Neoadjuvant Treatment for Pancreatic Adenocarcinoma: A False Promise or an Opportunity to Improve Outcome?
Abstract
:Simple Summary
Abstract
1. Introduction
2. Biomarkers
2.1. Diagnostic Biomarkers
2.2. Prognostic Biomarkers and Predictors of Resectability
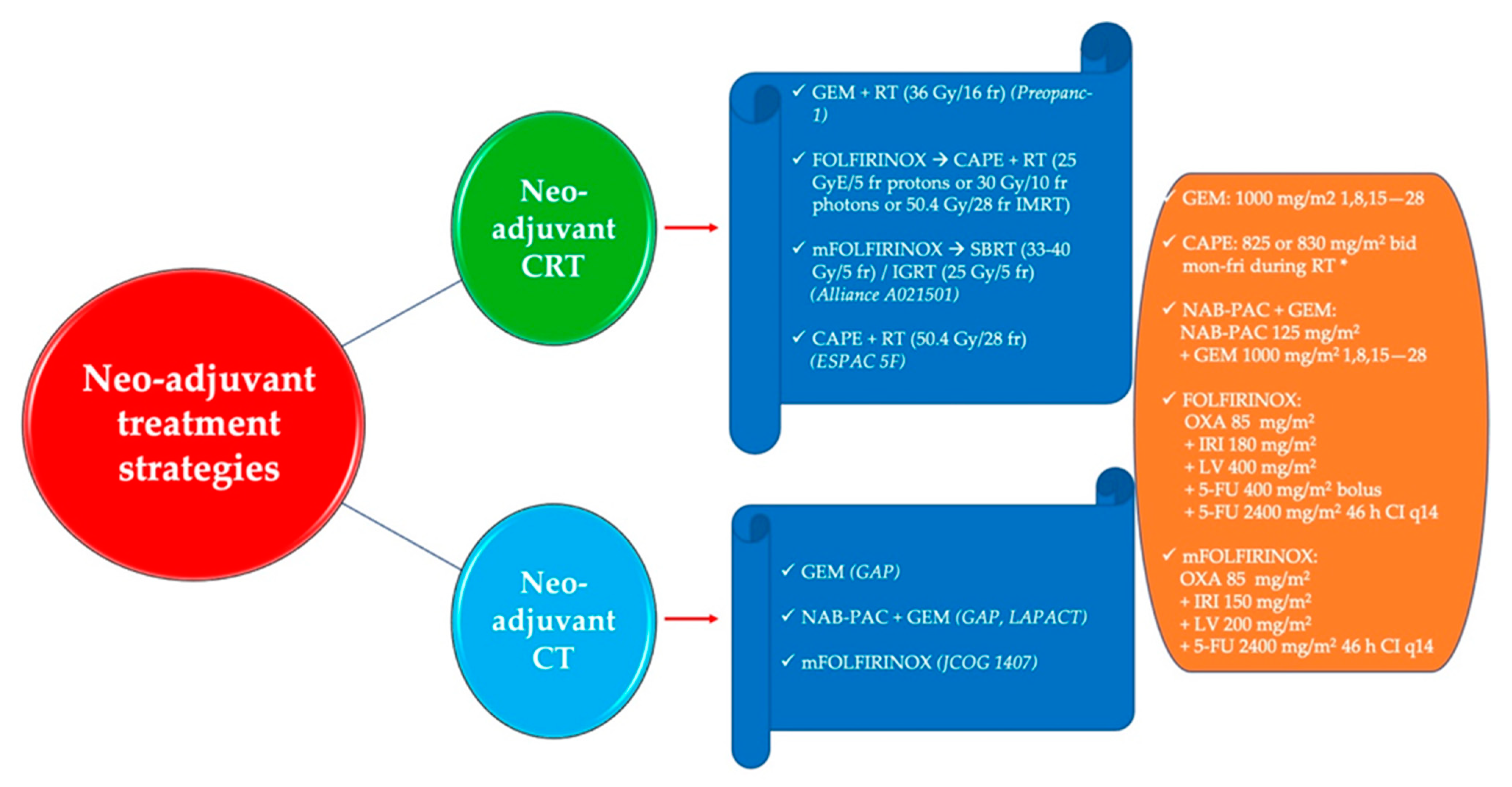
3. Neo-Adjuvant Treatment Strategies
3.1. The Role of Neo-Adjuvant Chemoradiotherapy
3.2. Neo-Adjuvant and Perioperative Chemotherapy
3.3. Immunotherapy in the Neo-Adjuvant Setting for PDAC
3.4. The Role of the Microbiome in the Neo-Adjuvant Treatment of PDAC
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. Cancer Today. Available online: https://gco.iarc.fr/today/online-analysis-map?v=2020&mode=population&mode_population=continents&population=900&populations=900&key=asr&sex=0&cancer=13&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&nb_items=10&gr (accessed on 23 August 2021).
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Dyba, T.; Randi, G.; Bettio, M.; Gavin, A.; Visser, O.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur. J. Cancer 2018, 103, 356–387. [Google Scholar] [CrossRef]
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the united states. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carioli, G.; Malvezzi, M.; Bertuccio, P.; Boffetta, P.; Levi, F.; La Vecchia, C.; Negri, E. European cancer mortality predictions for the year 2021 with focus on pancreatic and female lung cancer. Ann. Oncol. 2021, 32, 478–487. [Google Scholar] [CrossRef]
- Sahin, I.H.; Iacobuzio-Donahue, C.A.; O’Reilly, E.M. Molecular signature of pancreatic adenocarcinoma: An insight from genotype to phenotype and challenges for targeted therapy. Expert Opin. Ther. Targets 2016, 20, 341–359. [Google Scholar] [CrossRef] [PubMed]
- Ducreux, M.; Cuhna, A.S.; Caramella, C.; Hollebecque, A.; Burtin, P.; Goéré, D.; Seufferlein, T.; Haustermans, K.; Van Laethem, J.L.; Conroy, T.; et al. Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26, v56–v68. [Google Scholar] [CrossRef]
- Navez, J.; Bouchart, C.; Lorenzo, D.; Bali, M.A.; Closset, J.; van Laethem, J.-L. What Should Guide the Performance of Venous Resection During Pancreaticoduodenectomy for Pancreatic Ductal Adenocarcinoma with Venous Contact? Ann. Surg. Oncol. 2021. [Google Scholar] [CrossRef]
- Ouaïssi, M.; Turrini, O.; Hubert, C.; Louis, G.; Gigot, J.-F.; Mabrut, J.-Y. Vascular resection during radical resection of pancreatic adenocarcinomas: Evolution over the past 15 years. J. Hepatobil. Pancreat. Sci. 2014, 21, 623–638. [Google Scholar] [CrossRef] [Green Version]
- NCCN Clinical Practice Guidelines in Oncology Pancreatic Adenocarcinoma Version 1. 2020. Available online: https://www2.tri-kobe.org/nccn/guideline/archive/pancreas2020/english/pancreatic.pdf (accessed on 14 June 2021).
- Isaji, S.; Mizuno, S.; Windsor, J.A.; Bassi, C.; Fernández-del Castillo, C.; Hackert, T.; Hayasaki, A.; Katz, M.H.G.; Kim, S.-W.; Kishiwada, M.; et al. International consensus on definition and criteria of borderline resectable pancreatic ductal adenocarcinoma 2017. Pancreatology 2018, 18, 2–11. [Google Scholar] [CrossRef]
- Callery, M.P.; Chang, K.J.; Fishman, E.K.; Talamonti, M.S.; William Traverso, L.; Linehan, D.C. Pretreatment Assessment of Resectable and Borderline Resectable Pancreatic Cancer: Expert Consensus Statement. Ann. Surg. Oncol. 2009, 16, 1727–1733. [Google Scholar] [CrossRef]
- Katz, M.H.G.; Pisters, P.W.T.; Evans, D.B.; Sun, C.C.; Lee, J.E.; Fleming, J.B.; Vauthey, J.N.; Abdalla, E.K.; Crane, C.H.; Wolff, R.A.; et al. Borderline Resectable Pancreatic Cancer: The Importance of This Emerging Stage of Disease. J. Am. Coll. Surg. 2008, 206, 833–846. [Google Scholar] [CrossRef] [Green Version]
- Varadhachary, G.R.; Tamm, E.P.; Abbruzzese, J.L.; Xiong, H.Q.; Crane, C.H.; Wang, H.; Lee, J.E.; Pisters, P.W.T.; Evans, D.B.; Wolff, R.A. Borderline Resectable Pancreatic Cancer: Definitions, Management, and Role of Preoperative Therapy. Ann. Surg. Oncol. 2006, 13, 1035–1046. [Google Scholar] [CrossRef]
- Katz, M.H.G.; Marsh, R.; Herman, J.M.; Shi, Q.; Collison, E.; Venook, A.P.; Kindler, H.L.; Alberts, S.R.; Philip, P.; Lowy, A.M.; et al. Borderline Resectable Pancreatic Cancer: Need for Standardization and Methods for Optimal Clinical Trial Design. Ann. Surg. Oncol. 2013, 20, 2787–2795. [Google Scholar] [CrossRef]
- Bengtsson, A.; Andersson, R.; Ansari, D. The actual 5-year survivors of pancreatic ductal adenocarcinoma based on real-world data. Sci. Rep. 2020, 10, 16425. [Google Scholar] [CrossRef]
- Sener, S.F.; Fremgen, A.; Menck, H.R.; Winchester, D.P. Pancreatic cancer: A report of treatment and survival trends for 100,313 patients diagnosed from 1985–1995, using the National Cancer Database 11 No competing interests declared. J. Am. Coll. Surg. 1999, 189, 1–7. [Google Scholar] [CrossRef]
- Conroy, T.; Hammel, P.; Hebbar, M.; Ben Abdelghani, M.; Wei, A.C.; Raoul, J.-L.; Choné, L.; Francois, E.; Artru, P.; Biagi, J.J.; et al. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N. Engl. J. Med. 2018, 379, 2395–2406. [Google Scholar] [CrossRef]
- Von Hoff, D.D.; Ervin, T.; Arena, F.P.; Chiorean, E.G.; Infante, J.; Moore, M.; Seay, T.; Tjulandin, S.A.; Ma, W.W.; Saleh, M.N.; et al. Increased Survival in Pancreatic Cancer with nab-Paclitaxel plus Gemcitabine. N. Engl. J. Med. 2013, 369, 1691–1703. [Google Scholar] [CrossRef] [Green Version]
- Tempero, M.A.; Reni, M.; Riess, H.; Pelzer, U.; O’Reilly, E.M.; Winter, J.M.; Oh, D.-Y.; Li, C.-P.; Tortora, G.; Chang, H.-M.; et al. APACT: Phase III, multicenter, international, open-label, randomized trial of adjuvant nab-paclitaxel plus gemcitabine ( nab-P/G) vs gemcitabine (G) for surgically resected pancreatic adenocarcinoma. J. Clin. Oncol. 2019, 37, 4000. [Google Scholar] [CrossRef]
- Tempero, M.; O’Reilly, E.; Van Cutsem, E.; Berlin, J.; Philip, P.; Goldstein, D.; Tabernero, J.; Borad, M.; Bachet, J.; Parner, V.; et al. LBA-1 Phase 3 APACT trial of adjuvant nab-paclitaxel plus gemcitabine (nab-P + Gem) vs gemcitabine (Gem) alone in patients with resected pancreatic cancer (PC): Updated 5-year overall survival. Ann. Oncol. 2021, 32, S226. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Dunn, J.A.; Stocken, D.D.; Almond, J.; Link, K.; Beger, H.; Bassi, C.; Falconi, M.; Pederzoli, P.; Dervenis, C.; et al. Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: A randomised controlled trial. Lancet 2001, 358, 1576–1585. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Stocken, D.D.; Friess, H.; Bassi, C.; Dunn, J.A.; Hickey, H.; Beger, H.; Fernandez-Cruz, L.; Dervenis, C.; Lacaine, F.; et al. A Randomized Trial of Chemoradiotherapy and Chemotherapy after Resection of Pancreatic Cancer. N. Engl. J. Med. 2004, 350, 1200–1210. [Google Scholar] [CrossRef] [Green Version]
- Oettle, H.; Post, S.; Neuhaus, P.; Gellert, K.; Langrehr, J.; Ridwelski, K.; Schramm, H.; Fahlke, J.; Zuelke, C.; Burkart, C.; et al. Adjuvant Chemotherapy with Gemcitabine vs. Observation in Patients Undergoing Curative-Intent Resection of Pancreatic Cancer. JAMA 2007, 297, 267–277. [Google Scholar] [CrossRef]
- Oettle, H.; Neuhaus, P.; Hochhaus, A.; Hartmann, J.T.; Gellert, K.; Ridwelski, K.; Niedergethmann, M.; Zülke, C.; Fahlke, J.; Arning, M.B.; et al. Adjuvant Chemotherapy with Gemcitabine and Long-term Outcomes Among Patients With Resected Pancreatic Cancer. JAMA 2013, 310, 1473–1481. [Google Scholar] [CrossRef] [Green Version]
- Neoptolemos, J.P.; Stocken, D.D.; Bassi, C.; Ghaneh, P.; Cunningham, D.; Goldstein, D.; Padbury, R.; Moore, M.J.; Gallinger, S.; Mariette, C.; et al. Adjuvant Chemotherapy with Fluorouracil Plus Folinic Acid vs. Gemcitabine Following Pancreatic Cancer Resection. JAMA 2010, 304, 1073–1081. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Palmer, D.H.; Ghaneh, P.; Psarelli, E.E.; Valle, J.W.; Halloran, C.M.; Faluyi, O.; O’Reilly, D.A.; Cunningham, D.; Wadsley, J.; et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): A multicentre, open-label, randomised, phase 3 trial. Lancet 2017, 389, 1011–1024. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Palmer, D.H.; Ghaneh, P.; Valle, J.W.; Cunningham, D.; Wadsley, J.; Meyer, T.; Anthoney, A.; Glimelius, B.; Falk, S.; et al. ESPAC-4: A multicenter, international, open-label randomized controlled phase III trial of adjuvant combination chemotherapy of gemcitabine (GEM) and capecitabine (CAP) vs. monotherapy gemcitabine in patients with resected pancreatic ductal adenocarcin. J. Clin. Oncol. 2020, 38, 4516. [Google Scholar] [CrossRef]
- Uesaka, K.; Boku, N.; Fukutomi, A.; Okamura, Y.; Konishi, M.; Matsumoto, I.; Kaneoka, Y.; Shimizu, Y.; Nakamori, S.; Sakamoto, H.; et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: A phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet 2016, 388, 248–257. [Google Scholar] [CrossRef]
- Altman, A.M.; Wirth, K.; Marmor, S.; Lou, E.; Chang, K.; Hui, J.Y.C.; Tuttle, T.M.; Jensen, E.H.; Denbo, J.W. Completion of Adjuvant Chemotherapy After Upfront Surgical Resection for Pancreatic Cancer Is Uncommon Yet Associated With Improved Survival. Ann. Surg. Oncol. 2019, 26, 4108–4116. [Google Scholar] [CrossRef]
- Bilimoria, K.Y.; Bentrem, D.J.; Ko, C.Y.; Tomlinson, J.S.; Stewart, A.K.; Winchester, D.P.; Talamonti, M.S. Multimodality therapy for pancreatic cancer in the U.S. Cancer 2007, 110, 1227–1234. [Google Scholar] [CrossRef]
- Ma, S.J.; Oladeru, O.T.; Miccio, J.A.; Iovoli, A.J.; Hermann, G.M.; Singh, A.K. Association of Timing of Adjuvant Therapy with Survival in Patients With Resected Stage I to II Pancreatic Cancer. JAMA Netw. Open 2019, 2, e199126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valle, J.W.; Palmer, D.; Jackson, R.; Cox, T.; Neoptolemos, J.P.; Ghaneh, P.; Rawcliffe, C.L.; Bassi, C.; Stocken, D.D.; Cunningham, D.; et al. Optimal Duration and Timing of Adjuvant Chemotherapy After Definitive Surgery for Ductal Adenocarcinoma of the Pancreas: Ongoing Lessons From the ESPAC-3 Study. J. Clin. Oncol. 2014, 32, 504–512. [Google Scholar] [CrossRef] [Green Version]
- Jones, R.P.; Psarelli, E.-E.; Jackson, R.; Ghaneh, P.; Halloran, C.M.; Palmer, D.H.; Campbell, F.; Valle, J.W.; Faluyi, O.; O’Reilly, D.A.; et al. Patterns of Recurrence After Resection of Pancreatic Ductal Adenocarcinoma. JAMA Surg. 2019, 154, 1038–1048. [Google Scholar] [CrossRef]
- Hanna-Sawires, R.G.; Schiphuis, J.H.; Wuhrer, M.; Vasen, H.F.A.; van Leerdam, M.E.; Bonsing, B.A.; Mesker, W.E.; van der Burgt, Y.E.M.; Tollenaar, R.A.E.M. Clinical Perspective on Proteomic and Glycomic Biomarkers for Diagnosis, Prognosis, and Prediction of Pancreatic Cancer. Int. J. Mol. Sci. 2021, 22, 2655. [Google Scholar] [CrossRef]
- Xing, H.; Wang, J.; Wang, Y.; Tong, M.; Hu, H.; Huang, C.; Li, D. Diagnostic Value of CA 19-9 and Carcinoembryonic Antigen for Pancreatic Cancer: A Meta-Analysis. Gastroenterol. Res. Pract. 2018, 2018, 8704751. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Lee, E.; Park, K.-J.; Park, H.-D.; Kim, J.-W.; Woo, H.I.; Lee, K.H.; Lee, K.-T.; Lee, J.K.; Park, J.-O.; et al. Large-scale clinical validation of biomarkers for pancreatic cancer using a mass spectrometry-based proteomics approach. Oncotarget 2017, 8, 42761–42771. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.; Bamlet, W.R.; Oberg, A.L.; Chaffee, K.G.; Donahue, G.; Cao, X.-J.; Chari, S.; Garcia, B.A.; Petersen, G.M.; Zaret, K.S. Detection of early pancreatic ductal adenocarcinoma with thrombospondin-2 and CA19-9 blood markers. Sci. Transl. Med. 2017, 9, eaah5583. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Zheng, W.; Wang, W.; Shen, H.; Liu, L.; Lou, W.; Wang, X.; Yang, P. A new panel of pancreatic cancer biomarkers discovered using a mass spectrometry-based pipeline. Br. J. Cancer 2017, 117, 1846–1854. [Google Scholar] [CrossRef] [PubMed]
- Staal, B.; Liu, Y.; Barnett, D.; Hsueh, P.; He, Z.; Gao, C.; Partyka, K.; Hurd, M.W.; Singhi, A.D.; Drake, R.R.; et al. The sTRA Plasma Biomarker: Blinded Validation of Improved Accuracy Over CA19-9 in Pancreatic Cancer Diagnosis. Clin. Cancer Res. 2019, 25, 2745–2754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sefrioui, D.; Blanchard, F.; Toure, E.; Basile, P.; Beaussire, L.; Dolfus, C.; Perdrix, A.; Paresy, M.; Antonietti, M.; Iwanicki-Caron, I.; et al. Diagnostic value of CA19.9, circulating tumour DNA and circulating tumour cells in patients with solid pancreatic tumours. Br. J. Cancer 2017, 117, 1017–1025. [Google Scholar] [CrossRef]
- Lee, B.; Lipton, L.; Cohen, J.; Tie, J.; Javed, A.A.; Li, L.; Goldstein, D.; Burge, M.; Cooray, P.; Nagrial, A.; et al. Circulating tumor DNA as a potential marker of adjuvant chemotherapy benefit following surgery for localized pancreatic cancer. Ann. Oncol. 2019, 30, 1472–1478. [Google Scholar] [CrossRef]
- Wang, Z.-Y.; Ding, X.-Q.; Zhu, H.; Wang, R.-X.; Pan, X.-R.; Tong, J.-H. KRAS Mutant Allele Fraction in Circulating Cell-Free DNA Correlates with Clinical Stage in Pancreatic Cancer Patients. Front. Oncol. 2019, 9, 1295. [Google Scholar] [CrossRef]
- Bernard, V.; Kim, D.U.; San Lucas, F.A.; Castillo, J.; Allenson, K.; Mulu, F.C.; Stephens, B.M.; Huang, J.; Semaan, A.; Guerrero, P.A.; et al. Circulating Nucleic Acids Are Associated with Outcomes of Patients With Pancreatic Cancer. Gastroenterology 2019, 156, 108–118.e4. [Google Scholar] [CrossRef] [Green Version]
- Buscail, E.; Maulat, C.; Muscari, F.; Chiche, L.; Cordelier, P.; Dabernat, S.; Alix-Panabières, C.; Buscail, L. Liquid Biopsy Approach for Pancreatic Ductal Adenocarcinoma. Cancers 2019, 11, 852. [Google Scholar] [CrossRef] [Green Version]
- Heredia-Soto, V.; Rodríguez-Salas, N.; Feliu, J. Liquid Biopsy in Pancreatic Cancer: Are We Ready to Apply It in the Clinical Practice? Cancers 2021, 13, 1986. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, R.; Taly, V.; Zhao, S.; Pietrasz, D.; Bachet, J.-B.; Basile, D.; Mas, L.; Zaanan, A.; Laurent-Puig, P.; Taieb, J. Plasma circulating tumor DNA in pancreatic adenocarcinoma for screening, diagnosis, prognosis, treatment and follow-up: A systematic review. Cancer Treat. Rev. 2020, 87, 102028. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhang, H.; Chen, N.; Hao, J.; Jin, H.; Ma, X. Diagnostic value of various liquid biopsy methods for pancreatic cancer: A systematic review and meta-analysis. Medicine 2020, 99, e18581. [Google Scholar] [CrossRef]
- Liu, H.; Qiao, S.; Fan, X.; Gu, Y.; Zhang, Y.; Huang, S. Role of exosomes in pancreatic cancer. Oncol. Lett. 2021, 21, 298. [Google Scholar] [CrossRef]
- Mortoglou, M.; Tabin, Z.K.; Arisan, E.D.; Kocher, H.M.; Uysal-Onganer, P. Non-coding RNAs in pancreatic ductal adenocarcinoma: New approaches for better diagnosis and therapy. Transl. Oncol. 2021, 14, 101090. [Google Scholar] [CrossRef]
- Ikuta, S.; Aihara, T.; Yamanaka, N. Preoperative C-reactive protein to albumin ratio is a predictor of survival after pancreatic resection for pancreatic ductal adenocarcinoma. Asia. Pac. J. Clin. Oncol. 2019, 15, e109–e114. [Google Scholar] [CrossRef] [PubMed]
- Dimitrakopoulos, C.; Vrugt, B.; Flury, R.; Schraml, P.; Knippschild, U.; Wild, P.; Hoerstrup, S.; Henne-Bruns, D.; Wuerl, P.; Graf, R.; et al. Identification and Validation of a Biomarker Signature in Patients with Resectable Pancreatic Cancer via Genome-Wide Screening for Functional Genetic Variants. JAMA Surg. 2019, 154, e190484. [Google Scholar] [CrossRef]
- Miyake, K.; Mori, R.; Homma, Y.; Matsuyama, R.; Okayama, A.; Murakami, T.; Hirano, H.; Endo, I. MZB1 in borderline resectable pancreatic cancer resected after neoadjuvant chemoradiotherapy. J. Surg. Res. 2017, 220, 391–401. [Google Scholar] [CrossRef]
- Gao, C.; Wisniewski, L.; Liu, Y.; Staal, B.; Beddows, I.; Plenker, D.; Aldakkak, M.; Hall, J.; Barnett, D.; Gouda, M.K.; et al. Detection of Chemotherapy-resistant Pancreatic Cancer Using a Glycan Biomarker, sTRA. Clin. Cancer Res. 2021, 27, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Cho, H.J.; Kang, I.; Choi, S.H.; Lee, S.; Lee, J.-S. Integrative multi-omics profiling of resectable pancreatic cancer reveals clinically relevant molecular subtypes with precision strategies beyond the clinical staging system. Ann. Hepato-Biliary-Pancreat. Surg. 2021, 25, S152. [Google Scholar] [CrossRef]
- Chan-Seng-Yue, M.; Kim, J.C.; Wilson, G.W.; Ng, K.; Figueroa, E.F.; O’Kane, G.M.; Connor, A.A.; Denroche, R.E.; Grant, R.C.; McLeod, J.; et al. Transcription phenotypes of pancreatic cancer are driven by genomic events during tumor evolution. Nat. Genet. 2020, 52, 231–240. [Google Scholar] [CrossRef]
- Janssen, Q.P.; O’Reilly, E.M.; van Eijck, C.H.J.; Groot Koerkamp, B. Neoadjuvant Treatment in Patients with Resectable and Borderline Resectable Pancreatic Cancer. Front. Oncol. 2020, 10, 41. [Google Scholar] [CrossRef]
- Janssen, Q.P.; Buettner, S.; Suker, M.; Beumer, B.R.; Addeo, P.; Bachellier, P.; Bahary, N.; Bekaii-Saab, T.; Bali, M.A.; Besselink, M.G.; et al. Neoadjuvant FOLFIRINOX in Patients with Borderline Resectable Pancreatic Cancer: A Systematic Review and Patient-Level Meta-Analysis. J. Natl. Cancer Inst. 2019, 111, 782–794. [Google Scholar] [CrossRef] [PubMed]
- Strobel, O.; Lorenz, P.; Hinz, U.; Gaida, M.; König, A.-K.; Hank, T.; Niesen, W.; Kaiser, J.; Al-Saeedi, M.; Bergmann, F.; et al. Actual Five-year Survival After Upfront Resection for Pancreatic Ductal Adenocarcinoma. Ann. Surg. 2020. [Google Scholar] [CrossRef]
- Hartwig, W.; Strobel, O.; Hinz, U.; Fritz, S.; Hackert, T.; Roth, C.; Büchler, M.W.; Werner, J. CA19-9 in Potentially Resectable Pancreatic Cancer: Perspective to Adjust Surgical and Perioperative Therapy. Ann. Surg. Oncol. 2013, 20, 2188–2196. [Google Scholar] [CrossRef]
- Bergquist, J.R.; Puig, C.A.; Shubert, C.R.; Groeschl, R.T.; Habermann, E.B.; Kendrick, M.L.; Nagorney, D.M.; Smoot, R.L.; Farnell, M.B.; Truty, M.J. Carbohydrate Antigen 19-9 Elevation in Anatomically Resectable, Early Stage Pancreatic Cancer Is Independently Associated with Decreased Overall Survival and an Indication for Neoadjuvant Therapy: A National Cancer Database Study. J. Am. Coll. Surg. 2016, 223, 52–65. [Google Scholar] [CrossRef]
- Park, S.; Jang, J.K.; Byun, J.H.; Kim, J.H.; Lee, S.S.; Kim, H.J.; Hong, S.B.; Park, S.H. CT in the prediction of margin-negative resection in pancreatic cancer following neoadjuvant treatment: A systematic review and meta-analysis. Eur. Radiol. 2021, 31, 3383–3393. [Google Scholar] [CrossRef]
- Ta, R.; O’Connor, D.B.; Sulistijo, A.; Chung, B.; Conlon, K.C. The Role of Staging Laparoscopy in Resectable and Borderline Resectable Pancreatic Cancer: A Systematic Review and Meta-Analysis. Dig. Surg. 2019, 36, 251–260. [Google Scholar] [CrossRef]
- Truty, M.J.; Kendrick, M.L.; Nagorney, D.M.; Smoot, R.L.; Cleary, S.P.; Graham, R.P.; Goenka, A.H.; Hallemeier, C.L.; Haddock, M.G.; Harmsen, W.S.; et al. Factors Predicting Response, Perioperative Outcomes, and Survival Following Total Neoadjuvant Therapy for Borderline/Locally Advanced Pancreatic Cancer. Ann. Surg. 2021, 273, 341–349. [Google Scholar] [CrossRef]
- Barreto, S.G.; Loveday, B.; Windsor, J.A.; Pandanaboyana, S. Detecting tumour response and predicting resectability after neoadjuvant therapy for borderline resectable and locally advanced pancreatic cancer. ANZ J. Surg. 2019, 89, 481–487. [Google Scholar] [CrossRef]
- Primrose, P.J. NICE Guidelines: Pancreatic cancer in adults: Diagnosis and management. Pancreatology 2020, 20, e3. [Google Scholar] [CrossRef]
- Ghaneh, P.; Hanson, R.; Titman, A.; Lancaster, G.; Plumpton, C.; Lloyd-Williams, H.; Yeo, S.T.; Edwards, R.T.; Johnson, C.; Abu Hilal, M.; et al. PET-PANC: Multicentre prospective diagnostic accuracy and health economic analysis study of the impact of combined modality 18fluorine-2-fluoro-2-deoxy-d-glucose positron emission tomography with computed tomography scanning in the diagnosis and managemen. Health Technol. Assess. 2018, 22, 1–114. [Google Scholar] [CrossRef] [PubMed]
- Tamburrino, D.; Riviere, D.; Yaghoobi, M.; Davidson, B.R.; Gurusamy, K.S. Diagnostic accuracy of different imaging modalities following computed tomography (CT) scanning for assessing the resectability with curative intent in pancreatic and periampullary cancer. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef] [Green Version]
- Stessin, A.M.; Meyer, J.E.; Sherr, D.L. Neoadjuvant Radiation is Associated with Improved Survival in Patients With Resectable Pancreatic Cancer: An Analysis of Data From the Surveillance, Epidemiology, and End Results (SEER) Registry. Int. J. Radiat. Oncol. 2008, 72, 1128–1133. [Google Scholar] [CrossRef]
- Cloyd, J.M.; Chen, H.-C.; Wang, X.; Tzeng, C.-W.D.; Kim, M.P.; Aloia, T.A.; Vauthey, J.-N.; Lee, J.E.; Katz, M.H.G. Chemotherapy vs. Chemoradiation as Preoperative Therapy for Resectable Pancreatic Ductal Adenocarcinoma. Pancreas 2019, 48, 216–222. [Google Scholar] [CrossRef]
- Versteijne, E.; Vogel, J.A.; Besselink, M.G.; Busch, O.R.C.; Wilmink, J.W.; Daams, J.G.; van Eijck, C.H.J.; Groot Koerkamp, B.; Rasch, C.R.N.; van Tienhoven, G. Meta-analysis comparing upfront surgery with neoadjuvant treatment in patients with resectable or borderline resectable pancreatic cancer. Br. J. Surg. 2018, 105, 946–958. [Google Scholar] [CrossRef] [Green Version]
- Van Eijck, C.H.J.; Versteijne, E.; Suker, M.; Groothuis, K.; Besselink, M.G.H.; Busch, O.R.C.; Bonsing, B.A.; Groot Koerkamp, B.; de Hingh, I.H.J.T.; Festen, S.; et al. Preoperative chemoradiotherapy to improve overall survival in pancreatic cancer: Long-term results of the multicenter randomized phase III PREOPANC trial. J. Clin. Oncol. 2021, 39, 4016. [Google Scholar] [CrossRef]
- Versteijne, E.; Suker, M.; Groothuis, K.; Akkermans-Vogelaar, J.M.; Besselink, M.G.; Bonsing, B.A.; Buijsen, J.; Busch, O.R.; Creemers, G.-J.M.; van Dam, R.M.; et al. Preoperative Chemoradiotherapy vs. Immediate Surgery for Resectable and Borderline Resectable Pancreatic Cancer: Results of the Dutch Randomized Phase III PREOPANC Trial. J. Clin. Oncol. 2020, 38, 1763–1773. [Google Scholar] [CrossRef]
- Murphy, J.E.; Wo, J.Y.; Ryan, D.P.; Jiang, W.; Yeap, B.Y.; Drapek, L.C.; Blaszkowsky, L.S.; Kwak, E.L.; Allen, J.N.; Clark, J.W.; et al. Total Neoadjuvant Therapy With FOLFIRINOX Followed by Individualized Chemoradiotherapy for Borderline Resectable Pancreatic Adenocarcinoma. JAMA Oncol. 2018, 4, 963–969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katz, M.H.G.; Shi, Q.; Meyers, J.P.; Herman, J.M.; Choung, M.; Wolpin, B.M.; Ahmad, S.; Marsh, R.d.W.; Schwartz, L.H.; Behr, S.; et al. Alliance A021501: Preoperative mFOLFIRINOX or mFOLFIRINOX plus hypofractionated radiation therapy (RT) for borderline resectable (BR) adenocarcinoma of the pancreas. J. Clin. Oncol. 2021, 39, 377. [Google Scholar] [CrossRef]
- Ghaneh, P.; Palmer, D.H.; Cicconi, S.; Halloran, C.; Psarelli, E.E.; Rawcliffe, C.L.; Sripadam, R.; Mukherjee, S.; Wadsley, J.; Al-Mukhtar, A.; et al. ESPAC-5F: Four-arm, prospective, multicenter, international randomized phase II trial of immediate surgery compared with neoadjuvant gemcitabine plus capecitabine (GEMCAP) or FOLFIRINOX or chemoradiotherapy (CRT) in patients with borderline resectable pan. J. Clin. Oncol. 2020, 38, 4505. [Google Scholar] [CrossRef]
- Conroy, T.; Desseigne, F.; Ychou, M.; Bouché, O.; Guimbaud, R.; Bécouarn, Y.; Adenis, A.; Raoul, J.-L.; Gourgou-Bourgade, S.; de la Fouchardière, C.; et al. FOLFIRINOX versus Gemcitabine for Metastatic Pancreatic Cancer. N. Engl. J. Med. 2011, 364, 1817–1825. [Google Scholar] [CrossRef] [Green Version]
- Suker, M.; Beumer, B.R.; Sadot, E.; Marthey, L.; Faris, J.E.; Mellon, E.A.; El-Rayes, B.F.; Wang-Gillam, A.; Lacy, J.; Hosein, P.J.; et al. FOLFIRINOX for locally advanced pancreatic cancer: A systematic review and patient-level meta-analysis. Lancet Oncol. 2016, 17, 801–810. [Google Scholar] [CrossRef] [Green Version]
- Cascinu, S.; Berardi, R.; Bianco, R.; Bilancia, D.; Zaniboni, A.; Ferrari, D.; Mosconi, S.; Spallanzani, A.; Cavanna, L.; Leo, S.; et al. Nab-paclitaxel/gemcitabine combination is more effective than gemcitabine alone in locally advanced, unresectable pancreatic cancer—A GISCAD phase II randomized trial. Eur. J. Cancer 2021, 148, 422–429. [Google Scholar] [CrossRef]
- Philip, P.A.; Lacy, J.; Portales, F.; Sobrero, A.; Pazo-Cid, R.; Manzano Mozo, J.L.; Kim, E.J.; Dowden, S.; Zakari, A.; Borg, C.; et al. Nab-paclitaxel plus gemcitabine in patients with locally advanced pancreatic cancer (LAPACT): A multicentre, open-label phase 2 study. Lancet Gastroenterol. Hepatol. 2020, 5, 285–294. [Google Scholar] [CrossRef]
- Williet, N.; Petrillo, A.; Roth, G.; Ghidini, M.; Petrova, M.; Forestier, J.; Lopez, A.; Thoor, A.; Weislinger, L.; De Vita, F.; et al. Gemcitabine/Nab-Paclitaxel versus FOLFIRINOX in Locally Advanced Pancreatic Cancer: A European Multicenter Study. Cancers 2021, 13, 2797. [Google Scholar] [CrossRef]
- Ozaka, M.; Ueno, M.; Ishii, H.; Mizusawa, J.; Katayama, H.; Kataoka, T.; Okusaka, T.; Ikeda, M.; Miwa, H.; Kaneko, S.; et al. Randomized phase II study of modified FOLFIRINOX vs. gemcitabine plus nab-paclitaxel combination therapy for locally advanced pancreatic cancer (JCOG1407). J. Clin. Oncol. 2021, 39, 4017. [Google Scholar] [CrossRef]
- Reni, M.; Balzano, G.; Zanon, S.; Zerbi, A.; Rimassa, L.; Castoldi, R.; Pinelli, D.; Mosconi, S.; Doglioni, C.; Chiaravalli, M.; et al. Safety and efficacy of preoperative or postoperative chemotherapy for resectable pancreatic adenocarcinoma (PACT-15): A randomised, open-label, phase 2–3 trial. Lancet Gastroenterol. Hepatol. 2018, 3, 413–423. [Google Scholar] [CrossRef]
- Ahmad, S.A.; Duong, M.; Sohal, D.P.S.; Gandhi, N.S.; Beg, M.S.; Wang-Gillam, A.; Wade, J.L.; Chiorean, E.G.; Guthrie, K.A.; Lowy, A.M.; et al. Surgical Outcome Results From SWOG S1505. Ann. Surg. 2020, 272, 481–486. [Google Scholar] [CrossRef]
- Sohal, D.; McDonough, S.; Ahmad, S.A.; Gandhi, N.; Beg, M.S.; Wang-Gillam, A.; Wade, J.L.; Guthrie, K.A.; Lowy, A.M.; Philip, P.A.; et al. SWOG S1505: Initial findings on eligibility and neoadjuvant chemotherapy experience with mfolfirinox vs. gemcitabine/nab-paclitaxel for resectable pancreatic adenocarcinoma. J. Clin. Oncol. 2019, 37, 414. [Google Scholar] [CrossRef]
- O’Kane, G.M.; Grünwald, B.T.; Jang, G.-H.; Masoomian, M.; Picardo, S.; Grant, R.C.; Denroche, R.E.; Zhang, A.; Wang, Y.; Lam, B.; et al. GATA6 Expression Distinguishes Classical and Basal-like Subtypes in Advanced Pancreatic Cancer. Clin. Cancer Res. 2020, 26, 4901–4910. [Google Scholar] [CrossRef] [Green Version]
- A Phase 0, Pre-Operative, Window-of-Opportunity Study to Assess Gene Expression in Patients with Resectable, Locally Advanced, or Metastatic Pancreatic Cancer (NEOPANC-01). Available online: https://pancreaticcancercanada.ca/press-release-neopancone-clinical-trial-launch/ (accessed on 21 June 2021).
- Klein, A.P. Pancreatic cancer epidemiology: Understanding the role of lifestyle and inherited risk factors. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 493–502. [Google Scholar] [CrossRef]
- Golan, T.; Barenboim, A.; Lahat, G.; Nachmany, I.; Goykhman, Y.; Shacham-Shmueli, E.; Halpern, N.; Brazowski, E.; Geva, R.; Wolf, I.; et al. Increased Rate of Complete Pathologic Response After Neoadjuvant FOLFIRINOX for BRCA Mutation Carriers with Borderline Resectable Pancreatic Cancer. Ann. Surg. Oncol. 2020, 27, 3963–3970. [Google Scholar] [CrossRef]
- Ramnaraign, B.H.; Hughes, S.J.; Hitchcock, K.; Lee, J.-H.; Rogers, S.C.; Fan, Z.H.; Allegra, C.J.; Trevino, J.G.; El-Far, A.; Russell, K.B.; et al. A phase II, open-label pilot study evaluating the safety and activity of liposomal irinotecan (Nal-IRI) in combination with 5-FU and oxaliplatin (NALIRIFOX) in preoperative treatment of pancreatic adenocarcinoma (NEO-Nal-IRI Study). J. Clin. Oncol. 2021, 39, TPS446. [Google Scholar] [CrossRef]
- Wang-Gillam, A.; Li, C.-P.; Bodoky, G.; Dean, A.; Shan, Y.-S.; Jameson, G.; Macarulla, T.; Lee, K.-H.; Cunningham, D.; Blanc, J.F.; et al. Nanoliposomal irinotecan with fluorouracil and folinic acid in metastatic pancreatic cancer after previous gemcitabine-based therapy (NAPOLI-1): A global, randomised, open-label, phase 3 trial. Lancet 2016, 387, 545–557. [Google Scholar] [CrossRef]
- Pompella, L.; Tirino, G.; Pappalardo, A.; Caterino, M.; Ventriglia, A.; Nacca, V.; Orditura, M.; Ciardiello, F.; De Vita, F. Pancreatic Cancer Molecular Classifications: From Bulk Genomics to Single Cell Analysis. Int. J. Mol. Sci. 2020, 21, 2814. [Google Scholar] [CrossRef] [Green Version]
- Hewitt, D.B.; Nissen, N.; Hatoum, H.; Musher, B.; Seng, J.; Coveler, A.L.; Al-Rajabi, R.; Yeo, C.J.; Leiby, B.; Banks, J.; et al. A Phase 3 Randomized Clinical Trial of Chemotherapy With or Without Algenpantucel-L (HyperAcute-Pancreas) Immunotherapy in Subjects with Borderline Resectable or Locally Advanced Unresectable Pancreatic Cancer. Ann. Surg. 2020. [Google Scholar] [CrossRef]
- Berg, G.; Rybakova, D.; Fischer, D.; Cernava, T.; Vergès, M.-C.C.; Charles, T.; Chen, X.; Cocolin, L.; Eversole, K.; Corral, G.H.; et al. Microbiome definition revisited: Old concepts and new challenges. Microbiome 2020, 8, 103. [Google Scholar] [CrossRef]
- Goodman, B.; Gardner, H. The microbiome and cancer. J. Pathol. 2018, 244, 667–676. [Google Scholar] [CrossRef] [Green Version]
- Abdul Rahman, R.; Lamarca, A.; Hubner, R.A.; Valle, J.W.; McNamara, M.G. The Microbiome as a Potential Target for Therapeutic Manipulation in Pancreatic Cancer. Cancers 2021, 13, 3779. [Google Scholar] [CrossRef] [PubMed]
- Riquelme, E.; Zhang, Y.; Zhang, L.; Montiel, M.; Zoltan, M.; Dong, W.; Quesada, P.; Sahin, I.; Chandra, V.; San Lucas, A.; et al. Tumor Microbiome Diversity and Composition Influence Pancreatic Cancer Outcomes. Cell 2019, 178, 795–806.e12. [Google Scholar] [CrossRef]
- Mohindroo, C.; Rogers, J.E.; Hasanov, M.; Mizrahi, J.; Overman, M.J.; Varadhachary, G.R.; Wolff, R.A.; Javle, M.M.; Fogelman, D.R.; Pant, S.; et al. A retrospective analysis of antibiotics usage and effect on overall survival and progressive free survival in patients with metastatic pancreatic cancer. J. Clin. Oncol. 2019, 37, e15781. [Google Scholar] [CrossRef]
- Hasanov, M.; Mohindroo, C.; Rogers, J.; Prakash, L.; Overman, M.J.; Varadhachary, G.R.; Wolff, R.A.; Javle, M.M.; Fogelman, D.R.; Pant, S.; et al. The effect of antibiotic use on survival of patients with resected pancreatic ductal adenocarcinoma. J. Clin. Oncol. 2019, 37, e15773. [Google Scholar] [CrossRef]
- Goel, N.; Nadler, A.; Reddy, S.; Hoffman, J.P.; Pitt, H.A. Biliary microbiome in pancreatic cancer: Alterations with neoadjuvant therapy. HPB 2019, 21, 1753–1760. [Google Scholar] [CrossRef]
- Nadeem, S.O.; Jajja, M.R.; Maxwell, D.W.; Pouch, S.M.; Sarmiento, J.M. Neoadjuvant chemotherapy for pancreatic cancer and changes in the biliary microbiome. Am. J. Surg. 2021, 222, 3–7. [Google Scholar] [CrossRef]
| Guidelines | Resectable | Borderline Resectable | Locally Advanced |
|---|---|---|---|
| NCCN [10] | No tumor contact: CA, SMA, CHA, SMV, or PV, or ≤180° contact without vein contour irregularity | Contact with SMV or PV of >180° or contact ≤180° with thrombosis of the vein with suitable vessel proximal and distal to the affected site. Contact with IVC. Pancreatic head/uncinate process: tumor contact with CHA without extension to CA or HA bifurcation. Contact with SMA of ≤180°. Pancreatic body/tail: contact with the CA of ≤180°, contact > 180° without involvement of the aorta and with intact, uninvolved gastroduodenal artery. | SMV/PV that cannot be reconstructed due to tumor involvement or vessel occlusion due to thrombus or tumor. Pancreatic head/uncinate process: contact with SMA >180°, contact with the CA of > 180°. Pancreatic body/tail: contact >180 ° with SMA or CA, contact with the CA and aortic involvement. |
| IAP Consensus Definition [11] | No tumor contact SMV, PV, SMA, CA, CHA | Tumor contact ≥180° with SMV/PV or bilateral narrowing/occlusion, not exceeding the inferior border of the duodenum with no tumor contact with SMA, CA, or CHA. Tumor contact of <180° with SMA, CA but without showing deformity/stenosis. Tumor contact with CHA without tumor contact of the PHA and/or CA. Biological criteria: CA19-9 > 500 IU/mL, regional lymph node metastasis on biopsy or PET-CT. Conditional criterion: PS ≥ 2. | SMV/PV: bilateral narrowing/occlusion, beyond the inferior border of the duodenum. Tumor contact/invasion with SMA, CA of ≥180°. CHA: tumor contact/invasion showing tumor contact/invasion of the PHA and/or CA. Tumor contact or invasion of aorta. |
| Study | Population | N | Comparators | Primary Endpoint | Other Outcomes |
|---|---|---|---|---|---|
| ESPAC-1 [22,23] | R0 or R1 resection | 541 | CRT: 20 Gy tumor dose in ten daily fractions over 2 weeks with 500 mg/m2 5-FU IV bolus d 1–3, repeated after a planned break of 2 weeks. CT: IV bolus FA 20 mg/m2 followed by IV bolus 5-FU 425 mg/m2 d 1–5 every 28 d for six cycles. | mOS: 15.5 mo for CRT vs. 16.1 mo for no CRT, p = 0.24 mOS: 19.7 mo for CT vs. 14.0 for no CT, p = 0.0005 | 5-year survival: 10% CRT vs. 20% no CRT, p = 0.05 5-year survival: 21% CT vs. 8% no CT, p = 0.009 |
| CONKO-001 [24,25] | KPS ≥ 50% R0 or R1 resection Post-operative CEA/CA19-9 > 2.5 times ULN were excluded | 368 | Gem: 1 g/m2 d 1, 8, and 15 IV every 4 weeks for 6 mo (A) vs. Obs: (B). | DFS: 13.4 mo (A) vs. 6.7 mo (B), p < 0.001 | mOS: 22.8 mo (A) vs. 20.2 mo (B), p = 0.01 5- and 10-year survival: 20.7% and 12.2% (A) vs. 10.4% and 7.7% (B) 5- and 10-year DFS: 16.6% and 14.3% (A) vs. 7.0% and 5.8% (B) |
| ESPAC-3 [26] | WHO PS ≤ 2, R0 or R1 resection | 1149 | 5-FU+FA: FA, 20 mg/m2, IV bolus, followed by 5-FU, 425 mg/m2 IV bolus d 1–5 every 28 d (A) vs. Gem: 1 g/m2 d 1, 8, and 15 IV every 4 weeks for 6 mo (B). | mOS: 23 mo (A) vs. 23.6 mo (B), p = 0.39 | DFS: 14.1 mo (A) vs. 14.3 mo (B) p = 0.53 1- and 2-year survival: 78.5% and 48.1% (A) vs. 80.1% and 49.1% (B) |
| ESPAC-4 [27,28] | WHO PS ≤ 2, R0 or R1 resection | 732 | Gem: 1 g/m2 d 1, 8, and 15 IV every 4 weeks for 6 mo (A) vs. Gem+Cap: Gem with Cap orally for 21 days followed by 7 days’ rest for 6 mo at a daily dose of 1660 mg/m2. | mOS: 25.2 mo (A) vs. 28.0 mo (B), p = 0.032 | RFS: 13.1 mo (A) vs. 13.9 (B), p = 0.082 3-year RFS: 20.9% (A) vs. 23.8% (B) 5-year RFS: 11.9% (A) vs. 18.6% (B) 5-year survival: 20.0% (A) vs. 28.0% (B), p = 0.049 |
| PRODIGE-24 [18] | WHO PS ≤ 1 R0 or R1 resection Post-operative CA-19.9 ≤ 180 U/mL | 493 | Gem: 1 g/m2 d 1, 8, and 15 IV every 4 weeks for 6 mo (A) vs. mFOLFIRINOX: oxaliplatin 85 mg/m2, irinotecan 150 mg/m2, leucovorin 400 mg/m2, and 5-FU 2400 mg/m2 every 2 weeks (B). | DFS: 12.8 mo (A) vs. 21.6 mo (B), p < 0.001 | mOS: 35.0 mo (A) vs. 54.4 mo (B), p = 0.003 3-year survival: 48.6% (A) vs. 63.4% (B) 1-, 2-, and 3-year DFS: 53.7%, 30.7%, 21.4% (A) vs. 69.0%, 47.0%, 39.7% (B) MFS: 17.7 mo (A) vs. 30.4 mo (B), p < 0.001 |
| APACT [20,21] | WHO R0 or R1 resection Post-operative CA-19.9 < 100 U/mL | 866 | Gem: 1 g/m2 d 1, 8, and 15 IV every 4 weeks for 6 mo (A) vs. Gem/Nab-Paclitaxel: Gem with Nab-Paclitaxel 125 mg/m2 d 1, 8, and 15 IV every 4 weeks (B). | DFS: 18.8 mo (A) vs. 19.4 mo (B), p = 0.182 | mOS: 37.7 mo (A) vs. 41.8 mo (B), p = 0.0091 5-year OS: 31% (A) vs. 38% (B) |
| JASPAC-01 [29] | WHO PS ≤ 1 R0 or R1 resection | 385 | Gem: 1 g/m2 d 1, 8, and 15 IV every 4 weeks for 6 mo (A) vs. S1: 40, 50, or 60 mg depending on BSA, orally for 28 d followed by a 14 d rest, every 6 weeks for up to 4 cycles. | mOS: 25.5 mo (A) vs. 46.5 mo (B), pnon-inferiority < 0.0001, p < 0.0001 for superiority | 3- and 5-year OS: 38.8% and 24.4% (A) vs. 59.7 and 44.1% (B) RFS: 11.3 mo (A) vs. 22.9 mo, p < 0.0001 |
| Study Name (NCT Number) | Country | Phase | Population | N | Treatment | Primary Endpoint | Secondary Endpoints | Reference |
|---|---|---|---|---|---|---|---|---|
| PREOPANC-1 (NCT04927780) | The Netherlands | III R | Resectable/borderline resectable | 246 | Gemcitabine + RT → surgery → gemcitabine (A) vs. surgery → gemcitabine (B) | mOS 15.7 mo (A) vs. 14.3 mo (B), p = 0.025 | Resection rate 61% (A) vs. 72% (B), p = 0.058 R0 resection rate 72% (A) vs. 43% (B), p < 0.001 | [72,73] |
| FOLFIRINOX + RT for PDAC (NCT01591733) | USA | II | Borderline resectable | 48 | FOLFIRINOX → capecitabine + RT | R0 resection rate 65% (95% CI 49–78) | mPFS 14.7 mo mOS 37.7 mo | [74] |
| Alliance A021501 (NCT02839343) | USA | II R | Borderline resectable | 126 | FOLFIRINOX (A) vs. FOLFIRINOX → SBRT (B) | 18-mo OS 67.9 (A) vs. 47.3% (B) | pts with pancreatectomy 18 mo OS 93.1 (A) vs. 78.9% (B) mOS 31.0 vs. 17.1 mo | [75] |
| ESPAC5F (CTI89500674) | UK | II R | Borderline resectable | 90 | Surgery → Gem/Cap (A) vs. Gem/Cap or FOLFIRINOX or CRT → surgery → Chemotherapy (B) | Resection rate 62% (A) vs. 55% (B), p = 0.668 | R0 resection rate 15% (A) vs. 23% (B), p = 0.721 1-year survival: 42% (A) vs. 77% (B), p < 0.001 | [76] |
| Study Name (NCT Number) | Country | Phase | Selected Population | N | Treatment | Primary Endpoint | Secondary Endpoints | Reference |
|---|---|---|---|---|---|---|---|---|
| GAP (NCT02043730) | Italy | II R | Locally advanced unresectable | 124 | Nab-paclitaxel + gemcitabine (A) vs. gemcitabine (B) | PDR3 25.4 (A) vs. 45.6% (B), p = 0.01 PDR6 20.8 (A) vs. 35.6% (B) | RR 27 (A) vs. 5.3% (B) mPFS 7 mo (A) vs. 4 mo (B) mOS 12.7 (A) vs. 10.6 mo (B) | [79] |
| LAPACT (NCT02301143) | Western | II | Locally advanced | 107 | Nab-paclitaxel + gemcitabine | mTTF 9.0 mo (90% CI 7.3–10.1) | mPFS 10.9 mo mOS 18.8 mo DCR 77.6% Resection in 17 (16%) | [80] |
| JCOG1407 (jRCTs031180085) | Japan | II R | Locally advanced | 126 | FOLFIRINOX (A) vs. nab-paclitaxel + gemcitabine (B) | 1 y OS 77.4 (A) vs. 82.5% (B) 2 y OS 48.2 (A) vs. 39.7% (B) | mOS 2 y (A) vs. 1.8 y (B) PFS 1 y 47.5 (A) vs. 40.2% (B) MFS 1 y 64.2 (A) vs. 57.3% (B) RR 30.9 (A) vs. 41.4% (B) | [82] |
| Study Name (NCT Number) | Country | Phase | Selected Population | N | Drugs | Primary Endpoint | Secondary Endpoints |
|---|---|---|---|---|---|---|---|
| NCT03983057 | China | III R | Locally advanced/borderline resectable | 830 | mFOLFIRINOX vs. mFOLFIRINOX + anti-PD-1 Ab | PFS | RR R0 rate ORR DCR OS AEs CA 19.9 EORTC QLQ-PAN26 score |
| NCT03161379 | USA | II | Locally advanced | 30 | GVAX vaccine + cyclophosphamide + nivolumab + SBRT | CD8 count in tumor microenvironment | pCR rate |
| NCT02305186 | USA | Ib/II R | Resectable/borderline resectable | 68 | Pembrolizumab + capecitabine-RT vs. capecitabine-RT | TILs per HPF in resected tissue DLTs | DFS OS RR |
| NCT04327986 | USA | I/II | Borderline resectable/locally advanced unresectable | 126 | Arm 1: M9241 (immunocytokine) + M7824 (ICI) Arm 2: M9241 + M7824-SBRT Arm 3: M7824 + M9241-SBRT | BOR | RP2D |
| NCT03970252 | USA | I/II | Borderline resectable | 36 | mFOLFIRINOX + nivolumab | Clinically relevant pancreatic fistula in post-operative period | pCR rate |
| NCT03373188 | USA | I R | Resectable stage I–III | 32 | Surgery vs. VX15/2503 (anti-SEMA4D) vs. VX15/2503 + ipilimumab vs. VX15/2503 + nivolumab | CD8 T cell infiltration | AEs |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khakoo, S.; Petrillo, A.; Salati, M.; Muhith, A.; Evangelista, J.; Seghezzi, S.; Petrelli, F.; Tomasello, G.; Ghidini, M. Neoadjuvant Treatment for Pancreatic Adenocarcinoma: A False Promise or an Opportunity to Improve Outcome? Cancers 2021, 13, 4396. https://doi.org/10.3390/cancers13174396
Khakoo S, Petrillo A, Salati M, Muhith A, Evangelista J, Seghezzi S, Petrelli F, Tomasello G, Ghidini M. Neoadjuvant Treatment for Pancreatic Adenocarcinoma: A False Promise or an Opportunity to Improve Outcome? Cancers. 2021; 13(17):4396. https://doi.org/10.3390/cancers13174396
Chicago/Turabian StyleKhakoo, Shelize, Angelica Petrillo, Massimiliano Salati, Abdul Muhith, Jessica Evangelista, Silvia Seghezzi, Fausto Petrelli, Gianluca Tomasello, and Michele Ghidini. 2021. "Neoadjuvant Treatment for Pancreatic Adenocarcinoma: A False Promise or an Opportunity to Improve Outcome?" Cancers 13, no. 17: 4396. https://doi.org/10.3390/cancers13174396
APA StyleKhakoo, S., Petrillo, A., Salati, M., Muhith, A., Evangelista, J., Seghezzi, S., Petrelli, F., Tomasello, G., & Ghidini, M. (2021). Neoadjuvant Treatment for Pancreatic Adenocarcinoma: A False Promise or an Opportunity to Improve Outcome? Cancers, 13(17), 4396. https://doi.org/10.3390/cancers13174396







