Cancer Pathogenesis. Endocrinology 2015, 156, 3442–3450. [Google Scholar] [CrossRef]
- Carroll, J.S.; Hickey, T.E.; Tarulli, G.A.; Williams, M.; Tilley, W.D. Deciphering the divergent roles of progestogens in breast can-cer. Nat. Rev. Cancer 2016, 17, 54–64. [Google Scholar] [CrossRef]
- Stanczyk, F.Z.; Hapgood, J.; Winer, S.; Mishell, D.R. Progestogens Used in Postmenopausal Hormone Therapy: Differences in Their Pharmacological Properties, Intracellular Actions, and Clinical Effects. Endocr. Rev. 2012, 34, 171–208. [Google Scholar] [CrossRef]
- Rakha, E.A.; El-Sayed, M.E.; Green, A.; Paish, E.C.; Powe, D.G.; Gee, J.; Nicholson, R.I.; Lee, A.H.; Robertson, J.F.; Ellis, I. Biologic and Clinical Characteristics of Breast Cancer With Single Hormone Receptor–Positive Phenotype. J. Clin. Oncol. 2007, 25, 4772–4778. [Google Scholar] [CrossRef]
- Graham, J.D.; Yeates, C.; Balleine, R.L.; Harvey, S.S.; Milliken, J.S.; Bilous, A.M.; Clarke, C. Progesterone receptor A and B protein expression in human breast cancer. J. Steroid Biochem. Mol. Biol. 1996, 56, 93–98. [Google Scholar] [CrossRef]
- Horwitz, K.; McGuire, W. Estrogen control of progesterone receptor in human breast cancer. Correlation with nuclear processing of estrogen receptor. J. Biol. Chem. 1978, 253, 2223–2228. [Google Scholar] [CrossRef]
- Chlebowski, R.T.; Manson, J.E.; Anderson, G.L.; Cauley, J.A.; Aragaki, A.K.; Stefanick, M.L.; Lane, D.S.; Johnson, K.C.; Wactawski-Wende, J.; Chen, C.; et al. Estrogen Plus Progestin and Breast Cancer Incidence and Mortality in the Women’s Health Initiative Ob-servational Study. JNCI J. Natl. Cancer Inst. 2013, 105, 526–535. [Google Scholar] [CrossRef]
- Hankinson, S.E.S.E. Towards an integrated model for breast cancer etiology: The lifelong interplay of genes, lifestyle, and hor-mones. Breast Cancer Res. 2004, 6, 213–218. [Google Scholar] [CrossRef]
- Lydon, J.P.; Ge, G.; Kittrell, F.S.; Medina, D.; O’Malley, B.W. Murine mammary gland carcinogenesis is critically dependent on progesterone receptor function. Cancer Res. 1999, 59, 4276–4284. [Google Scholar]
- Collett, K.; Hartveit, F.; Skjaerven, R.; O Maehle, B. Prognostic role of oestrogen and progesterone receptors in patients with breast cancer: Relation to age and lymph node status. J. Clin. Pathol. 1996, 49, 920–925. [Google Scholar] [CrossRef] [PubMed]
- Bardou, V.-J.; Arpino, G.; Elledge, R.M.; Osborne, C.K.; Clark, G.M. Progesterone Receptor Status Significantly Improves Outcome Prediction Over Estrogen Receptor Status Alone for Adjuvant Endocrine Therapy in Two Large Breast Cancer Databases. J. Clin. Oncol. 2003, 21, 1973–1979. [Google Scholar] [CrossRef] [PubMed]
- Viale, G.G. Prognostic and predictive value of centrally reviewed expression of estrogen and progesterone receptors in a ran-domized trial comparing letrozole and tamoxifen adjuvant therapy for postmenopausal early breast cancer: BIG 1-98. J. Clin. Oncol. 2007, 25, 3846–3852. [Google Scholar] [CrossRef]
- Blows, F.M.; Driver, K.E.; Schmidt, M.K.; Broeks, A.; Van Leeuwen, F.E.; Wesseling, J.; Cheang, M.C.U.; Gelmon, K.; Nielsen, T.O.; Blomqvist, C.; et al. Subtyping of Breast Cancer by Immunohistochemistry to Investigate a Relationship between Subtype and Short and Long Term Survival: A Collaborative Analysis of Data for 10,159 Cases from 12 Studies. PLoS Med. 2010, 7, e1000279. [Google Scholar] [CrossRef]
- Van Belle, V.V. Qualitative assessment of the progesterone receptor and HER2 improves the Nottingham Prognostic Index up to 5 years after breast cancer diagnosis. J. Clin. Oncol. 2010, 28, 4129–4134. [Google Scholar] [CrossRef] [PubMed]
- A Purdie, C.; Quinlan, P.; Jordan, L.B.; Ashfield, A.; Ogston, S.; A Dewar, J.; Thompson, A.M. Progesterone receptor expression is an independent prognostic variable in early breast cancer: A population-based study. Br. J. Cancer 2013, 110, 565–572. [Google Scholar] [CrossRef]
- Campbell, E.J.; Tesson, M.; Doogan, F.; Mohammed, Z.M.; Mallon, E.; Edwards, J. The combined endocrine receptor in breast cancer, a novel approach to traditional hormone receptor inter-pretation and a better discriminator of outcome than ER and PR alone. Br. J. Cancer 2016, 115, 967–973. [Google Scholar] [CrossRef]
- Voduc, K.D.; Cheang, M.C.U.; Tyldesley, S.; Gelmon, K.; Nielsen, T.O.; Kennecke, H. Breast Cancer Subtypes and the Risk of Local and Regional Relapse. J. Clin. Oncol. 2010, 28, 1684–1691. [Google Scholar] [CrossRef]
- Singhal, H.; Greene, M.E.; Tarulli, G.; Zarnke, A.L.; Bourgo, R.J.; Laine, M.; Chang, Y.-F.; Ma, S.; Dembo, A.G.; Raj, G.V.; et al. Genomic agonism and phenotypic antagonism between estrogen and progesterone receptors in breast cancer. Sci. Adv. 2016, 2, e1501924. [Google Scholar] [CrossRef] [PubMed]
- Vignon, F.; Bardon, S.; Chalbos, D.; Rochefort, H. Antiestrogenic Effect of R5020, a Synthetic Progestin in Human Breast Cancer Cells in Culture. J. Clin. Endocrinol. Metab. 1983, 56, 1124–1130. [Google Scholar] [CrossRef]
- Musgrove, E.A.; Swarbrick, A.; Lee, C.S.L.; Cornish, A.L.; Sutherland, R.L. Mechanisms of Cyclin-Dependent Kinase Inactivation by Progestins. Mol. Cell. Biol. 1998, 18, 1812–1825. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-C.; Hardy, D.B.; Mendelson, C.R. Progesterone Receptor Inhibits Proliferation of Human Breast Cancer Cells via Induction of MAPK Phosphatase 1 (MKP-1/DUSP1). J. Biol. Chem. 2011, 286, 43091–43102. [Google Scholar] [CrossRef] [PubMed]
- Kabos, P.; Finlay-Schultz, J.; Li, C.; Kline, E.; Finlayson, C.; Wisell, J.; Manuel, C.A.; Edgerton, S.M.; Harrell, J.C.; Elias, A.; et al. Patient-derived luminal breast cancer xenografts retain hormone receptor heterogeneity and help define unique estrogen-dependent gene signatures. Breast Cancer Res. Treat. 2012, 135, 415–432. [Google Scholar] [CrossRef] [PubMed]
- Badwe, R.R. Single-injection depot progesterone before surgery and survival in women with operable breast cancer: A random-ized controlled trial. J. Clin. Oncol. 2011, 29, 2845–2851. [Google Scholar] [CrossRef]
- Abrams, J.; Aisner, J.; Cirrincione, C.; Berry, D.A.; Muss, H.B.; Cooper, M.R.; Henderson, I.C.; Panasci, L.; Kirshner, J.; Ellerton, J.; et al. Dose-Response Trial of Megestrol Acetate in Advanced Breast Cancer: Cancer and Leukemia Group B Phase III Study. J. Clin. Oncol. 1999, 17, 64. [Google Scholar] [CrossRef]
- Alexieva-Figusch, J.; Van Gilse, H.A.; Hop, W.C.J.; Phoa, C.H.; Der Wijst, J.B.-V.; Treurniet, R.E. Progestin therapy in advanced breast cancer: Megestrol acetate—an evaluation of 160 treated cases. Cancer 1980, 46, 2369–2372. [Google Scholar] [CrossRef]
- Muss, H.B.; Paschold, E.H.; Black, W.R.; Cooper, M.R.; Capizzi, R.L.; Christian, R.; Cruz, J.M.; Jackson, D.V.; Stuart, J.J.; Richards, F. Megestrol acetate v tamoxifen in advanced breast cancer: A phase III trial of the Piedmont Oncology Association (POA). Semin. Oncol. 1985, 12, 55–61. [Google Scholar]
- Pannuti, F.; Martoni, A.; Di Marco, A.; Piana, E.; Saccani, F.; Becchi, G.; Mattioli, G.; Barbanti, F.; Marra, G.; Persiani, W.; et al. Prospective, randomized clinical trial of two different high dosages of medroxyprogesterone acetate (MAP) in the treatment of metastatic breast cancer. Eur. J. Cancer (1965) 1979, 15, 593–601. [Google Scholar] [CrossRef]
- Robertson, J.; Williams, M.; Todd, J.; Nicholson, R.; Morgan, D.; Blamey, R. Factors predicting the response of patients with advanced breast cancer to endocrine (Megace) therapy. Eur. J. Cancer Clin. Oncol. 1989, 25, 469–475. [Google Scholar] [CrossRef]
- Bines, J.; Dienstmann, R.; Obadia, R.M.; Branco, L.G.P.; Quintella, D.C.; Castro, T.M.; Camacho, P.G.; Soares, F.A.; Costa, M.E.F. Activity of megestrol acetate in postmenopausal women with advanced breast cancer after nonsteroidal aromatase inhibitor failure: A phase II trial. Ann. Oncol. 2014, 25, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Birrell, S.; Bentel, J.; Hickey, T.; Ricciardelli, C.; Weger, M.; Horsfall, D.; Tilley, W. Androgens induce divergent proliferative responses in human breast cancer cell lines. J. Steroid Biochem. Mol. Biol. 1995, 52, 459–467. [Google Scholar] [CrossRef]
- Espie, M. Megestrol Acetate in Advanced Breast Carcinoma. Oncology 1994, 51, 8–12. [Google Scholar] [CrossRef]
- Ingle, J.N.; Ahmann, D.L.; Green, S.J.; Bisel, H.F.; Frytak, S.; Edmonson, J.H.; Kvols, L.K.; Nichols, W.C.; Creagan, E.T.; Hahn, R.G.; et al. Randomized Clinical Trial of Diethylstilbestrol versus Tamoxifen in Postmenopausal Women with Advanced Breast Cancer. N. Engl. J. Med. 1981, 304, 16–21. [Google Scholar] [CrossRef]
- Izuo, M.; Iino, Y.; Endo, K. Oral high-dose medroxyprogesterone acetate (MAP) in treatment of advanced breast cancer. Breast Cancer Res. Treat. 1981, 1, 125–130. [Google Scholar] [CrossRef]
- Jonat, W.; Howell, A.; Blomqvist, C.; Eiermann, W.; Winblad, G.; Tyrrell, C.; Mauriac, L.; Roche, H.; Lundgren, S.; Hellmund, R.; et al. A randomised trial comparing two doses of the new selective aromatase inhibitor anastrozole (Arimidex) with megestrol acetate in postmenopausal patients with advanced breast cancer. Eur. J. Cancer 1996, 32, 404–412. [Google Scholar] [CrossRef]
- Mattsson, W. Current status of high dose progestin treatment in advanced breast cancer. Breast Cancer Res. Treat. 1983, 3, 231–235. [Google Scholar] [CrossRef]
- Morgan, L.R. Megestrol acetate v tamoxifen in advanced breast cancer in postmenopausal patients. Semin. Oncol. 1985, 12, 43–47. [Google Scholar] [PubMed]
- Clarke, C.L.; Graham, J.D. Non-Overlapping Progesterone Receptor Cistromes Contribute to Cell-Specific Transcriptional Outcomes. PLoS ONE 2012, 7, e35859. [Google Scholar] [CrossRef]
- Yin, P.; Roqueiro, D.; Huang, L.; Owen, J.K.; Xie, A.; Navarro, A.; Monsivais, D.; Coon V, J.S.; Kim, J.J.; Dai, Y.; et al. Genome-Wide Progesterone Receptor Binding: Cell Type-Specific and Shared Mechanisms in T47D Breast Cancer Cells and Primary Leiomyoma Cells. PLoS ONE 2012, 7, e29021. [Google Scholar] [CrossRef]
- Baird, R.; Carroll, J. Understanding Oestrogen Receptor Function in Breast Cancer and its Interaction with the Progesterone Receptor. New Preclinical Findings and their Clinical Implications. Clin. Oncol. 2015, 28, 1–3. [Google Scholar] [CrossRef][Green Version]
- Bardon, S.; Vigkpn, F.; Chalbos, D.; Rochefort, H. RU486, A Progestin and Glucocorticoid Antagonist, Inhibits the Growth of Breast Cancer Cells via the Progesterone Receptor*. J. Clin. Endocrinol. Metab. 1985, 60, 692–697. [Google Scholar] [CrossRef]
- Horwitz, K.B. The antiprogestin RU38 486: Receptor-mediated progestin versus antiprogestin actions screened in estrogen-insensitive T47Dco human breast cancer cells. Endocrinology 1985, 116, 2236–2245. [Google Scholar] [CrossRef] [PubMed]
- Musgrove, E.A.; Lee, C.S.; Cornish, A.L.; Swarbrick, A.; Sutherland, R.L. Antiprogestin inhibition of cell cycle progression in T-47D breast cancer cells is accompanied by induction of the cyclin-dependent kinase inhibitor p21. Mol. Endocrinol. 1997, 11, 54–66. [Google Scholar] [CrossRef][Green Version]
- Klijn, J.G.; Setyono-Han, B.; A Foekens, J. Progesterone antagonists and progesterone receptor modulators in the treatment of breast cancer. Steroids 2000, 65, 825–830. [Google Scholar] [CrossRef]
- Bakker, G.H.; Setyono-Han, B.; Henkelman, M.S.; De Jong, F.H.; Lamberts, S.W.; Van Der Schoot, P.; Klijn, J.G. Comparison of the actions of the antiprogestin mifepristone (RU486), the progestin megestrol acetate, the LHRH analog buserelin, and ovariectomy in treatment of rat mammary tumors. Cancer Treat. Rep. 1987, 71, 1021–1027. [Google Scholar] [PubMed]
- Michna, H.; Schneider, M.R.; Nishino, Y.; El Etreby, M.F. Antitumor activity of the antiprogestins ZK 98.299 and RU 38.486 in hormone dependent rat and mouse mammary tumors: Mechanistic studies. Breast Cancer Res. Treat. 1989, 14, 275–288. [Google Scholar] [CrossRef]
- Bakker, G.; Setyono-Han, B.; Portengen, H.; De Jong, F.; Foekens, J.; Klijn, J. Treatment of breast cancer with different antiprogestins: Preclinical and clinical studies. J. Steroid Biochem. Mol. Biol. 1990, 37, 789–794. [Google Scholar] [CrossRef]
- Iwasaki, K.; Underwood, B.; Herman, M.; Dinda, S.; Kodali, S.; Kloosterboer, H.; Hurd, C.; Moudgil, V. Effects of antiprogestins on the rate of proliferation of breast cancer cells. Mol. Cell. Biochem. 1999, 198, 141–149. [Google Scholar] [CrossRef]
- Perrault, D.; Eisenhauer, A.E.; Pritchard, I.K.; Panasci, L.; Norris, B.; Vandenberg, T.; Fisher, B. Phase II study of the progesterone antagonist mifepristone in patients with untreated metastatic breast carcino-ma: A National Cancer Institute of Canada Clinical Trials Group study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 1996, 14, 2709–2712. [Google Scholar] [CrossRef] [PubMed]
- Jonat, W.; Bachelot, T.; Ruhstaller, T.; Kuss, I.; Reimann, U.; Robertson, J.F.R. Randomized phase II study of lonaprisan as second-line therapy for progesterone receptor-positive breast cancer. Ann. Oncol. 2013, 24, 2543–2548. [Google Scholar] [CrossRef]
- Robertson, J.; Willsher, P.; Winterbottom, L.; Blamey, R.; Thorpe, S. Onapristone, a progesterone receptor antagonist, as first-line therapy in primary breast cancer. Eur. J. Cancer 1999, 35, 214–218. [Google Scholar] [CrossRef]
- Lim, E.; Ni, M.; Cao, S.; Hazra, A.; Tamimi, R.M.; Brown, M. Importance of Breast Cancer Subtype in the Development of Androgen-Receptor-Directed Therapy. Curr. Breast Cancer Rep. 2014, 6, 71–78. [Google Scholar] [CrossRef]
- Hickey, T.E.; Robinson, J.L.L.; Carroll, J.S.; Tilley, W.D. Minireview: The Androgen Receptor in Breast Tissues. Mol. Endocrinol. 2012, 26, 1252–1267. [Google Scholar] [CrossRef] [PubMed]
- Aleskandarany, M.; Abduljabbar, R.; Ashankyty, I.; Elmouna, A.; Jerjees, D.; Ali, S.; Buluwela, L.; Diez-Rodriguez, M.; Caldas, C.; Green, A.; et al. Prognostic significance of androgen receptor expression in invasive breast cancer: Transcriptomic and protein expression analysis. Breast Cancer Res. Treat. 2016, 159, 215–227. [Google Scholar] [CrossRef]
- Ricciardelli, C.; Bianco-Miotto, T.; Jindal, S.; Butler, L.M.; Leung, S.; McNeil, C.M.; O’Toole, S.A.; Ebrahimie, E.; Millar, E.K.A.; Sakko, A.J.; et al. The Magnitude of Androgen Receptor Positivity in Breast Cancer Is Critical for Reliable Prediction of Dis-ease Outcome. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2018, 24, 2328–2341. [Google Scholar] [CrossRef]
- Peters, A.A.; Buchanan, G.; Ricciardelli, C.; Bianco-Miotto, T.; Centenera, M.; Harris, J.; Jindal, S.; Segara, D.; Jia, L.; Moore, N.L.; et al. Androgen Receptor Inhibits Estrogen Receptor-α Activity and Is Prognostic in Breast Cancer. Cancer Res. 2009, 69, 6131–6140. [Google Scholar] [CrossRef]
- Truong, T.H.; A Lange, C. Deciphering Steroid Receptor Crosstalk in Hormone-Driven Cancers. Endocrinology 2018, 159, 3897–3907. [Google Scholar] [CrossRef] [PubMed]
- Panet-Raymond, V.; Gottlieb, B.; Beitel, L.K.; Pinsky, L.; A Trifiro, M. Interactions between androgen and estrogen receptors and the effects on their transactivational properties. Mol. Cell. Endocrinol. 2000, 167, 139–150. [Google Scholar] [CrossRef]
- A Greeve, M.; Allan, R.K.; Harvey, J.M.; Bentel, J.M. Inhibition of MCF-7 breast cancer cell proliferation by 5alpha-dihydrotestosterone; a role for p21(Cip1/Waf1). J. Mol. Endocrinol. 2004, 32, 793–810. [Google Scholar] [CrossRef]
- Cochrane, D.R.; Bernales, S.; Jacobsen, B.M.; Cittelly, D.M.; Howe, E.N.; D’Amato, N.C.; Spoelstra, N.S.; Edgerton, S.M.; Jean, A.; Guerrero, J.; et al. Role of the androgen receptor in breast cancer and preclinical analysis of enzalutamide. Breast Cancer Res. 2014, 16, R7. [Google Scholar] [CrossRef] [PubMed]
- D’Amato, N.C.; Gordon, M.A.; Babbs, B.L.; Spoelstra, N.S.; Butterfield, K.T.C.; Torkko, K.C.; Phan, V.T.; Barton, V.N.; Rogers, T.J.; Sartorius, C.A.; et al. Cooperative Dynamics of AR and ER Activity in Breast Cancer. Mol. Cancer Res. 2016, 14, 1054–1067. [Google Scholar] [CrossRef] [PubMed]
- Castellano, I.; Allia, E.; Accortanzo, V.; Vandone, A.M.; Chiusa, L.; Arisio, R.; Durando, A.; Donadio, M.; Bussolati, G.; Coates, A.S.; et al. Androgen receptor expression is a significant prognostic factor in estrogen receptor positive breast cancers. Breast Cancer Res. Treat. 2010, 124, 607–617. [Google Scholar] [CrossRef] [PubMed]
- Tormey, U.C.; Lippman, M.E.; Edwards, B.K.; Cassidy, J.G. Evaluation of Tamoxifen Doses with and Without Fluoxymesterone in Advanced Breast Cancer. Ann. Intern. Med. 1983, 98, 139. [Google Scholar] [CrossRef]
- Ingle, J.N.; Long, H.J.; Twito, D.I.; Schaid, D.J.; Cullinan, S.A.; Gerstner, J.G.; Krook, J.E.; Mailliard, J.A.; Tschetter, L.K.; Windschitl, H.E.; et al. Combination hormonal therapy with tamoxifen plus fluoxymesterone versus tamoxifen alone in postmenopau-sal women with metastatic breast cancer. An updated analysis. Cancer 1991, 67, 886–891. [Google Scholar] [CrossRef]
- Macedo, L.F.; Guo, Z.; Tilghman, S.L.; Sabnis, G.; Qiu, Y.; Brodie, A. Role of Androgens on MCF-7 Breast Cancer Cell Growth and on the Inhibitory Effect of Letrozole. Cancer Res. 2006, 66, 7775–7782. [Google Scholar] [CrossRef]
- Chia, K.M.; Milioli, H.; Portman, N.; Laven-Law, G.; Coulson, R.; Yong, A.; Segara, D.; Parker, A.; E Caldon, C.; Deng, N.; et al. Non-canonical AR activity facilitates endocrine resistance in breast cancer. Endocrine-Related Cancer 2019, 26, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; He, S.; Wang, D.; Patel, H.K.; Miller, C.P.; Brown, J.L.; Hattersley, G.; Saeh, J.C. Selective Androgen Receptor Modulator RAD140 Inhibits the Growth of Androgen/Estrogen Receptor–Positive Breast Cancer Models with a Distinct Mechanism of Action. Clin. Cancer Res. 2017, 23, 7608–7620. [Google Scholar] [CrossRef]
- Lim, E.; Tarulli, G.; Portman, N.; Hickey, T.; Tilley, W.D.; Palmieri, C. Pushing estrogen receptor around in breast cancer. Endocrine-Related Cancer 2016, 23, T227–T241. [Google Scholar] [CrossRef] [PubMed]
- Overmoyer, B.; Sanz-Altamira, P.; Taylor, R.P.; Hancock, M.L.; Dalton, J.T.; Johnston, M.A.; Steiner, M.S. Enobosarm: A targeted therapy for metastatic, androgen receptor positive, breast cancer. J. Clin. Oncol. 2014, 32, 568. [Google Scholar] [CrossRef]
- Palmieri, C.; Linden, H.M.; Birrell, S.; Lim, E.; Schwartzberg, L.S.; Rugo, H.S.; Cobb, P.W.; Jain, K.; Vogel, C.L.; O’Shaughnessy, J.; et al. Efficacy of enobosarm, a selective androgen receptor (AR) targeting agent, correlates with the degree of AR positivity in advanced AR+/estrogen receptor (ER)+ breast cancer in an international phase 2 clinical study. J. Clin. Oncol. 2021, 39, 1020. [Google Scholar] [CrossRef]
- Vetter, M.; Rothgiesser, K.; Li, Q.; Hawle, H.; Schönfeld, W.; Ribi, K.; Riniker, S.; Von Moos, R.; Müller, A.; Thürlimann, B. SAKK 21/12: A stratified, multicenter phase II trial of transdermal CR1447 in endocrine responsive-HER2 negative and triple negative-androgen receptor positive metastatic or locally advanced breast cancer. Ann. Oncol. 2019, 30, iii52. [Google Scholar] [CrossRef]
- Yin, A.Y.; Htun, M.; Swerdloff, R.S.; Diaz-Arjonilla, M.; Dudley, R.E.; Faulkner, S.; Bross, R.; Leung, A.; Baravarian, S.; Hull, L.; et al. Reexamination of Pharmacokinetics of Oral Testosterone Undecanoate in Hypogonadal Men With a New Self-Emulsifying Formulation. J. Androl. 2011, 33, 190–201. [Google Scholar] [CrossRef]
- Swerdloff, R.S.; Wang, C.; White, W.B.; Kaminetsky, J.; Gittelman, M.C.; Longstreth, J.A.; Dudley, R.E.; Danoff, T.M. A New Oral Testosterone Undecanoate Formulation Restores Testosterone to Normal Concentrations in Hy-pogonadal Men. J. Clin. Endocrinol. Metab. 2020, 105, 2515–2531. [Google Scholar] [CrossRef]
- Vera-Badillo, F.E.; Templeton, A.J.; De Gouveia, P.; Diaz-Padilla, I.; Bedard, P.; Al-Mubarak, M.; Seruga, B.; Tannock, I.F.; Ocana, A.; Amir, E. Androgen Receptor Expression and Outcomes in Early Breast Cancer: A Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2013, 106, djt319. [Google Scholar] [CrossRef]
- Proverbs-Singh, T.; Feldman, J.L.; Morris, M.J.; Autio, K.A.; Traina, T.A. Targeting the androgen receptor in prostate and breast cancer: Several new agents in development. Endocrine-Related Cancer 2015, 22, R87–R106. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, B.D.; Bauer, J.A.; Chen, X.; Sanders, M.E.; Chakravarthy, A.B.; Shyr, Y.; Pietenpol, J.A. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of target-ed therapies. J. Clin. Invest. 2011, 121, 2750–2767. [Google Scholar] [CrossRef]
- Brumec, M.; Sobočan, M.; Takač, I.; Arko, D. Clinical Implications of Androgen-Positive Triple-Negative Breast Cancer. Cancers 2021, 13, 1642. [Google Scholar] [CrossRef]
- Gucalp, A.; Tolaney, S.; Isakoff, S.J.; Ingle, J.N.; Liu, M.C.; Carey, L.A.; Blackwell, K.; Rugo, H.; Nabell, L.; Forero, A.; et al. Phase II trial of bicalutamide in patients with androgen receptor-positive, estrogen receptor-negative metastatic Breast Cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2013, 19, 5505–5512. [Google Scholar] [CrossRef]
- Traina, T.A.; Miller, K.; Yardley, D.A.; Eakle, J.; Schwartzberg, L.S.; O’Shaughnessy, J.; Gradishar, W.; Schmid, P.; Winer, E.; Kelly, C.M.; et al. Enzalutamide for the Treatment of Androgen Receptor–Expressing Triple-Negative Breast Cancer. J. Clin. Oncol. 2018, 36, 884–890. [Google Scholar] [CrossRef] [PubMed]
- Krop, I.; Abramson, V.G.; Colleoni, M.; Traina, T.A.; A Holmes, F.; Garcia-Estevez, L.; Hart, L.; Awada, A.; Zamagni, C.; Morris, P.G.; et al. A Randomized Placebo Controlled Phase II Trial Evaluating Exemestane with or without Enzalutamide in Patients with Hormone Receptor–Positive Breast Cancer. Clin. Cancer Res. 2020, 26, 6149–6157. [Google Scholar] [CrossRef]
- Christenson, J.L.; O’Neill, K.I.; Williams, M.M.; Spoelstra, N.S.; Jones, K.L.; Trahan, G.D.; Reese, J.; Van Patten, E.T.; Elias, A.; Eisner, J.R.; et al. Activity of Combined Androgen Receptor Antagonism and Cell Cycle Inhibition in Androgen Receptor Positive Triple Negative Breast Cancer. Mol. Cancer Ther. 2021, 20, 1062–1071. [Google Scholar] [CrossRef]
- Gucalp, A.; Boyle, L.A.; Alano, T.; Arumov, A.; Gounder, M.M.; Patil, S.; Feigin, K.; Edelweiss, M.; D’Andrea, G.; Bromberg, J.; et al. Phase II trial of bicalutamide in combination with palbociclib for the treatment of androgen receptor (+) meta-static breast cancer. J. Clin. Oncol. 2020, 38, 1017. [Google Scholar] [CrossRef]
- Gucalp, A.; Traina, T.A. Targeting the androgen receptor in triple-negative breast cancer. Curr. Probl. Cancer 2016, 40, 141–150. [Google Scholar] [CrossRef]
- Michmerhuizen, A.R.; Chandler, B.; Olsen, E.; Wilder-Romans, K.; Moubadder, L.; Liu, M.; Pesch, A.; Zhang, A.; Ritter, C.; Ward, S.T.; et al. Seviteronel, a Novel CYP17 Lyase Inhibitor and Androgen Receptor Antagonist, Radiosensitizes AR-Positive Triple Negative Breast Cancer Cells. Front. Endocrinol. 2020, 11, 35. [Google Scholar] [CrossRef] [PubMed]
- Abduljabbar, R.; Negm, O.H.; Lai, C.-F.; Jerjees, D.A.; Al-Kaabi, M.; Hamed, M.R.; Tighe, P.; Buluwela, L.; Mukherjee, A.; Green, A.; et al. Clinical and biological significance of glucocorticoid receptor (GR) expression in breast cancer. Breast Cancer Res. Treat. 2015, 150, 335–346. [Google Scholar] [CrossRef]
- Noureddine, L.; Trédan, O.; Hussein, N.; Badran, B.; Le Romancer, M.; Poulard, C. Glucocorticoid Receptor: A Multifaceted Actor in Breast Cancer. Int. J. Mol. Sci. 2021, 22, 4446. [Google Scholar] [CrossRef]
- Pan, D.; Kocherginsky, M.; Conzen, S.D. Activation of the Glucocorticoid Receptor Is Associated with Poor Prognosis in Estrogen Receptor-Negative Breast Cancer. Cancer Res. 2011, 71, 6360–6370. [Google Scholar] [CrossRef]
- West, D.C.; Pan, D.; Tonsing-Carter, E.; Hernandez, K.M.; Pierce, C.F.; Styke, S.C.; Bowie, K.; Garcia, T.I.; Kocherginsky, M.; Conzen, S.D. GR and ER Coactivation Alters the Expression of Differentiation Genes and Associates with Improved ER+ Breast Cancer Outcome. Mol. Cancer Res. 2016, 14, 707–719. [Google Scholar] [CrossRef]
- Miranda, T.B.; Voss, T.C.; Sung, M.; Baek, S.; John, S.; Hawkins, M.; Grøntved, L.; Schiltz, R.L.; Hager, G.L. Reprogramming the chromatin landscape: Interplay of the estrogen and glucocorticoid receptors at the ge-nomic level. Cancer Res. 2013, 73, 5130–5139. [Google Scholar] [CrossRef] [PubMed]
- Voss, T.C.; Schiltz, R.L.; Sung, M.-H.; Yen, P.; Stamatoyannopoulos, J.A.; Biddie, S.; Johnson, T.A.; Miranda, T.B.; John, S.; Hager, G.L. Dynamic Exchange at Regulatory Elements during Chromatin Remodeling Underlies Assisted Loading Mechanism. Cell 2011, 146, 544–554. [Google Scholar] [CrossRef]
- Keith, B.D. Systematic review of the clinical effect of glucocorticoids on nonhematologic malignancy. BMC Cancer 2008, 8, 1–19. [Google Scholar] [CrossRef]
- Lietzen, L.W.; Ahern, T.; Christiansen, P.; Jensen, A.B.; Sørensen, H.T.; Lash, T.L.; Cronin-Fenton, D.P. Glucocorticoid prescriptions and breast cancer recurrence: A Danish nationwide prospective cohort study. Ann. Oncol. 2014, 25, 2419–2425. [Google Scholar] [CrossRef]
- Skor, M.N.; Wonder, E.L.; Kocherginsky, M.; Goyal, A.; Hall, B.A.; Cai, Y.; Conzen, S.D. Glucocorticoid Receptor Antagonism as a Novel Therapy for Triple-Negative Breast Cancer. Clin. Cancer Res. 2013, 19, 6163–6172. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Lan, X.; Wu, D.; Sunkel, B.; Ye, Z.; Huang, J.; Liu, Z.; Clinton, S.K.; Jin, V.X.; Wang, Q. Ligand-dependent genomic function of glucocorticoid receptor in triple-negative breast cancer. Nat. Commun. 2015, 6, 8323. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, G.; Ruggeri, N.; Zannini, A.; Ingallina, E.; Bertolio, R.; Marotta, C.; Neri, C.; Cappuzzello, E.; Forcato, M.; Rosato, A.; et al. Glucocorticoid receptor signalling activates YAP in breast cancer. Nat. Commun. 2017, 8, 14073. [Google Scholar] [CrossRef] [PubMed]
- Obradovic, M.; Hamelin, B.; Manevski, N.; Couto, J.P.; Sethi, A.; Coissieux, M.-M.; Muenst, S.; Okamoto, R.; Kohler, H.; Schmidt, A.; et al. Glucocorticoids promote breast cancer metastasis. Nature 2019, 567, 540–544. [Google Scholar] [CrossRef]
- Nanda, R.; Stringer-Reasor, E.M.; Saha, P.; Kocherginsky, M.; Gibson, J.; Libao, B.; Hoffman, P.C.; Obeid, E.; Merkel, D.E.; Khramtsova, G.; et al. A randomized phase I trial of nanoparticle albumin-bound paclitaxel with or without mifepristone for advanced breast cancer. SpringerPlus 2016, 5, 947. [Google Scholar] [CrossRef]
- Sasano, H.; Frost, A.R.; Saitoh, R.; Matsunaga, G.; Nagura, H.; Krozowski, Z.S.; Silverberg, S.G. Localization of mineralocorticoid receptor and 11 beta-hydroxysteroid dehydrogenase type II in human breast and its disorders. Anticancer. Res. 1997, 17, 2001–2007. [Google Scholar]
- Leo, J.C.L.; Guo, C.; Woon, C.T.; Aw, S.E.; Lin, V.C.L. Glucocorticoid and Mineralocorticoid Cross-Talk with Progesterone Receptor to Induce Focal Adhesion and Growth Inhibition in Breast Cancer Cells. Endocrinology 2004, 145, 1314–1321. [Google Scholar] [CrossRef]
- Doan, T.B.; Cheung, V.; Clyne, C.D.; Hilton, H.N.; Eriksson, N.; Young, M.J.; Funder, J.W.; Muscat, G.E.O.; Fuller, P.J.; Clarke, C.L.; et al. A tumour suppressive relationship between mineralocorticoid and retinoic acid receptors activates a transcrip-tional program consistent with a reverse Warburg effect in breast cancer. Breast Cancer Res. 2020, 22, 122. [Google Scholar] [CrossRef]
- Johansson, H.J.; Sanchez, B.C.; Mundt, F.; Forshed, J.; Kovács, A.; Panizza, E.; Hultin-Rosenberg, L.; Lundgren, B.; Martens, U.; Máthé, G.; et al. Retinoic acid receptor alpha is associated with tamoxifen resistance in breast cancer. Nat. Commun. 2013, 4, 2175. [Google Scholar] [CrossRef]
- Garattini, E.; Bolis, M.; Garattini, S.K.; Fratelli, M.; Centritto, F.; Paroni, G.; Gianni’, M.; Zanetti, A.; Pagani, A.; Fisher, J.N.; et al. Retinoids and breast cancer: From basic studies to the clinic and back again. Cancer Treat. Rev. 2014, 40, 739–749. [Google Scholar] [CrossRef]
- Fettig, L.M.; McGinn, O.; Finlay-Schultz, J.; LaBarbera, D.V.; Nordeen, S.K.; A Sartorius, C. Cross talk between progesterone receptors and retinoic acid receptors in regulation of cytokeratin 5-positive breast cancer cells. Oncogene 2017, 36, 6074–6084. [Google Scholar] [CrossRef][Green Version]
- Xu, H.; Liu, Z.; Shi, H.; Wang, C. Prognostic role of vitamin D receptor in breast cancer: A systematic review and meta-analysis. BMC Cancer 2020, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hossain, S.; Beydoun, M.A.; Beydoun, H.A.; Chen, X.; Zonderman, A.B.; Wood, R.J. Vitamin D and breast cancer: A systematic review and meta-analysis of observational studies. Clin. Nutr. ESPEN 2018, 30, 170–184. [Google Scholar] [CrossRef] [PubMed]
- Estébanez, N.; Gómez-Acebo, I.; Palazuelos, C.; Llorca, J.; Dierssen-Sotos, T. Vitamin D exposure and Risk of Breast Cancer: A me-ta-analysis. Sci. Rep. 2018, 8, 9039. [Google Scholar] [CrossRef] [PubMed]
- Dizdar, O.; Harputluoglu, H.; Altundag, K. Vitamin D Intake and Breast Cancer Risk in Postmenopausal Women. Arch. Intern. Med. 2007, 167, 2532. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.; Elser, C.; Ennis, M.; Goodwin, P.J. Blood levels of vitamin D and early stage breast cancer prognosis: A systematic review and meta-analysis. Breast Cancer Res. Treat. 2013, 141, 331–339. [Google Scholar] [CrossRef] [PubMed]
- So, J.Y.; Lee, H.J.; Smolarek, A.K.; Paul, S.; Wang, C.-X.; Maehr, H.; Uskokovic, M.; Zheng, X.; Conney, A.H.; Cai, L.; et al. A Novel Gemini Vitamin D Analog Represses the Expression of a Stem Cell Marker CD44 in Breast Cancer. Mol. Pharmacol. 2010, 79, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Cohen, D.J.; Schwartz, N.; Muktipaty, C.; Koblinski, J.E.; Boyan, B.D.; Schwartz, Z. 24R,25-Dihydroxyvitamin D3 regulates breast cancer cells in vitro and in vivo. Biochim. Biophys. Acta (BBA)—Gen. Subj. 2019, 1863, 1498–1512. [Google Scholar] [CrossRef]
- Narvaez, C.J.; Zinser, G.; Welsh, J. Functions of 1alpha,25-dihydroxyvitamin D(3) in mammary gland: From normal development to breast cancer. Steroids 2001, 66, 301–308. [Google Scholar] [CrossRef]
- Welsh, J. Vitamin D and breast cancer: Past and present. J. Steroid Biochem. Mol. Biol. 2018, 177, 15–20. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).